• • • •


• • • • •










NeuromuscularElectricalStimulationasaNovelTreatmentofDysphagia:A Meta-AnalysisofEfficacyandSafety
ArnoldKeane1,DerrenDavidChristianHomentaRampengan2 , JoshNatanielJowono1,JessieLaurenciaAffaratu1
AMSA-UniversitasIndonesia1,AMSA-UniversitasSamRatulangi2
Introduction:Dysphagiaisacommonanddebilitatingconditionthatimpairsnormal swallowingfunction.Researchindicatesthat15-22%ofadultsover50experienceit,with hospitalandlong-termcarefacilitiesshowinganincreasedrateof40-60%.Dysphagiacan causemalnutrition,dehydration,aspirationpneumonia,andsocialisolation,significantly reducingthepatient'squalityoflife.However,currenttreatmentapproaches,including compensatorystrategies,posturaladjustments,andexercises,havelimitedefficacy.Asa result,alternativetherapiesarebeingexplored,withnosystematicreviewormeta-analysis evaluatingneuromuscularelectricalstimulationasatreatmentfordysphagia.
Objectives:Todeterminetheeffectivityofneuromuscularelectricalstimulationfor improvingswallowingfunctionindysphagiapatient
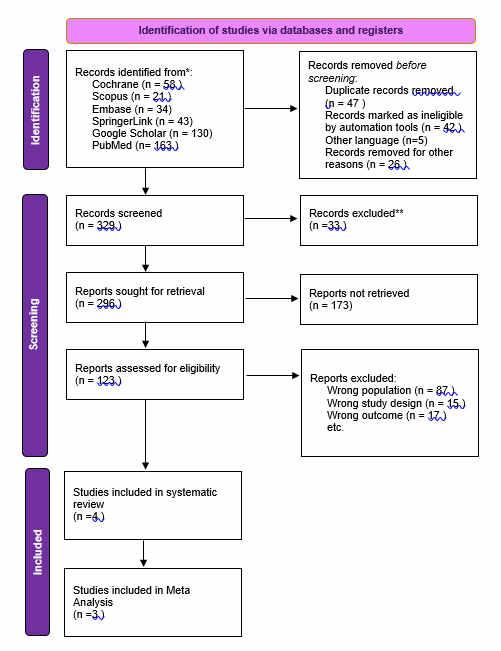
Method: ThisstudywasconductedusingthePreferredReportingItemforSystematic ReviewandMeta-analysis(PRISMA).WesystematicallysearchedPubMed,Cochrane, Embase,andScienceDirectforliteratureupto4April2023.Theincludeddocumentswere screenedandassessedforriskofbiasusingtheCochraneRiskofBias2.0.Effectestimates werepooledusingrandom-effectsmeta-analysisusingReviewManager5.4.
ResultsandDiscussion: Fourteenstudiesculminatingatotalof743participantswere includedwithlowriskofbias.Neuromuscularelectricalstimulation(NMES)depictsa significantswallowingfunctionrecordedbyPenetration-AspirationScale(PAS)(HR=1.97; Z=4.21;p=0.002;95%CI:0.39-9.86)andFunctionalOralIntakeScale(FOIS)(HR=2.79; Z=4.1;p=0.0002;95%CI:1.29-6.03).Moreover,NMESalsoimprovedpatientlifein generalbyloweringthepainscoreandincreasingthequalityoflife.
Conclusion: NMEStherapyshowsamoresignificantimprovementinoralfunctionon dysphagiapatientscomparedtotraditionaltherapy.Therefore,NMEScanbeanexcellent choiceoftherapyfordysphagiaandrecommendedtobeusedindysphagiaguidelinesas supportivenon-pharmacologicaltherapy.
Keywords: elderly,neuromuscularelectricalstimulation,dysphagia,swallowingfunction
Neuromuscular Electrical Stimulation as a Novel Treatment of Dysphagia: A Meta-Analysis of Efficacy and Safety

Arnold Keane, Derren David Christian Homenta Rampengan, Josh Nathaniel Jowono, Jessie Laurencia Afaratu
Introduction

Dysphagia is an impairment of normal swallowing function, 15-22% on >50 years old 40-60%
Increased in Nursing Homes or Facilities
Significant impact on quality of life, such as

Current therapeutic approaches (e.g. compensatory swallowing strategies, postural adjustment, exercises) ARE NOT effective in many cases
Objective
To determine the effectivity of neuromuscular electrical stimulation (NMES) for improving swallowing function in dysphagia patient.
Methods
JNJ and AK extracted data independently, DD rechecked the data accuracy while conducting statistical analysis.
Keywords
("Neuromuscular Electrical Stimulation" OR "NMES") AND ("dysphagia" OR "swallowing disorder") AND ("elderly" OR "older" OR "older adults)

results and discussions
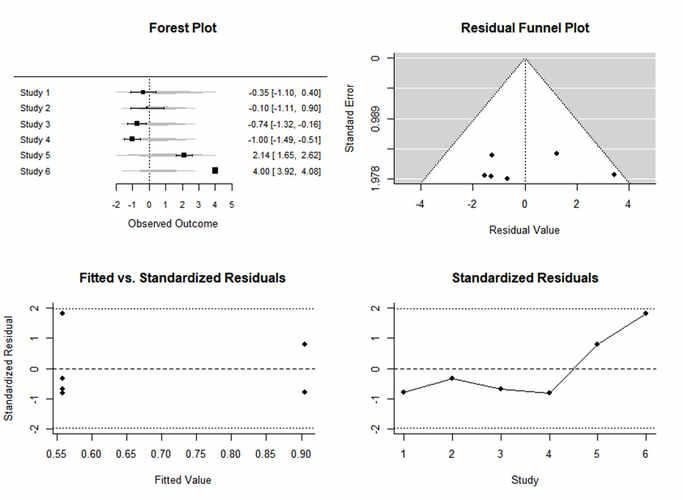
The Source of high heterogeneity was found in App 2. with R square values ranged from 5060% and variables are significant (p<0.05)
NMES are more effective when combined with TDT and TSTP

DSRS, VAS, DOSS, SWAL-Qol, NIHSS and mRS are found to be improved as well, yet needed more research
NMES uses a non-invasive, easily used, and efficient application method NMES focused on improving pharyngeal phase of swallowing and hyoid movement which can be combined by other stimulation methods and improved by resistance training
Its effect on Type II Muscle Fibers factors for muscle strengthening in long period which positively affects skeletal muscle rehabilitation
The first systematic review and meta-analysis with meta-regression analysis in assessing NMMES effect on oral function in dysphagia patient




All studies are RCTs
CONClusions
NMES therapy shows a more significant improvement in oral function on dysphagia patients compared to traditional therapy. Therefore, NMES can be an excellent choice of therapy for dysphagia and recommended to be used in dysphagia guidelines as supportive non-pharmacological therapy.
There is no conflict of interest
Only English Studies are retrieved 1 2 3 4 5,6 4,5 10,14,16,18 8 11,14 16,17

References and appendix

Databases PubMed, Cochrane, EMBASE, Science Direct Bias assessment using Cochrane RoB 2.0 Meta Regression Analysis are run using Review Manager 5.4 Randomized Controlled Studies Elderly with Dysphagia Retrievable full-text 1. 2. 3. Inclusion Criteria Incomplete outcome report Non-english literature 1. 2. Exclusion Criteria SWALLOWING FUNCTION QUALITY OF LIFE ADVANTAGES of NMES
Strength Limitation Z score= 4.21 overall HR of 1.97 95% CI range 0.39-9.86 Z score = 4.10 overall HR of 2.97 95% CI range 1.29 - 6.03 p= 0.0002 p= 0.002 Malnutrition Dehydration Aspiration Pneumonia Social Isolation
sEMG/Trace FOIS PAS
Table 1. Baseline demography Characteristics, Interventions and outcomes reported in each included studies
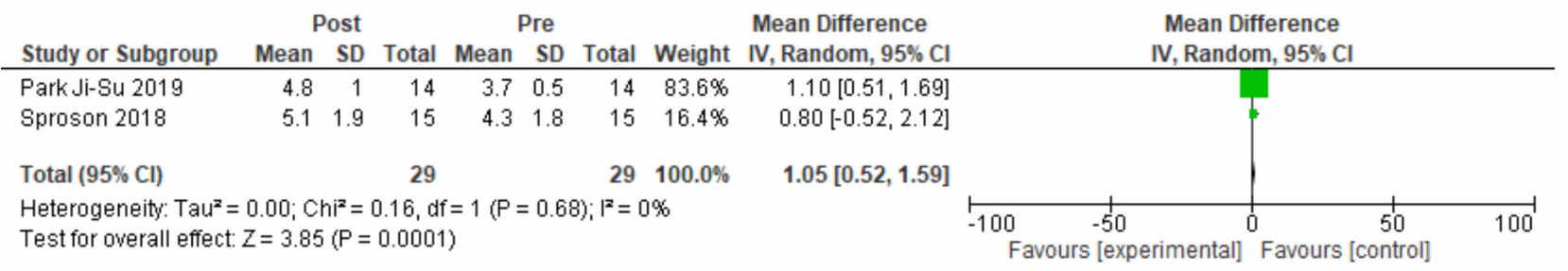
Fig 2. Forest Plot of NMES Within intervention group before and after Meta-Analysis for PAS
Fig 3. Subgroup Analysis of NMES Within intervention group before and after Meta-Analysis For PAS
Fig 4. PAS; Assessment of publication bias and residual diagnosis
Fig 5. Forest Plot of NMES Within intervention group before and after Meta-Analysis for FOIS
Fig 6. Subgroup Analysis of NMES Within intervention group before and after Meta-Analysis For FOIS
Fig 7. FOIS; Assessment of publication bias and residual diagnosis
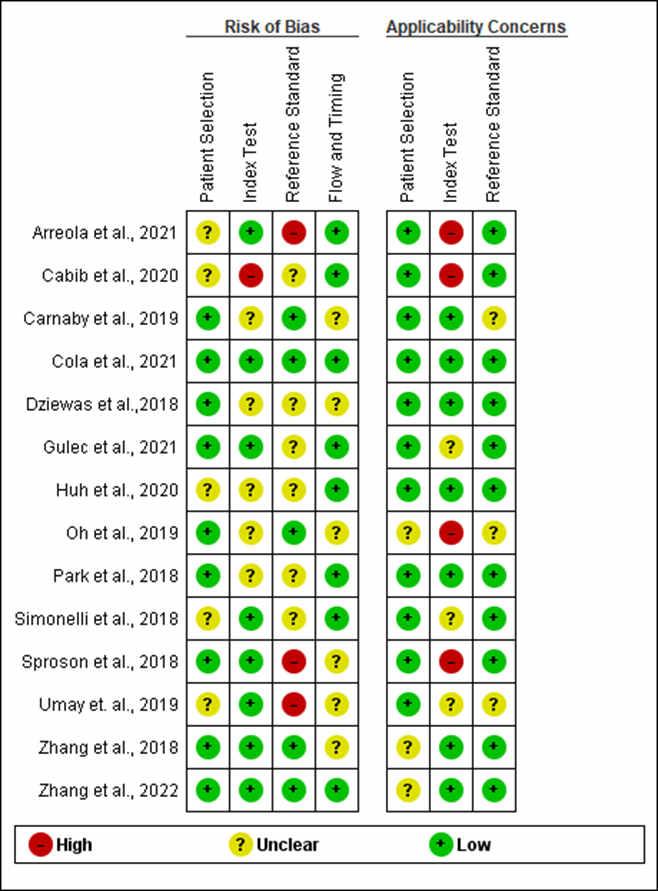
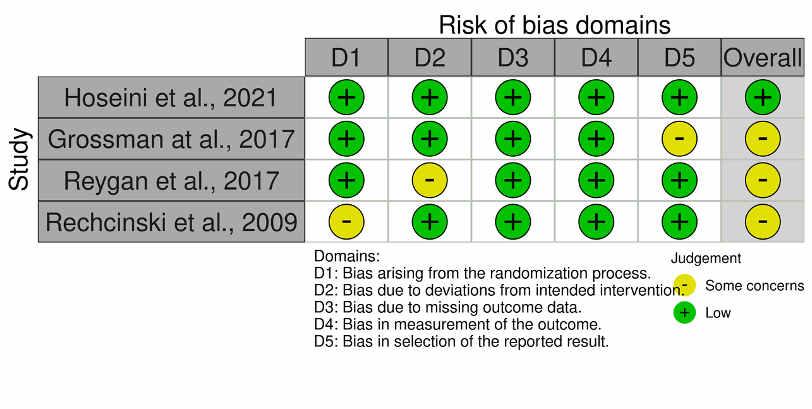
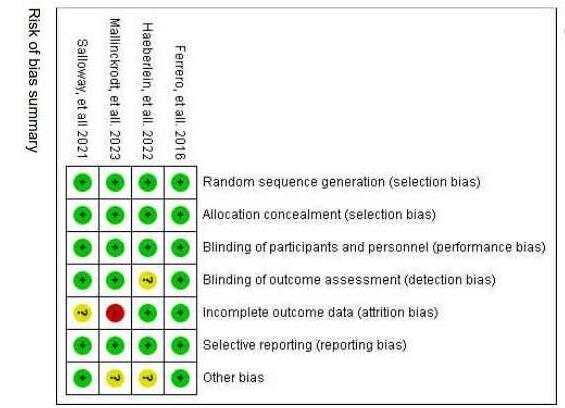
Fig 9. Risk of bias and applicability concern percentage of the assessment
Fig 8. Risk of bias and applicability concern summary graph
Fig 1. PRISMA flow for literature search strategy
Large sample size with various underlying conditions (stroke and parkinsons There is no conflict of interest and acknowledgements within this study.
EffectivenessAndComparisonBetweenLandAndWaterExercisesAsTreatmentFor Osteoporosis:ASystematicReviewAndMeta-Analysis
GabriellaSachikoJanneshaSudirman,DerrenDavidC.H.Rampengan,PutriUtamiLestari, KeishaHanifaAlmaMayra
Introduction: Osteoporosisisapervasiveglobalhealthissuecharacterisedbylowbone mass,deteriorationofbonetissue,andincreasedbonefragility.InternationalOsteoporosis Foundationestimatesthatover200millionpeopleworldwideareaffected.Therefore,itis significanttoidentifytheeffectivepreventionandtreatmentstrategiestoprevent osteoporosis,oneofwhichisexercise.
Objective: Thissystematicreviewandmeta-analysisisaimedtocomparetheeffectiveness betweenlandandwaterexercisesinosteoporosismanagement.
Method: ThisstudyfollowedthePreferredReportingItemsofSystematicReviewand Meta-Analysis(PRISMA)onseveraldatabases,namelyPubMed,ScienceDirect,Wiley,and GoogleScholar.Ameta-analysiswasconducted,whichassessesthedataextracted,resulting in10studiesthatwereincluded.
Results: Tentrialsareincludedintherandomeffectmeta-analysisofefficacyofland-based exercisecomparedwithwater-basedexercise.Theresultssuggestthatland-basedexercise woulddecreasetheoddsofpostmenopausalwomenexperiencingosteoporosis(OR=0.47, 95%CI;0.23to0.96,p–value=0.04).However,thesubgroupmeta-analysisofthefour proxythatmeasureBoneMineralsdensityaftertheinterventionshowsthat,landbased exercisehasnosignificanteffectonthetotalBMD(SMD=0.34,p=0.20),FemoralNeck BMD(SMD=0.29,p–value=0.50),LumbarSpineBMD(SMD=0.06,p–value=0.91) andTotalhipsBMD(SMD=0.01,p–value=0.94)incomparisonwithwaterbased exercise.
Conclusion: Alltypesofland-basedexercisesarebetterinimprovingosteoporosisthan water-basedexercises.However,itisstillrecommendedthatosteoporosispatientsarealso providedwithcalciumandvitaminDsupplementstohelpimprovebonemineraldensity.
Keywords: landexercise,waterexercise,osteoporosis,bonehealth

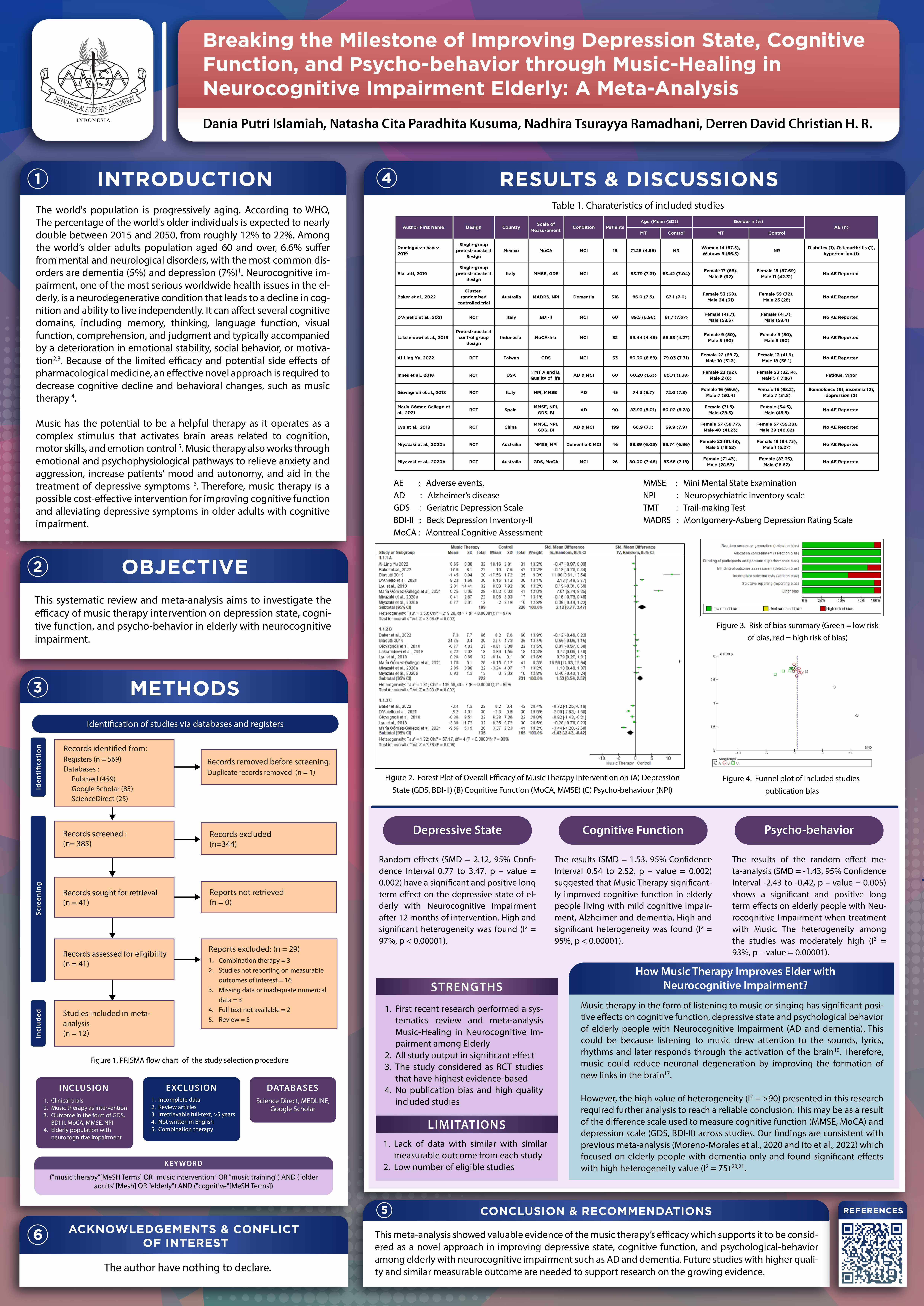
BREAKING THE MILESTONE OF IMPROVING DEPRESSION STATE, COGNITIVE FUNCTION, AND PSYCHO-BEHAVIOR THROUGH MUSICHEALING IN NEUROCOGNITIVE IMPAIRMENT ELDERLY: A METAANALYSIS
1Faculty of Medicine, Universitas Sriwijaya, 2Faculty of Medicine, Universitas Tarumanagara, 3Faculty of Medicine, Universitas Sam Ratulangi
Introduction: Global population aging and Neurocognitive impairment are becoming one of the most significant issues in the elderly. Among the world’s older adult population aged 60 and over,6.6%sufferfrommental andneurological disorders,withthe most commondisorders being dementia (5%) and depression (7%). It can affect several cognitive domains and leads to a decline in cognition and the ability to live independently. Because of the limited efficacy and potential side effects of pharmacological medicine, an effective novel approach is required to decrease cognitive decline and behavioral changes, such as music therapy.
Objective: To investigate the efficacy of music therapy intervention on depression state, cognitive function, and psycho-behavior in elderly with neurocognitive impairment.
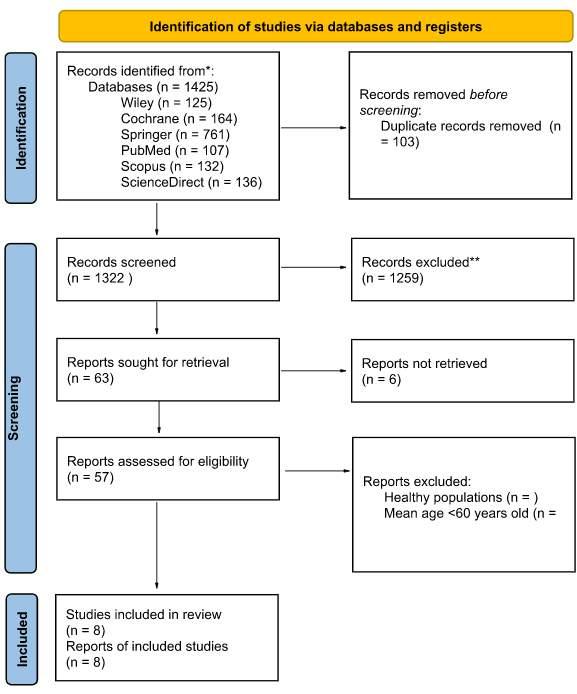
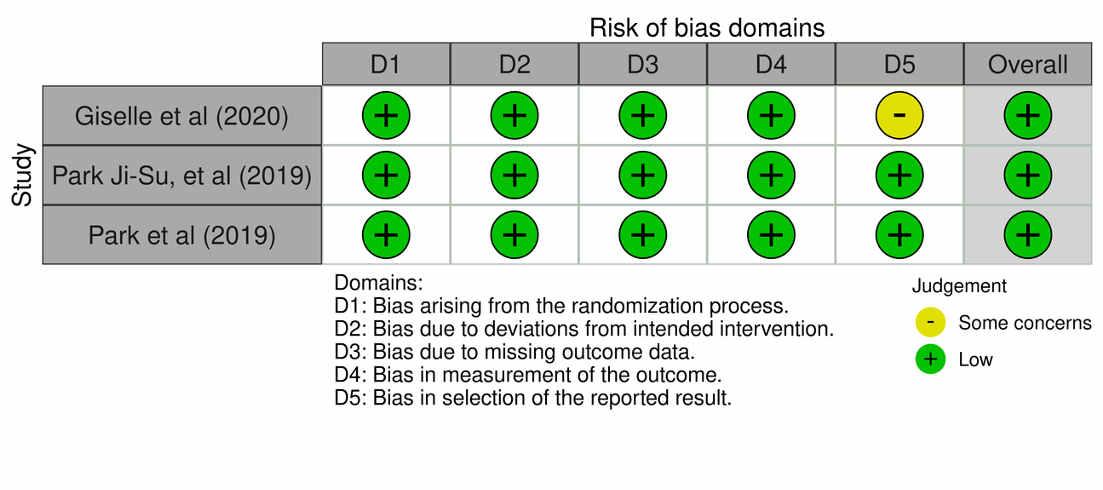
Methods:Thisstudy wasconductedusingthe(PRISMA)guidelinebasedonourPICOcriteria. Several sources of literature including Pubmed, Google Scholar, ScienceDirect were systematically searched up 2018-2023 based on our inclusion and exclusion criteria. The selected studieswerethoroughlyscreenedandevaluatedfor potential biasusing Cochrane Risk of Bias 2.0. Random-effect meta-analysis was performed using Review Manager 5.4. Result: Twelve trials involving 1000 patients were included in this study. Meta-analysis was performed in three groups. We found that depression state (SMD = 2.12, 95% CI 0.77 to 3.47, p – value= 0.002, I2 = 97%), cognitive function SMD = 1.53, 95% CI 0.54 to 2.52, p – value = 0.002,I2 = 95%), and psycho-behavior(SMD= -1.43, 95%CI -2.43 to -0.42,p – value = 0.005, I2 = 93%) are significantly improved after music therapy intervention on elderly with neurocognitive impairment.
Conclusion: This study showed evidence of the efficacy of music therapy in improving depression state, cognitive function, and psychological behavior among elderly with neurocognitive impairment.
Keywords: Music therapy, Depression, Cognitive, Psycho-behavior, Elderly, Neurocognitive Impairment
Dania Putri Islamiah1, Natasha Cita Paradhita Kusuma2, Nadhira Tsurayya Ramadhani1 , Derren David Christian Homenta Rampengan3
EffectivenessofOralExerciseforImprovingDysphagiainGeriatricProblems:ASystematic ReviewandMetaAnalysis
Introduction: Difficultieswithswallowing(dysphagia)areacommonsymptomfoundin elderlypatients.Thetwoprominentdiseasesassociatedwithdysphagiaintheelderlyare Parkinson'sdisease(PD)andpost-stroke,whichaffectmorethan80%and50%ofpatients, respectively.Rehabilitativeoralexerciseprogramsremainarecommendedchoicetooptimize swallowingfunctionbecausetheycanbeeasilyconductedinashortperiodoftimeand independentlyathome,makingthemmoreefficientandconvenientfortheelderlypatients. Furthermore,thereisnosystematicreviewandmeta-analysisthatspecificallyanalyzesthe effectivenessoforalexerciseprogramsinelderlypatientsthroughparticularaspectsof swallowingfunction.
Objective: Tocomparetheoutcomesoforalexerciseprogramsrelatedtoswallowing functionspecificallyinmultipleaspectsintheelderlywithgeriatricproblems.
Methods: Thisstudysystematicallysearchedpublishedclinicaltrialsaboutrelevanttopics withinthepast10yearsaccordingtothePreferredReportingItemsforSystematicReview andMeta-analysis(PRISMA)guideline.Includeddocumentswerefurtherassessedforriskof biasusingRoB2.0forRandomizedControlledTrial(RCT)andROBINS-Ifornon-RCT. QuantitativeanalysiswasconductedusingReviewManager5.4.
ResultsandDiscussion: Comparedtocontrol,oralexercisesignificantlyimprovesoral functionbasedontheFunctionalOralIntakeScale(FOIS)withameandifferenceof1.9(p 0.0001,95%CI:1.17-2.63;I2=0%).Furthermore,otherparameterssuchasQoL(mean difference22.61[p=0.12,95%CI:-5.68--50.90;I2=92%]),anteriortonguestrength(mean difference7.04[p=0.00001,95%CI:4.76--9.32;I2=0%]),andPAS(meandifference-1.14 [p=0.00001,95%CI:-1.51-(-0.77);I2=2%])alsoshowbetterresults.
Conclusion: Oralexerciseprogramsareproventoimproveswallowingfunctionindysphagia patients(PDandpost-stroke)invariousaspects.
Keywords: oralexercise,dysphagia,swallowingproblem,geriatricproblems,elderly.
Effectiveness of Oral Exercise for Improving Dysphagia in Geriatric Problems: A Systematic ReviewandMeta-analysis
Introduction
Difficulty swallowing, medically known as dysphagia, is a common symptom found in the elderly, of which two areParkinson'sdisease (PD) and post-strokepatients.
>80% ParkinsonDisease (PD)patients
>50%Post-strokepatients
Develop dysphagia which may lead to complications, such as pneumonia and impaired nutrition intake.
Rehabilitation programs can be easily conducted in a relatively short period of time as well as independently at home, making them more efficient and convenient for the elderly patients.
There is no systematic review and meta-analysis that specifically analyzes the effectiveness of oral exercise programs in elderly patients through particular aspects of swallowing function.
Objective
To compare the outcomes of oral exercise programs related to swallowing function specifically in multiple aspects (functional oral intake, quality of life, penetration-aspiration, and tongue strength) in elderly with geriatric problems.
Methods
Keywords: (oral exercise OR tongue exercise OR mouth exercise OR jaw exercise OR oral training OR tongue training OR mouth training OR jaw training) AND (dysphagia OR deglutition disorders OR swallowing problems OR difficulty swallowing) AND (elderly OR aged OR elder OR older OR geriatric)
Databases: Wiley, Cochrane, Springer, PubMed, Scopus, ScienceDirect
InclusionCriteria:
RCT and clinical trial
Post-stroke or Parkinson's Disease elderly patients mean age ≥ 60 years old receiving oral exercise programs
English language Studies from 2013 – 2023
ExclusionCriteria:
Inaccessible full text Incompleteoutcomedata
Bias Assessment: ROBINS-I for non-RCT and Cochrane RoB 2 for RCT
Statistical analysis: Review Manager 5.4
Results & Discussion
Oral exercise significantly improves oral function based on the Functional Oral Intake Scale (FOIS) with a mean difference of 1.9 (p 0.0001, 95% CI: 1.17-2.63; I2 = 0%) compared to control.
Other parameters such as QoL (mean difference 22.61 [p = 0.12, 95% CI: -5.68--50.90; I2 = 92%]), anterior tongue strength (mean difference 7.04 [p = 0.00001, 95% CI: 4.76--9.32; I2 = 0%]), and PAS (mean difference -1.14 [p = 0.00001, 95% CI: -1.51-(-0.77); I2 = 2%]) also show better result compared to control.

OutcomeMeasures
FunctionalOralIntakeScale(FOIS)
A scale to quantify the variety and amount of oral intake versus tube feeding.
RosenbekPenetration-AspirationScale(PAS)
A scale to evaluate the presence and severity of any penetration/aspiration of contrast.
Swallow-relatedQualityofLife(SWAL-QoL)

Patient's ratings of dysphagiadomains and its impactonQoL AnteriorTongueStrength


Assessed by using the the Iowa Oral Performance Instrument to assess the maximum isometric tongue pressures (MIPs) of the anterior and posterior tongue.
Strengths
First systematic review & metaanalysis specifically assessing oral exercise programs for elderly patients with dysphagia in multiple aspects related to swallowingfunction.
All study output improves in the interventiongroup.

Limitations
Some of the studies are pilot and preliminary studies. Heterogeneity found in one of the studies.
The implementation of oral exercise programs has been proven to improve swallowing function in dysphagia patients (PD and poststroke) in various aspects. Further meta-analysis studies are recommended to evaluate the effectiveness of oral exercise programs on particular aspects of swallowing function and integratedintoastructuredguideline.
ScanthisQRcodefor moreinformation
 Introduction
Defin Allevia Yumnanisha, Mukhlis Akmal Taher N, Elvina Firdaus, Kelvin Kohar
Introduction
Defin Allevia Yumnanisha, Mukhlis Akmal Taher N, Elvina Firdaus, Kelvin Kohar
bit.ly/AppendixOralExerciseDysphagiaDAYMATNEFKK More?
Figure1.ROBINS-1forNon-RCT
Figure3.FOIS Intervention
Figure4.FOIS Control
Thereisnoconflictofinterestandacknowledgementsinthisstudy.
Table 1.Summary of Results
Figure2.CochraneRoB2forRCT
Efficacy and Safety of Melatonin Supplementation on Regulating Blood Pressure in Elderly with Cardiovascular Disease: A Systematic Review and Meta-Analysis
Muhammad Syifaul Afnan1, Tsabita Nafisa1, Ni Putu Desya Chandraka Dewi1, Syanda Aisyah1
1Faculty of Medicine, Jember University, Jember, Indonesia
ABSTRACT
Introduction: Cardiovascular disease has a higher prevalence in the elderly, with hypertension as the highest risk factor. In elderly, the amount of melatonin decreases due to aging, lowering sleep quality. Studies have proven that aging, sleep quality, and hypertension have close relationship. There are currently no hypertension guidelines representing elderly. Previous studies have shown that melatonin has good efficacy and safety as an antihypertensive agent.
Objective: This study aims to review the efficacy and safety of melatonin supplementation on regulating systolic and diastolic blood pressure in elderly.
Materials and Methods: This study was reported based on criteria from Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). And already registered to International Prospective Register of Systematic Review (PROSPERO) with ID CRD42023407389. The study search process was carried out on various databases. The bias assessment was carried out using RoB 2.0 tools. Mean and Standard deviation (SD) with a 95% confidence interval (CI) were used to determine the association between melatonin supplementation and blood pressure reduction. The Fixed and Random effect model was used based on the level of heterogeneity, and a p-value of 0.05 was interpreted as a statistically significant result.
Results: Four studies were included through qualitative analysis, and three of them were for quantitative analysis. A recent study showed that Melatonin supplementation in the elderly with cardiovascular disease had promising results with a significant reduction in SBP (Pooled MD=-2.44, 95% CI (-4.80, -0.07), p=0.04, I²= 47%). However, it was found that there was no significant decrease in DBP (Pooled MD=-0.51, 95% CI (-3.12,2.11), p=0.11, I²= 56%). Melatonin supplementation has been studied and received a thorough agreement regarding its non-toxicity so that it is safe to use if it is still under the maximum dose.
Conclusion: Melatonin supplementation significantly reduced SBP but not considerably reduce DBP.
Keywords: Melatonin, blood pressure, cardiovascular disease.
Supplementary: https://linktr.ee/scipostamsc2023
Efficacy
and
Safety of
Melatonin





Supplementation
on Regulating Blood Pressure in Elderly with Cardiovascular Disease: A Systematic Review and Meta-Analysis
Current guidelines do not represent elderly population → cause burden, exacerbates comorbidities, and causes adverse events due to drug interaction. Melatonin cause vasodilatation, inhibit sympathetic nerve, improves sleep quality, and has antioxidant properties → potentially effective and safe antihypertensive agent.
"There were no systematic reviews and meta-analyses assessing Melatonin affection and safety on elderly with CVD"
OBJECTIVE
To determine the effectiveness and safety of Melatonin for regulating blood pressure in elderly with cardiovascular disease (CVD).
METHODS & MATERIALS
DATABASE
Cochrane, Scopus, Embase, SpringerLink, Google Scholar, PubMed.
Bias assessment using Cochrane RoB 2.0.

