






Dividends paid out when you retire throughour Retirement Reward Plan
Access medico-legal experts, 24/7 inemergencies
Local support, from Avant Law’s 80+ medico-legal solicitors nationwide Expert advice to reduce your claimsrisk
















Dividends paid out when you retire throughour Retirement Reward Plan
Access medico-legal experts, 24/7 inemergencies
Local support, from Avant Law’s 80+ medico-legal solicitors nationwide Expert advice to reduce your claimsrisk








This month, we look at how the conversation around menopause and hormone treatments is still not clear-cut, even among health experts.
As regular as Medical Forum arriving in thousands of WA letterboxes each month, so is the menstrual period for women – an event that will span across their lives for 40 years or more.
And when their periods eventually taper off, marking the end of their reproductive life, it can be highly liberating for many women – no more tampons or pads on the grocery list!
While menopause is a biologically inevitable event, the part that is not a given is how it impacts on a woman’s physical and mental wellbeing.
The experience is highly variable, with some women gliding through that life stage, barely aware of their giant hormone reshuffle and grateful that their periods have come to an end.
For others – research suggests one in three midlife women – menopause is life-altering, but not in a good way, with symptoms so severe they struggle to get out of bed or even string together a sentence. This can last for several years.
This month, we look at how the conversation around menopause and hormone treatments is still not clear-cut, even among health experts.
Some argue that the recent release of a series of opinion papers in The Lancet, which collectively argued that menopause is over-medicalised, has further muddied the water.
The call now is for fewer population surveys (do we really need them, still?) and less use of language that perpetuates the myth that women should just follow a healthy lifestyle and “get on with it.”
If doctors can’t agree on the use of menopause hormone therapy, how confusing must it be for their patients.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.

FEATURES


12 Cover story: Menopause and mental illness – it is a thing!
16 Close-up: Dr Rosalie Schultz
22 The stigma of stomas
26 WA gears up for a digital world
LIFESTYLE
56 Drawing the heart of the matter
57 German film festival
58 Legally speaking drama
59 Wine review: West Cape Howe – Dr Craig Drummond


1 Editorial: Individualising menopause experience – Cathy O’Leary 4 News & views 20 Alcohol guidelines behind the science
WAAC’s syphilis testing campaign 39 Progress in a strange world
– Dr Joe Kosterich
55 Call to help PNG kids
The happy winner of our March doctors dozen from Duke’s Vineyard is Dr Steve Swift.
This month we have another selection of premium wine to give away, this time from West Cape Howe, and you can read Dr Craig Drummond’s review on page 59.
We also have a bumper movie give-away, with five double tickets to any film at the German Film Festival in Perth from May 16 to June 5, and 10 double passes to the action-comedy Bad Boys: Ride or Die.
To win the wine or movie tickets use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor Cathy O'Leary 0430 322 066 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au
Journalist Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer 0424 883 071 andrew@mforum.com.au
Clinical Services Directory Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
















All
women having routine mammography should be told if they have dense breasts and are of greater risk of breast cancer, the peak body for radiologists says.
In a position statement published last December, the Royal Australian and New Zealand College of Radiologists joined calls for widespread breast density reporting to inform patients of their particular risk.
Breast density — the ratio of fibro-glandular tissue to fatty tissue — can be an independent risk factor for breast cancer and can also affect the accuracy of mammogram reporting, because dense tissue and tumours both appear white in mammograms.
About 40-50% of women have dense breasts, but currently there is no national policy on optimal management of notifying women of breast density, with only Western Australia and South Australia requiring patients to be assessed and notified.
Last year, the US Food and Drug Administration introduced a requirement that breast density be reported on all mammogram results nationwide, and for that report to go to both clinicians and patients. Previously this was the rule in some states, but not in others.
There are now calls to have a consistent national policy on breast density notification across Australia.
“While a future risk-based model for breast cancer screening is being developed, RANZCR recommends mandating the reporting of breast density in both screening and diagnostic settings,” the college statement said.
One in 10 Australian women are estimated to have Breast Imaging-Reporting and Data System (BI-RADS) category D density, or extremely dense breasts.
“Studies have demonstrated that extreme (mammographic breast density) is associated with a 2.1fold increased risk of breast cancer compared with the average risk scattered category of BI-RADS category B,” the RANZCR said.
Pregnancy issues link
Curtin University research has revealed a link between miscarriage and the increased risk of developing complications of gestational diabetes and high blood pressure-related disorders in later pregnancies.

Meanwhile a new Australian trial is looking at the potential harms and benefits of notifying women of the risks associated with breast density during routine breast screening.
A randomised control trial undertaken in Queensland aims to examine the longer-term effects of notifying women about breast density in relation to breast cancer risk factors.
The trial, which started last September in BreastScreen Queensland clinics, has been outlined in a study protocol published in the Medical Journal of Australia
The researchers said there had been continued international debate surrounding the pros and cons of widespread breast density notification. They hope the evidence from the study would guide best practice and policy for breast screening in Australia and abroad.
The trial is a world-first in assessing the impact of notification (versus not) using a randomised design, and to also test different ways of telling women that they have dense breasts on mammograms.
It will look at the benefits and harms of notification, including the effect over time – two years or more.
The study will look at psychological outcomes of notifying patients – whether they feel anxious, confused or informed – and also whether it influences them to have follow-up GP consultations and supplemental breast screening.
Researchers hope the findings will help BreastScreen Australia to develop best practice policies for notifying women of breast density and to find the most effective way.
ED: Congratulations to BreastScreen WA, which turns 35 this year after starting as a pilot program in 1989. It targets women aged 50-74 years, offering free screening every two years, but women can access it from the age of 40. Go to www.breastscreen.health.wa.gov.au
Researchers from the Curtin School of Population Health analysed 52 studies involving more than 4 million pregnancies across 22 countries to investigate the health impacts of miscarriage, abortion and recurrent pregnancy loss on subsequent pregnancies.
The study found different health risks for each group.
People who had experienced a miscarriage were 44% more likely to develop gestational diabetes during later pregnancies but only 6% more likely to develop high blood pressure in subsequent pregnancies.
People who had experienced recurrent pregnancy loss showed no increased risk of gestational diabetes but were 37% more
likely to develop pre-eclampsia, a potentially dangerous complication characterised by high blood pressure, in later pregnancies.
There was no evidence linking abortion to diabetic or hypertensive related issues, either during or outside of pregnancy.
Lead study author Dr Jennifer Dunne said establishing the links between pregnancy loss, diabetes and high blood pressure could have a far reaching impact.
On November 1, 2023, genetic carrier screening for cystic fibrosis (CF), spinal muscular atrophy (SMA), and fragile X syndrome (FXS) was added to the MBS, marking a significant milestone in accessible healthcare for all Australians.
This shift represents a significant advancement in preventative medicine within the domain of general practice, ultimately enhancing accessibility and affordability for patients.
Genetic carrier screening should now be a routine part of pre- and early pregnancy clinical management by GPs and specialists, with both RANZCOG and RACGP guidelines recommending that genetic carrier screening be offered to every woman and couple who are planning or in the first stage of pregnancy, regardless of their risk factors.
Importance of early screening
It is recommended that testing is undertaken before pregnancy so greater reproductive choices can be made such as pre-implantation genetic diagnosis through IVF, using donor eggs (or donor sperm for CF and SMA) donor embryos, or adoption. Early detection is paramount as it also allows more time for counselling.
CF, SMA & FXS screening
Screening for CF, SMA and FXS provides patients with information regarding their chances of having a child with any of these conditions.
• One in 20 people are carriers of at least one of these conditions
• 90% of carriers have no family history
• One in 160 couples will be found to be at risk of having an affected child.
Cystic fibrosis (CF)
• Approximately 1 in 25 people are carriers of CF
• Clinical Labs’ CF screening covers more than 75 common mutations in the CFTR gene
• CF affects about 1 in 2500 people.
By
Spinal muscular atrophy (SMA)
• About 1 in 35 people are carriers of SMA
• Clinical Labs’ SMA screening identifies deletions of the SMN1 gene (one copy), which account for approximately 96% of the mutations in this gene
• SMA affects approximately 1 in 6000 people.
Fragile X syndrome (FXS)
• FXS, an X-linked condition, is the most common inherited form of intellectual disability
• Approximately 1 in 330 people are carriers of FXS
• FXS affects approximately 1 in 3600 men and 1 in 6000 women
• FXS carrier screening is recommended for females, as it is inherited in a different way to CF and SMA. Female patients who have the gene change (number of CGG triplet repeats) in the FMR1 gene are found to be at risk of having a child affected by FXS, as the abnormal gene may expand over generations.
• The size of these CGG triplet repeats determines the chance of the FXS gene failing to function in a normal way and, therefore, the clinical presentation
• Males can also carry the faulty FMR1 gene on their one X chromosome and may pass it on to their daughters. (Testing would incur a private fee – not eligible for Medicare billing).
In addition to bulk-billed screening, Clinical Labs also offers expanded carrier screening options at an outof-pocket cost for patients who want
a broadened assessment of their risk of having a child with a genetic condition. For information about our Comprehensive and Ashkenazi Jewish Carrier Screening tests, visit antenatal.clinicallabs.com.au/doctor/ carrier-screening
Medicare criteria
Testing is available for all individuals, even those with no symptoms or family history. Male partners of the biologically female positive cases for CF or SMA (not FXS) are eligible for testing under Medicare cover. Private fees may apply if criteria are not met.
New items 73451 and 73452
The patient who is planning pregnancy or already pregnant should be tested first under MBS item 73451 before testing the reproductive partner under MBS item 73452 to ensure an informative and clinically relevant test result is obtained in the relevant gene.
73451: Tests a pregnant patient or who is planning pregnancy to identify carrier status for pathogenic or likely pathogenic variants in the following genes, for the purpose of determining reproductive risk of cystic fibrosis, spinal muscular atrophy, or fragile X syndrome: (a) CFTR; (b) SMN1; (c) FMR1. One test per lifetime.
73452: Testing of the reproductive partner of a patient who has been found to be a carrier of a pathogenic or likely pathogenic variant in the CFTR or SMN1 gene identified by testing under item 73451, for the purpose of determining the couple’s reproductive risk of cystic fibrosis or spinal muscular atrophy. One test per condition per lifetime.
continued from Page 4
“Miscarriages occur in 15-25% of all pregnancies — which is around 23 million per year, globally,” Dr Dunne said.
“Gestational diabetes and high blood pressure disorders in pregnancy can cause a variety of significant health problems; understanding the relationship between pregnancy loss and later pregnancy complications could reveal new ways to mitigate risks or possibly prevent these conditions from progressing.”
Researchers at the Fiona Wood Foundation have won Telethon 7 grants for two projects that could help them better understand the psychological and physiological aspects of burn recovery.
The first project, led by early career postdoctoral researcher Blair Johnson, will look at the long-term cardiovascular consequences of paediatric burn injuries, with an emphasis on non-severe injuries.
The second study will use MRI technology to compare the brain scans of burn-injured children with uninjured children. It is spearheaded by the senior research team and Dr Amira Allahham, along with Professor Helen Milroy and Dr Pradeep Rao, leading experts in childhood and adolescent psychiatry, with support from the WA National Imaging Facility.
Finnish brand Vuokkoset is about to release a gender-neutral tampon, For Menstruation.
It follows the launch of Tampon for Men for transgender men during last year's Transgender Awareness Week, which became a global talking point.
It highlighted the fact that menstruation can affect people who do not identify as women, such as men, non-binary or intersex people.
The company said the feedback it received suggested the need for completely gender-neutral
A doctor and nurse have been appointed to lead roles at the new Orthonova Orthopaedic Hospital to be built on the St John of God Murdoch Hospital campus by late 2026.
Dr Alex Swann will be Orthonova Commissioning Director – Medical, a part-time role on top of his existing position as Director of Anaesthetics and Pain Management at SJOG Murdoch.
Kimberley Montgomery will start as Commissioning Director – Nursing, moving from her former position at SJOG Murdoch where she is Director of Nursing, Specialist Services.
Orthonova will be the first specialist orthopaedic hospital of its kind in WA. Under a joint venture, 24 orthopaedic surgeons will join with St John of God Health Care to develop and operate the hospital.
A national stroke rehabilitation trial is seeking more participants in Perth.
WA’s Perron Institute is a partner in the UPLIFT trial which is evaluating intensive communication and combined arm training for people who have had a stroke in the past 3-24 months and are having difficulty with communication and arm movement.
These problems can persist long term for many people after experiencing a stroke and this can cause difficulties with everyday tasks such as talking, eating, dressing, bathing, shopping, texting, reading and asking for help.
University of Melbourne physiotherapist and Coordinating Principal Investigator of the trial Associate Professor Kate Hayward said it was thought that communication and arm movement shared common pathways in the brain.
The aim is to recruit up to 160 patients across sites in four Australian states.
Principal investigator and neurophysiotherapist Claire Tucak, who is based at the Perron Institute, said participants would complete some assessments before starting training to measure their current level of communication and arm function.
“Once this is determined, those with mild to moderate disability are assigned to at-home telerehabilitation training,” she said. “Volunteers with more severe limitation of communication or arm


movement as a result of a stroke have supervised, in-person training at the Perron Institute clinic.”
Several Perron physiotherapists are involved including Linh Le-Kavanagh, Tanya Smith, Taya Hamilton and Ruby Shehatha, as well as therapists coordinated by speech pathologists Associate Professor Erin Godecke and Dr Emily Brogan through Edith Cowan University.
Training sessions run for either two or four hours a day, five days a week, for four weeks.
People who are living in the community, have had a stroke within the past 3-24 months, are having trouble with communication or arm movement can email uplift-trial@unimelb.edu.au




