3/2023 THE TIGHTROPE WALKER A perspective on Dry Eye Disease, from the first recognition to the most recent observations SPOTLIGHT ON THE EXPERT Cosimo Mazzotta INNOVATIONS The Innovation of Simplicity NIGHTMARE CASES Better Late Than Never ITALIAN NEWS MAGAZINE FOR EYE SPECIALISTS FGE S.r.l.-Reg. Rivelle 7/F - 14050 Moasca (AT) - Editorial board: Strada 4 Milano Fiori, Palazzo Q7 – 20089 Rozzano (MI) - Year IV - N. 3/2022 - Quaterly publication YEAR V
Editorial Staff:
Timothy Norris
Laura Gaspari, MA
redazione@eyeseenews.it www.eyeseenews.it
Advertisement info@fgeditore.it Phone +39 01411706694
Editor-in-chief
Ferdinando Fabiano f.fabiano@fgeditore.it
Graphics and Layout

Cristiano Guenzi
English Language Copy Editor
Jeremy Paul Norris
Cover Silvia Schiavon
Scientific coordination
Vittorio Picardo, MD
Collaborators:
Chiara Mazzoni
Participants to the current issue:
Pasquale Aragona, MD
Stefano Barabino, MD, PhD
José Manuel Benítez Del Castillo, MD, PhD
Roberto Carassa, MD
Giuseppe Catanuto, MD
Francesco Cutrupi, MD
Antonio Di Zazzo, MD
Emanuele Erroi, MD
Matteo Forlini, MD
Cosimo Mazzotta, MD, PhD
Rita Mencucci, MD
Stefano Miglior, MD, PhD
Ken K. Nischal, MD, FRCOphth
Olga Prenat
Luciano Quaranta, MD, PhD
Luca Rossetti, MD
Giuseppe Trabucchi, MD
Aldo Vagge, MD, PhD
Luca Vigo, MD
Edoardo Villani, MD
Tea Zeppola, MD
Editor
FGE srl – Fabiano Gruppo Editoriale
Editorial Board: Strada 4 Milano Fiori, Palazzo Q7 – 20089 Rozzano (MI)
Registered Office: Regione Rivelle, 7 14050 Moasca (AT)
Phone +39 0141/1706694
Fax +39 0141/856013
Registration at the Court of Asti n. 1/2020 del 05/02/2020
1 Contents editorial Cover story THE TIGHTROPE WALKER spotlight on the expert A PROFESSIONAL VOW innovation THE INNOVATION OF SIMPLICITY nightmare Cases BETTER LATE THAN NEVER Flash news insight THE DIALOGUE BETWEEN SCIENCE AND POLITICS NOT JUST A PEDIATRIC DISEASE EVERYONE HAS THEIR OWN VISCOELASTIC AN OPTIMAL SOLUTION AGAINST DRY EYE DRY EYE IN WOMEN optiCs MYOPIA MANAGEMENT: ESSILORLUXOTTICA AND WSPOS TOGETHER TO RAISE AWARENESS industry news
3/2023 THE TIGHTROPE WALKER A perspective on Dry Eye Disease, from the first recognition to the most recent observations SPOTLIGHT ON THE EXPERT INNOVATIONS The Innovation of Simplicity NIGHTMARE CASES ITALIAN NEWS MAGAZINE FOR EYE SPECIALISTS YEAR V 12 4 2 24 22 18 28 38 36 32 40 44 46
Copy
Free
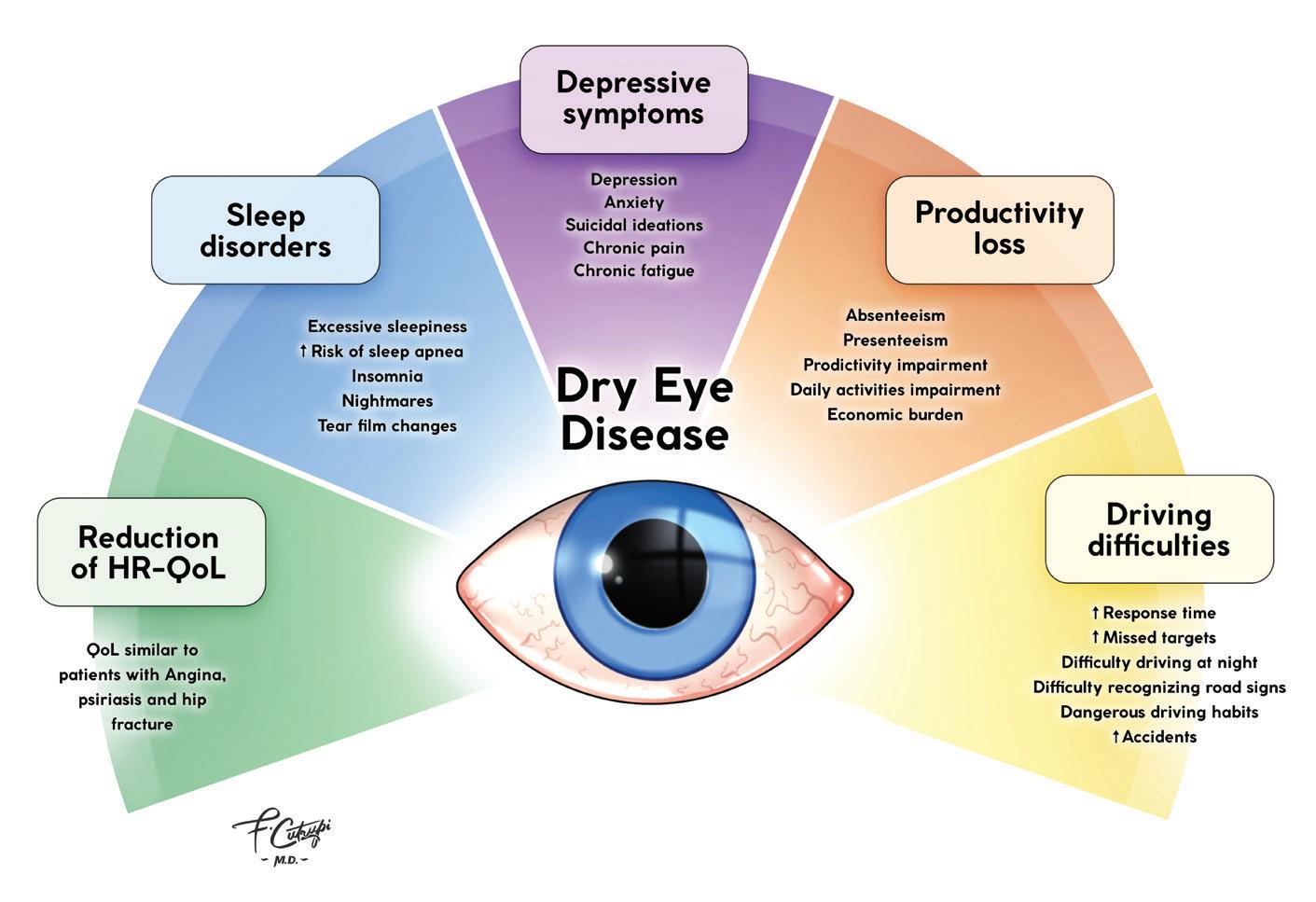
GETTING TO KNOW THE DRY EYE
By Professor Pasquale Aragona, University of Messina
As we know, the ocular surface system is composed of a set of glands which participate in the production and distribution of the tear film on the anterior surface of the eye: namely the cornea and the conjunctiva. Among these glands we have the main lacrimal glands and the accessory lacrimal glands, the conjunctival goblet cells, and the Meibomian glands, located in the palpebral tarsus. The secretory activity of these glands is finely organised thanks to the control exercised by the nervous system, the endocrine system (activated by sexual hormones and above all, testosterone, which has a trophic effect on the glands), and the immune system, which regulates the inflammatory response and the reaction to potentially infectious agents.
A series of factors and events, which can be both intrinsic and external to the organism, can lead to a condition of altered functionality in the production of tear film. This can trigger a vicious cycle which tends to self-maintain because of the alterations occurring on the ocular surface system: the universally recognised dry eye disease. Tear film instability, which frequently results from an altered lipid production of the Meibomian glands, constitutes the primum movens of the insult to the ocular surface system. The consequence is a hyperosmolarity of the tear film that leads to epithelial cell stress which, together with the altered tear film inability to contrast the oxidative stress, causes the epithelial cells to activate two responsive mechanisms: the apoptosis and protracted cellular stress which triggers the inflammatory mechanisms. This is possible due to the production of pro-inflammatory substances that maintain the harmful stimulus and lead to a state of chronic suffering. These steps occur whatever the pathogenic noxa responsible for the original damage and respond to two fundamental mechanisms: reduced production or increased evaporation of tears. These two pathogenetic mechanisms coexist and it is clinically impossible to determine in the acute phases of the disease which mechanism originated the problem.
Professor Pasquale Aragona
What are the steps to take when we see a patient with potential dry eye disease?

2 C Editorial
Tutte le interviste contenute in questo numero sono consultabili collegandosi al sito: www.eyeseenews.it
An accurate diagnosis is crucial and can be achieved with simple means based on clinical analysis generally available in any eye clinic. In addition to a complete medical and family history, it is important to collect information on the timeline of the symptoms’ manifestation. The symptoms which tend to manifest upon waking indicate a suffering linked to eyelid problems caused by Meibomian gland dysfunction or to Floppy Eyelid Syndrome. Whereas in the disease caused by reduced production of tear film, symptoms tend to manifest later during the day and also during the night in some cases.
It is also possible to use validated questionnaires grading the severity of dry eye disease, such as the Ocular Surface Disease Index (OSDI), or the Symptom Assessment Questionnaire in Dry Eye (SANDE). The next step is the observation at the slit lamp of some structures of the ocular surface system, including tear meniscus height, eyelid margin, tear film characteristics, presence of debris, undissolved mucus, or foamy secretions. It is therefore fundamental to evaluate the entity of conjunctival hyperaemia which occurs as a consequence of inflammation, and is a sign of discomfort often reported by patients and a source of sometime improper questions from others. Clinical investigation continues with fluorescein staining and Wood’s Lamp examination, preferably with a yellow filter. Staining allows the physician to evaluate tear film sta-
bility or break-up time (BUT): the general index of tear film condition. Three minutes after the examination, staining of the epithelium of the ocular surface can be evaluated to verify its condition. Moreover, lissamine green staining allows us to identify the areas where the glycocalyx barrier has collapsed, thus highlighting those cells that are under inflammatory stress.
Tear clearance is another important test as it indicates how much time toxic tears caused by the presence of pro-inflammatory cytokines remain on the ocular surface. At the end of this diagnostic procedure, the squeezing of the excretory ducts of the Meibomian glands can be performed to evaluate the type of secretion: a transparent secretion indicates a good condition of the glands, while a cloudy, thick, toothpaste-like secretion or no secretion indicate an increasing level of MGD. Through this process, it is possible to achieve a fairly accurate diagnosis of dry eye disease and to assess the degree of severity and impact on the health status of the overall ocular surface.
There are other, more refined diagnostic tests that can be used to evaluate in detail the different structures that compose the ocular surface system, but these can only be found in specialised clinics. They allow us to better quantify the severity of the disease and to choose the most appropriate therapy to answer our patients’ need for a better quality of life.
3
An accurate diagnosis is crucial and can be achieved with simple means based on clinical analysis generally available in any eye clinic.
Pasquale Aragona
THE TIGHTROPE WALKER
A perspective on Dry Eye Disease, from the first recognition to the most recent observations

Although dry eye was always there to afflict humanity, only recently humanity started to really understand how dry eye works. At the time of the first attempts of treating dry eye with honey, herbs, spices, even chemical compresses or lacrimal gland incisions, and the many observations of Hippocrates and Aulo Aurelio Celso, this condition did not even have a name per se. What we now call Dry Eye Disease (DED) was for many years considered as a part of the wide set of ocular surface conditions called xerophthalmia, a term that now indicates one single very different and known condition. In fact, many centuries
went by before Dry Eye was recognized as a unique disease among the many disorders of the ocular surface. Nonetheless, despite the many and many steps forward made in recent years, DED is still a widely underestimated disease both in causes and complications. “On an international level, the first definition of Dry Eye was presented by Mike Lemp in the National Eye Institute/Industry Workshop in ‘95”, said José Manuel Benítez Del Castillo. “It was not defined as a disease, but as an alteration, a disorder regarding tear production only.”
José Manuel Benítez Del Castillo,
4 A Cover Story
Interview with José Manuel Benítez Del Castillo, San Carlos Hospital of Madrid, University Complutense of Madrid; and Stefano Barabino, L. Sacco Hospital of Milan, University of Milan
The ocular surface is a bit like a man walking on a tightrope, in a sometimes very precarious balance.
by Timothy Norris
José
Benítez
and took part in the TFOS Dry Eye Workshop II (DEWS II) in the Management and Therapy Subcommittee.
“In 2007 we had our first TFOS DEWS, that actually changed things quite a bit with a new definition of DED as a condition that not
only affects tear production, but the ocular surface as a whole”, he added.
MD, PhD, is Director of the Ocular Surface and Inflammation Unit at the San Carlos Hospital of Madrid and Professor and Chairman of the Faculty of Medicine and Ophthalmology at the University Complutense of Madrid. He is an internationally renowned expert of ocular surface, ➧
From alteration to condition, a further step was still necessary. “The definition of ocular surface as a system, as described by Richard A. Thoft e Judith Friend for the first

5
On an international level, the first definition of Dry Eye was presented by Mike Lemp in the National Eye Institute/Industry Workshop in ‘95. It was not defined as a disease, but as an alteration, a disorder regarding tear production only
Manuel
Del Castillo
José Manuel Benítez Del Castillo, MD, PhD, is Director of the Ocular Surface and Inflammation Unit at the San Carlos University Hospital in Madrid and Professor and Director of the Faculty of Medicine and Ophthalmology at the Complutense University of Madrid. An international ocular surface expert, Benitez del Castillo served on the TFOS DEWS II Management and Treatment subcommittee.
time, was really a necessary step,”
Stefano Barabino MD, PhD, said. “In 2017 things were already on the verge of change and we were all starting to realise how the definition of Dry Eye as a condition was limiting, at best”.
Stefano Barabino is Professor of Ophthalmology at the University of Milan and Director of the Centre of Ocular Surface and Dry Eye at the L. Sacco Hospital of Milan.