Random-effectandFixed-effectmetaanalysisusingReviewManager5.4.
Prospero ID CRD42023407389.
Inclusion Criteria
1. RCT design.



2. Population elderly with CVD.

3. Assess Blood Pressure (SBP and DBP).
4. Melatonin supplementation.
Exclusion Criteria
1. Irretrievable full text.
2. Non-English language study.
KEYWORDS
"Melatonin" AND "Blood Pressure" AND "Cardiovascular Disease"
RESULTS
EFFICACY FOR REGULATING SBP
Pooled MD = -2.44, 95% CI (-4.80, -0.07), P = 0.04, I² = 47%
EFFICACY FOR REGULATING DBP
Pooled MD = -0.51, 95% CI (-3.12,2.11), P = 0.11, I² = 56%





SAFETY
3. Did not report any changes in Blood pressure.
Table 1. Characteristic and Outcome of Studies
This result showed a significant effect of melatonin supplementation in regulating SBP. From studies by Raygan et al., 2017 and Grossman et al., 2006 showed a significant decrease in SBP and potential treatment for some CVD, which marks the potential effect of melatonin as cardioprotective. Two studies by Hoseini et al., 2021 and Rechcinski et al., 2009 showed non-significant effects. Those might be affected by the unbalanced diuretics, and betablocker use between the 2 groups and drug interaction. This interaction results in lower efficacy of melatonin.

Melatonin showed promising effects in regulating DBP, yet this result is insignificant. This is due to a greater decrease in placebo group in a study by Grossman et al., 2006. In spite of that, a previous study stated that an increase in DBP is aligned with arterial stiffness due to aging. Therefore, SBP is a better predictive factor than DBP.

All included studies showed no adverse event in Melatonin supplementation as long as melatonin supplementation is below 10g/day. Previous human and animal studies also showed the non-toxicity of melatonin.
STRENGTH AND LIMITATION
Although our study has limitations, this is the first systematic review and meta-analysis that analyzes the potential of melatonin supplementation in regulating blood pressure to manage cardiovascular disease among the elderly. Furthermore, some of our included studies fall into the category of concerns in analysis risk of bias which proves the reliability of this study. Our result showed that melatonin had significant and promising efficacy and low heterogeneity. Thus, this review can be a shred of strong evidence for cardiovascular disease guidelines, specifically for the elderly.

RECOMMENDATIONS
We recommend conducting further studies regarding the characteristics and relationships with melatonin supplementation in blood pressure regulation in the elderly with cardiovascular disease of longer duration to see the long-term effects of melatonin supplementation in the elderly. Also, we recommend that future studies consider other confounding variables.
CONCLUSIONS
This systematic review and meta-analysis provide valuableevidencethatmelatoninhasafavourableeffect on regulating blood pressure among elderly with cardiovasculardisease.
We are grateful to our family and friends that supported us and also to our seniors for advising us throughout creating this systematic review and meta-analysis. The authors declare no conflict of interest.
Muhammad Syifaul Afnan, Tsabita Nafisa, Ni Putu Desya Chandraka Dewi, Syanda Aisyah
[10,11]
Figure 1. PRISMA Flow Chart
Figure 2. Risk of Bias
Figure 3. Meta-analysis Forest plot of the effect of Melatonin Supplementation treatment in elderly patients with cardiovascular disease based on SBP change score.
Figure 4. Meta-analysis Forest plot of the effect of Melatonin Supplementation treatment in elderly patients with cardiovascular disease based on DBP change score.
ACKNOWLEDGEMENTS
REFERENCES
75% Need urgent treatment and management of risk factors Preventing hypertension as CVD major risk factor has proven to have good benefits in managing CVD
Melatonin decrease sleep quality Hypertension[4-6] [1, 2] [3] [5, 7] [8,9] [14] [14] [13] [12] [8] linktr.ee/scipostamsc2023
DISCUSSIONS
ExploringTaiChiEfficacyasaNon-InvasiveTreatmentofMildCognitiveImpairmentin Elderly:AMeta-AnalysisofClinicalOutcomes
FeliciaAngelicaGunawan1,DerrenD.C.H.Rampengan1,JuanA.J.M.Nuralele2 , JadeAudreyH.Rampengan3
AMSA-UniversitasSamRatulangi1,AMSA-UniversitasKristenIndonesia2 , AMSA-UniversitasAtmajaya3
ABSTRACT
Introduction MildCognitiveImpairment(MCI)isadecliningcognitivestatebetweennormal aginganddementia,wherethereisadeclineinmemoriesandthinkingabilitieswithinage.There arenoeffectivemedicationsapproved,but evidencefromrandomizedclinicaltrials(RCTs) indicatedthat TaiChiiscapableoftraining,postponing,counteracting,andimprovingcognitive functioninindividuals,especiallyinelderswithMCI.
Objective ThisstudyaimedtoassessthepotencyofTaiChiasoneofthealternative non-invasivetreatmentsfortreatingelderlypatientswithMCI.
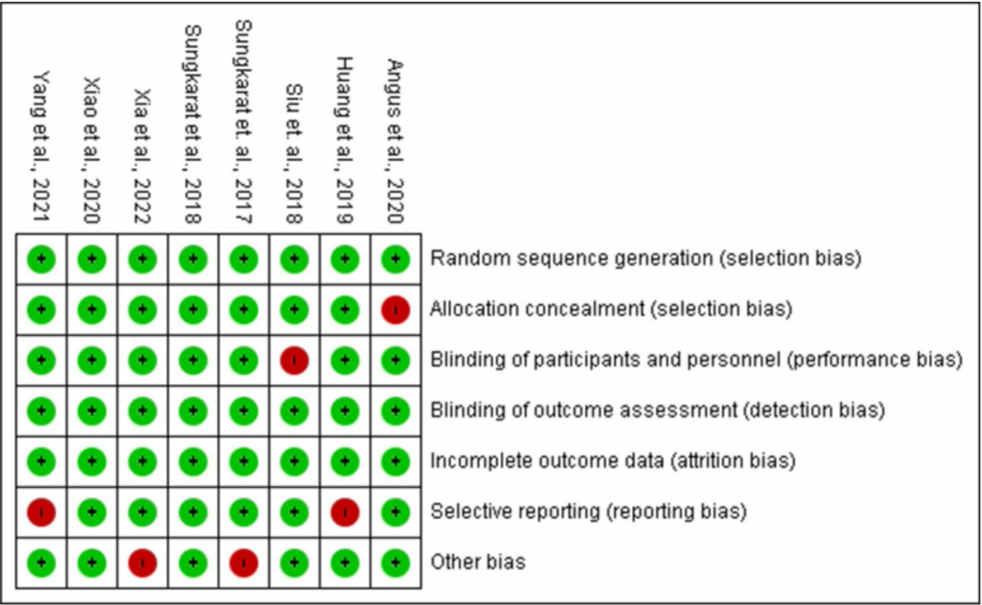
Method ThisreviewarecomposedofstudiesgeneratedfromPubMed,ScienceDirect, EuropePMC,andClinicalKey.Theriskofbias(ROB)qualityassessmentwasemployed, justifyingthatalltheincludedstudiesarealowriskofbias.ReviewManager5.4.1wasutilized fordataextraction,resultingineightstudiesincludedinthisstudy.
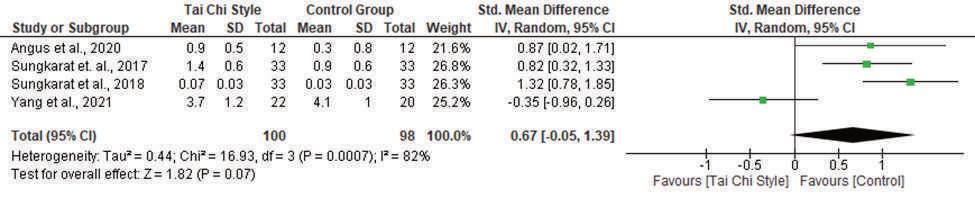
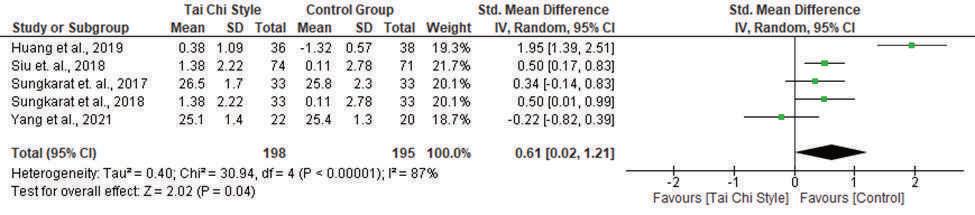
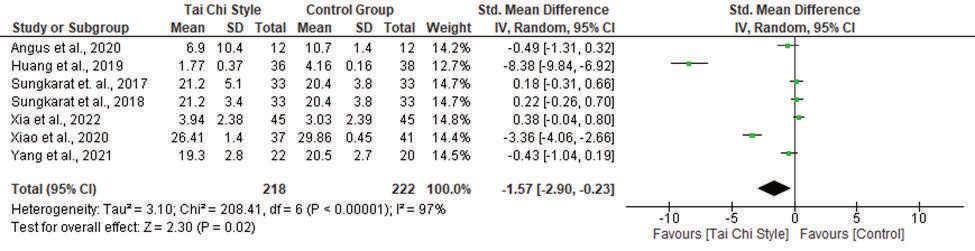
Results EightRandomizedControlTrialswith661participantsareincludedinthis meta-analysis.SeventrialsassessedthroughMontrealCognitiveAssessment(MoCA)scores meta-analysissuggestthatTaiChiinterventionimprovedcognitivefunctionandreducedtherate ofcognitiveimpairmentinelderlypatients(SMD=-1.57,95%Confidenceinterval-2.90to -0.23,p–value=0.02)comparedtothecontrolgroupafter24weeksofintervention.Inthe Meta-analysisofMMSE,fivetrialswereincluded.TheresultsalignwiththeMoCAtestasTai Chiinterventionimprovedcognitivefunctionandslowdowntherateofcognitiveimpairmentin elderlypatients(SMD=0.61,95%Confidenceinterval0.02to1.21,p–value=0.04)compared tothecontrolgroup.
Conclusion Thissystematicreviewandmeta-analysisprovidestrongevidenceforTaiChi efficaciousnessasTaiChiisabletoimprovecognitivefunctionandslowdowntherateof cognitiveimpairmentinelderlypatients,asshownbyboththeMoCAscoreandMMSE.
Keywords:Elderly,MildCognitiveImpairment,Non-InvasiveTretament,TaiChiExercise
ExploringtheEfficacyofTaiChiasaNon-Invasive TreatmentofMildCognitiveImpairmentinElderly:A SystematicReviewandMeta-AnalysisofClinicalOutcomes
FeliciaAngelicaGunawan,DerrenD.C.H.Rampengan, JuanA.J.M.Nuralele,JadeAudreyH.Rampengan
MildCognitiveImpairment(MCI)isadecliningcognitivestatebetween normalaginganddementia,wherethereisadeclineinmemoriesandthinking abilitiesthathappenwithinage1.Apparently,thereisnoexactcausefor developingMCI2.AccordingtoCohortStudiesofMemoryinanInternational Consortium(COSMIC),MCIprevalenceisestimatedtoberangingfrom 6–12%globally3.ItisimportanttonotethattheprevalenceofMCIislikelyto increaseinthecomingyearsduetotheagingoftheglobalpopulation. Therefore,itiscrucialtodevelopeffectivestrategiesto preventordelayits progressiontowardsdementia.

Asoflate,therearenoeffectivemedicationsapproved2,but accumulating evidencefromrandomizedclinicaltrials(RCTs)indicated thatphysicalactivity couldbenefitthecognitivefunctionsinMCIpatients.Accordingtostudies,the processofmovementactuatestherelevantbrainareasandstimulatesthe excitabilityofbraincells,whichishelpfultostrengthen thebrain,maintainits perceptualfunctions,andimprovethememoryoftheelderly4 Studies proposethatTaiChiisoneofthebeststrategiestopreventMCI.


TaiChiiscapableoftrainingcognition,postponing,counteractingthe detrimentaleffectsofneurocognitiveillnesses,andimprovingcognitive functioninindividuals5 However, TaiChidiffersfromothertypesofexercise inseveralrespects,asTaiChiincorporatesthetheoryoffivetraditional Chinesemedicineelements,whichconsistofwater,wood,fire,metal,and earththatbecomethefoundationforeachmovement.Italsocombines physicalmovementwithrespiration,mindwithconsciousness,consciousness withthebody,andqiwiththebody4.ThenoveltyofusingTaiChiasa treatmentforMCIliesinitsuniquecombinationofphysical exerciseand mind-bodypracticethatcanbeadaptedtodifferentlevelsofphysicalability, whichmayhavelimitationsinmobilityorbalance.Thismind-bodyexerciseis non-invasiveandcanbeeasilyadaptedforanyone,especiallyelderlypatients.
OBJECTIVES
ThisstudyaimedtoassessthepotencyofTaiChiasoneofthealternative non-invasivetreatmentsfortreatingelderlypatientswithMCI.
METHODS
SystematicReviewandMeta-AnalysisbasedonPRISMA
StatementGuidelines
Keywords:("TaiChi")AND("MildCogdnitiveImpairment") OR("MCI")AND("Elderly")OR('GeriatricPatients")

8RandomizedControlTrialacrossAsianCountries andAustralia

Riskofbiasassessment:ROB;Meta-analysis:: RevMan5.4.1



TheMeanDifferenceiscalculatedwithaconfidence intervalof95%. P<0.05 wasconsideredsignificant

LIMITATIONSOFTHESTUDY
•ProvingtheefficacyofTaiChi impementationforelderly patientwithMCI
•Lowriskofbias
•RCTasinclusioncriteria


ACKNOWLEDGEMENTSAND CONFLICTOFINTEREST
•Smallnumberofstudies
•Languangerestrictions
•Highheterogeneitydueto differentfollow-uptimes







CONCLUSION
RESULTS
DISCUSSION
TaiChiExerciseandMildCognitiveImpairment
Findings: Ourmeta-analysisshowsthatthereisalowriskofbiasandsignificantresultsshownthroughthe MMSEandtheMoCAscaleandMMSEbetweentheTaiChitraininggroupandthecontrolgroupasboth showingimprovementsincognitivefunctionandreducingtherateofcognitiveimpairment.The improvementssuggestedbyourfindingsmightbearesultofbodymovementrecall,taskswitching,and visuospatialprocessingsimultaneouslywithbodymovementduringTaiChitraining.
PreviousMeta-analysis: Theresultsofthismeta-analysisisconsistentwithastudyconductedbyWayneet al,whichreportedimprovementsinglobalcognitivefunctionafter12weeksto24weeksofTaiChitraining inelderlypatientswithmildcognitiveimpairment14
•TheimprovementoftheTaiChiInterventiongroup manifestedsignificantresultsinMMSE.Taichi isshowntohaveimprovedawiderangeofcognitivecomponents,including attention,language, memory,orientation,andvisuospatialproficiencyintheinterventiongroup.MMSEhas asensitivity of81%andspecificityof89%15
•TheMoCAscalealsoshowsbetterimprovementintheTaiChigroup, asthereareimprovementsof attention,executivefunctioning,language,memory,andorientationaspectsthatcanbeseeninthe TaiChigroup.TheMoCAhas asensitivityandspecificityof91%and81%, respectively15
•However,ourstudyshowsnosignificantresultintheTrailMakingTest(TMT), whichconsistsofpart AandpartBisaneuropsychologicalinstrument,usedasascreeningtoolfor assessingneurological diseaseandneuropsychologicalimpairment.Evenso,TMTpartBisshowntomeasure cognitive flexibility, ratherthanthepatient’sabilitytomaintainacognitiveset16
•Ourmeta-analysisalsoshowsnosignificantmanifestationbetweenthetwo groupsintheDigit spantest. Digitspantestisaverbalshort-termandmemorytestthatisusedasascreeningtoolfor assessingcognitivedomain.However,thestimuliwerepresentedauditorily,enablingthepatientto achievealowscoreiftheyhavehearingproblems17


BenefitsofTaiChiinOlderPatients
Cardiovascular: SunetaldemonstratetheimpactofTaiChioncardiacrehabilitationasitimproves cardiopulmonaryfunction.TaiChiisalsoabletoreduceobesity,asitaffectshumanbodymetabolismand energyconsumption18
Psychiatry: Yangetalshowlowerscoresinanxiety,stress,andQoLintheTaiChigroup,comparedtothe usualcaregroup,orevencomparedtotheaerobicexercisegroup19
Musculoskeletal: SungkaratetalshowTaiChiimprovesbalancingabilityamongstolderadultswithMCI duetoitsmovements20
FutureImplication
MCIisadegenerativedisease,whichisinevitableaswegetolder.Duetoitsdiscreetsymptoms,thisdisease oftenwent unnoticed andeven misdiagnosed21,22.Ifnottreated assoonaspossible,MCIhasthepotential toworsenanddevelopintothe dementiastage21,22,23.TaiChiisamind-bodyexercise,whichhasnumerous benefits.Hence,generalpractitionerscanadvisethismind-bodyexerciseforelderlywithmildcognitive impairmentinorderto slowdowntheprogress ofcognitiveabilitydeteriorationandevenimprovetheir cognitivestatus.
TheimplementationofTaiChiforelderlypatientwithMCIhasmanifesttremendousefficacyasitable to improvecognitivefunction withinelderswithMCIand slowdowntherateofcognitiveimpairmentin elderlypatients, shownbytheMoCAscoreandMMSE.Thus,thissystematicreviewandmeta-analysis providesstrongevidenceforTaiChiefficaciousnessasoneofthealternativenon-invasivetreatmentsfor treatingelderlypatientswithMCI.
REFERENCES
Identification of studies via databases and registers Identification PubMed n= 43 ScienceDirect n= 432 Total records for identified database n = 2530 Screening Full Reports assessed for eligibility n = 34 Screened by title (n=1338) Screened by abstract (n=54) Reports not retrieved (n=79) Screened by inclusion and exclusion criteria (n=819) Included Reports of included meta-analysis n= 8 Reports excluded (n=26) Irretrievable full-text (n=7) Irrelevant data (n=21) Europe PMC n=1589 ClinicalKey n=466 Records removed due to duplication n=217 Records screened based on title and abstract n = 2313 Records sought for retrieval n = 932
Figure2.PRISMAflowchartdiagramofthestudy
Figure1.ConceptualFramework
INTRODUCTION
Table1.InclusionCriteriaTable2.ExclusionCriteria
TheAuthorshavenoconflictofinteresttodeclare.
Table3.Characteristicsoftheincludesstudies Figure3:ForestPlotofMontrealCognitiveAssessment(MoCA)scoresthatassessed cognitivefunctionbetweenthetwogroups
Age (M(SD) years Angus et al., 2020 China RCT Tai Chi style Conventional Exercise ≥ 50 years 34 MoCA-HK Trail Making Test (TMT), Victoria Stroop test, digit-Span Forward Test, Digit-Span Backward Test 1224 Weeks Huang et al., 2019 China RCT Tai Chi style Control Group ≥60 years 80 MoCAMMSE, MoCA, TMT 365 Months Siu et. al., 2018 China Quasiexperimental study Yang-style simple form of Tai Chi Recreational activity aged ≥60 160 CMMSE IADL-CV 7416-week Sungkarat Australia RCT Tai Chi Control Group 60(5.9)66 MoCA TMT (B-A), Digit Span, MMSE 3312 weeks Sungkarat et al., 2018 Thailand RCT Tai Chi (TC) Control Group 68.3(6.7)66 MoCA TMT (B-A), Digit Span, MMSE 333 Weeks Xia et al., 2022 China RCT Baduanjin exercise training Brisk walking 66.16(4.16)135 MoCAMoCA 456 months Xiao et al., 2020 China RCT Tai Chi (TC) Control Group 58.92(8.03)78 MoCA TUGT 3712 weeks) Yang et al., 2021 Taiwan RCT Tai-Chi style multicomponent exercise program Care Control group 83.1(5.7)42 MoCA-TSMMSE, MoCA MIS, TMT A-B 2224 Weeks Primary Outcome Secondary Outcome Allocated to Received Tai Chi Follow up Period Author First Name Country Design Intervention Training received Control group Number of Adults
Figure8.FunnelPlotofstudiesincludedinMoCA
Figure.7RiskofBiasAssesment Figure9.FunnelplotofstudiesincludedinMMSE Figure4:ForestPlotofMMSEthatassessedcognitivefunctionbetweenthetwogroups Figure5:ForestPlotofTMTthatassessedcognitivefunctionbetweenthetwogroups Figure6:ForestPlotofDigitspanbackwardthatassessedcognitivefunctionbetweenthetwogroups
EffectivenessandSafetyofVitaminEtoPreventFurtherComplicationsin Type-2DiabetesMellitusElderlyPatients:ASystematicReview
Pre-conferenceCompetitionAsianMedicalStudents’Conference
AUTHORS:
VetherFernhandho,LouisJulian,EmanuelaClarisaKarinaSucahyo,andNatasha Theodora FacultyofMedicine
UniversityofPelitaHarapan 2023

EffectivenessandSafetyofVitaminEtoPreventFurtherComplicationsin
Type-2DiabetesMellitusElderlyPatients:ASystematicReview
VetherFernhandho,LouisJulian,EmanuelaClarisaKarinaSucahyo,Natasha
Theodora
[CorrespondenceE-mail: vetherfernando88@gmail.com]
Introduction:Type-2diabetesmellitus(T2DM)canaffectmanyotherorgansandcause seriouscomplications,especiallyintheelderly.Notinfrequently,thesecomplicationsleadto death.In2019,diabetesandkidneydiseaseduetodiabetescausedanestimated2million deaths.Untilnow,rarelyfoundawaytoreducecomplicationsfromtype-2diabetesmellitus otherthantakingdrugsorchanginglifestyle.However,itissuspectedthatconsuming vitaminEsupplementationcanreducesomeofthecomplicationsofdiabetes.Itishopedthat theresultswillprovethatusingvitaminEsupplementationcanreducethecomplicationsof type-2diabetesmellituspatientstoreducemortality.
Objective:TodeterminetheeffectivenessandsafetyofconsumingvitaminEinpatientswith diabetesmellitusinreducingtheriskoffurthercomplications.
Method:Articlesforthissystematicreviewwerecollectedfromseveraldatabases(PubMed, ProQuest,Cochrane,andGoogleScholar)usingtermsrelatedtotype-2diabetesmellitus, vitaminE,elderly,anddiabetescomplications. ThesearchwasoccurringfromMarch18ᵗʰ,2023 untilApril3ᵗʰ,2023.Allthesearchresultswereextractedandevaluatedwithinclusionandexclusion criteria.The qualityofincludedstudieswasassessedusingtheNewcastle-OttawaScale (NOS).
Result:Thissystematicreviewconsistedoffivehigh-qualityrandomizedcontroltrialswith 314participants.AllavailablestudiesshowthatvitaminEeffectivelypreventscomplications intype-2diabetesmellituselderlypatients.Threestudiesshowthatafterbeinggivenvitamin E,diabeticneuropathypatientscanimprovenerveconductionvelocityandlipidprofile.Two otherstudiesshowedthatvitaminEcouldpreventearlydiabeticretinopathyprogression, suchasretinalhemorrhage.However,furtherstudiesareneededtofindthespecificityof certaincomplications.
Conclusion:VitaminEiseffectiveandsafeforpreventingfurthercomplicationsintype-2 diabetesmellituspatients.
Keyword: T2DM,vitaminE,elderly,diabetescomplication

The Effectiveness of Vitamin D on Cognitive Function to Prevent Dementia in Elderly: A Literature Review
Afina Ariana Natawibawa, Adelia Irmanda, Salma Mardhiyah
Introduction: Alzheimer’s disease is the most common type of dementia, caused by alterations in cognitive processes, behaviour and mood, with a chronic, neurodegenerative and progressive condition. Alzheimer’swas the seventh-leadingcause ofdeathby 2020 and2021.Rightnow,more than 50 million people around the world live with dementia and in 2050, this number will be nearly triple. Previous research found that taking vitamin D was associated with living dementia-free for longer, but clinical trials is needed to confirm whether this is really the case.
Objective: This review aims to discover the effectiveness of vitamin D on cognitive function to prevent dementia in elderly in published study within last ten years with a hope that the elderly could eventually work up the medication and patients’ quality of life.
Method: A search was conducted in Pubmed, ALZ Journal, Springer Link, and Google scholar databases using the keywords (Vitamin D), (Cognitive function) AND (Dementia). A total of 9 studies were found that match our inclusion and exclusion criteria.
Results: Eleven studies were included in this study. We found that vitamin D significantly improves cognitive function, lower the risk of dementia, and associated with the incidence of dementia in elderly. Vitamin D could prevent dementia and improve elderly’s cognitive function through several mechanism.
Conclusion: Vitamin D deficiency appears to be associated with dementia and cognitive impairment in older adults. Daily oral vitamin D supplementation (800 IU/day) for 12 months improves cognitive function in elderly AD patients.
Keywords: dementia, vitamin D, cognitive function, Alzheimer’s dementia
The Effectiveness of Vitamin D on Cognitive Function to Prevent Dementia in Elderly: A Literature Review
Afina Ariana Natawibawa, Adelia Irmanda, Salma Mardhiyah
INTRODUCTION
Alzheimer’s disease is the most common type of dementia, aused by alterations in cognitive processes, behavior and mood, with a chronic, neurodegenerative and progressive condition. Alzheimer’s was the seventh-leading cause of death by 2020 and 2021. Right now, more than 50 million people around the world live with dementia and in 2050, this number will be nearly triple. Previous research found that taking vitamin D was associated with living dementia-free for longer, but clinical trials is needed to confirm whether this is really the case. This review aims to discover the effectiveness of vitamin D on cognitive function to prevent dementia in elderly in published study within last ten years with a hope that the elderly could eventually work up the medication and patients’ quality of life.
METHOD
A search was conducted in Pubmed, ALZ Journal, Springer Link, and Google scholar databases using the keywords (Vitamin D), (Cognitive function) AND (Dementia). A total of 11 studies were found that match our inclusion & exclusion criteria.
INCLUSION CRITERIA
Suspected/confirmed Alzheimer dementia patients


age > 65 years old
Vitamin D supplementation
Vitamin D level in serum
10 years past
EXCLUSION CRITERIA
Non accessible articles
Non-English or Bahasa Indonesia article

RESULTS
DISCUSSION & LIMITATION
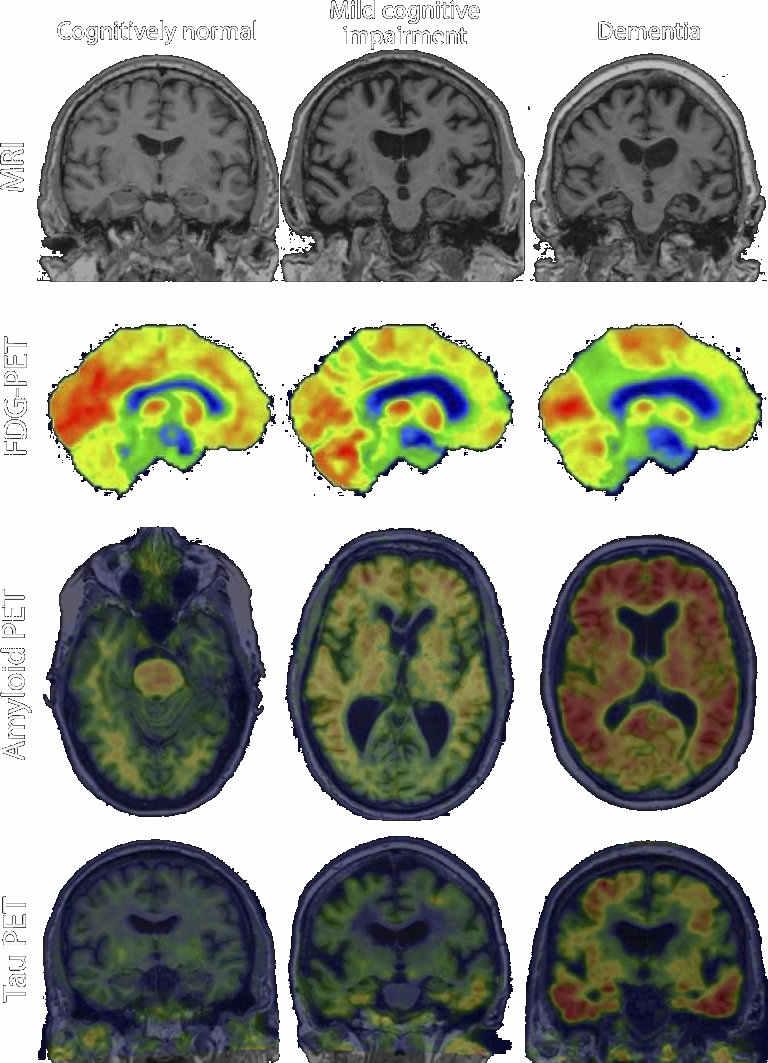
Vitamin D, a lipid soluble vitamin, is known for its benefits towards bone health but it is surely having more function than just that. Vitamin D is also known as an antioxidant that brings a protective effect to the brain and could improve its function, especially cognitive function. Our findings show the correlation between vitamin D towards the cognitive function in elderly and risks of dementia in several study. Cognitive function was the most assessed and it shown that vitamin D could improve the cognitive function in elderly. The mechanisms are because vitamin D have a decreasing effect towards Ab protein in the brain, the protein could result in neuronal dysfunction that could lead into dementia. Our findings show the correlation between vitamin D towards the cognitive function in elderly and risks of dementia in several study. Cognitive function was the most assessed and it shown that vitamin D could improve the cognitive function in elderly.
There are several mechanisms on how vitamin D could prevent dementia and enhance the brain functions in elderly. Vitamin D have protective effect towards the brain, where the receptors of vitamin D are presents in the hypothalamus thus promoting the growth of neurons. Other mechanisms also explained that vitamin D could reduce thrombosis and regulate the RAAS and suppress the inflammations that were caused by proinflammatory cytokines and amyloid proteins. Vitamin D have a decreasing effect towards Ab protein in the brain, the protein could result in neuronal dysfunction that could lead into dementia. Vitamin D was also involved in several brain functions that counteracting the oxidative stress that could lead to higher level of ROS, thus induces a cellular dysfunction and brain degeneration. Adequate vitamin D intake significantly could lead into a higher dementiafree incidence thus there is a significant correlation between vitamin D intake and the incidence of dementia and lower risk to develop dementia. Those who are dementia rely more on the use of vitamin D supplements . Other study also shows that vitamin D could affect to the volume of hippocampus and structural brain connectivity, thus it could improve the function of memory processing in older adults with MCI.
Groups that were given intervention shows a higher MMSE score rather than the control group and this result shows that vitamin D significantly could improve the cognitive function in elderly and deficiency of vitamin D also significantly associated with mild cognitive impairment (MCI) and Alzheimer dementia (AD).
On the other hand, study that were conducted by Kang, et al. in 2021 shows that there is no significant difference between those who were given vitamin D supplementation and placebo for 2-3 years. This might be the result from the difference of assessment tool that were used, TICS and 3MS, when most of other study were using MMSE. To assess which one is more effective to assess AD in elderly, might need a further study. Other study that uses FSIQ as the tool to assess the cognitive function, shows a consistent result with previous study. It shows that after given 800 IU of vitamin D per day for 12 months there is a significant improvement in the cognitive function in elderly compared to other study of four months RCT that shows no effect. This might be caused by the differences of geographic location since both studies did not assess the duration of sun exposure. This could be used for further study to assess the duration of sun exposure towards dementia.

