The cycle of life

















It is fitting that in this edition, with a women’s health theme, we cover the breadth of female reproductive life, from having babies to the ‘change of life.’
Our profile on fertility specialist Dr Tamara Hunter brings home the fact that while some women can fall pregnant in the blink of an eye – weren’t we warned about that in school sex ed classes? – for others having a baby remains elusive.

IVF has been a huge game-changer but fertility treatments can come at a high price, financially and emotionally. And there are no guarantees that a bouncing baby will be forthcoming.
Having children is regarded as a pivotal life event by many people – and even the gender-reveal of the unborn baby has been turned into a social media event, complete with secretly coloured balloons and cakes.
At the other end of the reproductive spectrum is menopause – a bit less exciting but a time of great relief for some women who no longer have to worry about monthly periods or contraception.
However, as our feature story explores, it can be anything but smooth sailing for women with significant and debilitating symptoms. Many are left to ‘put up with it’ for fear of talking openly about what is still considered secret women’s business.
Perhaps the ‘change of life’ needs an image make-over. With the feminisation of the workforce, menopause is increasingly impacting on many women while they are still working or enjoying productive lives. A bit of support can go a long way.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment. Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
However, [menopause] can be anything but smooth sailing for women with significant and debilitating symptoms. Many are left to ‘put up with it’ for fear of talking openly about what is still considered secret women’s business.
FEATURES
12 Let’s talk about menopause

16 Script rules demand common sense
18 Diabesity – chronic disease or lifestyle choice
24 Close-up – Dr Tamara Hunter

LIFESTYLE
58 Doing good in a better way
60 Deep-sea discoveries
61 Wine review: Singlefile Wines
– Dr Craig Drummond
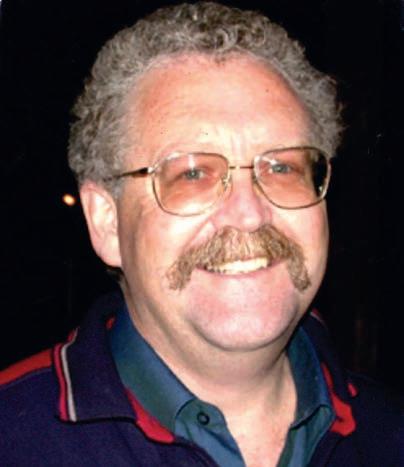
Cover picture: Dr Tamara Hunter
1 Editorial: Supporting women for the long haul – Cathy O’Leary

4 News & views
8 In brief
22 Health-care spiral

29 RNA and ovarian cancer
41
The lucky winner of the March doctors dozen wines from Cape Mentelle is Dr Diane Comley, left, from the Royal Flying Doctors Service WA. And Dr Alison Stanning is in for a laugh, winning a double ticket to Georgie Carroll’s show at this month’s Perth Comedy Festival.

In this edition, we have a great selection of wine from Singlefile in the Great Southern to be won. See Dr Craig Drummond’s review, including his take on the range’s flagship Cabernet Sauvignon, on page 61.
To enter go to the competitions link at www.mforum.com.au or use the QR code on this page.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au

EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au


Journalist Eric Martin 08 9203 5222 eric@mforum.com.au



Clinical Editor Dr Joe Kosterich 0417 998 697 joe@mforum.com.au



Marketing Rhiannon Arnold rhiannon@mforum.com.au





Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Andrew Bowyer 08 9203 5222 andrew@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222
Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au
OUR



He opted for voluntary assisted dying after spending his last four years staring down Progressive Supranuclear Palsy.
As readers of Medical Forum will instinctively know, PSP never takes kindly to defiance, but as readers will also know, Rob could do defiance pretty well.
In life, as in the moment of his passing, his business partner and partner in life, Jenny McEvoy (yes, the knot was tied at a wonderful, intimate ceremony several years ago), was right by his side. Medical colleagues will all have their own Rob McEvoy story. He was blunt, at times forceful, in his opinions on all subjects that affected his beloved profession and magazine. He was fiercely committed to the values of medicine – the healing part, where the patient in front of him took precedence over pretty much everything else.
Researchers at Curtin University have identified the genetic signature of pre-malignant liver cells, offering hope to the almost 3000 Australians diagnosed with the deadly cancer each year.
The study, published in the journal Cell Genomics, found that quantifying pre-malignant liver cells in patients with liver disease could help determine their future risk of developing cancer.
First author Dr Rodrigo Carlessi, from Curtin Medical School and Curtin Health Innovation Research Institute, said the discovery had the potential to save lives by changing how chronic liver disease patients are staged and monitored, based on their cancer risk.
“The research used cuttingedge technology to identify the molecular fingerprint of thousands of genes, one cell at a time,” Dr Carlessi said.
“During this process, we discovered
He was a fearless champion for the undervalued and underappreciated general practitioner, of which he was one for the first 30 years of his career, and he had a distrust of the business of medicine – partly
because he felt awkward about the transactional aspects of it, and partly because he could see how it could erode the very values he held dear.
Rob and Jenny started Medical Forum, in its current form, 23 years ago as an independent, ethical free-to-readers news magazine for West Australian doctors – every WA doctor they could find. When I began working at the magazine as managing editor in 2012, I had to memorise and incant daily –independent, ethical, local and, not irregularly, no conflict of interest. Those underlying publishing values have seen the magazine become staple reading for WA doctors and a valued voice for the medical profession.
Vale Dr Rob McEvoy, your legacy lives on.
 By Jan Hallam
By Jan Hallam
the genetic signature and its diagnostic value, which was subsequently confirmed in several hundred individual patient liver samples.
“This finding is significant because it gives us a vital piece of the puzzle that could pave the way for a new diagnostic test for liver cancer, which causes 10% of all cancerrelated deaths in Australia.”
Colleague Professor Nina TirnitzParker, also from Curtin, said liver cancer was often diagnosed late in Australians.
“Due to a lack of readily available and accurate laboratory tests or biomarkers, many patients of advanced liver cancer live less than 12 months as treatment options are limited when patients are diagnosed at later stages,” she said.
A series of programs for people with eating disorders is getting underway in WA.
The Body Esteem Program,
developed and run by Women’s Health and Family Services, is the only community-based peer program in WA supporting people with eating disorders.
More than one million Australians are living with an eating disorder and less than a quarter receive treatment or support.
The WA program offers peer support groups including a youth program starting in May for 16-20 year olds (all genders, all eating disorders); a youth carer program also starting in May, an adults program for all genders aged 18 and over, starting in July; and an online program for rural and remote people (all genders, aged 18 and over, all eating disorders).
BEP is a free service for people with eating disorders such as anorexia nervosa, bulimia nervosa, binge eating disorder or other specified feeding and eating disorders.
It has been specifically designed to enable participants to take personal
continued on Page 8
Dr Rob McEvoy, co-founder of this magazine, died on Monday, April 17 with the same courage and determination in which he lived.
The
Iron deficiency anaemia is a common condition that can have a significant impact on a patient’s quality of life. The incidence of iron deficiency anaemia in Australia is estimated to be 12% in non-pregnant and up to 15% of pregnant females.1 Iron deficiency without anaemia may be up to three times more common but is often undiagnosed. 2
While oral iron therapy is often the first-line treatment, some patients are unable to tolerate it due to gastrointestinal side effects or poor absorption. 3 In these cases, iron infusions may be a suitable alternative.
A common iron infusion therapy in Australia is ferric carboxymaltose (FCM). FCM is a complex of iron and carbohydrate that is administered intravenously and has been shown to be safe and effective in treating iron deficiency anaemia in patients who are unable to tolerate oral iron therapy. 4
However, there have been reports of symptomatic hypophosphatemia associated with FCM use. This is a rare condition where the levels of phosphate in the blood are abnormally low, which can cause a range of symptoms including weakness, fatigue, and bone pain.
By Associate Professor Chris Barnes MBBS, FRACP, FRCPA
Associate Professor Chris Barnes is the National Director of Clinical Pathology and provides strategic direction nationally for haematology at Clinical Labs. He is a clinical and laboratory-trained haematologist who has worked with Melbourne Hematology and Clinical Labs (and previously Healthscope) for several years. A/Prof Barnes also works at the Royal Children’s Hospital and is director of the Haemophilia Treatment Centre. He has experience in both management and leadership positions. A/Prof Barnes has an active clinical research interest and is also the director of Melbourne Haematology (Clinical) and Melbourne Paediatric Specialists.
It is thought to occur due to the rapid increase in fibroblast growth factor 23 (FGF23) which increases phosphate secretion. Prolonged hypophosphatemia and associated secondary hyperparathyroidism may be a risk factor for metabolic bone disease, including the development of ostemalacia.
To help manage this potential risk, doctors may consider monitoring serum phosphate, calcium, vitamin D, and parathyroid hormone (PTH) levels in patients who present with symptoms following FCM infusions. If symptomatic hypophosphatemia occurs, treatment may include phosphate and vitamin D supplementation, along with discontinuation of FCM use.
Despite this potential risk, iron infusions with FCM can offer significant benefits for patients who are unable to tolerate oral iron therapy. By restoring iron levels in the body, patients may experience improved energy levels and improved quality of life. Clinical review and laboratory monitoring for side effects are recommended in patients who present with concerning symptoms following iron infusion.
References
1. Pasricha S-RS, Flecknoe-Brown SC, Allen KJ, Gibson PR, McMahon LP, Olynyk JK, et al. Diagnosis and management of iron deficiency anaemia: a clinical update. Medical Journal of Australia. 2010;193(9):525-32.
2. Ioannou GN, Rockey DC, Bryson CL, Weiss NS. Iron deficiency and gastrointestinal malignancy: a populationbased cohort study. Am J Med. 2002;113(4):276-80.
3. Tolkien Z, Stecher L, Mander AP, Pereira DIA, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0117383-e.
4. Bailie GR. Efficacy and safety of ferric carboxymaltose in correcting irondeficiency anemia: a review of randomized controlled trials across different indications. Arzneimittelforschung. 2010;60(6a):386-98.



St John of God Subiaco Hospital recently farewelled retiring general physician Associate Professor David Watson after 45 years of service.
SJOG Subiaco has confirmed plans for an emergency department are still on the table. A proposed expansion, which includes a new clinical block, has capacity for an ED to cater for future demand. Plans are with the State Development Assessment Unit.
Dr Zoe Bradfield from Curtin University’s School of Nursing will lead a clinical trial offering first-time mothers melatonin tablets in a bid to reduce rates of induced labour. It is funded by the National Health and Medical Research Council’s Medical Research Future Fund.

The MRFF has also allocated $5m to Perth-led research trying to solve the genetic mystery that causes rare conditions. UWA’s Associate Professor Gina Ravenscroft at the Perkins Institute will lead teams from nine universities and institutes.
Finalists in the 2023 HESTA Australian Nursing and Midwifery Awards include Richmond Wellbeing’s MH Connext, which supports people in mental distress. Specialised mental health nurses work with GP clinics, and have received more than 1500 referrals from 300 GPs across Perth.
Cancer Council WA has awarded researcher Professor Jenette Creaney $480,000 over four years to look at treatments for people with lung cancer and mesothelioma.
continued from Page 4
control of their recovery using the support and learned experience of peer-facilitators.
For more information or referrals go to whfs.org.au/services/eatingdisorders/
The immune-boosting power of a healthy gut microbiome is being harnessed in an Australian-first “poo transplant” trial aimed at saving the lives of severely ill blood cancer patients and meeting an urgent need for new treatments.
The clinical trial is being led by QIMR Berghofer clinician-scientist Dr Andrea Henden at the Royal Brisbane and Women's Hospital,
using a biological product made by Australian Red Cross Lifeblood from the Rotary WA Health Innovation Centre in Perth.
Faecal microbiota transplant is emerging as a potential treatment for a range of conditions. Trillions of gut microbes from the stool of a healthy donor are transferred into a patient to replenish their depleted gut microbiome and improve their immune response to fight disease.
This is the first time FMT will be trialled in Australia in blood cancer survivors who have developed severe Graft-versus-Host-Disease, which is caused by their lifesaving bone marrow transplant when donor immune cells attack the recipient’s organs and tissues.
“A bone marrow transplant can be a double-edged sword. It saves
continued on Page
St John of God Murdoch Hospital has become first hospital in Perth to introduce a type of robotic surgery technology to replace worn knees.
The VELYS Robotic-Assisted Solution helps surgeons perform knee replacement surgery that can be tailored to each patient, and is designed to provide digital precision and accuracy to get them mobile quickly.
Orthopaedic surgeon Associate Professor Chris Jones, who played an advisory role in the robot’s development, performed the first knee replacement surgery in WA using the VELYS system at SJOG Murdoch.

The technology is designed to help surgeons achieve a well-balanced and precisely positioned total knee replacement, without the need for preoperative CT scans.
Health Networks’ Cancer Network contribution to cancer information for culturally and linguistically diverse consumers was recognised at the recent WA Multicultural Awards.
On average, SJOG Murdoch does about 1300 total knee replacements a year, with this number predicted to increase rapidly over the coming years due to the ageing population and obesity crisis.
The robotic system is also being installed at several other SJGHC hospitals including Bunbury, and Geelong and Ballarat in Victoria.
Fact: 1-in-4 women suffer from heavy periods.1
As recommended in the Heavy Menstrual Bleeding Clinical Care Standard, uterine-preserving procedures should be the first-line surgical treatment for women who have completed their childbearing.2 Informed choice is also recommended. When presenting options to your patients, consider the NovaSure® endometrial ablation:

5 minute procedure*
Minimally-invasive alternative to hysterectomy
Effective in 9-in-10 patients3–4
www.novasure.com
4. NovaSure® Instructions for Use. Bedford, MA: Hologic, Inc. ADS-03338-AUS-EN Rev.001. ©2021 Hologic, Inc. All rights reserved. Hologic, NovaSure and associated logos are trademarks and/or registered trademarks of Hologic, Inc. and/or its subsidiaries in the United States and/or other countries. This information is not intended as a product solicitation or promotion where such activities are prohibited. Because Hologic materials are distributed through websites, eBroadcasts and tradeshows, it is not always possible to control where such materials appear. Hologic (Australia and New Zealand) Pty Ltd, Suite 302, Level 3, 2 Lyon Park Road, Macquarie Park NSW 2113. Tel. +61 2 9888 8000. ABN 95 079 821 275.
continued from Page 8
the lives of people with aggressive blood cancers but can then take their lives by causing GVHD,” Dr Henden said.
“GVHD is particularly hard to treat in the gut, with patients often hospitalised for long periods of time where they are dependent on hospital care and intensive immune suppressing medications. Conventional immune-suppressing steroid medication fails to work in half of all GVHD patients.
“FMT is a really exciting new approach that could save lives. If we can restore a healthy gut microbiome in these patients, we can potentially influence immune function in the gut and treat the GVHD in a safer way that preserves the patient’s immunity.”
Lifeblood is at the forefront of FMT development in Australia, becoming the first licensed FMT manufacturer 18 months ago, and now offering the product to hospitals Australia-wide.
Just like blood donors, microbiota donors are screened. Stool is collected from volunteers and then processed and tested at Lifeblood’s TGA-licensed facility before being supplied to researchers and clinicians.
The research also hopes to discover if a specific microbe or its derivative is responsible for improving GVHD during faecal transplant, with a goal of eventually being able to offer patients a simpler targeted supplement or tablet that treats their disease.
New information uncovered by the trial could lead to more effective treatments for conditions such as Crohn’s disease and ulcerative colitis.
A study into the safety and effectiveness of painkillers to treat low-back pain has raised questions about their value.
The evaluation of analgesic medicines for acute, nonspecific low-back pain found that uncertainty remained around their overall impact on pain relief and safety.
The study, published in BMJ, looked at 69 different medicines or

Organ donor activist Simone McMahon – WA’s Young Australian of the Year for 2008 – passed away last month at the age of 40. Born with poor kidney function and suffering chronic renal failure by the age of nine, Simone had a kidney transplant when she was 11. After becoming unwell about 15 years ago, she was forced back onto dialysis. After failing to find a new kidney on the living donor transplant list, she then went on a deceased donor list.
Simone spent her life promoting organ and tissue donation and was a wish granter with the Starlight Foundation, spending much of her time supporting seriously ill children.
She was also a law graduate and Churchill Fellow recipient, whose scholarship allowed her to identify successful international models of organ and tissue donation and look at ways to support transplant
recipients, donor families and living donors.
Simone volunteered for Transplant Australia, later becoming the founder and CEO of Organ Donation and Transplant Foundation of WA. She was made a Member of the Order of Australia in 2013.
Vale Simone.
combinations of analgesics. These included non-steroidal antiinflammatory drugs, paracetamol, opioids, anticonvulsants, antidepressants, skeletal muscle relaxants and corticosteroids, to compare their effectiveness for adults with acute low-back pain.
The review concluded that clinicians should take a cautious approach in the use of analgesics and make treatment decisions in consultation with patients to address their specific causes of pain, severity of symptoms and individual preferences.
Dr Matthew Bagg, a research fellow at Curtin University, the Perron Institute and NeuRA, had a leading role in setting up the study and supervised it.