“We were talking about pathogenesis, osmolarity, inflammation and, most importantly, of neurosensory alterations. All these aspects were later gathered in the new definition of Dry Eye Disease published by the TFOS DEWS II in the same year,” Barabino said.
THE WATERSHED
Undoubtedly an important milestone for the anterior segment, the new DEWS II definition was still just a child of its time. “The real change really started at the end of the nineties, with the introduction on the market of topical cyclosporine. This has set in motion the study of the role and the process of inflammation in DED, leading to the new understanding that dry eye was not only a matter of lack of tear production, but involved a far more complex process in which inflammation plays a primary role,” Barabino said. “The investigation of this specific pathogenetic aspect was what later led to the most recent definition of the disease.”
In 2021, with a group of Italian experts, Stefano Barabino added the concept of homeostasis of the ocular surface to the definition of DEWS II, and loss of homeostasis was included amongst the pathogenetic factors of DED. According to Barabino, this was one of the last accomplishments in the understanding of the pathogenesis of DED, especially regarding inflammation. Both research and development are now more focused on the improvement of existing therapies. “From the point of view of managing inflammation, we are still relying on cyclosporine, which now comes in different formulations. We did clarify which steroid is better for the ocular surface,
6 Cover Story
This has set in motion the study of the role and the process of inflammation in DED, leading to the new understanding that dry eye was not only a matter of lack of tear production, but involved a far more complex process in which inflammation plays a primary role
Stefano Barabino
Stefano Barabino, MD, PhD, is Professor at the School of Specialization in Ophthalmology at the University of Milan and Head of the Ocular Surface and Dry Eye Center at the L. Sacco Hospital in Milan.
and there is now a new molecule called lifitegrast that blocks T cell movement in the tissues of the ocular surface, leading to effective control of inflammation, as confirmed by recent studies. However, this product is not yet available in the European market.”
From the perspective of Meibomian gland treatments, many options are now available. “We have new devices for the treatment of evaporative dry eye, including IPL, Jett Plasma, Rexon-Eye, and devices providing ultrasound or thermal gland heating and expression, such as LipiFlow o MiBoFlo,” Benítez del Castillo explained. “However, if these new instruments can effectively address evaporative dry eye, for aqueous deficient DED the only weapons we have are cyclosporine and corticosteroids,” he noted.
STEPS FORWARD IN MUCIN DEFICIENT DED
The key role of mucins in the stability and quality of tear film, and how an alteration of the goblet cells (GSc) can lead to the development of ocular surface disorders as DED, has been recently clarified by international researchers.
“In Asia, and especially in Japan, thanks to the efforts of the Asian Dry Eye Society, Dry Eye is now divided not only in evaporative and aqueous deficient,” Benítez del Castillo explained. “They now consider reduced wettability caused by the lack of mucin in the tear film, as a third type of dry eye.”
According to Benítez del Castillo, the use of new mucin secretagogue drugs could soon be a valid option for the physician. “The
same drug company that distributes cyclosporine in Europe also distributes diquafosol, a mucin secretagogue that we are looking forward to using. Another company is now producing a similar compound called rebamipide. None of the above are available right now on the European market, but with a bit of luck we could have some good news soon.”
THE MDR PARADIGM AND THE NEW GENERATION OF ARTIFICIAL TEARS
The 26th of May 2021 was officially the date of implementation for the new EU Medical Device Regulation (MDR), that replaced the previous MDD and AIMDD. From its first implementation in May 2017, the MDR immediately imposed a positive change for the treatment of DED, introducing new and better safety and quality standards, especially related to artificial tears. “Things sensibly changed in the last year,” Barabino said. “Before the MDR was introduced, if you wanted to place a new eye drop on the market, the only thing you
the new product,” he said.
A highly praised precaution, especially in the aftermath of the tragic events related to the distribution of contaminated eye drops in the US. “With the MDR, it is even harder than before to import a product that does not meet very strict safety standards,” Barabino said. “This is a great advantage of living in the European Union, because we are protected from dreadful scenarios like the one that recently shocked the United States,” he added.
“There are pros and cons in this regard,” said Benítez del Castillo. “Providing a patient that needs to be protected with higher safety standards is the positive side. On the other hand, meeting these higher standards is going to be a burden and a cost for the manufacturing companies.” This still represents a positive outcome, according to Barabino, especially for a crowded market like Italy. “Everything was so unregulated before, with more than three hundred different kinds of eye drops sitting on the market at the same time,” Barabino noted. “Many of these products will eventually disappear and be replaced by better and higher quality artificial tears. This is positive for us,” he added.
needed to do was to pass a Draize test on a rabbit. Now we need to meet standards almost comparable to the approval of a new drug both in terms of safety and quality. Clinical studies are needed, along with a technical dossier to guarantee the safety profile of
“By everyone who was not a specialist, artificial tears were considered something almost comparable to water. They are not water,” Benítez del Castillo pointed out. “These are products that contain formulas that can affect our ocular surface. We also had our share of problems in Europe with an eye drop that contained high levels of phosphates and eventually caused severe
7
By everyone who was not a specialist, artificial tears were considered something almost comparable to water. They are not water
José Manuel Benítez Del Castillo
Then comes the brunt of cataract surgery, and it is hard for the eye to recover after a fall from this tightrope
➧
Stefano Barabino
Cover Story
calcareous keratopathies leading to corneal transplants. As a fact, this is not an inert liquid.”
The new safety standards will lead drug companies to enhance the quality of their products, with new and more effective options coming to the market. “We already have new options, like eye drops combining hyaluronic acid and mucomimetic molecules, and with low concentrations of corticosteroids as an enhancer. New formulations with crosslinked hyaluronic acid and 3D structured hyaluronic acid hydrogels are going to be soon a must-have for our clinical practice”, Barabino said.

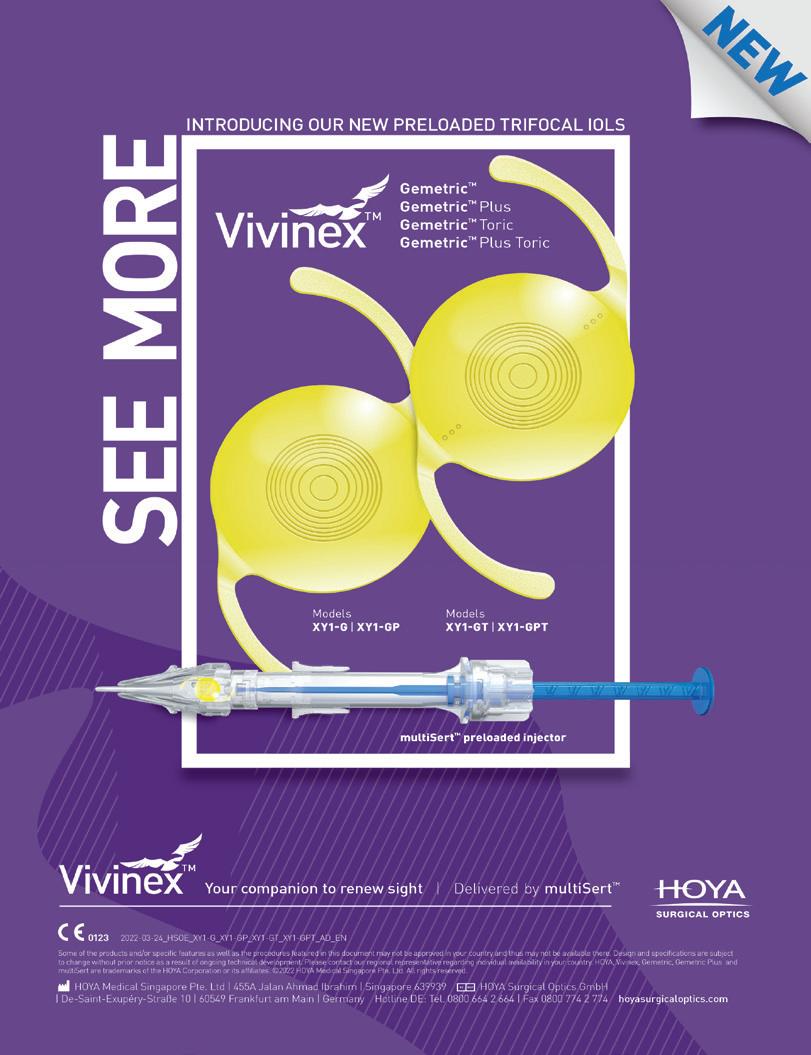
CATARACT AND REFRACTIVE SURGERY: THE IMPORTANCE OF A HEALTHY OCULAR SURFACE
How important it is to treat the ocular surface before and after cataract surgery has recently become more and more a hot topic, and efforts are being made to raise awareness amongst physicians
of how a healthy ocular surface is important for the benefit of both patients and surgeons.
“This is especially important. Many patients are unhappy with their surgery, especially if they are implanted with a premium IOL,” Barabino noted. “Because if the tear film is unstable, these kinds of lenses do not work properly.”
“Some patients may become symptomatic even if they did not show any symptoms before surgery, and in other cases patient’s symptoms may get worse after surgery. This is not only a matter of discomfort, but of significant visual problems,” said Benítez Del Castillo. “During Keratometry, a patient with DED can show two very different results before and after blinking, and this could give the surgeon a hard time in choosing the appropriate premium IOL. These patients will not settle for less than 20/20, with a good near, probably also a good intermediate vision. They have spent a fair amount of money
and are going to be very unhappy and disappointed if they do not achieve these goals after surgery,” he added.
“I would like to use a metaphor, courtesy of Professor Maurizio Rolando,” said Barabino. “The ocular surface is a tightrope walker, standing on a very thin line. In a patient with cataract, the Meibomian glands are usually old, and so are the epithelium and the conjunctiva, which could already show signs of conjunctivochalasis, but everything is still somehow balanced. Then comes the brunt of cataract surgery, and it is hard for the eye to recover after a fall from this tightrope,” he noted. “If we help the tightrope walker to find a better balance and brace for impact, we can avoid a disastrous plummet. Using some good eye drops after surgery may also be a viable solution, because it is quite difficult to restore balance on the surface of the eye, no matter how healthy it was before the operation,” he concluded.
“Prevention is key in these cases,” Benítez Del Castillo pointed out. “We are in an era where cataract surgery has been included in the refractive procedures, where patients have very precise expectations and there is no place for mistakes. When evaluating candidates, physicians now need to include tests such as tear break-up time and corneal staining, check the Meibomian glands, the tear volume, and of course treat the ocular surface if needed, and be sure that it is perfectly fit for surgery. Also, adding a suitable eye drop to the standard postoperative treatment can be very useful to keep the inflammation and symptoms of Dry Eye in check”, he concluded.
8
We are in an era where cataract surgery has been included in the refractive procedures, where patients have very precise expectations and there is no place for mistakes
José Manuel Benítez Del Castillo
Stefano Barabino, together with a group of Italian experts, added the concept of homeostasis of the ocular surface and its alteration as a pathogenic factor of DED to the DEWS II definition.
Sodium salt hyaluronic acid solution for intraocular use

































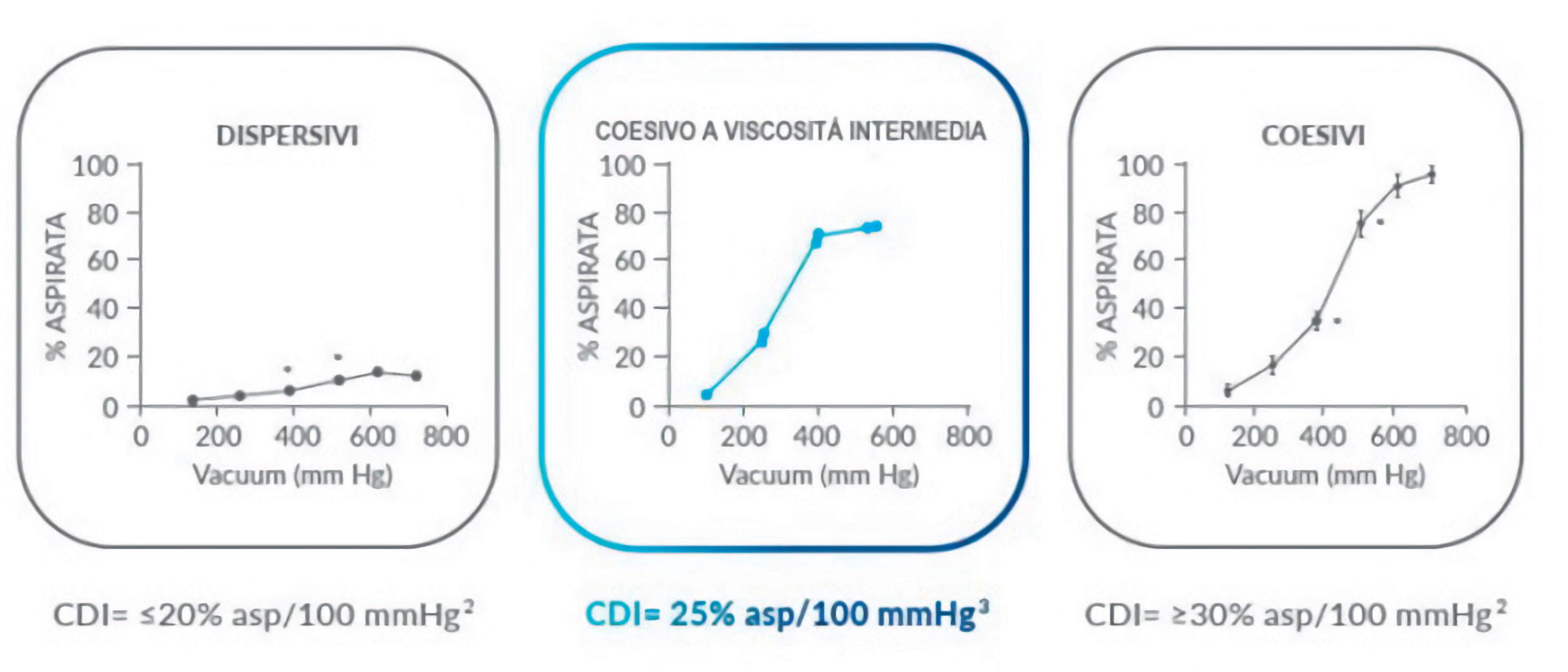
VISCOSITY AND COHESIVE BEHAVIOR









Maintains depth of the anterior chamber

















































for healthcare professionals - Cod. 99002764
FIDIAL®Plus is a 0373 medical device. Carefully read the instructions for use. Material intended
1
1 • • • •
1 Protects the corneal endothelium 1 Allows for an easy reconstruction of the anatomical shape at the operated site
Rapidly and physiologically eliminated
INTERMEDIATE
1. FIDIAL® Plus leaflets.
DRY EYE Diagnosis and therapy


Lucio Buratto
Luigi Marino
Maria Luisa Verbelli
Giuseppe Di Meglio
To order: www.fgeditore.it Editorial office: Strada 4 Milano Fiori, Palazzo Q7 – 20089 Rozzano (MI) – Italy Headquarters: FGE srl − Regione Rivelle 7/F − 14050 Moasca (AT) – Italy Ph. +39 0141 1706694 – Fax +39 0141 856013 e-mail: info@fgeditore.it − www.fgeditore.it
My interest in dry eye started in 2014 when I was visiting the ESCRS Congress in London and I met Marguerite McDonald. It was a totally unknown field to me, and I didn’t know a thing. However, by talking to my American friend and colleague, I realized that it would be a professional topic in full expansion in the future, so I returned home to read and study about it. I discovered a totally new world - not as fascinating and stimulating as that of cataracts or refractive surgery - but still new, unexplored and deserving of further study and in-depth investigation.
But my commitments in other areas of ophthalmology were too many for me to be able to devote adequate space to this new world, so I took action to add one of the best specialists to my team: Luigi Marino. Then, I founded the first center in Italy dedicated entirely to the diagnosis and treatment of dry eye, the CIOS Centro Italiano Occhio Secco [Italian Center for Dry Eye] and entrusted the management to Marino. Soon afterwards, I decided to publish on the subject - the first publication in Italy. The volume was widely disseminated, despite a lack of interest by pharmacological companies in the sector and even less by manufacturers of instruments for diagnosis and therapy.
My interest in dry eye did not limit itself to these two initiatives; in 2017, I promoted, throughout Italy, the first of three important annual campaigns on Dry Eye to raise awareness on the prevention and treatment of this unknown disease, which can lead to serious vision problems and can severely alter the quality of life. These campaigns were all sponsored by the Ministry of Health and the Italian Ophthalmological Society, and showed broad interest, involving numerous public hospitals, university clinics, and private facilities. Participating centers all over Italy carried out tests and exams, free of charge, informed by the promotional campaign, making it possible to request screening by booking on dedicated websites.
And with the aim of doing this in a deeper and more complete manner, I made sure the campaigns were also preceded by a broad-spectrum public opinion poll on the Italian population to ascertain the actual knowledge of this disease.
The raise of awareness of the population brought to light the emergence of hidden cases of dry eye disease and encouraged many people affected by it to seek specialist eye visits and to comply with the therapies, which beneficial results.
In addition to improved medical performance, this also led to new and interesting opportunities for companies producing diagnostic and therapeutic instruments and a strong increase in the use of products useful to alleviate the symptoms of dry eye. This happened despite the almost total disinterest of the abovementioned companies - apart from some rare exceptions - which, on the other hand, could have or had, in their interest, benefited greatly from the dissemination of the book and all other related projects. Now the second edition of the Dry Eye volume is coming out, thanks to the precious work of Giuseppe Di Meglio, Luigi Marino and Maria Luisa Verbelli, as well as the important contribution of other Italian and international colleagues.
The book does not represent a clinical research work. It does not purport to be a volume of highly scientific content. It is instead a practical manual especially for those who want to approach this disease now and for those who are already involved in improving their education a little. At first glance, dry eye syndrome seems to be an ordinary disease; instead it is making life and vision more difficult for a large proportion of Italians and the world population and being able to treat it with competence is of great importance and enormous social utility.
Enjoy your reading.
Lucio Buratto
NEW
Spotlight on the expert