CONCLUSION AND RECOMMENDATION
Vitamin D deficiency appears to be associated with dementia and cognitive impairment in older adults. Daily oral vitamin D supplementation (800 IU/day) for 12 months improves cognitive function in elderly AD patients.
REFERENCES

ACKNOWLEDGMENT & CONFLICT OF INTEREST
Writers declares that there is no conflict of interest nor acknowledgement.
1 2 3 4
5,7 5 5,7 12 5 9 4,8 9 13 14, 15 7 10 6 14 16
PhotobiomodulationasNovelTherapeuticApproachforDementia:ExploringThe PotentialandClinicalEfficacythroughaSystematicReviewandMeta-Analysis AletheiaPrastyo,DerrenD.C.H.Rampengan,GioninaHalim,MargarethaAmandaTulung AMSA-SamRatulangiUniversity
Introduction: Dementiaisaprogressiveneurodegenerativedisorderanditisestimatedthat thereareover55millionpeoplewithdementiaworldwide,particularlyinlow-and middle-incomecountries.Photobiomodulation(PBM)isanemergingnon-invasive therapeuticapproachthatutilizeslow-levellighttherapy.Itisanovelandpromisingavenue ofresearchthathasgainedsignificantattentioninrecentyearsfortreatingdementia.
Objective: TodeterminetheefficacyofPhotobiomodulationfordementiatreatmentsin geriatricpatients.
Method: ThisstudyfollowedthePreferredReportingItemforSystematicReviewand Meta-analysis(PRISMA)guidelinefromvariousdatabasesusingasetofkeywords.The databasewasgeneratedfromPubMed,ScienceDirect,EuropePMC,SageJournal,andWiley. Wethenperformedscreeningandselectionfollowedbydataextractionandquantitative analysiswithReviewManager5.4Software.
Results: Sevenrandomizedstudiescumulatingatotalof201participantsareincluded.This meta-analysissuggestedthatPBMislikelytoreducetheoddofriskcausingdementiain elderlypatientswithdementia(OR=0.41,95%CI;0.18to0.97,p-value=0.04).Another resultshowsthatTheMini-MentalStateExamination(MMSE)significantlyimprovedthe globalcognitivestatusofelderlypatientswithdementiaaftertheadministrationofPBM (MD=-5.37,95%ConfidenceInterval-10.30to-0.45).Theresultsreportedinfourtrials whichassessedtheglobalseverityofcognitiveperformanceshowedthatPBMsignificantly improvedglobalcognitivefunctioninpatientswithdementiacomparedwiththecontrol group.
Conclusion: Thissystematicreviewandmeta-analysisfoundthatphotobiomodulationtobe apromisingandsafetherapeuticapproachfortreatingdementia,thatcanimprovecognitive function,reducebehavioralsymptoms,andenhancequalityoflifeinindividualswith dementia.
Keywords: Dementia,Photobiomodulation,Alzheimer
Photobiomodulation as Novel Therapeutic Approach for Dementia : Exploring The Potential and Clinical Efficacy through a Systematic Review and Meta-Analysis

Aletheia H. Prastyo, Derren D. C. H. Rampengan, Gionina Halim, Margaretha A. Tulung
Universitas Sam Ratulangi

Dementia is a neurodegenerative disease that currently affects approximately 50 million people worldwide. The global prevalence of dementia is expected to increase up to 300% by 2050, making it a pressing public health concern. Despite the extensive research dedicated to understanding the complex pathophysiology of dementia, effective treatments remain elusive. In this context, exploring innovative therapeutic strategies has become paramount. However recently Photobiomodulation (PBM) has emerged as a promising non-invasive therapeutic approach with potential applications in various medical conditions, including neurodegenerative diseases such as dementia.
OBJECTIVE
This systematic review and meta-analysis are aimed to explore the efficcy of potential and clinical photomodulation as novel therapeutic approach for dementia.
The database hits 202 trails was generated from the five database (PubMed, ScienceDirect, Europe PMC, Sage Journal, Wiley). At first, 52 duplicate were removed. Two author read through the abstracts and title and 101 articles were removed due to articles not relevant (that is., trails published before 2018, trials with no control group). The remaining 49 was assessed for full text screening. These articles were assessed for eligibility based on the exclusion criterions established previously. 11 articles were excluded due to poor results, 9 was removed due to lack of outcome measure, and 8 articles was reported in another language. The remaining 21 articles was retained for data extraction and quality assessment.
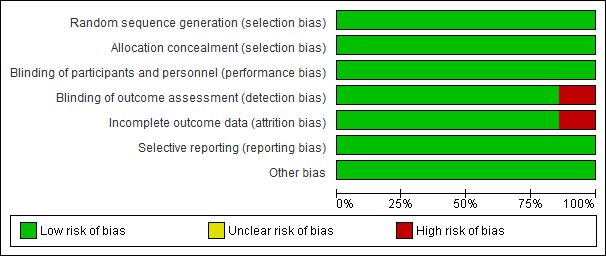
RESULTS & DISCUSSION
Dementia is a global health problem mostly affected aged people. The most prevalent type of dementia is Alzheimer’s disease, followed by vascular dementia and lewy body dementia (Burns and Iliffe, 2009). Several Pharmacological trials in treatment and interventions for dementia have failed. Researchers have tried to investigate the important non-pharmacological interventions (Liu et al., 2020). To the best of our knowledge, this is the first meta-analysis to investigate the efficicay of Photobiomodulation for dementia and to focus on cognitive performance after therapy in patients with dementia. The present systematics review and meta-analysis have shown that Photobiomodulation as a neuromodulation via transcranial phototherapy was an effective technology in treatment of dementia. The findings is consistent with the previous meta-analysis who included 601 participants and 13 trials (Zhu et al., 2022).
Photobiomodulation therapy (PBMt) is a safe, non-invasive, and non-thermal method that is proposed to involve the stimulation of mitochondrial action by the absorption of photons in specific transmembrane proteins (e.g., cytochrome c oxidase), resulting in increased ATP production, leading to reduced oxidative stress, anti-inflammatory effects, improved cellular energy, increased synthesis of enzymes, and increased focal cerebral blood flow (Bullock-Saxton et al., 2021). With PBMt, the therapy can minimize pain and improve the patient's quality of life.
PBMt could be a novel therapy for dementia. The literature found that there was an improvement in cognitive impairment in the group receiving PBMt therapy, while the control group did not show the same thing. PBMt has no side effects compared to drug therapy for dementia, where higher doses will cause headaches (Berman et al., 2017). In addition, PBMt has many advantages, such as promoting microcirculation, cell proliferation, and regeneration, and can also relieve pain, edema, oxidative stress, and inflammation in several traumatic, acute, and chronic diseases. PBMt also directly plays a role in the brain where it activates several signaling pathways, including those involved in neuroprotective, antioxidant, anti-apoptotic, and anti-inflammatory pathways, upregulating neurotrophic factors (e.g., brain-derived neurotrophic factor [BDNF] and nerve growth factor [NGF]), stimulate adult hippocampal neurogenesis, as well as synaptogenesis and neuroplasticity (Salehpour et al., 2021).Compared to current standard therapy, PMBt has advantages and hopes to become the primary treatment for dementia patients. This is proven through the results of our meta-analysis.
The results of the Mini-Mental State Examination reported in four trials which assessed the global severity of cognitive performance showed that PBM was significantly improved global cognitive function in patients with dementia compared with the control group. The previous meta-analysis Zhu et al., 2022 found similar findings. However, Alzheimer’s disease Assessment Scale-cognitive (ADAS-cog) subscale showed no significant improvement. This was as a results of small number of trials and different control used in the trials. Also, we could not performed meta-analysis on other primary outcome such as MoCA, TUG, DST, CDR, SWT, ST (Dynamic Step Test) and 9-HPT due to number of trials < 3. Nevertheless, significant improvement of TUG, DST, SWT, 9-HPT and MoCA was found in Bullock-Saxton et al., 2021, significant improvement was reported in Kheradmand et al., 2022.


All the seven (7) included studies used in the meta-analysis were randomized controlled studies design. Each of the seven (7) studies were published in different countries in California, Australia, USA, France, China, and Canada except for Kheradmand et al., 2022 whose publication country was not recorded. A sum of 201 participants were included in the trials, with an average of 67.7. The patients was randomized into two group, the first group received Photobiomodulation therapy why the second group received Sham or usual care for a duration of 4 weeks.
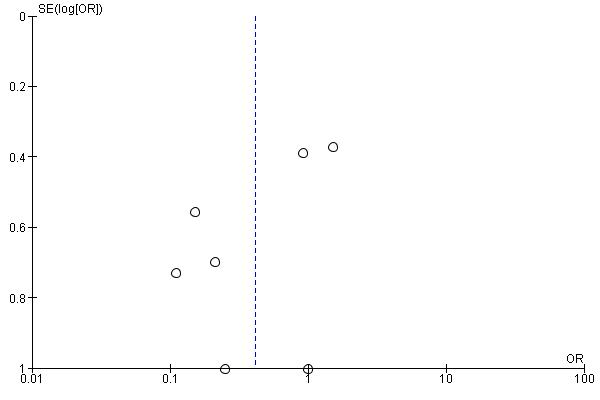
META-ANALYSIS OF EFFICACY OF PHOTOBIOMODULATION (PBM) THERAPY FOR DEMENTIA
Seven studies were included in the meta-analysis of efficacy of photobiomodulation therapy for dementia using random effect model. The result of the meta-analysis shows that PBM is likely to reduce the odd of risk causing dementia in elderly patients with dementia (OR = 0.41, 95% CI; 0.18 to 0.97, p – value = 0.04). The heterogeneity among the studies was high and significant. (I2 = 73%, P 0.001) Fig 2. The funnel visualization of the included studies shows a symmetric shape which implies that no publication bias in the studies Fig 3.
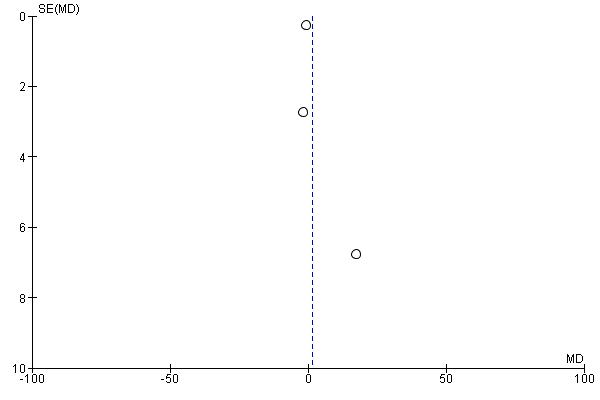
META-ANALYSIS OF PBM ON COGNITION PERFORMANCE (MMSE AND ADAS-COG)
Four trials was included in the meta-analysis of MMSE which assessed the global severity of cognitive defects using random effect model. The results shows that The Min-Mental State Examination (MMSE) significantly improve global cognitive status of elderly patients with dementia after the administration of PBM (MD = -5.37, 95% Confidence Interval -10.30 to -0.45). Moderately High and non-significant heterogeneity was found among the included studies (I2 = 60%, p = 0.06). The funnel plot presented in Fig 5. Shows no evidence of publication bias Fig 5.


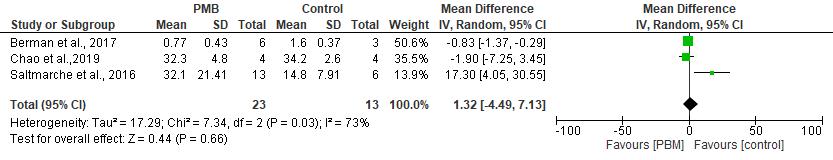
Three trials was included in the Meta-analysis of ADAS-cog using a random effect model with a mean difference between the two groups as the effect size. The results of the meta-analysis suggest that Alzheimer’s disease Assessment Scale-cognitive (ADAS-cog) subscale has no significant effect on cognitive function after the administration of PBM to elderly patients with dementia (MD = 1.32, 95% Confidence Interval -4.49 to 7.13). High and significant heterogeneity among the patient was found (I2 = 73%, p – value = 0.03) Fig. 6. The funnel visualization of the included studies shows no evidence of publication bias (Fig 7).


LIMITATION
There are few limitations during the study selection process that results interpretation. There are a lot of excluded trials conducted on animal dementia which might have a negative effect on our results. Limiting the study to human study caused the small number of trials included in some outcomes. Expanding the research to animal study will increase the significant of the results and also allow metaanalysis of some outcomes. Secondly, the overall heterogeneity of the study was considerably which limit the interpretation of one of the results. Therefore, sensitivity and subgroup analysis are needed to perfect the results.
CONCLUSIONS
Photobiomodulation has been found to be a promising and safe therapeutic approach for treating dementia by improving cognitive function, reducing behavioral symptoms, and enhancing quality of life in individuals affected. However, future research is needed to investigate the optimal parameters of PBM, such as wavelength and intensity, and to determine the long-term effects of PBM on dementia
REFERENCES
outcomes.
INTRODUCTION
included Screening Identification PubMed 65 ClinicalKey 35 Europe PMC 204 Cochrane 19 Google Scholar : 1340 Records identified from*: Database (n=1663) Records Screened (n = 476) Reports assessed for eligibility (n = 36) Studies included in review (n = 11) Duplicate records removed Records marked as ineligible by automation tools Records removed before screening : (n = 1187) Poor results Not relevant Record excluded ** (n = 440) Missing data or inadequate numerical data Studies not reporting on measurable outcomes of interest, Full text not available No control group Reports excluded: (n = 225) INCLUSION MATERIALS AND METHOD Figure 3. ROB Summary Figure 2. The Outcome Results of quality assessment using ROB Fig. 1: PRISMA Flow chart RCT Design Full Text Articles Assess MMSE & ADAS-cog Studies included 2013-2023 EXCLUSION Irretrievable full text Incomplete data Non english language study KEYWORDS Photomodulation AND Dementia Table 1. Characteristics of the included studies Fig 2. Forest plot showing the efficacy of PBM for dementia Fig 4. Forest plot of the outcome MMSE that measures performanceFig Funnel plot showing the studies included in the meta-analysis of PBM against the control group.
Fig 5. Funnel plot of studies included in MMSE of the photobiomodulation therapy
cognitive
Fig
6. Forest graph of ADAS-cog for assessing
function
Fig 7. Funnel plot of studies included in the meta-analysis of ADAS-cog for assessing
cognitive function
ia
SafetyandEfficacyofAducanumab(BIIB037)asaMonoclonalAntibodyindicatedtotreat Alzheimer’sdisease:ASystematicReview
FralkyGabrielMarselinoMaramis,AnastasiaMariaAngelicaMontolalu,Richard LeonardSantoso,SinclairJorlandoKakambong
Abstract
Introduction:Alzheimer’sdiseaseisaprogressiveandfatalneurodegenerativedisorderthat insidiouslytakesoverthememories,cognitivefunction,andlivelihoodofthosediagnosed. Approximatelymorethan50millionindividualssufferfromitgloballyandby2050,itis expectedtoexceed150million.Upuntilnow,thereareonly4drugsthathavebeenapprovedfor ADtreatment.Inspiteofthat,thesedrugsonlyreducesymptomsbutdonottargetAD’stwo mainrecognizedpathologicalfeatures.Therefore,aducanumab(BIIB037)becamethefirst disease-modifyingtherapyforAD.Aducanumabisaselectivemonoclonalantibodywith demonstratedpotencyintheclearanceofaggregatedAβplaques.ResearchersbelievedthatAβ clearancebyaducanumabisawaytoslowcognitivedeclineinADandnormalizationof neuronalactivityinthebrain.
Objective:Toanalyzethesafetyandefficacyofaducanumab(BIIB037)asatreatmentfor Alzheimer’sDisease
Methods: Thestudyincludedwereobtainedbyperformingarandomcontrolledtrialsin5 databasesnamelyPubmed,ScienceDirect,andResearchgate,thenthestudyassessedaccording tothePRISMAflowdiagram.RiskofbiaswasassessedusingRiskofBias2.0Cohrane.
Results:NounexpectedsecurityconcernsassociatedwithusingAducanumabinpatientswith mildtomoderateADobserved.Theresultsofthisplacebo-controlledPhase1multicenterstudy, supportcontinuationEvaluationofaducanumabasapotentialdisease-modifyingagent TreatmentofADpatients.Inphase3,ENGAGEdoesnotmeetareacodeorsecondaryendpoint andEMERGEhighdoseAducanumabgroupfulfilledallprimaryandsecondaryendpoint.
Conclusion
Inconclusion,aducanumabiseffectiveinsignificantlyreducingAβplaquesinthebrainand decreasingtaubrainlevelsinallcorticalbrainregionsexamined.Aducanumabservesasa potentialdisease-modifyingtherapyinthemanagementofAD
Keywords: (ADUCANUMABORADUHELMORBIIB037)AND(TREATMENT)AND (ALZHEIMER’SDISEASE)
Safety and Efficacy of Aducanumab (BIIB037) as a Monoclonal Antibody indicated to treat Alzheimer’s disease
Fralky Maramis, Anastasia Montolalu, Richard Santoso, Sinclair Kakambong

INTRODUCTION
Alzheimer’s disease is a progressive and fatal neurodegenerative disorder that insidiously takes over the memories, cognitive function, and livelihood of those diagnosed. AD causes 60-80% cases of dementia. Approximately more than 50 million individuals suffer from it globally and by 2050, it is expected to exceed 150 million. Up until now, there is only 4 drugs that had been approved for AD treatment. In spite of that, these drugs only reduce symptoms but do not target AD’s two main recognized pathological features: deposits of amyloid β (Aβ) plaques and intracellular neurofibrillary tangles. Therefore, aducanumab (BIIB037) became the first disease-modifying therapy for AD. Aducanumab is a selective monoclonal antibody with demonstrated potency in the clearance of aggregated Aβ plaques. Researches believed that accumulation of Aβ is the main cause of neuronal loss and dysfunction and the main driver of AD pathogenesis. Hence, it is believed that Aβ clearance by aducanumab is a way to slow cognitive decline in AD and normalization of neuronal activity in the brain.
OBJECTIVE
To analyze the safety and efficacy of aducanumab (BIIB037) as a treatmentforAlzheimer’sDisease
MATERIAL AND METHODS
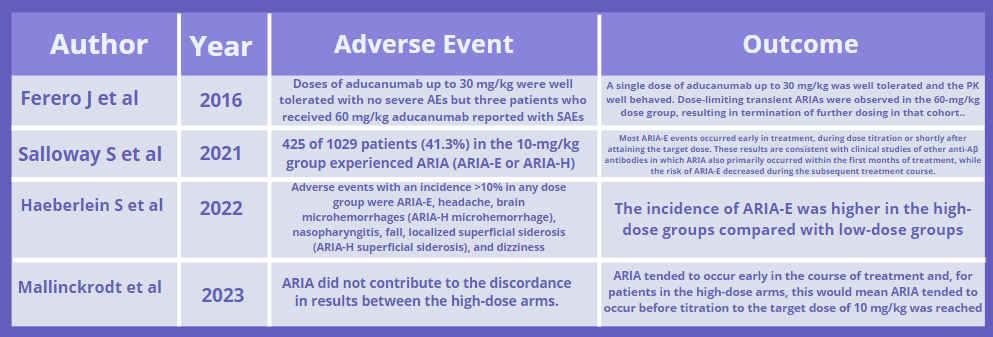
RESULT AND DISCUSSION
Keyword
Aducanumab

The logic behind anti-amyloid drug therapy can be simplified by the following: the removal of plaques disrupts the major pathogenic process vital to the progression of AD thus slowing development of the disease.The drug functions by selectively binding amyloid aggregates in both the oligomeric and fibrillar states rather than amyloid monomers.This binding discrimination by the drug is what distinguishes aducanumab from its contemporary Aβ immunotherapeutic agents. The Aβ aggregates have been shown to exert neurotoxic effects while monomeric Aβ has exhibited beneficial neurological functions.Although other monoclonal antibodies have overlapping binding sites on amyloid, aducanumab provides unique amino acid interactions which allow for more shallow and compact binding with minimized interactions by the epitope scarce monomers. Conversely, the high affinity for aggregates can be explained by a greater concentrationofepitopesspecificforthemonoclonalantibodygrantingagreateraffinity.
Complications
Aducanumab can induce ARIA-E, which manifests as sulcus effusions or cerebral edema on MRI, and ARIA-H, which includes superficial siderosis and microhemorrhages. Clinical symptoms of ARIA were found in 24% of radiographic ARIA participants during clinical examination. Symptoms included headache , delirium , confusion, dizziness , visual disturbances , altered mental status , and disorientation, nausea, and headache are the most common symptoms
Safety
There are no unexpected security concerns associated with using Aducanumab in patients with mild to moderate AD observed. EMERGE is the first Phase 3 trial, shows the relationship between the reduction of Alzheimer's disease biomarkers and statistically significant biomarkers delay clinical decline, Removal of Aβ from the brain (along with modification downstream biomarkers of disease).

Clinically useful in early AD patients

The results of this placebo-controlled Phase 1 multicenter study, support continuation Evaluation of aducanumab as a potential diseasemodifying agent Treatment of AD patients.
In phase 3, ENGAGE does not meet area code or secondary endpoint and EMERGE high dose Aducanumab group fulfilled all primary and secondary end point. The clinical efficacy of aducanumab is being further evaluated It will be evaluated in future clinical studies.

CONCLUSION
In conclusion, aducanumab is effective in significantly reducing Aβ plaques in the brain and decreasing tau brain levels in all cortical brain regions examined. However, the post hoc analysis did not show sufficient clinical benefit. Additionally, there was no reliable
evidence that corresponds Aβ plaques reduction with clinical efficacy. Nevertheless, aducanumab serves as a potential disease-modifying therapy in the management of AD
aducanumab - Written in English PubMed : 366 Sciencedirect : 736 REFERENCE Reports assessed for eligbility (n= 22) Studies included in qualitative synthesis (n=4) Records excluded on the basis of inclusionandexclusion(n=1589) Document excluded on the basis of lackessentialdata(n=18) ELIGIBILITY INCLUDED
Figure 1 Risk of bias graph Risk of bias summary Figure 2 Exclusion (ADUCANUMAB OR ADUHELM OR BIIB037) AND (TREATMENT) AND (ALZHEIMER’S DISEASE)
Figures
Mechanism of Action
- Review paper - Expert opinion - irretrievable full text
Records screened (n=1611) Document exluded on the basis of duplication (n=491) IDENTIFICATION SCREENING
CouldLightTherapybetheFutureTreatmentforSleepDisturbancesinDementia Patients?
TesalonikaKyveniaWilar,CharissaMelodyPali,StefanusVickyBernhardElisaRuntunuwu, GeniaAbigailManuelaPaat
tesalonikawilar011@student.unsrat.ac.id
ABSTRACT
Introduction:
Sleepdisturbancesareprevalentinpatientswithdementia,asitaffectsupto70%ofthepatients. Peoplewithdementiafrequentlyshowcircadiandysregulationthatcausessleepdisturbancesand otherproblems.Thisoftenincreasescaregiverburdenandtheriskofinstitutionalization.Light therapyhasbeensuggestedtobeapromisingnon-pharmacologicalinterventionfordementia patientswithsleepdisturbancesbyimprovingthecircadianrhythm.Wehopethatthisreview willbeofuseinprovidingtheappropriateinterventiontohelppeopleinloweringsleep disturbancesinpatientswithdementia.
Objective:
Toanalyzetheefficacyoflighttherapyasaninterventionforsleepdisturbancesinpatientswith dementia.
Method: ThissystematicreviewwascarriedoutbasedonthePRISMAguidelinefrommultipledatabases usingsetkeywords.WeperformedasystematicsearchinPubmed,ScienceDirect,SageJournal, andCochraneforstudiesreportingtheusageoflighttherapyinterventiontoincreasesleep qualityinpatientswithdementia.Atotalof885studieswerefoundandthenfilteredbasedon theinclusionandexclusioncriteria.QualityassessmentwasbasedontheCochraneRiskofBias tool.
Results: Atotaloffourstudieswerereviewed.Allmeasuredtheefficacyoflighttherapyinreducingthe sleepdisturbancesbyincreasingsleepqualityindementiapatients.Twoofsixstudiesstudiedthe effectivenessofbrightlighttherapy,onestudiedtailoredlighting,whileonestudiedtimed blue-enrichedtherapy.Allstudiessupporttheobjectiveofourreview.
Conclusion:
Inconclusion,lighttherapyshowssignificantresultsinreducingsleepdisturbances,thusbeinga promisingtherapyinincreasingsleepqualityinpeoplewithdementia.Furtherstudiesareneeded toassesstheoptimalprocedureregardingtheusageofthistherapy.
Keywords: Lighttherapy,Dementia,Sleep,Intervention
Could Light Therapy be the Future Treatment for Sleep Disturbances in Dementia Patients?
A Systematic Review of Randomized Clinical Trials
Tesalonika Kyvenia Wilar, Charissa Melody Pali, Stefanus Vicky Bernhard Elisa Runtunuwu, Genia Abigail Manuela Paat tesalonikawilar011@student.unsrat.ac.id
INTRODUCTION
Sleep disturbances are prevalent in patients with dementia, as it affects up to 70% of the patients [1]. People with dementia frequently show circadian dysregulation, with several sleep and wake periods occurring throughout the 24-h day [2]. Sleep disturbances are characterized by symptoms of fragmented sleep, night–day reversal, disrupted sleep–wake rhythms, and so forth. This has been known to increase caregiver burden and the risk of institutionalization [3]. Although there are pharmacological treatments used to manage sleep disturbances, medications are often associated with side-effects such as sedation and risk of falling [1]. Light therapy has been suggested to be a promising non-pharmacological intervention for dementia patients with sleep disturbances by improving circadian rhythm, sleep disorders, insomnia, and sleep problems [4]. We hope that this review will assist the government and medical health workers in providing the appropriate intervention to help people inloweringsleepdisturbancesinpatientswithdementia.
OBJECTIVE
To analyze the efficacy of light therapy as an intervention for sleep disturbances inpatientsdiagnosedwithdementia.
METHOD
Systematic review process based on the PRISMA guidelines
Screening studies based on inclusion and exclusion criteria
Explore and extract all the required data various database
Quality assessment yielded
6 Randomized Clinical Trial
Bias assessment using the Cochrane Risk of Bias Tool
Figure 1. FrameworkConceptual
Records identified through database searching (n=883): PubMed (n=28)
Science Direct (n=125)
Sage Journal (n=727) Cochrane (n=3)
INCLUSION
Randomized Clinical Trial
Reported sleep outcomes on patients diagnosed with dementia
Intervention in the form light therapy
In English
Published between 2018-2023
EXCLUSION
Review articles, expert opinion
Incomplete clinical trials, no results to be extracted
Irrelevant study or outcome
Keywords: (“Light therapy” OR “Light treatment” OR “Light intervention”) AND (“Intervention”) AND (“Dementia”) AND (“Sleep”)
Document excluded on the basis of duplication (n=101)
Faculty of Medicine, Sam Ratulangi University
RESULTS AND DISCUSSION
Author, Year Design Participants Place Type of Therapy Measurement Tool
Kim et al, 2021 RCT 25 (14 TG, 11 CG) Chuncheon, South Korea Timed blue-enriched white LT PSQI
Cibeira et al, 2021 RCT 39 (20 CG, 19 BLT group) A Coruña, Spain BLT Interact short Hjetland et al, 2021 RCT 69 Bergen, Norway BLT SDI
Records screened based on title and abstract (n=784)
Full-text articles assessed for eligibility (n=58)
Studies included in qualitative synthesis (n=4)
Document excluded on the basis of inclusion and exclusion (n=726)
Document excluded on the basis of lack essential data (n=54)
Hjetland et al, 2021 BLT mountedCeilingLED light panels 1000 lx and 6000 K (vertically)
Figuiro et al, 2019 TLI floor luminaires, light boxes,tables.light
sessions were 30 min/day, between
10:30 a.m. and noon, 5 days a week (Monday to Friday), for 4 weeks (total 20 sessions)

floor luminaires 600 lux of 5000 K or 550 lux, light boxes 350 lux of 6000 K, light tables delivered 750 lux of 5000 K

6:00–8:00 AM
(accordingindividualto participants’ habitual wake times)
At session, in the 10 min periods before, after each session
Baseline, after 8, 16 and 24 weeks
Week 1, 5, 10, and 14.
Table 3. Outcome of studies.
Stimulation level construct showed a signifificant increase in score: Relaxed, content or sleeping appropriately (p = 0.001)
SDI was significantly improved in the intervention group compared to the control group from baseline to week 16 (B = − 0.06, 95% CI -0.11 - -0.01, p < .05) and from baseline to week 24 (B = − 0.05, 95% CI -0.10-0.01, p < .05).
PSQI scores in TG were signifcantly reduced at both immediate post-treatment and 4-week follow-up of the LT compared to those at baseline.
Figuiro et al, 2019 RCT 46 Bennington, New York TLI PSQI LT, Light Therapy; BLT, Bright Light Therapy; CCT, Correlated Color Temperature; TLI, Tailored Light Therapy; K, Kelvin; LED, Light Emitting Diode; BWL. BrightWhiteLight;PSQI,PittsburghSleepQualityIndex;SDI,SleepDisorderInventory;TG,Treatmentgroup.
A total of 4 randomized clinical trials were reviewed, with a total of 179 participants. All studies showed similar outcomesofincreasedsleepqualityandreducedsleepdisturbanceswiththeuseoflighttherapyintervention demonstrated in people with dementia (PwD). Measurement tools for sleep outcomes that we included in this review consist of PSQI, SDI, and Interact Short. 2 studies showed that BLT increases sleep quality, each by reducing sleep disorder and providing immediate positive effects on stimulation level [1,5]; 1 study showed that timed blue-enriched white light therapy (Timed BLT) reduces sleep disturbances [3]; 1 study showed that TLI also reduces sleep disturbances[6].
CurrentStateofLightTherapyonPeoplewithDementia(PwD)
Light therapy has been reported to be effective for improving the sleep of healthy older people, and patients with dementia [4]. For example, BLT has been shown to have positive effects on BPSD, sleep, and circadian rhythms in dementia. Timed BLT and TLI has also shown better effectiveness on subjective sleep quality (shown in Table 3.). Though,theamountofstudiesregardinglighttherapythatspecificallyfocusesonitseffecttowardssleepdisturbances on PwD are still very limited. Light therapy is an affordable, effective, fast-acting therapy for age related disturbances, with many advantages over pharmacological alternatives. Medications used to treat sleep disorders, such as benzodiazepines, are considered unsafe for the elderly because the drugs may exacerbate their existing risk of drowsiness, cognitive degradation, high risk of fracture, drug dependence, and other adverse reactions associated with long-term use [4]. For that reason, it is necessary to explore and consider nondrug therapy to improve sleep disordersinPwD.
Mechanisms
Biologically, PwD may experience the degeneration of the suprachiasmaticnuclei (SCN), which explains their disturbedsleep-wakecircadiansystem[7,8].