“Using meta-analysis, this has been the most comprehensive evaluation of its kind to inform clinical decision-making,”
Dr Bagg said.
“It's encouraging that these study results indicate the
kind of trials that are necessary. At the completion of each new trial, we’ll systematically update the overall evidence base.”
Researchers found that while analgesics could provide effective pain relief for some patients, the impact on individual patients varied. They said it was important for clinicians to take into account patients' medical histories and tolerance for side effects to determine the most effective and safe treatment.
Back pain continues to be the number one cause of disability worldwide. According to the Royal Australian College of General Practitioners, musculoskeletal concerns are the second-most common reason for GP visits, after psychological concerns.
Most people who visit their doctor for acute non-specific low back pain, defined as low-back pain lasting fewer than six weeks, are prescribed an analgesic to manage their symptoms.
Updates in endocrine therapy for metastatic hormone receptor positive advanced breast cancer management and mechanisms of overcoming endocrine resistance.
The oestrogen receptor has been a molecular target for treatment in this breast cancer (BC) subtype for over four decades, since the development of the selective oestrogen receptor modulator (SERM), Tamoxifen. This was followed by aromatase inhibitors (AI) and selective estrogen receptor degrader (SERD), fulvestrant. As hormone receptor (HR) positive advanced breast cancer (ABC) utilises estrogen to support and promote its growth, it is a powerful target of therapy and the mainstay of first and subsequent line treatment.
Treatment resistance, however, remains a challenge for patients with the majority of patients having metastatic disease that progresses despite an initial response.
Patients who have had previous earlystage treatment may have primary resistance (relapse within 2 years of commencing adjuvant therapy) or secondary resistance (relapse after two years of commencement of endocrine therapy). The patient is considered to have endocrine sensitive disease if there is a minimum of twelve months of remaining disease-free after adjuvant therapy completion.
One of the mechanisms of resistance stems from mutations in the breast cancer cell genome. The most well documented targetable acquired mutations include the oestrogen receptor mutation (ESR1), at the oestrogen binding domain, and altered regulation of the cell cycle including cyclin D1 and CDK4/6 overexpression. PIK3CA gene mutation is another targetable mechanism of resistance. These mutations can be detected in up to 40% of treated ER positive ABC. Other mechanisms of resistance include loss of ER expression and other cellular growth signal pathway molecules such as upregulation of mTOR.
In cases of de novo or relapsed estrogen receptor positive metastatic BC, the current evidence is to

BCRC-WA breast medical oncologist and education lead Dr Beecroft completed her medical oncology training in WA after completing a fellowship at the Breast Cancer Research CentreWA in 2021. She is currently working as a medical oncologist at BCRC-WA and is involved in investigator-initiated local research.
commence treatment with an AI and a CDK4/6 inhibitor (ribociclib, palbociclib or abemaciclib) based on multiple phase III trials confirming benefit. There have been no head to head studies comparing the different CDK 4/6 inhibitors and all are PBSsubsidised. The MONALEESA-2 trial updated in 2022, with a median follow up of 6.6 years has seen an improvement in overall survival from 51.4 months to 63.9 months with the addition of ribociclib to letrozole v letrozole and placebo. There is no overall survival data yet for palbociclib or abemaciclib, but both treatments have progression free survival benefits and are used in clinical practice.
CDK4/6 Inhibitors
CDK4/6 inhibitors have shown to be effective, even in heavily pretreated patients. In patients with endocrine resistant disease, the first line therapy of choice is a CDK4/6 inhibitor combined with a SERD. The MONARCH2 trial with abemaciclib, which exclusively enrolled endocrine resistant patients for first line metastatic therapy (approximately 25% had primary resistance) has an overall survival benefit when combined with fulvestrant of 9.4 months compared with fulvestrant alone. Ribociclib and palbociclib have also shown efficacy in endocrine resistant patients when combined with fulvestrant. All three agents have been PBS subsidised for use with fulvestrant in endocrine resistant disease.
Selective estrogen receptor degraders (SERDs) have proven efficacy in ESR1 mutation, as it degrades the receptor, thereby blocking nuclear signalling. Two examples include fulvestrant or newer oral agent, elacestrant.
Elacestrant was recently reported in the EMERALD trial as an effective single agent in patients pre-treated with ≤ 2 lines of endocrine therapy (including CDK4/6 inhibitors) with a 12 month PFS rate of 22.3% in the treatment arm v 9.4% in the standard of care arm. This benefit was seen regardless of ESR1 mutation status, but a stronger effect was seen in this subgroup. It is not currently available as PBS-subsidised treatment.
Growth signalling pathways in breast cancer cells are another molecular target. PIK3CA can be targeted with alpelisib. In the SOLAR-1 trial alpelisib combined with fulvestrant had a significant PFS of 11 v 5.7 months compared with fulvestrant alone in patients with a PICK3CA mutation. Approximately 70% of patients had endocrine resistant disease and patients were allowed to have had previous CDK4/6 inhibitor treatment. Alpelisib is not yet available on the PBS for treatment.
The mTOR inhibitor, everolimus, in combination with an AI has PFS benefit in endocrine resistant ABC and is available on the PBS.
Endocrine therapy alone on in combination with newer targeted agents offer a relatively low toxicity (as compared to chemotherapy) and high activity treatment option for ER positive ABC and is the backbone of first line treatment. In order to delay or overcome ET treatment resistance molecular targeted treatments have been added to sequential endocrine therapies and are improving PFS and OS in ABC.
If the female reproductive life was depicted in a single social media post, it would probably have happy hashtags around baby ultrasound images and glowing mothers-to-be.
Considered less ‘Instagrammable’ would be pictures of older women struggling with hot flushes and sleepless nights – even though menopause is as much a part of life for women – if not more so – than having babies.
One of the biggest myths about menopause – held even by seasoned health professionals – is that it is a brief blimp in older life that the vast majority of women sail through.
But while menopause is often defined as a single event – marked by the final menstrual period as the ovaries’ egg supply comes to an end – symptoms associated with menopause can start years earlier – known as perimenopause – and extend years beyond.
Some women face early-onset menopause when they are only in their 20s and 30s.
The usual age of menopause is between 45 and 55 years, and with rising life expectancy in Australia, most women can now expect to live a third of their life –perhaps 30 years or more – in menopause.

While about 20% of women have no symptoms, another 20% experience severe symptoms such as hot flushes, sweats, sleep disturbances, mood fluctuations, vaginal dryness and urinary issues.
And despite half of the population going through menopause, it is a life stage that is not acknowledged or discussed enthusiastically like pregnancy and childbirth.
Dr Lesley Ramage, a UK-trained GP who morphed away from mainstream general practice to focus on midlife and menopause issues, feels the pain of women who struggle with

Once known as the change of life, menopause remains a neglected and misunderstood period in a woman’s life. Cathy O’Leary looks at efforts being made to normalise the conversation and better support women.
“About 20% of women will still have bothers in their 60s, and 10% will have ongoing bother, and it’s sort of implied that there’s something wrong with women if they haven’t ticked the magic box and graduated with flying colours.”
menopause – both their physical symptoms and the dearth of awareness in the community.
“There is such a lack of information about menopause, so women suddenly find themselves in menopause and aren’t that prepared,” she told Medical Forum
“I think as a gender, we’re reasonably well-prepared for things up until childbirth but beyond that there’s a gaping hole. Most of us will spend 30-plus years in menopause, but we’re badly prepared for it.”
Dr Ramage often gets asked by women when will they be through menopause, but often there is no finite end point.
“Symptoms often get better with time, but when you’re in menopause, you’re in menopause – you don’t graduate or get a certificate for going through it.
“About 20% of women will still have bothers in their 60s, and 10% will have ongoing bother, and it’s sort of implied that there’s something wrong with women if they haven’t ticked the magic box and graduated with flying colours.”
She brings her GP-perspective to the table at the newly-formed Menopause Alliance Australia, which aims to provide healthcare professionals with up-to-date and evidence-based education on perimenopause, menopause and post-menopausal health.

Part of her mission is to promote good communication between women and their GPs, and that includes developing education packages for doctors, so they are better informed about menopause and contemporary treatments. While she consults at menopause clinics at King Edward Memorial Hospital and is involved in the teaching and training of medical undergraduates and doctors, she knows the pressures and challenges facing GPs.
“I have lovely fond memories of general practice but do appreciate that heart-sink moment when you’re running late on a Monday morning and a lady comes in with menopausal symptoms and you think ‘oh crumbs.’
“That in itself shows one of the problems. We need to advise women that if they think they’re entering menopause to, first of all, book a longer appointment.

“Otherwise, it can lead into snap decisions being made by doctors because, if they’re time-poor, they’ll take short cuts, and the problem with short cuts is that sometimes you don’t get to the correct point.
“Women may be offered blood tests to ‘confirm’ their menopausal status but if it’s not taken at an appropriate time in a cycle it can be very misleading, so women might be informed they’re not in menopause, and must be depressed so are given antidepressants.
“I’ve probably done it myself, so I’m not critical of doctors. I don’t think there is anything malicious about it.”
Dr Ramage said some GPs had dated views about the use of hormone therapy, and their only exposure to gynaecology might have been a brief stint during their student life.
She is trying to get a special learning group to improve education for GPs, because that is where women are going to be heading as their first port of call.
“There are pockets of GPs who are interested and keen to work in this area, as well as specialised services, and of course there is the menopause clinic at KEMH where I triage, and while some of the referrals are really appropriate, others are really lacking in basic knowledge,” she said.
“But again, we’re not trying to be punitive – we’re trying to be educative and supportive.”
Dr Ramage said education about menopause also needed to be societal, and with a trend of more women working into their early 60s, it was important to have strong role models and high-profile women – not unhelpful stereotypes.
“We need women not to be caricatured as short, dumpy with a grey curly perm when they’re in menopause,” she said.
This is where the Menopause Alliance Australia’s chief executive Natalie Martin plays a crucial role. When she founded the charity in October last year, it was to help stamp out the shame and misinformation around menopause she recognised after talking to friends and colleagues, whose lives and careers had been affected by not only the symptoms, but reactions from family and workplaces.
“The majority of my friends, family and work colleagues have experienced symptoms of menopause and some have felt embarrassed to discuss it, so I felt it was important to have more information out there,” Ms Martin said.
continued on Page 14

continued from Page 13
“We’re the fastest growing demographic in the workplace, and women aged 45 to 55 represent an increasing part of the global workforce. Menopause symptoms often occur at the peak of a woman’s career, but can also affect women in their 20s and 30s, even though in workplaces it tends to be seen as an old woman’s problem.
“Businesses have made great strides around accommodating pregnancy and child-raising, but that attention stops at the onset of menopause.”
Ms Martin said change had to start at the top down, with a menopause policy that was communicated effectively and where employers “walked the talk.”
It was important to educate managers and line managers about menopause and perimenopause, and have a workplace where women could speak openly about their needs.
“Around 20% of women won’t have any symptoms but for others it can be very severe and incredibly disabling,” she said.
“I had one comment from a friend who works in the mining industry that it’s secret women’s business, and another, who is an engineer, felt she had to hide her symptoms because she was fearful of redundancy and being replaced with a male.
“The conversation is not yet normalised, and not many companies in Australia have a menopause policy – the UK is way ahead of us in supporting menopause.
“If a woman has had night sweats and difficulty sleeping, she should be able to come into a meeting and can say ‘I can participate but I might not be myself at this meeting’ and that should be okay.”
Some companies allowed flexible working hours so that women could work from home; others ensured cold water was available at work and used cotton uniforms. Some provided UV umbrellas for teachers out in the playground.
Ms Martin said the benefits of
a menopause-friendly business included gender equality, retaining and developing talent, increased performance and financial success, employee engagement and lower absenteeism, while supporting a menopause-friendly culture could also avoid the potential for litigation.
The menopause alliance has good credentials, with an impressive board of directors, including some of the State’s leading medical practitioners in their field. These clinicians have helped prepare a comprehensive range of information around perimenopause and menopause and effective treatments, aimed at the general public but also tools for doctors, particularly GPs.
Among them is Professor Roger Hart , an expert on fertility impacted by early-onset menopause caused naturally or by radical radiological or chemotherapy treatments.