A PROFESSIONAL VOW
The search for an alternative to corneal transplantation: a constant aim in the career of Cosimo Mazzotta

W
When the professional and personal life of a nationally and internationally recognized expert of ophthalmology is considered, passion and dedication are often recurring factors, to the point of becoming crucial requirements in the acquisition of prestige and fame in the field. From this point of view, the professional career of Cosimo Mazzotta, MD, PhD is no exception. He graduated in medicine cum laude in 1997 and specialized in ophthalmology cum laude in 2001 at the University of Siena. Subsequently, Mazzotta was awarded a PhD in degenerative, involutive and ocular neoplastic pathology, and a four-year research grant and a contract pro -
fessor position at the school for orthoptists in Siena. In the following years he distinguished himself in this field for his extensive knowledge of keratoconus and corneal ectasias, obtaining a double role as researcher at the University of Siena, where he has been Adjunct Professor at the School of Specialisation in Ophthalmology since 2015. After a brief period as Associate Professor at the University of Sassari, he resumed the practice of his profession mainly in Siena, where he lives with his family, and in Lecce (in the region of Salento, in Apulia), his birthplace of which he is very proud. However, Mazzotta is a different kind of expert, as not only is he noted for his passion and dedication, but also, he distinguishes himself by a third element: devotion in his field of interest. A professional vow that pursues the research for an alternative to corneal transplantation through pushing the boundaries of innovation.
Today Cosimo Mazzotta is Scientific Supervisor for the Siena Crosslinking Center, one of the most important and internationally recognized centers of excellence in the research and treatment of corneal ectasias, that he founded ten years ago and still manages to the present day. Mazzotta is passionate, skilled and an engaging communicator, who has participated as lecturer and instructor in hundreds of national and international congresses and courses. He also is one of the most valuable supporters of
12
Interview with Professor Cosimo Mazzotta, USL Toscana Sudest and University of Siena To connect
to the video, scan the QR code
Cosimo Mazzotta, MD, PhD, FWCRS is Associate Professor at the School of Specialisation in Ophthalmology since 2015. He is founder and Scientific Supervisor for the Siena Crosslinking Center
EyeSee, to which he shares in this interview part of his professional and personal life.
What is your subspecialty or main area of interest in ophthalmology?
My subspecialty is keratoconus. It has been my passion since I was a PhD student and therefore, I followed this training path before it officially became a subspecialty of ophthalmology. Above all, I dealt with this conservative therapy by introducing the corneal cross-linking technique in Italy for the first time.
During my PhD research activity, in 2004 I went to the Dresden University of Technology where I had a one-year fellowship. That was an experience that allowed
me to bring the corneal cross-linking technique to Siena and to Italy the same year, winning an award granted by the Italian Society of Ophthalmology (SOI) for scientific research, an experience I repeated successfully in 2021. So, keratoconus is my passion; as well as cross-linking and all the conservative therapies, including laser-assisted corneal reshaping treatments to improve vision, with the aim of avoiding corneal transplantation in these patients.
What was your contribution to the progress of ophthalmology? What do you think are the professional goals you have achieved?
I think I certainly contributed to ophthalmology in the last fifteen
by Timothy Norris
years thanks to the introduction of corneal cross-linking at the University of Siena; this is a technique that I pursued with research that contributed to the development of various therapeutic protocols, among which, the M Nomogram, which allows the treatment of ectatic corneas of any thickness and which was awarded at the ESCRS in Paris for research on keratoconus (Joseph Colin award).
It has been a continuous translational research which has led to benefiting the patient at a clinical level, moving from one-hour protocols to twenty-minute accelerated protocols, with a marked improvement in compliance and clinical workflow.
I also published the first studies in the world regarding confocal microscopy in vivo in humans, and this was certainly a pioneering research that raised my H-Index, which is currently twenty-six points, and my Citation Report, which is about four thousand points. Introducing cross-linking in Italy, developing it further by implementing research towards ever faster and more effective protocols, has had the positive consequence of reducing the number of corneal transplants by over 50%.
In my opinion, together with the introduction of intravitreal injections, this made a breakthrough in ophthalmology not only in Italy, but also internationally. I also would like to mention that I will be receiving the Golden Medal for my contribution in international ophthalmology by ➧

13
Introducing cross-linking in Italy, developing it further by implementing research towards ever faster and more effective protocols, has had the positive consequence of reducing the number of corneal transplants by over 50%
Cosimo Mazzotta
Research in the field of keratoconus, as well as all the conservative therapies of the cornea are first and foremost a passion for Cosimo Mazzotta
Spotlight on the expert
Professor Amar Agarwal in Chennai at the Intraocular Implant and Refractive Surgery Society Conference the 5th and 6th July 2025. This excites me and makes me proud of what I have done and continue to do.
Who were the most influential figures in your career? Who would you consider a teacher or mentor? I had a lot of teachers and each one of them gave me something since my first experiences as a resident and still do today in my daily practice. During my education and research period I attended the Siena eye clinic managed by Professor Caporossi. Then I had various experiences abroad, with Dr. Nirav Patel in Vadodara and especially, at the Agarwal Eye Center Hospital with Dr. Soosan Jacob and Professor Amar Agarwal, with whom a scientific
Cosimo Mazzotta
collaboration was created. We shared a lot of publications and scientific projects. Each one of them left a visible mark in my career. I believe I had many teachers who have given me solid foundations thanks to which I have managed to develop my own skills that have led me to what I am today. Receiving the Gold Medal for contributions to Ophthalmology from Professor Agarwal in 2025 will be a memorable moment for me that will seal what I have achieved and continue to achieve, and at the same time, repaying the many sacrifices I have had to make.
What progresses of international and national ophthalmology have seen you as a protagonist or have involved you? How much did this contribute to your daily practice? My congress activity has led me

14
My wish would be to develop pre-clinical diagnosis, that is, the genetic diagnosis and a gene therapy for the disease, aiming at completely preventing the development of this degenerative disease.
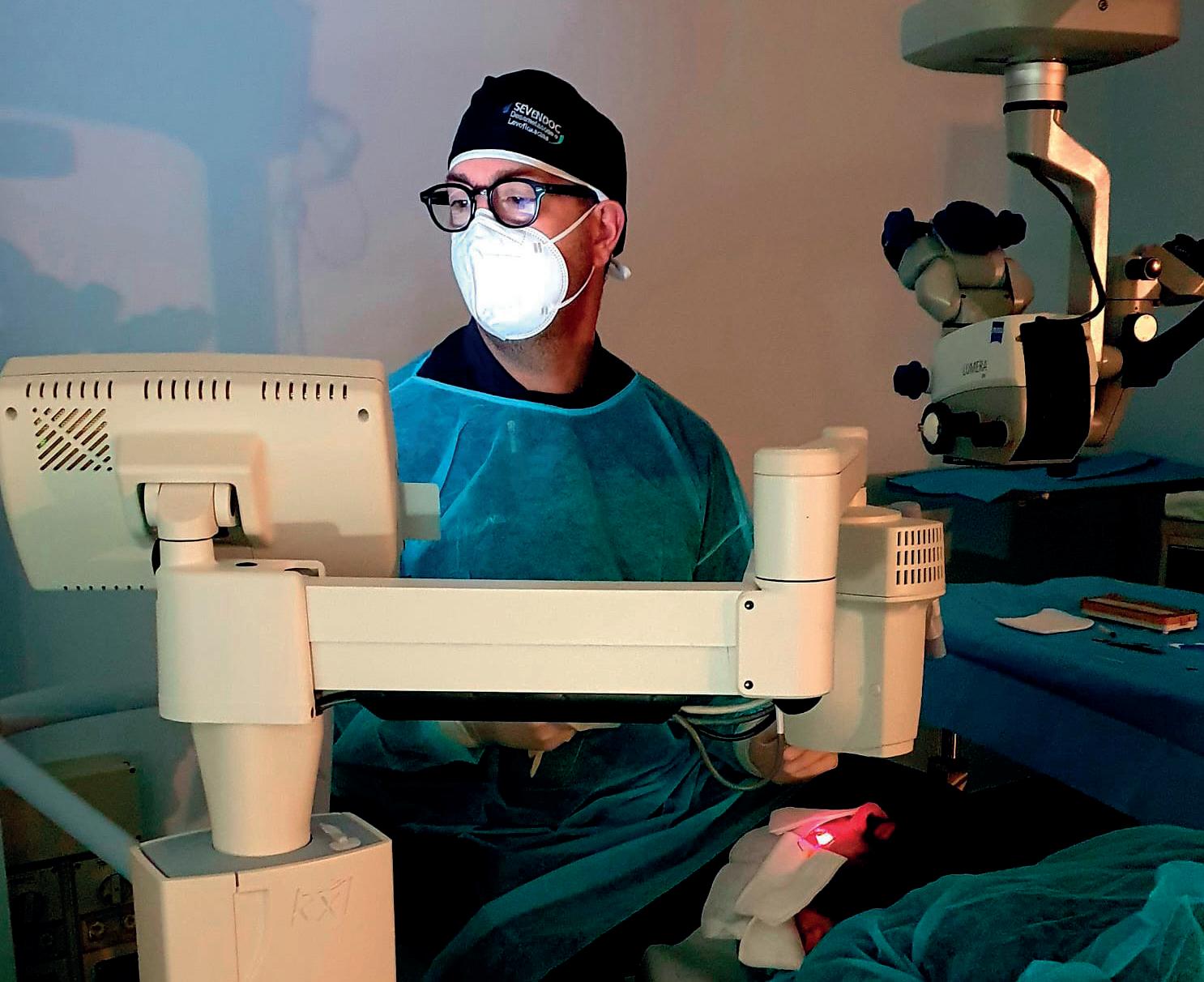
Corneal cross-linking performed by Mazzotta
Farhad Hafezi and Cosimo Mazzotta
to have many personal involvements, as well as to obtain very important international visibility.
I am currently one of the founders and a member of the Board of Directors of the newly formed International Keratoconus Society, which will hold its first world congress in Muscat, Oman. Since 2005 I have been part of the Cross-Linking Expert International Meeting in Zurich, where I presented the world’s first studies of in vivo confocal microscopy in humans after cross-linking, demonstrating how and what were all the tissue cellular changes at the level of the epithelium of the nerve plexus, cornea, keratocytes of the endothelium. I have to say that all these pioneering studies are highly cited and were considered in a major review on The Ocular Surface, which was extremely important at a global level. In addition to epi-off accelerated treatment nomograms, I recently developed the new high fluence transepithelial light and pulsed light treatment protocols and combined protocols of laser therapy with ray tracing and customized cross-linking to improve the vision of keratoconus patients intolerant to contact lenses. These protocols are subject to forthcoming publication
in prestigious journals, including Frontiers in Medicine and Cornea. Keratoconus is an increasingly frequently diagnosed pathology which afflicts young patients. It is widespread not only in Italy, but also in the Middle East, Asia and in the African continent. For this reason, among the various international panels on which I sit, the one that stimulates me the most is precisely that of the International Keratoconus Society, a very ambitious project and finally a response to the need to have an international scientific society exclusively dedicated to this pathology.

How much do you consider the profession in your life on a scale of importance from 1 to 10? I might say ten. We have got to the point where we just work. This is a great problem, but it is also a great privilege. Ours is a beautiful job; therefore, I agree with those who say that when one has passion in one’s work, one does not feel its weight, but experiences it as a pleasure. Certainly, our work takes away a lot of time from family, hobbies, and many other things.
Professional career aside, what are your passions and hobbies?
Let’s say I cannot cultivate many
hobbies, but the most important has always been the sea. Along with boating, sports are also my passion, such as crossfit and golf, which unfortunately I cannot devote much time to, considering my professional activity.
The Aladdin’s lamp: a wish, an innovation that you would like to already have for your patients today.
I would like to continue researching the topic of keratoconus. It is a highly impacting disease, especially because it affects young people, the future ruling class and their quality of life, as well as their families.
My wish would be to develop pre-clinical diagnosis, that is, the genetic diagnosis and a gene therapy for the disease, aiming at completely preventing the development of this degenerative disease. However, I am also happy to have contributed to greatly improving the quality of life and vision of these patients and I thank my colleagues who have always had admiration and trust in me and my work, often entrusting me with the most difficult and delicate cases, especially children with keratoconus.
15
Cosimo Mazzotta with Ashraf Armia


Editorial office: Strada 4 Milano Fiori, Palazzo Q7 – 20089 Rozzano (MI) – Italy Headquarters: FGE srl − Regione Rivelle 7/F − 14050 Moasca (AT) – Italy Ph. +39 0141 1706694 – Fax +39 0141 856013 e-mail: info@fgeditore.it − www.fgeditore.it To order: www.fgeditore.it OPHTHALMOLOGY
Volume 1
UP-TO-DATE
It is with great pleasure and honor that I present, on behalf of the Board Members, the first edition of the Ophthalmology Up-To-Date Textbook edited by the University Italian Society of Ophthalmology (SOU).
The aspiration of this book is to be a repository of knowledge and provide doctors with an up-to-date, organized and systematic approach to the visual system. This opera is thought to be useful in the daily practice of any ophthalmologist, but also to act as a guide for the general learning of the young ophthalmologists and trainees. The text is supported by a rich iconography with essential bibliography for further insights, and each chapter provides both basic descriptions and more in-detail knowledge in the various topics treated throughout the book.
This publication is divided into three compact but complete volumes that cover the majority of routine ophthalmological practice. In this first volume, dedicated to the dissertation of clinical pathologies, the different sections will be focused on the “Basics in ophthalmology” (from the anatomy of the eye to clinical refraction), “Diseases of the external eye and orbit”, “Pathologies of the anterior segment of the eye” and “Glaucoma and diseases of the uveal tract”.
In the following volume the “diseases affecting the posterior segment of the eye”, “pediatricand neuro-ophthalmology”, “genetic diseases, ocular oncology and correlations between systemic disorders and the eye” will be covered. The last volume of the opera will be dedicated to a complete description of “Instrumental diagnosis, imaging and technology in ophthalmology” and will contain specific and vast sections dedicated to therapeutics including “Laser and surgical procedures in ophthalmology”.
It is common belief by all the Authors, whom I personally thank for the great effort and work done in producing the chapters of this textbook, that these three volumes can provide an excellent study basis for ophthalmologists in training, (and also for the most experienced physicians) integrating their learning and skills during the clinical work and the surgical experiences, always suggesting to update their knowledge with the essential study of recent research papers and review monographs. I hope that the readers will enjoy it and they will be stimulated by our ophthalmology textbook.
Leonardo Mastropasqua
NEW
InnovatIons
THE INNOVATION OF SIMPLICITY
Vision-AR-IOL Simulator, augmented reality for a better-informed choice of the best IOL
SSometimes a brand-new idea comes in the shape of a very intuitive app. So simple, that it sounds obvious in hindsight. A ‘why has nobody thought of it before?’ kind of idea. It is pure simplicity as a key to success, a concept that in a blink of an eye, could become a part of everyday clinical practice as a true helping hand.
The latest advancements in software technology in recent years have surely expanded everyone’s perspective – particularly in specialised fields like ophthalmology – opening up new and uncharted paths for physicians, patients, and sector companies. Along this path came the idea for a new software, the Vision-AR-IOL Simulator created by Luca Vigo, MD, from the Advalia Clinic in Milan. This is a software that can be used with an iPad Pro, using augmented reality (AR) to simulate the result of different intraocular lenses before implantation. Dr. Vigo explained how the Vision-AR-IOL Simulator app works, what its potential is, and how this can affect physicians, patients, and companies, in the hope that one day we will see this software becoming a standard issue for clinical practice.
THE EASIER, THE BETTER
“Vision-AR-IOL IOL Simulator is an app I created in collaboration with the Italian medical developers of SBM Sistemi”, Vigo explained. “It can be easily downloaded and installed on an iPad, and it simulates the visual result of an IOL implantation based on the patient’s parameters”. Thus, it is an easy-going app, cre-
ated by Dr. Vigo and inspired by some of the technology that was presented in different congresses of ophthalmology in recent years.
“My idea came during the AECOS congress in Antwerp, where I saw a head-mounted device for IOL simulation that gave the patient an idea of the visual results of a cataract surgery using AR and preloaded photo imagery”, he explained While being fascinated by this technology, Dr. Vigo soon realised how expensive and complicated this was. “I was looking for something more user friendly, obtainable, and with no preloaded images. My aim was to give our patients the idea of different visual outcomes at different distances, while focusing on the screen of a portable device with the camera turned on”
The idea was to use an iPad Pro powerful enough to run the application, with an advanced, high-tech camera capable of focusing on any distance. “The engineers who worked on the app added some very useful expedients to enhance quality of vision and depth of focus”, he added.
Easier and better, to really meet the needs of patients and physicians. “As ocular surgeons, we seldom use Premium IOLs, not because we are not capable, but because we have difficulty in finding ways of recommending suitable lenses to our patients”, Vigo explained. “We know a lot about our Premium lenses’ strengths and weaknesses and their side effects, but we don’t want to be bogged down in post-operative predicaments. Instead, having an app that can help the physician