Intimate partner violence is a pervasive issue that extends across all spectrums of gender and sexual identity. But contemporary understandings about intimate partner violence, also known as domestic or family violence, have primarily focused on cisgender heterosexual women. There is less awareness of the unique experiences of intimate partner violence in LGBTIQA+ relationships.
Examples include ‘outing’ or threatening to reveal a partner’s LGBTIQA+ identity to friends or family without their consent,
More needs to be done to address intimate partner violence in LGBTIQA+ relationships and the barriers to support, says Dr Roanna Lobo
employing homophobia, transphobia, or biphobia to exert coercive control or abuse over their partner, and exerting control over or threatening to withhold access to medication, such as HIV treatment or gender affirming treatment.
New research from Curtin University has revealed that intimate partner violence is prevalent among LGBTIQA+ individuals in WA, with one in two people having experienced intimate partner violence in their relationships. Findings also highlighted a critical need for improvements to primary care
Perth researchers have discovered that some ovarian cancer cells appear to tell the immune system to ‘stay away’ from them.
A project involving researchers from the Harry Perkins Institute of Medical Research, St John of God Subiaco Hospital, Curtin University, Clinipath, UWA and Edith Cowan University found that ovarian tumours alter their local environment by changing the sets of messages they send to cells nearby.
Using an advanced technique known as spatial transcriptomics, the team generated cellular maps of ovarian cancer samples from patients in Perth who donated their tumours for research.
This revealed that in five of the eight samples studied, subclones (tumour cells with different mutations) coexisted in the same sample.
“These can be thought of like cancer siblings, related but a bit different. This is important as some subclones can be resistant to treatment,” according to Professor
services to ensure LGBTIQA+ individuals experiencing abuse have access to more inclusive and responsive care.
The Safer Options study identified preferences for support services, obstacles to accessing appropriate help and effective pathways for assistance. It also examined the capacity and inclusivity of primary care services in WA to support LGBTIQA+ individuals experiencing intimate partner violence.
Our state-wide survey showed 68% of 523 LGBTIQA+ individuals reported experiencing abuse
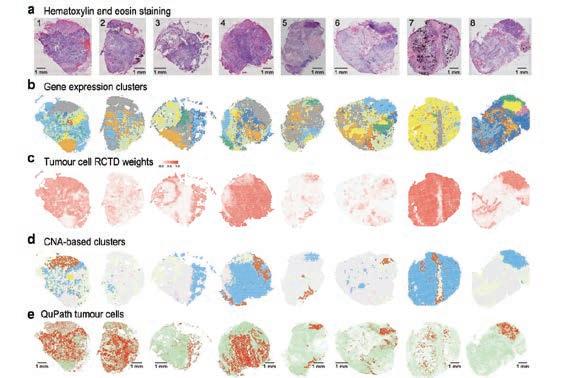
Alistair Forrest, head of the Genome Biology and Genetics program at Perkins.
By studying these subclones using spatial transcriptomics, the researchers saw that some subclones were more likely to be neighboured by immune cells while others had less. Subclones could
from an intimate partner, with emotional abuse the most common form. Some participants did not recognise that the abuse they had experienced was a form of intimate partner violence or that support may be available to them. Alarmingly, 48% of those who experienced abuse did not seek professional support because of fears of judgment and discrimination.
Medical and allied health practitioners such as GPs, psychologists and social workers are well positioned to identify at risk LGBTIQA+ individuals and to connect them with specialised services. However, LGBTIQA+ individuals reported adverse experiences within primary care services such as discrimination or rejection, typically due to problematic cisgendered and heteronormative assumptions, making it challenging to identify safe options for support.
Interviews with primary care providers revealed a lack of confidence in recognising intimate partner violence in LGBTIQA+ clients and providers expressed a desire to give better support.
Barriers to providing inclusive care were related to:
1. Heteronormative assumptions around intimate partner violence in primary care services. These cause LGBTIQA+ individuals
to conceal their identities, due to fears of exclusion or discrimination, or not being believed.
2. Knowledge gaps. Insufficient training and education about intimate partner violence in the context of LGBTIQA+ relationships, leading to ineffective service provision and potential missed opportunities to identify abuse in LGBTIQA+ relationships.
3. Greater inclusion of LGBTIQA+ experiences. Educational and awareness-raising resources should have more information about how intimate partner violence may present in LGBTIQA+ relationships, tools to recognise unhealthy and healthy relationships, an LGBTIQA+ inclusive primary care service directory with emergency contacts, and information for how primary care providers can modify their service provision to be more inclusive of LGBTIQA+ individuals experiencing IPV.
Training and education are critical to build providers’ competency in LGBTIQA+ topics, including gender identity and culturally sensitive care. More inclusive and accessible care can be achieved in multiple ways. For example, by updating administrative systems and forms, fostering stronger collaborations between researchers and practitioners, and implementing
more appropriate screening processes and trans-competent care.
The Safer Options study has laid the groundwork for tangible solutions, including the development of educational materials and clear guidelines for primary care services. Ongoing investment is required for specific workforce training, research to monitor the prevalence of intimate partner violence in LGBTIQA+ communities, and to develop and evaluate targeted solutions to respond to specific needs.
Co-design of additional resources to meet the needs of specific sub-populations is recommended including for LGBTIQA+ people with disabilities and LGBTIQA+ people living in regional and remote areas at risk of or with lived experience of intimate partner violence.
By equipping primary care providers with the necessary tools and resources, we can strive towards a healthcare system that is truly inclusive and responsive to the needs of all individuals, regardless of their sexual orientation or gender identity.
Dr Roanna Lobo, from Curtin University’s School of Population Health, is the chief investigator of the Safer Options research funded by WA Primary Health Alliance. www.saferoptions.org.au
send different protein messages to immune cells that either said ‘come here’ or ‘stay away.’
“By studying subclones in such samples it may be possible to identify new drugs that can help bring immune cells into the tumour to kill it,” Professor Forrest said.
Ovarian cancer is the eighth leading cause of cancer deaths in women worldwide. High-grade serous ovarian carcinoma (HGSOC) is the most common and lethal subtype, accounting for 70-80% of ovarian cancer deaths.
The research was funded by Cancer Council WA, the Cancer Research Trust and funds raised by participants in the Perkins’ major fundraising event, the MACA Cancer 200 Ride for Research.
products that would recognise nonbinary individuals as well. It had also received requests for other products, such as underwear liners and menstrual pads.
Existing non-invasive screening tools may miss heart failure among patients with atrial fibrillation and should be used with caution, according to the latest research.
The warning follows a University of Adelaide study looking at the effectiveness of the internationally recommended screening tools for diagnosing a specific condition called heart failure with preserved ejection fraction in AF patients.
“This is the first study to look at whether two of these noninvasive scoring systems can be used to detect this condition in AF patients,” said first author Dr Jonathan Ariyaratnam, a PostDoctoral Fellow with the Centre for Heart Rhythm Disorders.
“Diagnosing this type of heart failure in AF patients is particularly challenging because the symptoms of both conditions are very similar and can be overlooked to the detriment of the patient’s long-term treatment.”
A previous study by the Centre for Heart Rhythm Disorders used an invasive testing protocol to reveal that almost 75% of patients with symptomatic AF had features of heart failure.
A series of papers in a prominent medical journal claiming menopause is being over-medicalised has set the cat among the pigeons in one of the most debated areas of women’s health.
By Cathy O’LearyHormone replacement therapy and controversy seem to go hand in hand. HRT has been one of the most common menopause treatments for women faced with debilitating symptoms such as mood swings and hot flushes, but it has faced a bumpy road.
Back in 2002, a big US study of women triggered a huge rethink of HRT, when the Women’s Health Initiative uncovered an apparent link between the risk of breast cancer, venous thromboembolism and coronary heart disease in women taking oral oestrogen plus progestogen.
It scared off millions of women and their doctors around the world from using the pills, leading to a dramatic reduction in prescribing – and many distraught patients.
Since then, the findings have been put into perspective, with a more balanced picture of risks and benefits, encouraging many women to take up hormone therapy again.
But now, more than 20 years after the WHI furore, debate has been reignited by a series of articles in The Lancet in March suggesting the use of menopausal hormone therapy (the newer term for HRT) is overdone.
Four literature reviews and opinion pieces argue that menopause is being over-medicalised and treatment options are too simplistic and often swayed by commercial interests. The writers argue menopause is wrongly being treated
like a disease, with some women getting unnecessary treatment, and this disempowered them.
"One problem is that a normal event that affects [women] has been turned into a disease, a hormone deficiency disease, which requires diagnosis and treatment," said lead author Professor Martha Hickey, from the Department of Obstetrics and Gynaecology at the University of Melbourne.
MHT should be available for those who need it, Professor Hickey said, but it should not be seen as a "solve all" and the risks needed to be weighed against its benefits.
But not everyone has agreed with those views, sparking strong debate among some doctors who are worried the claims will further discourage women from seeking treatment and undo years of work trying to reassure women ‘they’re not going mad.’
They say it is far more likely that women with severe symptoms are not offered evidence-based treatment than for women to be overtreated, compounded by the fact that some MHT products are not PBS-listed which creates equity issues for those struggling with cost of living pressures.
Among those hitting back against The Lancet series is psychiatrist Professor Jayashri Kulkarni, director of the HER Centre at Monash University, who works at the coalface and is now questioning why women are still missing out on help.
big increase in depression, with 4-16 times increased rate between the ages of age 45 to 55, and an associated increased suicide rate.
Menopausal depression is poorly understood, under-recognised and poorly treated, she argues. And to compound the problem, antidepressants in many menopausal women are not very effective, nor are the psychotherapies.
Professor Kulkarni said there is considerable brain biology research showing the impact of fluctuating gonadal hormones changing brain chemistry and circuitry causing mental ill health.
Clinically, menopause hormone therapy is used in women with other symptoms of menopause, and not usually for menopausal depression. But in many women, it worked and improved panic, anxiety, brain fog, rage, and tearfulness.
“There is very scant understanding and recognition that menopausal mental health issues exist, and they are different to standard depression in men or even younger women,” she told Medical Forum
“That is a problem among the general community but it’s a bigger problem in the health professional community and it’s an even bigger problem in the psychiatric community.

She is calling out what she believes is a preoccupation with governments and others to do population surveys, rather than fund meaningful clinical studies that could really help women.
Professor Kulkarni spoke at a menopause summit organised by Menopause Alliance Australia in Perth in March and was recently announced winner of the Royal Australian and New Zealand College of Psychiatrists’ Ian Simpson Award for research over 30 years to improve the care for women with mental illnesses.
She says midlife women have a
“It’s been a long time of trying to campaign to even get any kind of recognition, but we’re held back by the lack of good clinical trial evidence.”
The Lancet researchers said the pendulum had swung from 'put up and shut up' about menopause to sensationalising it, and claimed the widely held belief that menopause was associated with poor mental health did not stack up.
But Professor Kulkarni says the research that is done in menopause continues to be survey-style, which is not helpful because it is difficult to pick up the exact percentage of women in the general community who experience mental health issues. The definition of it in this group is very fluctuating and unusual, and it does not meet the criteria for major depressive disorder, which all the standard tools for measuring depression use.
“So, the epidemiological surveys are
always going to have a regression to the mean, because you’ll get women who will sail through menopause and don’t even notice it, and at the other end women who are very disabled by a severe depression,” she said.
“When you’re forced to take the average, it means that most women are okay, and that’s what’s been touted and put about, and that the evidence doesn’t show any mental illness.
“But there is a significant population affected and that number varies anywhere between 20% to 60%, depending on which surveys you’re looking at.
“In clinical mode, for example for the people who work in the menopause area in London and in our work which is a mental health clinic, there is no doubt there is a different beast called menopausal depression that has different types of symptoms and presentations that can fluctuate, and have a partial response to standardised antidepressants, and unless you’re actually in the area of mental health of menopause you’re not going to be in the position to understand that.”
Professor Kulkarni said conferences like the recent one in Perth were important because there was still a group of women who had been left behind, thinking they had bipolar disorder which was the worst differential for the diagnosis for this condition.
“Or they are just left behind in the sense of ‘here’s your antidepressant, oh it doesn’t work, well sorry there’s nothing else we can do,” she said.
“That’s what we’re trying to address but then we get caught up in the weird debates about ‘stop medicalising and pathologising menopause’ – because that’s what The Lancet articles were about –they were saying ‘look most women are fine, leave them alone, so don’t make this to be a condition’ which is fine if you’re a fortunate woman who doesn’t have any symptoms.”
She said a valid analogy might be that epidemiologists were useful in developing the association between smoking and lung cancer, but it was the research that followed – the randomised clinical trials in oncology or new treatments, molecular

• Obstetric ultrasound including first trimester screening and cervical length assessment
• Gynaecological imaging
• Pelvic MRI
• Breast implant volumetric assessment, using low dose CT
• Five breast imaging clinics across the metropolitan area (North, South, East and Central) for ultimate patient convenience
• All breast imaging modalities offered including—
Digital mammography
3D mammography (tomosynthesis)
Breast MRI
• All forms of breast biopsy performed.

continued from Page 13
biology or stem cell research – that changed outcomes.
“We need to change the language somehow so that we get away from this first-base discussion that we seem to be going round and round in circles about – is there menopause depression or is there not, stop pathologising or can we use HRT,” she said.
“We’ve almost reached religious fervour at both ends, when we have groups saying under no circumstances should you pathologise, and then others saying oestrogen should be in the water supply.”
Professor Kulkarni said that while professional debate could be healthy, it was very confusing for the general community and primary health professionals to know what they were supposed to do.
“And the group who miss out are the women with severe mental illness or any incapacitating mental illness, and, okay, that’s not the general population perhaps, but it’s a proportion, and it’s not a small proportion,” she said.
“The people who are often writing these kinds of articles or involved in the research are in an epidemiological background, so they don’t take into account the clinical presentations because that’s not their work.
“And neither do they take into account the burgeoning amount of neuroscience modelling of the brain, work from animal models and also human imaging to see the impacts of what the neurosteroids do in the brain.”
Funding for randomised control trials was difficult to get because menopause depression was not welldefined and it did not have a place in the psychiatric classification books, so it did not exist.
“And because it doesn’t exist, we can’t get funding to do the trials, and then HRT or MHT don’t make it into any of the guidelines as a potential treatment,” she said.
“Then you have about 20% of women going through significant mental ill-health conditions that

don’t respond to antidepressants, or antipsychotics or whatever.
“We have to break this awful cycle at some point, and it’s like we’re trying to prove that the Earth is round, and I think we have to stop trying to do that – we’ve been there, done that –can we just get on with it, because there’s still a real proportion of women that we can’t help if we don’t change our clinical approach.”
Professor Kulkarni said she was tired of surveys that asked the wrong questions, when what was needed was a focus on the people who were unwell, physically or mentally, or both.
“We’re not in the preventative game – that’s what the WHI study was trying to do back in the early 2000s, to prevent cardiovascular disease -- but what we’re trying to do is treat an acute illness that has a different origin of causality, and that we can treat better if we tackle the origin.
“The group that I see – not the ones in The Lancet articles – are women who can’t get out of bed, who have lost their jobs because their brain fog means they are struggling with simple tasks they have done a thousand times before, and women who lose their families because their hostility, irritability and short-fuse ends up destroying their relationships.
“And there is so much economic burden by women across the community, from the factory floor to the highest paid CEOs of companies, dropping out of the workforce because of brain fog and anxiety primarily, with depressions secondary.”
Professor Kulkarni said effective
treatments should be readily available for the women who are struggling while “we can leave the rest alone who are fine and can get on with it.”
“And with the question of how you define this group – well they define themselves, and we shouldn’t be saying to them ‘you’re a drama queen.’
“Instead, we need to say here’s a palette of treatments that we have available, and we’ll tell you the benefits and side effects, and you decide what you want.”
There has been some progress in the menopause space in the past year, as groups agitate for action. The Commonwealth’s Senate Standing Committees on Community Affairs is due to report back in September on its inquiry into menopause and perimenopause.
In its submission, the Australian Medical Association said GPs played a central role in helping women to make informed decisions about their healthcare and were also the first port of call for 90% of people with mental health issues.
The AMA argued that while for some women the transition to menopause could be uneventful, for others it was vastly different, with them suffering from prolonged and severe symptoms.
Hot flushes, insomnia, anxiety and depression, fatigue, irritability, muscle aches and pains, vaginal dryness and low libido were just some of the symptoms well documented as long-term risks.
Professor Kulkarni said she wanted targeted research to run clinical trials of antidepressants versus MHT, to get some evidence and change the treatment approach for menopausal depression.
“Of course everyone should be a certain healthy weight, eat well and exercise – they’re good health strategies for everything –but they’re not going to prevent menopause,” she said.
“We’re dealing with an important group of women, and it’s not small. And we need to be careful that we’re not invalidating them with articles that suggest that everyone should just deal with menopause by not being too dramatic.”

Dr Rosalie Schultz works in communities in the vast region where WA meets the Northern Territory and South Australia, looking after the health of Aboriginal people in the Ngaanyatjarra lands.
By Ara JansenA UWA medicine graduate, Rosalie says she didn’t think too hard about what her career would be, just that when you got high marks at school, medicine was the thing you did. Her parents were academics. Rosalie’s mum started her law degree the year her youngest sibling started school, with the goal of protecting our forests. Her dad Phill is a lecturer in maths, who at 90 is still a professor at UWA and has been for almost 54 years.
A UWA medicine graduate, Rosalie says she didn’t think too hard about what her career would be, just that when you got high marks at school, medicine was the thing you did. Her parents were academics. Rosalie’s mum started her law degree the year her youngest sibling started school, with the goal of protecting our forests. Her dad Phill is a lecturer in maths, who at 90 is still a professor at UWA and has been for almost 54 years.

“Mum was in her 40s and I just saw her doing a law degree, but I had no idea how hard it was to study at university,” says Rosalie. “She already had a PhD in romance languages. She definitely showed us a commitment to learning.”
After university, Rosalie did her internship at Fremantle Hospital, knowing she wanted to work overseas but lacked experience. Instead, she found herself in Darwin and then worked throughout regional Northern Territory. To sate her desire for overseas work, she did a two-year placement in the Solomon Islands, a brief stint in East Timor and six weeks working in the Ebola response in Sierra Leone in West Africa.
Now Rosalie and her husband live in Alice Springs, where they have been since 2004. She’s the senior medical officer at the Ngaanyatjarra Health Service, an Aboriginal communitycontrolled health service which sits in remote WA, near the NT and SA borders.
Rosalie met her Adelaide-trained husband Dr Nick Tyllis (an emergency doctor at Alice Springs Hospital) during her work and travel in the NT and dragged him along on the Solomon Island placement in 2002.
“He didn’t care one way or another where we went, but I really wanted to work overseas. So early on in our relationship it was quite an experience. But thankfully it only strengthened it. We were the only doctors, and we ran a little hospital which serviced a collection of islands. It’s a bit like what I do now, supporting nurses as the lead healthcare professionals and visiting remote communities via road or air.
“One of the things I learnt in Solomon Islands was the high quality of care that can be provided by nurse-led services. Through best practice guidelines, strong community relationships and solid external support when needed, I believe healthcare in remote regions can be as high or higher standard than in urban regions, where services must compete with one another and have no formal responsibility to their communities.
“Nurses provide the vast bulk of care in Ngaanyatjarra health, while through telephone and video consults, GPs, emergency physicians and other specialists are available.”

Rosalie’s job isn’t that of a classic rural GP as she acts much more as a guide to the nurses in the group, rather than doing a lot of the handson work herself. She says one of the biggest issues they face is the small numbers of Aboriginal health workers and nurses but equally she encourages anyone with the passion and curiosity to come and experience the truly unique opportunity to work in Aboriginal communities.
“I learn so much working in Aboriginal communities, which is probably why I have done it for the last 25 years.” She can’t see herself working anywhere but in remote Australia.
A nominee for GP of the year at the 2024 Rural Health Excellence Awards, Rosalie loves working in primary healthcare. “You never know what the day will bring, what you will need to do, who you’ll need to see or where you might have to go. In primary care, we see people of all ages who present with any issue. There’s always something we can do to support and improve health and wellbeing.”
Rosalie’s work includes medical leadership and administration from Alice Springs and regular travel to the communities in the Ngaanyatjarra region, such as Warburton, Warakurna, Wingellina, Blackstone/Papulankutja, Jameson/ Mantamaru and Kiwirrkurra. The Ngaanyatjarra lands cover approximately 250,000km2 across the Great Victoria and Gibson Deserts, with a population of about 2000 people. The communities
are about mid-way between the regional centres of Kalgoorlie and Alice Springs, 800km to west and east respectively, with Kalgoorlie the referral hospital for the region.
In 2019, Rosalie finished a PhD in how services can promote Aboriginal wellbeing and health. “It’s about how culture is such a strong determinant of wellbeing with Aboriginal people. Healthcare services can get in the way of wellbeing and in Indigenous cultures we need to support both.
“Many Aboriginal people are strongly attached to land, culture and family, and our healthcare and medicine needs to work with all those elements. I wanted to explore climate change as an issue, but people felt that other concerns are much more pressing. Much more work to address the changing climate and its impact on people’s health is urgently needed.
“We provide care for people who may have suffered losses, grief and sadness. There’s great care needed in talking to people who may have been recently bereaved. Many Aboriginal community people travel widely and may need to be a long way away for sorry business. We have to work with their needs, not against them.
“I am so privileged to learn about people and their lives. We need to understand their needs and provide a service that meets their needs, not the service we think they want. Our role is to provide care, not tell people what to do.