His message is that menopause is not necessarily an old woman’s condition, and can start in women aged in their 20s or 30s, and completely blindside them when it comes to family planning.
Professor Hart, who is medical director of Fertility Specialists of WA and Professor of Reproductive Medicine at KEMH and the University of WA, said early-onset menopause occurred in about one in 100 women before the age of 45, and one in 1000 women before the age of 40.
It was easy to miss, as many women might be on hormonal contraception, effectively masking any symptoms.
“Others may have a significantly reduced ovarian reserve, although they may get a regular, or intermittent, menstrual cycle so their GP does not consider premature ovarian insufficiency (POI) as a potential underlying concern,” he said.
“As is often the way, as ovarian function is failing at an unexpected time, most patients and clinicians will not think about this as a cause of their symptoms, hence leading to a delay in diagnosis.
“These women need hormonal support because delaying intervention can have longer term adverse health outcomes.”
Professor Hart said GPs needed to know that fertility was still potentially possible, but because the ovarian function was severely compromised the answer was not IVF.
“Very careful cycle monitoring, often looking for signs of rare spontaneous follicle development, with appropriate triggering of ovulation and good luteal phase hormonal support into pregnancy, can, in a young woman, often result in a pregnancy,” he said.
“It is frustrating and time consuming for the woman, and often leads to substantial emotional distress, and is not always successful. Obviously, a woman in her late 30s and onwards will have a substantially reduced chance of conception due to aneuploidy in the oocytes.
“Hence, it’s a place for the young woman with POI. Unfortunately, if not successful, the only remaining option is oocyte donation treatment.”
A/Professor Amanda Vincent, an endocrinology and menopause expert at Monash Medical Centre, is part of a consortium trying to identify the causes of POI among young women, to help with early diagnosis and management.
The group is updating POI management guidelines to be released next year.
She wants GPs to be aware of the significant psychological impact of this diagnosis for young women and the need for support and counselling.
“I reiterate the problem that diagnosis is often delayed as women and clinicians think they are ‘too young’ for menopause," she told Medical Forum
“I also stress the need to start estrogen replacement and continue this until the usual age of menopause at about 50 years (unless contra-indicated due to estrogen sensitive cancer such as breast cancer) to manage symptoms and avoid long-term health issues such as heart disease or osteoporosis.
“I have had GPs cease HRT in women with POI after five years or so because they translate the findings of concerns about breast cancer risk seen in older women in the Women's Health Initiative study to these younger women, but this is a different group of women.”
Back at the Menopause Alliance, Dr Ramage said the overall message when it came to menopause
and treatment options was the importance of finding what was right for each woman.
“It’s about respecting their thought processes and providing good education, and certainly not trying to bully someone into a pathway they’re not comfortable with,” she said.
And Ms Martin said offering education online for GPs so they felt better-equipped to treat menopause was a key way forward.
“But only 20% of women in perimenopause will see their GP, and we want to see improved access to care in the public health system for people with menopause – for those who can’t necessarily afford to get help in the private system,” she said.
“It’s an ongoing journey but we will get there.”
ED: For more details about Menopause Alliance Australia go to www.menopausealliance.com.au
GPs can also refer women with earlyonset menopause to the Ask Early Menopause app, which is available freely from Android or Apple stores or at https://www.askearlymenopause.org/
WA health authorities are being urged to take a nuanced approach to compliance with its new digital tool to crack down on patients ‘doctor shopping’ for drugs of addiction.
This follows the launch in March this year of the State Government’s ScriptCheck WA platform, which is modelled on systems already used in some other States.
Doctor shopping is a growing problem across Australia, driven by addiction and abuse of controlled medicines, with people typically visiting different doctors over time to obtain multiple prescriptions for drugs such as oxycodone.

The Government claims the new real time monitoring platform will be a gamechanger for doctors and pharmacists.
Royal Australian College of GPs’ WA chair Dr Ramya Raman told Medical Forum that while she supported the new system, she urged the WA Health Department to take an educative rather than punitive approach if some GPs had difficulties complying with it.

About 5000 prescribers in Queensland received an email earlier this year saying they had forgotten to check the State’s real-time prescription monitoring system, QScript, before prescribing a monitored medicine.
While health authorities there said the letters were intended to be educational and not punitive, they did not include basic details such as the dates or patients for whom the practitioners had allegedly failed to check QScript when the letters were emailed out at 8pm on a Friday evening.
Real-time script monitoring has finally reached WA and doctor groups are cautiously optimistic it will achieve its goal to stop doctor shopping.
Cathy O’Leary reports
sense”
“ScriptCheck WA has the potential to be a very useful mechanism to help GPs make safer clinical decisions about which medicines to prescribe, and to reduce the risk of patients ‘doctor shopping’ to access drugs such as opioids and benzodiazepines, which can have adverse outcomes,” Dr Raman said. “But in implementing ScriptCheck, the Health Department must ensure that it is straightforward for GPs to use, including the practicalities of integration into practice clinical software.
“We have seen from other jurisdictions including Queensland that this has not always been the case, with GPs receiving emails late on a Friday and being ‘pinged’ at times when the site had actually crashed.
Site ‘freezes’
“GPs in that State also reported that the site regularly freezes and that they often have to manually go in and check a box when trying to enter a prescription.”
Dr Raman said enabling a good user interface with GP software was key to ensuring the system was effective for improving patient outcomes.
Australian Medical Association WA president Dr Mark Duncan-Smith agreed that ScriptCheck was in principle a great idea and in general terms should be supported.

“ScriptCheck ‘should’ save time, assist with identifying
drug-seeking patients quickly and identify patients who may need counselling regarding their drug or prescription use,” he said.
“However, the ‘should’ is yet to be determined if practically it will achieve these goals.
“ScriptCheck must integrate seamlessly with practice software to be user friendly and be efficient for the user. If this does not occur, it will not be used and not achieve these goals.”
Given these provisos, he said ScriptCheck could save a lot of time with the potential ‘drug seeker’ patient, especially if they were “less than truthful.”
“It will allow more accurate identification of ‘drug seeking’ patients so the conversation can be better directed rather than spent identifying if the patient is drugseeking,” he said.
ScriptCheck has been released to all GPs and community pharmacies throughout WA, after undergoing testing with a select group of doctors in the first two months of this year. There is a series of three modules to train prescribers and pharmacists on the use of the WA system, with the first module detailing the functionality of real-time prescription monitoring and its safety benefits.
The second module has a focus on safe and appropriate dispensing of monitored medicines and managing concerns about patient safety regarding the use of monitored medicines.
The third module details best practice communication strategies to help prepare for conversations with patients about monitored medicines.
Drugs reported in the platform include controlled drugs for the treatment of severe pain, such as opioids (morphine, oxycodone, fentanyl and methadone) and stimulants such as dexamphetamine for the treatment of ADHD.

Health Minister AmberJade Sanderson said the Health Department would closely monitor the outcomes of ScriptCheck and consider adding other problematic prescription medicines to the system.
"Early users of the system say it has vastly improved the way they can support their patients and manage any risks in relation to these medications,” she said.
"The platform allows doctors and pharmacists to instantly detect doctor shopping – meaning they can intervene where people are accessing excessive amounts of these medicines.
"The strength of the new ScriptCheckWA system is that it now gives health practitioners instant, secure access to this data, as it occurs.”

Ms Sanderson said better access to this data would allow the rapid identification of people with a drug problem and help get them referred to a drug treatment program.
Victoria became the first Australia State to introduce mandatory real-time prescription monitoring, launching SafeScript in 2020, which was followed by similar systems in other jurisdictions including Queensland and South Australia.
As the incidence of diabetes grows in the community, attention is turning to obesity as one of the causes and what weight-loss therapies can be applied.
By Eric MartinFew people would argue that the limited supplies of the diabetes drug Ozempic should be directed firstly to people with that condition. However, the current shortage and the use of the drug to treat obesity raises important questions.
In 2020, an estimated one in 20 (almost 1.3 million) Australians were living with diabetes, including 48,300 people newly diagnosed with type 2 diabetes registered on the linked NDSS and APEG data, equating to 188 diagnoses a day per 100,000 population.

Numbers could be even higher, with the 2011–12 ABS Australian Health Survey, which collected blood glucose data, revealing that 20% of participants aged 18 and over had undiagnosed diabetes before the survey. Yet of these, more than one million are estimated to have developed diabetes due to obesity.
The latest available data shows that in 2017-18, 31% of Australian adults were obese, 36% were overweight, and 25% of children aged 2-7 were also either overweight or obese. That is more than 9,266,000 people who were overweight, and more than 7,979,000 who were obese.
With the condition listed as one of the major contributors to the burden of disease in 2018 at 8.4%, just behind tobacco at 8.6%, and a 2% increase forecast for 2023, obesity looms as a healthcare crisis.
Globally, the World Obesity Federation just released a report which showed that at current rates over half the world’s population (51%) will be overweight or obese by 2035.
Medical Forum spoke with Dr Julie Manasseh, a practising GP who specialises in obesity management, on the stigma around the use of Ozempic and other weight loss drugs, as well as the implications of the failure to train more health professionals in this area.
“There was a huge demand for Ozempic when it was recognised and popularised on social media to prompt weight loss, people wanted a medication that would be effective at helping them to lose weight,” she said.

“This group of drugs, including Ozempic (semaglutide), are called JL P1 agonists and were originally developed for the treatment of type 2 diabetes, but as a result of noticing that they also produced weight loss, manufacturers have gone into the development and production of these drugs specifically for this purpose.
“For example, although Ozempic was originally developed as a diabetes drug, it has now been marketed and approved as Wegovy, which is just a higher dose of semaglutide, for weight loss.
“The difficulties we face, though, are to do with access to the medication for obesity.”

Dr Manasseh believes this is largely caused by the outdated attitude among governments and health departments, and even health professionals, that obesity is simply a lifestyle choice.
“There is a misguided belief that obesity can be fixed either by dietary changes alone or diet and exercise – the eat less, move more philosophy. Yet we know studies have shown that this is only a short-term intervention, and invariably, biological adaptations will lead them to regain any weight that they have lost,” she said.
“We are still stuck in that paradigm and not moving forward to accept the scientific, evidence-based model that obesity is not that simple, and once developed, it is a complex and chronic disease. In addition to the obvious weight gain, it changes the physiology of appetite hormones, cytokines, and inflammatory mediators – obesity is a proinflammatory state.
“We now have effective drugs for the treatment and control of obesity, but we don’t want to know about it because that could cost too much money on this side of the equation.
“There is this huge disconnect between constantly having these obesity summits and meetings, and pulling out all these dire statistics about how much obesity is costing the economy, and the reality of trying to lose weight under the current system.”
For example, in 2018-19, an estimated $3 billion of expenditure in the Australian health system was attributed to diabetes, representing 2.3% of total disease expenditure, yet according to the National Obesity Strategy 2022-2023, obesity cost $11.8 billion in 2018 and could cost an estimated $87.7 billion by 2032.
“However, more medication has been developed to target diabetes rather than obesity – even though being overweight is one of the best predictors of developing the disease,” Dr Manasseh said.
“The current model of thinking about health care is that we will treat a disease once it is established, but we are not really interested in funding medications for a condition that we know can lead to all of these.
“Governments are just not brave enough to envision a different model of health care where we consider prevention or reduction of
continued on Page 21


continued from Page 19
future risks rather than just treating downstream complications.”
About 25% of Australian children are either overweight or obese, and multiple studies have demonstrated that childhood obesity is one of the major predictors of developing a wide range of serious comorbidities in later life.
“We are already seeing issues that previously would only have been found in obese adults –metabolic syndrome such as high blood pressure, high cholesterol and high blood glucose or diabetes,” Dr Manasseh said.
“The health trajectory for these children is not good at all, and the same physiological rules apply to children who have obesity – diet and exercise alone is not going to be enough.”
Dr Manasseh cited the American Paediatrics Association guidelines around the management of children with obesity, which strongly indicates the appropriateness of weight loss medications for children who have well-established obesity and may also have developing comorbidities.
“But there has been a lot of controversy about this with people saying we shouldn't be sticking children on drugs, but what about these children developing health problems and having a heart attack before they reach the age of 21?
“Early intervention is generally argued as the best possible step for almost any other condition, so why would obesity or overweight be any different?”
She said that another argument against the use of weight loss medication was what happened once the patient had achieved their target weight and treatment was stopped.

“Many studies have shown, including the step trials with semaglutide, that weight is regained over time after drug cessation. The question then arises, will people have to stay on weight loss drugs for the rest of their life to maintain their new lower weight?” she said.
“Many commentators say that this is too costly or offer other excuses. But if we view obesity as a chronic disease like we do diabetes or high blood pressure or someone with heart problems, then what do we do? Do we stop medication?
“Of course, we don’t, we continue them on their treatment in a lifelong manner to manage their underlying chronic condition. Obesity is a chronic disease and the concept that we cannot continue, or that it is too expensive to provide lifelong treatment, is flawed.”
Dr Manasseh explained that obesity is multifactorial, caused by a combination of genetic predisposition and our modern environment, which promotes a lifestyle with plenty of cheap, very palatable foods, high stress levels, and an increased risk of mental health conditions.
“It is very easy to become overweight and, in fact, it is the prevalent body type now,” she said.
“We only have one third of the population who satisfy the normal criteria for BMI and the irony is found in asking, ‘why is it then, that we are still holding on to this image that it is so important that you must
have this specific look to feel like you are a worthy person?’
“People who are considerably obese can be afraid or feel ashamed to even step out of their homes because they immediately feel that just by looking at them, people are going to judge them negatively.”
WA-based research has shown that individuals who were on the receiving end of weight bias or discrimination had a 60% greater risk of mortality and were 2.5 times more likely to experience mental health disorders such as anxiety.
Dr Manasseh believes that the body positivity movement is an understandable pushback against the stigma that overweight and obese people face in our society.
“However, it is at risk of going too far the other way in a sense that there is a strong element of denial that obesity does carry health risks. It most definitely does. We cannot say ‘look, let us just not worry about our weight, let us just be happy about it,’” she said.
“But you can understand how
continued on Page 23
Weight stigma can be an insurmountable barrier to accessing health care, according to health consumer Jeni, who has shared her experiences with the Health Consumers’ Council.
“It is easy to look at me and make assumptions,” says Jeni, a 53-yearold single mother of two children. “My life has been defined and shaped by my weight – particularly since a series of health issues knocked me for six in my late 20s.
“Living with obesity means I experience subtle attitudes from others at every turn. When I’m in the waiting room at a clinic. When I’m in a consult with a clinician. When I’m at the shops. Negative judgmental biases are held about people with obesity that lead to unfiltered language and adverse responses when seeking help.
“Looking back over my life, I now know that when I was growing up, I had complex medical conditions that were not diagnosed. What they mistook for awkwardness and socially offbeat behaviour was autism, dyslexia and sensory disorder not to be diagnosed until I was 51.
“I was not always ‘fat’. At the age of 10, I started to develop a chubby face. I wasn’t overweight, however, but this is when the teasing started, and I had pressure from my mother about losing weight and exercising. By the time I was 13, again not overweight, I was encouraged to do aerobics and diet.
“I had never had a focus on food until I started dieting and now I was starving and thinking of food every minute of the day.
“I began loathing myself and developing a fear of looking in a mirror or having a photo taken. I still was not overweight, just on the high side of the average weight for my height, but my family doctor told me to diet in case I got fatter.
“The things that happened to me as a child were nobody’s fault, it was a sign of the times, and I am not alone in having been treated with dysfunctional and harmful
influences from people in positions of authority with well-meaning intentions. I was constantly on diets and exercise routines for years, trying to keep my weight down. I wasn’t huge but over the average weight so was called obese.”
Jeni says that weight stigma has, and continues, to play a large part in her struggle with weight as she has faced poor quality of care, a lack of understanding from health professionals, and an absence of real-life supports.