Light therapy has the ability to counteract this issue by modulating circadian rhythms. Exposure to light synchronizes the master circadian clock located in the SCN in the hypothalamus. Light information reaches the SCN via a direct retinalprojection.TheSCNregulatesoutputrhythmsincludingmelatoninandcortisol[9].
Strengths
First systematic review that specifically focuses on the efficacy of light therapy as an intervention for sleepdisturbancesinPwD
AllstudywereRandomizedClinicalTrials
All study significantly supports the objective of our study in proving that light therapy is a promising non-pharmacological intervention in reducing sleepdisturbancesandincreasingsleepquality.
Limitations
Differentobjectivesandtypeoflightinterventionin includedstudies
Lownumberofeligiblestudy
CONCLUSION AND RECOMMENDATION
In conclusion, our findings are consistent, with light therapy showing significant results in reducing sleep disturbances and sleep disorders, thus being a very promising therapy in increasing sleep quality in people with dementia (PwD). Further studies are needed to assess the optimal type of light intervention, methodology, light output, duration and frequency for this therapy. We recommend the dissemination of further research and applications regarding light therapy as a non-pharmacological intervention in reducing sleep disturbances in dementia patients to strengthen the evidenceoftheireffectiveness.
Author, Year Kim et al, 2021 Cibeira et al, 2021 Hjetland et al, 2021 Figuero et al, 2019 Randomization Concealed Allocation Blinding of Participants and Personnel Blinding of Outcome Assessment Incomplete Outcome Data Selective Reporting Other bias LOW UNCLEAR HIGH Author, Year Light Intervention Follow-up Results/Sleep Outcomes Type of Therapy Method Output Duration and frequency Kim et al, 2021 Timed blueenriched white LT LED light box, 60 cm away 30 lx at the eyes 1 h each morning for 2 weeks Baseline, Immediate post-treatment, 4 weeks after the end of the 2 weeks
PSQI scores were significantly lower after the active intervention. Cibeira et al, 2021 BLT BWL lamp, 70 cm away 10000 lx The
Mean
IDENTIFICATION INCLUDEDSCREENINGELIGIBILITY
Figure 2. Search Method
Table 1. Risk of bias based on Cochrane Risk of Bias tool
RCT, Randomized Clinical Trials; TG, Treatment group; CG, Control group; TLI, Tailored Lighting; PSQI, Pittsburgh Sleep Quality Index; SDI, Sleep DisorderInventory. Table 2. Characteristics of studies.
REFERENCES HjetlandGJ,KolbergE,PallesenS,ThunE,NordhusIH,BjorvatnB,etal.Ambientbrightlighttreatmentimprovedproxy-ratedsleepbutnotsleepmeasuredbyactigraphyinnursinghomepatientswith dementia:aplacebo-controlledrandomisedtrial.BMCGeriatr.2021;21(1):1–15. Hjetland GJ, Pallesen S, Thun E, Kolberg E, Nordhus IH, Flo E. Light interventions and sleep, circadian, behavioral, and psychological disturbances in dementia: A systematic review of methods and outcomes.SleepMedRev[Internet].2020Aug;52:101310.Availablefrom:https://linkinghub.elsevier.com/retrieve/pii/S1087079220300538 Kim SJ, Lee SH, Suh IB, Jang JW, Jhoo JH, Lee JH. Positive effect of timed blue-enriched white light on sleep and cognition in patients with mild and moderate Alzheimer’s disease. Sci Rep [Internet]. 2021;11(1):1–12.Availablefrom:https://doi.org/10.1038/s41598-021-89521-9 Zhang M, Wang Q, Pu L, Tang H, Chen M, Wang X, et al. Light Therapy to Improve Sleep Quality in Older Adults Living in Residential Long-Term Care: A Systematic Review. J Am Med Dir Assoc [Internet].2023Jan;24(1):65-74.e1.Availablefrom https://linkinghub.elsevier.com/retrieve/pii/S1525861022007903 CibeiraN,MasedaA,Lorenzo-LópezL,González-AbraldesI,López-LópezR,Rodríguez-VillamilJL,etal.Brightlighttherapyinolderadultswithmoderatetoveryseveredementia:Immediateeffectson behavior,mood,andphysiologicalparameters.Healthc.2021;9(8). Figueiro MG, Plitnick B, Roohan C, Sahin L, Kalsher M, Rea MS. Effects of a tailored lighting intervention on sleep quality, rest-activity, mood, and behavior in older adults with Alzheimer disease and relateddementias:Arandomizedclinicaltrial.JClinSleepMed.2019;15(12):1757–67. Fong KN, Ge X, Ting K, Wei M, Cheung H. The Effects of Light Therapy on Sleep, Agitation and Depression in People With Dementia: A Systematic Review and Meta-analysis of Randomized ControlledTrials.AmJAlzheimer’sDisOtherDementias®[Internet].2023Jan16;38:153331752311606.Availablefrom:http://journals.sagepub.com/doi/10.1177/15333175231160682 Bromundt V, Wirz-Justice A, Boutellier M, Winter S, Haberstroh M, Terman M, et al. Effects of a dawn-dusk simulation on circadian rest-activity cycles, sleep, mood and well-being in dementia patients.ExpGerontol[Internet].2019Sep;124:110641.Availablefrom:https://linkinghub.elsevier.com/retrieve/pii/S0531556519302347 Rubiño JA, Gamundí A, Akaarir M, Canellas F, Rial R Nicolau MC. Bright Light Therapy and Circadian Cycles in Institutionalized Elders. Front Neurosci [Internet]. 2020 May 6;14. Available from: https://www.frontiersin.org/article/10.3389/fnins.2020.00359/full 1. 2. 3. 4. 5. 6. 7. 8. 9. Additional records identified through other sources (n=2)
EFFECTIVITYOFGINKGOBILOBAEXTRACTEGb761ASANALTERNATIVE TODONEPEZILFORALZHEIMER'SDISEASETHERAPY:ASYSTEMATIC REVIEWANDMETA-ANALYSIS
ShakiraKhansaAudieKurniawan,RichardNelsonCahya,VionaTitaniaRiskikallail,Ida AyuKyaraFerbenaTrininta
[CorrespondenceE-mail: shakirakhansa29@gmail.com]
Introduction: Alzheimer'sdisease(AD),oneofthemostfrequentformsofdementia,isa stealthyneurodegenerativeailmentthatisirreversibleandcommoninolderpeople.ADis characterizedbygradualcognitiveandintellectualdeficits.Lateinterventionsandtreatments negativelyimpactthepatientandplaceaheavyburdenonthefamilyandsociety.Numerous clinicaltreatmentplansforADarenowavailable,butonlyafewhavedemonstratedcurative results. Ginkgobiloba extract,EGb761,showsapromisingpotentialtobecomean alternativeapproachintreatingAlzheimer'sdisease.
Objective: TodeterminetheeffectivityofEGb761fromtheextractof Ginkgobiloba asan alternative,accessible,andcurativeapproachinADpatients.
MaterialandMethods: ThisstudywasconductedusingPreferredReportingItemfor SystematicReviewandMeta-analysis(PRISMA).Wesystematicallysearchedin correspondencetoinclusionandexclusioncriteriathroughdatabases,namelyPubmed, Scopus,andFrontiers.Furthermore,weassessedthequalityofstudiesusingtheRoB2.0 Cochranetool.
ResultsandDiscussion: VariouscognitivefunctionswereassessedthroughtheMini-Mental StatusExam(MMSE),IADLexamination,andtheSyndromKurztest(SKT).TheMMSE results(MD=2.43[1.47,3.89])suggestEGb761improvedthecognitivefunctionsin Alzheimer'sdiseasepatientsbetterthandonepezil,thoughIADLtests(MD=0.82[2.25, 3.39])andSKT(-0.69[0.86,2.26])showednosignificantdifferencesbetweenbothgroupsin treatmentefficacythroughdailytasksanddementiaseverity.Morediscontinuationsdueto sideeffectswereseeninthedonepezilgroup(n=7).Thenon-inferiorityofEGb761from suchresultssuggestsEGb761maybeanalternativeforAlzheimer'sdisease.
Conclusion: EGb761showspotentialabilitiestowardstreatingAlzheimer’sdiseaseseen throughthesmallerprobabilityofsideeffectsthandonepezil.
Keywords: donepezil,Ginkgobiloba,Alzheimer’sdisease
EFFECTIVITY OF GINKGO BILOBA EXTRACT EGb761 AS AN ALTERNATIVE TO DONEPEZIL FOR ALZHEIMER'S DISEASE
THERAPY: A SYSTEMATIC REVIEW AND META-ANALYSIS

INTRODUCTIONRESULTS
Donepezil hydrochloride

The use of donepezil for treatment of Alzheimer's has been closely associated with severe adverse effects in the form of: anorexia, muscle cramps and insomniaamongstmanyothers.
EGb 761 is an extract derived from the Ginkgo biloba plant, proposed to be an alternativetodonepezil.
Drug Mechanism of Action
Acts on:
Amyloid aggregation. Neurogenesis.

Amyloidinduced hippocampus celldysfunction.
Drug Mechanism of Action
Acts as acetylcholinesterase (ACh) inhibitors in the brain.
↑amount of ACh at the synaptic cleft for cholinergic neurotransmission which aidsincommunication betweennervecells.
Protects against glutamateinducedtoxicity. Cellsurvival.
Drug Impact
Improves cognitive performance, daily living activities, and overall impression scores.
Disadvantages:
Side effects include: Headaches, rashes and gastrointestinalproblems.
Advantages:
Greaterdrugaccessibility. Moreaffordablecomparedtoitsadversaries. Promotesabreakthroughinherbalmedicine.

Produces a neuroprotective effect in a variety of neurodegenerative disorders. Provides nootropic effects.
EGb 761
Drug Impact
An alternative treatment
Alzheimer's disease (AD): One of the most frequent forms of dementia, neurodegenerative disease, irreversible, and common in elderly.
AD's clinical signs: Gradual cognitive and intellectual deficits, impaired language skills, absent mindedness, and variable degrees of personality changes.
This systematic review and meta-analysis is conducted to determine the effectivity of EGb761 from the extract of Ginkgo biloba as an alternative, accessible, and curative approachinADpatients.
OBJECTIVE METHODS
Keywords: (Donepezil OR Donepezil Hydrochloride) AND (Ginkgo Biloba OR Ginkgo Biloba Extract) AND (Alzheimer’s disease OR Dementia)
DISCUSSION
Utilizing the Mini-Mental Status Exam (MMSE), this review aims to evaluate a wide variety of cognitive functions. In this meta-analysis, a mean difference of 2.43 [1.47, 3.89] toward the EGb 761 group was obtained. This finding indicates that not only does EGb 761 successfully contribute to improving cognitive abilities, which include: language, attention, orientation, memory and computation, but it also suggests that the efficacy for EGb 761 in those with Alzheimer’s disease is stronger than that of donepezil.
On the other hand, IADL examinations revealed no statistically significant differences between EGb 761 and donepezil in terms of treatment outcome on the ability to perform daily living. In a retrospective analysis of demented AD patients aged 80 or older, EGb 761 demonstrates a higher treatment efficacy for IADL through a mean difference of 0.82 [2.25, 3.39]. Although another study reveals a greater outcome in the donepezil group, the mean difference appears as small as -0.69 [0.86, 2.26] – stressing the non-inferiority of EGb 761 towards donepezil in IADL.
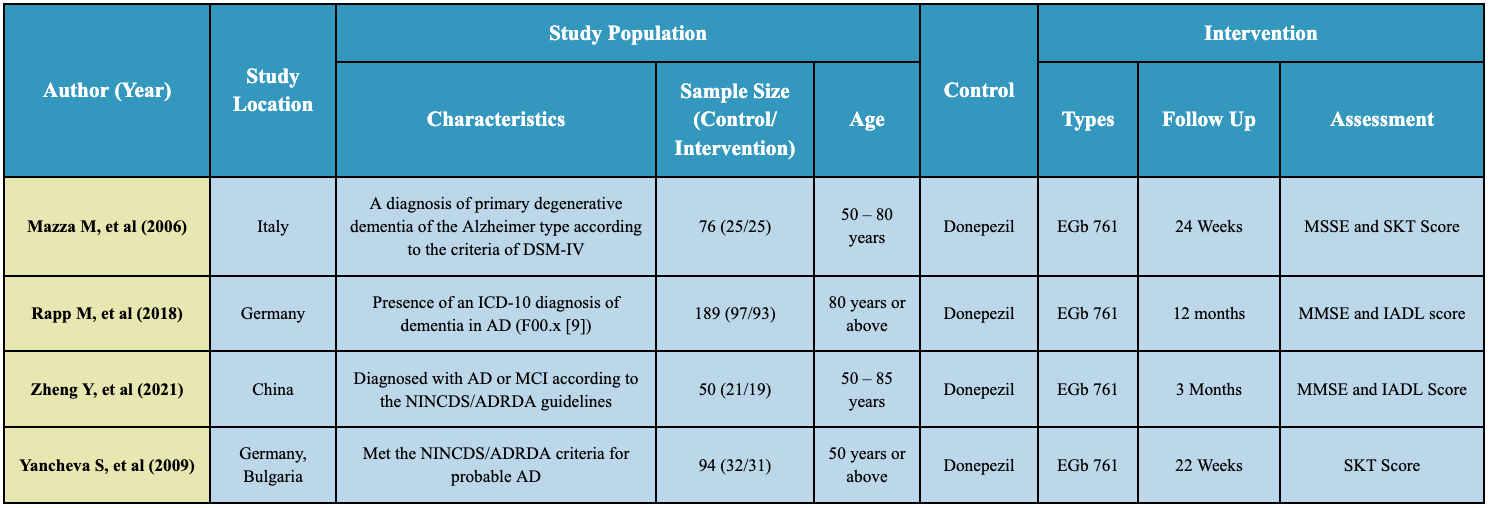
Random-effects meta-analysis using Review Manager 5.4

Bias assessment using Cochrane RoB 2.0
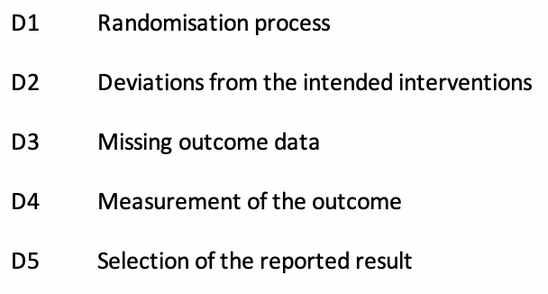
Databases
PubMed, Scopus, Frontiers
Figure 1: PRISMA Flow Chart
Inclusion CriteriaExclusion Criteria
Measures cognitive functions by eitherMMSE, IADL,SKT
Wrong PICO component Irrelevant study or outcomes

Similar results were represented by the non-significant mean differences in SKT (Syndrom Kurz test) which assesses memory and attention to measure dementia severity. Yancheva S, et al. found a mean difference of -1.70 [3.05, 6.35] with higher results on the donepezil group, but through a mean difference of 1.30 [1.85, 4.25], Mazza M, et al. discovered otherwise.



Furthermore, the number of discontinuation owing to adverse effects was greater in the donepezil group (n = 7) than that of EGb 761 (n = 1; 2 = 4.51, df = 1, p 0.05), demonstrating a beneficial impact of therapy on the EGb 761 group. Since there were no statistically significant or clinically pertinent differences between both treatment groups, these results pose a comparable efficacy of EGb 761 towards donepezil on improving cognitive functions – hence, amplifying the possibility of EGb 761 as an alternative approach for Alzheimer’s disease.
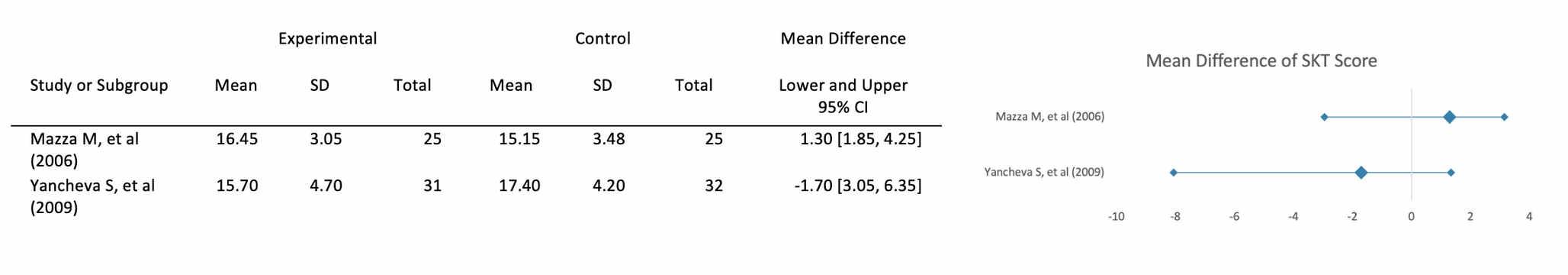
STRENGTHS LIMITATIONS
Among the strengths of our study is the novelty of reckoning the effectivity of EGb 761 on Alzheimer's disease patients. The inclusion of studies in various countries suggests moderate heterogeneity.
CONCLUSION
A low number of studies were included, and were limited in English literature. Different baselines were also utilized in the studies used.
REFERENCES
The use of EGb761 shows promise in improving cognitive abilities in those with Alzheimer’s disease. In comparison to donepezil, EGb761 remains non-inferior to the gold standard in terms of ability to perform daily living as well as attention and memory, with a reduced risk of adverse effects. While studies regarding its potential have only been evident in more recent years, these results may become a lead point for future exploration on refining the management of Alzheimer's disease.
Status Quo Treatment
Shakira Khansa Audie Kurniawan, Richard Nelson Cahya, Viona Titania Riskikallail, Ida Ayu Kyara Ferbena Trininta
Improved blood rheology and vasoregulating ability. Avoids toxin-induced brain edema. Inhibition of platelet activating factor. Neuroprotective action through direct or indirect effects on the nervous system.
Figure 2. Control vs Intervention Meta-Analysis Effect of EGb761 in MSSE Score
Figure 3. Control vs Intervention Meta-Analysis Effect of EGb761 in IADL Score
Figure 4. Control vs Intervention Meta-Analysis Effect of EGb761 in SKT Score
Table 1. Characteristics and Outcomes of Studies
Figure 5. Summary of Risk Bias Assessment
WholeBodyVibrationTechnologyImprovesMobilityandDecreasesFallRiskin
Post-StrokeElderly:AMeta-AnalysisofRandomizedControlledTrials
AnandaPipphaliVidya,KarenEllioraUtama,JansenJayadi,StephanieAmabellaPrayogo [CorrespondenceE-mail:anandapipphalividya@gmail.com]
Introduction: Strokeisasignificantandemergingglobalhealthburden,with50%ofstroke casesoccurringinelderlypopulation.Mobilityandfallriskaretwomajorconcernsin post-strokeelderly.Wholebodyvibration(WBV)isatechnologydevelopedforhelping peopletrainphysicalfunctionandfoundmoreeffectiveinelderlywithlackofphysical mobility.VariousoutcomesobtainedfromstudiesevaluatingtheusageofWBVfor post-strokeelderly.Thus,ameta-analysispresenceneededtoestablishclearrisksand benefits.
Objective: Wewouldliketoincludepost-strokeelderlyandinvestigatetheroleofWBVin improvingmobilityanddecreasingfallrisk.
Method: ThisstudywasconductedusingPreferredReportingItemsofSystematicReview andMeta-Analysis(PRISMA)reportingguidelinesonseveraldatabases.Articlescreening, selectionanddataextractionweredoneindependentlybytheauthors.Quantitativeanalysis wasdoneusingReviewManager5.4Software,whileriskofbiaswasassessedusingthe CochraneRoB2.0tool.
Results: Sevenstudieswithmostlylowriskofbiaswereincluded.Improvementofmobility andreducingfallriskwerefound,observedinreduceTimeUpandGoTest(TUG)(MD -3.05[95%CI-5.92,-0.18;p=0.04])andincrease6MinuteWalkingTestdistance(MD6.18 [95%CI-27.80,40.16;p=0.72]).Furthersubgroupanalysisspecificallyshowedbetter performanceofLowWBV(LWBV)withanMDof-3.44[95%CI-7.88,1.00;p=0.13] comparedHighWBV(HWBV)withanMDof-1.67[95%CI-5.00,1.67;p=0.33].Other thanthat,LWBVwasreportedtobesaferthanHWBV.
Conclusion: Wholebodyvibrationisbeneficialfortheimprovementofmobilityand reducingthefallriskinpost-strokeelderly.However,futurelargerscalestudieshavetobe conductedtofurtherconfirmtheeffectivenessandsafetyofWBV,bothHWBVandLWBV forpost-strokeelderly.
Keywords: Geriatric,Elderly,Post-stroke,Wholebodyvibration,WBV,mobility,fallrisk

EFFECTIVITYofACTIVEMUSICTHERAPYinCOGNITIVE,DEPRESSION,and QUALITYofLIFESCOREofDEMENTIAPATIENTS:SYSTEMATICREVIEWand META-ANALYSIS
TeresaAlmadita,FilzatuzZahroIbrahim,FarahiyahSharfinaSaputri,MuhammadRicoAbdul Karim
Introduction: Dementiastillbecomesamajorpublichealthproblemduetounavailabilityof definitivetreatment.Recentstudiesstatethatmusictherapyisapromisingandpotentially cost-effectivenon-pharmacologicalapproachforpeoplewithdementia.Thereisstillno systematicreviewandmeta-analysesassessingactivemusictherapyeffectivenessonimproving cognitive,depression,andqualityoflifeindementiapeople.
Objective: Thisreviewaimstodeterminetheeffectivenessofactivemusictherapyon improvingcognitive,depression,andqualityoflifeinpeoplewithdementia.
Method: AsystematicreviewwasconductedbasedonPRISMAGuidelinesthroughPubMed, Scopus,Cochrane,Wiley,ProQuest,TaylorandFrancisuntilApril10,2023.TheCochraneRoB 2.0instrumentwasusedtoanalyzethequalityoftheliterature.Byusingthecombinedfixed effectsmodel(pooledStandardizedMeanDifferenceandStandardDeviationchangesfromthe baseline),efficacyandqualityoflifescoresquantitatively.
Result: Activemusictherapyshowsapositiveimpactoncognitive,qualityoflife,and depressionscoresofpatientswithdementia.Thismeta-analysisshowedthatactivemusic therapyhavemorestatisticallysignificanteffectinimprovingcognitivescorecomparedto normal(pooledSMD=+0.65,95%CI:0.05-1.25,p=0.03,).Ourmeta-analysis
��2 = 95% resultalsosuggestedaneffectinqualityoflifeimprovement(pooledSMD=+0.10,95%CI: -0.11-0.32,p=0.35,)anddepressionscorereduction(pooledSMD=-0.12,95%CI:
-0.29-0.04,p=0.15,)althoughnotstatisticallysignificant.
Conclusion: Thisstudyprovidesvaluableevidencetosupporttheuseofthistherapyasa supportivenon-pharmacologicaltreatmentalongwithdementiatreatmentguidelines.Future studiesshouldfocusonspecifictypesofdementiaandshouldassessmorestudies.
Keyword: Activemusictherapy,Dementia,Cognitive,QualityofLife,Depression
��2 =0%
��2 =0%

EFFECTIVENESSOFAICHIAQUATICPROGRAMFORPAINCONTROLAND MOBILEFUNCTIONALITYINPARKINSONDISEASEPATIENTS:SYSTEMATIC REVIEWANDMETA-ANALYSIS
AngelicaAlethaAlegria,AudreyGunawan,PutuMoradhaKharismaPutri,AlifiaDaffa Alfarizy,NathaliaAngelina
[CorrespondenceE-mail: angelicaaletha2@gmail.com]
Introduction: Parkinson'sdiseaseistheneurologicalconditionwiththefastestglobalgrowth rateandiscurrentlytheleadingcauseofdisability.Parkinson'sdiseasehaslongbeen consideredararedisease.However,demographyandconsequencesofindustrializationhave resultedinaParkinson'spandemicthatwilldemandincreasedactivity,targetedplanning,and creativeapproaches.Thus,seeingalimitationinpharmacologicaltreatment,exerciseshould beprescribedandencouragedinallPDpatients.StudiesshowthatAiChiisapromisingand practicalaquatictreatmentforenhancingpainperceptionandfunctionalcapacityinpatients withmildormoderateParkinson'sdisease.ThereforeithasthepotentialtobeappliedinPD rehabilitation.
Objective:DeterminetheeffectivenessoftheAiChiAquaticProgramincontrollingpain andincreasingmobilefunctionalityinpeoplewithParkinson’sdisease.
Methods: ThisstudyusedthePreferredReportingItemsofSystematicReviewand Meta-Analysis(PRISMA).WesystematicallysearchedPubmed,Proquest,GoogleScholar, andWiley.IncludeddocumentswerefurtherassessedforriskofbiasusingtheCochraneRisk ofBias2.0.Effectestimateswerepooledusingrandomeffectsofmeta-analysiswithReview Manager5.4.
ResultsandDiscussion: 6randomizedandnon-randomizedcontrolledstudiesaccumulating 159participantsareincludedinoursystematicreview.Themeta-analysisresultsshowthatAi ChisignificantlyimprovedthecontrolofpainwithaVisualAnalogScale(VAS)MDof-2.36 (p<0.00001;95%CI:-3.62to-1.09;I2 =17%)aswellasmobilefunctionalitywithaTimed UpandGoTest(TGUGT)MDof-1.5(p=0.0003;95%CI:-1.98to-1.02;I2 =0%)
Conclusion: AiChiAquaticProgramsignificantlyimprovedpaincontrolandmobile functionalityinPDpatients.Therefore,iftheresourcesareavailableforitsimplementation, thisisarehabilitationoptionthatneurologistsandotherhealthcareprofessionalsinvolvedin neurorehabilitationshouldconsider.
Keywords: AiChi,aquaticprogram,mobilefunctionality,pain,Parkinson'sdisease,water exercise
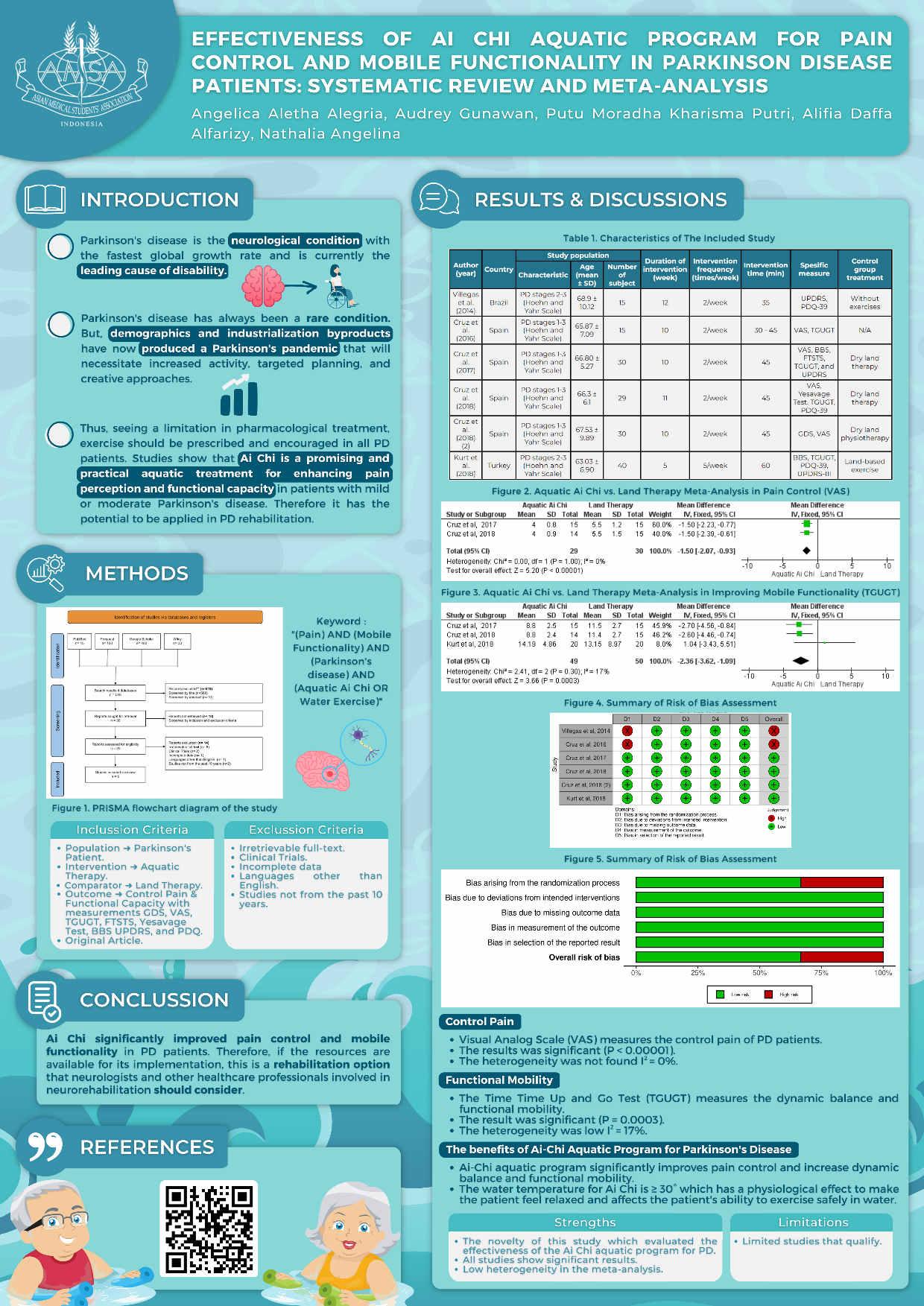
EFFICACYOFPROBIOTICSASADJUNCTIVETHERAPYONEARLYTO MODERATESTAGEALZHEIMER’SDISEASE:AMETAANALYSIS
RosalieDorothea1 ,NailaNirmalaPuspitasari2 ,VaniaAgustine3 ,MuhammadKemas Khadafi4
FacultyofMedicine,UniversitasSriwijaya
Introduction:
Alzheimerdiseaseisthemostcommonformofdementiaforabout60–70%ofcasesandover 60%liveinlow-andmiddle-incomecountries.PharmacologicaltherapyforAlzheimer'sis stilllimited,andthereisnodrugthatcancompletelycureAlzheimer's.Therefore,finding alternativetreatmentsthatareeffectiveandsafeisbecomingincreasinglyimportant,and probioticsofferpotentialasoneofthesealternatives. Duetoitsfatalityandcausinga progressivedeclineincognitivefunction,Probioticswasproventorestorethehomeostasisof gutmicrobiotaanddelaytheprogressionofAlzheimerDisease.Therearenosideeffectsthat havebeenreportedfortheusageofprobioticsforAD. Thus,itisalsonecessarytoidentify thatprobioticsisworthbeinginculcatedinthetherapeuticfieldtotreatAlzheimer.
Objective:
Thismeta-analysisisaimedtoinvestigatetheoveralleffectivenessofprobioticsinreducing theriskofAlzheimer'sdisease.
Methods:
WesearchedliteraturesfromdatabasessuchasEBSCO,Embase,ProQuest,PubMed,and Scopusandfound434literatures.Afterconsideringourinclusionandexclusioncriteria,we foundfourfull-textarticlestoassess. Ameta-analysiswasconductedusingRevMan5.4to computethesummaryofmeandifference(MD)and95%confidenceintervals(CI)forthe effectofprobioticsoncognitivefunction.
Result:
Weanalyzedfourfull-textarticlesandwefoundnosignificantdifferencebetweenprobiotic interventiongroupandplacebooncognitivefunctionimprovement.However,onthe parameterofplasmamalondialdehyde(MDA),probioticsinterventiongroupshows significantresultcomparedtoplacebo.
Conclusion:
Fromourmeta-analysis,weconcludethatprobioticshasn’tshownanyclearevidencetouse onAlzheimer’sDiseasepatientsonthebasisofimprovingthecognitivefunction.However, furtherresearchonprobioticseffectonoxidativemarkerisneededtounderstandhow probioticscanhelptoimproveoxidativemarker(plasmaMDA)onADpatients.
Keywords:
Alzheimer’sDisease,CognitiveFunction,Probiotics
Efficacy of Probiotics as Adjunctive Therapy on Alzheimer's Disease: A Meta Analysis
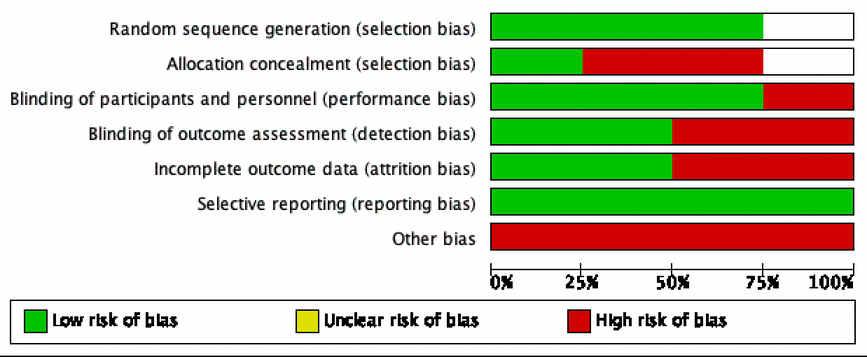

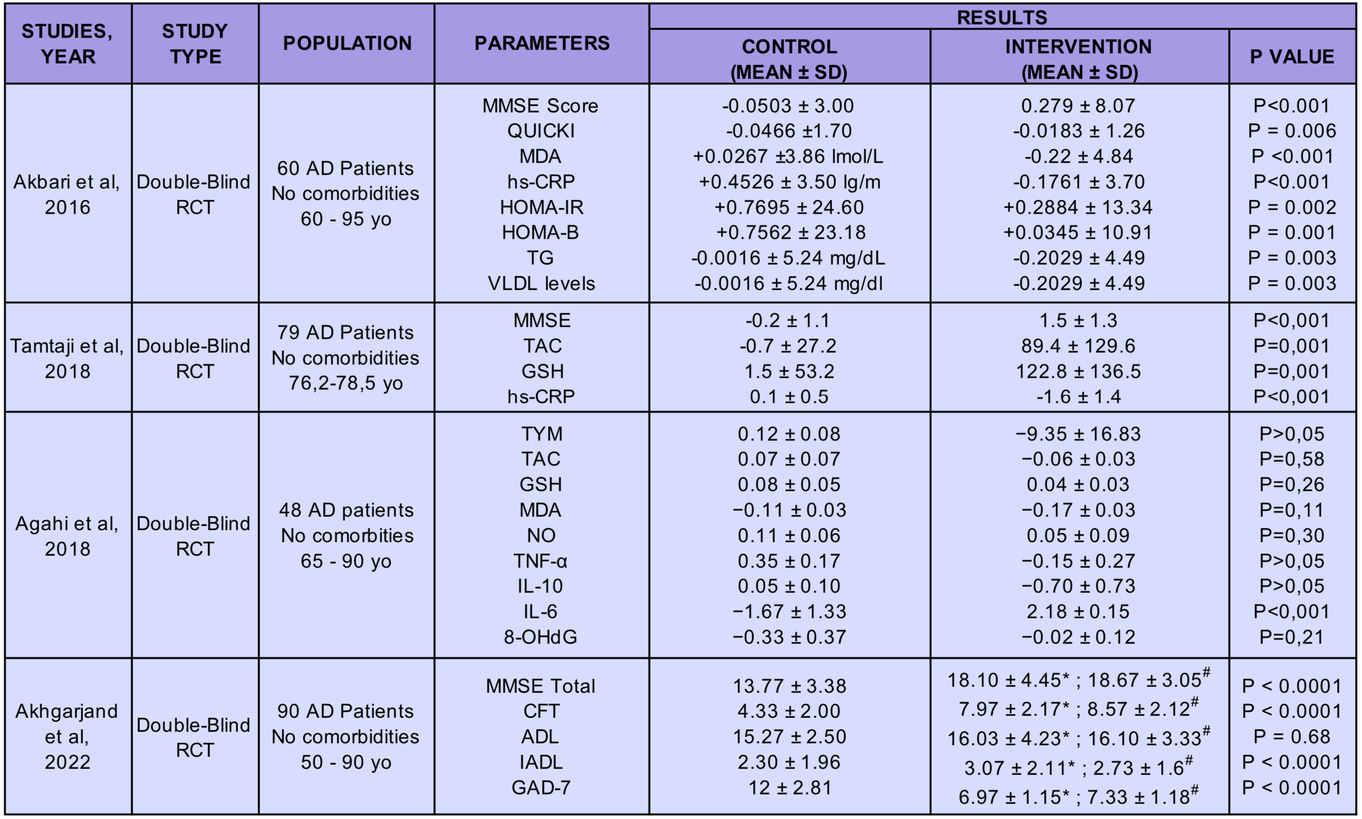
Rosalie Dorothea, Naila Nirmala Puspitasari, Vania Agustine, Muhammad Kemas Khadafi