18
Interview with Dr. Luca Vigo, Advalia Vision, Milan
Dr. Luca Vigo
to guide and inform a patient and help him find the perfect solution, is basically what I had in mind”.
INTUITIVE
According to Luca Vigo, this IOL Simulator is a very user friendly and intuitive software. All a physician has to do is to set the parameters based on the patient’s refractive data, such as astigmatism, myopia, presbyopia, stage of cataract. The iPad will then be handed to the patient, and he or she can scroll between different kinds of lenses to see what the outcome could be. The patient can choose between the four classic lenses, both premium and standard, such as monofocal standard, for far, intermediate or near vision; the EDOF monofocals, with a good depth of focus from 1 meter; multifocal EDOF with
a depth of focus starting from 5060 centimeters; and finally, quadrifocal or diffractive trifocals with a depth of focus starting from 30-35 cm. “This is a simulation, of course. We want to show our patients how, with different solutions, their postoperative visual acuity could change”, Vigo said. “The app will also simulate possible halo and glares depending on the type of lens, such as multifocal and multifocal EDOF. So, by using the Vision-ARIOL Simulator we can effectively show how a lens might behave in low light or other different conditions”.
All the physician has to do is to purchase and download the app (cost, 2500€) on an iPad that can be used in many ways in a clinic. “The cost of both the app and the iPad can be covered with just a couple of surge-
by Laura Gaspari
Simulator: Home screen of the VisionAR-IOL Simulator application
ries performed”, Vigo observed.
VISION-AR-IOL SIMULATOR, PROS AND CONS
Vision-AR-IOL Simulator can benefit a patient undergoing a crystalline lens exchange, sometimes during the early onset of cataract, and for the correction of ametropia.

“By looking at the screen of the device, a patient can immediately understand if he or she can feel comfortable with one kind of lens or another. This can be done easily in the office, and without using any preloaded picture,” Vigo said.
“They can be aware of the side effects of one lens compared to another, how the lens can behave in different scenarios like how a simple driving experience could be. Sometimes patients are unaware of what the result can be, and they could feel disappointed by the wrong choice of a lens, especially if the patient has previously suffered from myopia and astigmatism. With this app the patient can have all the necessary information and choose wisely, knowing that a new lens could probably be for life”, Vigo said. “We are all well aware that a lens can be changed in the first months after the implantation, but there are very few surgeons who would go for a fibrotic lens in the bag”.
Thanks to this device, a patient can ➧
19
I was looking for something more user friendly, obtainable, and with no preloaded images. My aim was to give our patients the idea of different visual outcomes at different distances, while focusing on the screen of a portable device with the camera turned on
Luca Vigo
InnovatIons
be well informed of all the available options and be guided towards a conscious lens choice, facing the upcoming surgery with confidence and with less risk of post-op disappointment. “With Vision-AR-IOL Simulator we can show an early onset cataract patient how their crystalline opacification may affect their visual acuity in the future”, Vigo said. A great boon for the physician as well. “Many are the benefits for our clinical practice: we can use the device for ourselves or with our orthoptist and make it more time-efficient to help our patient choose the right lens”.
A great support, also from a legal point of view. “A patient who is more in control of their choices is going to more greatly value the informed consent he or she is going to sign immediately before surgery”, Vigo explained. Surely, nothing is perfect. “This is a simulation, so it is not going to be
100% identical to the postoperative result, but I can assure that every patient that used it said that it was very close to the real outcome. We still have the final word on what is the best lens for our patient, and not the opposite”, he remarked. Another ‘con’ however, could be the slight difference between every patient interfacing with the device, especially in some specific conditions. “Every patient has some variables that can slightly affect the performance. This app is ideally set for a patient with a healthy eye, retina, and optic nerve, but with a cataract that is not in a too-advanced stage. Some patients may also have different and non-optimal pupillary dynamics, and the lens can be affected differently because of that”, he explained. “Same if we have to deal with a very advanced cataract; a patient with an impaired visual acuity would simply not be able to have a clear idea of what the simulation could provide”.
Luca Vigo
A VALID DEVICE FOR CLINICAL PRACTICE
Despite some few limitations to its use, there is a lot of potential in the Vision-AR-IOL Simulator. “I would really like to see it widespread, because I think this could become an essential device in the future”, Vigo explained. A useful device for colleagues and patients, and of course for IOL manufacturers. “A company can purchase and brand this software and add their lens”, Vigo suggested, “and give it to their key opinion leaders for educational and informative purposes.” The educational aspect is fundamentally important to the aim that Luca Vigo has for this instrument. “I think that this software has a much more important role than what we can envisage now. It can be very useful for gathering statistical data, thanks to the implementation of customised surveys aiming to improve the software, as well as some feedback on the use of intraocular lens”, he explained.
Luca Vigo suggests that colleagues should try Vision-AR-IOL Simulator to better realise all the potential of this app. “It is essential to have a direct experience of this app to fully understand how good it is. I am also looking forward to hearing from colleagues if there are things to modify or add to improve this software. All ideas and suggestions are welcome, because we can all benefit from this”, he concluded.

20
Instead, having an app that can help the physician to guide and inform a patient and help him find the perfect solution, is basically what I had in mind
Example of what the patient sees using the Vision-AR-IOL Simulator
Proteggi la loro visione del mondo con MiYOSMART.
60% di riduzione della progressione miopica sostenuta e confermata nei 6 anni1,2
Efficacia dimostrata dal primo studio italiano su occhio caucasico3
Correggi la miopia e rallentane la progressione anche in condizioni di luce solare intensa con le nuove lenti MiyoSmart Chameleon e MiyoSmart SunBird.

Per informazioni, scrivi a oculisti@hoya.it
Lam CS, et al. Myopia control in children wearing D.I.M.S. spectacles lens: 6 year results. Invest Ophtalmol Vis Sci. 2022;63: ARVO E-abstract 4247
3. Nucci P, Lembo A, Schiavetti I, Shah R, Edgar DF, Evans BJW. A comparison of myopia control in European children and adolescents with defocus incorporated multiple segments (DIMS) spectacles, atropine, and combined DIMS/atropine. PLoS One 2023 Feb 16; 18 (2): e0281816.
1.
Lam CSY, Tang WC, Tse DY, Lee RPK, Chun RKM, Hasegawa K, Qi H, Hatanaka T, To CH. Le lenti per occhiali con tecnologia DIMS (Defocus Incorporated Multiple Segments) riducono la progressione della miopia: uno studio clinico randomizzato di 2 anni. British Journal of Ophthalmology. Pubblicato online per la prima volta il 29 maggio 2019. doi: 10.1136/bjophthalmol-2018-313739
2.
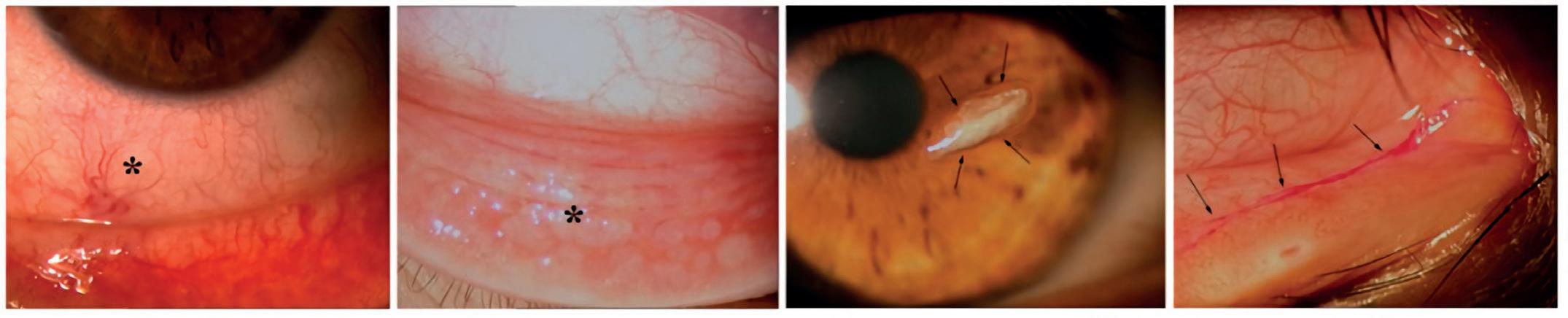
Nightmare Cases BETTER LATE THAN NEVER
I

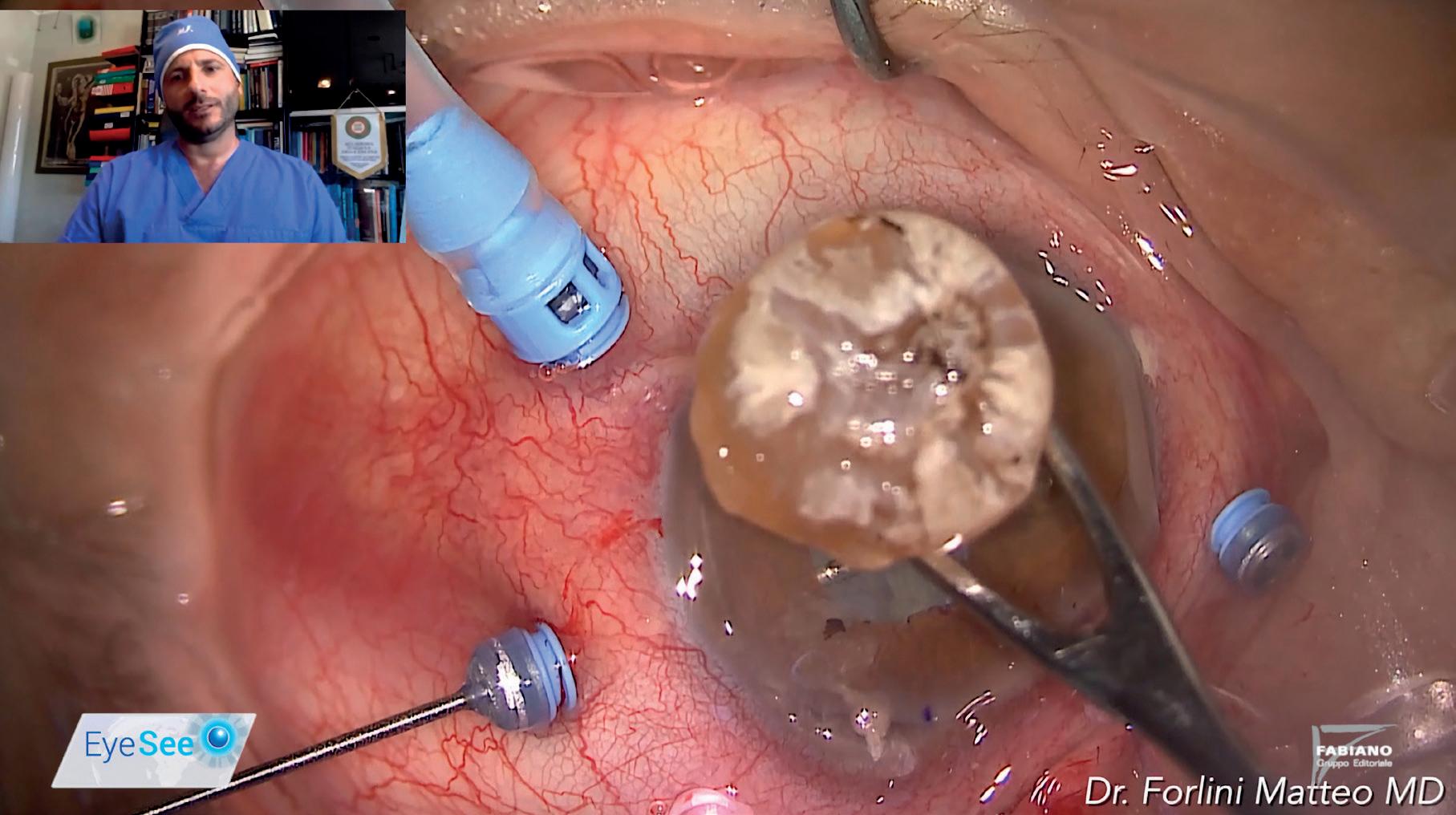
In some cases, a surgeon may decide not to intervene. This is a choice that, in the short term, could be considered in the best interest of a patient. However, in the long term, this decision could create a significant number of problems, eventually leading to necessary surgery even thirty years later.
This is exactly what happened in this case presented by Matteo Forlini, MD, vitreoretinal surgery consultant at the San Marino State Hospital.

It all started in 1992, when a patient arrived – thirty years old at the time – suffering from a severe closed globe injury. “It was an amblyopic eye, and for this reason, the patient was not at that time considered eligible for a surgical procedure. As a result, he had to live with a traumatic cataract for three decades”, Forlini said. Inevitably, something had to go wrong, and in 2023 the patient arrived at the San Marino State Hospi-
tal reporting ocular pain, showing signs of inflammation, ocular hypotony (IOP 32 mmHg) and a motu manu visual acuity. At that point, a surgical procedure was inevitable. “This was now a hypermature cataract, so tough and rocky that it made it impossible for us to opt for a standard phacoemulsification,” Forlini said. “So, we went for an Intracapsular Cataract Extraction (ICCE), thus removing the crystalline lens and the bag altogether, and then implant an iris claw lens secondary implant behind the iris”. Preserving the iris tissue during the whole surgery is something of vital importance for a correct implantation of this kind of IOL. “At the beginning of implementing the ICCE, we had to perform a wide 6mm incision in the anterior chamber while keeping a very keen eye on the iris, that was at high risk, either of prolapse at any moment during the whole procedure, or of being damaged during the crystalline lens extraction,” Forlini said.
Firstly, the rocky cataract was displaced in the anterior chamber with the use of viscoelastic, then, using a lens loop, the lens and the bag were extracted through the incision, and finally the residual vitreous was removed from the anterior chamber through a triamcinolone-assisted anterior vitrectomy.
“It is very important to keep the iris claw lens steady with the dominant hand, and with the spatula on the other hand, perform an inclavation of the haptics in the mid-peripheral iris. By doing so, the iris’ physiology can be kept almost unaltered”
Forlini explained. “To perform the inclavation we need to gently pull the iris tissue from the camerular angle to the center – from the outside to the inside – thus, in a
22
To connect to the video, scan the QR code
Tips and tricks for the management of a hypermature traumatic cataract
Interview with Dr. Matteo Forlini, San Marino State Hospital
Matteo Forlini, MD, is vitreoretinal surgery consultant at the San Marino State Hospital.
centripetal and not a centrifugal direction.”
After performing the iris claw implantation, the wide corneal incision was sutured with Nylon 10/10 separate stitches. “At the end of the procedure the pupil was round, regular and well-centered on the lens,” Forlini noted. “We definitely improved our patient’s quality of vision, with 0.3 decimals of visual acuity on the amblyopic eye and a 12 mmHg IOP. The cornea was transparent, the pupil was regular and with no pupillary distortion, and the retropupillary Iris Claw was well enclavated,” Forlini added. “Even after the retropupillary IOL implantation, we were able to obtain a good drug-induced mydriasis and we were also able to examine the ocular fundus. No macular edema was observed, so the retina was in good condition.”
As a consequence of both the
wide corneal incision and the suturing that followed, the patient presented a high post-operative astigmatism (+6.50 D cylinder). “The astigmatism will gradually become lower after removing the sutures”, Forlini confidently noted. “In an amblyopic eye, however, this is one of the less relevant issues”.
As in every other surgical procedure, the implantation of an iris claw retropupillary IOL has its pros and cons. “It is a rapid procedure, with a lower incidence of side effects such as corneal decompensation, secondary glaucoma and cystoid macular edema: definitely a good set of advantages”, Forlini explained. “Moreover, this surgical technique can avoid the conjunctival opening, and by inclavating the iris claw lens in the mid-peripheral, it is possible to minimise the physiological altera -
by Chiara Mazzoni
tion of the iris and the camerular angle”, he noted.
Post-operative astigmatism is among the ‘cons’ observed by Matteo Forlini, as well as the complexity of the technique, especially for training surgeons. “The risk of a pupillary distortion is always around the corner, but it can be avoided by inclavating the lens haptics with a centripetal direction, by pulling the tissue from the camerular angle to the center,” he explained.
“A difficult case, with a positive outcome”, Forlini said. “We managed to obtain some pretty good results for a very complicated case of a hypermature traumatic cataract. This case is key to understanding how important it is for the surgeon to be able to master not only standard and modern techniques, but also the older and less common ones, like the ICCE”, he concluded.
23
The risk of a pupillary distortion is always around the corner, but it can be avoided by inclavating the lens haptics with a centripetal direction, by pulling the tissue from the camerular angle to the center
Matteo Forlini
180 MILLION EUROS
FINE CONFIRMED BY ITALY ON THE AVASTIN/LUCENTIS CASE
On the 8th of May 2023, the Italian State Council declared inadmissible the pleas presented by Roche and Novartis regarding the 180 million euros fine set by the Italian Antitrust agency in 2014. Starting in 2013, the two pharmaceutical companies were put under the investigation by the Antitrust accused of forming a ‘cartel’ that was favouring Lucentis (ranibizumab) for the use in ophthalmology rather than the cheaper Avastin (bevacizumab).
The decision of the Italian State Council goes in the opposite direction of the two issued by France and Turkey at the beginning of 2023, which called off the financial penalty.
According to SOI President Matteo
Piovella, “The extraordinary importance of this news, that certified and will further certify in the next decades the significance and referentiality of the Italian Ophthalmological Society (SOI): after nine years and nine trials, three at the European Court, we cleared the way and let the truth emerge, with a final and definitive judgement,” he said in a video published in the official SOI website.
The two companies acknowledged the decision of the Italian State Council, remarking on the pages of Quotidiano Sanità that they always worked in compliance of the Italian antitrust laws and for the benefit of the patients.