Whatever your next steps as an independent practitioner, Avant is here to support you. And with $5,000 to be won, you could get a financial head start to help build your future.

continued from Page 17
“Everybody should be well, and I have this focus on wellness, and people being as well as they can be, even when they’ve got sickness. I’m interested in making things better for people who have not had the privileges I have had.”
After all this time spent in remote areas, Rosalie reckons she’s incapable of dressing up, which explains why she could never again work in a city. Most of the week her dress code is a polo shirt, shorts and closed-in sandals.
Among a small local medical community, the bonus of having a doctor for a spouse is that if there’s an incident or unexpected outcome, there’s someone who understands deeply to debrief with.
Rosalie and Nick also share a love for nature and hiking and have explored plenty of the West MacDonnell Ranges (Tjoritja) just outside Alice Springs. Those walks might last a
few hours or several days, as they camp under the stars.
They particularly like seeing Aboriginal art sites and local waterholes but are highly conscious of the sacredness of both. No photos are shared and most of the waterholes are too precious to swim in. They make an effort to get cultural information about the places they plan to visit. Because they like to head off the beaten track, they are rarely besieged by noisy tourists and often don’t see another soul.
In Alice Springs the pair travel by bike. This saves travel time, as nothing is more than a half hour pedal. Even in the heat of summer, cycling works where there is a cool building at the end of the trip. While Alice is no shopping mecca, there’s enough for what’s needed and Rosalie says the Araluen Cultural Precinct offers arty engagement and includes galleries, a theatre, aviation museum, public art and Arrernte sacred sites. They’ve seen the Australian Ballet and Paul Kelly
among other visiting national and international performers.
“I love knowing every nook and cranny of my hometown,” she says with affection. “There’s a beautiful public pool I swim in every morning. Then I’ll ride to work, along the (usually) dry riverbed and I might see some wallabies. I love being close to nature – there’s birds, lizards and snakes to see.”
Rosalie and Nick also travel further afield to hike, their adventures including the Bibbulmun Track, the 1200km of the Heysen Trail in South Australia, the Great North Walk (250 km from Sydney to Newcastle) and Queensland’s week-long Great Carnarvon Gorge Walk.
Cutting back on alcohol is a no-brainer according to a global review of the latest evidence about the health effects.
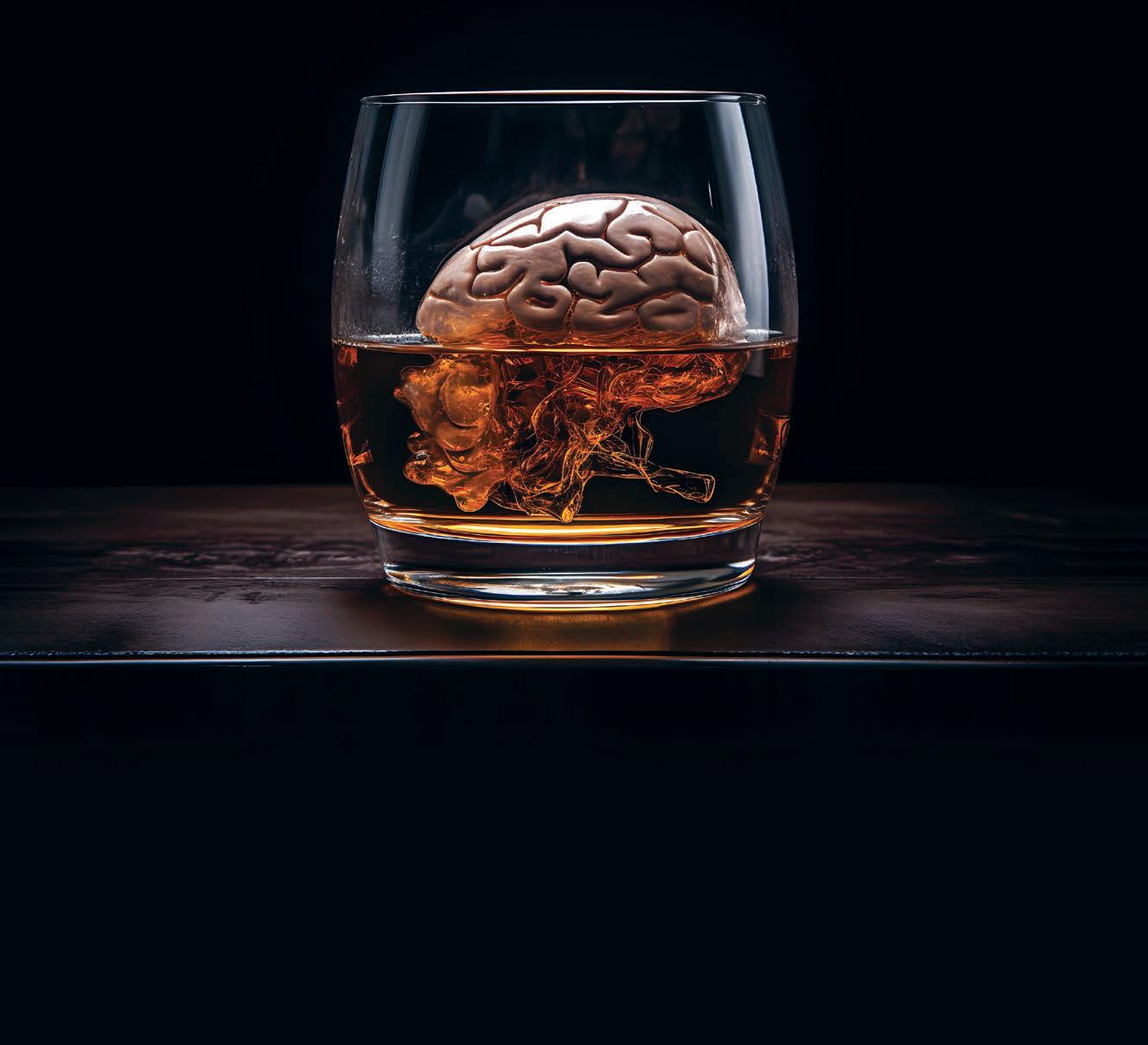
Times have changed since the prevailing thought that drinking red wine was good for you, especially for the heart. Now the most credible evidence about the effects of alcohol leans heavily in favour of harm rather than benefits.
One of the latest studies – a global review including Perth input –paints a sobering picture of the impact of alcohol on the brain – and not just for big drinkers.
Published by the group Alcohol and Society, the report is the 10th written by a group of international researchers initiated by several Nordic voluntary and academic organisations.
Alcohol and the Brain looks at
By Cathy O’Learyimpacts on neurological, cognitive and psychological health across the life course, with researchers weeding out unreliable studies that in the past have been used to prop up the ‘alcohol is good for you’ message.
Their overall finding is blunt – reducing or eliminating alcohol consumption is arguably the most important modifiable way to promote cognitive and neurological health.

That is because ethanol, the active ingredient in alcohol, has more negative impacts on the human brain than perhaps any other chemical originating outside
the human body. It affects most structures within the brain and causes many types of short and long-term impairments.
Professor Tanya Chikritzhs , who leads the Alcohol Policy Research team at the National Drug Research Institute at Curtin University, joined experts based in Sweden, the US and Canada for a deep dive into the effects of alcohol on the brain, including dementia risk.
Their report was recently released in the European Parliament and underlines the brain health benefits from avoiding alcohol. This applies to both occasional drinking, as
well as to intensive or regular consumption over time.
Professor Chikritzhs has been working in the field for decades, and has seen alcohol go the full circle, from when it was widely considered ‘good for you’ to it being potentially beneficial in small or moderate amounts, to now.
“In this most recent review, we did a broad sweep of the literature, to identify the most recent systematic reviews and meta-analyses and through our own knowledge we know the biggest-hitting ones,” she said.
“And then we looked for quality, so we could keep an eye out for all the problems with the alcohol literature that can lead to erroneous conclusions, like protective effects.
“This latest study is a real neat one, because it brings in some of the past reports we’ve done on things like blood pressure, and it looks at why alcohol might be causal for dementia. There are many pathways, but one of them is blood pressure, and we know alcohol, even a low dose of 1-2 drinks, can raise blood pressure which is a wellestablished risk factor for dementia, stroke and so on.
“In the short-term, even low doses have effects, but as your use increases, so do the risks of injuring yourself. That’s why alcohol a risk factor for falls, because it has a direct impact on the cerebellum, which is necessary for a balance, but it also affects other functions.”
Professor Chikritzhs said that young people tended to binge drink, so they dominated the injury statistics related to alcohol.
When a young person drank more frequently and their consumption increased, that could set them up for developing dependence.
“But it also affects parts of the brain like the hippocampus, which is responsible for memory and emotion, and if you’re a regular, heavy binge drinker and you do that for the first few decades of your life, that’s not going to be unfelt as you get older.
“When you’re younger you have more powers of regeneration and coping, but as you get older a lot of that falls away. So, it’s not surprising that we have studies that show that being a heavy drinker even as young as late adolescence,
can then reveal itself in alcoholrelated brain injury, which is often diagnosed as early-onset dementia, and then later as dementia.”
Professor Chikritzhs said alcoholrelated brain injury was still not well-diagnosed, but in people with early-onset dementia, a great proportion were related to injury caused by excessive alcohol consumption.
A Norwegian study using 500,000 male conscripts found that a young male who at the age of 18 had been hospitalised for alcohol poisoning or passing out was five times more likely to develop early-onset dementia by the time they were in their 40s. If being in the lower-third for cognitive function was added in, they were 14 times more likely to get early-onset dementia.
“And people with early-onset dementia often escape detection because you work ways around it,” Professor Chikritzhs said. “If you add a third factor – high blood pressure – the risk was over 20 times greater.”
A large UK study in 2022 which used MRI scans on over 36,000 healthy brains in middle-age showed that even consumption as low as eight grams a day – less than an Australian standard drink – created measurable reductions in brain volume throughout the entire brain.
“So that’s grey matter and white matter. And the greater you drank, the greater the reduction in brain volume. Whether that was having a measurable effect on performance or memory, they can’t say from that study, but they can say that even low levels of consumption affect brain structure.”
So where does that leave current recommendations on safe drinking levels?
National Health and Medical Research Council guidelines advise having no more than four drinks a day, or 10 a week, and state that if you stay within the limits, you have less than a 1% chance of dying from an alcohol-related disorder.
But Professor Chikritzhs said science was never static. NHMRC guidelines from 20 years ago, based on the literature at the time, advised a maximum 28 drinks a week for men, and 14 for women.
“We published in The Lancet a few years ago a study which showed that drinking above 168g a week – so about 17 standard drinks –increased your risk of any type of dementia (not just early-onset but also things like Alzheimer’s) by about 20%. It doesn’t sound large, but the risk increases very swiftly and exponentially with increased use.
“So, if men were told 20 years ago that they could have 28 drinks a week, then they would have quite easily crossed that threshold, and those men are now in their 60s.
“With the most recent NHMRC guidelines – maybe the four drinks a time needs to be looked at – but there is also a line in there to the effect that if you want no risk, it’s better not to drink at all.
“But how far can you push it before people say it is just ridiculous.”
Professor Chikritzhs said that while young people heard the newer advice about limiting intake, older people had grown up with more generous messages.
“If you want to address alcohol problems in older age you have to start middle-age or younger,” she said. “It’s too late to wait till someone is in their 60s because the damage is done, and they have far less regenerative power.
“And while you have risks from alcohol on young developing brains, it then takes more alcohol to damage a brain that is fully developed in middle-aged, but then in older age you’re more vulnerable again.”
She said alcohol use was sometimes a difficult and avoided conversation between doctor and patient. A colleague of hers had been trying to get health professionals to answer a questionnaire about their awareness of the effects of alcohol on older bodies, and the contraindications. They contacted GPs, occupational therapists and physiotherapists who dealt with older people but could not get them to answer the survey.
“Doctors drink, and we’ve known for a long time that doctors, and not just in Australia, are quite happy to ask patients about their smoking but not about their alcohol use,” Professor Chikritzhs said.
“We also know there is interaction too between alcohol and medications, but a lot of people aren’t told this.”
There are 46,000 people in Australia living with a stoma and many of them struggle to live freely without shame. The WA Ostomy Association wants to change that.By Eric Martin
One of the procedures that many people, including doctors, shy away from is the thought of completely losing the ability to go to the bathroom normally.
The thought of having to use a bag, strapped to their abdomen, to collect their waste can jolt potential patients into shock or dismay.
The creation of a surgically formed fistula, be it a colostomy, an ileostomy or urostomy, brings a range of issues to the surface, not just for the practical operation and maintenance of the stoma and appropriate bag but also psychologically. And in a huge State like WA, managing those impacts can be especially challenging.
Medical Forum spoke with stomal therapy nurse (STN) Tania Norman from the WA Ostomy Association, one of 26 specialist nurses who assist some 4000 ostomates across WA about the obstacles many people still face trying to arrange appropriate care for a procedure that was first performed in 1776.
“Stoma surgery is a life-changing event, and even though patients can live an otherwise normal life thanks to modern advances in care, they still need to make significant adjustments to their lives,” Ms Norman explained.
“A stoma nurse is pivotal in the preparation prior to surgery: people need to be shown what the bags are like, what their stoma could potentially look like, what they could expect after the operation, and most importantly, how they can manage it after returning home.
“The nurses in the hospital will follow patients up post-surgery to check that everything is healing and then choose the right bag for them to wear. If you don't have the right fitting bag, then leakage can occur, and you can imagine the effect that has. Some people won’t leave their house because they're worried it could happen.
“Not only is that horrendous for their quality of life, but it also impacts their skin, which breaks down very quickly under those conditions. Trying to get anything to stick on it is almost impossible, which starts a vicious cycle if there is not intervention.
“Patients’ mental health can really suffer, and the post-traumatic stress is often particularly pronounced for younger people.”
So, situating the stoma appropriately for the ostomate’s needs is important. Putting it in a position where that person can see it away from any creases or folds in the abdomen, or scar tissue that might interfere with the bags sticking properly.
Ms Norman pointed out that lifestyle factors were the other important consideration when working out the best location for a stoma, including recreational activities such as sport and more private pastimes such as sex.
“There are many things that STNs take into consideration when placing the mark for a stoma on their patient and, basically, we say that you should be able to do anything with it. You can take your bag off, you can shower with your bag off, swim with the bag on, you can jump out of planes – you can do all those things if the underlying reason why you've had a stoma isn't impacting the rest of your life.
“But those who have emergency

surgery and the surgeon's not familiar with those factors, it frequently becomes problematic for the ostomate.”
Ms Norman said for people in regional centres, it was often an emergency procedure, with little or no warning for the patient. A fact further complicated by the lack of any STNs employed north of Geraldton.
“These are often among the most impacting procedures for ostomates. Yet we have over 1000 members who do not have direct access to the support of a STN. To address this issue, I run a stomal therapy clinic at the association and travel across the State running stoma clinics and providing education sessions to health professionals.”
And during her travels, she regularly encounters what would normally be considered outlandish breaches of patient care in a metropolitan setting.
“For example, there is an awful story from the Pilbara of a lady who had to go in for emergency surgery who woke up with a bag, no stoma nurse onsite to prepare her as to what to expect afterwards and, because it was the weekend, she was discharged with three hospital bags to wash out and a phone number of the stoma nurse at Royal Perth Hospital, which she couldn't do until the following Tuesday.
“She taught herself how to change her bags by watching YouTube,
which while great, is also absolutely horrendous in terms of outpatient care. I met her again some years after and luckily, she was able to have her stoma reversed, but she was still suffering post-traumatic stress from her ordeal.
“Kalgoorlie's another centre where it’s been historically challenging for ostomates. Last year, there were six new stoma procedures performed, with no stoma nurse to support them. Kalgoorlie is a major regional hub – we've got nearly 45 ostomates in total living in that region.”
Ms Norman has been traveling to Kalgoorlie annually for eight years to run the stomal therapy clinic and was thrilled that there were now two nurses at the local hospital that had completed the course – and were planning on staying in the region.
“If there is someone that has to have that surgery, then that care can be provided as part of the outpatients services,” she said.
“But otherwise, if you are in a smaller regional community, the expectation is that ostomates fly to Perth and ideally stay for a good six months while they are going through the introduction to care, training, checkups, and refits, as well as undergoing monitoring for complications, which are most likely to occur 2-3 months after surgery.
“But as you can imagine, most ostomates don't stay that long. You
continued on Page 25

continued from Page 23
are taking them away from their family and everyone else in their support network.”
Ms Norman explained that even though some hospitals, such as RPH, could provide telehealth services for ostomates living in areas north of Perth, it was not on par with the hands-on care that ostomates could get with regular follow-up in the city.
“We have over 2,500 different products to choose from, and we are incredibly fortunate in Australia that they are government funded. But if you are not given the correct product in that first instance, then you're already behind the eight ball, and as most people require a stoma over a relatively long period of time, the requirements for the bag can also change,” she said.
“That's why we recommend regular reviews at two weeks post-surgery, 6-8 weeks, 12 weeks and then at six months until the end of the first year. Following that, we recommend a review every 1-2 years, because if you put on or lose weight, your stoma changes shape and will need refitting.
“Similarly, if you develop a hernia, which unfortunately is a common complication, then the stoma changes again. There are things that can happen that people, and many doctors, are not fully aware of.”
Ms Norman explained that providing stoma services in the bush was also potentially more challenging given the tough rural mentality that exists in the regions.
“The rural mentality is that ‘Well, we don't have access to these facilities – this is what we've got, and this is what we put up with.’ They are much less likely to go to a doctor or to approach a nurse, or to reach out,” she said.
“When I started doing these rural trips, I met a gentleman in Carnarvon, who’d had his urostomy for six years and every night since had wet the bed. He hadn't thought to reach out to anybody. When I reviewed him and put him on a different bag, he had his first dry night in six years – and has been dry ever since.”