“If you are obese, you are labelled and dehumanised as a drain on society, or someone who has made poor lifestyle choices. I feel this makes it easier for those people who should be helping us, to sweep us aside and dismiss our needs or our right to a better life by putting the blame squarely on the individual.
“In 1997 I became very ill. For six months I presented at the emergency department of a Perth hospital on more than seven
occasions – only to be sent home with no solution to my problem. I couldn’t eat and lost 15kg, but because they still thought I was overweight I was ignored. They didn’t realise I was actually suffering from serious malnutrition and pancreatitis.
“I finally had an emergency operation, but my life and health would never be the same. My mobility was reduced, and my weight bloomed.
“I was offered anti-depressants, but I was not ‘depressed’, I was in pain, and no longer could do the thing I loved – horse riding. I had to leave my job as they did not understand how sick I was, and I could no longer physically move like I had before.
“I never thought that I wouldn’t get back to my old self. If I had been given the correct care at the right time, the surgery would have been successful, and my mobility wouldn’t have been impacted.”
continued from Page 21
that view came about because of enormous stigma that people have experienced in their lives, the amount of bullying and ostracism. “And the fact that diet and exercise has failed them repeatedly, they are saying, ‘look, you are just telling us all the wrong things, you are telling us that we need to eat less and move more. We have done that, and we have ended up at a higher weight, and we are not going to diet anymore. We just want to live our lives’.”
Even health-care professionals are not immune from messaging. Curtin University-led research has found that Australian health-care students often hold negative attitudes and beliefs towards people living with obesity, which could lead to poor clinical care.
“Obesity management from a medical sense is a specialised area,” Dr Manasseh said.
“Aside from a knowledge of weight loss drugs, to work properly with a patient, we really must examine all the factors that have contributed to weight gain. We need to look at their mental health, stress management, sleep, eating behaviours and the contribution of any other medications.
“It is expected that a GP should know about everything and be able to help patients with everything, but the reality is that they have not received the training – they are playing it by ear themselves. Which
is why attitudes can vary when discussing weight management with a patient, or whether they will even raise the issue.”
Doctors and other health professionals get minimal training, if any, in obesity management, she said.
“They know about the associated co-morbidities like high blood pressure, and they are quite comfortable in treating that, writing them prescriptions, and reviewing them. But they haven't been taught how to address weight in a sensitive way with patients, and might struggle with the question of, ‘how do I help my patient with their weight?’,” Dr Manasseh said.
“This is a major disconnect. Two thirds of our population is overweight or obese and consequently present with all these health problems, but doctors and other health professionals are not trained to deal with it.
“One of the reasons why I took an interest in this exact area was that when I graduated from medical school over 30 years ago, obesity was not an issue, and it certainly was not in our curriculum.
“But in the 30 odd years that I have been practising as a GP, there were increasing numbers of patients carrying extra weight and I was telling them they have high blood pressure; they are getting diabetes – ‘you've got to go lose some weight’ – and then prescribing medications.
“That was all I could offer them, and
I could not help thinking that from a first principle’s perspective, it did not make sense: why was I writing all these scripts for complications when I could help them with their weight, which might address those issues too.”
The impact of this lack of training is that many patients miss the benefit of sound medical advice from their GP.
“I have never done a survey, but just my impression from patients that I have spoken to is that when a patient thinks, ‘I need to lose weight and I need help with this’... who do they go to?” Dr Manasseh said.
“I would say that personal trainers are at the top of the list, along with commercial weight loss operators. Dietitians might be there somewhere at the third rung, but their GP is, in fact, not anywhere in the top five.
“Yet even dieticians receive little training in weight loss in a private practice situation. The curriculum for dietitians is very much geared towards prescribing specialised diets for hospital in-patients, such as people with kidney disease, and to develop that further, they too will need to do extra training after they graduate.
“We are all experiencing the same lack of education on obesity, and this is another major barrier for patients seeking help for their condition.”
Jeni’s health was further impacted when she developed an eating disorder in the wake of her medical condition and lack of mobility.
“It was a downward spiral,” she said. “Future illnesses were not treated due to my weight gain, and this just perpetuated itself into the body I live in today.”
Over the years Jeni has presented a number of times to hospitals and been sent home without treatment.
“I felt due to my weight I was put in the too hard basket. I have
developed a fear of medical centres due to the abuse I have received from staff and struggle to attend appointments due to anxiety.
“I feel there is an insidious lack of health care for those who are obese, which creates more health complications and that has prevented me from everyday life enjoyment.
“Maybe if we acknowledge more that obesity is a disease and not a lifestyle choice, more patients would be taken more seriously when asking for help.”
Jeni has joined The WELL Collaborative to work with government and Health Consumers’ Council (WA) regarding health and obesity, in the hope of educating and gaining more funding in the right areas to give patients a better outcome and improve people’s lives.
ED: Further resources are available on the SHAPE (Supporting SHAPE (Supporting Holistic and Person centred weight Education) website https://shape.wapha.org.au/
 By Ara Jansen
By Ara Jansen
Maybe it’s six degrees of separation, it’s just Perth or perhaps Dr Tamara Hunter’s dad knew something.
The gynaecologist and fertility specialist was named after the sister of one of her dad’s high school mates. When she turned up at King Edward Memorial Hospital for Women well over two decades later to start her obstetrics and gynaecology training, she met gynaecologist Dr Tamara Walters. Co-incidentally, this Tamara was the woman she was named after.
“I’ve spent the last 17 years working with the woman I was named after,” says Tamara Hunter happily.
Medicine has always been Tamara’s passion but large doses of teenage angst meant the Perth-born student didn’t get enough marks to get in after high school. A career counsellor suggested human movement studies and she graduated as an exercise physiologist from UWA.
She moved to Sydney and spent a number of years working as an exercise physiologist and corporate health consultant, including assisting in the set-up and operation of Sydney Heart Image in 1999. Then at 25 she was accepted into medicine at the University of Sydney.
Expecting to feel a little odd as a mature student, she was surprised to see so many more students her age than expected, plus they were from varied backgrounds too. That definitely made the experience a little easier.
Setting her sights on cardiology, in her third year, Tamara moved to Canberra. There she met some obstetricians and gynaecologists and became enamoured with the specialty.
“I watched this husband-and-wife team managing six children between them, alongside their busy careers and I was inspired. This specialty is a mixture of medicine and surgery. I love the frenetic nature of it – the adrenaline rush of an emergency caesarean – balanced against the investigative nature of reproductive endocrinology and gynaecology.”
She moved back to Perth in 2004 and spent time working in emergency departments on women who presented with gynaecological issues. She started training in obstetrics and gynaecology as a resident, getting into the training program in 2006. In 2012 Tamara received her fellowship and did her advanced subspecialty training in reproductive endocrinology and infertility, taking five years (and two children) to complete.
“I believe in managing the whole person when managing reproductive health and leaning into my allied health colleagues to assist in educating and empowering women around their health.”
Fertility specialist Dr Tamara Hunter came to medicine as a mature-age student and has used both her previous profession and becoming a mother later in life to inform her holistic care.
Her passion for holistic, evidencebased reproductive care led to the establishment of Woom, a practice which cares for numerous aspects of women’s health through a collaborative team of gynaecologists, fertility specialists, women’s health GPs, dietitians, physiotherapists, psychologists and other allied health practitioners.
“I remember meeting women’s health physiotherapist Rebekah Taylor and thinking it would be amazing to have various allied health practitioners working side-by-side where there was true collaborative health care in place. “We established Woom in 2020 and all our practitioners are passionate about women’s health and about increasing each other’s skill set. I believe by working

together this way we can do a lot of good for women.”
Tamara has received two academic prizes for her work in preterm birth and in-vitro maturation. In 2011 she obtained a Certificate of Reproductive Endocrinology and Infertility, the highest qualification available to a fertility specialist in Australia.
Tamara also works as a paediatric gynaecologist at Perth Children’s Hospital and is a senior lecturer at the School of Women and Infants Health at UWA. She’s also part of Monash IVF through the Pivet Medical Centre.
“I get great joy helping couples conceive, hand them over to my obstetric colleagues and see the end result eight to nine months later,” she says. “I have a deep understanding of struggles of infertility. Like many people in this era, I put off having a family until I had achieved a career.
“I didn’t meet my husband until 34 and had my first child at 37. You never really think infertility will happen to you. By the time I came around to my second child, I was 39 and it was hard. My second child happened through IVF and was born when I was 40.”


Our solutions are designed to maximise your block’s potential in the easiest way possible. So if you’re considering upgrading your family home, or a multiple dwelling development, we can take care of everything. From the demolition of your current home to the design and rebuild of your beautiful new home and everything in between, we’ll keep it seamless and hassle-free.


Atrium Homes are proud to have many members of the Perth medical community as valued clients, to whom we have undertaken many demolition and rebuilds, and designed luxury custom-built homes over many years.



continued from Page 25
Tamara says for a long time there was a stigma around children who were born through IVF. She encourages her patients to tell their kids, rather than keep it a secret and perpetuate a totally unnecessary psychological burden.
“Fertility treatments are a huge emotional investment and an incredible emotional challenge for a lot of people. Although many of my patients achieve their dreams, I’ve had to learn along the way that someone wanting to be a parent is not necessarily a dream I can always satisfy in the way they want me to.

“It breaks my heart that there are some patients who will walk away without a baby. I have to make sure they are as well supported as possible, and they feel they have done everything they can and have made their peace with the process – that’s really important.”
Tamara is no stranger to mainstream and social media –notably her evening Instagram live videos where she shares everything from how to handle the holidays to answering questions about progesterone in easy-tounderstand language.

“I’ve become comfortable on social media and use it as a way to educate and empower. I don’t shy away from it. As doctors, we have an opportunity to use it as a way to ensure our patients are getting the right information, especially when speaking to the younger generations.”
She recently used the platform – where she calls herself Dr T – to share that she has been diagnosed with breast cancer. She’s committed to sharing her journey online, talking about her chemo treatments and talking about her “blessons”. She wants to empower women, in particular to do essential health checks, such as breast and cervical screens, making health a priority.
“I know I’m going to be a breast cancer survivor. I have caught it early and am fortunate. Most importantly, I know it doesn’t discriminate. I’m a healthy person with great respect for my body,
but I was not excused from cancer. I encourage other doctors to not put off their health checks because they are too busy. As doctors we can tend to sacrifice ourselves for our patients.”
She’s a believer in looking after your personal temple as well as possible. As an older parent she’s an advocate of a good diet, regular exercise and meditation. Daily exercise is Tamara’s commitment to herself as a stress reliever and strength-builder. She loves weights and does body building.
Going to bed at a sensible hour and getting up daily at 4.30am keeps that commitment to self and allows her to be present for her two daughters. While some of her habits might have to temporarily change, Tamara’s positive attitude and a desire to “grab everything with both hands” is standing her in good stead.
She and husband Mike believe education is important and encourage an appreciation and participation in sport, music and
the arts in their family. They also believe in service and have let their girls choose how they want to contribute. One daughter is part of the Student2Student peer reading program with The Smith Family and the other swam 30km for charity during summer. Woom follows suit by not only donating money but expert time and knowledge as well as supporting the education of two children.
Despite the last few years, travel is high on the agenda for Tamara and her family. Now her daughters are a little older, a feature of their family trips is going somewhere they can learn about the environment. Their last trip was to the Maldives where they stayed on an island which was 100% sustainable, while swimming and snorkelling taught them about local marine life. Next on their bucket list is to go to Sarawak and visit the orangutans.

WA Health is looking for skilled and experienced health professionals to strengthen its workforce. Be part of the team as we continue to provide world-class public health care for all Western Australians. Be part of WA Health, where you belong.

Scientific discoveries often emerge like a patchwork quilt, with one field of research layering atop another in surprising ways, and a biomarker for ovarian cancer may be one of them.
The media was recently filled with stories about the development of a ‘cancer vaccine’ designed to help the body’s immune system fight off melanoma. Cancer treatments like these often use circularised RNA molecules to train the body’s immune system to identify the cancer. It’s these molecules Associate Professor Jason Lee hopes will hold the key to finding patients with early-stage ovarian cancer – when they have the best chance of survival.
A/Prof Lee now wants to sew together different small pieces of research, published in the past five years, on the role of these molecules in ovarian cancer. Thanks to an Ovarian Cancer Research Foundation grant of $852,343, his team may be able to complete the quilt.
“We want to show expression of circular RNAs from the ovarian tumour, and how much of that is actually found in the blood,” says the cancer epigeneticist, who leads the Epigenetics and Disease Group at QIMR Berghofer and is an adjunct associate professor at University of Queensland and Queensland University of Technology.
A/Prof Lee’s dream is to be able to detect the presence of ovarian cancer using just a few drops of a patient’s blood.
Until recently, people did not think of RNA as a possible biomarker because the molecule is especially fragile. The standard RNA we are more familiar with is linear and degrades over time from the ends. But circular RNAs don’t have ends, making them far less likely to degrade, and the “perfect candidate” for testing and development.
“It makes them much more stable in blood, urine, saliva, sweat, and so on,” he said.
Research has shown these molecules are found at different levels in cancer patients, so if the research team can identify the right circular RNAs for ovarian cancer, they could be key to a non-invasive, easy to collect method of testing people at the earliest stages of disease.
People identified with earliest-stage ovarian cancer have a 90% survival rate at five years, but this plummets to under 30% if diagnosed in the later stages. This solution, however, reaches beyond the goal of an early detection test.
“If some of the circular RNAs are highly expressed in ovarian cancer, then is it possible for us to develop a therapy to block that elevation? That could actually treat ovarian cancer or be hopeful as a as a prophylactic kind of preventative medicine,” A/Prof Lee said.
The team must first find the right
molecules, a task that has led the professor to be affectionately being called a “vampire” because the first step in the process is to get as many blood samples as possible from people with ovarian cancer.
The team is currently analysing the blood of patients who had aggressive ovarian cancer and searching for distinct circular RNA from the tumour itself. The next step will be to work with an epidemiologist to identify those at a high risk of developing the cancer, such as people with a family history or BRCA gene mutations, to see how early circular RNA can be detected.
If successful, A/Prof Lee hopes that high-risk women can be targeted with a screening program.
A 24-hour turnaround test would be a world away from the MRI and PET imaging tests women must currently undergo and could be used in conjunction with the standard tests that patients with a previous cancer already have done.
“By taking a simple blood test, we can actually see whether the cancer is coming back and at what stage,” he said.
A/Prof Lee has been awarded another grant from PanKind Australia – the Australian Pancreatic Cancer Foundation – for the early detection of that cancer.
The discovery of such a biomarker could also help in the maintenance and surveillance of other cancers such as ovarian, melanoma, breast or lung cancer, in patients who often have blood work taken as part of their management after remission.

Situated in the leafy riverside suburb of Mt Lawley, we offer a boutique hospital experience with large rooms and relaxing views over the Swan River or Mt Lawley. Our team of expert obstetricians, midwives and lactation consultants are incredibly passionate about their role in bringing babies into the world and supporting parents as they get to know their newest family member. We empower, encourage, support and educate women and their families to have the birth of their choice in the safest way, and to help them on their journey as parents.

Partner can stay • Antenatal and postnatal education • Longer hospital stay • Private room


Antenatal and postnatal lactation consultants support






Meet our Obstetric Team


From dream to birth and beyond, we’re with you.
@sjogmtlawley facebook.com/sjogmtlawley • sjog.org.au/mtlawleymaternity

Australian’s first guideline outlining best practice for providing therapy support to autistic children and their families was launched in February this year, representing a landmark moment for autism.