24 News
O
APPROVAL OF AFLIBERCEPT BIOSIMILAR RECOMMENDED BY
EMA’S COMMITTEE
B
Biocon Biologic subsidiary company of Biocon Ldt from India, has announced that the Committee for Medicinal Products for Human Use (CHMP), gave a positive opinion on YESAFILI®, Biocon’s aflibercept biosimilar, for the treatment of wet AMD, DME and myopic choroidal neovascularization. According to a company press release clinical trials on YESAFILI® showed a non inferior safety and efficacy profile compared to aflibercept.
“We are very pleased to receive a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) for our YESAFILI® biosimilar. This is further confirmation of our strong commitment to providing high-quality and affordable medicines and represents another significant
milestone as we continue to expand our biosimilar offerings across the globe,” CEO and Managing Director, Biocon Biologics Ltd Shreehas Tambe stated in the press release. “We look forward to making a meaningful difference to patients in the EU impacted by macular degeneration and diabetic retinopathy.”

The Committee for Medicinal Products for Human Use is part of the European Medicines Agency’s; its opinion will be taken into consideration by the European Commission, and a final decision is expected in September this year.
Reference: https://www.biocon.com/biocon-biologics-announces-positive-chmp-opinion-for-yesafili-biosimilar-aflibercept/
25
CSO AT ESCRS AMONG ENVIRONMENTAL SUSTAINABILITY, ACADEMY AND BREAKFAST SYMPOSIUM

C
CSO is participating in the 41st edition of the ESCRS International Congress in Vienna. CSO focuses on three concepts: sustainability, academy and symposium dedicated to professionals. As for environmental sustainability CSO is present with a booth (Hall B Booth 218) designed according to the guidelines of the United Nations Agenda 2030 Sustainable Development Goals (SDGs) to compete for the Sustainable Exhibitor Award; the award will be given to the exhibitor who has concretely embraced environmentally responsible behavior as well as sustainable work practices both inside and outside the congress. Moreover, CSO is dedicating an area
of the booth to its Academy, where Key Opinion Leaders will be available on Saturday, Sept. 9 and Sunday, Sept. 10, to answer visitors’ questions on specific topics, particularly related to the main themes of the congress. Building on its success in 2022, CSO is organizing a Breakfast Symposium with six international Key Opinion Leaders on topics related to cataract and refractive surgery on Saturday, September 9 from 6:45 to 9:15 a.m. at the MAK-Austrian Museum of Applied Arts.
Participants are invited to the scientific session chaired by a prestigious panel that includes strong interaction with the audience; a great opportunity for exchange and discussion with experts such as Francesco Carones on “Understanding objective optical performances of different IOLs once implanted”; Dan Z. Reinstein on “Diagnostic Power is Clinical Power - Make your life easier with the right information.”; Emilio Torres-Neto on “Total corneal wavefront transPRK using MS39 data: first results.”; Farhad Hafezi on “Scheimpflug and OCT technology revisited: success rates after corneal cross-linking”; Andrea Russo on “Utilizing the MS-39 in ICL Surgery: Prevention of intraoperative and postoperative complications.”; Jorge L. Alio del Barrio on “Development of a Virtual Model System for refractive Surgery Treatment using latest CSO technology”.
For directions to the booth and symposium, to make an appointment, or for other information, write to cso@csoitalia.it
26 News

THE DIALOGUE BETWEEN SCIENCE AND POLITICS
The fundamental role of AISG in the insertion of the new DRG of the Lombardy Region for glaucoma surgery
Interviews with Professor Stefano Miglior, Director of the Ophthalmology Clinic of the Monza Polyclinic; Professor Luciano Quaranta, Councilor of AISG and Director of Centro Oculistico Italiano, Brescia; Professor Roberto Carassa, Councilor of AISG and Director of Centro Italiano Glaucoma, Milan, and Professor Luca Rossetti, Councilor of AISG and Director of ASST
Santi Paolo and Carlo Eye Clinic, Milan
IIn Italy it is estimated that people affected by glaucoma, ‘the silent thief of sight’, are around eight hundred thousand. According to the latest estimates, 1 out of 3 Italians is not aware that they suffer from glaucoma. The surgical treatment of primary open-angle glaucoma (POAG) – the purpose of which is to normalize the intraocular tone – has made great strides: from trabeculectomy, that is, the more traditional surgery, to minimally invasive subconjunctival filtering procedures using implantable medical devices. However, unlike traditional surgery, these latter procedures are not reimbursed by the Italian National Health System, making access to them more difficult for patients. For this reason, the Lombardy Region has recently updated the DRG tariffs to also include microstent devices for glaucoma drainage. This was also made possible thanks to the great effort of a scientific society like the Italian Association for Glaucoma Studies (Associazione Italiana per lo Studio del Glaucoma - AISG) which cooperates with regional authorities in the sharing of scientific evidence supporting the usage of these innovative surgical devices. We spoke about this extraordinary good practice with the President of AISG, Professor Stefano Miglior and three of its Councilors, Professor Luciano Quaranta, Professor Luca Rossetti, and Professor Roberta Carassa. They told EyeSee about the path taken to arrive at this significant resolution, and explained its importance for accessibility to glaucoma surgery.
GLAUCOMA SURGERY, THE UNMET NEEDS
“Glaucoma surgery is one of the most unpredictable eye surgeries today, even in the most expert hands.
Each surgeon adopts personal variations to improve the result”, Professor Luciano Quaranta, Director of the Centro Italiano Glaucoma of Brescia, said. It is not the simplest surgery to deal with and its development has seen many passages, as Professor Carassa of the Centro Italiano Glaucoma in Milan also recalled. “In glaucoma surgery we want to be able to have safety, efficacy, and reproducibility. Trabeculectomy, the traditional surgery, was very effective, but burdened by possible complications and not even reproducible”.

According to Professor Quaranta, one of the unmet needs in the surgical treatment of glaucoma is the lack of standardization of procedures. “It would be helpful to better understand what to expect from each individual procedure, with specific indications for each different glaucoma phenotype and patient. That is, to have operations that can be performed with good safety and efficacy profiles, together with rapid functio-
28
InsIghts
Professor Luciano Quaranta
Professor Stefano Miglior
nal recovery even in the early stages of the disease”, he said.
The introduction of new devices for micro-invasive filtering surgery proceeds in a very specific direction. “There has been an effort to optimize different types of techniques to arrive at something more efficient. The introduction of new subconjunctival filtration devices for micro-invasive filtering surgery has therefore made it possible to have efficacy and safety”, Carassa explained.
THE MICRO-INVASIVE FILTRATION SURGERY DEVICES, BETWEEN ADVANTAGES AND LIMITATIONS
The two protagonists involved are PRESERFLOTM Microshunt (Santen)
and XEN 45 Gel Stent® (Abbvie), which allow the surgeon to perform a filtration surgery while maintaining the central role of the filtration of the aqueous humor at the subconjunctival level for the control of intraocular pressure. “Medium-term literature data indicate that the surgical implantation of these devices allows for a good control of intraocular pressure; the implantation technique is rapid, relatively simple, and highly standardized. We are getting closer to satisfying those ‘unmet needs’, even if these procedures require a particularly delicate post-operative follow-up to optimize the result of the surgery”, Quaranta explained. “The great advantage is that of
by Laura Gaspari
being able to offer the patient surgical procedures even in the earliest stages of the disease, due to their low invasiveness and high efficacy”. Effectiveness, safety, but also reproducibility. “Since this surgical technique is performed by inserting a small tube with a calibrated internal diameter, it is much more reproducible because it is not conditioned by the personal tricks of each surgeon”, Carassa added.
However, there are limitations to the use of this type of surgery, not so much in its feasibility, but in the costs involved. “Costs and lack of an appropriate DRG are the main obstacles of these devices”, Luca Rossetti, Director of the ASST Santi Paolo e Carlo Eye Clinic, Milan, explained.

“The operated patients are either those who have continued with medical treatments until now, with higher costs spread over time and not covered by hospitals, or the patients operated with traditional surgery, with very low costs. It is therefore a new path with significant additio-

29
Lombardy Region Headquarters in Milan
➧
Professor Roberto Carassa
InsIghts
nal costs without adequate reimbursement”. It is precisely to overcome this problem that AISG and the authorities of Lombardy region have reached an extraordinary agreement in favor of patients.

THE LOMBARDY ‘CASE’: THE DIALOGUE BETWEEN SCIENCE AND POLITICS IN FAVOR OF PATIENTS
DRG is an acronym that stands for Diagnosis Related Group, i.e., a classification system for resources and for hospital admissions. These are grouped in such a way that all hospitalizations belonging to the same DRG have a similar care burden and consumption of monetary resources. Before today, micro-invasive surgery using filtering devices was not covered by the Italian National Health System, as explained by Professor Stefano Miglior, President of AISG and Director of the Ophthalmology Clinic of the Monza Polyclinic. “Due to regional autonomy in terms of health management, there are sometimes significant differences in the reimbursement of this procedure. In Lombardy the reimbursement was insufficient to cover the expenses related to the use of these devices compared to some other Italian Regions”.
For this reason, AISG, in compliance with its training based on the relevant clinical activities to be implemented in daily practice - a vocation it has had since its foundation in 1984 – has, through an extraordinary effort, set itself the task of drawing up a document to be presented to the regional authorities and thus opening a dialogue between science and politics. “In 2019, with the introduction of XEN® in Italy, AISG evaluated the opportunity of preparing a
critical and scientifically solid document, drawn up by Professor Quaranta, Professor Rossetti, Professor Carassa and myself, to be presented to the Lombardy Region to introduce this new surgical procedure which could not be used by all surgeons within the Italian National Health System due to the high costs of the device, and which could not be covered by the DRG included in the Regional Handbook at the time”, Professor Miglior said.
After an inevitable stop due to the COVID-19 pandemic, the document drawn up by AISG arrived on the tables of the Lombardy Region at the end of 2022. “The document takes into consideration the XEN® and PRESERFLOTM devices, since both are draining microdevices, with different ways of implanting them, but both with good efficacy and safety characteristics”, Miglior stated. In May, the Lombardy Region recognized the specificity and innovation of this surgical procedure compared to the traditional procedure, introducing a second surgical DRG, again in the field of glaucoma surgery. “The Lombardy Region has appropriately modified the reimbursement, increasing it by 1000 euros and making the procedure much more affordable”, Rossetti added. “The introduction of a dedicated DRG allows the use of this device in glaucoma surgery in public hospitals and affiliated private clinics. We are dealing with an excellent result, especially for patients with glaucoma who will more easily benefit from of a very safe surgery with an excellent efficacy profile”, Miglior stated.
A MILESTONE
Without a doubt, this is a huge success for AISG and for Italian glaucoma surgery. “On behalf of AISG, I believe that this very important achievement in the administration of health can certainly be interpreted on the one hand, by the scientificity, objectivity and critical representation of the problem by a scientific society and by the high scientific and clinical credibility of the four co-authors, and on the other, from the particular attention of the Lombardy Region in the persons of Doctor Giovanni Pavesi, Director General of the Council and Guido Bertolaso, Councilor for Welfare of the Lombardy Region”, Miglior commented.
This experience marks a milestone in the real possibility that a scientific society collaborates with the administra-
tors and the political authorities for the good of the citizens. “We are very proud of the result achieved”, Luciano Quaranta added. “It was not obvious to us that the work done by AISG would lead to the result obtained. The great sensitivity of the authorities in Lombardy, together with a detailed analysis of costs and benefits, have had a highly positive outcome”.
“Today it is not so frequent that there is a dialogue between politics and scientific bodies”, Roberto Carassa concurred. “More frequently, companies are the promoters of such projects. Instead, the role of a scientific society is precisely that of selecting the innovative solutions based on literature and clinical experience in order to gain a positive clinical response for patients: these were the strengths that prompted the Region to talk to us”.
The good example of AISG, therefore, is more than recognized. “I would like to underline the importance of the virtuous path that starts from a clinical need supported by scientific evidence, and that arrives at a prestigious scientific society that deals with interacting constructively with regional policy, and which must make choices based on what is suggested and for the benefit of sick citizens”, Luca Rossetti said.
Finally, AISG Board invites fellow ophthalmologists to adopt a cautious approach to treatment, for the good of patients. “As President of AISG and as a surgeon, I believe that this opportunity in the Lombardy Region is very important, but it must be managed carefully: glaucoma surgery is not a ‘one shot surgery’ like phacoemulsification with an IOL implant for cataracts, for example. Any glaucoma surgery requires a continuous and constant re-evaluation of the operated patient during the first month of post-surgical follow-up and after three and six months”, Miglior said. “We should all remember that post-operative procedures are more effective the sooner they are performed. The hope, therefore, is that this opportunity will not be trivialized and that it will be used with clinical and scientific rigour. The risk could be that a future assessment by the Region of the numbers and methods of intervention could lead to a reconsideration of the DRG, causing physicians and patients to no longer benefit from what has been made available to us today with so much attention and foresight on the part of regional policy”, he concluded.
30
Professor Luca Rossetti