Introduction
the most common type of dementia for about of cases 60-70%

was proven
Probiotics
Method
to restore the homeostasis of gut microbiota and has significant potential in deceleration of Alzheimer’s disease and delay the progression of Alzheimer Disease demonstrated significant potential in deceleration of Alzheimer’s disease and delay the progression of Alzheimer Disease
Pharmacological therapy for Alzheimer's is still limited and there is no drug that can completely cure Alzheimer's.
Objective
To assess the effectiveness of probiotics to reduce cognitive impairment for geriatric with Alzheimer's, especially above 65 years old
To identify whether probiotics could be adjunctive therapeutic in the treatment of Alzheimer's disease
Results and Discussion
1. Randomized controlled trials (RCTs)
2. Conducted on human subjects with a diagnosis Alzheimer's disease
3. Investigating the effect of probiotics as an adjunctive therapy to standard care

4. Report outcomes such as cognitive function, quality of life, or adverse events
Inclusion Criteria Exclusion Criteria
1. Investigated probiotics as a sole intervention

2. Did not include a control group
3. Not in english
Keyword
"Alzheimer Disease", "Cognitive Impairment", "Probiotics", and its related terms with boolean operator
Databases
Cognitive Function Plasma
Probiotic supplementation, compared with placebo, on the cognitive function of individuals withAlzheimer’sdisease
SDM=1.16;95%CI,0.22to2.10;P=0,02,I2=91% sothereisnosignificanteffect

Probiotics significantly improved on plasma malondialdehyde compared with placebo on individualswithAlzheimer'sDisease

MD = 0.39 lmol/L; 95%CI, 0.73 to 0.06 lmol/L; P = 0.60,I2=97%withsignificantheterogeneity


How Probiotics can Affect Cognitive Function on AD Patients
The relationship between probiotics and cognition is not fully understood yet. However, a pathway called the microbiota-gut-brain axis (MGBA) that constantly transmits and interprets information from the periphery to the brain and back. Probiotics utilize a beneficial effect on MGBA by preventing the hyperactivation of hypothalamic-pituitary-adrenal axis following gut microbiota dysbiosis and inflammatory processes. [5,3]MGBA is a modifiable target with certain probiotics for potential psychobioticsinthetreatmentofcognitivefunction.[5]
Conclusion and Recommendation
From our meta-analysis, we conclude that probiotics hasn’t shown any clear evidence to use on Alzheimer’s Disease patients on the basis of improving the cognitive function. However, further research on probiotics effect on oxidative marker is needed to understand how probiotics can help to improve oxidative marker (plasma MDA) on AD patients.
References
Acknowledgement and Conflict of Interest
There is no conflict of interest and acknowledgements within this study
2 Probiotics Treatment
year-old and older
Alzheimer’s Disease 1 in 65
EBSCO, Embase, ProQuest, Pubmed, Scopus Figure 2. Forest Plot of the Effect of Probiotic vs Placebo on Cognitive Function
Malondialdehyde
Therefore, finding alternative treatments that are effective and safe is becoming increasingly important, and probiotics offer potential as one of these alternatives Table 1. Characteristic of Studies Table 2. Outcomes of Studies
Figure 3. Forest Plot for Studies the Effect of Probiotic vs Placebo Administration in Individuals with AD: Plasma Malondialdehyde Figure 4. Risk of Bias Assesment Figure 1. Prism Strategy
EfficacyofVitaminB12forNerveRepairinElderlywithTrigeminalNeuralgia:A SystematicReview
DhianiEkaPutri,AsiyaAudah,AnnisaNurulHamidah,WildanAlexandraMuhammad
Introduction: Trigeminalneuralgiaaffects4to13per100000peopleannuallywithmost casesoccurringafterage50.Thecurrentfirst-linetreatment,carbamazepine,isknownto increasetheriskofStevens-JohnsonsyndromeinpatientswithAsianancestry.Thehigh morbidityofthediseaseandthepotentialriskofcurrenttreatmenturgetheneedforpossible alternativetreatment.Researchshowsstrongevidenceforanerve-regeneratingfunctionof vitaminB12(cobalamin)whichmighthaveapositiveeffectonpatientswithtrigeminal neuralgia.
Objective: ToinvestigatetheefficacyofVitaminB12fornerverepairinelderlywith trigeminalneuralgia
Method: Cohortclinicalstudiesfromvariousdatabases(PubMed,CochraneLibrary,Science Direct,andGoogleScholar),resultingin101journalstobescreenedusing Preferred ReportingItemsforSystematicReviewsandMeta-Analyses(PRISMA)guidelines. Fromthe inclusionandexclusioncriteriaspecified,intotal3journalswereincludedandaccessedfor theirqualityusingRiskOfBiasInNon-RandomizedStudies-ofInterventions(ROBINS-I).
Results: TherearesignificantimprovementsinvitaminB12supplementationforpatients withtrigeminalneuralgia.AsvitaminB12wasfoundtobeabletobeprotectiveagainst neurotoxicitybyenhancingbraincellmethylation,alowlevelofvitaminB12hasincreased theriskoftrigeminalneuralgiacasesin23%ofpatientsevaluated. Presentstudyrevealeda statisticallysignificantcorrelation(p=0.001)betweenthedurationofpainandmeanserum vitaminB12levelsofTrigeminalNeuralgiapatients.Thisshowsthatthedurationofpain increasesastheserumvitaminB12leveldecreases.
Conclusion: ThisreviewsuggeststhatVitaminB12iseffectivefornerverepairinelderly withTrigeminalNeuralgia,alsoitdeterminestheriskfactorofTrigeminalNeuralgiacases amongelderly.Thoughavailable,evidenceaccessedinthisisverylimited,severalstudies reviewedshowsthatvitaminB12hasthepotentialtoenhancenerverepair.However,further studiesonthistopicareencouraged.
Keywords: Elderly,TrigeminalNeuralgia,VitaminB12

Dark Chocolate and Its Effect on Enhancing Cognitive Function of Elderly
Rafi Rahman, Hudayah Apryanita, Attha Ghaly Ridho Ananda, Fella Nadiyatul Husna
ABSTRACT
Introduction: One of the most prevalent health issues affecting the elderly is cognitive impairment. Evidence suggests that some chocolate varieties may have health advantages due to the high polyphenol content, especially flavanols, present in the non-fat solids of cocoa liquor. In the Cacao, Cognition, and Aging (CoCoA) Study, it was discovered that giving elderlypersonswithmildcognitiveimpairmentabeverageenrichedwithcocoaflavanols(CFs) improved their cognitive function.
Objective: To know the effect of dark chocolate on cognitive function of elderly.
Method: This systematic review and meta-analysis of randomized controlled trials was conducted using the PRISMA guideline and statement, with inclusion and exclusion criteria for articles published in the last 10 years, fully accessible, written in English, and using elderly and in good health participants.
Results: Dark chocolate intake has been shown to have a positive effect on cognitive function, with scores on Verbal Fluency, Trail Making Test A, and Trail Making Test B increasing significantly. Daily cocoa flavanols consumption can also increase cognitive function, with scores on Verbal Fluency, Trail Making Test A, and Trail Making Test B increasing significantly.
Conclusion: The overall findings of this systematic review show that the intake of dark chocolate may increase the cognitive function in the elderly, but further research might have to be conducted more since there was a different result corresponding to the articles that is included.
Keywords: cognitive function, dark chocolate, elderly
DARK CHOCOLATE AND ITS EFFECT ON ENHANCING COGNITIVE FUNCTION OF ELDERLY
Rafi Rahman, Hudayah Apryanita, Attha Ghaly Ridho Ananda, Fella Nadiyatul Husna
INTRODUCTION
One of the most prevalent health issues affecting the elderly is cognitive impairment [5]. It is crucial to discover effective strategies for maintaining cognitive function to lessen the substantial societal burden brought on by Alzheimer's disease (AD) and associated dementia, which afflict more than 46 million people globally [3]. Though some areas of cognitive function, such as processing speed, working memory capacity, inhibitory processes, and long-term memory, are typically accompanied by deficits as people age. Several studies have examined the connection between consuming particular foods and preventing dementia [2]. Evidence suggests that some chocolate varieties may have health advantages due to the high polyphenol content, especially flavanols, present in the non-fat solids of cocoa liquor [4]. In the Cacao, Cognition, and Aging (CoCoA) Study, it was discovered that giving elderly persons with mild cognitive impairment a beverage enriched with cocoa flavanols (CFs) improved their cognitive function [1]. Consuming cocoa flavanols on a regular basis may prevent cognitive decline by improved cerebral vasodilatation [3]. According to a recent analysis, greater doses of cocoa flavanols (500-750 mg/day) seem to be most beneficial for memory and executive function [3].
METHOD
1. This systematic review and meta-analysis of randomized controlled trial was conducted based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline and statement.

2. Articles used in this review were randomized controlled trials. Review, case report, case series, cohort, study protocol, and letter to editor were excluded.
3. The inclusion and exclusion criteria used in this review were following: articles published in the last 10 years, fully accessible, articles were written in English, using participants who are elderly and in good health. Participants who were given the dark chocolate intervention to measure cognitive function. The articles which did not meet the inclusion criteria were excluded.
4. The selected studies quality was assessedusing the Risk of Bias tool for Randomized trials (RoB 2).
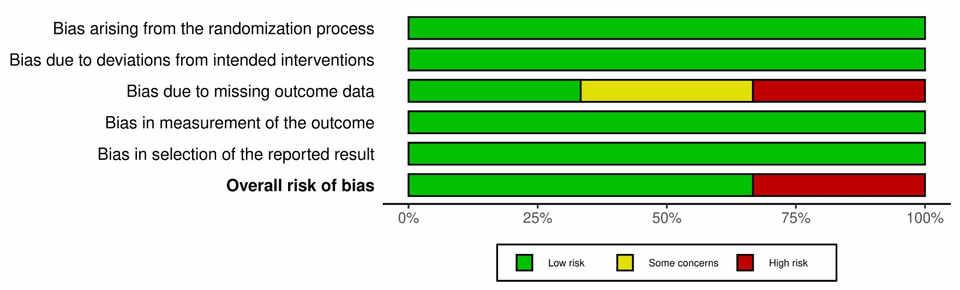

RESULT
ACKNOWLEDGEMENTS AND CONFLICT OF INTEREST
DISCUSSION & LIMITATIONS
We aim to acknowledge the effect of dark chocolate intake on the cognitive function of the elderly. There was clearly a significant result that may be implicated with the intake of dark chocolate and its compound related to cognitive function. From a total of three studies that are reviewed, with the total sample of 2,431 people, with 1,197 people in the intervention group, with 1,234 people as a control group. The studies also have different ranges of tests to conduct but still have some similarities between the tests. The test taken was MMSE, verbal fluency test (VFT), trail making test A (TMT-A), and trail making test B (TMT-B). For each of the tests there was also a range of normal results. MMSE has a normal result with a score of 25 or higher [6]. For VFT, count up the total number of words that an individual is able to produce, a score of under 17 indicates concern [7]. The TMT-A and TMT-B specifically take the cut off at over 79 and over 273 sequentially [8].
The study from Baker L, et al. (2022) showed that cocoa extract has a positive effect on cognitive function. It’s shown by the score on Verbal Fluency test (34,89 ± 8,26), Trail Making Test A (9 (8,11)), and Trail Making Test B (30 (24,46)).
However, Ichinose T, et al. (2020) showed that there were no differences between the DHA group and placebo group on cognitive function evaluation. The MMSE score was 27,4 ± 3,5 for the DHA group and 28,0 ± 3,3 for the placebo group. Mastroiacovo D, et al. (2015) showed that daily cocoa flavanols consumption can increase cognitive function. It’s shown by the score on MMSE (29,20 ± 0,17), Verbal Fluency Test (32,58 ± 1,60), Trail Making Test A (25, 25 ± 1,45), and Trail Making Test B (62,71 ± 2,80). All studies have pointed out that the consumption of dark chocolate considering all of its compounds inside could make a cognitive improvement, except for Ichinose T, et al (2020) stating no correlation between DHA intake and cognitive function.
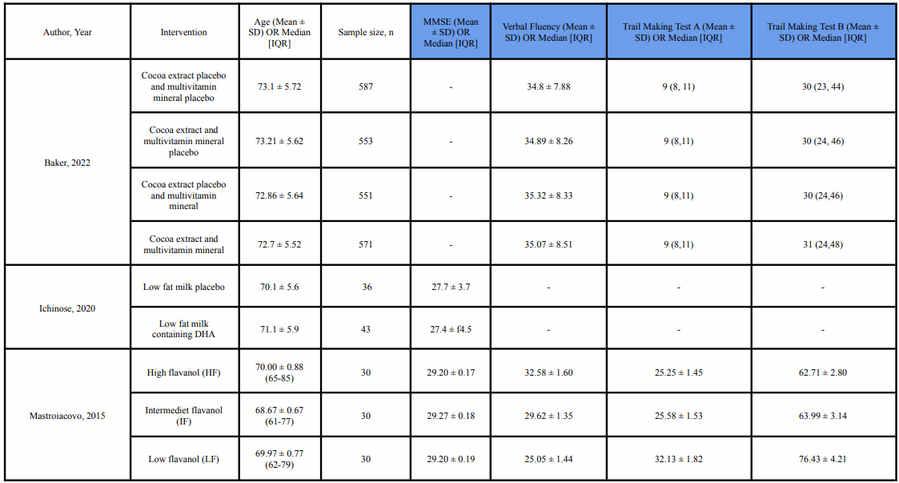
The limitation of the study from Baker, L et al. (2022) is the race and ethnicity of the cohort was not representative of older Americans, which affects generalizability of the results. The limitations of the study from Ichinose T, et al. (2020) are the study conducted on a small sample size of only 87 participants, which may limit the generalizability of the findings to larger populations. Additionally, the study was conducted on healthy elderly Japanese people, so the results may not apply to elderly individuals with health issues or from different cultural backgrounds. The limitation of the study from Mastroiacovo D, et al. (2015) is that the study was conducted on a relatively small sample size of only 90 participants, which may limit the generalizability of the findings to larger populations. In addition, the study only lasted for 8 weeks, so the long-term effects of cocoa flavanol consumption on cognitive function are still unknown
CONCLUSION AND RECOMMENDATION

The overall findings of this systematic review show that the intake of dark chocolate may increase the cognitive function in the elderly, but further research might have to be conducted more since there was a different result corresponding to the articles that is included.
Based on the findings of these studies, it can be recommended that regular consumption of cocoa extract or cocoa flavanols may have a positive effect on cognitive function, particularly on verbal fluency and executive function. However, the results on the effect of DHA intake on cognitive function were inconclusive. Therefore, it may be beneficial to incorporate cocoa extract or cocoa flavanols into a balanced diet to potentially improve cognitive function in older adults. However, it's also important to consider individual health conditions and consult with a healthcare professional before making any significant changes to one's diet. Further research is needed to confirm these findings and determine the optimal dose and duration of cocoa extract or cocoa flavanols consumption for cognitive benefits.

REFERENCES
Keywoard: Dark Chocolate, Cognitive Funtion, Elderly
[1] Mastroiacovo D, Kwik-Uribe C, Grassi D, Necozione S, Raffaele A, Pistacchio L, et al.Cocoa flavanol consumption improves cognitive function, blood pressure control, and metabolic profile in elderly subjects: the Cocoa, Cognition, and Aging (CoCoA) Study--a randomized controlled trial. Am J Clin Nutr. 2015 Mar;101(3):538-48. [2] Ichinose T, Matsuzaki K, Kato M, Tanabe Y, Tachibana N, Morikawa M, et al.Intake of Docosahexaenoic Acid-Enriched Milk Beverage Prevents Age-Related Cognitive Decline and Decreases Serum Bone Resorption Marker Levels. J Oleo Sci. 2021 Dec 3;70(12):1829-1838. [3] Baker LD, Manson JE, Rapp SR, Sesso HD, Gaussoin SA, Shumaker SA et al. Effects of cocoa extract and a multivitamin on cognitive function: A randomized clinical trial. Alzheimers Dement. 2022 Sep 14:10.1002/alz.12767. [4] Marsh CE, Carter HH, Guelfi KJ, Smith KJ, Pike KE, Naylor LH, et al. Brachial and Cerebrovascular Functions Are Enhanced in Postmenopausal Women after Ingestion of Chocolate with a High Concentration of Cocoa. J Nutr. 2017 Sep;147(9):1686-1692. [5] Ren L, Zheng Y, Wu L, Gu Y, He Y, Jiang B, et al. Investigation of the prevalence of Cognitive Impairment and its risk factors within the elderly population in Shanghai, China. Sci Rep. 2018 Feb 23;8(1):3575. [6] Bleecker ML, Bolla-Wilson K, Kawas C, Agnew J. Age-specific norms for the Mini-Mental State Exam. Neurology. 1988 Oct;38(10):1565-8. [7] Kim N, Kim JH, Wolters MK, MacPherson SE, Park JC. Automatic Scoring of Semantic Fluency. Front Psychol. 2019 May 16;10:1020. [8] Llinàs-Reglà J, Vilalta-Franch J, López-Pousa S, Calvó-Perxas L, Torrents Rodas D, Garre-Olmo J. The Trail Making Test. Assessment. 2017 Mar;24(2):183-196.
Figure 1. PRISMA Flowchart
Table 1. Study Characteristic
The authors whose names are listed certify that they have NO affiliations with or involvement in any organization or entity with any financial or non-financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements).
Table 2. Efficacy Assesment of MMSE Group, VF Group, TMT A Group, and TMT B Group
Figure 2. Risk of Bias table assessed with RoB 2.0 tool
THEEFFECTOFMEDITERRANEANDIETFORMEMORYIMPROVEMENTAND COGNITIONINELDERLYPOPULATION:ASYSTEMATICREVIEWOFRANDOMIZED CONTROLLEDTRIAL
AlifiahZalikaAzharra,MuhammadFarhanHibatulloh,CandraAgungWibisana,Qotrunada PermataYumna
Introduction: Theelderpopulationisrapidlygrowing,leadingtomoreinstancesofhealth problemssuchascognitiveabilities.MedDiet(MediterraneanDiet)isassociatedwithcaloric restriction,balancednutrientintake,andahighintakeoffishandalcoholtodelaycognitive decline,andthatantioxidant-richdietsmayofferprotectionagainstneurodegenerative disorders.TheMedDietisaplant-based,antioxidant-richdietarypatternthathasbeenlinked tonumeroushealthadvantages,suchasenhancingmemoryinbothcognitivelynormaland cognitivelyimpairedolderpersons,loweringdepressedsymptoms,reducingfrailty,and shorteninghospitalstays.
Objective: TheaimofthissystematicreviewistoanalyzewhethertheMedDietintervention havingeffectivenessforcognitivefunctionandmemoryimprovement,especiallyinelder population.
Method: ThePRISMAguidelineswerefollowedinthissystematicreview.Various electronicdatabases,suchasPubMed,ScienceDirect,CochraneLibrary,Scopus,andGoogle Scholar,wereusedforthestudysearches.Eachstudy'sriskofbiaswasevaluatedusingthe CochraneRiskofBias(RoB)2.0.
Result: Theresultsofthisanalysisshowedthattherewasanimprovementinsomeindicators relatedtothecognitivebrain,suchasMiniMentalStateExamination,ReyAuditoryVerbal LearningTest,andothersinaninsignificantway.DependsonthetypeofMedDiet (Extra-virginOliveOilorNuts)comparedtodietcontrol.
Conclusion: ThissystematicreviewisevidencethatMedDiethasaninfluenceonimproved cognitivefunctionintheelderlyofavarietyofindicators.However,theresultisnot significant.WerecommendthatfurtherresearchbeconductedtoinvestigatehowMedDiet canmaximizetheeffectoncognitivefunction.
Keyword: Cognitivefunction,MediterraneanDiet,Elderly
THE EFFECT OF MEDITERRANEAN DIET FOR MEMORY IMPROVEMENT AND COGNITION IN ELDERLY POPULATION:
A SYSTEMATIC REVIEW OF RANDOMIZED CONTROLLED TRIAL


INTRODUCTION

The elder population is rapidly growing, leading to more instances of health problems such as cognitive abilities [1]. MedDiet (Mediterranean Diet) is associated with caloric restriction, balanced nutrient intake, and a high intake of fish and alcohol to delay cognitive decline [2], and that antioxidant-rich diets may offer protection against neurodegenerative disorders [3]. The MedDiet is a plant-based, antioxidant-rich dietary pattern that has been linked to numerous health advantages, such as enhancing memory in both cognitively normal and cognitively impaired older persons, lowering depressed symptoms, reducing frailty, and shortening hospital stays [4].
RESULT

The aim of this systematic review is to analyze whether the Mediterranean Diet intervention has effectiveness for cognitive function and memory improvement, especially in the elderly.
OBJECTIVE METHODS
Inclusion criteria:

RCT that enrolled elderly participant aged 60 years or over

Mediterranean diet with or without additional supplement as intervention Studies publish in English
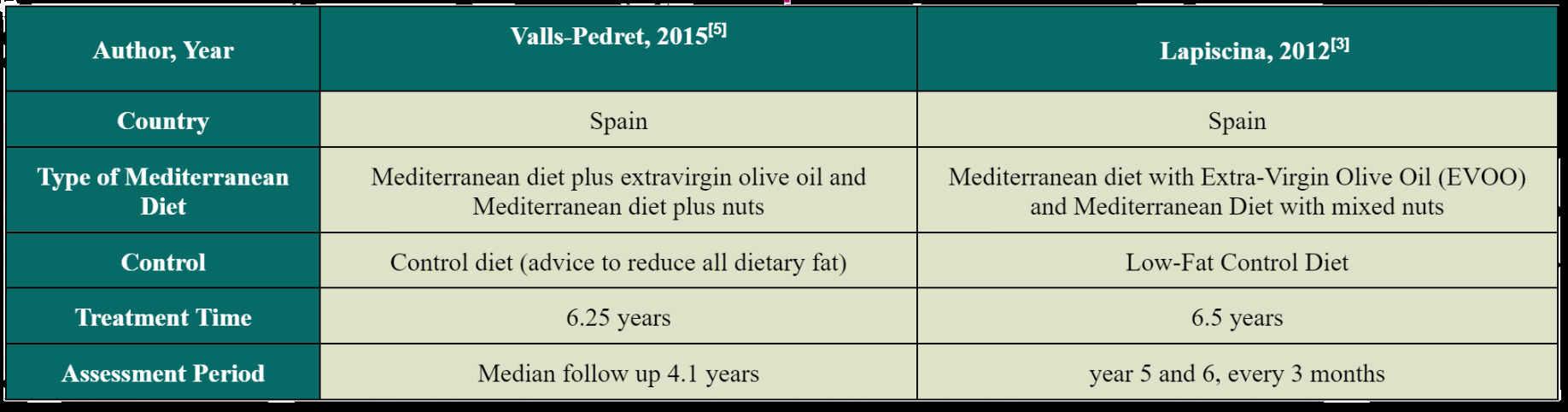
Exclusion criteria:
Irretrievable full text
Inappropriate study type
Incomplete study content Foreign language
Noted: MMSE, Mini Mental State Examination; RAVLT, Rey Auditory Verbal Learning Test.
DISCUSSION
The Potency Mediterranean Diet



The MedDiet (Mediterranean Diet) with characteristics dominated by consumption of vegetables, fruits, whole grains, legumes, unsaturated fatty acids, and modest alcohol consumption with meals is often associated with slowing cognitive decline. Healthy dietary fats and antioxidant- and polyphenol-rich foods abundant in the MedDiet may work synergistically to improve cognitive function through improved glucose metabolism, reduced blood pressure and lipids, and lower systemic inflammation and oxidative stress [6]. Study conducted by Lapiscina, 2013 showed there was an improvement in cognitive function on MMSE (Mini Mental State Examination) indicators among the MedDiet group with Extra-Virgin Olive Oil (EVOO) compared to a control diet of 0.66. For the MedDiet group with mixed nuts there was an increase of 1.35 [4]. In contrast to the study conducted by Valls-Pedret, 2015 [2], the MedDiet group with EVOO increased by 0.05 while the MedDiet group with mixed nuts actually experienced a decrease of 0.08. On other indicators such as Digit Span and Verbal Fluency there was also an improvement in cognitive function in both types of MedDiet compared to the control diet in both studies [2,4].

Strength and Limitation
This is the first systematic review to focus on the effects of the MedDiet on improving cognitive function in healthy older adults. The studies used were also low risk of bias. However, unfortunately that studies that fit our chosen topic are still very minimal. Most similar studies use elderly populations with dementia or alzheimer's as samples. While in this review we want to know how significant the effect of MedDiet for improving cognitive function in the elderly who have not experienced problems in their brain as a preventive measure.
CONCLUSION
This systematic review is evidence that MedDiet has an influence on improved cognitive function in the elderly of a variety of indicators. However, the result is not significant. We recommend that further research be conducted to investigate how MedDiet can maximize the effect on cognitive function.
REFERENCES & SUPLEMENTARY
Systematic review conducted based on PRISMA statement Literature search process conducted with multiple electronic databases: PubMed, Cochraane, ScienceDirect, Springer, and Google Scholar Inclusion and exclusion screening Study selection and quality assessment resulted 2 Randomized Controlled Trial Bias assessment using Risk of Bias tool for Randomized Trials (RoB 2)
Qatrunada Permata Yumna
Figure 1. Conceptual framework
Figure 2. PRISMA 2020 Flow Diagram
1 2 3 4 5
Table 1. Risk of bias table assessed with RoB 2.0 tool
Table 2. Summary of Include Study Result
https://bit.ly/SuplementaryMedDiet
THE POTENCY OF QUERCETIN FOR IMPROVEMENT OF COGNITIVE FUNCTION IN HEALTHY ELDERLY :AMETA-ANALYSIS OF RANDOMIZED CONTROLLED TRIAL
Muhammad Farhan Hibatulloh, Stela Salsabilla Fambudi, Nala Wahyudi, Muhammad Yusuf Fadhil
Introduction: Indonesia has entered the era of aging population. In 2021, the proportion of elderly people in Indonesia reached 10.82 percent or around 29.3 million people. Decreased cognitive function in the elderly can be one of the factors inhibiting the achievement of the elderly demographicbonus. Therefore,aninterventionisneededthatcanimprovethecognitive abilities of the elderly and is easy to apply in everyday life. Quercetin is a natural compound that belongs to the flavonoid group of plants. Quercetin has antioxidant and anti-inflammatory properties that have been reported to be good for brain health by protecting it from diseases such as Alzheimer's and dementia. Therefore, the neuroprotective effects of Quercetin make it an attractive choice for possible development of clinical application in humans.
Objective: This systematic review and meta-analysis aimed to find out whether the innovative use of Quercetin can improve cognitive function in healthy elderly.
Methods: This systematic review followed the guidelines provided by PRISMA. Study searches wereconducted throughvarious electronicdatabases, such as PubMed,ScienceDirect, Cochrane Library, Scopus and Google Scholar. The risk bias assessment of each study was carried out using the Cochrane Risk of Bias (RoB) 2.0
Results: The results of the efficacy analysis showed that there was no significant difference between the control group and the experimental group in MMSE (Mini Mental State Examination) scores.
Conclusion: This systematic review and meta-analysis is evidence that the utilization of quercetin for improving cognitive function in the elderly with MMSE is less significant. We recommend further research examining the use of quercetin with improved dose, dosage, treatment time, and other aspects to maximize the effect of quercetin.
Keywords: Cognitive Function, Elderly, Quercetin
THE POTENCY OF QUERCETIN FOR THE IMPROVEMENT OF COGNITIVE THE POTENCY OF QUERCETIN FOR THE IMPROVEMENT OF COGNITIVE FUNCTION IN HEALTHY ELDERLY : A META-ANALYSIS OF A RANDOMIZED FUNCTION IN HEALTHY ELDERLY : A META-ANALYSIS OF A RANDOMIZED CONTROLLED TRIAL CONTROLLED TRIAL
Muhammad Farhan Hibatulloh - Stela Salsabilla Fambudi - Nala Wahyudi - Muhammad Yusuf Fadhil
Indonesia has entered the era of an aging population. In 2021, the proportion of elderly people in Indonesia reached 10.82 percent, or around 29.3 million people [1].

The aging population phenomenon can be a second demographic bonus if the elderly population is still productive. [2]. However, the elderly are a group that is vulnerable to various diseases due to the decline in various physiological functions of organs in the body [3]. Cognitive function decline is no exception. Decreased cognitive function in the elderly can be one of the factors inhibiting the achievement of the elderly demographic bonus [4]. Therefore, an intervention is needed that can improve the cognitive abilities of the elderly and is easy to apply in everyday life. One of them is the administration of quercetin, which can be found in various types of fruits and vegetables [5].
Quercetin is a natural compound that belongs to the flavonoid group of plants [6]. Quercetin has antioxidant and anti-inflammatory properties that have been reported to be good for brain health by protecting it from diseases such as Alzheimer's and dementia [7]. In an animal study, mice that received quercetin injections every two days for three months experienced a reduction in Alzheimer's markers [8]. Therefore, the neuroprotective effects of quercetin make it an attractive choice for the possible development of clinical applications in humans.
This systematic review and meta-analysis aimed to find out whether the innovative use of quercetin can improve the cognitive function in healthy elderly.
INTRODUCTION OBJECTIVE METHODS
RESULTS DISCUSSION
placebocontrolled trial
Double-blind, randomized, placebo -controlled trial


Placebo-controlled, randomized, double-blind, and parallel-group study
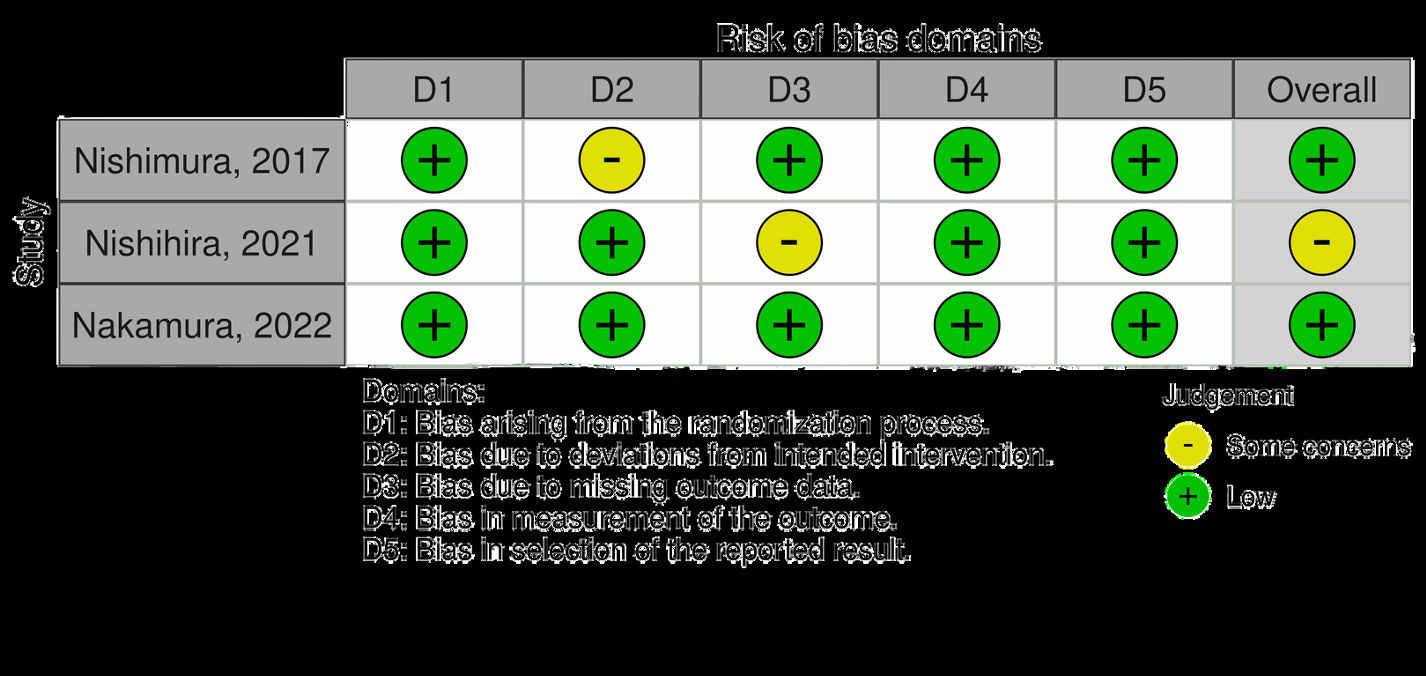
weeks 0, 12, and 24 after the start of therapy
occurred at baseline and post 40 weeks of intake (Week 40)
The Potency of Quercetin
Quercetin has been considered to have many benefits, such as being an antiallergen [12], inhibiting LDL oxidation [13], antiinflammatory, anti-cancer [14], preventing diabetic complications [15], and a strong antioxidant [16]. However, quercetin is more well known as the anti-inflammatory and antioxidant agent that also contributes as a neuroprotective agent [17]. Our meta-analysis suggested insignificant effects for Mini-Mental State Examination (MMSE) scores. We analyzed the results using a forest plot, as can be seen in Figure 3. This meta-analysis in Figure 3 shows that quercetin cannot improve MMSE scores compared to control. There are several reasons why quercetin cannot significantly improve cognitive ability. Based on one study [18], it is said that quercetin has difficulty penetrating the BBB due to its small particle size. Therefore, the bioavailability of quercetin in circulating blood vessels in the brain is low. Besides, quercetin consumption should also be followed by other physical activities in order to get maximum results [19]. In the 3 inclusion studies we selected, all subjects were not encouraged to do sports or other physical activities [9,10,11]. It was also explained in one study that it takes a long time to determine the effect of quercetin on improving cognitive abilities [18]. In the 3 inclusion studies we selected, the treatment period was 6 and 10 months [9,10,11].
We also evaluated one study that cannot be meta-analyzed. A study showed significant cognition-enhancing effects by increasing the percentage of memory and accuracy response tests [20]. In addition, the study also reported the decreased activities of AChE, MAO-A, and MAO-B in serum, leading to the enhancement of synaptic transmission and synchronization of neurons, which play a role in improving attention and cognitive functions.
Safety and Other Effects
Several studies reported that quercetin had positive effects on cognitive function, with MMSE scores as the primary endpoint [9,10]. Besides, one of the three studies revealed that some subjects showed side effects experiencing only mild symptoms and recovered from those symptoms within a few days [9]. It was mentioned in the study that quercetin has some other beneficial effects on the vascular system, leading to changes in cerebrovascular blood flow, which in turn can alter neuronal morphology, causing neurogenesis and angiogenesis [9]. In addition, intake of quercetin glycosides as a beverage can improve reaction time and potentially inhibit the decline in CBF and suppress the accumulation of Aβ in the brain [11].
Strength and Limitation

This is the first systematic review and meta-analysis using Randomized Controlled Trial that evaluates quercetin for improvement of cognitive function, especially in the elderly. This review is also made mostly by using low risk of bias studies. Besides, our included studies are homogeneous (I² = 0%) and the samples provide a mean ± SD (Standard Deviation) for the MMSE. However,the number of studies discussing the utilization of quercetin to improve cognitive function in the elderly is still very small. Although our study shows an insignificant result and has some limitations, we still suggest that administration of quercetin is still potential for healthy elderly to improve cognitive function or even other health conditions.