The other issue that Ms Norman highlighted was that many GPs were unfamiliar with stomas and were hesitant to advise because they don't know what to do with it.
“It is still a taboo subject. I have worked in breast cancer nursing, and everyone will talk about breast cancer, but even though we tell our stoma patients that there is no reason why they cannot live a normal life, people will still dramatically change their lives because they don't want others to know that they have a stoma.
“And, unfortunately, that stigma has partially transferred to the medical profession in terms of service provision.
“If patients are going back to their surgeon for review and they happen to mention that they have a problem with their stoma, they will often be told to contact the STN.”
The WA Ostomy Association is negotiating to offer specific training for GPs on stoma care and has made inroads on addressing the initial stigma by making presentations to medical student studying at Curtin University and UWA.
“We’re hosting third-year medical students here at the association and are able to discuss stoma care right at the start of their education. I can be very hit and miss during the doctors’ hospital training, whether they actually see a stoma
formed or deal with an ostomate. We would like to see it incorporated into the actual program and then be offered as CPD points as well.
“It’s important to realise there are several reasons why a patient might need a stoma, such as cancer, inflammatory bowel disease and Crohn’s. We have had people who've been sick for years with Crohn's disease and have put up with it because to them, they would rather die than have a stoma.
“But once the procedure is done –because they have no choice – they say they wish they’d had it done years ago, because suddenly, they feel well again.
“Embracing your stoma does help people to deal with it psychologically and we now have ostomates, including weightlifters and even women in bikinis, willing to take their bag off and talk positively about it to help raise general awareness.
“But then there are also those people where their best friend of 50 years doesn't even know they have had a stoma for the past 20.
“No one talks about it, even though nationally there's 46,000 people with stomas. There are more than a million ostomates in America, it is not something that just happens sporadically.
“The lack of knowledge is quite apparent and that must change.”
The time for head scratching is coming to an end as major WA health providers sign up for a digital revolution.
Government and private West Australian healthcare providers are taking the leap to modernise their digital systems in a bid for greater efficiency as well as safety.
The WA Country Health Service (WACHS) has joined the South Metropolitan Health Network and St John of God Subiaco in adopting the Charm Evolution laboratory information management system (LIMS), which allows clinicians remote access and streamlines clerical tasks.
This software recently became the first oncology system to integrate with My Health Record.
 By Eric Martin
By Eric Martin
The digital push is being led by health tech companies Citadel Health, Wellbeing Software and Genie Solutions that consolidated operations across Australia and the UK under the new brand, Magentus.
Magentus advisory board member David Wells says LIMS is at the forefront of large-scale improvements to workflow and patient care across disparate disciplines and vast geographies.
“Innovative diagnosticians are collaborating with clinicians beyond traditional organisational silos throughout labs, hospitals, and trusts to deliver a higher quality of
care that is increasingly integrated and multidisciplinary,” he said.
“Our most advanced pathology and radiology networks are also successfully incorporating the fast-growing plethora of clinical AI apps, giving greater access to more predictive analytics and putting more personalised care within reach.”
For SJOG Subiaco, Evolution’s centralised oncology patient record combined treatment plans with appointment scheduling, simplified reporting for all outpatient consultations and same-day and overnight inpatient services
and provided oversight of all prescriptions and treatments.
WACHS believes the LIMS will help deliver safer cancer services for patients across an area spanning more than 2.5 million square kilometres.
“To truly move diagnostics forward, we must accelerate the adoption of scalable data and interoperability standards,” Mr Wells said.
“The evolving virtual lab management across all patient settings can accelerate diagnosis, reduce the need for intervention, and keep more people healthy in the long run.
“Beyond this, plugging a clinical AI into this process could identify correlations of concern between image reporting and test results, helping clinicians optimise treatment plans based on similar patient cohorts.”
However, while the LIMS address the clinical and managerial aspects of healthcare operations, the lynchpin of the campaign in WA (and the rest of Australia) is likely to depend on the effectiveness of the end user application designed for consumers.
The results of the latest Australian digital review last year found that globally, “easier digital patient navigation was strongly linked to increased and successful rates of screening, earlier medical diagnosis, and cancer outcomes worldwide,” and lead author, Professor Raymond Chan, Director of the Caring Futures Institute and Dean of Research (Nursing and Health Sciences) at Flinders University, has called for cancer patient programs, including navigators and digital tools, to be funded through the health system.
navigation improves quality of life and patient satisfaction with care in the survivorship phase and may reduce hospital re-admission.”
Professor Chan explained that barriers included lack of health and system knowledge, lack of financial resources or health insurance coverage, geographic distances from care providers, and lack of social support – which describes the situation faced by many WACHS patients.
For regional West Australians, the design and implementation of the patient interface has the potential to ‘make or break’ the system.
The State Government appointed the Atos Group to provide a scalable Hybrid Cloud to speed up the deployment of these digital services and manage the public interface architecture, which will be built with technology supplied by Dell/EMC, VMware and ServiceNow.
Atos was selected as one of three strategic partners under a five-year agreement to deliver the government’s GovNext-ICT Program, which endeavours to use the maturing capability of the private sector to provide flexible Cloud-based Computer/Storage, Network and Communications infrastructure services to all government agencies.

The aim is for a more governed and coordinated approach to ICT utilisation, procurement, and delivery, and to make high quality services available throughout WA.
However, phone and internet issues often experienced in the regions, is a considerable barrier.
compared to 9.4% of the Australian population.
With residents in remote communities typically on low incomes, 84% of these respondents with access to a mobile shared it with others, 94% of these used pre-paid services, and 53.3% said they had sacrificed paying for essentials such as food or bills to stay connected, compared to 19.1% of other Australians.
“It’s clear that First Nations people, and those from the culturally and linguistically diverse populations and rural and remote areas have worse cancer outcomes and experiences,” Professor Chan said.
“This challenge can begin even before the cancer diagnosis, during screening and early detection, at the time of diagnosis, and continue throughout treatment, follow-up care, survivorship, and palliative care and end-of-life care.”
Boston University and the American Medical Association have described digital access as one of the key invisible structural determinants of health.
“Disparities in digital access contribute to inequitable access to health information and inefficient patient-clinician communication, delaying timely delivery of relevant health communication, appointment reminders, and followup care,” the statement said.
Mr Wells explained that these digital health tools supported clinicians with insights drawn from historical and real-time patient data, accelerated diagnosis and reduced the need for intervention.
"Our research (published in CA: A Cancer Journal for Clinicians) shows that patient navigation is clearly improving participation in cancer screening for breast, cervical, colorectal, and lung cancer and reducing times from screening to diagnosis, and diagnosis to starting treatment,” he said.
“Navigating the healthcare system as a cancer patient can be an overwhelming experience…but the evidence suggests good patient
RMIT-led research published September last year highlighted the significant gap in digital inclusion for First Nations people compared with other Australians, which widened substantially with remoteness.
They found that about 43% of the 1,545 First Nations communities and homelands across Australia had no mobile service – including some with only a shared public phone or no telecommunications access – meaning that 45.9% of remote First Nations research participants were ‘highly excluded,’
“More accurate and integrated diagnostics could serve as an early alarm for future pandemics or help uncover previously unknown genetic links to chronic conditions. Interconnecting wearable technology, mobile apps, or home cameras could even help predict mental health issues or the potential for falls based upon movement, gait analysis, or other indicators,” he said.
“The richness of data collected and analysed would mean any change in patient pathways could be quickly identified and the most appropriate treatments and actions implemented.”


Dr Gayatri Borude
Fertility Specialist - Clinical Director
MBBS, MD, DNB, FRANZCOG, M Rep Med

Dr Mahalakshmi Ragunath
Fertility Specialist
MBBS, DGO, MRCOG, MSc, FRCOG, FRANZCOG

Dr Shanthi Srinivasan
Fertility Specialist
MBBS, MD, DNB, FNB (Rep Medicine), FRANZCOG
Adora Fertility provides affordable IVF without compromising on quality. By referring your patient to one of our highly qualified specialists, they will receive a tailored approach to their fertility treatment plans with medications sensitive to their needs. Out-of-pocket costs are typically less than $2,000 for a fully stimulated IVF cycle. Give your patients the best chance of conception without the financial sacrifice.
Our range of fertility treatment options has expanded to include our newly launched Known Donor Program. As part of this program, patients can access affordable fertility treatment with donated sperm, eggs or embryos from a donor known to the patient. By facilitating sperm, egg and embryo donation in this way, we know that we can help more people grow their families in more ways.
continued from Page 27

RMIT’s Digital Health Hub Director, Professor Kerryn Butler-Henderson, explained that from the humble pedometer to smartwatches that warned of heart problems, many Australians have been using digital technology to help make health decisions for decades.
“But despite its enormous potential in addressing healthcare challenges, an accessible overview of people’s understanding of health information and digital health tools has been lacking,” she said.
“Health literacy is about having the ability and skill to obtain, comprehend, evaluate, and utilise trusted health and wellbeing related information, so people can play a greater role in their own care.”
According to the CSIRO, these digital literacy issues, if left
Ramsay
unaddressed, can lead to longterm digital disadvantages for families and communities.
“Having little or no access leads to reduced familiarity with digital technology, which then erodes confidence, fuels disengagement, and ultimately sets in motion an intrinsic sense of not being ‘digitally capable,’” the CSIRO’s Dr Sarah Bentley and Dr Claire Naughtin said.
“And as AI tools increasingly reshape our workplaces, classrooms and everyday lives, there is a risk AI could deepen, rather than narrow, the digital divide.”
For those living in metropolitan areas, “digital technology could potentially contribute to an enhanced standard of healthcare, empowering individuals to manage their well-being more proactively with greater ease and accuracy,”
Professor Butler-Henderson said. While for those in the bush, the breakthrough could just as easily be considered a utopian work of science-fiction.
“Yet with a better understanding of digital literacy levels, work to improve these [digital health tools] can be better targeted towards the often-marginalised groups who need it most.”
Her team of researchers from RMIT have been part of an international body developing The Global Atlas of Literacies for Health (GALH), one of the first online tools displaying interactive data visualising levels of health literacy and digital health literacy from evidence-based studies conducted with patients and health professionals across Europe.
“The atlas makes health and digital health literacy evidence visible to the public, government, health organisations, policy makers and educators… and will become a critical tool in literacy reform,” she said.
Ramsay Clinic Hollywood provides specialised inpatient and day patient services for patients struggling with eating disorders. Treatment comprises a mix of psychiatric interventions, psychological care, nutritional support and peer worker involvement.
• GP-referred (patient does not need own psychiatrist prior to admission)
• Patients are assessed prior to admission for the Day Program and admitted under the Consultant Psychiatrist, Dr Richard Clarke
• Inpatient Program Consultant Psychiatrist
– Dr Leighton Chadwick
• Patients can enter the Day Program at any time
• An onsite support group is also available

Further information is available on the Ramsay Clinic Hollywood web site (see ‘For Doctors’ pages) or by contacting Wendy Henson E: hensonw@ramsayhealth.com.au
M: 0417 404 776
Referral:

Scan to learn more
• A Best Practice template or writable pdf referral is available
• Email to: rchbookings.hph@ramsayhealth.com.au
• Phone 9346 6850 to discuss pre-admission tests that may be required
Note: Private health insurance, DVA cover or self-funding required
35 years!

Opened first BreastScreen WA clinic in Cannington.

BreastScreen WA is mobile! By 1995 there are 4 mobile units travelling around WA.
BreastScreen WA extends North by welcoming a Mirrabooka clinic.
Service continues to expand with a Midland clinic.
Perth City clinic opens and BreastScreen WA becomes first state service to go statewide.
BreastScreen WA achieves full accreditation with BreastScreen Australia.

Launch of website.
BreastScreen WA
Consumer Reference Group is formed.
Cannington clinic relocates.
One million screens!
Online bookings, new website and social media is launched. Cockburn clinic opens. 2015
Wanneroo clinic opens. New breast assessment centre at Fiona Stanley Hospital.
2016

Mandurah clinic opens. Introduction of electronic GP notifications.
2017

performs its 2 millionth screen!
Assessment comes under the BreastScreen WA umbrella - Sir Charles Gairdner and Royal Perth Hospitals. GP Advisory committee is convened.
“Screening Saves Lives” partnership with National Cervical and Bowel Screening Programs to promote screening in the LGBTQIA+ community. 1990
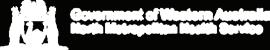
Padbury clinic opens.

The digital revolution begins.
New mobile screening units are launched.
David Jones Rose Clinic opens in Perth City store. Health Promotion team can make opportunistic bookings at events.
A secure client result portal is launched.
2020
COVID-19 Pandemic causes 2 month suspension of services. Clients can now receive

East Perth- Mardalup Clinic opens, first to be Aboriginal co-named.

screening units are launched.

New screening and assessment centre opened in Joondalup. clinic reopens after a


New guidelines for concussion management in community and youth sport provide a realistic guide, according to Curtin University expert Dr Sarah Hellewell, PhD.
The Australian Institute of Sport and the Australian Sports Commission have recently released the Concussion and Brain Health Position Statement, which provides a unified framework for managing concussion and return to play for community and youth athletes across different sports. Unlike professional-level athletes, there have not previously been clear guidelines for how concussion should be handled when it occurs in community sport, or when it is safe for athletes to return to training and contact sports.
This has made it difficult for patients, medical professionals, parents, schools and sports clubs to make informed decisions about concussion management and recovery.
These new guidelines integrate the latest scientific evidence on recovery trajectories to place community and youth athletes on a clear plan for return to competitive sports.
This advice has changed over time from the original concept of concussion recovery, which stipulated that a person should rest in a darkened room until their symptoms resolve. Increasing evidence suggests that those who rest for longer report more symptoms and recover more slowly, whereas early resumption of daily living activities is associated with more rapid symptom resolution and shorter recovery.
Similarly, early light physical activity has been shown to speed recovery. A graded approach to return to work or school is also recommended, with concessions made as needed e.g. working from home, reduced hours.
The Sport Concussion Office Assessment Tool-6 (SCOAT-6)
helps health care professionals to evaluate concussion in a controlled office environment, recommended for administration within 3-4 days of sports-related concussion. The SCOAT-6 evaluates symptoms and past medical history of relevance, includes tests for cognition and physical presentation (e.g. cervical spine, gait, vestibular function) and assists practitioners in providing advice on return to school, work and sports play.
Training & competition
The guidelines recommend that non-contact cardiovascular training exercises can be commenced and gradually increased in intensity if they do not exacerbate or bring on an athlete’s symptoms. Athletes should only commence resistance training once head movement activities are tolerated. A minimum of 14 days without symptoms is stipulated before returning to full contact training.
It is now established that symptomatic recovery precedes brain recovery, though the trajectories are likely highly individual. A prolonged recovery is more likely if the athlete returns to sport too early and makes the injured brain more susceptible to another concussion.
While we lack tools to examine brain recovery in detail, this guideline allows additional time for the brain to heal before resuming contact training. Similarly, a player is now recommended to be at least 21 days post-concussion before they return to competitive sport.
This recommendation aims to ensure that a player has sufficient time to recover and demonstrate clear capacity to perform normal activities of daily living, has returned fully to work or schooling, and can exercise at full capacity without exacerbation of symptoms before they return to the playing field.

This mandatory stand-down time away from competition attempts to strike a balance between allowing the brain sufficient time for recovery without being punitive to players and disincentivising them from reporting concussions and following the guidelines.
The guidelines also recommend the nomination of a ‘concussion officer’ for sports clubs and schools. This officer is envisaged as a single point of contact for information and coordination of response to concussion. This officer is not expected to be a medical professional nor expert on concussion; rather, they would act similarly to a fire warden to coordinate response to concussion and ensure that anyone diagnosed with concussion follows organisational protocols.
The AFL has instituted these guidelines for community and youth sports clubs falling under their purview, though they have chosen to retain their 12-day return to play concussion policy for AFL and AFLW players, with the rationale that elite-level players receive close medical supervision in their recovery.
These guidelines are not binding for the West Australian Football League, so it will be up to individual clubs as to whether they choose to implement them. However, the guidelines provide a realistic, step-wise framework for activity resumption, which is likely to be of benefit to community sports clubs who are without close medical direction.
For more information on the diagnosis and management of sports concussion, a free online short course is at: www.connectivity.org.au/