It is the first time that a consensus view has been published on what represents best practice therapy for autistic children in Australia and having this clear and agreed definition goes a long way towards ensuring that Australian children and families receive high-quality, safe and effective therapies that support their development.
Autism in Australia
Autism became a formal diagnosis in Australia with the introduction of the third edition of the Diagnostic and Statistical Manual in 1980. But it was not until the fourth edition was published in 1994 that autism in Australia was diagnosed in large numbers.
The most common types of interventions for autistic children – now, more commonly referred to as ‘therapies’ or ‘supports’ –are not biologically based. They are therapies that are focused on directly supporting the learning, participation and wellbeing of autistic children, including changing the environment around the child. These therapies are most often provided by allied health practitioners such as speech pathologists, occupational therapists and psychologists. While for many children, these therapies are supported by medication prescribed by medical practitioners, it is the non-biological therapies that this guideline is focused on.
Many therapies for autistic children have good evidence for their safety and effectiveness. However, like all areas of health and medicine, good practice is not uniform across the country. This can lead to confusion for children and families, and
expose them to clinical practices that may be ineffective or harmful.
This issue has long been recognised in Australia. Over the past two decades, there have been important steps taken to provide increasingly better guidance to clinicians and policymakers about what represents good practice. However, there hasn’t been a Guideline until now that was developed using internationally agreed methods.
This guideline has been developed to help ensure that practitioners who provide therapies to autistic children and their families do so in ways that are safe, effective, and desirable.
The guideline was developed by the Autism CRC, which brought together a group of researchers, clinicians, and autistic people to consult with more than 1000 community members. These community voices were then combined with evidence from three systematic reviews of international research to develop 84 recommendations that will guide best practice in Australia.
The recommendations help clinicians work with children and families to set therapy goals, select continued on Page 33
Research is helping to find new ways to support neurodiverse people, says Curtin University’s Dr Ben Milbourn.

The shift from adolescence to adulthood can be challenging for young people on the autism spectrum, and opportunities for employment have historically been limited. There is a need both here and internationally for greater support for neurodiverse jobseekers and our team’s newly developed learning framework could help.
It builds on autistic individuals’ already-existing strengths, to enhance their employability and may help them build skills to improve job-seeking prospects. Modern approaches in this field already highlight the importance of strength-based frameworks, which match strengths and interests of autistic youth to future career pathways. Previous research shows the strengths of many autistic individuals are considered beneficial for employment in the information and communication technology sector.
The Autism Academy for Software Quality Assurance runs a strengthsbased intervention program for autistic adolescents. This program involves an extra-curricular outreach and mentoring program encouraging them to leverage their unique skills across science, technology, engineering, arts and mathematics (STEAM). The program was recently the recipient of the Western Australia Premier’s Science Award.
The purpose of the Curtin-led study was to develop a framework to suit technology clubs incorporating coding and ICT learning modules. These clubs provide opportunities for autistic youth to develop their technological and social skills, meet role models working in the industry and help them find work experience.

In developing a strength-based model, researchers drew on four elements incorporating interests, value, autonomy and requirements (IVAR).
Interests refers to applying strategies that draw on adolescents’ areas of interest and changing activities to ensure they are included. Value represents a culture of valuing autistic adolescents and their unique strengths and skills. Autonomy refers to providing opportunities for adolescents to make decisions during the program and Requirements incorporates the design of the social and physical environment.
The elements of the IVAR
framework could work when applied to technology club service delivery.
Interests: In recruiting facilitators, service providers should consider the personal interests of facilitators beyond teaching and general experience with autism. Ideally, service providers want facilitators who share common interests with autistic adolescents.
When teaching, technology activities should be flexible and customised, so they align with
adolescents’ interests. For example, facilitators may teach video game design and encourage each adolescent to develop a game based on their areas of interest.
Value: This is evident when facilitators adapt teaching based on individual needs and at the end of each semester, a presentation day is arranged where autistic youth present their work to family, friends, and other students. Facilitators then discuss technology skill goals with adolescents and parents. Goals should not be centred on autism deficits, but rather suited to students’ strengths.
Autonomy: Facilitators should be trained in individualised and collaborative teaching approaches. Technology clubs could provide at least three activities to choose from, for instance robotics, website design or video game design. Autistic adolescents may first be taught how to code a robot but
then encouraged to apply the coding in a manner of their choice; such a using code to create a robot racecourse or making a robot dance.
Requirements: To apply this, service providers would consult with parents and adolescents to understand participants’ sensory needs and preferences. Program facilitators would be educated based on these needs and the program environment modified accordingly.
The importance of consistent attendance and routine would be emphasised as consistence helps build rapport which improves teaching and learning outcomes. The technology club’s location is also considered within this element which should provide ample room to reduce overcrowding – for example, having a ‘noisy’ room and a ‘quiet’ room to suit people with these sensory needs.
Future research should focus on exploring how practical and appropriate the IVAR framework is in supporting the delivery of strength-based technology clubs for autistic adolescents. Extending the effectiveness of the strengthbased IVAR framework, potential scope also exists to apply the four components that comprise the model to other general areas within autism research.
ED: Dr Ben Milbourn is a Senior Lecturer at Curtin University’s School of Allied Health.
continued from Page 31
and deliver the most appropriate therapies to meet those goals, and then monitor the therapy to ensure the therapies are safe and effective.
The guideline was reviewed and approved by the National Health and Medical Research Council, indicating that it has been developed to the highest standards.
Providing therapies to autistic children can be complex, and involves the considerations of many factors. A therapy approach that may be appropriate for one autistic child, may be quite unsuitable for another.
Children can learn in different ways. For example, some children may receive benefit from learning to talk with the help of a technology device. Other children may not receive any benefit from this kind of support, and instead, the device could be an added and unnecessary complication in the family’s life.
There are similar considerations for
a variety of other factors. These include where a therapy is delivered (in a clinic, in the home, or in the community), how it is delivered (individually or in a group), and through what means (in person or telepractice).
The guideline is particularly focused on therapies provided by allied health practitioners. For these professionals, it provides a stepby-step process that helps them consider these factors in a logical and systematic way. This will help these practitioners understand the unique factors of each child and their family, and to turn this knowledge into the most effective plan to support them.
However, the guideline also has great importance to medical practitioners. The step-by-step process that it outlines can also help structure the engagement that medical professionals have with autistic children and their families. The guideline also provides very clear insight for medical practitioners into the clinical interactions that the children and families will be having with other professionals. Both of these factors
can significantly improve the experience of kids and families with the medical system. While the guideline is not mandatory, it has important implications for government systems such as the NDIS.
At a time when there is concern about how the NDIS can best support its participants, this guideline provides evidencebased guidance to support that endeavour. We are in ongoing dialogue with the NDIS about how the guideline can better support the NDIS system, and ensure that all children in Australia have access to safe, effective and desirable therapies.
ED: Professor Andrew Whitehouse is Bennett Chair of Autism at the Telethon Kids Institute and the University of WA.


Any health professional who provides services to mothers and infants should be aware of the World Health Organization guidelines regarding infant feeding.
Infants under six months should be exclusively breastfed, with family food being introduced at six months and breastfeeding continuing until two years or beyond if the mother and child desire.
The health benefits for infants, mothers and the community are well-reported.
However, according to the latest Australian Bureau of Statistics (2021), only 35.4% of Australian infants are currently exclusively breastfed for up to six months, which is well below the WHO’s target of 70% and the current world average of 44%.
Although breastfeeding is a biological norm and most mothers desire to breastfeed, the act of breastfeeding is a learnt behaviour. Mothers require support from well-trained and knowledgeable professionals to learn how to attach their baby and understand their baby's cues.
Since the late 1990s, hospital length of stay following birth has greatly reduced, sometimes less than 24 hours but more commonly one to two nights. However, intervention rates are increasing and more than 37% of Australian mothers currently give birth by caesarean, 12% by vacuum or forceps. Approximately 43% of first-time mothers are being induced, with only 40% of women presenting to maternity services in spontaneous labour.
In the first few days following birth, newborns receive colostrum, with mothers’ milk volumes starting to increase by day three to four. Interventions such as caesareans can delay this by 5-7 days. Similarly, increased interventions can decrease a baby’s desire to feed
in the early days after birth. This means many mothers and babies are potentially being discharged before milk volumes start to increase and when babies are not yet feeding efficiently.
For healthcare professionals who see new mothers and babies immediately following birth, it is important to understand that early, uninterrupted skin-to-skin and 24-hour rooming-in can positively influence the duration of breastfeeding.
Although, medical interventions can impact a woman’s ability to experience skin-to-skin immediately and care for her baby without physical support. Those who have had caesareans and epidurals may also struggle to care for their babies immediately following birth, which in turn can decrease women’s ability to be involved in their baby’s care and decrease opportunities for early milk removal.
A literature review by James, Sweet, and Donnellan-Ferandez (2016) reported that breastfeeding success can be impacted by length of stay (LOS) in hospital, advocating for individually tailored LOS to the mother's needs and desires.
The authors found some mothers benefited from longer hospital stays, while others benefited from being in their own home environment. The authors also reported that a lack of practical advice regarding breastfeeding can negatively impact a mother's confidence, which may decrease the duration and exclusivity of breastfeeding.
Yet, research currently being conducted through Edith Cowan University confirms that conflicting advice and lack of practical breastfeeding support is still an issue for new mothers while in hospital.
According to Swerts et al (2016), the first two weeks post-birth are
crucial for breastfeeding support. After discharge, Australian mothers are generally seen at home by visiting midwives provided by the hospital of birth, with the majority receiving support only once or twice in the first week.
Following that, care is transferred to the child health nurse, who traditionally visits the woman and her infant once in the second week following discharge. New parents can then be left on their own until a GP or follow-up obstetric appointment at six weeks postpartum, which may leave new mothers lacking breastfeeding support during the crucial first few weeks.
A Cochrane Review by McFadden et al (2017) reported "when breastfeeding support is offered to women, the duration and exclusivity increases." The authors of this review reported that maternal breastfeeding support is best offered by trained professionals or peer support counsellors, with the most benefit seen with the support being delivered face-to-face and tailored to the individual needs to the mother and baby.
A schedule of at least 4-8 postnatal visits has also shown to have a positive impact on breastfeeding duration.
To optimise Australian breastfeeding rates, health professionals and policy makers need to advocate for more time with women at the bedside prior to discharge, provide consistent and practical breastfeeding support in hospital and once discharged, and increase accessibility to regular breastfeeding support in the first few weeks, even months, after birth.
ED: Justine is a registered nurse, midwife and International Board-Certified Lactation Consultant, and a Master of Midwifery (Research) candidate at Edith Cowan University.





The rise in antimicrobial resistance is a global health priority, predicted to account for over 10 million deaths annually by 2050. With very little investment being made into developing new antibiotics, there is now a desperate need for alternative and adjunct treatments.
Bacteriophages (phages) are natural viral predators of bacteria. They can be found everywhere in the environment, including in soil and water. They are highly specific to their bacterial hosts and are self-propagating, meaning they naturally expand as long as their host bacteria are present, utilising the bacteria’s cellular machinery for
their own replication. These phages are referred to as “lytic” phages, as they successfully kill bacteria in the pursuit of their own expansion.
Following the discovery of these ‘superhero viruses’ by Felix d’Herelle and Frederick Twort in the early 1900s, their use in treating human and animal bacterial infections, referred to as “phage therapy”, began around 1919.
Falling out of favour to penicillin and other antibiotics, phage therapy was practised almost exclusively in selective Eastern bloc countries while the West pursued antibiotics. As we are faced with a global AMR crisis, there is now widespread

rejuvenated interest in phage therapy.

With successful phage therapy cases increasing and an explosion of phage research laboratories all over the world, it seems that we are very much living in the renaissance of the humble bacteriophage, where “going viral” might be just the alternative/adjunct treatment we are looking for.
Our laboratory at the Telethon Kids Institute has had an interest in bacteriophages since 2017 – formed largely by working closely with clinical specialists at Perth hospitals,
continued on Page 38




continued from Page 37
to whom the burden of multiple drug resistant bacteria had become increasingly apparent, especially in the context of chronic lung diseases such as cystic fibrosis .
With funding and support from the Rothwell Family Foundation, we have been able to curate a biorepository of more than 3500 phages against various bacteria including Pseudomonas aeruginosa, Burkholderia cepacia, Staphylococcus aureus and Acinetobacter baumanii which will expand further to include Mycobacterium abscessus, Mycobacterium avium and Stenotrophomonas maltophilia among others.
In response to local consumer interest spurred by several well-publicised cases, our team at the Wal-yan Respiratory Research Centre formed a state-based phage therapy taskforce for the local establishment of phage therapy in 2021.
The WA taskforce has been named START Phage WA (Strategic Taskforce for treatment of Antimicrobial Resistant bacteria with Targeted Phage therapy), with the name representing consumer sentiment, where amongst the WA CF community, phage therapy has been identified as the number one research priority.
START Phage WA partners clinical representatives from major Perth public health campuses and PathWest, together with consumers and experts in pharmacy, governance and basic science. Its primary function is to champion the establishment of phage therapy in WA, initially through an ethics approved protocol for compassionate access, delivered under the Therapeutic Goods Administration’s Special Access Scheme pathway. The protocol has been approved by Sydney Children’s Hospitals Network and allows all participating sites in Australia to proceed with a standardised approach to phage therapy under the National Mutual Acceptance system. Site approvals in WA are currently being finalised at Perth Children’s Hospital, Sir Charles Gairdner Hospital, Royal Perth Hospital, Fiona Stanley Hospital and PathWest.
To support the compassionate use of phage therapy in WA and our translational vision, in 2022 we were awarded a $650,000 grant from the WA State Government Future Health Research and Innovation Fund to establish a small-scale phage production facility in Perth. With additional support from Therapeutic Innovation Australia, the facility is currently being established in partnership with Cell and Tissue Therapies WA located at Royal Perth Hospital and is anticipated to be operational by mid-2023.
Its purpose is to meet the state’s needs for treating those most in need due to MDR infections. If there is a need beyond our collection, engagement with our national and international networks will be able to source appropriate phages.
The prospects for phage therapy in WA have grown remarkably in the past several years. Research in our
laboratory is continuing and upscaling of the entire phage pipeline has been supported by a $1.98 million Medical Research Future Fund grant awarded at the beginning of 2023.
This grant will support the expansion of the phage biorepository, continue to generate preclinical safety and support the “TERMINATE” trial - the first in human trial of phages against
Pseudomonas aeruginosa. With support from Conquer Cystic Fibrosis and Cystic Fibrosis WA, outcomes are now likely to drive mainstream recognition of this therapy and guide future larger scale clinical trials.
Phage therapy implementation in WA is testament to the integral partnerships established between consumers, clinicians and scientists alike, where a need has been


identified and expediently enacted upon.
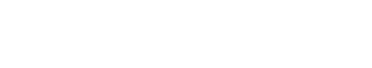
Our phage platform has now placed us on a world stage in the current “age of the phage”, where our vision is to support national and international treatment needs, primarily in neighbouring Asian countries. The prospect of delivering locally manufactured phage to those in greatest need is something to be celebrated and we are grateful to our clinical and consumer partners who continue to champion this cause.
ED: For more information about Phage WA, Associate Professor Kicic’s research and the compassionate use (STAMP) protocol, go to https://walyanrespiratory. telethonkids.org.au/projects/phage-wa/ Dr Anthony Kicic is Associate Professor at the School of Population Health, Curtin University and Head of Airway Epithelial Research at the Wal-yan Respiratory Research Centre – a partnership between the Telethon Kids Institute, Perth Children’s Hospital Foundation and Perth Children’s Hospital.
Dr Angela Fuery is a Postdoctoral Researcher at the Wal-yan Respiratory Research Centre and Chair of the WA phage therapy task force, START Phage WA.
Whilst screening mammography has been shown to be effective in reducing breast cancer mortality in women aged 50-74 years, the World Health Organisation has found that there is insufficient evidence of benefit to recommend screening in women 74 years and older.1
As the first point of contact for health issues for many Australians, GPs have a key role in communicating the potential benefits and harms (eg. over-diagnosis and over-treatment) of screening mammography to older women.
A reasonable approach to optimising the benefits of screening for older women is for GPs to individualise their advice based on comorbidity status and life expectancy. A decision to stop breast cancer screening does not mean abandoning health promotion, but rather refocusing on interventions more likely to be of benefit sooner.

Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
A couple of stories caught my eye over the Easter break. The first was from The Wall Street Journal on a trend in the US for patients with cancer to have more personalised care based on their unique circumstances. It quotes an 81-year-old woman from Connecticut with breast cancer who “skipped some treatments to keep her dance card full” after opting for partial mastectomy.
“Once I got my arms around it and really understood it wasn’t a death sentence, then next thing I wanted to do was say, OK, how do I maintain my lifestyle?” she said. The article quotes doctors on a move away from slavish following of protocols to patients having more options and more involvement in the decision-making process. That there is a trend to prioritise lifestyle and enjoyment of life postpandemic is perhaps not a surprise.
We typically follow US more than UK trends these days, so we will likely see more of this personalisation here. And probably not just in cancer care but in all facets of health care, with women’s health at the forefront given women are disproportionately greater users of health services than men.
Some doctors may see this as a threat, but it is massive opportunity. An informed patient knowing their options, making a conscious choice will be more engaged with the management plan. This can improve compliance and outcomes.
The Australian reported on a community health practice dealing with complex cases in a low SES area including refugees, homeless and drugaddicted people. The centre focuses on multidisciplinary care performing an above average number of case conferences. Their thanks was a Medicare audit.
It is estimated, that on average, female doctors spend more time with patients than their male colleagues. The Medicare rebate (or private fee) is identical, but if the number seen per hour is less the earnings per hour are also less.
The report commissioned by the Federal government on the back of alleged $8 billion in Medicare fraud found that most of the “fraud” was in fact honest error caused by the massive complexity of the system. Report author Dr Pradeep Philip noted that doctors were terrified and tended to underbill and provide less services. This hits the disadvantaged the most.
The message to the government from Dr Philip was clear “You want the system to support clinical judgment, not the other way around”. Whether this message is heeded, or we get more platitudes about “strengthening Medicare” remains to be seen.

It is estimated, that on average, female doctors spend more time with patients than their male colleagues. The Medicare rebate (or private fee) is identical, but if the number seen per hour is less the earnings per hour are also less.




Various screening options are available during the first trimester. These can be broadly grouped under i) Aneuploidy screening +/- diagnostic testing, ii) Screening for severe structural fetal abnormalities, and iii) Preeclampsia screening (and initiation of prophylaxis for high-risk women).
Sonographic determination of the nuchal translucency (NT) and biochemical markers (PAPP-A, free BHCG) are used along with clinical factors to determine risks for Trisomy 21, 18 and 13. Performed at 11-13+6 weeks, cFTS has a good detection rate (around 85%) at a false positive rate of 4-5%. For a high probability result, further testing is offered via diagnostic test (CVS or amniocentesis) or secondary screening by Cell freeDNA (cfDNA) testing.
Women with a very high probability result (generally >1:100), any structural fetal abnormality on first trimester scan or a very thick NT measurement, should be recommended a diagnostic test.
Commonly referred to as NIPT (NonInvasive Prenatal Testing), CfDNA testing is another screening option available with excellent detection rates for aneuploidy (>99% for T21, and around 96% for T18 and approximately 91% for T13) at a low false positive rate of under 1%.
Accurate gestation age, fetal number, and viability should be confirmed before testing with ultrasound. It can be offered as primary screening or as follow-up testing when conventional cFTS has returned a high probability result, or suboptimal risk reduction.
All screen-positive results need to be confirmed by a diagnostic test, and a screen-negative result does not eliminate the possibility of an affected fetus as there can be
First trimester ultrasound at 13-14 weeks is suggested for screening, even in the setting of a low probability Non-Invasive Prenatal Testing (NIPT) result. If there is a high probability result for NIPT, referral to a subspecialist is suggested for counselling regarding invasive testing. Pre-eclampsia screening can be performed at the time of the First Trimester Ultrasound. If screen positive, low dose aspirin needs to be started before 16 weeks for it to be effective.
other chromosomal abnormalities or non-chromosomal structural abnormalities not detected by cfDNA. Discuss the possibility of a failure to get a result with the patient.
First trimester ultrasound survey (usually around 13 weeks) should always be performed, even if the cfDNA screening returns a low probability result, for the detection of structural lesions.
Pre-eclampsia (PE) affects roughly 2-8% of pregnancies and is best described as a syndrome with maternal manifestations of new onset hypertension and proteinuria, and fetal manifestation of intrauterine growth restriction. In its most severe form, it can cause severe maternal multi-organ dysfunction leading to various complications and increased perinatal morbidity and mortality due to preterm birth.
There are at least two distinct forms of PE, one which has its onset earlier in pregnancy leading to delivery before 32 weeks, and another with later onset in the third trimester and usually delivery at or after 37 weeks. Decades of research has produced a better understanding of its pathophysiology.
We are now able to accurately predict if PE is possible. In recent years, several randomised trials and meta-analyses have shown beyond doubt that aspirin taken at an appropriate dose (>100 mg daily) and started before 16 weeks, can prevent most of the early onset and severe forms of PE.
Traditionally, screening has been based on maternal demographic characteristics/risk factors and MAP (Mean Arterial Pressure). However, screening using just these has a low detection rate (39% for preterm PE and 34% for term PE, with a false positive rate of 10.3%). The current preferred approach, recommended by FIGO, is performed at 11-14 weeks, and is coordinated by ultrasound providers. The a priori risk is combined with biophysical MAP, Uterine Artery pulsatility index (Ut-PI) measured on ultrasound and biochemical markers (Placental Growth Factor – PLGF). Extensively studied in various large prospective trials, this screening method, using a risk cut-off of 1:100, has shown detection rates of 88%, 69% and 40% for early onset, preterm and term PE respectively.
Following screening, women identified as high risk for developing PE should receive aspirin 150mg nocte daily from 11-14 weeks until 36 weeks, when delivery occurs, or when PE is diagnosed.
Various effective first trimester screening strategies are available, and they enable the clinicians to help provide information upon which informed decisions can be made by the couple and effective prevention strategies can be implemented for the better health and outcome of the pregnancy.
Author competing interests – nil.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Generalisation can lead to systematic biases affecting patient care. For example, in the United States, a correction factor for the determination of estimated glomerular filtration rate (eGFR) in patients of African American ancestry, presumed to have higher creatinine concentrations owing to greater muscle mass, has historically been applied. The effect is to increase the eGFR, which might overestimate it in some patients, leading to an underdiagnosis of early (and late) kidney disease and consequently delayed care. Therefore, the ancestry-based correction factor is now falling out of favour across North America.
The healthcare sector has also been slow to keep up with the needs of transgender (including non-binary) people. Large gaps remain in the capability of clinical software, including laboratory information systems, to adequately cater for this group. The evidence base for transgender-specific reference intervals (RIs) permitting accurate interpretation of laboratory results is also lacking.
Many reference intervals (RIs) published on laboratory reports are sex-specific. Some are widely divergent with no overlap (for example testosterone, expected in all cases to be much lower in healthy cisgender adult females than males). Others exhibit significant overlap (such as haemoglobin and creatinine, which are on average higher in males, but with overlapping distributions). Assumptions about sex-based biological differences will not hold true in every individual (for example, an athletic female could have higher creatinine than a sedentary male, without it implying any pathology).
Nonetheless, sex-specific RIs are thought to be mostly valid and broadly useful. For example, colorectal cancer causing borderline low haemoglobin in a cisgender male might be
Laboratory software providers, like many other medical software providers, have not adequately catered for specific transgender issues
For many laboratory values that are sex-dependent, reference intervals for transgender patients are not well established Gender affirming hormone therapy complicates the establishment of transgenderspecific cut-off values, but there is increasing evidence supporting particular cut-offs after a minimum period of therapy.
missed if a female RI were used, or polycythaemia vera missed in a cisgender female patient in the reverse scenario.
However, RIs for transgender people are not well-established. A greater degree of physiological heterogeneity might exist in transgender people than in cisgender people, especially in those recently commenced on gender-affirming hormonal therapy (GAHT), potentially making reference intervals more difficult to establish.
For any parameter likely to significantly change with GAHT, the duration of therapy required to do this and the point at which the change becomes stable need to be determined. For some tests, data (albeit limited) exist to support the use of the cisgender RI for transgender patients of the corresponding gender after a certain duration of GAHT.
High-sensitivity cardiac troponin results in healthy transgender men and women after at least 12 months of GAHT approximate those of cisgender men and women, respectively. This is also true of haemoglobin.
Prostate specific antigen (PSA) testing in trans women is another area in which evidence is lacking.
Given that oestrogens and antiandrogen therapies suppress PSA, what cut-off should be used to determine the need for further investigation (such as magnetic resonance imaging or prostate biopsy) in a trans woman who wishes to have PSA testing, given the standard thresholds are likely to be too high? Some advocate further investigation above a PSA concentration of 1.0 ug/L in this setting.
Better data about RIs for transgender people that correspond with the presence, type and duration of hormonal therapy received could enable more accurate interpretation of results, but implementation would be difficult.
The clinical laboratory may not be provided with sufficient clinical information to provide the most appropriate thresholds. Furthermore, transgender patients often see more than one doctor (for example, a general practitioner and an endocrinologist), and the documented gender can vary from one request form to the next.
Consistent with many types of medical software, inflexible laboratory information systems are unable to record that the patient’s preferred gender and sex assigned at birth might differ. Given the increasing ability and desire of patients to access their own pathology results directly, the potential for psychological harm by unintentionally misgendering the patient is also a consideration.
Continued efforts on the part of assay and medical software providers and health services are needed to address the particular needs of transgender people. This must be respectful and inclusive, and wherever possible incorporate evidence bases equivalent to those taken for granted for cisgender people.
Author competing interests - nil


In the rare event that a child is born with a recessive genetic condition, the impact on the family can be devastating. One in 20 individuals carry a gene for a recessive condition, and if both individuals in a reproductive couple are carriers (for autosomal conditions), then their children have a one in four chance of being affected.
The Australian Government is set to fund triple gene reproductive carrier screening from November 2023 through Medicare.
Currently carrier gene testing is treated as an adjuvant to preconception or early pregnancy assessment, rather than standard care. Infrequency of couples seeking pre-conception review, limited awareness by clinicians and cost are all hurdles to couples being offered testing.
The three most common and serious recessive conditions, included in the triple gene screen, are cystic fibrosis (occurring in about 1 in 3000 births), spinal muscular atrophy (1 in 10,000 births) and fragile X syndrome (1 in 5000 births). Testing for these has been available for the past 20 years and when ordered together cost about $400, often with free testing for the partner in the event of a positive result.
In the past 10 years, nextgeneration sequencing has allowed development of expanded carrier screens, through blood and salivary sampling, of more than 700 conditions, including thalassaemia and some myotonic and muscular dystrophies, at a cost of up to $2000+ per couple. Gene panels for extended screens vary between pathology providers, and cost generally parallels in a number of included conditions.
Reproductive carrier screening can be ordered by all providers with a specialist registration, but is most often requested by general practitioners, fertility specialists and obstetricians.
Reproductive carrier screening has been available for 20 years, but awareness and cost have meant that uptake has been low Identifying carrier couples can reduce the number of babies born with inherited conditions that are fatal or carry significant disability
Carrier couples require timely access to investigation and management options, whether it be prior to or following conception.
Traditionally testing was for individual genes, targeted at highrisk populations: carriage of cystic fibrosis has an incidence of one in 25 in the Caucasian population but one in 94 in East Asian population; alpha thalassaemia has a one in three carriage rate in Middle Eastern and African populations; the Ashkenazi-Jewish population are at the highest risk of Tay-Sachs disease with carriage at one in 27.
As a result of mixed-race conception, there has been a move toward pan-ethnic screening, where an expanded screen would test for the most common and serious recessive conditions identified globally.
Carrier gene testing has its limitations, where not all mutations of a gene can be tested for. The detection rate of spinal muscular atrophy gene mutation is over 90%

in most populations but only 71% in the African American population.
If both members of a reproductive couple are carriers of the same condition, options include IVF and pre-implantation genetic testing of embryos, spontaneous conception and prenatal diagnosis, with or without an option of termination of pregnancy, or neonatal testing.
In order for couples to navigate these decisions it is imperative that they have timely and affordable access to appropriate genetic counselling and diagnostic services. While reproductive carrier screening was developed in order to identify at-risk offspring, it is important to include in pretest counselling that diagnosis of carrier status can also have implications for the patient’s own health. Female carriers of fragile X mutation or premutation are at risk of premature ovarian insufficiency and fragile X-associated tremor and ataxia syndrome, a neurodegenerative condition with onset in middle age. Female carriers of ataxia-telangiectasia are at increased risk of breast cancer.
The Medicare rebate for the triple gene reproductive carrier screen will increase access for, and identification of, carrier couples. It is imperative that this is met with access to appropriate information and management options.
Author competing interests – nil
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

As a woman who had her second child using ART at 40, I understand what it is to be an older woman seeking assisted reproduction for couple infertility. Recent data from the Australia and New Zealand Assisted Reproduction Database (ANZARD) suggests that one in four (23.9%) female patients were aged 40 years or older seeking treatment for infertility.
Age-related infertility is largely a result of the reduced quality of oocytes. However, reduced quantity does hamper the efforts of fertility specialists. Although IVF was never touted as overcoming age-related infertility, many women over age 40 are shocked to learn of their limited chance of success.
An independent, Australian government funded website www. yourivfsuccess.com.au, provides information on all Australian fertility clinics. The IVF success estimator algorithm is generated from data provided by all fertility clinics to ANZARD.
Consider a couple where the woman is 41 years and the man 40 years old with unexplained infertility (all tests normal). Their chance of a live birth is 11% with one IVF cycle (including transfer of all the embryos in both the fresh and frozen cycles) and if they have a second cycle their cumulative chance would be 19%. The numbers drop to 7% and 13% at age 42
And 5% and 8% at 43. By age 44, 90% of a woman’s embryos are aneuploid (abnormal). However, increasingly, women will pursue autologous IVF, even into their late 40s.
Currently there is a push towards ovarian rejuvenation techniques in an attempt to improve IVF success in this group. In the anti-ageing revolution, this sounds like the elixir of youth, however are we simply selling the dream?
One such technique is intraovarian injection of platelet rich plasma (PRP), a product used in areas including plastic surgery
IVF doesn’t overcome age-related infertility. Success rates beyond 40 years drops below 10% There are many ‘ovarian rejuvenation’ techniques, none of which have been proven efficacious
Ovarian-injected PRP is a novel technique but, as yet, not subject to high quality study and should remain in the context of research before widespread clinical adoption.
and orthopaedics. Platelets release over 200 different growth factors and cytokines involved in angiogenesis, cell division and tissue regeneration. Thus, PRP has found its way into use in reproductive medicine including treatment of thin endometrium, intrauterine adhesions and recurrent implantation failure.
In ovarian rejuvenation, a patient’s own PRP is injected into the ovarian cortex close to the remaining primordial follicle pool, which then results in the release of growth factors and cytokines that promotes new healthy follicle development. These follicles are considered to be otherwise ‘resistant’ to development and recruitment by follicle stimulating hormone (FSH).
A systematic review suggests that PRP intervention improved ovarian reserve parameters (AMH, antral follicle count) and ICSI cycle outcomes such as fertilisation and embryo numbers, though made no comment on pregnancy or live birth rates. Ages and ovarian reserves in the groups studied varied widely.
A further retrospective study, using PRP in women with low ovarian reserve in an IVF setting, considered women in four welldefined age and AMH groups (POSEIDON criteria) finding significantly increased egg numbers in all groups post-PRP injection. This was particularly significant in
women over 35 with an expectedly low ovarian reserve (median age 40). They gave a pregnancy rate of 10.7% in this group but no live birth rates. Without a control group, it is difficult to determine if this could simply be the background pregnancy rate for these women.
A more recent Australian case series of older women with low ovarian reserves in a single centre demonstrated no improvement in egg numbers but appeared to increase the number of embryos generated compared to the patient’s pre-PRP IVF cycles.
In this poor prognosis group (n=20), there were six pregnancies post-PRP, and no miscarriages. Like previous publications, the authors noted limitations including the small cohort, lack of a control arm and the possibility that merely injuring the ovarian cortex may be enough of a stimulus to promote follicle recruitment.
Regardless, the 22% pregnancy rate in an otherwise poor prognosis population without time to wait for the obligatory RCT evidence is enough for these authors to continue to offer this to a select group of women. Other centres in Australia and globally are following suit. Without opening Pandora’s box on the acceleration of novel techniques into clinical practice, it is important to consider that this is a fairly ‘evidence-free’ treatment for ovarian rejuvenation, though biologically plausible.
The specific population of women for which this is beneficial has yet to be determined, there are different techniques for preparation of PRP and various protocols for its use. Long-term safety data in human reproduction is also lacking. Based on all of these factors, this is an ovarian rejuvenation technique that should remain within the confines of a research protocol before being released to the masses.
– References available on request
Author competing interests – nil