REFERENCES & SUPLEMENTARY
This systematic review and meta-analysis is evidence that the utilization of quercetin for improving cognitive function in the elderly with MMSE (Mini mental state examination) indicators is less significant. We recommend further research examining the use of quercetin with improved dose, dosage, treatment time, and other aspectstomaximizetheeffectofquercetin.

MMSE (Mean ± SD) CADi2 (Mean ± SD)
CONCLUSION &
Figure
ConceptualFramework Irrelevantoutcomes Reviewarticles Ambiguity in study design (original research,non-RCT) Irretrievablefull-textarticles Exclusion Criteria Randomized Controlled Trial that enrolledhealthyelderlypatients Intervention in the form of Quercetin The control group received ingredients that did not contain quercetinasacomparison StudiespublishedinEnglish Inclusion Criteria : The literature search process was carried out with multiple electronic databases PubMed, Cochrane, ScienceDirect, Scopus and Google Scholar Systematic review conducted based on PRISMA statement Study selection and quality assessment yielded 3 Randomized trials (RoB 2) We will perform a meta-analysis using Revman v5.4 The Meta-analysis will be presented as forest plot, focused on the effect of Quercetin on cognitive function in healthy elderly (Mini Mental State Examination (MMSE)) Quercetin Placebo Total Cholesterols (Mean ± SD) Author, year Country Study Design Sample size, n (Quercetin/Control) Quercetin Source Form Placebo Dosage Route of Intervention Treatment Time Assessment Period Adverse Reactions Age (Mean ± SD) Nishimura et al, 2017 Japan 50 (25/25) 71.52 ± 4.67 71.96 ± 5.05 Quergold and Sarasaragold onion Onion powder White onion 10g powder/day Oral 24 weeks 28.32 ± 1.65 27.92 ± 1.75 NI NI 215.12 ± 40.00 220.80 ± 40.75 Mild symptoms 28.9 ± 3.5 28.5 ± 2.6 9.3 ± 1.9 9.0 ± 2.0 235 ± 54 228 ± 68 NI 28.2 ±1.6 28.3 ±1.9 NI NI 234.6 ± 30.8 245.0 ± 36.2 NI Asessment occurred
Assessment
Assessment
0, 12,
24 weeks 40 weeks OralOral 11g powder/day 500 mL barley tea/day White onion Beverage without quercetin glycosides Onion powderBarley tea 71 ± 4 Quercetin-rich Sarasara Gold onion Quercetin glycosides 65.3 ± 3.6 69 ± 4 67.1 ± 3.8 Double-blind,
Nishihira et al, 2021 Japan 61 (28/33)68 (33/35)
RECOMENDATION
1.
on
occurred on
and 24 weeks
Nakamura et al,
Japan
2022
Quercetin Quercetin Quercetin Placebo Placebo Placebo Noted : MMSE, Mini Mental State Examination ; CADi2, Cognitive Assessment for Dementia, iPad version 2 ; NI, No Information
Figure 3.ForestplotofMiniMentalStateExaminationbetweenExperimentalandControl
Figure 2. PRISMA2020FlowDiagram
[9][10][11]
Table 1. RiskofbiastableassessedwithRoB2.0tool
https://me-qr.com/l/SuplementaryQuercetin
Table 2. SummaryofIncludeStudyResult
THE EFFECT OF LECANEMAB FOR IMPROVING COGNITIVE IMPAIRMENT
IN ELDERLY WITH EARLY ALZHEIMER’S DISEASE USING BAYESIAN DESIGN ANALYSIS: A SYSTEMATIC REVIEW OF RANDOMIZED CONTROLLED TRIALS
Takbir Sabda Akhiru Ramadhan1, Namira Kirana Djatmiko2, Lise Putri Sesotyaningati3, Kirafara Ghaitsa4
[Correspondence E-mail: takta412@gmail.com]
Abstract
Introduction: Alzheimer's disease is a neurodegenerative disease with insidious onset and progressive impairment of behavioural and cognitive functions, including memory, comprehension, language, attention, reasoning, and judgment (1). The early symptom of Alzheimer’s disease affects memory, thinking, and reasoning skill. Lecanemab, a humanized IgG1 monoclonal antibody that targets soluble aggregated Aβ species (protofibrils) which help remove beta-amyloid, one of the hallmarks of Alzheimer's disease, and resulted in moderately less decline in measures of cognition and function than placebo (5). Based on the issues, we created this study with the express goal of providing evidence-based literature for therapeutic reference.
Objective: This systematic review aims to asses a new approach to slowing cognitive decline by ameliorating cognitive impairment with lecanemab in the elderly with early Alzheimer’s disease using the Bayesian design.
Methods: This systematic review followed guidelines provided by PRISMA. A literature search was conducted with multiple electronic databases, such as PubMed, Google Scholar, ScienceDirect, and Cochrane Library. The risk of biases was assessed for each study using the Cochrane Risk of Bias tool 2.0 for a randomized trial.
Result and Discussion: These findings of a dose-ranging efficacy study using a novel Bayesian adaptive design were initiated to assess the effects of lecanemab in subjects with early Alzheimer’s disease. Lecanemab at 10 mg/kg biweekly showed significant results on progression rates in the ADCOMS and CDR-SB assessments at 18-month follow-up (8). The 10 mg/kg biweekly and monthly doses were identified as potential effective doses of lecanemab, with 10 mg/kg biweekly dose determined to be the final ED90 dose (6).
Conclusion: Lecanemab was adequate for slowing clinical decline and improving cognitive impairment in the elderly with early Alzheimer’s disease.
Keyword: lecanemab, mild cognitive impairment, alzheimer’s disease, systematic review
ELDERLY WITH EARLY ALZHEIMER'S DISEASE USING BAYESIAN DESIGN ANALYSIS: A SYSTEMATIC REVIEW OF RANDOMIZED CONTROLLED TRIALS
 Takbir Sabda Akhiru Ramadhan, Namira Kirana Djatmiko, Lise Putri Sesotyaningati, Kirafara Ghaitsa
Takbir Sabda Akhiru Ramadhan, Namira Kirana Djatmiko, Lise Putri Sesotyaningati, Kirafara Ghaitsa
INTRODUCTION
Alzheimer's disease is a neurodegenerative disease with insidious onset and progressive impairment of behavioural and cognitive functions, including memory, comprehension, language, attention, reasoning, and judgment (1). The early symptom of Alzheimer’s disease affects memory, thinking, and reasoning skill. However, some risk factors of Alzheimer’s disease cannot be changed, such as age, genetics, and family history. More than 55 million people have dementia that can lead to Alzheimer’s disease, over 60% of whom live in low-and middle-income countries (2). In the early stages, it is characterized by mild memory loss, but in the late stages, people with Alzheimer's will lose the ability to communicate with their environment. Lecanemab, a humanized IgG1 monoclonal antibody that targets soluble aggregated Aβ species (protofibrils) which help remove beta-amyloid, one of the hallmarks of Alzheimer's disease, and resulted in moderately less decline in measures of cognition and function than placebo (5).
METHOD
("lecanemab" OR "lecanemab-irmb" OR "BAN2401") AND ("mild cognitive impairment" OR "Cognitive Dysfunction" OR "Cognitive Decline") AND ("alzheimer's disease" OR "Early Onset Alzheimer's Disease" OR "Alzheimer's Dementia")
Inclusion Criteria
Randomizedcontroltrialthatenrolled elderlywithearlyAlzehimer’sdisease

Mentionlecanemabastreatment
Mention beta-amyloid reduction for outcome


UsingBayesiandesign
WritteninEnglish

Irrelevantstudyoroutcomes
WrongPICOscomponent Reportandanothereditorialarticles



CONCLUSION & RECOMENDATION
The findings in this double-blind trial on multiple cognitive endpoints and biomarkers are supportive of the therapeutic concept for targeting specific oligomeric species (protofibrils) in the process of pathophysiologicalamyloidgenerationinAD.
Futurestudiesshouldbeconductedwithlargesample sizes and over an extended period to assess lecanemab'sefficacyintreatingAlzheimer'sdisease.

This systematic review aims to asses a new approach to slowing cognitive decline by ameliorating cognitive impairment with lecanemab in the elderly with early Alzheimer’s disease using theBayesiandesign.
RESULT
DISCUSSION
Lecanemab as a potential treatment for early Azheimer’s disease.
Lecanemab, also called BAN2401, is a humanized monoclonal antibody targeting amyloid protofibrils (a soluble aggregated form of Aβ) for treating AD, which was explored in the BAN2401-G000-201 trial (12). Lecanemab was generally well-tolerated, with the key adverse event being ARIA-E, with an incidence rate of less than 10% at the two highest doses for the overall population. The 10 mg/kg biweekly and monthly doses were identified as potential effective dose 90% (ED90) doses early in the study, with 10 mg/kg biweekly dose determined to be the final ED90 dose (defined as the most superficial treatment group that achieves at least 90% of the modelled maximum treatment effect) (6). Based on table 1, slowing clinical decline showed significant results in the ADCOMS and ADAS-Cog14 assessments (7), as well as the CDR-SB (6) at a dose of 10BW. This dose also showed significant results on progression rates in the ADCOMS and CDR-SB assessments at 18-month follow-up (8).
The use of Bayesian adaptive design
Using decision-theoretic approaches, a Bayesian adaptive design is proposed for a comparative two-armed clinical trial (11). These findings of a dose-ranging efficacy study using a novel Bayesian adaptive design were initiated to assess the effects of lecanemab in subjects with early Alzheimer’s disease (6). A properly conducted Bayesian adaptive study that achieves robust positive results on the primary endpoint could be discussed with regulators for possible use in supporting drug registration. Bayesian statistics can enhance the efficiency of analyzing the study data. Adaptive randomization generates more data on doses that appear to be more efficacious, which can improve dose selection for phase 3 (10). According to Bayesian and frequentist approaches, lecanemab treatment resulted in a dose-dependent and consistent reduction in clinical decline relative to placebo across several clinical endpoints (6). Bayesian design can ensure the effectiveness of the design to achieve study objectives, such as minimizing the risk of inadequate phase 2 trials and costly phase 3 failures (11). Thus, Bayesian design could help in improving the efficacy of lecanemab for patients with early Alzheimer's disease.
Study strengths and limitations
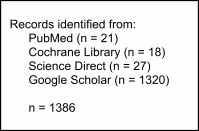
This study analyzes lecanemab for slowing cognitive decline in the elderly with early Alzheimer’s disease. Our systematic review indicated that lecanemab resulted in a significant reduction in amyloid plaques and a slowing of clinical decline. This analysis was also strengthened by the consistently positive conclusions across multiple statistical models, efficacy endpoints, and over time, despite missing data. The gap period between the interventions in one of our journals may be the limitation. However, the gap period presented the opportunity for the data. There aren’t many journals either because it’s a novel treatment.
 Figure 1: PRISMA 2020 flow diagram
Figure 2: Risk of Bias Asessment for RCT
Figure 1: PRISMA 2020 flow diagram
Figure 2: Risk of Bias Asessment for RCT
Exclusion Criteria
OBJECTIVE Study, year Swanson et all, 2021(6) Dhadda et all, 2022(7) McDade et all, 2022(8) Country USA USA USA Study design RCT RCT RCT Sample size (10 mg/kg BW, 10 mg/kg M, Placebo) (152, 246, 238) (161/253/247) (152/246/238) Dose regimens versus placebo (p-value) 10BW 10M 10BW 10M 10 BW 10 M less decline (18 month) ADCOMS 0.140 0.615 0.034* 0.228 NR CDR-SB 0.044* 0.275 0.125 0.255 ADAS-Cog14 0.227 0.525 0.017* 0.736 progression rates (18 month) ADCOMS NR NR 0.073 0.079 CDR-SB 0.022* 0.103 ADAS-Cog14 1.373 0.495 Note: ADCOMS: Alzheimer's Disease Composite Score; CDR-SB: Clinical Dementia Rating-Sum-of-Boxes; ADASCog14: Alzheimer’s Disease Assessment Scale-Cognitive Subscale; NR: not reported; *: statistically significant
REFERENCES Kumar A, Sidhu J, Goyal A, Tsao JW. Alzheimer Disease (2022). “Dementia.” World Health Organization. (2023) Schmidt R, Kienbacher E, Benke T, Dal-Bianco P, Delazer M, Ladurner G, Jellinger K, Marksteiner J, Ransmayr G, Schmidt H, Stögmann E, Friedrich J, Wehringer C. Geschlechtsspezifische Unterschiede der Alzheimer Demenz [Sex differences in Alzheimer's disease]. Neuropsychiatr. 22(1):1-15. German. (2008) McDade E, Cummings JL, Dhadda S, Swanson CJ, Reyderman L, Kanekiyo M, Koyama A, Irizarry M, Kramer LD, Bateman RJ. Lecanemab in patients with early Alzheimer's disease: detailed results on biomarker, cognitive, and clinical effects from the randomized and open-label extension of the phase proof-of-concept study. Alzheimer's Res Ther. 14(1):191. (2022) Van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, Kanekiyo M, Li D, Reyderman L, Cohen S, Froelich L, Katayama S, Sabbagh M, Vellas B, Watson D, Dhadda S, Irizarry M, Kramer LD, Iwatsubo T. Lecanemab in Early Alzheimer's Disease. N Engl J Med. 388(1):9-21. (2023) Swanson, C.J., Zhang, Y., Dhadda, S. et al. A randomized, double-blind, phase 2b proof-of-concept clinical trial in early Alzheimer’s disease with lecanemab, an anti-Aβ protofibril antibody. Alz Res Therapy 13, 80 (2021). Dhadda, S., Kanekiyo, M., Li, D. et al. Consistency of efficacy results across various clinical measures and statistical methods in the lecanemab phase trial of early Alzheimer’s disease. Alz Res Therapy 14, 182 (2022). McDade, E., Cummings, J.L., Dhadda, S. et al. Lecanemab in patients with early Alzheimer’s disease: detailed results on biomarker, cognitive, and clinical effects from the randomized and open-label extension of the phase 2 proof-of-concept study. Alz Res Therapy 14, 191 (2022). Logovinsky, V., Satlin, A., Lai, R. et al. Safety and tolerability of BAN2401 clinical study protofibril selective Aβ antibody. Alz Res Therapy 8, 14 (2016). Satlin, A., Wang, J., Logovinsky, V., Berry, S., Swanson, C., Dhadda, S., & Berry, D. A. Design of a Bayesian adaptive phase proof-of-concept trial for BAN2401, putative disease-modifying monoclonal antibody for the treatment of Alzheimer’s disease. Alzheimer’s and Dementia: Translational Research and Clinical Interventions, 2(1), 1–12 (2016). Cheng, Y., & Shen, Y. Bayesian adaptive designs for clinical trials. Biometrika, 92(3), 633–646. (2005). Tahami Monfared AA, Tafazzoli A, Ye W, Chavan A, Zhang Q. Long-Term Health Outcomes of Early Alzheimer's Disease Using Simulation Modeling. Neurol Ther;11(2):863-880. (2022). 1. 2. 3. 5. 7. 8. 10.
THE EFFECT OF LECANEMAB FOR IMPROVING COGNITIVE IMPAIRMENT IN









FamilyCaregiving101:ReachForElderCareExcellence
IMadeTobiasAbdiman¹,MadeRadityaArhyaPutra¹,RukmangganaSatyaPratiwi¹,Ni WayanCitraAyuSaraswati¹
¹FacultyofMedicine,UniversityofMataram,NusaTenggaraBarat,Indonesia
Email:tobias.abdiman@hotmail.com
Background: Aboutathirdofthe70-79yearsoldandoverhalfoftheolderadultsover80 yearswerelivingbythemselves,whichmeansalotofpeoplehavenotunderstoodthe importanceoffamilycaregivingonelders.Withtheircognitiveandphysicaldecline,the presenceofafamilycaregivertohelpandassistthemismuchneeded.Visitingadoctorand goingthrougheveryhealthcareprocessiscomplicatedanditisoneofthethingswhereelders needassistance.Withobservedlowermedicationcomplianceandlowercognitiveabilityto rememberandunderstandinformationgivenbyphysicians,familycaregivingintervention becomesimportantinordertoimprovehealthcareoutcomeongeriatricpatients.
Objectives :ThisposterthroughthemnemonicREACH(RegularVisit,Engage,Assistance, Compliance,andHelp),providesinformationonthebackgroundandreasoningbehindfamily caregivingongeriatrichealthcareprocesses,presentthenegativeimpactsofelderneglect, andtoprovideamemorableandeasytounderstandexplanationonwhatafamilymember candototakecareoftheirelders.Thisposteraimstoincreaseawarenessontheimportance offamilycaregiving,especiallyinaccompanyingeldersduringtheirhealthcareprocesses, andtoavoidelderneglect.
Keywords: olderadults,neglect,family,caregiving
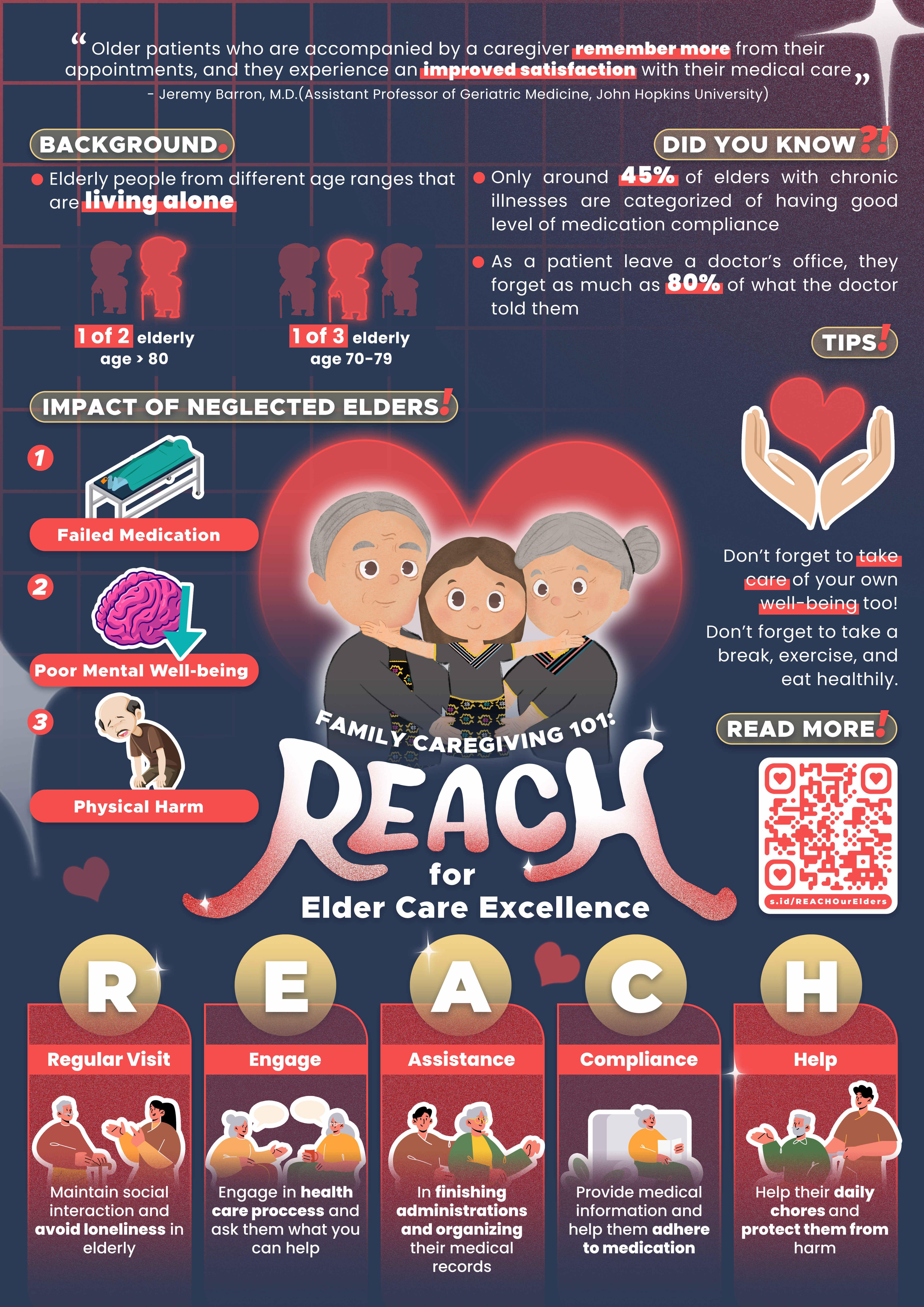
MEMORY: Making the Most Out of Alzheimer’s Symptoms
Elizabeth Charissa Atmawidjaja, Fadya Safitri, Aditya Putri Setyanegari
ABSTRACT
Because the aging population is on the rise, Alzheimer’s disease (AD)—an irreversible, progressive form of dementia that slowly destroys memory and thinking skills as people age contributes to 60–70% of dementia cases.
AD is a progressive neurodegenerative disease caused by neuronal cell death which typically starts in the entorhinal cortex in the hippocampus. Genetics, trisomy 21, increasing age, traumatic head injury, depression, smoking, cardiovascular and cerebrovascular disease increase the risk of AD. Higher education, use of estrogen by women, use of anti-inflammatory agents, leisure activities (reading or playing instruments), healthy diet and exercise decrease the risk of AD.
Early to mild symptoms of AD include disorganization, impairment of motor functions, language and multitasking problems, short-term memory loss, motivation and attention deficiency, anger, and anxiety.
Late diagnosis of AD happens due to diagnostic uncertainties, since the signs and symptoms of AD are sometimes not recognized or mistaken for signs of old age or other conditions.
Early diagnosis and intervention are beneficial for patients and carers and can result in substantial healthcare cost savings.
In hopes of increasing awareness and prognosis of individuals who exhibit symptoms of AD, this poster is aimed to promote common symptoms of AD with “DILEMMA”.
Keywords: Alzheimer’s Disease, Dementia, Symptoms, Diagnosis, Prevention

ABSTRACT
AhmadBintangMargaSakti,StellaAgathaWidjaja,RainaYoshioka UniversitasAirlangga
TITLE: ASSISTYourWaytoaBetterBladder:OvercomingOlderAdults’Urinary Incontinence
BACKGROUND: Urinaryincontinence(UI)istheinvoluntaryleakageofurinethatisa commoncomplaintinolderadults.UIistwiceascommoninolderwomenthanoldermen. Asiareportedhavingthehighestprevalenceofurineincontinenceinolderwomen,at45.1%. Urinaryincontinencehasasignificantimpactonolderpeople'squalityoflife,causingmany tolimittheirsocialandphysicalactivities.Itcanalsointerrupttheirdailyactivitiesand potentiallyleadtofalls.Despiteitsprevalence,manycasesofUIgounreportedand undertreatedduetothestigmasurroundingit.BylearningaboutUI,olderpeopleandtheir caregiverscanobtainappropriatetreatment.Thisiscrucialtoreducetheadversehealth outcomesofUI.
OBJECTIVES:
1.Increaseawarenessregardingthedefinition,causes,epidemiology,types& symptoms,andpreventionsofurinaryincontinencetoolderadults,theircaregivers, andthepublic.
2.Urgethoseaffectedtoseekmedicalassistanceandreducethestigmaattachedtothis condition.
3.Improvethequalityoflifeforolderadultswhohaveurinaryincontinence.
KEYWORDS: urinaryincontinence,olderadults,prevention,epidemiology,causesofUI

KeepyourMindSharpwithBRAIN!
2FacultyofMedicine,UniversitasSamRatulangi
3FacultyofMedicine,UniversitasTarumanagara
Abstract
Atpresent,thedynamicsofworldpopulationgrowthisveryhigh.Aspopulationsaregrowing andtheprevalenceofmajorcognitivedeclineincreaseswithage,cognitivedecline becamethe leadingcauseofdisabilityandtheseventhleadingcauseofdeathworldwide.AccordingtoWHO, currentlymorethan55millionpeoplehavedementiaworldwide.Everyyear,there arenearly10 millionnewcases,andthenumberofpeoplewithdementiaisexpectedtotriple by2050.Hence, preventivemeasureswithkeepwithBRAINaretheneededreducetheriskofcognitivedecline andmaintainmentalacuityinolderadults. Bementallyactive. Reducestress. Avoidharmful substances. Improvesleephabits. Nurturesocialconnections.Byfollowingthe“BRAIN",the goalistomoreawarenessaboutcognitiveimpairmentscanimpactdamagebrainifitisn’ttreated andtokeepspreadloveandcare,whichlimitstheavailabilityofpsychogeriatricsupport.We trulybelievethatkeepingyourmindsharpwithBRAINisimportantformaintaining independenceandqualityoflifeinyourgoldenyears.
Keywords: CognitiveDecline,Dementia,BRAIN
NadhiraTsurayyaRamadhani1,DerrenDavidChristianHomentaRampengan2,NatashaCita ParadhitaKusuma3,DaniaPutriIslamiah1 1FacultyofMedicine,UniversitasSriwijaya

Astrokeisanattackonthebrain’sbloodsupplythatcancausebraindamage.Incidentally,elderlystroke patientsaremorepronetodeath,poorqualityoflife,andlengthyhospitalstaysthanotheragegroups,with 66%ofalldeathsfromstrokeoccurringinpeopleover70.Furthermore,1in4elderlyareatriskof experiencingastrokeatleastonceintheirlifetime.Unfortunately,manycannotrecognizethesignsofstroke duetopoorstrokeliteracy.Thiscreatespre-hospitaldelaysinstrokemanagement,thussignificantly decreasingthepatient’slifeexpectancy.Therefore,wesuggesttheacronym“FAST”whichincludes: Facial drooping, Armscannotberaised, Speechisslurred,and Timetocallforhelp,whichaidsthecommunityin recognizing thesignsandinitiatingstrokemanagement.Evidently,thisdiseasecanbeprevented,increasing thepatient'slifeexpectancy.Hence,“AHEAD,”isproposed,whichmeans: Anticipatestroke-related conditions, Healthyliving, Eatwell, Avoidalcoholandsmoking,and Drinkyourmedicinethatcan minimizetheriskofstroke.Throughthisposter,wehopetoraiseawarenessamongtheelderlyandtheir caregiversworldwidetoidentifystrokesymptoms.Therefore,caregiverscancallforprofessionalhelpto maintaintheirqualityoflife.
Keywords: elderly, stroke,recognize,manage,prevention
Authors:NabielMuhammadHaykal,JaudaHanoon,ThalitaNadiraIzzaSenen,MuhammadBeyAli
ThinkFAST!BeAHEADofElderlySTROKE

DISCOVERTHESIGNAL,AVOIDDEMENTA
Elderlyaremoresusceptibletovariousdiseasesduetodecreasingbodyfunction,oneofthem isdementia,asyndromethatleadstochronicorprogressivecognitivedecline.Globally,55 millionpeoplesufferfromdementia,whereasInIndonesia,1.2millionpeoplehavedementia, andmanyarestillunderdiagnosed.Dementiainterfereswithaperson'sabilitytofunction, affectingphysical,psychological,social,andeconomicaspects.Theincreasingnumberof dementiacasesrevealsanemergingurgencytotreatandpreventdementia.
Therefore,itisimportanttoincreasepublicawarenesstowardsdementiathrougha communicativeandeasytoreadpublicpostertitled"DiscovertheSIGNAL,AVOID Dementia''.Dementia’ssignsandsymptomsaresimplifiedbythewordSIGNALwhich standsforstrugglingtoconcentrate,incapabletofollowaconversation,gettingdisorientedto timeandplace,noticeithardtocarryoutadailytask,alterationofmood,andlosingmemory.
Sincethereisnodefinitivetreatmentavailablefordementia,itissuggestedtooptimizethe prevention.ThemnemonicAVOIDisusedtosimplifythepreventionwhichisadvancinga healthydiet,verifyingbloodpressureatahealthylevel,offsmoking,implementexercise regularly,anddrinkinglessalcohol.
Keywords : Dementia,Cognitivedecline,DementiaPrevention
SIGNAL, DISCOVER THE AVOID AVOID DEMENTIA
WHAT IS DEMENTIA?
Dementia is known as a syndrome of impaired cognitive function that affect memory, thinking, or ability to make decisions that interferes with doing everyday activities
RISK FACTORS

Age Genetics
Unhealthy Lifestyle
Depression
Head Trauma
TO
YOU HAVE V V Verify your blood pressure at a healthy level
Advancing healthy diet
million people worlwide 55 1.2 million people in Indonesia experience dementia

IDENTIFY SIGNS & SYMPTOMS!
S Struggling to conentrate
I Incapable to follow a conversation
G Getting disoriented to time & place
N Notice it hard to carry out daily task
O O
Off Smoking

II Implement exercise regularly
DID YOU KNOW? A A
D D Drink less alcohol
SIGNAL,
Losing
A Alteration of mood L
memories
QONITA PUTRI ANAS | PEARLE GABRIALE NELWAN NAJLA AULIA SHAFA' NURFAUZI | AURORA ADILA ARDERIA
REFERENCE
Telemedicineisatechnologythathasrecentlybecomepopular,andmanypeopleuse telemedicineextensively.Devicessuchassmartphonesandsmartwatchescanuse telemedicine.Smartwatchisapracticalandpassivedevicewitheffectiveandefficient features,especiallyforthehealthofolderadults.Nevertheless,accordingtostudiesand surveysconductedinIndonesia,usingsmartwatchesamongolderadultsremainsrelatively modest.Mostsurveyrespondentsstatedthattheystillfeelunfamiliarwiththistechnology.
Diabetesmellitus,hypertension,coronaryheartdisease,stroke,rheumatoidarthritis,and mentalandemotionaldisordersareprevalentamongolderadultsinIndonesia.Smartwatches candetectvariousmedicalfactors.Thesmartwatchhasabiosensorthatcanmonitorvital signssuchasoximetry,bloodpressure,andheartrate.Thesmartwatchcanalsodetectcardiac eventssuchasarrhythmia.Notonlythat,butthesmartwatchcanalsomonitorthesemedical factorsdiscretelyandcanevendetectfalls.However,notallwearablefeaturesaidin preventingelderlymorbidity.
Aftergettingtheresultsfromthesmartwatchmeasurement,thenextstepistoconsultan offlinehealthserviceorusethetelemedicineapplicationavailableonthedigitalplatform. However,rememberthatsmartwatchresultsarenotalways100percentaccurate,sothey shouldusethemcautiously.
DetectingMorbiditythroughWearableTechnology
Source:
1NinaA.,EmilR.,GunawanW.,RiyantoJ.,(2019).UsabilityStudyandUsers’Perceptionof Smartwatch:StudyonIndonesianCustomer,ProcediaComputerScience,161(1266-1274).
2Anorital,A.(2015).MorbiditasdanMultiMorbiditasPadaKelompokLanjutUsiadi Indonesia.IndonesianJournalofBiotechnologyMedicine,4(2),77-88.
3Lu,T.C.,Fu,C.M.,Ma,M.H.,Fang,C.C.,&Turner,A.M.(2016).Healthcare ApplicationsofSmartWatches.ASystematicReview.Appliedclinicalinformatics,7(3), 850–869.
4Liu,etal.,(2022).WearableSmartwatchFacilitatedRemoteHealthManagementfor PatientsUndergoingTranscatheterAorticValveReplacement.JournaloftheAmericanHeart Association,11(7),e023219.
5Brew,B.,Faux,S.G.,&Blanchard,E.(2022).EffectivenessofaSmartwatchAppin DetectingInducedFalls:ObservationalStudy.JMIRformativeresearch,6(3),e30121.
6Bin,K.J.,DePretto,L.R.,Sanchez,F.B.,&Battistella,L.R.(2022).DigitalPlatformto ContinuouslyMonitorPatientsUsingaSmartwatch:PreliminaryReport.JMIRformative research,6(9),e404