NOT JUST A PEDIATRIC DISEASE

Understanding adult strabismus and how to deal with it
Interview with Professor Aldo Vagge, University Eye Clinic of Genoa, IRCCS San Martino General Hospital
SStrabismus, a condition in which the visual axes of the eyes are not aligned, is often closely linked to pediatric ophthalmology, especially in congress debates, meetings, and specialised symposia. However, the onset of strabismus is not exclusively in childhood, but may also occur in adulthood. Though not frequently debated, adult strabismus is a condition that should not be underestimated, because
it has many clinical and psychosocial implications. To know more about adult strabismus, its causes – particularly when associated with myopia –the different types of strabismus and the different surgical option, EyeSee interviewed Professor Aldo Vagge an expert in strabismus and pediatric ophthalmology serving at the University Eye Clinic of Genoa, IRCCS San Martino General Hospital.
32
InsIghts
Professor Aldo Vagge
STRABISMUS IN ADULTS: INCIDENCE, CAUSES AND IMPLICATIONS
“Strabismus is not so rare in adults, with an incidence of around 4%”, Vagge said. Adults with strabismus may have it since childhood, but others may develop it later, as a consequence of pathologic or traumatic conditions. “At the origin, there may be new conditions emerging in adulthood such as neurological or vascular diseases, which is in the case of paralytic strabismus, or endocrine conditions such as thyroid disorders; and again, trauma or loss of vision, as in the case of sensory strabismus, which frequently leads to esotropia in children or exotropia in adults. Finally, there are forms of strabismus which are ‘age-related’”, Vagge explained. The latter is the case of “sagging eye syndrome (SES), described for the first time by Rutar and Demer in 2009, resulting from age-related degeneration of the band of connective tissue suspending the superior and lateral rectus muscle pulleys (SR-LR band)”, Vagge continued. “This band sustains the

lateral rectus muscle pulley, preventing vertical displacement. The degeneration of this ligament system determines the inferior sag that gives the name to the syndrome, with consequent moderately incomitant exotropia with insufficient divergence, cyclovertical strabismus, or both. Patients affected with SES typically present aponeurotic blepharoptosis and a pronounced superior palpebral sulcus”.
One of the major implications of strabismus emerging in adulthood is diplopia, a particularly annoying symptom which may cause problems with the patient’s daily activities. “In the majority of cases patients experience double vision and loss of depth perception, which affect the ability to carry out common daily tasks such as driving or parking the car”, Professor Vagge explained Strabismus in adults does not only involve problems closely related to the visual apparatus, as Vagge pointed out. “Patients with strabismus may acquire abnormal head positions (AHP)
by Laura Gaspari
and other postural problems due to the attempt to reduce or get rid of double vision by tilting the head”, he explained.
Last but not least, psychosocial aspects of strabismus should be considered. “Many studies reported an improvement in quality of life in patients undergoing strabismus surgery, with or without diplopia, therefore regardless of the patient’s binocular potential”, Vagge said. “Many of these patients suffer stygmatisation also for cultural reasons, and sometimes are denied access to work. These are issues that we have to take into consideration”.
Among the causes of adult strabismus there is also myopia, a refractive condition with significant increase in prevalence, as shown by many studies and reports. For this reason, myopia should not be underestimated even when we deal with strabismus.
MYOPIA AND STRABISMUS
“There are forms of strabismus related to myopia”, Aldo Vagge
33
In the majority of cases patients experience double vision and loss of depth perception, which affect the ability to carry out common daily tasks such as driving or parking the car
➧
Aldo Vagge
InsIghts

pointed out. “In brief, there are two big categories: heavy eye syndrome, or strabismus fixus, and type III acute acquired concomitant esotropia, also called the Bielschowsky type”. The heavy eye syndrome, so called because it was erroneously thought that the eye was heavier, is a form of strabismus associated with high myopias with an axial length usually greater than 27 mm. “It is a form of strabismus characterized by large-angle esotropia and hypotropia, with limitations in the ocular movements, especially abduction and elevation”, he explained. “Thanks to MRI studies, today we know that it is determined by displacement of the superior rectus and lateral rectus muscles. The increased axial length of the eyeball and the development of staphylomatous deformities cause damage to the SR-LR band (like in the SES), with subsequent prolapse of the eyeball in the superotemporal quadrant between the superior rectus and lateral rectus muscles. The consequence is a downward dislocation of the lateral rectus muscle, which leads to reduced abduction and increased infraduction, while the nasal shift of the superior rectus muscle i increases adduction. The end result is significant limitation of the ocular movements of elevation and abduction”. However, it is important to remember that not all axial myopia cases result in strabismus fixus. In some cases, there is no superotemporal displacement of the eyeball and the patient can be treated in the same way we treat a classic divergence insufficiency.

According to Professor Vagge, when dealing with this kind of patients, it is important to include T1-weighted MRI in the evaluation of strabismus. This allows physicians to visualize the muscular displacement angle, which is on average 121°. Surgery is the gold standard treatment for these cases. “In case of muscular displacement and prolapse of the eyeball, the Yokoyama procedure is extremely efficient. It allows us to reestablish the correct position of the lateral rectus and superior rectus muscles by joining them with a non-absorbable suture placed at the equator of the muscle without muscle splitting, 15 mm posterior to the insertion of the muscle. This maneuver is often associated with recession of the medial rectus muscle”, Professor Vagge explained. In these cases, resection of the lateral rectus muscle should be avoided, because it would worsen the prolapse of the eyeball.
Type III acute acquired concomitant esotropia (AACE) is usually associated with more moderate myopia. “As the name suggests, it is characterized by an esotropia with an almost similar angle in the different gaze positions, an often sub-acute onset and good binocular function. It is called type III from a dated classification by Burian and Miller”, he explained. It is also named ‘Bielschowsky type’ after the well-known German ophthalmologist, and it is characterized by divergence-insufficiency esotropia, with a diplopia that begins for distance vision, followed by the involvement of near vision. A very common characteristic is that patients never report the onset of diplopia as acute, but as progressive and
worsening over time, often noticed during night driving. “In these cases it is crucial to perform a dissociative cover test as these patients maintain good fusion and we often tend to underestimate the misalignment angle. In these cases the best and most successful surgical technique is a generous recession of the medial rectus muscles”, he explained.
WHY IS IT IMPORTANT TO TREAT STRABISMUS IN ADULTS?



There are several reasons why strabismus is not always treated in adults. One one hand, there is the misconception that it is too late to treat, or that surgery is too risky and not efficient enough. On the other hand, some consider it as a merely cosmetic treatment. “Performing surgery in adult strabismus means not only realigning the eyes, but also performing a functional treatment that widens the binocular field of vision. It is not a ‘cosmetic’ treatment and I strongly discourage anyone from defining it in this way, also to avoid medico-legal issues”, Aldo Vagge explained.

Another important aspect to remember is that, although adult strabismus surgery is to be considered safe and effective, it is essential to adequately inform patients and discuss their expectations.
To conclude, when asked why is important to treat strabismus, we could answer that “these interventions have objectives, including re-establishing binocular potential, improving or re-establishing correct eye alignment, eliminating or reducing diplopia and improving abnormal head position or ocular torticollis”, Vagge concluded.
34
Performing surgery in adult strabismus means not only realigning the eyes, but also performing a functional treatment that widens the binocular field of vision
Aldo Vagge









































































HYDRATION AND PROTECTION FOR THE OCULAR SURFACE 1,2 Hyalfid® and Hyalfid® gel are 0373 medical devices. Carefully read the istructions for use. 1. Hyalfid® leaflet.; 2. Hyalfid® gel leaflet. Cod. 99002187 - Material intended for healthcare professionals 0,15% FHA 1.0 0,30% FHA 1.0® EYE DISCOMFORT OR DRYNESS? FHA 1.0® HYALURONIC ACID long-lasting moisturizing action 1,2 AMINO ACIDS protective action for the ocular surface
EVERYONE HAS THEIR OWN VISCOELASTIC
Choosing the best OVD according to its surgical function
 By Dr Giuseppe Trabucchi
By Dr Giuseppe Trabucchi
V
Viscoelastics (or OVDs, ophthalmic viscosurgical devices) are a very important tool in the intraoperative phases of many ophthalmic surgeries, especially in cataract surgery. Despite their relatively recent history, viscoelastics have revolutionized surgical practice in ophthalmology and, over time, have evolved with more and more new features and potential, as well as greatly improved surgical safety and efficacy.
The first use of sodium hyaluronate as a viscoelastic in cataract surgery dates back to 1979 by
Drs. Robert Stegmann and David Miller, with subsequent FDA marketing approval of the first OVD in the 1980s.
In general, viscoelastics serve primarily to create and maintain anterior chamber dep th and visibility, protect the corneal endothelium and other intraocular tissues during surgery. They are also very useful in complex cases, such as in mature cataracts, shallow anterior chambers, pseudoexfoliative syndrome (PEX), floppy iris syndrome, or glaucoma surgeries. Selecting the correct viscoelastic is very important when performing cataract surgery, and knowing the rheological properties helps to understand the behavior of these surgical devices and their advantages in order to best use them in specific situations.
THE CHARACTERISTICS OF VISCOELASTICS AND THEIR CLASSIFICATION
An ideal viscoelastic must meet certain characteristics such as not inducing any inflammatory reaction, not being immunogenic, having good viscosity to prevent anterior chamber collapse, having the ability to remain in the eye during surgery and, at the same time, being easily removed at the end of surgery. It must also be able to best protect the endothelium, not obstruct aqueous outflow, be elastic with cushioning properties, and be liquid enough to be injected with a small-diameter cannula.
The market today offers a very wide range of viscoelastics, differentiated by their chemical and physical properties, determined by levels of cohesiveness, viscosity and elasticity.
36
InsIghts
Dr Giuseppe Trabucchi
, ASST Ovest Milanese, Legnano, Milan
Most OVDs, especially those based on hyaluronic acid, follow the principle that if you increase the molecular weight and concentration of the molecules, you also increase viscosity and cohesiveness. This has resulted in a classification of viscoelastics into cohesive and dispersive to describe their intraoperative behavior. Cohesive viscoelastics are characterized by high viscosity and high molecular weight and are more effective in creating and maintaining space during anterior segment surgery and in filling the capsular bag during IOL implantation. They are also easier to remove at the end of the surgical procedure. Dispersive viscoelastics, on the other hand, have lower viscosity and cohesivity: for this reason, they tend to adhere more easily to intraocular structures, providing protection to the corneal endothelium during phacoemulsification. However, they are more difficult to remove after surgery because of their short molecular chains, and postoperative residues can lead to increased intraocular pressure. This classification was then updated by also taking into account zero-shear viscosity and dispersion/cohesion index (CDI): according to this update, viscoelastics are now divided into four
categories: cohesive, with CDI ≥30%asp/mmHg; dispersive with CDI<30%asp/mmHg; and, finally, viscoadaptive and OVD with intermediate viscosity and cohesive behavior.
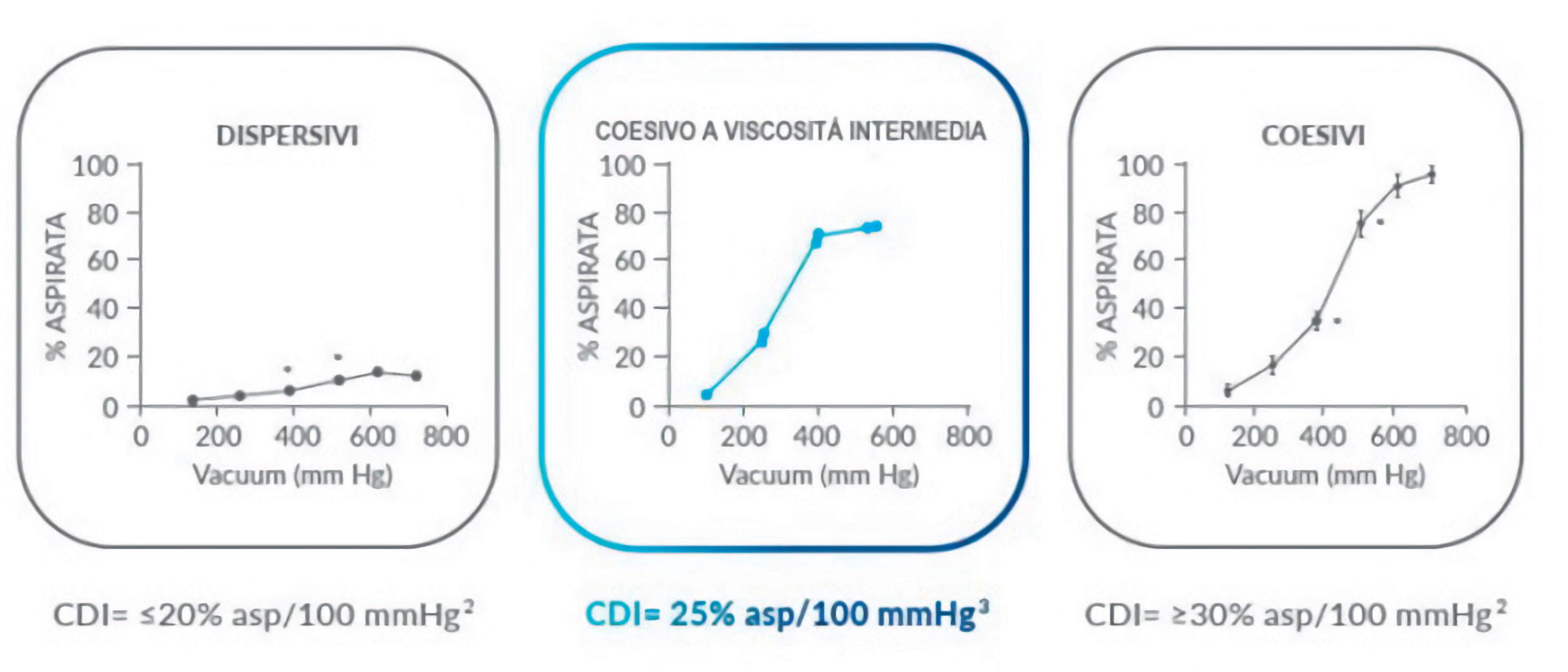
VISCOELASTICS WITH INTERMEDIATE VISCOSITY AND COHESIVE BEHAVIOR
These viscoelastics have recently entered the market and, although they have an intermediate viscosity and CDI between dispersive and cohesive OVS, they have a rheological behavior more similar to the latter. In fact, they allow adequate endothelial protection by creating a sufficiently aqueous environment in front of the lens and, at the same time, they maintain the depth of the anterior chamber where to perform capsulorhexis and distend the capsular bag prior to implantation of the artificial lens without risking impacting intraocular pressure if any residual is left. They also allow easy reconstruction of the anatomical shape of the operated site. These hyaluronic acid-based viscoelastics are particularly useful in standard cataracts because they can be used at all stages of surgery. In addition, because it is a registered MD class III product-like implantables, and prostheses - it can be left in place
and is quickly and physiologically cleared. This provides greater safety because it prevents increased ocular tone after surgery, not forcing the surgeon to perform a paracentesis if the intraocular pressure fails to return to optimal values in a short time. Early postoperative intraocular pressure rise after cataract surgery is a fairly common complication, which is why choosing the correct viscoelastic can best prevent it. Finally, this type of viscoelastic is also suitable for other ophthalmic surgeries, not just cataracts, such as vitreoretinal, glaucoma, post-traumatic ocular surgery, and keratoplasty.
BIBLIOGRAPHY
- Borkenstein AF, Borkenstein EM, Malyugin B. Ophthalmic Viscosurgical Devices (OVDs) in Challenging Cases: a Review. Ophthalmol Ther. 2021;10(4):831-843. doi:10.1007/s40123-021-00403-9;
- Arshinoff SA, Jafari M. New classification of ophthalmic viscosurgical devices--2005. J Cataract Refract Surg. 2005;31(11):2167-2171. doi:10.1016/j. jcrs.2005.08.056;
- Verolino M. Le indicazioni dei viscoelastici in chirurgia oculare. Viscochirurgia 1-2021
37
AN OPTIMAL SOLUTION AGAINST DRY EYE
The importance of the right hyaluronic acid
By Dr Emanuele Erroi, Cardinale Panico Hospital, Tricase (Lecce)
DDry eye syndrome (DED) is a multifactorial condition caused by tear film instability, neurosensory abnormalities, hormonal imbalances, or other comorbidities that can significantly negatively impact the patient in all aspects of daily life. One of the most relevant factors that characterizes the disease process is persistent inflammation, which over time can lead the superficial structures of the eye to suffer progressive and cumulative damage, which in turn can further exacerbate the clinical picture. This creates a real vicious cycle, leading in some cases to the patient suffering from the most severe and painful form of the disease.
THE VICIOUS CIRCLE
Dr Emanuele Erroi