WAAC’s M Clinic is on a mission to make syphilis testing as accessible as possible to the widest number of people. Here’s how.
The past five years have been worrying for health professionals working in the area of sexually transmitted infections as they move to stem the serious spike in syphilis throughout the nation, and especially here in WA, Northern Territory and Queensland.
While the number of cases is slowly trending downwards in WA since the peak in 2021 of 845 (697 in 2023), WA Health data also shows that 17 cases of congenital syphilis have been reported in the past five years and that has been stubbornly fixed at four cases a year since 2020.
Health clinics across the state have been focusing campaigns on their vulnerable populations. At WAAC (formerly known as the WA AIDS Council), Dr Fergus McCabe, Clinical Governor of WAAC’s M Clinic, says there is a focus for his team on reaching out to the proportion of its men who have sex with men (MSM) population who don’t identify as gay as well as FIFO workers.
WA Health reports that syphilis notifications that have the greatest proportional increases have occurred in non-Indigenous females (23%), with 77% of the WA women who have given birth to an infant with congenital syphilis having been diagnosed late in pregnancy.
“The vast proportion of our clients are very experienced and very open to testing for communicable
diseases – testing is seen as essential prevention. But there is a population of MSM that don't identify with being gay or bisexual, so they don't hear our health messaging and don't link in with our services. An important part of this syphilis campaign seeks to protect the transmission to women, particularly pregnant women,” he says.
“Testing is the key to arresting the outbreak and we need to remove barriers for these difficult-to-reach populations. We test frequently in and out of the clinic for HIV and now we’re adding syphilis to that regime.
“And we are also doing telehealth which gives a level of privacy and accessibility which we hope will encourage men to come forward for testing.
“To increase surveillance, we have started a HIV opt-out pilot program in some GP practices where participating GPs agree to test everyone in the risk age at least once a year – or more if their behaviours are higher risk for HIV. Testing for syphilis has now been added to that regime.”
“There are barriers with the population that we're trying to access because those conversations are fraught. The potential consequences of a positive result are confronting. However, that’s not to say the conversations shouldn’t happen, but they need to be
nuanced because 99.9% of those patients do not want to harm their partner. They're just terrified.
“There are also barriers to good surveillance in a busy general practice because it isn’t a quick conversation, it is very complex, and then some doctors may find bringing up this subject very difficult.”
Dr McCabe said colleagues needed support to overcome these anxieties and recognise the need to build conversations with patients with a focus on sexual behaviours, rather than “labels” in relation to sexuality.
“The syphilis campaign, along with the HIV update in testing and treatment, is all about normalising the conversations and putting aside the stereotypical image of the patient that you think you should test. Of course, those highrisk patients should be tested but we might start by prioritising any woman of reproductive age, any MSM and/or men who are sexually active and have multiple heterosexual partners,” he says.
“It is important to recognise that there's a population we're not reaching and find ways to test and screen those populations for syphilis. And then we need to look at supporting doctors requesting the test and then interpreting the test, because that's another issue.
“There may be fear in the back of
a doctor's mind, for instance, that if the test returns positive, what are the next steps, what is the treatment?”
WAAC has produced an effective graphic (published here) that is a good starting point for doctors.
“We at the M Clinic ask explicit questions every day and find it easy to open these conversations with patients but if you are not doing that every day, it can engender legitimate fear.
“It’s not just about educating and training GPs or any doctor, it's about educating the community because doctors are part of that community, so conversations become easier and easier to have.
“An opt-out process would break down those boundaries much quicker over time, so that in five years’ time syphilis testing would be as routine as pregnancy testing.
“We need to learn from that experience.”
Dr McCabe said support from GPs was available from a number of sexual health clinics, such as the M Clinic, who can help with a positive
test result. Dr McCabe said the M Clinic also offers anonymous testing off site which helps remove testing barriers. The venue where testing is conducted, Perth Steam Works, is a sauna for men who have sex with men.
“We had extraordinary results running a vaccination clinic there during the recent monkeypox outbreak and we also do PrEP[Preexposure prophylaxis] HIV clinics and STI testing.
“This is one of the places where MSM who don't identify with being gay go and who might also have partners. Right now, they can be tested under an assumed name, in which case we'll test and treat, and at the same time counsel about the need for any potential partners to be tested,” he said.
“We all just have to do what's clinically valid and relevant.”
Treatment is straightforward with syphilis being one of the infections that has not developed resistance to penicillin.
“It's exquisitely sensitive to penicillin,” Dr McCabe said. “The treatment for primary syphilis is
< 2 years
Commonly called Late Latent and Tertiary Syphilis
*Can also be asymptomatic
two injections of long-acting Bicillin. However, if it is latent syphilis, that’s where GPs may need help in interpreting results and offering treatment.
“It's not just about interpreting the results. It's knowing the sexual health and syphilis history of the patient and deciding on a course of treatment relevant to them.
“There had been lots of talk and some initial moves to establish a national syphilis register just before COVID broke out, some states such as Queensland have a state register. It would be very useful.
“Currently our experienced M Clinic nurses spend hours searching for and establishing a patient’s syphilis history for a requesting GP. So once the test has been done, they can support the GP’s clinical decisions.
“If a GP is not happy treating, we can take on the patient and return the patient with an explanation of treatment, which will equip that GP in the future. We want GPs to feel comfortable to pick up the phone and ask us questions.”

Back in 2017, the RACGP reported that varicose veins were a common reason for presentation to general practitioners, with many patients reporting symptoms such as aches and pains, cramps, restlessness and heaviness in the lower limbs.
According to the college’s summary of international treatment guidelines for varicose veins, swelling or skin damage, secondary to chronic venous insufficiency, occur in about 15% of the population and varicose ulcers develop in about 1% of the population.
With increasing levels of obesity in the community, and an ageing population, venous disease is expected to place an increasing burden on the Australian healthcare system in the future.
Truncal reflux from incompetence of the great or small saphenous veins is a major contributor to clinically significant venous pathology.
Historically, superficial venous incompetence has been treated by in-hospital open surgical repair, which requires general anaesthesia and hospitalisation, with some significant degree of post-operative morbidity being not uncommon.
Recurrence of varicose veins after surgery was a long-recognised complication, with incidence rates of 25-50% within five
years. Neovascularisation in the saphenofemoral junction is thought to be a significant cause of this postsurgery recurrence.
However, there has been a shift worldwide in best practice guidelines of varicose veins management, particularly in the development of minimally invasive technologies.
The European Society for Vascular Surgery’s 2022 Clinical Practice Guidelines on the Management of Chronic Venous Disease of the Lower Limbs (ESVS) reports that endovenous thermal ablation of truncal veins, with or without phlebectomies, is now widely acknowledged as the established standard of care and, ideally, should be performed in the ambulatory setting, in a properly equipped treatment room.
Endovenous thermal ablation (EVLA) causes an irreversible thermal injury in the vein wall, leading to fibrosis and, eventually, complete resorption over several months.
The ESVS now recommends that for patients with superficial venous incompetence, the procedures should be performed in the outpatient setting where possible.
In Australia, the efficacy and convenience of the minimally
invasive endovenous laser ablation has become the first-line treatment of choice for varicose veins for patients and practitioners alike. Alternatively, cyanoacrylate adhesive glue closure can also be used to close incompetent veins.
The in-rooms procedure takes about 45 minutes and begins with a locally anaethetised incision above the knee followed by an insertion of a thin laser wire – either near the knee or ankle. This is followed by tumescent local anaesthesia to protect the surrounding tissues from thermal injury and to reduce perioperative pain. Subsequently, with ultrasoundguided precision, the laser heats the vein and seals it shut.
More than 95% of patients achieve vast improvement in their symptoms and return to normal activity in a fraction of the time of the opensurgical option.
Typically, this is ‘walk-in, walkout’ procedure performed in the outpatient setting, with very little downtime. Most patients return to normal activities within a day, although it is recommended that strenuous exercise be avoided for a couple of weeks to ensure optimal healing.
Follow-up ultrasound imaging and appointments are crucial to monitor progress.

Perth’s newest iron infusion clinic has just opened in Subiaco as a result of its Medical Director and founder Dr Jason Oates’ concern about the difficulty of access to treatment.
He was spurred on by his own wife’s experience with restless leg syndrome (RLS), which was badly impacting her quality of life, and her frustration at the wait lists for infusions.
“There is plenty of evidence to say that iron infusions raise ferritin levels higher than you can achieve with oral iron, which is greatly beneficial for people with significant RLS,” said Dr Oates, who is an ENT facial plastic surgeon and owner of Academy Face and Body in Subiaco.

dose can be delivered in one infusion in about 15 to 30 minutes, and the risk of significant complications has plummeted,” Dr Oates said.
“So, the Iron Infusion Clinic is here to provide an individualised service, making it convenient for patients and for the prescribing doctors who don’t have to worry about the technicalities regarding the specific risk factors for their patient.
“But even after we had a referral for an iron infusion, there was a considerable wait.
“I had for some time been thinking that there was a need for a specific RLS clinic – I have gathered over 600 papers on the condition. I still believe in this idea, but it is incredibly complicated.
“So, we thought we would start with something more straightforward and set about addressing the need for easier access to iron infusions.”
Historically, an infusion could take all day to administer because of a high risk of allergic reaction that meant it was performed in a hospital-like setting, restricting access.
“But in the past decade, with access to intravenous iron, a total iron
“However, iron overload does have complications, such as haemochromatosis. Iron is a self-regulating nutrient and when you need more, your body absorbs it orally. As your iron levels rise, you naturally produce the hormone hepcidin to decrease your absorption rate. It is a naturally leveling process and oral iron is the best way to do it – but it is just not for everybody.”
Dr Oates pointed out that there were specific cohorts where iron infusions were needed, such as people with RLS, women with heavy menorrhagia; those who have iron absorption issues with inflammatory bowel disease, renal failure, bariatric surgery, cancer and cancer treatment where oral iron absorption can become limited.
“Doctors can easily refer patients through their practice management system with our supplied referral templates or referral pads. Our referral paperwork also makes it really clear to the patient how to contact us. When they make a booking, we send them detailed information about iron infusions and proper consent.

“While iron infusions are much less risky than they were previously, less risk does not mean zero risk.
“As such, we are a licensed day hospital, and while it is a nurse-led procedure, we have doctors on site. We can also treat haemosiderosis. We may not be able to eliminate iron staining 100% in everyone, but we can make a significant difference with our new tattoo removal laser.”
“As such, diagnosis and prescription are in the hands of the patient’s GP, but referrals can also be made by specialists such as gynaecologists, surgeons, cardiologists or oncologists,” he said.
Infusions are not needed by everyone with iron deficiency but make a huge difference for those where oral supplementation is not doing the job.
Pressures on the ‘sandwich generation’ caring for ageing parents and children will worsen over the next decade, according to healthcare start-up CEO Mark Woodland
Our ageing population, increased cost of living and onerous red tape means more Australians will be forced to forego caring for their parents to take care of their own families.
Governments need to start making long-term investments to solve long-term problems.
Australians are having children later in life, so they’re more likely to find themselves caring for elderly parents and their young family at the same time. It places a huge emotional and exhaustive financial strain on families, not to mention the guilt they feel for not being able to be there for everyone.
Families are going to max out their care capacity.
About 1.5 million middle-aged Australians are ‘sandwiched’ between caring for both their parents and their children and it’s a problem that will reach critical proportions in 10 years.
There’s a hidden army of grandparents helping their adult children with childcare arrangements now, but what happens when the elderly parents of adult children decline in health and need care themselves?
The reality is that as these grandparents age and start to encounter health problems, responsibilities shift to the adult children to support their elderly parents while still having to look after their own children.
Australia is on the brink of a healthcare crisis because of its ageing population and there’s an urgent need to find comprehensive solutions to affordable aged care and healthcare.
Yes, families are stretched, they’re already paying rent and mortgages and struggling to meet the costs of raising their own families. Do they have the capacity to care for their


ageing parents? Possibly not. There are cases of elderly people freezing to death in their homes in winter and dying from dehydration over summer.
This is happening with a smaller ageing population. Imagine the impact when most of the population is over 65.
The government is not in control of this problem and is not equipped to solve it because it’s currently led by people who won’t be impacted, so they don’t see it as their problem.
There are sustainable caregiving arrangements to help address the long-term challenges associated with caring for our ageing population and advances in administrative healthcare technologies is only a small part of the solution:
Cost of living: The increased cost of living means Australians are paying more healthcare costs, including medical treatments, equipment, medications, and specialised care. Having a clear plan can prevent unexpected costs and provide a roadmap for future care.
Ageing population: Solving the ageing population crisis requires a coordinated and multi-faceted approach that involves not only
government but investment, innovation, and support from the private sector to provide long-term solutions to long-term problems.
Infrastructure: Adapting the home environment for ageing parents, including accessibility modifications, may be a consideration and have less impact on the family's budget than moving them to an aged care facility.
Carers Leave: We need to think differently about how we use carers leave. Having access to carers leave doesn’t have to be a life-or-death situation. It’s dedicated leave to help ease the financial strain on employees who may otherwise need to take unpaid time off to spend time with their ageing parents.
Improved tech administration: Part of the solution is using technology to remove the emotional pain caused by navigating healthcare, so people have more time to spend with their families.
Private enterprise is crucial to grow healthcare infrastructure and services to meet the urgent need for healthcare services to support Australia’s ageing population.
ED: Mark Woodland is the co-founder and CEO of Kismet.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

More significantly, a woman requesting abortion may now self-refer to a private abortion provider without needing to consult a GP and obtain a referral.
The medical profession is not immune to societal trends, one of which is living in echo chambers where the only people you interact with are those who you agree with 100%.
New laws came into effect on March 27 regarding access to termination of pregnancy. You know you are getting older when the previous changes didn’t seem that long ago but were in fact 25 years ago.
Compared to those legal changes, there has been very little public discussion and (unless I have missed it) virtually no heated protests or vigils from either side. While I respect the views of those who are opposed to abortion on moral or religious grounds, this does not give them the right to impose their views on others. Fortunately, the issue does not get as political here as in other countries.
Now, only one health practitioner needs to be involved in abortion care provision up to 23 weeks A GP may now provide information, do the appropriate clinical assessment, and start early medical abortion processes or provide a referral for a surgical procedure in the first consultation. Beyond 23 weeks, two medical practitioners must be involved.
More significantly, a woman requesting abortion may now self-refer to a private abortion provider without needing to consult a GP and obtain a referral. This may improve access, which is I suspect the reason behind the change.
A piece which caught my eye was about the “hijacking of the feminist narrative” to market tests not backed by evidence. The BMJ article states “…promoting healthcare interventions that are not supported by evidence, or while concealing or downplaying evidence, increases the risk of harm to women through inappropriate medicalisation, overdiagnosis, and overtreatment. Importantly, the problem is not with the use of health technologies, tests, and treatments per se…The problem lies in the way commercial marketing and advocacy efforts push such interventions to a much larger group of women than is likely to benefit without being explicit about their limitations”.
On social media in particular, marketing is virtually impossible to police. The only solution is education.
Meanwhile, the increased focus on women’s health in general is paralleled by an increasing disregard for the safety and privacy of women. The good news is that women’s health is improving, and this is to be celebrated as we strive to make it even better.


Breast density (also called mammographic breast density) is a term used to describe how relative amounts of breast tissue appear on a mammogram.
Breast density cannot be seen or felt on examination. On a mammogram, non-dense fatty tissue appears as dark areas, while glandular and connective tissues appear white. Most breast cancers also appear white on a mammogram, so breast density can affect the accuracy of a mammogram. Breasts that have a high proportion of glandular and connective tissue are whiter on a mammogram and described as ‘dense’. In general, breast density is higher in younger women and reduces with increasing age. Increased breast density is
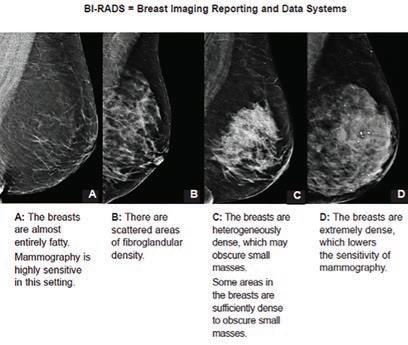
associated with a higher risk of breast cancer, although the risk is less than having a first degree relative with breast cancer diagnosed before menopause (doubles the risk) or carrying the BRCA gene mutation (three to six times the risk).

Breast density has not routinely been reported in Australia, apart from BreastScreen WA (since 2008) and BreastScreen SA (since 2023). BreastScreen WA notifies women and their GPs if they have heterogeneously or extremely dense breasts.
Breast density classification
Radiologists can estimate the level of breast density using the American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS).
The BI-RADS system defines breast density in the following categories:
• Type A (almost entirely fatty, the lowest density): around 10% of women have mostly fatty, very low density breasts
• Type B (scattered areas of fibroglandular tissue): approximately
Develop


Breast density is a complex topic requiring patient-centred care to provide information and decide on supplemental screening
Breast density is a breast cancer risk factor and can reduce the sensitivity of mammograms to detect cancer
Screening mammography is still beneficial irrespective of breast density score.
40% of women have this low level of density
• Type C (heterogeneously dense): approximately 40% of women have this type of breast density that may obscure small breast cancers
• Type D (extremely dense): around 10% of women have extremely dense breasts that lowers the sensitivity of mammograms due to the masking of some mammography features that identify cancer
Breast density can also be measured using computer software
to provide a percentage score and a BI-RADs score. BreastScreen WA notifies women if they have an empirically estimated breast density (BI-RADS Type C and Type D). Researchers at the University of WA found that over 70% of 5000+ woman surveyed said that knowing their breast density made them feel informed.
Breast density is complex and there are a number of known influencing factors:
• Age – younger women have higher mammographic breast density because of a higher proportion of fibro-glandular tissue compared to fatty tissue. Breast density generally declines with increasing age.
• Genetic factors
• Exogenous hormones (increases)
• Being on tamoxifen (decreases)
• Having children (reduces)
Breast size does not relate to breast density.
BreastScreen WA advises women
notified with breast density to see their GPs for a consultation and clinical breast examination (CBE). This is an opportunity to discuss mammographic breast density in the context of overall breast cancer risk of an individual woman (family history, long-term alcohol consumption, age at menarche, number of childbirths and breast feeding), perform a CBE and discuss further management.
There are no current randomised controlled trials to support routine supplemental breast imaging tests (e.g. ultrasound) in women with dense breasts. Research demonstrates that supplemental breast ultrasound in women with dense breasts increases cancer detection by 40% but has a high false positive biopsy rate (>90%). Tomosynthesis (3D mammography) has a high cancer detection rate but is not yet proven to show a survival benefit as a screening modality in women with dense breasts.
Without studies demonstrating a survival benefit, unnecessary
continued on Page 42