ABSTRACT
StellaAgathaWidjaja,AhmadBintangMargaSakti,RainaYoshioka UniversitasAirlangga
TITLE: Let’sPreventObstructiveSleepApneawithHELP
BACKGROUND: ObstructiveSleepApnea(OSA)isacommonsleepdisorderthataffects olderadultsandischaracterizedbythecollapseorpartialblockageoftheupperairway duringsleep,leadingtodecreasedoxygenlevelsinthebody.Studiesshowthatbetween 13–32%ofindividualsover65experiencesomeformofsleepapnea.OSAcansignificantly impactthequalityoflifeofolderadults,asitcanleadtoheartandmentalhealthdisorders. OSAisoftencalledasilentkillerdisease,asupto90%ofcasesremainundiagnosed.Thisis associatedwithincreasedmorbidityandmortality.Therefore,educatingolderadults, caregivers,andthepublicaboutOSAiscrucialtoreducethiscondition'snegativeimpacton olderadults'health.
OBJECTIVES:
1.Increaseawarenessregardingthedefinition,epidemiology,riskfactors,and preventionsofobstructivesleepapneatoolderadults,theircaregivers,andthepublic.
2.Urgethosewhohavetheriskfactorsandsymptomstoseekmedicalassistanceforthis condition.
3.Improvethequalityoflifeforolderadultswhohaveobstructivesleepapnea.
KEYWORDS: obstructivesleepapnea,olderadults,prevention,epidemiology,riskfactors

EMBRACE The Elderly to Prevent Depression
Calysta Yesika Perbina Saragih, Fathin Fatimah Dian Putri Gafur, Carissa Nindya Paskila, Benhur William Sitakar
Introduction: Depression is a common and serious medical illness that negatively affects how you feel, the way you think and how you act. Depression is not a normal part of aging, but elders are at increased risk for depression. The prevalence of depression in the elderly population in the world is very high, 31.74%, Where the prevalence was higher among developing countries. Although most cases of depression cannot be prevented, healthy lifestyle changes can have long-term benefits to their mental health.
Objective: To increase caregivers and public knowledge and awareness of depression in elderly, its symptoms, complications, and its prevention.
Keyword: Depression, Geriatric, Prevention
E
B M R A
Depression is...
A common and serious medical illness that negatively affects how you feel, the way you think and how you act. Depression is not a normal part of aging, but elders are at increased risk for depression.
Complication
Worsening of emotional well-being

Disability
Increased Morbidity

Suicidal thought and behavior
E






31,74% In the World, Elderly has depression
Sign & Symptomps





Loss of interest in pleasurable activities

Moving or talking more slowly
Feeling of hopelesness
"Empty" Mood

Sleeping disorder
Decreased energy or fatigue
E E M M B B R R A A C C E E
Encourage and provide healthy and enjoyable diet
Make the elderly feel loved. Have a great time with them!
Be there for them
Remind the elderly to be physically active


Accompany and support them in activities that they enjoy
Benhur SitakarCalysta SaragihCarissa PaskilaFathin Gafur
Create a joyful and safe environment
Enough sleep for 7-9 hours


DEPRESSION DEPRESSION Scan For Reference!
Lacristie Gabriella Manulang, Nathasya Inka Syakti Nasution, Jihan Salsabila
AMSA-Universitas Sriwijaya
Background: Blindness or vision problems are among the top ten disabilities among people aged 18 and older, according to the Centers for Disease Control and Prevention. Loss of vision causes loss of freedom, social deprivation, and increased morbidity, which is frequently linked with medication errors or poor nutrition. In keeping with studies, 36 million individuals worldwide are blind, with cataract contributing to more than 12 million of them. The Pooled Prevalence Estimate (PPE) of any cataract ranged between 54% in the over-60 age group. However, just because cataracts are common among the elderly doesn't mean they have to live with poor vision and declines in quality of life.
Objectives: The aim is to raise public awareness on important cataract-related issues in the hope that it will serve as a preventative or medical treatment guide, especially for their loved aging ones.
Keywords: elderly, vision, cataract, blind
References
Cataracts (2023) National Eye Institute. National Institutes of Health. Available at: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/cataracts (Accessed: April 15, 2023).
Chen, P., et al (2020) “Cataract and the increased risk of depression in general population: a 16-year nationwide population-based longitudinal study,” Scientific Reports, 10, p. 13421. Available at: https://doi.org/10.1038/s41598-020-70285-7.
Hashemi, H., et al. (2020) “Global and regional prevalence of age-related cataract: a comprehensive systematic review and meta-analysis,” Eye, pp. 1357–1370. Available at: https://doi.org/https://doi.org/10.1038/s41433-020-0806-3.
Seltman, W. (2021) How Can I Prevent Cataracts?, WebMD. Available at: https://www.webmd.com/eye-health/cataracts/how-can-i-prevent-cataracts (Accessed: March 15, 2023).
LET’S SEE
ABOUT CATARACT!

DEMENTIATHATWESHOULDKNOW
DaudHamonanganTambunan,DevinaMaharaniMangiri,FlorentSitumorang AMSA-UNDIP
ABSTRACT
Dementiacanbedefinedassymptomsfromsomediseasethataffectthebrain.Problemswith memory,thinking,orlanguage,aswellaschangesinmood,emotions,perception,and behavior,areallreferredtoas"dementia"symptoms.Dementiaisnotaninevitable consequenceofaging.Dementiacanaffectyoungerpeopletoo.Itoccurswhendiseasecauses damagetothebrain.Themostwell-knownkindsofdementiaareAlzheimer'sinfectionand vasculardementia.Itiscausedwhenadiseasedamagesnervecellsinthebrain.Nervecells carrymessagesbetweendifferentpartsofthebrain,andtootherpartsofthebody.Asmore nervecellsaredamaged,thebrainbecomeslessabletoworkproperly.Onemorefact, dementiaismorecommonamongwomenthanmen.Eventhoughdementiaisacommon disease,especiallyamongtheelderly,thereisstillalackofcarefordementia,especiallyin families.Eventhoughthefamilyhasaveryimportantroleintreatmentofdementiaathome. Sothisposterisexpectedtobeatoolforspreadinginformationaboutdementia.
Keywords:dementia,brain,nervecells,commondisease
Reference:
1.Widyastuti,RitaHadi.2011.“FamilyExperienceCaringforDementia”.IndonesianNers Journal.Vol.1(2)
2.Nisa,KanditaMahranandRikaLisiswanti.2016.“RiskFactorofAlzheimer’s Dementia”.MajorityJournal.Vol.5(4)
3.HelpsheetAboutDementia(dementia.org.id)
4.Factsheet400LP:"WhatisDementia?"byAlzheimer'sSociety(August2021)

HUMBLE Guide to Prevent Alzheimer
Narendra Lintang Mahadewa1, Armadina Fitra Choirunnisa1, Fadhila Najwa Almadani1
AMSA-UNDIP1
ABSTRACT
Alzheimer is a neurodegenerative disorder that causes memory loss and neuronal cell death in the brain. Alzheimer’s disease is one of the top 10 major causes of Death according to WHO. The burden of Alzheimer's will continue to rise rapidly by the year of 2050, since the ageing population continues to increase. Alzheimer disease is believed to be a degenerative disease that plagues our elderly because one of the major risk factors is people over 65 years old. The major challenge in tackling Alzheimer's is the social stigma that causes Alzheimer's disease patients to isolate themselves from others since patients have the tendency to confirm the stereotype. The method used in this poster is a literature study. This method was conducted to obtain information relevant to Alzheimer's and used as a theoretical basis for conducting poster content. The key to managing Alzheimer's is lifestyle modification, thus our project is to encourage societyaboutwhatdailyhabits thatcantriggerAlzheimer's.Thisprojectuses a word that is often used in everyday life, namely "HUMBLE" as a friendly approach to the audience. It stands for High Blood Pressure, Understanding symptoms, Maintain Healthy Weight, Limit Alcohol Consumption, and Encourage Social Interaction.
Keywords: Alzheimer, Death, Degenerative, Elderly, Lifestyle Modification
Reference:
1. Kumar A, Sidhu J, Goyal A, et al. Alzheimer Disease. (2022). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
2. National Institute on Aging (NIA). (2021). What Is Alzheimer’s Disease?. National Institute on Aging.
3. Stites S, & Karlawish J. (2018). Stigma of Alzheimer’s Disease Dementia - Practical Neurology. Practical Neurology. https://practicalneurology.com/articles/2018june/stigma-of-alzheimers-disease-dementia
4. Teipel S, Gustafson D, Ossenkoppele R, Hansson O, Babiloni C, Wagner M, RiedelHeller SG, Kilimann I, Tang Y. (2022). Alzheimer Disease: Standard of Diagnosis, Treatment, Care, and Prevention. Journal of Nuclear Medicine. 1;63(7):981-5.
5. World Health Organization. (2020). The Top 10 Causes of Death.
6. Center for Disease Control and Prevention. (2022). Reducing Risk of Alzheimer’s Disease.

SAVEELDERLYFROMHYPERTENSION
Abstract
Background
Theelderlyarethemostrapidlygrowingpopulationgroupintheworld.Datacollectedover a30-yearperiodhavedemonstratedtheincreasingprevalenceofhypertensionwithage.The riskofcoronaryarterydisease,stroke,congestiveheartdisease,chronickidneyinsufficiency anddementiaisalsoincreasedinthissubgroupofhypertensives.Hypertensionisan importantriskfactorforcardiovascularmorbidityandmortality,particularlyintheelderly.It isasignificantandoftenasymptomaticchronicdisease,whichrequiresoptimalcontroland persistentadherencetoprescribedmedicationtoreducetherisksofcardiovascular, cerebrovascularandrenaldisease
Objective
Tocontrolhypertensionandpreventtheoccurrenceofcardiovasculardiseasesdueto sustainedhighbloodpressure,therebyreducingmortality
Keywords: hypertension,cardiovascular,elderly

Let’s Prevent Diabetes Mellitus With ABCDE
Chesanica Luciani PH, Britney Rachel P, Kenaya Intan SS, Reynard Alexander N
ABSTRACT
Background : Diabetes Mellitus is a metabolic disorder characterized by chronic hyperglycemia, resulting from defects in insulin secretion, insulin action, or both. The disease has become a significant public health concern worldwide due to its high prevalence, morbidity, and mortality. According to the International Diabetes Federation (IDF), in 2021, the global prevalence of diabetes among adults aged 20-79 years was estimated to be 10.9%, which translates to approximately 537 million people worldwide.1
Objective :
Diabetes is one of the world's health problems. We focus on preventing diabetes mellitus through ABCDE in order to reduce the prevalence diabetes mellitus, especially in Indonesia.2
Keywords : Prevent, Diabetes Mellitus
References :
1. International Diabetes Federation. IDF Diabetes Atlas, 10th edn. Brussels, Belgium: International Diabetes Federation, 2021.
2. World Health Organization. Diabetes. 2022. Available from: https://www.who.int/newsroom/factsheets/detail/diabetes#:~:text=A%20healthy%20diet%2C%20regular%20physical,screeni ng%20and%20treatment%20for%20complications.

STROKE?BeAWAREandKEEPtheARTERYHEALTHY
VirnalisiLestariRomauliSilitonga,PutriMariaAngelica,PutuDezhifaRestuPutri,AureliaCallista
[CorrespondenceE-mail: virnasilitonga28@gmail.com ]
Introduction: Strokehascausedthesecond-highestdeathintheworldandbecoming dangerous,especiallyfortheelderly.Toreducetheriskofstroke,everyoneshouldbeaware ofthesignsandsymptomsofastroke.BeFASTstandsforBalanceloss,Eyesblurredvision, Facedroop,Armdriftdownward,Speechslurred,andTimeforearlytreatmentcanbea standardformanagingearlysymptomsofastroke,consideringtheimpactofstrokefor patientsissevere,bothphysicallyandmentally.
Somewayscanbetakentominimizetheriskbydetectingearlysymptomsand implementingdiseasepreventionforelderly.“HEALTHY”canbeasolutiontopreventstroke intheelderlybychoosingHealthfulnutrition,Exercisingregularly,Avoidingsmoking, limitingalcohol,TestforBEFASTsymptoms,Hypertensionmanagement,andlowerYour cholesterol.Nowadays,peopleunderestimatehowimportantthesesimplethingsareuntilwe feeltheconsequences.So,doitnoworregretitlater!
Objective: Toraiseawarenessregardingcurrentlifestylethatcantriggerdiseasesinthe elderlylife,especiallystrokewhichhasanextremelyhighmortalityrate.Furthermore,we hopethatpeoplecanrecognizeearlydetectiontominimizetheriskofdeath,andhencewill decreasetheprevalenceofstroke.
Keywords: stroke,elderly,prevention,earlydetection.
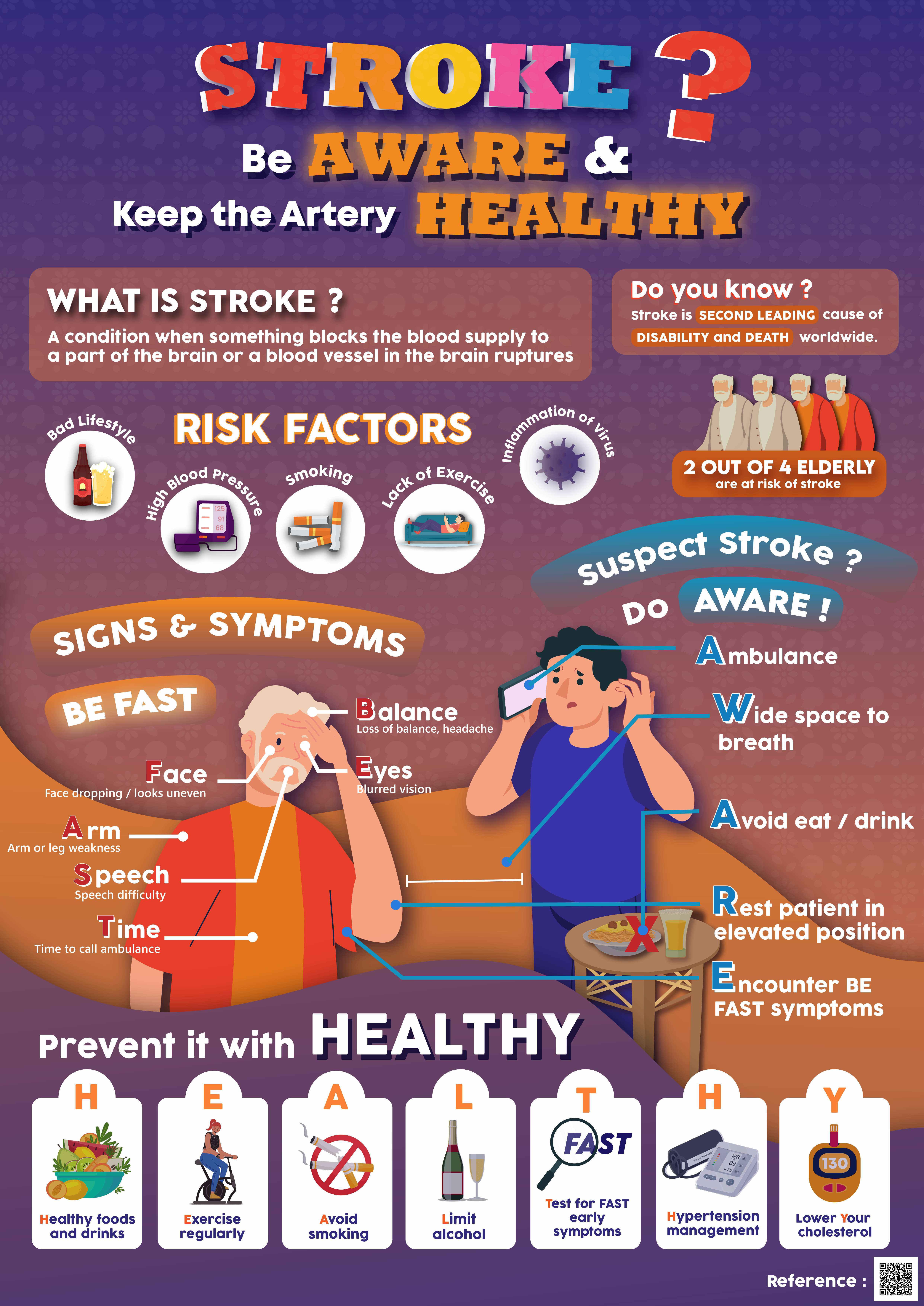
StayingOnThe“DASHTRACK”ToManageHypertension
AnugrahAlifio,AurellyaShabrina,TheresiaLeonita,ClaudiaSabrinaWilhelminaSidabutar UniversitasPembangunanNasionalVeteranJakarta
CorrespondenceE-mail: anugrah14september@gmail.com
Abstract
Hypertensionisaglobalburdenresponsibleforlong-termillness,disability,anddeathfor about7.3millionindevelopingcountries,primarilyaffectingpeopleinolderage.Datafrom WHOestimatedthat46%ofadultsworldwideareunawareiftheyhavehypertension,andolder adultslivinginpovertyareathighriskofhypertension.Despitethesefacts,hypertensionis treatableandpreventablebymanagingorcontrollingthelifestyle.Therefore,actionmustbe takentoreducetheincidenceofhypertensionamongolderpeoplethroughsimpleandcheap treatments.
Togetanoptimalhealthprofileforhypertensioninolderadults,peoplemustknowthe stepsoflong-termcaretosupportandmaintainaperson'shealth.Therefore,weintroducesimple long-termcare,namely"DASHTRACK,"whichstandsforDietaryApproachestoStop Hypertension,Takethemedicineasprescribed,Regularlyexercise,Avoidstressandsmoking, Controlyourweight,andKnowyourhealthstatusthroughroutinecheck-ups.
Afterreadingthisposter,wehopethatpublicawarenessandknowledgewillincreasein managinghypertension,especiallyinolderadultswiththemostsimpleandcheapformof management.
Keywords: Olderadults,Hypertension,Long-termcare,lifestylechanges.

AwareofDIABETESwithSUGAR:ACreativeCampaignforDiabetesAwareness
SeanDanielSteward¹,SonyaVerdyscaEllysia
², RidhaBethaZahra³
¹FirstYearMedicalStudent,AsianMedicalStudents’AssociationPadjadjaranUniversity ridhabz.rbz@gmail.com
²FirstYearMedicalStudent,AsianMedicalStudents’AssociationPadjadjaranUniversity asds1509@gmail.com
³FirstYearMedicalStudent,AsianMedicalStudents’AssociationPadjadjaranUniversity sonyaverdysca@gmail.com
Background: Diabetesisadiseasecommonlyfoundintheelderly,whichisassociatedwithhigh morbidityandmortalityrates.Itisametabolicdiseasethatresultsinabnormalbloodglucose levels.Theprevalenceofdiabetesmellitusamongindividualsover65yearsoldinTaiwanwas 26.5%from2015to2018accordingtoareportpublishedbytheTaiwanHealthPromotion Administration(THPA).Asiaishometo60%ofpeoplewithdiabetes,withChinaandIndia beingthebiggestcontributors.Shockingly,Indonesiarankssixthintheworldforthehighest numberofdeathsfromdiabeteswith236,000deathsin2021.Diabetessymptomscanbesubtle, makingitchallengingforindividualstorealizetheyhavethecondition.Lateandinadequate treatmentcanleadtoincreasedmorbidityandmortality.Tocombatthis,apublicpostertitled "AWAREOFDIABETESWITHSUGAR"wascreated.Thisposterhighlightsthesymptomsof diabetesandprovidespreventativemeasurestomakeindividualsmoreawareofthedisease.
Objective: Thegoalistoraisepublicawarenessofdiabetesbypresentingvariousassociated information,suchassymptomsandpracticalpreventativemeasurestolowerthechanceof developingdiabetes.
Keywords: diabetes,awareness,preventative
References
Ramachandran,A.,Snehalatha,C.,Shetty,A.S.,&Nanditha,A.(2012).Trendsinprevalenceof diabetesinAsiancountries.Worldjournalofdiabetes,3(6),110–117. https://doi.org/10.4239/wjd.v3.i6.110
Liang,C.C.,Hsu,W.C.,Tsai,Y.T.,Weng,S.J.,Liu,S.C.,&Lin,C.H.(2020).FactorsRelated toDiabetesMellitusintheMiddle-AgedandOverinTaiwan.Healthcare(Basel, Switzerland),8(3),242. https://doi.org/10.3390/healthcare8030242

BrittleBone:Osteoporosis
AzzahraPutriKhansha,AnnisaPutriAdrianto,NafisaAdithyaSekar,IndiartoNindyo Prasetyadi
Osteoporosisisanimbalanceinboneresorption,remodeling,resultinginadecreaseinbone mass,andcommonage-relateddiseaseclinicallymanifestedbyskeletalfractures,especially fracturesofthevertebrae,hip,anddistalforearm.Theprimarycauseofthesefracturesislow bonemass,althoughincreasedtraumafromfallsintheelderlyalsocontributes.Lowbone masshasmultiplecauses,eachcontributingdifferentlytothedevelopmentofosteopenia.The mostimportantgroupofcausesarefailuretoachieveadequatepeakbonemass,slowbone lossduetoaging-relatedprocesses,femalemenopause,andvarioussporadicbehavioral, nutritional,andenvironmentalfactorsthatcontributetoaffectingbonemassbutarenotinon otherpeople.
Inordertotheposter,weshoulddo“STAND”(Stayactiveforatleast30minutesofphysical activityeveryday;Treathormonalimbalances;Avoiddangerousactivities;Nutritional balance,consumefoodrichincalcium,protein,VitD,C,K,B,andmineraltomaintain strongandhealthybones;Don’tsmoke),becauseSTANDisgenerallyeffectivefor promotingbonehealthtomostpeople.
Afterreadingthisposter,wehopethatpeople,especiallytheelderly,havemoreawareness andknowledgeabouthowtodoearlypreventionofdiseasesthatwilldisrupttheirdailylives.
Keywords: calcium,decreaseinbonemass,elderly,physicalactivities

“FacingGeriatricIssueswithVIT5C”
Tema:COMMONHEALTHISSUESINGERIATRICCARE
ABSTRACT:
Geriatrics:AccordingtotheWorldHealthOrganization(WHO),theelderlyaresomeone whichhasenteredtheageof60yearsandabove.TheelderlyaretheagegroupInhumans whohaveenteredthefinalstageofthephasehislife.Groupscategorizedastheelderlywill experienceaprocesscalledagingprocessoragingprocess.PatientGeriatricsareelderly patientswithmulti-diseaseand/ordisruptionduetodecreasedfunctionoforgans, psychology,social,economicandtheenvironmentthatrequiresintegratedhealthservices.
Geriatricsyndromesareaseriesofclinicalconditionsinolderpeoplecanaffectpatient qualityoflifeandisassociatedwithdisability.AppearanceAtypicalclinicalfeaturesoften leadtoundiagnosedgeriatricsyndromes.
DatafromtheCentralStatisticsAgency(BPS)statesthatthenumberofelderlypeoplehas increasedfrom18millionpeople(7.6%)in2010to27millionpeople(10%)in2020.This figureisexpectedtocontinuetoincreaseto40millionpeople(13,8%)in2035.Theresults ofthisprojecthavethepotentialtobecomeaproblemforcountriesthatalsoexpecta demographicbonusin2030,whenthepopulationofproductiveage(15-64years) outnumbersthoseofnon-productiveage.

SYMPTOMP
● Riskoffallingwhenstandingorwalking
● Thebodywillfeelweak
● DifficultyinmovingSexualdisorder
● Dizzy
● Thebodyisdeficientinnutrition
● Impairedvisionandhearing
● Insomnia
● Difficultyinswallowingoreating
● Osteoporosis
SOLUTION
● ConsumptionofVit.D
● Calciumconsumption
● Consumptionofappropriatemedication
● Cautionandavoidcigarettesandalcohol
● Counselingbetweenfamiliesandtherapy

“ARTICULATE”WITHOUTOSTEOARTHRITIS
JasmineAurelliaKanittaSubrata,RaenenLiaw,Jeanes,NikolausAlbert
[CorrespondenceEmail:jasmine.kanitta@gmail.com]
BACKGROUND
Osteoarthritisimpactsaround3.3to3.6%oftheworldpopulation,withtheprevalenceof osteoarthritisinIndonesiansat12.7%inwomenand15.8%inmen.Therepercussionsof osteoarthritisshouldnotbeoverlooked,sinceupto43millionpeopleexperiencemoderateto severedisabilityduetothisdisease.Thismakesosteoarthritisthe11thmostdebilitatingdisorder globally.Osteoarthritisisthemostcommontypeofarthritisintheolderpopulation.Accordingto CDC,othercommonproblemsexperiencedbypatientsincludepain,stiffness,decreasedrangeof motionorflexibility,andswelling.
OBJECTIVE
Toeducatethepublicregardingthepreventionandriskfactorsthatcontributetothe developmentofosteoarthritis.
DESCRIPTION
Osteoarthritisisadegenerativejointdiseaseandamajorcauseofpainanddisabilityinadult individuals,whichmanifestsitselfwithjointpainandlossoffunctionsormobility.Thecartilage betweenboneswillbreakdown,causingthebonestochangetheirstructure.Riskfactorsforthis diseaseincludeoldage,overuse/injury,genetics,andheavyweight.Topreventthisdiseasefrom manifesting,thereisanumberofwaysonecanimplement,suchas Avoidjointoverwork, Routinecheckups, To Implementexercise, Consumefishtoincreaseomega-3s, Understand osteoarthritis, Loseweight, Alwaysmaintaingoodposture,and TErminatesmoking.
IMPACT
Wehopethispublicpostercanraiseawarenessandeaseconcernsoftheelderly,andthus decreasetheincidenceoftheseverityofthedisease.
CONCLUSION
Staylightonyourfeet,andkeepyourjointsfeelingsweet!Preventosteoarthritiswithsimple steps-move,groove,andwatchyourweight.Don'tletjointpaincrampyourstyle,takecareof yourselfwithasmile!
KEYWORDS
Geriatry,Osteoarthritis,Preventative.
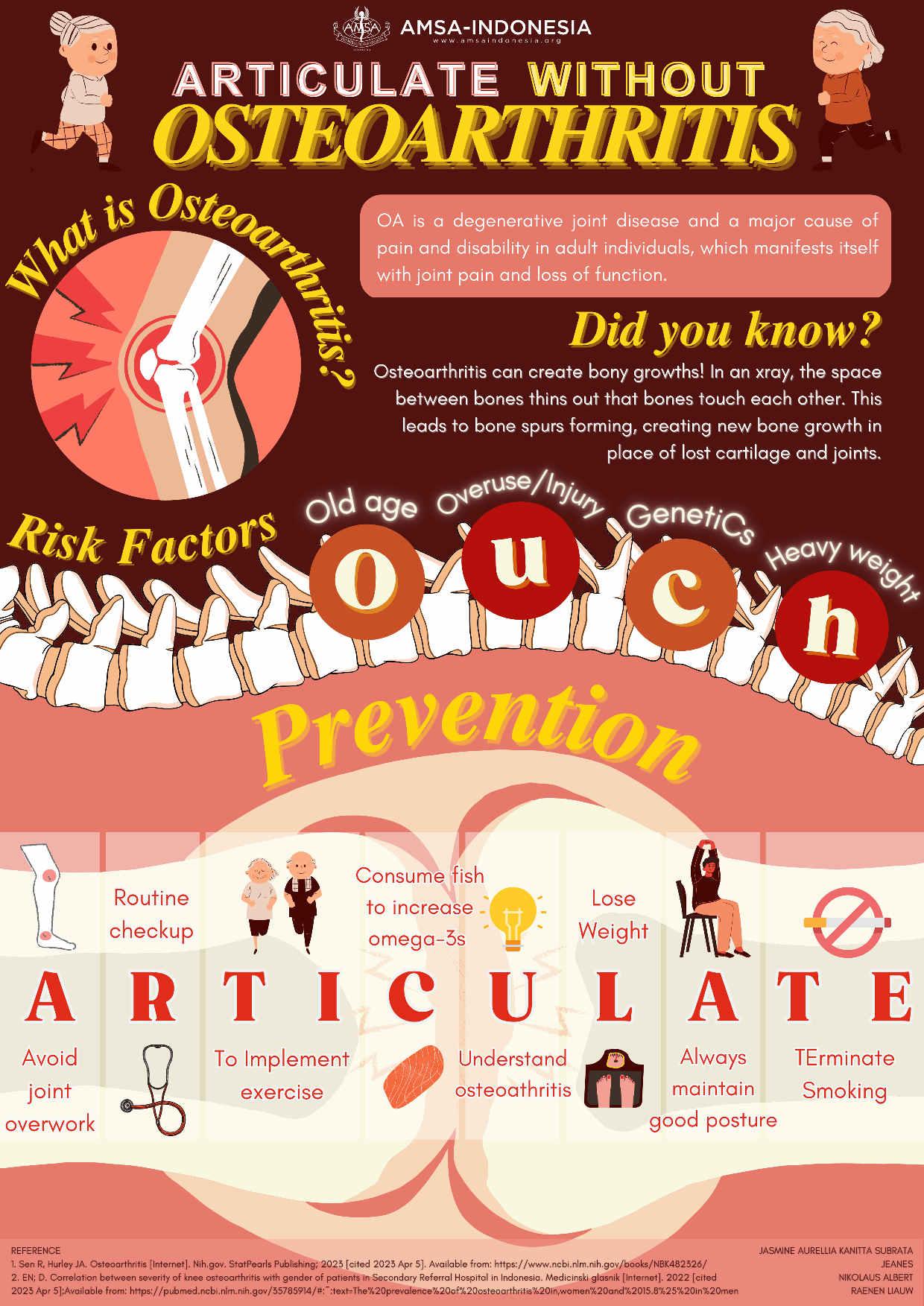
WITH“BEFAST”WEDETECTSTROKESEARLY Pre-conferenceCompetitionAsianMedicalStudents’conference
AUTHORS: LouisJulian,AngelyMariaSusanto,BryanSetyoputra