There can be many acute and chronic causes that can trigger or promote the onset of DED, generating not one, but as many as two circular processes that identify such a vicious circle. The main process is triggered by an instability of the tear film, leading to hyperosmolarity that also involves the epithelial cells of the cornea and conjunctiva, stimulating the immune system. The resulting cellular and apoptotic damage stimulates neurogenic and tear gland inflammation, releasing cytokines and increasing tear film instability perpetuating the circle. The secondary process, called the lipid hypothesis, involves inflammation of both the eyelid and the Meibomian glands, cascading changes in the quality of the lipid layer and consequently instability of the tear film, independently feeding the vicious cycle of DED.
Acting on this vicious cycle, it turns out to date to be the main therapeutic approach to stop the course of dry eye syndrome. This can be brought about by protecting the stability of the tear film, ocular surface and eyelid tissues.
ARTIFICIAL TEARS AND HYALURONIC ACID
On medical prescription, administration of a targeted artificial tear can effectively inhibit the inflammatory process underlying the vicious cycle of DED. Among commercially available active ingredients, hyaluronic acid (HA) appears to be one of the most effective in reducing the inflammatory processes typical of dry eye disease.
Naturally produced by our body, this molecule is already contained in large amounts in the connective tissues, and particularly at the ocular level in the aqueous humor, vitreous, and ocular surface tissues. For this very reason, artificial tears containing quality hyaluronic acid are distinguished by their high biocompatibility and tolerability by effectively promoting the restoration of tear film balance.
HYALURONIC ACID IS NOT ALL THE SAME
Not all hyaluronic acid, however, possesses the same characteristics: choosing an artificial tear with low-quality, low-molecular-weight hyaluronic acid may not only be ineffective, but may even have a pro-inflammatory effect. Therefore, it is important to select artificial tears carefully, preferring those containing high molecular weight hyaluronic acid.
38
InsIghts
Scientific studies have shown that in addition to the above properties, high molecular weight hyaluronic acid (HMW-HA) has re-epithelializing potential, reducing cell apoptosis to a greater extent than its low molecular weight counterpart. Among several quality HMW-HA hyaluronic acids on the market, FHA 1.0® is specifically patented for ophthalmology. At a high degree of purity, FHA 1.0® is a pharmaceutical-grade hyaluronic acid with a molecular weight range of 1.1 to 1.7 MDa. In laboratory tests carried out on human corneal epithelial cells, FHA 1.0® demonstrated an excellent viscosity level, with greater moisturizing action than
other types of HA, and an excellent degree of promotion of corneal cell regeneration.
THE PERFECT SOLUTION
A preservative-free tear substitute containing FHA 1.0® at concentrations of 0.15 percent and 0.3 percent can thus be an excellent solution for the treatment and management of dry eye disease from the mildest to the most severe stage. To this can be added the synergistic presence of amino acids to ensure a further enhancement of antioxidant, re-epithelizing and anti-inflammatory action, for a perfect combination against the vicious cycle of the disease.
BIBLIOGRAPHY
- Barabino S, Aragona P, di Zazzo A, Rolando M; with the contribution of selected ocular surface experts from the Società Italiana di Dacriologia e Superficie Oculare. Updated definition and classification of dry eye disease: Renewed proposals using the nominal group and Delphi techniques. Eur J Ophthalmol. 2021;31(1):42-48. doi:10.1177/1120672120960586
- Labetoulle M, Benitez-Del-Castillo JM, Barabino S, et al. Artificial Tears: Biological Role of Their Ingredients in the Management of Dry Eye Disease. Int J Mol Sci. 2022;23(5):2434. Published 2022 Feb 23. doi:10.3390/ijms23052434

39
DRY EYE IN WOMEN
Correlations between eye surface area and hormonal balance: quality of life and possible solutions
By Zazzo Antonioa , Mencucci Ritab , Catanuto Giuseppe
aUniversity Hospital Foundation, “Campus BioMedico”, Rome; bEye Clinic, University Hospital Careggi, NEUROFARBA Department, Florence; cHumanitas Clinical Institution of Catania, Contrada Cubba Marletta, Misterbianco (Catania); eClinical and Community Sciences Department, University of Milan, Milan; fEye Clinic, San Giuseppe Hospital, IRCSS Multimedica, Milan.
TThe pathogenesis of dry eye is complex and multi-factor, accompanied by increased osmolarity of the tear film and inflammation of the eye surface. The main symptoms reported by patients are foreign body sensation, burning, photophobia, blurred vision and itching, causing ocular discomfort, visual disturbances and lubrication problems, which can also lead to corneal damage.1
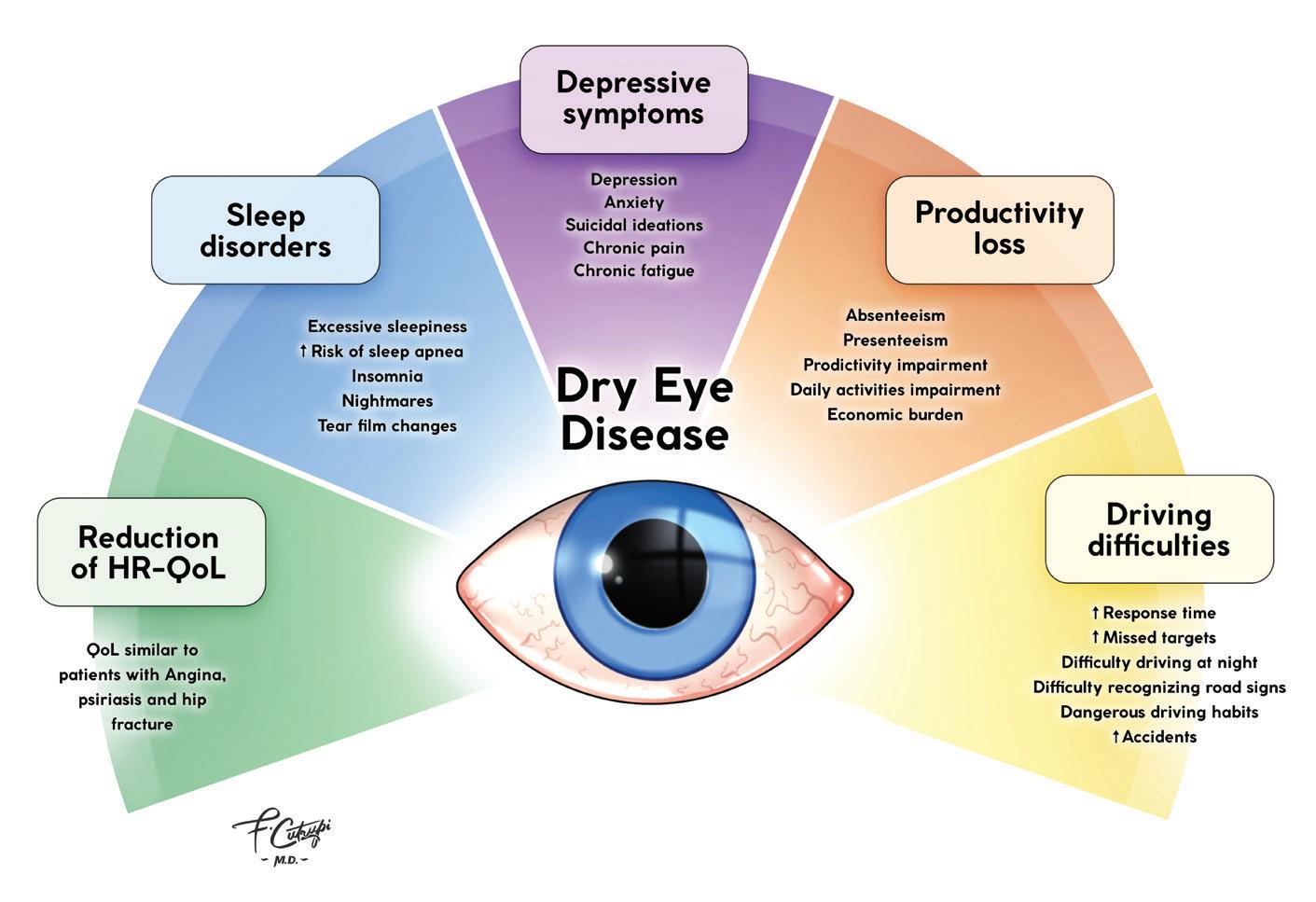
Dry eye disease is a major public health problem, the symptoms of which often interfere with activities such as reading, working on a computer and driving a car (Figure 1). It is generally perceived to be more severe among women, with a greater impact on their well-being.2
The prevalence of dry eye disease shows that women are affected two to four times more often than men of the same age - this gap
is bigger after menopause. These data suggest that sex hormones play an active role in the pathogenesis of the disease.1
Sex hormones are synthesised and secreted into the bloodstream mainly by the gonads (ovaries or testes) and adrenal glands ( endocrine mechanism ), but are also produced by the conversion of steroid precursors in peripheral tissues ( intracrine mechanism ). The eye surface and its adnexa are among the many peripheral tissues that contain the enzymes necessary for the synthesis and metabolism of androgens and oestrogens. 3
Estrogens and androgens appear to have opposite effects in the pathogenesis of dry eye, acting on the eye surface in the regulation of tear secretion and lipogenesis (Figure 2).1,4
40
InsIghts
Figure 1. Impact of dry eye disease on quality of life Courtesy Doctor Francesco Cutrupi
c , Zeppola Teaa , Cutrupi Francescoa , Villani Edoardoe,f
The balance between oestrogen and androgen is important in determining the risk of dry eye.5 Plenty of clinical evidence shows that dry eye disease is related to hormonal alterations and dysfunctions, such as during menopause, following breast cancer and gynaecological cancers as well as in polycystic ovary syndrome (PCOS) During menopause, dry eye is favoured by oestrogen and andro-
gen deficiency, which leads to a reduction in the fluid secreted by the lacrimal glands (Figure 3).4 The morphology of the corneal epithelium is altered by hormonal fluctuations, which has a considerable impact on the eye’s well-being and quality of life. Approximately 50% of post-menopausal women show symptoms related to dry eye.6

Women who undergo breast cancer surgery also suffer from a dra-

stic hormonal change, resulting in psychological and physical effects, such as systemic dryness. This iatrogenic breast cancer dryness (BCID) may be related to functional hyperandrogenism, pharmacologically induced menopause with aromatase inhibitors, or long-term peri-operative chemotherapy, which is often mandatory. Although validated protocols are not yet available, the administration of a subjective symptom questionnaire in conjunction with clinical assessment of the ocular surface is generally recommended among patients receiving more than four cycles of chemotherapy or targeted therapy.8
A study of 64 patients diagnosed with PCOS described the presence of bilateral ocular changes in 20 out of 62 patients (32%). The ocular signs and symptoms occurred about three years after the first ultrasound finding of polycystic ovary, and were conjunctival hyperemia, mild follicular and papillary
41
Figure 3. Expression of oestrogen (A) and progesterone (B) receptors in the lacrimal gland Picture from Figure 3, Ref. 7
Figure 2. Role of oestrogen and androgen on the eye surface Courtesy Doctor Francesco Cutrupi
InsIghts
reactions, mucus hypersecretion and superficial keratopathy (Figure 4) associated with itching, burning and foreign body sensation. The unusual coupling of itching and dryness was considered as a distinct clinical entity associated with hormonal imbalance, designated as Itchy-Dry Eye Associated Syndrome (IDEA).9
For an ophthalmologist, the pre-
structure of the tear film.10 Osmoprotectants play an important role through their ability to protect and restore the osmotic balance of corneal epithelia by counteracting damage to these structures.11 Specifically, recent studies have shown the direct action of L-carnitine on the inflammatory matrix that causes dry eye.12
Also of interest is the synergy
2 Schaumberg DA, et al. Patient Reported Differences in Dry Eye Disease between Men and Women: Impact, Management, and Patient Satisfaction. PLoS ONE. 2013; 8(9):e76121.
3 Truong S, et al. Sex hormones and the dry eye. Clin Exp Optom. 2014; 97:324–336.
4 Sullivan DA, et al. TFOS DEWS II Sex, Gender, and Hormones Report. The Ocular Surface. 2017; 15:284-333.
5 Nkiru Z, et al. Dry eye disease: A longi -
sence of IDEA syndrome may be cause for diagnostic suspicion of PCOS, in the presence of other local signs of hyperandrogenism, such as dry skin, hirsutism, hair loss (very thin and thinning), slight overweight (difficulty in losing weight), dyspareunia, menstrual cycle irregularities and cyclicity of eye symptoms.
Patients with a pathological or iatrogenic hormonal imbalance should be evaluated for dry eye disease, as well as for systemic dryness, in order to restore their social and personal quality of life.8 Only 7 per cent of women with major hormonal changes are treated or see a physician for treatment of the disorder. 6
A careful diagnosis of dry eye and a possible initial intervention with tear substitutes capable of guaranteeing an adequate level of osmoprotection and favouring hydration, would make it possible to re-establish the normal structure of the tear film, leading to a significant improvement in the quality of life of these patients.
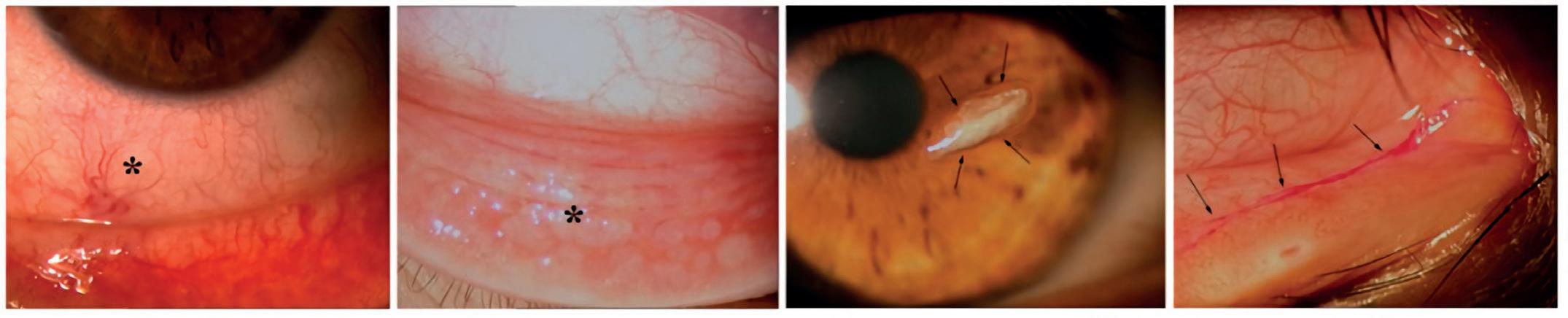
To this end, the use of tear substitutes with hyaluronic acid and osmoprotective components would benefit by restoring the normal
between hyaluronic acid, possibly with a high molecular weight, and carboxymethylcellulose, capable of increasing the viscosity and hydration of the tear film, helping reduce discomfort caused by hormonal alterations.13
CONCLUSIONS
The role of sex hormones on the eye surface is critical, controversial, but undeniably important. Undoubtedly, tear substitutes represent a first aid to improve the quality of life of these patients, but an ever closer collaboration between the various medical specialists is necessary in order to validate a synergistic and multidisciplinary approach. An educational, cultural and communication effort is needed between ophthalmologists, gynaecologists and oncologists, so that all those involved are aware of the impact dry eye disease can have on the patients’ quality of life.
BIBLIOGRAPHY
1 Nuzzi R and Caselgrandi P. Sex Hormones and Their Effects on Ocular Disorders and Pathophysiology: Current Aspects and Our Experience. Int J Mol Sci. 2022: 23:3269
tudinal study among pregnant women in Enugu, south east, Nigeria. Ocular surface. 2019; 17(3):458-463.
6 Nappi RE, et al. Female sexual dysfunction (FSD): Prevalence and impact on quality of life (QoL). Maturitas. 2016; 94:87-91.
7 Gligorijevi ć J, et al. Immunohistochemical detection of estrogen and progesterone receptors in the human lacrimal gland. Arch. Biol. Sci. Belgrade. 2011; 63(2):319-324.
8 Grasso A, et al. Sex Hormones Related Ocular Dryness in Breast Cancer Women. J. Clin. Med. 2021; 10:2620.
9 Bonini S, et al. Itchy-Dry Eye Associated with Polycystic Ovary Syndrome. Am J Ophthalmol. 2007; 143(5):763-771.
10 Jones L, et al. TFOS DEWS II Management and Therapy Report. The Ocular Surface. 2017: 15: 575-628.
11 Simmons PA and Vehige JG. Investigating the potential benefits of a new artificial tear formulation combining two polymers. Clinical Ophthalmology. 2017; 11:1637–1642.
12 Shoari A, et al. Inhibition of matrix metalloproteinase-9 for the treatment of dry eye syndrome; a review study. Exp Eye Res. 2021; 205:108523.
13 Hua X et al. Effects of L-carnitine, Erythritol and Betaine on Proinflammatory Markers in Primary Human Corneal Epithelial Cells Exposed to Hyperosmotic Stress. Curr Eye Res. 2015; 40(7): 657–667.
42
Figure 4. Slit-lamp examination of the ocular surface Images taken from Fig. 1 of Ref. 9. Patients with PCOS and ocular symptoms (N=20) had (asterisks) conjunctival hyperemia (A) and follicular reactions (B). In 23.53% of the patients, mucus filaments (arrows) were identified on the corneal epithelium (C) and conjunctival epithelium by staining with rose bengal (D).
Lens for myopic progression management in children and adolescents
Myopia is becoming an increasingly widespread problem worldwide.
To answer this problem Ital-lenti has developed MYOPICA, an innovative lens with defocus peripheral made with “Perifocal” technology, with aim of limiting the development of myopic progression in children and adolescents.

www.itallenti.com FOR MYOPIC PROGRESSION MANAGEMENT
Optics
by Laura Gaspari
MYOPIA MANAGEMENT: ESSILORLUXOTTICA AND WSPOS TOGETHER TO RAISE AWARENESS
The WSPOS educational material is now available on the Leonardo platform
EEssilorLuxottica’s commitment in the field of myopia management is going a step further by joining forces with the World Society of Paediatric Ophthalmology and Strabismus (WSPOS), with the aim of advancing knowledge of myopia management globally.
“We are pleased to continue our long-standing partnership with WSPOS, an organization that shares our vision to contribute to better vision for children. As part of our partnership to advance myopia education, the WSPOS medical education program content on myopia management is available globally for eye care professionals through our learning platform, Leonardo,” said Olga Prenat, Head, Medical and Professional Affairs and Vision Care Education, EssilorLuxottica. A digital supplement, three e-learning modules and three 60-minute webinars will be also available on the platform.