The average age of menopause in developed countries is 51 years old and is medically defined as one year after the final menstrual period (FMP). Medical confirmation of menopause in women over age 45 is based on two observable indicators, vasomotor symptoms and an irregular menstrual cycle.
For women with suspected early menopause (40-45 years) or premature ovarian insufficiency (under 40), the Australasian Menopause Society suggest that raised Follicle Stimulating Hormone levels on two separate occasions (4-6 weeks apart) is useful in informing a diagnosis of premature menopause.
The timeframe for menopauserelated changes is postulated to be between four and eight years,

Age is not an accurate marker of perimenopause/menopause therefore it is important to be mindful of the indictors when symptoms are being presented.
Listen to the whole experience and consider how changes are impacting on the person’s life
It can be empowering to have an understanding that changes are related to a ‘natural’ process, with advice being given that focuses on lifestyle changes and alternative therapies.
with hot flushes being the most commonly reported and the most bothersome change. They can occur years before or after the FMP, with one study finding hot
Perimenopause is defined as the time period preceding menopause to one year after menopause. It is characterised by hormonal fluctuations and irregular cycles secondary to declining ovarian function. Symptoms vary greatly and can begin more than 10 years before menopause.
Multiple biopsychosocial factors impact a woman’s experience during this transition including age, psychological and physical health, ethnicity, education and attitude to menopause.
The perimenopause is typified by a relative progesterone deficiency due to dwindling ovarian reserve and less frequent ovulation. Progesterone deficiency symptoms include brain
fog, poor sleep, headaches, anxiety, depression, weight gain and irregular and heavy bleeding.
Estrogen levels fluctuate significantly during the perimenopause and this can then lead to a range of symptoms resulting from estrogen deficiency and also a relative estrogen excess. The most significant estrogen deficiency symptoms are hot flushes, night sweats and urogenital symptoms. Breast pain, heavy periods, irritable mood and fluid retention generally occur as a result of relatively high estrogen levels. Furthermore metabolic changes that occur with age and declining estrogen levels increase the risk of cardiovascular disease.
flushes experienced by women into their 70s. With no clear trajectory, it makes it challenging for women to identify perimenopause often resulting in seeking medical advice. Menopause-related changes are purported to affect women from a biopsychosocial and cultural perspective and are inextricably linked to negative perceptions of female ageing. Studies find that in cultures where older women gain status, menopause is viewed as a positive change with fewer problematic symptoms.
Changes linked to this life stage can be challenging, affecting both wellbeing and quality of life. Undesirable physical symptoms include hot flushes and night sweats, urogenital atrophy, reduced libido, dyspareunia, dysuria and musculoskeletal pain. Vasomotor
Managing the troublesome symptoms requires a comprehensive assessment including screening for symptoms, risk of chronic disease and the development of an individualised management plan, taking into account the need for contraception. Management options include lifestyle measures, non-hormonal and hormonal therapies.
These include, maintaining a healthy weight, Cognitive Behavioural Therapy (group or individual can improve sleep and reduce vasomotor symptoms), yoga, slow breathing (for anxiety), hypnosis, and avoiding potential
symptoms are reported to reduce energy levels as well as impacting on social, emotional and mental wellbeing. Hot flushes and sweats are experienced as highly visual signs of reproductive ageing, which can lead to stress and anxiety particularly in contexts where women may not have much control over their environment such in the workplace. What
In my study, primary care practitioners were perceived as an important and reliable source of information. Health-care experiences during the first consultation about issues considered to be menopauserelated had a direct impact on decisions to engage in further help-seeking behaviour with a particular GP.
Participants reported an unwillingness or an inability on the part of some male GPs to understand and explain their menopause experiences. Lisa had been to her GP several times after she experienced similar early menopause changes to her mother:
“I went to a female doctor actually in the end and said, "I want to be
[blood] tested" and she said "yeah' cause the male doctor said "No", his actual words were "No, don't be ridiculous, you’re too young!". There was a perception that there would be more empathy and support from other midlife female professionals, and this was reinforced following consultations.
Experiences identified as having a negative impact through either being perceived as not being taken seriously, not being listened to, or immediately being offered a pharmacological intervention without consulting on the availability of alternative management strategies such as education, lifestyle changes including diet, exercise, smoking cessation and reduced alcohol consumption or alternative therapies such as cognitive behavioural therapy which has been receiving promising results in helping women manage for example hot flushes and night sweats.
Research suggests that while some women may want or need pharmacological interventions, they also want advice that facilitates self-management decision making.
This starts with the confirmation that changes are related to menopause.
Although we are thinking about the menopause experience from the patient’s perspective, it is important to highlight that a high proportion of the health-care workforce are women. Recommendations from a body of work exploring women’s experiences in the work context emphasise the importance of having a positive, open culture to empower women to speak up about any challenges they are experiencing during the perimenopause, menopause and post-menopause to normalise this life stage.
It is key that women know who is best to approach for advice, support and education that is reliable and well informed. This includes clarity (on website and in literature) about who in a practice is best placed to offer advice about menopause.
ED: Dr Middlewick is director of Post Graduate Studies at ECU’s School of Nursing and Midwifery.
Author competing interests - the author was involved in the study quoted.
triggers (e.g. nicotine, alcohol and cow’s milk).
Supplements of magnesium glycinate and taurine can boost GABA, reduce adrenaline and promote sleep. Ashwagandia may reduce anxiety and promote sleep via stablisation of the HPA axis.
Venlafaxine can reduce hot flushes by up to 60%. Dosing should start at 37.5mg once daily and increase to 75mg daily. Symptom relief usually occurs after a week. Side effects include dry mouth, decreased appetite, nausea, constipation and insomnia.
SSRIs (fluoxetine 10mg, citalopram 10mg, paroxetine 10mg) taken for around four weeks may result in a reduction in hot flushes. The dose should be increased slowly over 2-4 weeks. If symptom relief does not occur by six weeks or there are significant side effects, treatment should be stopped. Side effects include nausea, fatigue, tremor, weight changes, reduction in libido.
Gabapentin can be commenced at a dose of 100mg TDS up to
Perimenopause can be a troubling time for many women
A comprehensive assessment of symptoms and risks allows an individualised management plan Optimised treatment minimises troubling symptoms while also minimising long term risks.
a maximum dose of 300mg TDS. Reduction in frequency and severity of hot flushes is comparable to low-dose estrogen. Side effects include drowsiness, light headedness and dizziness.
Clonidine at 25mcg BD up to 75mcg BD can show therapeutic benefit by four weeks. Side effects include dry mouth, drowsiness, insomnia.
Local estrogen in the vagina is an effective treatment for vaginal dryness and dyspareunia as well as treating symptoms of urinary irritability due to urogenital atrophy. Systemic estrogen can be taken
orally (Oestradiol 1 or 2mg) or applied transdermally (Oestradiol 25/37.5/50/75/100mcg patch over 24 hours or Oestradiol gel 0.1% sachet or oestradiol 0.06% gel 1-4 pumps daily).
Oral micronised progesterone can be taken alone or combined with systemic estrogen. This should be taken in the evening to help with sleep and can either be taken daily or two weeks on and two weeks off. Other progesterones include norethisterone, dydrogesterone, levonorgestrel, drosperienone and medroxyprogesterone and can also be used alone or in combination with estrogen, depending on symptoms.
Hormonal contraceptives during the perimenopause include the intrauterine progesterone coil as well as oral progestogens that may be combined with oestradiol, depending on symptoms.
Intrauterine progesterone is also associated with an increased risk of breast cancer over time. The
continued on Page 53
Dermatologist-led cosmetic medicine service

Doctor-delivered treatments, for GP-referred patients
Laser modalities for
Rosacea
Acne
Hyperpigmentation
Lentigos, melasma etc.
Vascular Lesions
Tattoo removal
Hair removal
&
Hair loss service
Comprehensive medical service for alopecia and patterned hair loss
Injectables for medical indications
Wrinkle relaxers
Fillers for loss of facial volume
Birthmarks (pigmented & vascular)
Rejuvenation/ageing
Emphasis on ‘natural look’
Axillary Hyperhidrosis
Referrals accepted by Healthlink, Email, Fax, Post or Phone
Post: Karrinyup Dermatology, 5 Cheddar Place, Karrinyup WA 6018
Phone: (08) 9245 3376 Fax: (08) 9245 5033
Healthlink: karrinyd
Email: admin@karrinyupdermatology.com.au
As a specialist Dermatology Clinic, we continue to accept GP referrals for all general dermatology presentations.
According to evidence from the World Health Organization (WHO), one in five women will experience mental health disorders during pregnancy or in the year after birth. For those women who have been hospitalised for medical conditions in general hospitals, the reported rates of mental health disorders further increase up to 65%.
It is worth noting that based on scientific evidence, approximately seven out of 10 women with mental health disorders are parents (68%).
While the adverse neurocognitive and developmental consequences of maternal perinatal mental disorders in their children are well depicted, the impact of perinatal hospitalisation due to mental health conditions on children’s educational outcomes during adolescence is not really known.
In a recent Australian study using NSW NAPLAN data that examined the association between poor school performance in the adolescent offspring of mothers who experienced psychiatric hospitalisations during the prenatal and perinatal periods, offspring of mothers who were hospitalised for psychiatric conditions during their pregnancy or up to one year after birth were more likely to have poorer academic grades at the age of 14, with boys being impacted the most.
The link was seen with all domains of academic performance, with the highest impact on numeracy
Maternal mental health problems during the perinatal periods are linked with a higher risk of lower school grades in their offspring
The effects of maternal mental health problems during the perinatal periods were stronger in the academic performance of male offspring
Early intervention strategies enhancing academic performance are required to help offspring whose mothers had perinatal mental health issues.
followed by reading. Using multiple regression and controlling for relevant covariates, this study also found that the impact of severe mental health problems was higher when compared to other mental health issues.
Previous studies also found that prenatal and perinatal mental health disorders are often associated with increased risks of poor academic performance in young children.
There are several possible explanations for the association between maternal perinatal mental health hospitalisations and lower academic permanence in offspring.
One is that exposure to maternal mental health problems in the early life of the offspring is linked with a higher risk of neurocognitive deficit,
continued from Page 51
largest systematic review and metaanalysis to date found an increased risk of breast cancer for all women using this, although the numbers are very small. Venous thromboembolic disease is the other risk to consider. Transdermal preparations have not been associated with an increased
risk at doses less than 50mcg of Oestradiol. Absolute risk on oral Oestradiol is low, probably two to three per 1000 women years compared to one for never users.
For the majority of women, the benefits outweigh the risks of Menopausal Hormone Therapy (MHT). Risks can be reduced by commencing therapy early rather
subsequently leading to substantial impairment in memory, overall cognitive function, visual learning, and lower attention span, which are vital for learning and academic performance.
Another possible explanation is that maternal mental health problems in the early life of the offspring, particularly within the first year, are consistently linked with disruption of normal human brain development networks which are crucial for the development of cognition and human behaviours through conception to adulthood.
Additionally, maternal mental health problems early are linked with epigenetic changes in the developing brain, including in those areas vital for memory, learning, and academic performance.
Early intervention strategies are required to help offspring whose mothers had perinatal mental health issues, in order to ensure offspring are given the best opportunity to learn in school and achieve well in their academic performance.
Further robust studies investigating the exact mechanism of how maternal prenatal and perinatal mental health problems are linked with an increased risk for poor educational outcomes in offspring, specifically examining why boys are impacted the most are required.
Author competing interests – the author was involved in research described.

than late and by using transdermal preparations of estrogen with a micronised progesterone or lower risk progestogen. The main risk to highlight is the long-term risk of breast cancer. This mainly relates to the progesterone component of MHT and duration of use.
Author competing interests – nil
Your patients do not need to compromise success and qual ity for cost
Adora Ferti l ity is Austra l ia’s lead i ng provider of affordable and accessi ble IVF Give your patients the best chance of conception without the fi nancia l sacrifice

By referri ng you r patient to ou r hig h l y qua l ified specia l ists, you wil l g ive them access to hig h-qua l ity ferti l ity treatment that offers a n i nd ividua l ised a pproach a nd treatment p la ns a nd med ications sensitive to thei r needs. O ut-of-pocket costs a re ty pica l l y less tha n $2000 for a fu l l y sti mu lated IVF cycle
Between 10-30% of women will have symptoms of pelvic organ prolapse in their lifetime. Although it is a benign condition, the symptoms can have a marked effect on quality of life, affecting bowel, urinary and sexual function, self -esteem and interfering with work and leisure activities.