Paul is a locally trained surgeon who brings with him experience gained from several years of interstate and overseas fellowships, and specialises in: Hip & Knee replacement Sports knee Upper & Lower limb trauma Robotic-assisted joint replacement Foot & Ankle
Perth Hip and Knee are a specialist practice focused on the treatment of all aspects of hip and knee pathology. From arthroscopy to complex joint replacement and revision surgery, we deliver excellence in care utilising state-of-art surgical techniques and cutting-edge technologies to achieve optimal outcomes for our patients.
We are delighted to have Paul join Perth Hip & Knee and he is a valued addition to our group of experienced hip & knee surgeons. You can contact his rooms direct at rebgetz@hipnknee.com.au or on 08 6489 1766
Perth Hip & Knee
Suite 1/1 Wexford Street
Subiaco WA 6008
PHONE: 6489 1700
EMAL: admin@hipnknee.com.au www.hipnknee.com.au
 By Dr Purity Carr & Dr Christabel Samy, GPs, Rockingham
By Dr Purity Carr & Dr Christabel Samy, GPs, Rockingham
Several studies have recognised the menopausal symptoms such as joint pains, hot flushes and low morale impact significantly on the lives of women. Doctors need to appreciate the needs of individual women transitioning to menopause and perimenopause and assist in education and symptom management.
In a small study of 33 healthy premenopausal women, both total and free plasma testosterone showed steep declines with age. According to that study, a woman of 40 would have half the total testosterone concentration of a woman of 21. In those premenopausal women, plasma DHEA and DHEA(S) also declined steeply with age. Clearly, women also pass through an andropause with aging. We have also conducted a small local study.
The evolving significant menstrual period has significant impacts on the lives of women and society through economic, social, and physical wellbeing.
According to a study by ROCG (UK) 2019, “The menopause affects all women at some stage in their life, but many women do not know what to expect during the menopause nor do they feel empowered to seek help when needed or able to
manage their symptoms. This is particularly challenging for the 25% of menopausal women who experience severe symptoms and can lead to the onset of potentially avoidable health problems in the future.”
In a Lancet editorial, its quotes a study of 4000 of menopausal and perimenopausal women “almost half (45%) of women have not spoken to their general practitioner about their symptoms and 31% said it took multiple appointments with their GPs before they were properly diagnosed”.
Notwithstanding, the Women's Health Initiative (WHI) study reports that current data supports benefits of HRT, including symptom relief, quality of life improvement, prevention of coronary heart disease and osteoporosis, and mortality reduction. Notably, HRT does not increase all-cause, cardiovascular, or cancer mortality risk.
Variations in HRT efficacy and risks depend on factors like product origin (body identical or equine), dosage, route of administration, and timing of initiation. Transdermal oestradiol emerges as particularly effective for vasomotor symptoms. While oral estrogen increases venous thromboembolism (VTE) risk, transdermal forms are safer,
continued from Page 41
use of radiological investigations can lead to overdiagnosis and overtreatment. Therefore, it is important to have an individualised approach, which may result in some women, after a consultation and CBE, reasonably referred for
supplemental breast imaging. For example, a breast lump was detected on CBE, and a breast ultrasound requested.
Despite there being currently no clinical guidelines for breast screening or managing cancer risk for women with dense breasts, mammography provided by an

especially for women at higher VTE risk.
Oral estrogen also raises stroke risk, but transdermal options do not. Natural micronised progesterone (MP) offers advantages over synthetic progestogens, including lower VTE risk, cardiovascular neutrality, and possibly lower breast cancer risk, especially when used for over five years. MP also provides effective endometrial protection, making it a favourable choice in HRT. Recommendations favour transdermal estrogen to mitigate side effects, highlighting the importance of tailored treatment approaches in optimising menopausal symptom management.
Typically, one can observe significant improvement in symptoms within six weeks, and by three months, patients often score close to zero on their Australian Menopause Society (AMS) Diagnosing Menopause: Symptom Score Sheet. If a woman's symptoms persist beyond this point, explore other potential causes, with the most common missed diagnosis being ADHD and sleep apnoea. Hot flushes typically resolve within two weeks. Palpitations, tinnitus, and muscle spasms are among the first to improve.
audited, double-blind screening program such as BreastScreen WA still remains the best population screening modality for breast cancer in asymptomatic women aged 50-74 years.
– References available on request
Author competing interests – nil
Menopausal symptoms can have significant impact on quality of life
HRT has a legitimate role in alleviating symptoms
Individualised care is key.
Joint pain and back pain may take 6-9 months to significantly improve, depending on underlying pathology. Sleep and mood typically show rapid improvement, with the breakdown product of progesterone, allopregnanolone, exerting a sedating and relaxing effect without causing grogginess. Around 90% of women experience improved sleep within half an hour to one hour of taking progesterone while a small proportion may report symptoms of intolerance, including bloating, anxiety, headaches, and fatigue.
When topical oestrogen is used appropriately, symptoms of genitourinary syndrome of menopause (GSM) improve within six weeks. Longer and more severe symptoms may take
longer. Daily vaginal estrogen for two weeks followed by twice weekly thereafter may not provide adequate symptom control for some women, necessitating more frequent use. Notably, vaginal estrogen is generally safe for use, even in women not on HRT, with gynaecologists often permitting its use in women on Tamoxifen.
Testosterone therapy, typically prescribed for hypoactive sexual desire disorder (HSDD), can improve energy, sense of well-being, and muscle toning, with the aim of achieving a free androgen index (FAI) of 2-3.
Testosterone therapy complements estrogen therapy, with the goal of returning symptoms to premenopausal ranges. Contrary to misconceptions, testosterone therapy does not typically result in masculinising effects like facial hair growth or deepening of the voice.
The notion of a 3-5-year limit on HRT is not scientifically based, and long-term HRT use has been shown to provide better outcomes for patients in terms of cardiovascular protection and metabolic improvements. Thus, HRT can
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy

Surgery can be open or endoscopic. The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.
be used indefinitely to manage menopausal symptoms effectively.
From the viewpoint of a senior GP, the issues that have been identified with this research is that GPs in general are faced with compounding clinical issues based on the expectations of patients. This could also be the result of macro issues dealing with standard MBS consultation criteria, shortage, and turnover of GPs, and reducing number of bulk billing clinics affecting access and affordability. It is very common for patient to present with the ‘shopping list’ of complaints and this poses many diagnostic challenges for the time pressures for clinicians.
This brief update is based on a research study led by Professor (Dr) Martin Samy for Senate submission to the STANDING COMMITTEE ON COMMUNITY AFFAIRS Inquiry into Issues related to menopause and perimenopause. Submission 41 can be viewed under the public domain of the Parliament of Australia.

Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre
Suite 10, 100 Murdoch Drive, Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301
www.murdochorthopaedic.com.au
Murdoch Orthopaedic
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Endometriosis is a complex and often debilitating condition affecting millions worldwide. Characterised by the growth of endometrial-like tissue outside the uterus, it can lead to chronic pelvic pain, dysmenorrhoea, and infertility. Hormonal therapies are a cornerstone of endometriosis management, aiming to reduce oestrogen levels and alleviate symptoms. There remains an important clinical need for safe, highly effective, convenient medical treatments that can be used long term for endometriosis related pain, which may reduce the need for opioids and repeated surgery.
Ryeqo ® is an orally administered, gonadotropin-releasing hormone (GnRH) analogue that combines three active ingredients: relugolix 40mg, oestradiol hemihydrate 1mg, and norethisterone acetate 0.5mg. Although these ingredients have been used for many years, Ryeqo ® is the first treatment approved for endometriosis in 13 years.
Relugolix is an oral non-peptide selective gonadotrophin-releasing hormone (GnRH) receptor antagonist. It inhibits the pituitary release of luteinising hormone (LH) and follicle-stimulating hormone (FSH), leading to suppression of ovarian follicular growth and development which reduces oestrogen production. Prevention of an LH surge inhibits ovulation and development of the corpus luteum, which precludes progesterone production.
Monotherapy relugolix is unsuitable for long-term use, hence oestradiol is included to minimise hypooestrogenic symptoms, and loss of bone mineral density (BMD). Norethisterone acetate is included as a progesterone for endometrial protection in non-hysterectomised women.
Efficacy
The SPIRIT 1 and 2 trials
A significant advancement in the hormonal management of endometriosis, has been approved for use It can provide comprehensive hormonal suppression, leading to significant reductions in endometriosis-associated pain. Careful consideration of its risks, side effects, and longterm implications is essential in ensuring its safe and effective use in clinical practice.
demonstrated efficacy in reducing endometriosis-associated pain compared with placebo. More patients reported reduction in dysmenorrhoea (75% versus 2730%) and reduced non-menstrual pelvic pain (58-66% versus 4043%) at six months of follow-up. Some 62.5% reported amenorrhoea at 24 weeks of use.
LIBERTY 1 and 2 studied fibroidassociated heavy menstrual bleeding. More patients in the treatment arms achieved the primary endpoint (menstrual blood loss of less than 80 mL during the final month of treatment and at least a 50 percent reduction in menstrual blood loss from baseline to the final month) compared with placebo (71-80% versus 15-19%). An improvement in a number of other secondary endpoints was also seen, including anaemia, bulkrelated symptoms, and uterine volume [reduction of approximately 12-15%; range -3.2 to -23%]) with preservation of BMD.
In the LIBERTY trials, women with a fibroid uterus receiving active medication, were more likely to experience amenorrhoea (51.6%) or cyclic bleeding (15.4%), with the remainder (31.9%) reporting an irregular bleeding pattern at 24 weeks of use. At 52 weeks of use, 70.6% were likely to experience


amenorrhoea. In the SPIRIT trials, a majority of patients with endometriosis (65.2%) reported amenorrhoea at 24 weeks of use.
Anovulation can be observed 4 weeks following initiation leading to effective contraception after this time. A rapid return to ovulation occurs on discontinuation. Concomitant use of hormonal contraceptives is contra-indicated. Common side effects include vasomotor symptoms, headache, fatigue, nausea, nasopharyngitis, dizziness, abnormal uterine bleeding, loss of libido, hair loss, irritability, sweating and breast cyst formation. There has been an association with a potential decrease in bone mineral density. However, this loss was less than 1% in the SPIRIT trials and not considered clinically significant. An observational study of untreated age-matched women with endometriosis was subsequently conducted to characterise longitudinal BMD of premenopausal women aged 18-50 years. Through 52 weeks of observation, there was minimal change in BMD compared with those in an age-matched cohort of premenopausal women with endometriosis.
Regular monitoring of BMD is therefore recommended for patients receiving long-term therapy. Assessment of BMD by DEXA scan is recommended at baseline, after one year of treatment, and annually thereafter. Use is recommended to be limited to 24 months, with extension of therapy conditional on stability of DEXA and reassessment of risk/ benefit in the individual patient by the treating physician.
Data comparing to established treatments for endometriosisrelated pain are lacking. For endometriosis and fibroids, indirect
Endometriosis affects one in seven women and is more common in certain groups, affecting 50% of women with chronic pelvic pain, 40% of women with subfertility and 25% of transgender men. Symptoms include pelvic pain, dysmenorrhoea, dyschezia, dyspareunia, fatigue and subfertility.
Endometriomas, commonly called chocolate cysts, are collections of endometriosis within the ovary. Endometriomas often occur concurrently with deep infiltrating endometriosis (D.I.E), with over 60% of those with an endometrioma having D.I.E.
While most endometriomas are benign, larger endometriomas are more likely to be malignant, with 0.8% of endometriomas larger than 4cm being malignant. Size of the endometrioma should be used to risk-stratify patients as other markers, such as serum Ca125, are not a useful measure to distinguish cases of ovarian cancer as their level is often elevated with endometriosis.
The correct treatment depends on the symptoms, size of the cyst and the patient’s preference:
1. Endometriomas <4cm and asymptomatic
• Treatment is not required
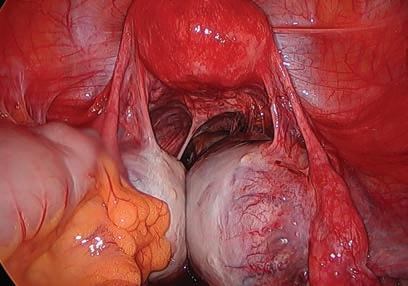

• Surveillance of the endometrioma is recommended. Reasonable surveillance involves ultrasound at 6 and 12 months, then yearly if stable in size and appearance
• Surgery may be considered for those at higher risk of

ovarian cancer, after counselling
2. Endometriomas <4cm size with pain
• Treatment options should include non-hormonal, hormonal and surgical
• Non-hormonal treatment: NSAIDs have the best evidence for pain management
• Hormonal treatment: The COCP or progesteroneonly medications such as progesterone-only contraceptive pills, depot injections or IUD coil. (The progesterone IUD is unlikely to shrink an endometrioma, however, it can provide symptom relief from other endometriosis)
• GnRH analogues can treat pain associated with endometriomas but given their side effects, should only be prescribed long term in a multidisciplinary setting by a gynaecologist who specialises in endometriosis management
• Surgical management should be offered as a treatment option to all patients who have persistent pain despite medical treatment or to those who prefer surgery as first-line treatment
3. Endometriomas >4cm
• Surgical management is recommended due to the
continued from Page 45
comparisons with other GnRH agonists such as Goserelin show similar efficacy.
Indications
This new medication is indicated for the management of endometriosisassociated pain. The effect is usually noted within the first four
weeks of use. It is recommended for patients who have not responded to, or who are intolerant of, other treatments. Before initiating treatment, other medical treatments should be considered.
Ryeqo ® is not currently PBS listed, however an application is underway. Currently in Australia, Ryeqo ® is indicated in adult women of reproductive age for:
• treatment of moderate to severe symptoms of uterine fibroids,
• symptomatic treatment of endometriosis in women with a history of previous medical or surgical treatment for their endometriosis.
– References available on request Author competing interests
60% of those with endometriomas have concurrent deep infiltrating endometriosis. All patients with an endometrioma having surgery need a pre-operative D.I.E Ultrasound
If D.I.E is found on imaging, surgery is of a high level of complexity, however a negative D.I.E scan does not completely exclude the presence of D.I.E or of significant pelvic adhesions
Endometriomas larger than 4cm should be surgically resected due to the higher risk of malignancy.
higher chance of malignancy with endometriomas of this size.
Surgical management of endometriomas
• Drainage of an endometrioma alone should not be performed for symptom management, as there is a 100% chance of recurrence
• 60% of patients with an endometrioma will have D.I.E, therefore a D.I.E Ultrasound
should be performed as part of a pre-operative work-up for all patients with an endometrioma who are planning to have surgery
• If imaging confirms D.I.E, surgery is of a high level of complexity and should be undertaken by a specialist with formalised training in advanced laparoscopic surgery
• Patients should be advised pre-operatively on the pain outcomes following surgery: 80% will experience a significant improvement in pain following surgery, just under 20% will notice no change to their pain and 1-2% will experience a worsening of pain following surgery
• Treatment of an endometrioma should be via laparoscopic ovarian cystectomy (removal of the cyst wall) as this has been associated with a lower chance of recurrence and a smaller decline in ovarian reserve compared to ablation of ovarian tissue. Other equally effective options are ovarian sclerotherapy.
Surgical excision of endometriomas has been shown to improve
spontaneous pregnancy rates in those with subfertility and should be offered as a management option. Surgery for endometriomas has no effect on IVF/ICSI outcome and therefore should only be offered to this group of patients for pain management or to exclude malignancy (i.e. the endometrioma is >4cm)
Any patient who has surgery for an endometrioma should be offered hormonal suppression post-operatively to reduce the recurrence rate as two or more surgeries on an ovary for an endometrioma has been shown to be a significant risk factor for unsuccessful fertility treatment.
Author competing interests – nil
Living Diabetes & Endocrinology is WA’s first integrated, comprehensive care centre for people living with diabetes and other endocrine and metabolic conditions delivered by a team of experienced endocrinologists and skilled allied health professionals including:
Endocrinologists
Diabetes educators
Dieticians
Exercise physiologists
Podiatrists
Psychologists and other allied health professionals
Centrally located in Osborne Park with free parking, Living Diabetes is the vision of one of Perth’s most experienced diabetes specialists, Dr Joey Kaye, providing care for adult patients with all forms of diabetes including GDM, pre-diabetes and cardiometabolic dysfunction. We are also accepting referrals for all forms of general endocrine conditions.

Rapid access for new patients from March 2024 and on-going urgent referral slots
Email: admin@livingdiabetes.com.au Phone: 08 6374 6438 Learn more at www.livingdiabetes.com.au and find out more about our GP education program

Dermatologist supervised total body photography and sequential digital dermoscopic imaging for high risk patients with multiple naevi and melanoma.
Urgent Lesion Clinic for suspected melanoma diagnoses or any urgent lesion (private health insurance rebates apply in our day procedure centre).
Personalised melanoma risk assessment to determine surveillance intervals and educate patients on risk factors.
Confocal microscopy for diagnosis and pre-surgical mapping of lentigo maligna (in situ melanoma) at complex and cosmetically sensitive sites (Dr Collgros).
Management of cutaneous toxicities related to medical oncology treatments.