Leonardo, which is EssilorLuxottica’s open learning digital platform, provides the vision care industry with content designed and taught by industry experts to further educate and help eye care professionals successfully integrate myopia management in practice, and guide their patients on how to best manage their myopia.
EssilorLuxottica and WSPOS have developed a strong partnership since 2020 to sustain their long-standing efforts to advance evidence-based myopia education globally. “Myopia management is an extremely important component of WSPOS’s public health initiatives and we are delighted to have support from EssilorLuxottica for our Myopia IME,” said Dr. Ken K. Nischal, WSPOS Co-founder and Division Chief, Pediatric Ophthalmology, Strabismus, and Adult Motility, Professor of Ophthalmology at the University of Pittsburgh, School of Medicine.
Moreover, EssilorLuxottica is committed to share knowledge and insights on myopia control interventions such as the Essilor Stellest lens, actively participating in WSPOS annual congresses and sub-specialty days. EssilorLuxottica is also a gold-level supporter of the WSPOS independent medical education program.
“We look forward to accomplishing more together this year to contribute to widespread adoption of myopia management,” Prenat concluded.
44
LA MIOPIA IN ETÀ PEDIATRICA E IL CONTROLLO DELLA SUA PROGRESSIONE
Aspetti fisiopatologici e soluzioni disponibili
Luigi Mele, Andrea Piantanida, Mario Bifani
STUDIO DELLA MOTILITÀ OCULARE
Dalla teoria alla pratica

Andrea Giuffrè
LA PATOLOGIA OCULARE MIOPICA

Dalla prevenzione al contenimento della progressione
Pasquale Troiano
FALSA DISGRAFIA E VIZI VISUO-POSTURALI CORRELATI

Postura di scrittura e funzione visiva: educazione, prevenzione, valutazione e recupero

Coralie Delliponti
Valerio Lupi
Redazione: Strada 4 Milano Fiori, Palazzo Q7 – 20089 Rozzano (MI)
Sede operativa: FGE srl − Regione Rivelle 7/F − 14050 Moasca (AT) Tel. 0141 1706694 – Fax 0141 856013 e-mail: info@fgeditore.it − www.fgeditore.it

Ordina la tua copia su www.fgeditore.it
HOYA SURGICAL OPTICS: INNOVATIVE SOLUTIONS DEDICATED TO CATARACT SURGERY
HHOYA Surgical Optics, whose products are used by eye surgeons around the world, is a world leader in the development of preloaded intraocular lenses to meet different surgical needs and methods. Always at the forefront with a range of products with unique features, HOYA Surgical Optics works closely with surgeons and patients to better
Flavio Longato Business Development Director EMEA HOYA Surgical Optics

NANEX multiSert+TM
understand their needs. With over 10 million intraocular lenses sold worldwide, HOYA Surgical Optics has won the trust of surgeons thanks to its quality and dedication.
Among our flagship products, we present the two novelties Vivinex™ Impress™ and Vivinex™ Gemetric™ in addition to the well-known NANEX multiSert +™.
Nanex multiSert +™ is the world’s smallest injection system for hydrophobic preloaded C-loop intraocular lens and designed for incisions up to 1.8 mm. With its innovative design it allows the surgeon to perform cataract surgery with sub-2.2 mm incisions without compromise.
Thanks to its active oxygen surface treatment system, the material of which Nanex multiSert +™ is made demonstrates strong capsular adhesion and a significant reduction in PCO compared to an untreated surface. Nanex multiSert +™ is a 4-in-1 preloaded system that provides several options available to the surgeon: push injection and screw injection in a single device, designed to allow fluid release of the lens compared to other injection systems and to mitigate the possibility of abrupt release.

46 Industry news
Vivinex™ Impress™
HOYA Surgical Optics introduces Vivinex Impress™ the new preloaded “Enhanced Monofocal” intraocular lens. Vivinex Impress™ is a monofocal lens with an extended depth of focus to allow a better vision at intermediate distance.

Vivinex Impress™ uses the preloaded multiSert +™ 4-in-1 system which provides several options available to the surgeon: push injection and screw injection in a single device, designed to allow fluid release of the lens compared to other injection systems and to mitigate the possibility of abrupt release.
Vivinex™ Gemetric™
The innovative Vivinex™ Gemetric™ hydrophobic glistening-free trifocal lens preloaded into the proven multiSert™ injector, offers unmatched patient vision and exceptional rotational stability. Equipped with proprietary technology, it is available in two versions (Gemetric™ and Gemetric™ Plus) to adapt to the visual needs of different patients and is also available in a toric version.
Among the benefits of this innovative trifocal IOL we could report the material of which it is composed, acrylic, hydrophobic and glistening free, the proprietary aspheric design of the optics, which greatly improves image quality. In the presence of decentration, coma is less in HOYA Vivinex™ Gemetric™ than in leading competitor IOLs for a pupil diameter of 4.0mm. It is also possible to precisely calculate the power of the cylinder with the help of the new HOYA Toric Calculator 4.3.
Sight as a primary interest for HOYA Surgical Optics
At HOYA Surgical Optics, we empower eye surgeons to improve the vision and quality of life of millions of people with cataracts, to help them celebrate life, visually. Our products are known for offering safety, reliability and easiness of use. Quality, trust, dedication and attention to detail are deeply rooted in our Japanese heritage and in the HOYA brand.
As our claim defines, we are focused on the individual needs of the surgeon and patient. At the same time, we have a global reach by engaging in the distribution of our preloaded lenses throughout the world.
47
AGE-RELATED
DEGENERATION


Presidente
Marcella Nebbioso (Roma)
Vice presidente
Emilia Gallo (Catania)
Segretario scientifico



Maria Rosaria Franco (Lecce)
Sponsor management
Patrizia Costanzo
Coordinamento segreteria on-site
Motus Animi
Consiglieri
Federico Bartolomei (Bologna)
Rocco Di Lorenzo (Palermo)
Luigi Donato (Messina)
Federica Franzone (Torino)
Paolo Giuseppe Limoli (Milano)
Marco Ulisse Morales (Padova)
Erika Rigoni (Latina)
Sergio Zaccaria Scalinci (Bologna)
Lucia Scorolli (Bologna)
Antonella Sidoti (Messina)
Gianfrancesco Villani (Verona)
Enzo Maria Vingolo (Roma)
MACULAR
Updates in ambito riabilitativo e clinico-terapeutico XXII CONGRESSO NAZIONALE DI IPOVISIONE www.lowvisionacademy.org
Consulta il programma preliminare Segreteria Organizzativa e Provider ECM Reg. Rivelle 7/F - Moasca (AT) Tel. 0141 1706694 - Fax 0141 856013 info@fgeditore.it Segreteria on-site 29-30 settembre 2023 LECCE HILTON GARDEN HOTEL Via Cosimo De Giorgi, 62 20 CREDITI ECM Acquisibili tramite corso FAD ECM BORSA DI STUDIO NICOLA PESCOSOLIDO* ALLA MIGLIORE TESI DI SPECIALIZZAZIONE O DOTTORATO IN OFTALMOLOGIA AA 2021/22












SCOPRI PERCHÉ È IMPORTANTE CONTROLLARE GLI OCCHI SIN DAI PRIMI ANNI DI VITA! 10/10 9/10 8/10 Lions Clubs International MULTIDISTRETTO 108 - ITALY Campagna di prevenzione dell’ambliopia INIZIATIVA PROMOSSA DA Con il patrocinio di Una iniziativa Lions Clubs International MULTIDISTRETTO 108 - ITALY LA VISIONE NEL istruzioniBAMBINO: per l’uso Manuale pratico per genitori consapevoli Puoi richiedere n. 50 copie gratuite da mettere a disposizione dei tuoi pazienti in sala d’attesa Richiedi gli opuscoli a: info@fgeditore.it ADERISCI ANCHE TU! www.sightforkids.it Con il sostegno di La soluzione oftalmica per la gestione della progressione miopica
GLAUCOMA: INNOVAZIONE NELLA NEUROPROTEZIONE




















































































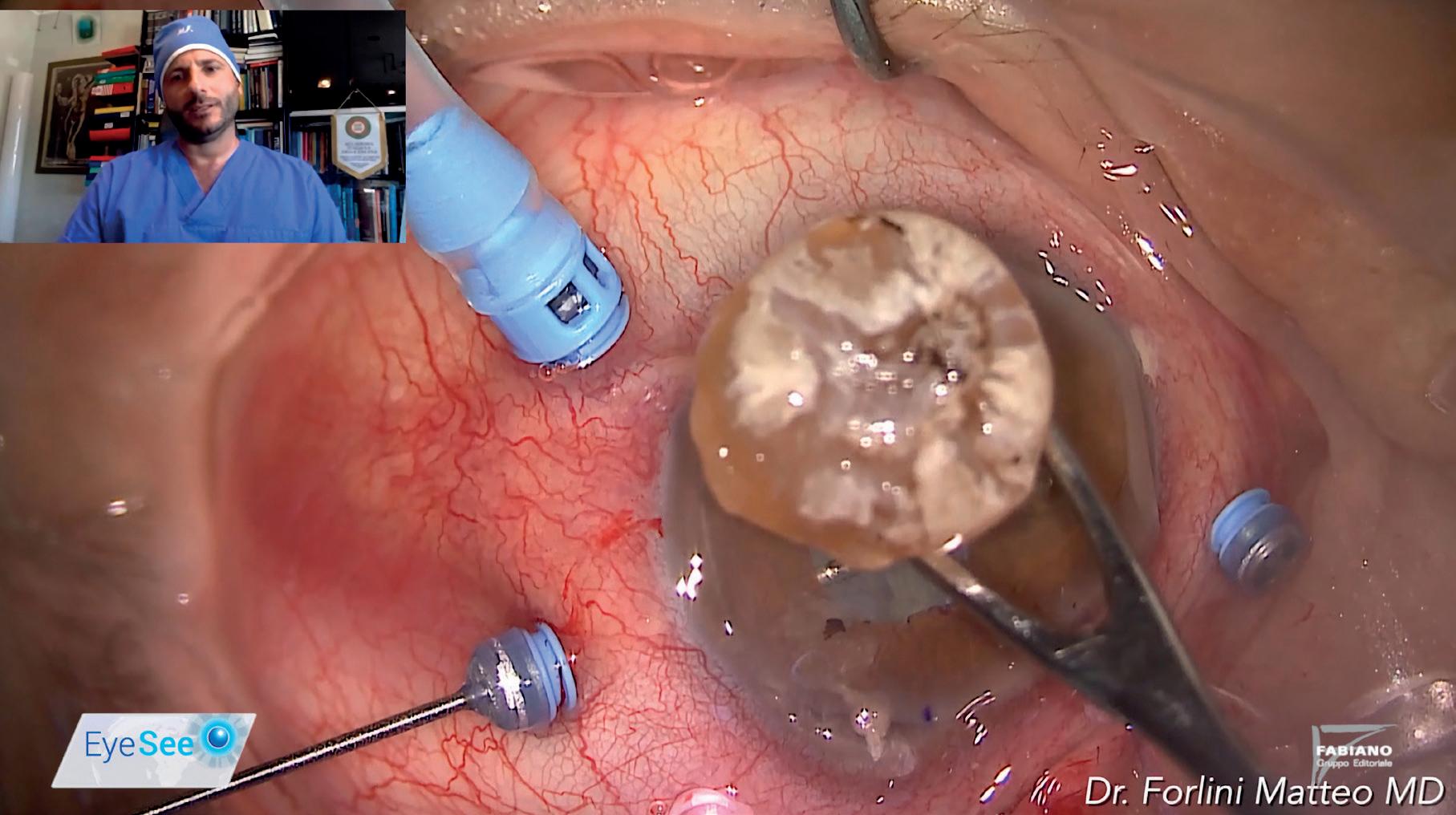





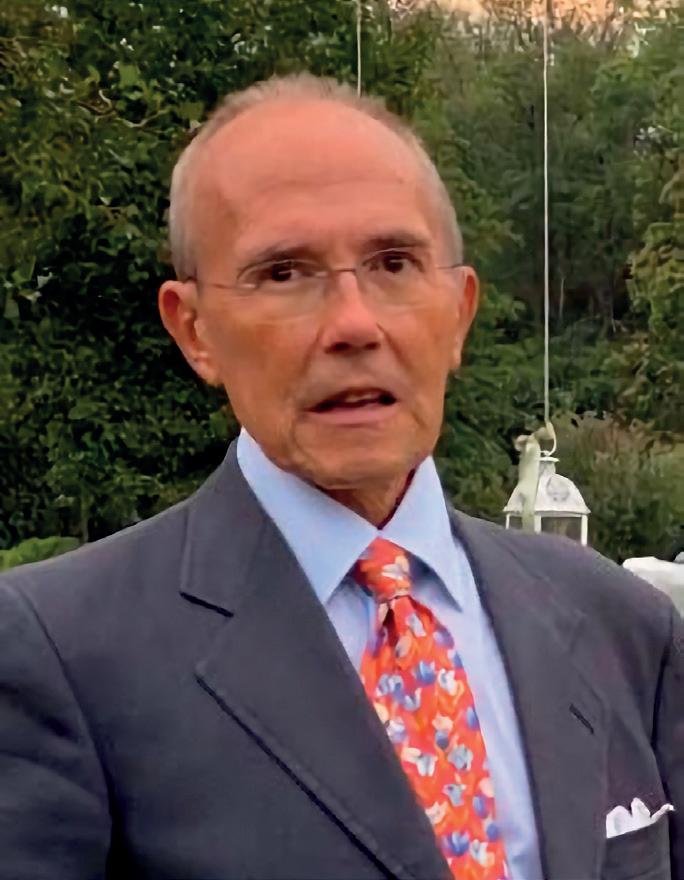









































































 By Dr Giuseppe Trabucchi
By Dr Giuseppe Trabucchi