Prolapse is a failure of the normal mechanisms of support of the pelvic floor, that is, the levator ani muscle complex and its ligamentous attachments to the bony pelvis.
Increasing age and increasing parity are the biggest risk factors. Menopause is related to increasing age but decreased oestrogen has been postulated to play a role.
Operative vaginal delivery – in particular forceps delivery – is now recognised a significant risk factor for all types of pelvic floor dysfunction. Obesity, chronic increase in intra-abdominal pressure (e.g. chronic cough, repeated heavy lifting and chronic constipation) can all play a role.
The terms cystocele and rectocele are commonly used but a more accurate description is anterior compartment (vaginal wall) descent and posterior compartment (vaginal wall) descent. This is because from clinical assessment alone, it is not possible to determine exactly which structure is behind the descending part.
Uterovaginal, apical or vault prolapse is the descent of the uterus or the vaginal apex (posthysterectomy). An enterocele – a cul-de-sac abnormality containing peritoneum and abdominal contents involving the apical, anterior or posterior compartments of the vagina.
Many women are asymptomatic, despite the degree of prolapse appearing to be significant. A sensation of a bulge in the vagina or a dragging feeling in the vagina are common descriptors from
Prolapse is common
Prolapse symptoms can have a marked effect on quality of life
Conservative management methods are best in the first instance.
patients. Dyspareunia or a feeling of an obstruction is sometimes described. Some women have a sensation of incomplete voiding or others may have urinary incontinence. Difficulty opening the bowels or needing to splint the vagina to open the bowels can point towards a posterior compartment prolapse.
The Baden-Walker system describes the descent of the prolapsing part in relation to the hymen, with 0 being no prolapse and 4 being outside the introitus. This method is somewhat subjective. The Pelvic Organ Prolapse Quantification System (POP-Q) is an international classification system that reduces inter-observer variability by using defined points in the vagina in relation to the leading points of the prolapse.
As prolapse is a completely benign condition and available treatments can have varying success rates, the most important factor to determine is how much the symptoms are impacting quality of life. If the woman is asymptomatic e.g. prolapse is noted during routine CST, then doing nothing is completely acceptable.
To this end, a thorough history is essential. Apart from the clinical features, it important to know the woman’s other general medical history, her occupation, her lifestyle, sexual activity and whether she smokes.
The first step in management is to address modifiable factors such as improving chronic cough by
cessation of smoking or optimising asthma management, decreasing caffeine intake to reduce urinary frequency, addressing constipation and addressing occupational factors like repeated heavy lifting. The advantages of pelvic floor physiotherapy cannot be understated. Educating the woman about her pelvic floor and using bio-feedback techniques to teach pelvic floor exercises can significantly improve symptoms for many women, especially if the prolapse is mild. However, it is important to note that this will be of minimal help for severe degrees of prolapse.
Pessaries are a simple and effective method of treating some types of prolapse. They are particularly beneficial in women who have other co-morbidities that make them unsuitable for surgical management. For women who are sexually active, they may be less appealing due to the requirement to remove and re-insert the pessary. Pessaries should be used with topical oestrogen if the woman is post-menopausal.
There are many surgical techniques to manage prolapse. However, prolapse surgery can have a significant failure rate with up to 30% of women treated surgically needing repeat surgery at some stage in the future. This is of particular relevance to younger (pre-menopausal) women. Their likelihood of needing another surgery is quite high so they need to be counselled appropriately before undergoing index surgery. More complicated cases and index surgical failures may be best referred to a urogynaecologist.
Author competing interests – nil
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Every year about 1,800 women are diagnosed with ovarian cancer in Australia. While it is only the ninth most common cancer among Australian women, it is the sixth leading cause of cancer-related death. Ovarian cancer can occur at any age but is most often diagnosed in post-menopausal women.
Unfortunately, about 75% of cases are diagnosed at an advanced stage when the tumour has already spread beyond the ovaries (stages 3 and 4).
Two of the main reasons for this are the lack of effective screening tests to detect ovarian cancer and the non-specific nature of early symptoms, most commonly abdominal and pelvic pain, bloating, difficulty eating or feeling full quickly, and urinary frequency or urgency, which are often vague and similar to symptoms of other more common and often less serious health conditions.
Women diagnosed with ovarian cancer will typically undergo abdominal surgery and receive chemotherapy treatment. Although most women respond well to the initial treatment, 70% of women with advanced-stage cancer and up to 30% of women with early-stage cancer will eventually experience disease recurrence requiring further treatment.
Ovarian cancer treatment often causes side effects such as fatigue, nerve damage in the hands and feet that causes weakness, numbness and pain, insomnia, sexual dysfunction, and anxiety and depression, which linger after the completion of treatment and affect women’s ability to function physically and mentally.
In addition to the burden of cancer itself, as well as the required treatment, many of these women battle other health issues such as osteoporosis, diabetes, or high blood pressure. While often overweight or obese (i.e., BMI ≥25 kg/m2), in many cases women with
Ovarian cancer is often diagnosed late due to non-specific symptoms and no screening test Evidence for benefits of exercise post cancer diagnosis is well established
Resistance exercise may have benefits for women with ovarian cancer.
ovarian cancer have low muscle mass and/or low muscle density, an indicator of muscle quality. Both low muscle mass and low muscle density are associated with decreased treatment tolerance and poorer survival.
The importance of exercise after a cancer diagnosis has been firmly established. Not only does exercise help alleviate the side effects of cancer treatment, it appears to delay cancer recurrence and improve survival outcomes. People with cancer are encouraged to increase their physical activity levels generally with recreational activities, supported by targeted exercise to specifically address disease and treatment-related health issues.
While a small number of studies have investigated the benefits of exercise for women with ovarian cancer, research is scant compared to published research in more common cancers such as breast and prostate cancer. The limited evidence available indicates that exercise is safe and feasible and confers physical and psychological benefits. Existing exercise studies consist mostly of home-based interventions of predominantly aerobic (cardio) exercise, with no or limited supervision. Currently, there are no research-based, cancer-specific recommendations for clinicians or women with ovarian cancer on the role of resistance exercise.
Our team at the Edith Cowan University Exercise Medicine
Research Institute recently conducted a research study to investigate the effects of resistance exercise, delivered in a supervised setting, on skeletal muscle mass and density, muscle strength and physical function in women with advanced-stage ovarian cancer who had completed initial treatment. We also investigated potential changes in health-related quality of life and self-reported pelvic floor function from pre- to post-intervention.
The 12-week exercise intervention consisted of three sessions/week and was delivered in an exercise clinic or by telehealth (online) based on participants’ preference.
Participants completed two supervised exercise sessions (either in-clinic or by telehealth) and one unsupervised home-based exercise session/week. Twelve weeks of resistance exercise resulted in significant increases in muscle mass and muscle density (a measure of muscle quality), upper and lower body muscle strength, and physical function.
There were clinically important improvements in several quality-oflife domains, with no deterioration in pelvic floor symptoms. Although our findings need to be confirmed in larger trials, preliminary recommendations are that targeted resistance exercise in a supervised setting is beneficial and should be included in supported care for this understudied cancer group.
Author competing interests – the author was involved in the research quoted

Kylie Wallace has always been a giver. It’s her passion and with a business partner has turned giving into Seedling Giving, a charity matching service.
For as long as she can remember, Kylie Wallace has given to charity.
“I get no bigger joy in my life than to give other people the opportunity to feel as good as I do every day,” says Kylie. “There’s great power and health benefits to giving. Being able to give someone else joy certainly makes us feel good. I also think it brings meaning to our lives – and we all need that.”
When Kylie got her first job out of high school, she immediately allocated $50 in her monthly budget for sponsoring a couple of children. She credits her dad with teaching her how to be financially independent but also always having enough to give.
“It just became ingrained in my values and was non-negotiable – it speaks to who I am. When
By Ara Jansentimes got tough, I would sacrifice other things or find a way to sell something on Facebook to make sure giving was part of my expenses.
“As a family we would get together and talk about what we would like to support. When my friends went off to Europe after school I went to India and Thailand to volunteer.”
After working in the not-for-profit space, Kylie and her business partner, analyst Jess Bowman, now have Seedling Giving, a service which helps people place donations by suggesting three aligned and diligently researched options, taking into account personal values, passions and life experiences. If your passion is medical research, literacy or saving a species, there is potentially a charity which would

both welcome your donation and make the most of it.
Jess has a background in advising groups like the UN and World Bank. She started her own business called The Good Cause Co, Australia’s first website that provided independent reviews of Australian charities. It was this business that linked her with Kylie and got the pair talking about how to create a business which would combine both their talents and experience while helping make the world a better place or in their words “do good, better”.
In August 2021, when Kabul was taken over by the Taliban, Kylie’s friends started asking her how they could help and who they could donate to. While there were the obvious options, Kylie went off and
did some research as to the groups which could potentially do the most good with her friends’ donations.
“There were the big aid organisations, some established ones and others trying to provide emergency relief. I found it really hard to know who to go to,” she admits. “I’d been working in the space, in development and fundraising and international development, which is why people always thought of me as a go to person. But even I didn’t know who to give to, which was a really big problem. In my research, I came across Jess and The Good Cause Co. and thought with her research background she could provide some answers for me.
“While her company was showing people how to do it, my experience is that people don’t have the time and give up because it’s too hard.”
So, they agreed to join forces and evolved into Seedling Giving. Already thriving after its first year, Seedling has placed almost half a million dollars with Australian charities for more than 40 people and foundations.

“We hear from so many of our donors how they feel such a great sense of abundance through their giving. When you have a roof over your head, the other things you need and you feel like you have enough, those people want to be able to do something good, help and give something back.
“Australians give away 0.25% of our income and around about 60,000 charities collect about $12.5
The Westin, East Perth
Saturday 10th June 2023
Please book a place for the conference at gpurologymasterclass.com.au
RACGP CPD Hours - Approval Pending As Per New CPD Requirements
billion a year. We’d like to see that percentage go up to 1.5% of the annual income. The impact of that rise could be quite transformative for so many of the social issues we’re dealing with and that charities support.
“A bit like my own story, it’s all about creating little habits and doing what you can. As a teen I started giving a little and I was able to give a little more over time and become more sophisticated with my giving. It’s all about starting small and growing.”
To help, Seedling Giving has a free eBook on their website which will help you spot a high performing charity and offers advice on what charities you should never donate to. More details are at https://seedlinggiving.com.au/
PLACES FILLING QUICKLY
Grants available for rural GPs to attend
You may be eligible for funding through the Health Workforce Scholarship Program (HWSP) to attend the GP Urology Masterclass. To apply for HWSP funding, you must meet the eligibility requirements: ruralhealthwest.com.au/ programs/health-workforce-scholarship-program
If you had gone for an ocean swim off our coast some 70 million years ago, you wouldn’t be worried about a crocodile or a shark, because you’d more likely be gobbled up by an even larger marine reptile called a mosasaur.
Welcome to Sea Monsters: Prehistoric Ocean Predators, an exhibition at the WA Maritime Museum in Fremantle that explores how three groups of giant marine animals – ichthyosaurs, plesiosaurs and mosasaurs – ruled the sea when dinosaurs ruled the land. Sea Monsters explores how these three groups, originally terrestrial animals, evolved and adapted to the marine environment.
Developed by the Australian National Maritime Museum in partnership with Queensland Museum, Sea Monsters is the first exhibition of its kind in Australia. This family-friendly and interactive exhibition combines real fossils, gigantic replicas, immersive multimedia and hands-on interactives to reveal ancient monsters of the deep. There are gigantic life-sized casts from actual specimens, including a 13-metre long Elasmosaurus which has an extremely long neck and nine-metre marine lizard called a Prognathodon.
“Ichthyosaurs (dating 251 million to 65.5 million years ago) are the most common type of marine reptile
in WA that we have found,” says palaeontologist Dr Mikael Siversson, Head of Earth & Planetary Sciences at the Western Australian Museum.
“Last year we found skeletons of three of them. They look like a cross between a dolphin and a shark. They’ve been found around areas like Kalbarri and Dandaragan.”
In the exhibition, there’s a huge 1.4 metre Kronosaurus jaw, incredible specimens such as an ichthyosaur giving birth and a five-metre-long fish that died after swallowing another fish whole.


These marine animals were bigger than the largest dinosaurs and developed into awesome apex marine predators. The biggest one was the 24-metre Shonisaurus and
some could swim up to 40kms an hour.
The exhibition details the fascinating story of these long-gone sea monsters through the latest science and amazing fossils from Australia and around the world.
The life-size models were made using original specimens and advanced photogrammetry technology, which uses many photographs of an object taken from different angles to create a 3D version.
Dr Siversson says while those large marine animals no longer exist in our oceans, we live in unique times as there has never been one bigger than the endangered blue whale, which can grow to almost 30 metres, about three school buses long.
“Mosasaurs (which were up to 17 metres long) have been featured in the Jurassic World movies and were pretty vicious and very dangerous. They had extra teeth which made it very difficult to escape. Keep an eye out for those teeth in the exhibition!”
Sea Monsters runs to July 16. For more details and tickets: https://visit.museum.wa.gov. au/maritime/sea-monstersprehistoric-ocean-predators
It’s hard to comprehend just how big marine reptiles were before we humans arrived. In the latest Maritime Museum exhibition, you’ll gain a great size perspective – and learn about what used to live in our waters.

It was in 2007 that South African-born Philip and Vivienne Snowden, after a successful career in the mining industry, purchased their picturesque property in Denmark in WA’s Great Southern and set out to chase their dream to produce high quality wines.

Daughter Pam and son-in-law Patrick Corbett have worked with them, and together they have unquestionably achieved this dream, with Singlefile Wines one of this State’s greatest small volume producers.
The property was planted in 1989, giving them access to some mature fruit. However, they retained the Chardonnay, and pulled the other vines, replacing them with more Chardonnay, a smart move given that Denmark Chardonnay has had significant success. Then their next clever ploy — to set up partnerships across the vast Great Southern Region and draw upon its strengths such as Riesling from the Porongurup subregion and Shiraz from the Frankland River subregion. In this way they are offering the best of the region. The quality is quickly evident. From the labelling, packaging, accompanying stationery and website, all reflecting a class act, and this carried through to the five wines I reviewed which were all indeed excellent.
And the Singlefile name? The family’s geese waddle single file to the property's lake each day.
This wine is from the family property in Denmark. Nose is immediately enticing. Initial roasted cashew and savoury characters from oak, which gives way to stone fruits – white peach/nectarine. Palate is rich, unctuous and complex. Oak is a touch dominant in its youth, but will mellow in time. Creaminess from lees stirring and partial malolactic ferment. A powerful Chardonnay with 8-10 years ahead of it.
I have been following the local iteration of this variety for 30 years now and continue to be impressed. And this is a very good expression of it. Appearance displays a vibrant beetroot red, youthful colour. Nose is of dark fruits – blackberry, plum and with violets. Displays rich ripe plum and blackberry. Mouth-filling, juicy, soft and lush. Ripe tannins with a gripping finish. Firm acid holds it all together. I like this Malbec.
In my opinion, Frankland grows WA's best Shiraz, and this wine is true to form. Appearance is a youthful garnet/brick red colour, with purple meniscus. The nose displays redcurrant, anise, cinnamon and allspice. Oak gives a savoury edge. Flavours are of dark cherry, black olive, blueberry. An easily approachable (in youth) style of Frankland River Shiraz, with elegance, but with generosity and wonderful persistence. Silky tannins. A very fine wine. Will go 15 years. So easy to drink now.
Riesling in WA doesn't get better than that from Porongurup, both for style and ageing, and this wine reflects that. Pristine mid-gold colour with a youthful green hue. Fresh floral aromas, with Meyer lemon and a hint of talcum powder. Flavours of citrus and green apple, minerality with a river pebble mouthfeel. Purity, linear acidity, great length, and a clean finish. This is what Riesling is all about – a 20-year-wine.
A blockbuster of a wine, and flagship of the Singlefile range. It is from that great 2018 vintage and from the incredible Riversdale Vineyard. This wine is still vibrant and youthful for its five years. Colour deep brick red. Aromas vibrant, lifted, exciting, with blackcurrant, earth, liquorice and wonderful oak. Flavours of blackcurrant and black olive. Tight, fine tannins. Smooth, clean, refined, elegance with power. Lingers on the palate. A great wine. Will go 30+ years.

We respect your time is precious. Humphrey Homes’ integrated model of architect, builder and interior designer working together ensures you realise your vision with unrivalled efficiency, quality and budget control. We invite you to experience our architecture and craftsmanship firsthand, at our latest Open House event on 13/14 and 20/21 of May Visit humphreyhomes.com.au for details