Ovarian reserve, defined by the quantity and quality of remaining oocytes within the ovaries, plays a pivotal role in female fertility. This article explores the concept of ovarian reserve, its impact on achieving pregnancy, and various factors influencing its decline, plus methods of assessment and potential management strategies.
The ovaries house immature oocytes (eggs) within follicles. From birth, a finite number of primordial follicles exist, and as a woman reaches puberty, a select few follicles mature each month, culminating in ovulation. This process continues until menopause, when the ovaries cease releasing eggs, and menstruation ceases.
Ovarian reserve, therefore, reflects the remaining pool of follicles and their capacity to produce viable eggs capable of fertilisation. A higher reserve translates to a greater potential for achieving pregnancy, while a diminished reserve can present challenges for natural conception and assisted reproductive technologies (ART) like in vitro fertilisation (IVF).
A woman's fertility demonstrably declines with age, directly linked to her ovarian reserve. As she ages, the number of follicles diminishes, and the remaining oocytes may exhibit decreased chromosomal competency, impacting the likelihood of a healthy pregnancy. Notably, diminished ovarian reserve can also occur in younger women due to various factors, leading to difficulties conceiving naturally and potentially lower success rates with fertility treatments.
Ovarian reserve assessment
Several tests can be employed to estimate a woman's ovarian reserve. These include:
• Basal Follicle-Stimulating Hormone (FSH) Level: This blood test measures the level of FSH, a hormone responsible for stimulating egg development. An elevated level on day three of the menstrual cycle may suggest a diminished reserve
• Anti-Mullerian Hormone (AMH)

Key messages
Ovarian reserve decreases with age
There are various assessment options Personalised management is important.
Level: This blood test measures AMH, a hormone produced by small follicles in the ovaries. A low AMH level can indicate a lower ovarian reserve
• Antral Follicle Count (AFC): This transvaginal ultrasound scan visualises and counts the small follicles present in the ovaries. A lower AFC can indicate a reduced ovarian reserve.
It is crucial to note that these tests provide an indirect assessment and are not definitive indicators of fertility potential. A woman with a lower ovarian reserve may still conceive naturally and, conversely, someone with a seemingly ‘normal’ reserve may face fertility challenges due to other factors.
Several factors can influence a woman's ovarian reserve, including:
• Age: The most significant factor, with a natural decline in reserve occurring with increasing age
• Genetics: Some women are predisposed to a lower reserve due to their genetic makeup
• Medical conditions: Certain
medical conditions and surgeries, such as endometriosis, PCOS, ovarian surgery and chemotherapy, can impact ovarian reserve
• Lifestyle factors: Smoking and substance abuse may potentially contribute to a decline in ovarian reserve.
So what are the management options given there is no established method to increase the number of eggs?
If a woman has concerns about her ovarian reserve then the discussion can include:
• Early family planning: If a woman desires children and has concerns about her ovarian reserve, earlier childbearing may be recommended
• Fertility preservation: Techniques like oocyte cryopreservation (egg freezing) or embryo cryopreservation can allow women to preserve their reproductive potential for future use, particularly if they plan to delay childbearing
• Fertility treatments: Depending on the individual situation, ART procedures like IVF can be considered to overcome challenges related to diminished ovarian reserve.
Ovarian reserve is a critical factor in female fertility, and understanding its implications is crucial for women planning their reproductive future.
Author competing interests – nil

Understanding the intricate relationship between diet, lifestyle and gastrointestinal health is paramount for medical professionals, especially when addressing conditions like irritable bowel syndrome (IBS) that significantly impact women's health.
With its complex symptomatology and multifactorial aetiology, managing IBS requires a comprehensive approach, with diet playing a pivotal role in symptom management and improving quality of life.
IBS affects millions of people worldwide, with women bearing a disproportionate burden of the condition. Various factors contribute to the pathophysiology of IBS, including alterations in gut motility, visceral hypersensitivity, immune activation and disturbances in the gut microbiota composition. These factors, along with hormonal fluctuations and psychological stressors, create a complex interplay that exacerbates gastrointestinal symptoms in women with IBS.
While triggers may vary among individuals, certain dietary patterns have been identified as common culprits in exacerbating symptoms. These include high-FODMAP (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) foods, ultra-processed foods, caffeine, and spicy foods.
The low-FODMAP diet targets fermentable carbohydrates that are poorly absorbed in the small
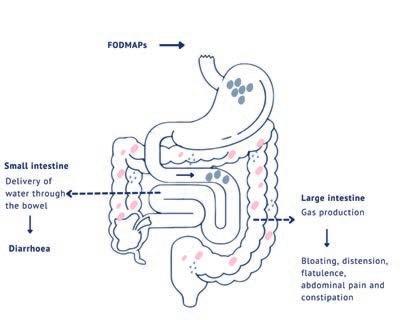
Diet plays a pivotal role in managing IBS symptoms, particularly in women, who bear a disproportionate burden of the condition
Evidence-based dietary interventions (e.g. low-FODMAP diet, mindful eating, and individualised advice), offer effective strategies for symptom management and improving quality of life in individuals with IBS
Collaboration between medical professionals and gastroenterology dietitians provides comprehensive care and optimising outcomes for patients with IBS.
intestine, leading to osmotic effects and increased gas production in the colon. By reducing intake of highFODMAP foods, individuals with IBS can alleviate symptoms such as bloating, abdominal pain, and altered bowel habits. It's important to note that the low-FODMAP diet is not a long-term solution but rather a short-term intervention to identify trigger foods and then gradually reintroduce them to establish individual tolerance levels.
High-FODMAP foods ferment in the gut, leading to the production of gas and short-chain fatty acids, which can cause bloating, distention, and discomfort in individuals with IBS. By reducing FODMAP intake, the lowFODMAP diet aims to alleviate these symptoms by minimising fermentation and osmotic effects in the gastrointestinal tract. Additionally, reducing FODMAP intake can help rebalance the gut microbiota composition, promoting gut health and overall well-being.
Low-FODMAP Diet: This dietary approach involves restricting foods high in fermentable carbohydrates, which can contribute to gastrointestinal symptoms in susceptible individuals. Studies

have demonstrated the efficacy of the low-FODMAP diet in reducing IBS symptoms. However, it's crucial to emphasise the importance of working with a gastroenterology dietitian to ensure the diet is appropriate for implementation, individual tolerance is established and long-term nutritional adequacy is achieved.
Mindful Eating and Stress Management: Incorporating mindfulness techniques and stress management strategies into dietary counselling can be beneficial for individuals with IBS. Mindful eating practices promote awareness of hunger and satiety cues, fostering a healthier relationship with food and reducing the likelihood of symptom triggers. Additionally, stress reduction techniques such as relaxation exercises, yoga, gut-directed hypnotherapy and cognitive-behavioural therapy can help mitigate the impact of psychological factors on gastrointestinal function.
Individualised Nutrition Advice: Recognising the heterogeneity of IBS presentations, individualised nutrition advise tailored to individual needs and symptoms are paramount. This approach involves identifying specific trigger foods through comprehensive dietary assessments and symptom monitoring. By empowering patients to make informed dietary choices and providing ongoing support, dietitians can optimise symptom management.
In conclusion, addressing the impact of diet on irritable bowel syndrome is integral to promoting women's health and enhancing the quality of life for individuals living with this chronic condition. By adopting evidence-based dietary interventions and embracing a multidisciplinary approach, we can empower patients to regain control over their gastrointestinal health and live fulfilling lives.
Author competing interests - nil
In the rapidly evolving landscape of orthopaedic surgery, the integration of robotic assistance in hip and knee arthroplasty, in my opinion, has become a game-changer.
While traditional arthroplasty techniques can yield excellent results and will continue a mainstay of orthopaedics, I believe that in most circumstances, the use of robotics introduces a new level of predictability and precision, contributing to enhanced patient satisfaction and long-term success.
One of the key advantages of robotic-assisted hip and knee arthroplasty lies in the unparalleled precision it offers during joint reconstruction. Traditional methods, while very successful, rely on the surgeon's skill and experience, which can vary. In contrast, robotics provide a level of accuracy that can exceed human capabilities.
Utilising preoperative planning and intraoperative feedback, robotic systems allow for meticulous bone resection, optimal implant positioning, and fine-tuned soft tissue balancing.
This heightened precision can translate into more reliable joint kinematics, ultimately contributing to improved postoperative function and reduced complications. Robotic-assisted arthroplasty can



empower surgeons with advanced tools to create highly individualised treatment plans for each patient.
Through detailed preoperative imaging and virtual modelling, the surgeon can tailor the procedure to the patient's unique anatomy, addressing specific deformities and optimising implant placement. This personalised approach may enhance the desired biomechanics of the joint but may also contribute to improved post-operative function.
The ability to account for variations in anatomy ensures a customised and predictable outcome, which can lead to increased patient satisfaction and improved long-term results.
While the debate around the necessity of robotics in hip and knee arthroplasty persists, real-
world cases can demonstrate the transformative impact of these technologies, especially in complex scenarios.
Consider the case of a young female patient with abnormal acetabular and femoral anatomy, severe osteoarthritis, and significantly contracted soft tissues due to childhood SUFE (slipped upper femoral epiphysis).
This challenging case necessitated a level of precision and customisation beyond what traditional methods could offer. By utilising CT-guided robotic planning and roboticassisted surgery, it was possible to navigate the intricacies of the patient's unique anatomy with unparalleled accuracy. The robotic system allowed for meticulous planning and execution, ensuring optimal placement of components
Robotic surgery can be a game changer
Surgery can be tailored to individual anatomy
Precision and predictability are key benefits.
to achieve the best possible range of motion without impingement.
The precision achieved during surgery went beyond routine cases, addressing the complexities presented by abnormal anatomy and soft tissue constraints. Through robotic assistance, accurate implant placement, alignment, and restoration of leg length were achieved with a level of confidence that traditional methods might struggle to replicate.
This not only resulted in a successful total hip replacement but also exemplified the adaptability and reliability of robotic-assisted techniques in overcoming challenging scenarios.
This case demonstrates the value of robotics in achieving consistently accurate outcomes, particularly in cases with abnormal anatomical variations. The ability to tailor the surgery to the patient's unique needs increases the likely success of the procedure but also the restoration of functionality and quality of life in challenging cases.
In turn, this reinforces the argument for the predictability and precision offered by robotic-assisted hip and knee arthroplasty.
In acknowledging the transformative potential of robotic-assisted hip and knee arthroplasty, it is crucial to address potential pitfalls that come with these advancements.
Firstly, in the event of a need to abort the robotic procedure midsurgery, the surgeon's expertise becomes paramount. The ability to seamlessly transition to conventional methods underscores the importance of a surgeon's experience, ensuring the continuity of the procedure.
Additionally, the use of two

separate, small stab incisions for the placement of pin arrays raises concerns about potential complications. These incisions, while necessary for robotic guidance, pose a risk of bone or soft-tissue injury and may become susceptible to post-operative wound infections.
Lastly, the learning curve for surgeons adopting robotic techniques can result in longer operative times. The initial phases of adaptation and proficiency development may extend the duration of procedures.
Despite these challenges, the potential benefits of roboticassisted surgery, as exemplified in precise and challenging cases, may outweigh these pitfalls when approached with careful consideration and ongoing professional development.
Author competing interests - nil

State of the Art Laboratory and Advanced Technology
Our state-of-the-art laboratory is equipped with cutting-edge technology to improve your chances of achieving a successful pregnancy.
Comprehensive Fertility and Gynaecology Services

We offer a comprehensive range of fertility services, such as Ovulation induction (OI), Intrauterine insemination (IUI), In-Vitro Fertilisation (IVF), Intracytoplasmic sperm injection (ICSI), frozen embryo transfer (FET), egg freezing and sperm freezing.
Our fertility specialists also perform a wide range of fertility related surgeries to address issues like endometriosis, fibroids, uterine septum, tubal disease and caesarean scar defect.
Ethical pricing
We offer bulk billing for all Medicare eligible items. For additional services we provide transparent pricing with no hidden fees or surprise costs.
Holistic approach
We understand that the journey to parenthood can be emotionally challenging, which is why we offer ongoing emotional support and counselling services throughout the treatment process. Our compassionate team of health professionals are available to provide support with the emotional aspects of infertility and IVF, ensuring that you feel cared for every step of the way.
Video consultation
Our video consultation service is available at no extra cost for those who are unable to attend consultations physically.
Convenient locations
Oasis fertility centre has created two state of the art beautifully designed practices to best facilitate the fertility journey at South Perth and Warwick.




Illicit drug use in young females has increased from 27% in 2019 to over 35% in 2023. Risky alcohol consumption has increased in young females from 28% (2019) to 35% (2023). Females are still seeking AOD treatment at lower rates than males despite these changes in behaviour.
Women often face greater discrimination and stigma for their AOD use than men, particularly in relation to pregnancy and parenting. This is often influenced by traditional gender-based roles and values placed on women.
Risk factors for Substance use Disorders:
Recurrent and easy access to substances
Stress and financial difficulties
Any mental illness or impairment
PTSD and trauma.
Signs & symptoms of a substance use disorder:
Frequent requests for early prescription refills
Social withdrawal or neglecting responsibilities
Physical changes; weight, poor hygiene or skin problems
Taking higher doses or more frequently than prescribed
Patient requesting prescriptions on first visit, “doctor shopping”
Changes in mood or behaviour; agitation, irritability and mood swings
Defensive or evasive when questioned about medications or drug use.
We can help...
If you think that a patient may have a substance use disorder, please refer them to Fresh Start, or a suitable specialist.
Referral forms can be found on our website www.freshstart.org.au or call our clinic on 08 9381 1333
Uterine fibroid embolisation (UFE), also known as uterine artery embolisation (UAE), can be seen as a transformative option in gynaecological healthcare, particularly for women with symptomatic fibroids aged 3550 who are premenopausal and have completed their childbearing years.
This minimally invasive procedure, performed by an interventional radiologist (IR), addresses symptoms associated with fibroids and adenomyosis, offering an alternative to traditional surgical interventions such as hysterectomy or myomectomy. The procedure has been available in WA to public patients on an ad hoc basis, and is now consistently available in the private system.
UFE involves blocking the blood flow to fibroids and adenomyosisaffected tissues by injecting embolic material into the uterine arteries. This procedure, performed through a pinhole incision in the groin or wrist, allows patients to remain awake, aided by sedation, analgesia and local anaesthesia.
Uterine fibroid embolisation is a minimally invasive non-surgical treatment option for fibroids
The procedure is performed by an interventional radiologist UFE can be effective at symptom management.
Post-procedure care usually involves a brief hospitalisation, typically lasting one night to manage any discomfort or side effects. Central to UFE is the collaborative decision-making process between patients, healthcare providers, and specialists. Thorough consultations with both a gynaecologist and an IR ensure that patients are wellinformed about their condition, treatment options, and the potential outcomes of UFE.
The advantages of UFE over surgery include its minimally invasive nature and preservation of the uterus. In addition, the effectiveness in reducing symptoms
Perth researchers are campaigning to get more oxygen machines in PNG to curb pneumonia deaths.
A study led by Telethon Kids Institute in collaboration with the PNG Institute of Medical Research has shown the importance of measuring oxygen levels in children with severe pneumonia, rather than solely relying on symptoms and signs.
In PNG, pneumonia is the leading cause of illness and death in children under five years, with 40% presenting for pneumonia having hypoxia, a condition occurring when oxygen drops to dangerous levels.
The Bill and Melinda Gates Foundation and Pfizer-funded study, published recently in The Lancet Regional Health, examined more than 2000 young children with pneumonia over seven years to see whether current methods could adequately predict oxygen levels, detecting the need for oxygen therapy. Hypoxia was observed in 36% of cases.
Although symptoms like blueish skin, nasal flaring or grunting when breathing, a rapid heart rate or drowsiness were more often seen in children with hypoxia, the study confirmed a combination of symptoms and signs were not accurate enough to detect hypoxia.

such as heavy menstrual bleeding and pelvic pain or pressure have been demonstrated as nearequivalent to myomectomy.
UFE boasts minimal blood loss, outpatient convenience, shorter hospital stays, and faster return to normal activities, making it a favourable choice for many eligible candidates.
However, it is essential to acknowledge potential disadvantages, such as postprocedural pain and discharge.
Nevertheless, for many women within the specified age range and clinical profile, UFE represents a significant advancement for women experiencing symptoms associated with fibroids and adenomyosis, without the need for major surgery. By offering a minimally invasive, uterus-preserving alternative, UFE empowers women to reclaim their health and quality of life.
Author competing interests – nil
Lead author Professor Chris Blyth from the Wesfarmers Centre of Vaccines and Infectious Diseases based at TKI, UWA and Perth Children’s Hospital said the research findings signalled the need to ensure technology to measure oxygen levels was made routinely available in all health care facilities.
“The study showed symptoms and signs of severe pneumonia were alone were not enough to detect the need for oxygen therapy,” Professor Blyth said.

As a medical illustrator, Ralph Baker’s job has changed a lot over the years, but he still loves it with an artistic passion.
Ralph Baker has made a career out of a niche profession. While its definition has widened as technology has progressed, his skills as a medical illustrator are still in demand.
After studying art and design at university with additional units in illustration, typography and design, Ralph started his medical illustration career at PMH. For eight years he drew, illustrated and made videos of procedures, body parts or anything which needed documenting. He also had fun drawing cartoon characters to put on the walls for the kids to enjoy.
By Ara Jansen
made videos and did a lot of anatomical drawings, which were often drawn from cadavers. Part of my job was to have extensive discussions with the doctors about what they wanted to see in the illustrations.”
laser printer appeared, alongside now indispensable illustration software. Every innovation has meant that across his career, Ralph has had to be open to learn new skills to add to his hand drawing.
“Perth in 1976 was a tiny place and there were not a lot of specialists in this type of work,” says Ralph. “We
A lot of the work was in colour but some of it was black and white. The tools of trade were Rotring pens, plastic lettering sets, tracing paper and lots of correction fluid. Often, if you made a mistake working in colour, you had to start from scratch, rather than just clearing the screen. Ralph got his first computer at work in the mid-1980s, which, while still rudimentary, was the start of things changing the way he worked. By the late ’80s, their first
“That obviously meant I could start drawing on a computer, but I still needed skills I’d always used to create the illustrations. If anything, this sort of illustration has become even more of a niche market and now with the advent of AI, it’s changing again.
“The doctors or specialists would often give me a simple and rudimentary pencil sketch of what they wanted. You needed to have enough anatomical understanding to know where to place what they were talking about and what system it was in. I learnt an enormous amount, saw lots of


medical lectures. That also really helped when I talked to medical staff because I knew what they were talking about.”
For more than 10 years, Ralph has been manager of the Medical Multimedia Design team at Royal Perth Hospital. He’s been at the hospital for almost 18 years, after spending nine years freelancing.
These days the job has expanded far beyond medical illustration to include many of the design needs of the hospital, which can include everything from a flyer or poster to an illustration or video. Three members of his team are medical artists. He says it’s a busy and exciting place to work.
While the team can be called on to do various different kinds of jobs, an example of where Ralph’s team’s work might be used these days is for an illustration to a research paper which is being published.
“I love drawing faces and hands. The weird thing is that after I draw a hand from a live model, it’s almost like you fall in love with that hand. It’s really strange. You become a
bit obsessed, the same way you do when you are doing an anatomical drawing. Nerves are fascinating to draw and you have to learn the difference between a vein and an artery.
“The fun part is getting the observer’s eye to pay attention to what you want them to see. If you are drawing a nerve and that’s what you want the viewer to see, you still need to draw the other parts around it but have the visual focus on the nerve.”
While these days he’s more likely to be drawing on a computer at work,
Ralph still loves to break out those old friends, his brushes. From his early 20s he’s had a personal art practice away from medical work. He’s a keen watercolourist who has exhibited regularly over the years. He paints landscapes, often around water, and loves big sized works. You’ll find his pieces on display at the John Julius Art Gallery in Subiaco, which showcases the work of those working in the medical field.

The 2024 German Film Festival returns to Perth from May 16 to June 5, with a program presenting the best of contemporary and classic German cinema, plus a handful of films from neighbours Austria and Switzerland.
Highlights include Foreign Language, which arrives direct from the 2024 Berlinale and is a coming-of-age drama about two teenage pen pals who forge a friendship through letters and language exchange; One For The Road, a touching story set between Berlin's famous bars and sober therapy rooms; Dark Satellites, an ensemble drama set in nighttime Leipzig that tells three stories about the impossibility of love; and Lubo, a historical drama set on the cusp of WWII.
The festival films are being shown at Palace Cinemas Raine Square, Luna Leederville and Luna on SX Fremantle. For more info see www. germanfilmfestival.com.au.
Thanks to Palace, we're giving away five double passes, valid for any film screening as part of the festival, excluding special events.
For those looking for more of an adrenaline rush, we also have 10 double passes to the action-comedy Bad Boys: Ride or Die, which is in cinemas from June 6. It stars Will Smith and Martin Lawrence.
To win tickets, use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.

Black Swan State Theatre is about to stage two legal dramas, both written by Australian playwright Suzie Miller.
Following her two loves – law and theatre – has given Suzie Miller some of the greatest satisfactions of her life. As a former human rights and children’s rights lawyer, Suzie’s experience has her well-placed to tackle two one-woman plays about the politics of law.
In June and July, Black Swan will stage these back-to-back legal dramas – the first being RBG: Of Many, One. It’s a story about Ruth Bader Ginsberg, the second women to be appointed to the US Supreme Court and celebrates the legacy and tenacity of the late cultural icon. She was an icon of Suzie’s while she was in law school. RBG is played by well-loved Australian actor Heather Mitchell.
The second play is Prima Facie, a one-woman show about a brilliant, young criminal defence barrister who specialises in defending men accused of sexual assault and suddenly finds herself standing on the other side of court after she is sexually assaulted.
Prima Facie will star WA actor Sophia Forrest. Working alongside Black Swan artistic director Kate Champion, the playwright is intrigued to see how they tackle it.
“Of course, I have seen quite a few versions but the direction changes
ByAra Jansen
everything in terms of the tone and the way they engage with the set,” says Suzie. “I have a lot of respect for Kate and have known her for a long time.
“As a lawyer I know how complex these situations are. It’s an examination of the legal system and how someone goes through it and how it changes the narrative. It’s also a meditation on class and gender and how that intersects. When the character goes on a date and something goes wrong, she realises she doesn’t have the power she thought she had.
“I also want men to think about it too. What’s really interesting is how men have responded to Prima Facie. If you love a legal story you’ll love it. If you love women, you’ll love it. Older men have found it really interesting too, because of the change in cultural attitudes and the realisation that they have a role in talking to younger men. It’s certainly starting a lot of conversations about consent.”
While that all sounds rather heavy for an evening at the theatre, Suzie says the play is not without humour and fun parts. “It is entertaining. I think you fall in love with the character because she’s fun, smart and sometimes frail.”
Since its premiere in 2019, Prima
Facie has continued to engage audiences and last year Suzie released a novel of the same name, which has already been nominated for several awards. There are currently some 30 productions of Prima Facie in 25 different languages being performed around the world. On a recent trip to Germany, she discovered no less than 20 different local productions in 16 state theatres and four festival productions.
The play has also garnered numerous awards, but Suzie says what’s even more satisfying are all the emails and conversations she has had with audience members, particularly members of the legal profession about both plays’ themes.
“Women lawyers are saying it’s great to be part of the theatre community with something that speaks to them. But it’s more than just lawyers because it is speaking to women everywhere. This is a story people have made their own, it’s no longer mine and really very much belongs to the audiences.”
RBG: Of Many, One runs from June 13 – 23 and Prima
July 1 – 21
From humble beginnings in 1997 in the Denmark sub-region, West Cape Howe has since grown to be a major WA producer of quality wines. Its success can be largely attributed to two of the four ownership partners – manager Gavin Berry, who has vast winemaking experience in the region, and adept viticulturist Rob Quenby.
A major turning point in their road to success was the purchase of the Langton property in Mt Barker –previously Goundrey Wines – which is now West Cape Howe’s home base, with a large winery and 100ha of quality vineyard. Fruit comes from their 210ha in the Frankland River sub-region, and from smaller parcels of fruit from other selected growers.
The five wines reviewed capture the varietal expressiveness of this great region and are exceptional value for money.

WEST CAPE HOWE 2023 Old School Mount Barker Chardonnay (RRP $22)
Displays fig, ripe honey dew melon and cashew. Supple. Malolactic secondary fermentation has softened this wine, but there is enough acidity to carry the flavours and give structure. French oak fermentation adds complexity. Drink now or over several years.
WEST CAPE HOWE 2022 Frankland River Tempranillo (RRP $22)
A fine example of this Spanish variety which continues to gain popularity in Australia. A deep red/purple colour. Aromas savoury, with red berries/redcurrant. The palate supple, with the ‘milkiness’ that I find in tempranillos. Blackcurrant flavours. Fine-grained ‘dusty’ tannins. Oak not central to the style if there at all. A complete easy drinking wine to drink now, and which will gain with 3-4 years’ cellaring.
WEST CAPE HOWE 2023 Mount Barker Riesling (RRP $22)
From the Langton property. Very much in the Lower Great Southern Riesling style, with pristine, pure, linear fruit profile. Crisp, fresh, and clean. Aromas of citrus lemon and lavender. Flavours of Meyer lemon, with a talcum and river pebble mouthfeel. Drinking well now but will gain in complexity for those who enjoy aged Riesling.

The next two wines tasted were from the more premium range, selected from the best parcels of fruit in the more mature vineyard sites, and are very good, and exceptional value.
WEST CAPE HOWE 2019 Book Ends Mount Barker Cabernet Sauvignon (RRP $36)
This is classic Cabernet. Attractive ruby/garnet colour. Nose complex with blackcurrant/cassis and cedary oak. Follows to blackcurrant and cassis on the palate. Fruit driven. Oak gives structure. Fine grained tannins glide across the palate. Supple, complex, integrated and longlingering flavours. Youthful for its five years, with another 10 years ahead for this wine.
WEST CAPE HOWE 2019 Two Steps Mount Barker Shiraz (RRP $36)
My wine of the tasting. Difficult to separate from the Cabernet in terms of quality, however, I am always vulnerable to Great Southern shiraz. Leaps from the glass with vibrant spices and white pepper. Flavours of powerful, mouth-filling ripe primary fruit. Rich plummy spice infused flavours. Savoury elements on the finish. Has elements that remind me of the great syrah wines of the French Rhone Valley, while still remaining very cool-climate Australian. Another 10-year wine. Cellar some now while still available.


SOUTH LAKE
Medical Rooms Available for Specialists and Allied Health
Lakes Shopping Centre, Shop 2, 620 Northlake Rd, South Lake WA 6164
•Available for ALL Specialists
•These consulting suites are situated on the ground floor of the medical practice, Featuring;
-Reception area and patient waiting rooms
-Staff kitchen and toilet.
Asking Rent: $30/Hour + GST, Annal rent $25,000 + GST (Per room)
For Further details and enquiries
please contact p.manager@southlakefamilypractice.com.au or 08 9417 1009
Hollywood Medical Centre
Suite 36, First Floor, 85 Monash Avenue, Nedlands
87sq m – fully fitted, large reception, 2 consulting, 2 treatment & 2 store rooms.
Contact: Irene 0409 688 339

JOONDALUP
87 McLarty Avenue – 2 units
Opportunities to secure 37m2 or 78m2 in this convenient location between the Health Campus and the CBD.
Contact Jackie Skubevski 0428 820 052 or visit Xceedre.com.au

Queens Road Surgery is a busy GP owned general practice located in Mount Pleasant.
We are looking for a VR GP to join our well established practice.
We offer a supportive team based culture, experienced administrative staff and quality full time nursing support. Queens Road Surgery is a fully equipped accredited practice.
For a confidential discussion
please contact our Practice Manager Narelle 0412 113 584 or narelle@queensroadsurgery.com.au

Niche, Boutique Medical Centre
looking for PART-TIME OR FULL-TIME VR GP
Our practice is situated in the Golden Triangle in the Western Suburbs.
Standard consult 23 - $100, 36 - $180 Practice nurse, and an outstanding administration support.
One Saturday per month (AM only) with higher rates.
Please send through your EOI to: manager@nedlandsmedicalcentre.com.au

We are looking for experience GPs with a passion to make a difference for people seeking help for substance use disorders to join our team at Fresh Start Clinic in Subiaco.
Fresh Start Clinic is the entry point for all clients and patients at Fresh Start. Our doctor’s perform general health checks, and create informed care plans for patient’s recovery.
•Fully bulk billed clinic
•Onsite Pathology
•Best Practice Software
•Nursing support
•Encourage special interest of addiction
•Immediate start
•Free parking
Business hours 9am – 5pm
Monday to Friday
For a confidential discussion please email Jeff Claughton ceo@freshstart.org.au
P/T GP required for our friendly practice in the heart of Fremantle. Young demographic with lots of student health, sexual health, women’s health and mental health. Fully equipped, accredited practice with full time practice nurse and onsite pathology, 2-3 days/week, days negotiable.
Contact Stephen on 0411 223 120 or at stephen@westendmed.com.au

KALAMUNDA/ HIGH WYCOMBE
•Well established and regarded medical practice, about to celebrate 60th year, offers a unique opportunity for a VR General Practitioner
•Long history of being a training practice, both GP Registrars and Medical Students.
•Main surgery in Kalamunda, with a further two surgeries in High Wycombe and second satellite surgery in Kalamunda
•Mixed billing (or private billing if preferred)
•Well organized for Chronic Disease Management and Care of the Elderly, with Primary Care (CDM) Nursing Staff at all four surgeries
•Very nurturing practice, empathic to patients and staff. Supportive of clinical team members with individual special interests (such as cosmetic and skin lesion skills, mental health, LGBTIQA+…)
•Excellent schools in the fantastic Perth Hills area, very welcoming community
•Work life balance a major priority that is respected by the team at Stirk
•Have the best of both worlds; country living with the city only 30 minutes away
Please forward a CV and any enquiries to either Karin Tatnell (0438 211 240) or Dr Mike Civil (0419 965 377 ) or email : manager@stirkmedicalgroup.com
75% OF BILLINGS!!
GP positions available in accredited mixed-billing clinics in Burswood and Claremont.
Looking for VR GPs and non-VR GP’s on a full time/part-time basis for weekday and Saturday afternoon sessions.
Fully computerised with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au

VR GP - Mount Lawley WA - Privately billed After Hours practice
GP After Hours Mount Lawley is a well-established, community-based after-hours practice. We privately bill and are GP owned and run.
We are looking for an experienced VR GP to join our team of clinicians in providing quality after hours care to our patients.
Our practice offers:
•Modern facilities with a fully equipped treatment room
•Fully computerised practice using Best Practice software
•Percentage of the billings with a minimum hourly rate guarantee
•All sessions are 4 hours in duration
•Opportunity for weekend / public holiday sessions
For all enquiries, please email Gina at gpahmtlawley@3rdave.com.au or call 0412760871
HIGH WYCOMBE
VR GP POSITION – Full time/Part time
•A busy, well equipped, fully computerized and AGPAL Accredited GP Practice in Perth, WA is looking for a VR Doctor
•Flexible days and hours tailored to your need
•Excellent RN and reception team as well as managerial support and onsite pathology
•Clinical full autonomy guaranteed
•Mixed Billings, using Best Practice Software
•GP private ownership
•Good income potential and emuneration at 72%, negotiable.
•$150 hourly minimum for the first three months.
The practice provides general GP services including skin check and many more.
For enquiries, Email: highwycombemc@bigpond.com Phone: 08 9454 6987
Opening for VR GP - F/time or P/time
Full Private List available now from retiring GPs
FRACGP essential
Up to 70% private billings
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
Enjoy working for a doctor-owned, non-corporate, well supported, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au
Contact Andrew, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
Contact Andrew, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
Contact Andrew, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert

Exciting opportunity with a leading medical research institute. Attractive salary packaging benefits. Previous clinical research experience is not essential.
RESPONSIBILITIES
Clinical assessments of research participants. Obtaining informed consent. Perform study activities as required by the protocol and regulations.
Interpretation of laboratory results, ECG, imaging. Monitor and evaluate study participants for the duration of the study.
Documentation of clinical care and research findings.
REQUIREMENTS
Current unconditional AHPRA Medical Practitioner Registration. Knowledge of ICH/GCP guidelines, MA Code of Conduct, National Statement is desirable.
TO APPLY
For full details and to apply, please go to seek.com.au CONTACT: yasmin@zesthr.au


Join the Soleil Health Team –Your Gateway to Exceptional Healthcare!
Soleil Health, the future hub of unparalleled medical care and holistic well-being, is on the lookout for passionate and skilled General Practitioners to join our dynamic team in Cottesloe. As we prepare to open our doors in August 2024, we invite you to be a part of a healthcare revolution that prioritises clinical excellence, patient well-being, and a collaborative work environment.
About the Role: As a General Practitioner at Soleil Health, you’ll experience clinical autonomy, allowing you to practice on your own terms. Our commitment to providing the best healthcare is reflected in the use of Best Practice Software, ensuring streamlined and efficient processes. Embrace a collegial and collaborative culture where teaching and education are at the forefront of our mission. GPs working for the practice also have the opportunity to provide home visit service to the neighbouring aged care residences.
Key Highlights:
Clinical Autonomy: Have the freedom to practice medicine focusing on your special interest.
Best Practice Software: Utilise cutting-edge tools to enhance the efficiency of your practice.
Collegial Culture: Engage in a collaborative environment, emphasising teaching and education.
Private Billing: Be a part of a practice that values your expertise with a private billing model.
About the Requirements:
Current unrestricted registration with the Medical Board of Australia / AHPRA
VR status with Medicare
AHPRA Registration
Valid working rights in Australia
Phone 0493 977 301 Email Manpreet.kaur@soleilhealth.com.au
soleilhealth.com.au


We have six consulting rooms and it is a lovely calm, caring environment with a great patient base.
We are close to all amenities including shopping, cafes, beaches and river.
This can be a full-time or part-time position with scope for all GP areas of interest.
Our team of friendly receptionists is complemented by two experienced practice nurses at all times.

For more information please contact admin@mosmanparkmedicalcentre.com.au

Gosnells Healthcare Centre has a great opportunity for General Practitioner to join a very well-established practice.
The role would suit a new Fellow or GP who wants to curate their own patient base with a guaranteed minimum offered for 6 months.
Wonderful, friendly practice
Experienced Doctors
Very Large existing and loyal patient base
Mixed billing practice
Enjoy an innovative, modern practice with the latest equipment and software (Best Practice)
70% of billings- plus attractive relocation package
Choose your hours, Our Clinic is open from 8am-5pm Monday-Friday.
On-site services include Pathology, Physiotherapy, Podiatry, Dietician
Fully Accredited practice
DPA Replacement Provider Number available
Safety Net of $150 per hour for 6 months
If you are interested in the exciting opportunity please contact Phil at ceo@spectrumhealth.net.au
Gosnells HealthCare Centre
2227A Albany Highway, Gosnells WA 6110
Join our team at Bullsbrook Medical Centre where you will enjoy every aspect of general practice. We are a well-established clinic with a strong and loyal patient base.
• Value driven, innovative, non-corporate GP owned medical centre with a highly competent administrative and nursing team, supporting the practice and allowing you to focus on servicing the patient demand.
• Large patient base with broad demographics.
• Team of GPs providing high quality care with a strong focus on comprehensive chronic disease management
• Fantastic opportunity for GP’s with special interests
• Friendly working environment of mutual support
• On-site Practice Manager, pathology and allied health.
• Fully computerised (Best Practice).
• AGPAL accredited.
• Training Practice for GP Registrars.
• Independent Contractor Agreement with high income potential
• Incentivised opportunity for FRACGPs interested in providing supervision to training GP’s.
Requirements:
For a confidential discussion please contact Dr Raf Francikiewicz on 0424436663 or email raf@bullsbrookmedicalcentre.com.au

Are you a GP seeking an exceptional opportunity in Perth’s bustling CBD? Look no further! Doctor Northbridge, a private doctor-owned practice, is offering a dynamic VR GP position in one of the city’s most sought-after locations. Our state-of-the-art medical centre, nestled within heritage-listed buildings, boasts top-notch facilities and a supportive environment.
Enjoy the perks of:
High-earning potential with private billing
Highly-trained administrative team
Private billing practice with excellent earning potential
On-site parking and convenient proximity to Perth CBD
Strong nursing support and low Did Not Attend (DNA) rate
With over 100 new patients a week and effective marketing strategies driving growth, Doctor Northbridge is the perfect place to advance your career. Join us and be part of a collegial environment dedicated to excellence in patient care.
Contact us today to learn more and schedule a visit!
Dr Yoon Low | Phone: 0431299328 Email: careers@drnorthbridge.com.au www.drnorthbridge.com.au







Spectrum Health has a team of professional and skilled managers with many years of industry experience who ensure the seamless and successful operation of medical practices.
Dr Vishnu Gopalan, the Chairman of Spectrum Health helms an expansive network of medical centres with a
strong intent to build genuine partnership with
The Spectrum Health team welcomes the opportunity to partner with you in general practice.