FacultyofMedicine UniversityofPelitaHarapan 2023
WITH“BEFAST”WEDETECTSTROKESEARLY
LouisJulian,AngelyMariaSusanto,BryanSetyoputra
[CorrespondenceE-mail: louisj527@gmail.com]
Background:Astroke,alsoknownasatransientischemicattackorcerebrovascular accident,happenswhenbloodflowtothebrainisblocked.Strokecancauselastingbrain damageandlong-termdisability;insevereconditions,strokecarriesahighriskofdeath. AccordingtoWHO(WorldHealthOrganization),15millionpeopleworldwidesuffera strokeannually.Ofthese,5milliondie,andanother5millionareleftpermanentlydisabled, placingaburdenonfamilyandcommunity.Strokeisuncommoninpeopleunder40years; whenitdoesoccur,themaincauseishighbloodpressure.However,strokealsooccursin about8%ofchildrenwithsicklecelldisease.
Objective:Toraiseknowledgeandawarenessaboutstroke,suchashowtodetectstrokes early.
Keywords: Geriatry,Stroke,EarlyDetection
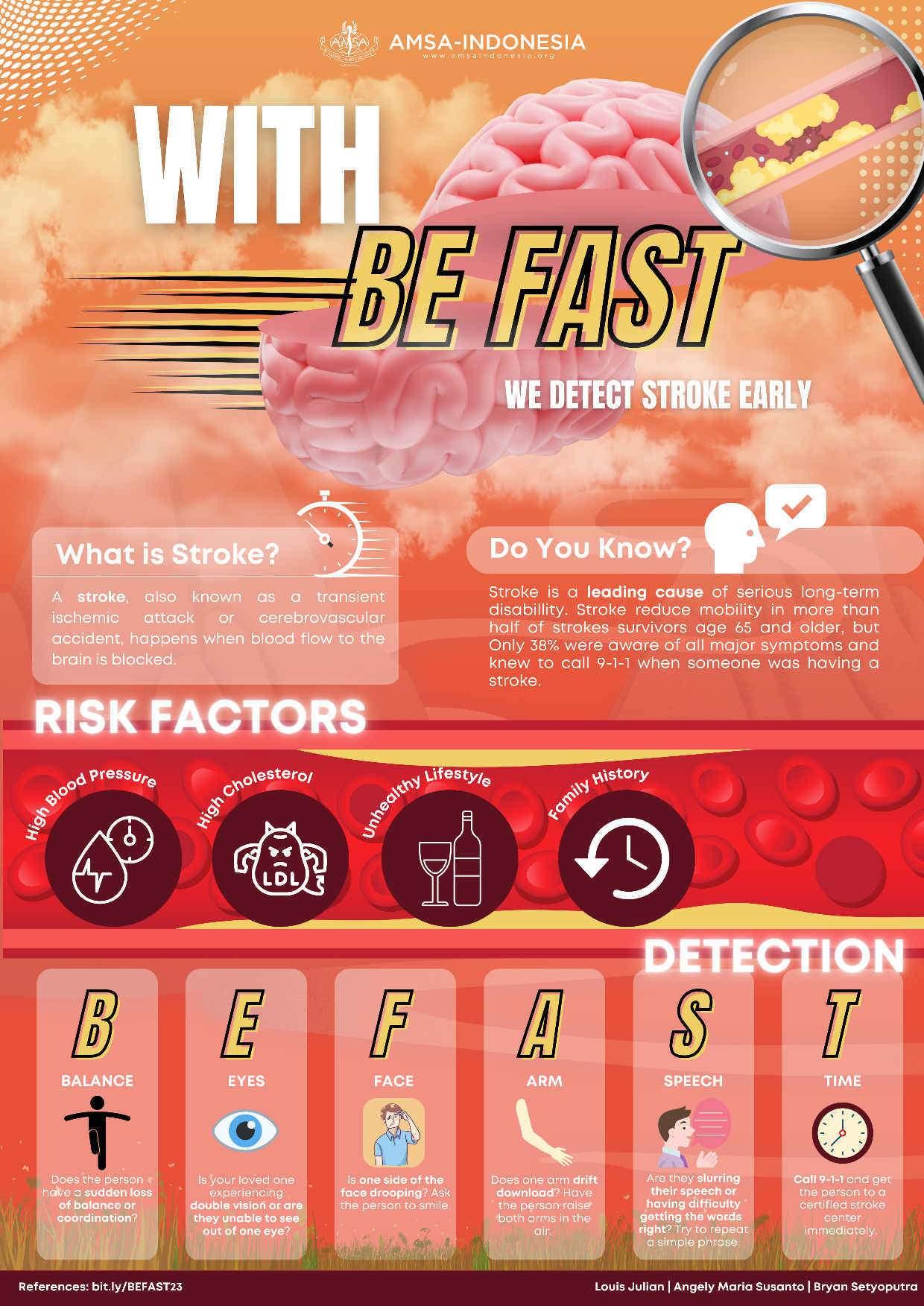
LET’S PREVENT OSTEOARTHRITIS WITH “DRUGS”
Yosef Raynard Gunawan, Teresa Jeanice, Eleonora Carmen Liem, Cecilia Audie Sutedja
[Correspondence
E-mail: raynardgunawan@gmail.com]
Background
Osteoarthritis (OA) is a degenerative joint disease in which joint cartilage is gradually lost. OA is commonly known as “wear-and-tear” arthritis. There are several risk factors that mostly contribute in osteoarthritis such women above 40-50 years old, obesity, poor nutrition, excessive activities, and hereditary osteoarthritis.
OA is one of the most prevalent disabling joint disorders that affects about 3.3 to 3.6% of the population globally. According to World Health Organization (WHO), the prevalence of osteoarthritis in the world is still high. Its impact on individuals results in pain and moderate to severe disability in 43 million people. Osteoarthritis mainly affects the knee, hand, hip, and spine. Therefore, as a result, of the total population worldwide, it is estimated that 80% will suffer from the limitation of movement, and another 20% will have a decreased quality of life. A study has shown that the majority of people, while waiting in a waiting room tends to read posters that are hanged around them. Therefore, this public poster hopefully contribute to raising public knowledge and awareness of osteoarthritis.
Objective
To increase public knowledge and awareness about osteoarthritis, including it’s definition, risk factors, and preventions.
Keywords
Geriatry, Osteoarthritis, Prevention

Alzheimer: Help! I Lost Myself Again
Gaisha Hayya, Cut Safira, Ghina Alhaya, Rifkah Ulimanisa
ABSTRACT
Did you know? Advanced age by itself does not createvulnerability. However, certain problemsthat are discovered and happen mostly during old age canincrease vulnerability. They include decrease strength, sensory awareness, and one of them is dementiathat most of them leaded by Alzheimer which is a progressive disease that destroys mental function then made the patient experience brain cells death, memory loss abnormalities and the awful fact that it is uncurable andaccounting for 50-70% of cases not just made the elderly more prone to the environment around them, but alsopossiblyburden people especially their close ones. As demographic ageing occurs, the global prevalence ofAlzheimerdisease is expected to continue to rise This figure is expected to increase almost 4 times by 2050, leading to a costly burden of disease. There are manytherapiesthat couldease the symptoms but palliative care or the care from people around them are the most important ones.Thesupport thatpeople can provide is keep a positive interaction with thepatient, do sports together, and other particular role as a part of society to decrease the chance of the disease to get even worst.
Keywords: alzheimer, disease,abnormalities, elderly
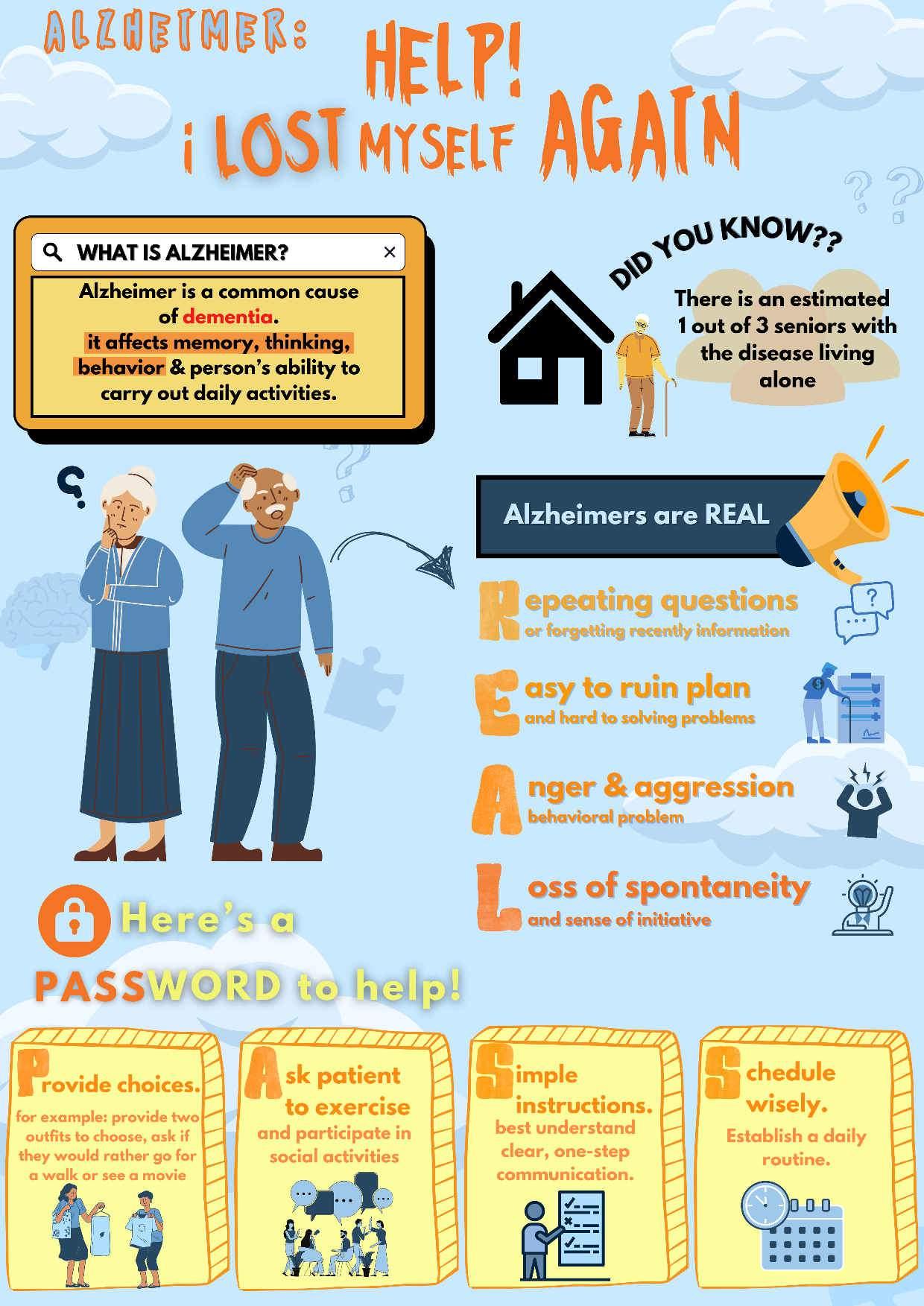
Recognizing the Appeared Difficulties of Dementia
Shafa Rizki Azzahra, Uswatul Fajri, Muhammad Daffa Zhafran, Irchi Amanda Az’Zahra
AMSA-Universitas Syiah Kuala
Abstract
Background: Dementia is a syndrome that can be caused by a number of diseases which over time destroy nerve cells and damage the brain, typically leading to deterioration in cognitive function beyond what might be expected from the usual consequences of biological aging. Centers for Disease Control and Prevention predict that of those at least 65 years of age, there is projected to be nearly 14 million adults with dementia by 2060.
We can recognize the common symptoms of dementia with 5 Difficulties which are Difficult to memorize, Difficult to perform familiar tasks, Difficult in managing the right words, Difficult in orientating time and place, and Difficult to handle mood changes. Dealing with the disease can be abbreviated with DEMENTIA that stands for Distractions need to be reduced, Establish a daily routine, Make simple instructions to be done by the person, Encourage the person to talk about something they like, Never forget to watch daily food intake, Try to help the person find answers themselves, Involve the person in mental or social activities, and Allow time for breaks during tasks.
Objective: We aim to convey visually appealing and easily understandable information to raise public awareness about dementia issues.
Keyword: dementia, difficulties, dealing with
Prevalence Prevalence
RECOGNIZING RECOGNIZING
THE APPEARED THE APPEARED OF OF DIFFICULTIES DEMENTIA DEMENTIA DEMENTIA
DIFFICULTIES DIFFICULTIES
Dementia is a syndrome that can be caused by a number of

Dementia is a syndrome that can be caused by a number of diseases which over time destroy nerve cells and damage the diseases which over time destroy nerve cells and damage the brain, typically leading to deterioration in cognitive function. brain, typically leading to deterioration in cognitive function.
The risk factors
The risk factors
Of those at least
Of those at least 65 years 65 years of age, there of age, there is an estimated is an estimated 5.0 million 5.0 million adults with adults with dementia dementia in 2014 in 2014 and, projected to be and, projected to be nearly nearly 14 million 14 million by 2060 by 2060. .
Distractions istractions need to be need to be reduced reduced
E stablish a stablish a daily routine daily routine M ake simple ake simple instructions instructions to be done to be done by the by the person person
Modifiable: Modifiable: Non-Modifiable: Non-Modifiable:

E N
ncourage the ncourage the person to person to talk about talk about something something they like they like
High blood pressure
High blood pressure
Smoking Smoking
Diabetes Diabetes
High cholesterol High cholesterol
Obesity and lack of Obesity and lack of physical activity physical activity
Poor diet Poor diet
ever forget ever forget to watch to watch daily food daily food intake intake
Try to help the ry to help the person find person find answers answers themselves themselves


Genetics Genetics
Gender Gender
Age Age
DIFFICULT
Involve the nvolve the person in person in mental or mental or social social activities activities
A
llow time llow time for breaks for breaks during during tasks tasks

For More For More Information, Information, Scan Here

to perform familiar tasks to perform familiar tasks to handle mood changes to handle mood changes to memorize to memorize
in orientating time and place in orientating time and place in managing the right words in managing the right words
SHAFA RIZKI AZZAHRA • USWATUL FAJRI • IRCHI AMANDA AZ'ZAHRA • MUHAMMAD DAFFA ZHAFRAN SHAFA RIZKI AZZAHRA • USWATUL FAJRI • IRCHI AMANDA AZ'ZAHRA • MUHAMMAD DAFFA ZHAFRAN
! Scan
Here !
ASimpleHacktoKeepYourKidneyinCheck:ChronicKidneyDiseaseinGeriatry
MeganAlyssaGunawan,ZeinabAbbaci,StevenGill,FarahFauzikaHaikal Abstract
Background: ChronicKidneyDisease,commonlyknownasCKD,referstoacondition involvingthedeteriorationorlossinfunctionofthekidneyinfilteringoutwastesandexcess fluidsfromtheblood,eventuallyleadingtoanaccumulationoffluidsandwastesinthehuman body.Accordingtopreviousstudies,theprevalenceofCKDinelderlywas30%,withatotalof 10.8%inAsiaalone.Thereareseveralriskfactorsassociatedwithchronickidneydiseasesuch as;diabetes,hypertension,ageequaltoormorethan55years,obesityormetabolicsyndrome, andthepresenceoffamilyhistoryofkidneydisease.Basedonthedatagathered,someofthe commoncausesofchronickidneydiseaseinclude;heartfailure,liverfailure,anduseof nonsteroidalanti-inflammatorydrugs.Inordertopreventoneselffromdevelopingchronic kidneydisease,theguidecalled“HACK”canbeutilized,whichencompasses4majorfactors: HealthyWeight, Avoid Smoking, ControlBloodPressure&Bloodsugar,and KidneyFunction Tests.
Objectives: Toraiseawarenessandenhancethepublic’sunderstandingoftherarelydiscussed butdeadlyillnesscalledChronicKidneyDisease
Keywords: ChronicKidneyDisease,Geriatry,Prevention

STOPYOURWORRIES,FIGHTALZHEIMER
LouisDarwinSusanto,MarchellaImmanuelHeriyanto,ThaliaKaylynAveril,JansenJayadi
[CorrespondenceE-mail:louisdarwinsusanto@gmail.com]
Background
Astheworld’spopulationcontinuestoagerapidly,withanestimated2.1billionpeopleoverthe ageof60by2050,coupledwithadeclineinthenumberofchildren,amonumentalshiftissetto occurincountries’populationdemographicsworldwideasaresult.Withthisinmind,itisinour bestinteresttoraiseawarenessregardingsomeofthedebilitatingdiseasesaffectingouraging population,namelyAlzheimer’sdisease,whichhastheabilitytoaffectapersonforlifeandmay leadtoadrasticreductioninqualityoflife.Inaddition,itisfoundthatawarenessamongthe populaceregardingAlzheimer’sdiseaseappearstobelow,whichisunfortunatewhentakinginto accounthowpivotalearlypreventionis.
Objectives
HencetheurgencytodetectAlzheimer’sdiseaseearlybyrealizingitssignsandsymptoms. Equippedwiththisinformation,wesetouttohelpolderadultsalongwiththeirprimary caregiverstoidentifytheearliestsignsofthisdiseasesuchthatitsprogressionmaybeslowedor evenhaltedentirelybeforeitprogressesfurther.Evenbeforethemanifestationofthefirstsigns, however,wealsowanttoeducatepeopleonhowtoreducetheirrisksofcontractingsaiddisease.
Keywords: Alzheimer’sdisease,elderly,prevention
Alz he m i e r ??
A declining condition of the brain which causes significant impairment in cognitive function and behaviour
Older Adults
Alzheimer :
of COGNITIVE IMPAIRMENT in elderly
Genetic Factors
andering/ Getting lost
People with Alzheimer: 33 million Worldwide ≥
Injuries & Infection Diabetes, cardiovascular disease, obese

Comorbidities
Bad Lifestyle
bstruction of daily tasks

emembering/ memory problem
easoning problem
ncreased anxiety and/or aggression
xperience mood & behavior changes
olving problem gets hard
Strengthen the connections between nerve cells
References: Get vitamin D to protect the brain

et some rays
alt bad lifestyle
Stop smoking, sleep well, eat healthy & exercise
Train some new skills
Play an instrument, read, learn a new language, etc
Alzheimer !!
1st SIGN!! FI
Stop Your FIGHT WORRIES H
nd social support G
.
Did you know?? LEADING CAUSE
OO RR RR II EE SS
Do You Have the Risks? Symptoms W W
FIGHT to Prevent
65 years
old
PRE-CONFERENCECOMPETITIONASIANMEDICALSTUDENTS’CONFERENCE
Geriatrics: CarefortheFuture
MINDMAYFAIL,BUTI-MINDWILLPREVAIL IntegratedTechnologyInnovationforAlzheimer’sPatients
GraceNataliaSari,IlonaNathania,RuthAngelica,TheresiaFelineHusen
Background: Alzheimer’sdiseaseisacommonandprogressivediseasethatimpairscognitivefunction andaltersmoods,thusdisturbingdailyactivities.Thisneurodegenerativedisorderhasbecomeadaunting healthproblem,whichcontributesto60–70%ofdementiacases.Approximately36.1millionindividuals wereaffectedbyAlzheimer'sdiseasein2019.Thisnumberispredictedtoalmostdoubleby2030(65.7 million)andeventripleby2050(115.4million).MostpeoplewithAlzheimer'sdiseaseareolderadults(> 65years).DuringtheCOVID-19pandemic,however,themajorityofolderadultpopulationswereunable toobtainadequatehealthcareaccess.Asaresult,telemedicineutilizationrosefrom21%in2020to43.3% in2021.Thisgrowthindicatesthattelemedicinemightbecomeapromisingalternativesolutionfor Alzheimer'spatients.Nevertheless,notelemedicineapproachhasbeenabletoprovideAlzheimer'spatients withall-encompassingcareuptothispoint.
Objectives: Thus,wewouldliketoproposeanovel,integratedtechnologyinnovation,intheformof telehealthwithadditionalfeaturesthatwillhelptoassistAlzheimer'spatients'needsholistically.
Keywords: Alzheimer’s,olderadults,telehealth,innovation

University : Universitas Swadaya Gunung Jati
Member :
1. Andi Mirelle Besse Amirah
2. Leegihan Varinsalova Y
3.
Siti Fatimah
The Effect of Diabetes in the Elderly on the Aging Population Issue
Indonesia is facing a period of aging population, characterized by low elderly mortality due to an increase in life expectancy along with a declining birth rate. With an increasing number of elderly individualsin Indonesia,theconcernfor theirhealthisbecomingamajorissue.Diabetesisahealth issue that’s the leading cause of death among the elderly, and its impact on the aging population is not yet fully understood. Many elderly people lack awareness of diabetes prevention, as seen from unhealthy eating habits and decreased physical activity. Unmanaged diabetes in the elderly will worsen the situation, leading to an increase in death rates among the elderly in the future. This’ll have a negative impact on Indonesia's economy and reduce the quality of health services. Health services should prioritize elderly health problems by implementing promotive, preventive, curative, and rehabilitative activities to help them regain their health, independence, and productivity. This study aims to identify the effect of diabetes on the elderly population in Indonesia and its significance in addressing the aging population problem. It will also highlight the importance of addressing diabetes among the aging population in Indonesia to ensure a better quality of life in the future.
Keywords: diabetes, aging population, health, elderly, future.
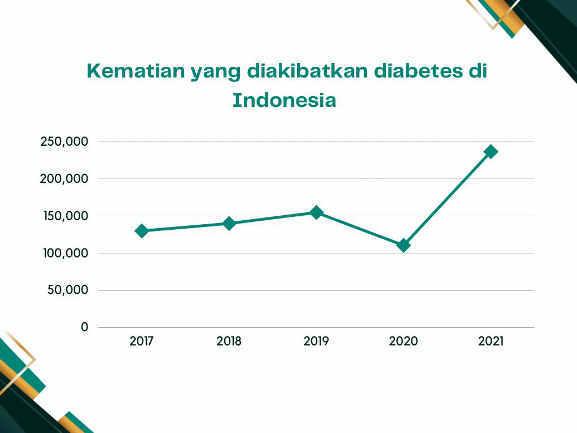

RECOGNIZE AND PREVENT ALZHEIMER DEMENTIA
M.Fathir Rahadian Ansary1 , Hasna Tazkia Aghni2 , Nafisya Ayu Evana3, Hadil Hudati Awwari Rameci4 , Faculty of Medicine Universitas Mataram
Email: radiansary011@gmail.com
ABSTRACT
Introduction: Dementia is a condition of decreased cognitive function where general symptoms are known, among others, difficulty thinking, remembering, making decisions, reducing emotions and difficult to communication well. The most common dementia is Alzheimer's Dementia. The reason we take thistopic, seenfrom the urgency where the prevalence of Indonesiansexperiencing Alzheimer's Dementia reached 1.2 million people in 2015, which is expected to continue to increase to 4 million people by 2050. Through this poster, we target our poster to be read by all circles of society, young and old so that this Alzheimer's problem is not considered trivial in society.
Purpose: provide insight to readers on how to recognize and prevent Alzheimer's Dementia in families and surrounding communities, especially the elderly who are prone to Alzheimer's Dementia
Keywords : Alzheimer Dementia, Recognize, Prevent

EmbracetheElderswithDementia
DeboraRiadiAlimSuprapto,FathinFathimahDianPutriGafur,NadiaDamayanti, AvantiHardianAnggraeni
Introduction: Dementiaisamedicalconditionwhichprogressivelydestroysnervecellsand damagesthebrain.Thisworsensthememory,thinking,andtheabilitytoperformdailyactivities.In 2020,over55millionpeopleworldwidesufferdementia,withonenewcaseevery3.2seconds.By 2030,itisestimatedthatthenumberwillincreaseto78millionpeople.Thus,thisshowstheurgency toeducatesocietyondementia,especiallytocaretakersofelderlypeoplewithdementia.Such measurestakenbythecaretakerwouldbeeffectivetocontributeabetterqualityoflifeforthe dementiapatients.
Objective: Toraiseawarenessondementiaalongwithitssymptomsandprevention.
Keywords: dementia,elders,memory
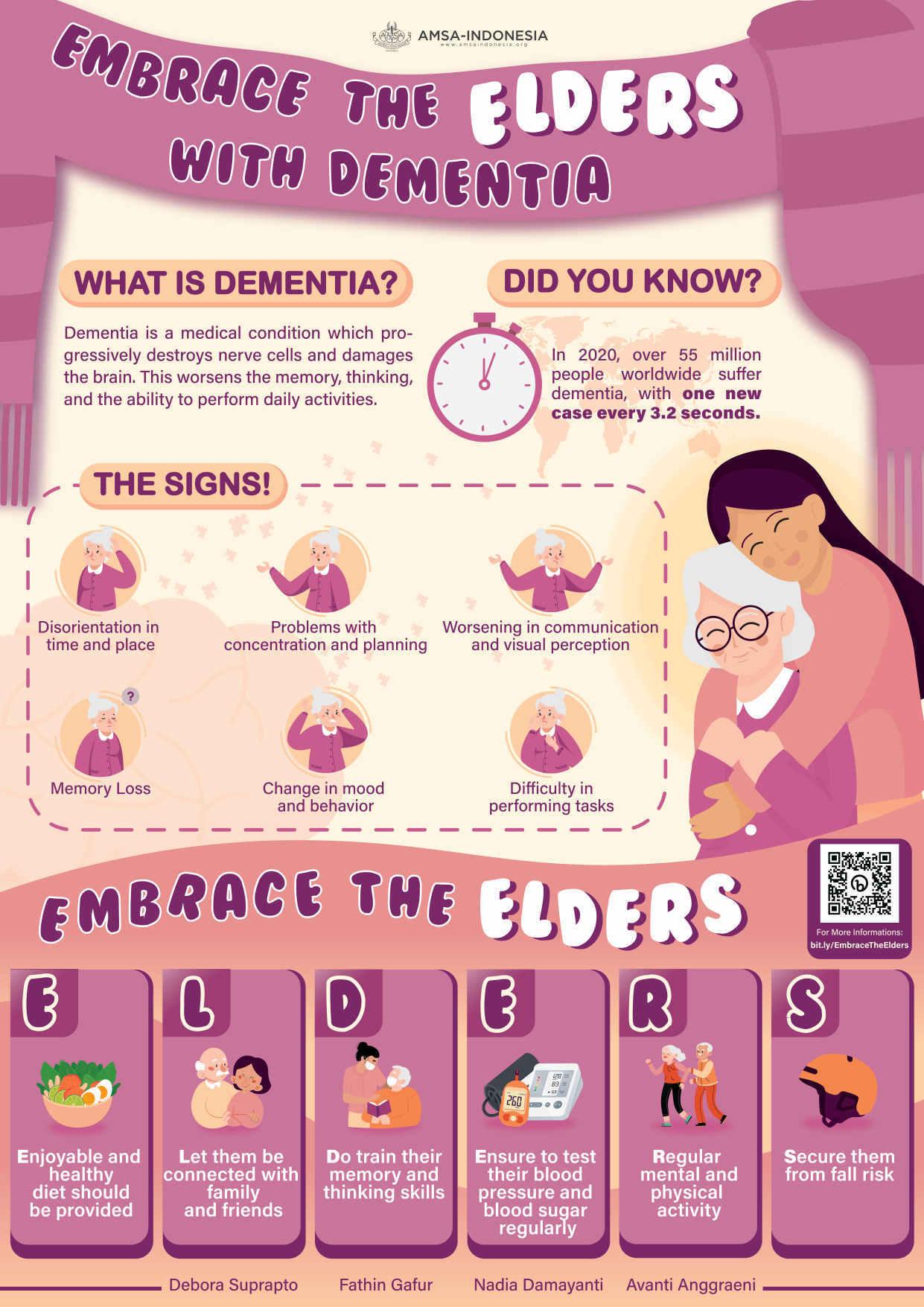
JadeAudreyHomentaRampengan1,DenisseOliviaTanoto1,DerrenDavidChristian HomentaRampengan2
AMSA-UniversitasKatolikIndonesiaAtmaJaya1,AMSA-UniversitasSamRatulangi2
Background: Asweage,there'sagraduallossofmusclemassandstrengthwhichdecreases ourphysicalcapability.Thisimpactstheelderly’squalityoflifesinceitreducestheirstrength whichhindersthemtoperformdailyactivities.Itcanleadtothelossoftheirindependence andtheneedforlong-termcare.Itaffects10%-16%oftheelderlyworldwide.
Objective: Wehopeourpostercanmotivatepeopletoimprovetheirphysicalcapability.Our mnemonic“STRONG”consistsof:
S -StretchDaily
Gentlystretchyourmuscleseverydaytomaintainflexibilityandpreventstiffness.
T -TakeShortWalks
Walkingisalow-impactexercisethatcanimprovecardiovascularhealthandbalance.
R -ResistanceTraining
Strengthenyourmusclesbyengaginginresistancetrainingatleasttwiceaweek.Uselight weightsordobodyweightexerciseslikesquats.
O -OptimizeBalance
Practicebalanceexercisestoincreasestabilitylikestandingononefoot.
N -NourishYourBody
Fuelyourbodywithabalanceddietrichinfruits,vegetables,leanproteins,andwholegrains.
G -GroupActivities
Participateingroupexerciseclassessuchastaichioryoga.Socializingandstayingactive canboostmoodandmotivation.
Keywords: Elderly,Physicalcapability,Strength.
StaySTRONG,AgeGracefully!

HYPEUpYourHealth
Background: AccordingtotheWorldHealthOrganization,approximatelyonebillionadults worldwidehavehypertension.Hypertensionismorecommoninolderadultsduetothe naturalagingprocess,increasedstiffnessofbloodvessels,andthedevelopmentofother healthconditionssuchasobesityanddiabetes.
Objective: Thispublicposterismadetoeducateabouthypertension.Weuse“HYPE”as abbreviationtopromoteahealthylifestylewhichconsistsof:
H -Homemonitoringofbloodpressure
It'sessentialtomonitoryourbloodpressureregularly,especiallyasyouage.Thiscanbedone athomewithabloodpressuremonitor.
Y -Yourdietmatters
Adietrichinfruits,vegetables,wholegrains,andleanproteinscanhelpaswellaslimiting salt,sugar,andprocessedfoods.
P -Physicalactivityiskey
Regularphysicallowersyourbloodpressure.Aimforatleast30minutesofmoderate exerciseperday,suchasbriskwalking,
E -Extraweight?Loseit
Excessiveamountsofalcoholandcaffeinecanraiseyourbloodpressure.Aimtolimityour intaketonomorethanoneortwodrinksperdayandavoidcaffeinelateintheday.
Keywords: Healthylifestyle,Hypertension,Olderadults.
AlexandraAudreyEustakia1,DenisseOliviaTanoto1,JadeAudreyHomentaRampengan1 , DerrenDavidChristianHomentaRampengan2 AMSA-UniversitasKatolikIndonesiaAtmaJaya1,AMSA-UniversitasSamRatulangi2

HandleDeliriumWithDEAL
DenisseOliviaTanoto1,JadeAudreyHomentaRampengan1,DerrenDavidChristian HomentaRampengan2
AMSA-UniversitasKatolikIndonesiaAtmaJaya1,AMSA-UniversitasSamRatulangi2
Background: Deliriumisanacutebraindysfunctionthatusuallydevelopsintheelderlyand isassociatedwithlong-termcognitiveimpairmentandfuturedementia.Itreducesthe patient’squalityoflifegreatlysincepatientssufferwithhallucination,poormemory,tothe pointofhavingslowedmovementsandspeechproblems. Deliriumiscommoninhospitalized olderadultsingeneralmedicalsettings,withoveralldeliriumprevalenceof 23%.
Objective: Wehopetocreateabetterworldfortheelderlybybringingthisissuetolightso thatpeoplemaybemoreawareandeducatedaboutdelirium.Weuse“DEAL”asan abbreviationwhichconsistsof:
D -Detectingthesymptomsofdeliriumearlyoniscrucialformanagingandpreventingit. Symptomscanincludeconfusion,agitation,hallucinations,andchangesinsleeppatterns.
E -Engagingwiththepatientandprovidingthemwithreassuranceandcomfortcanhelpto reducetheirsymptomsandpreventdeliriumfromworsening.
A -Assessingtheriskfactorsfordelirium,suchasmedicationchanges,dehydration,and infections,canhelptoidentifyandaddresspotentialcauses.
L- Limitingdisruptiveenvironmentalfactors,suchasnoiseandbrightlights,canhelpto createacalmenvironment
Keywords: Braindysfunction,Delirium,Elderly.
risk







A AL L
E SYMPTOMS SYMPTOMS HANDLE
DELIRIUM HOW TO HANDLE ? HOW TO HANDLE ? D D DETECT THE SYMPTOMS E E ENGAGE WITH THE PATIENT A A medications social isolation
D DE
WITH
factors risk factors DEHYDRATION Delirium is a serious change in mental abilities. It results in confused thinking and lack of awareness of someone's surroundings. L L LIMIT DISRUPTIVE environmental POOR MEMORY NONSENSE SPEECH HALLUCINATION MOOD SWINGS SLUGGISH !! !! ASSESS THE RISK FACTORS factors References: Mayo Clinic. Delirium - Symptoms and causes [Internet]. Mayo Clinic. 2020. Available from: https://www.mayoclinic.org/diseases-conditions/delirium/symptoms-causes/syc-20371386 Cleveland Clinic. Delirium and Mental Confusion: Symptoms, Causes, Treatment & Prevention [Internet]. Cleveland Clinic. 2020. Available from: https://my.clevelandclinic.org/health/diseases/15252-delirium NHS. Sudden confusion (delirium) [Internet]. NHS. 2019. Available from: https://www.nhs.uk/conditions/confusion/ 1. 2. 3. references
Prevent Osteoporosis with CARE
Authors: Hanggar Indra Kharisma, Sinclair Jorlando Kakambong, Derren David C.H. Rampengan, Ryan Bagy
ABSTRACT
Introduction: Osteoporosis is a prevalent condition that affects millions of people worldwide, particularly older adults. It results in weak and fragile bones, increasing the risk of fractures, disability, and reduced quality of life. This condition is associated with age-related decline in bone density and the inability of bones to absorb necessary minerals. It is estimated that 1 in 3 women and 1 in 5 men over 50 will experience an osteoporotic fracture. Risk factors include low body weight, smoking, excessive alcohol consumption, and physical inactivity. Early detection and treatment of osteoporosis can prevent fractures and improve quality of life.
Objective: Our public poster focuses on raising awareness about bone health from simple and practical actions by introducing, “CARE”
Consume calcium and vitamin D: Incorporate foods rich in calcium and vitamin D, like dairy products, leafy greens, fortified cereals and also consume supplements if needed.
Actively exercise: Stay active with exercises like walking, dancing, or lifting weights. Aim for at least 30 minutes of physical activity daily.
Reduce harmful habits: Quit smoking and limit alcohol to moderate levels for optimal bone health.
Establish a routine for regular screenings: We can always monitor the health of our bones.
Keywords: osteoporosis, bone, fracture, health, older
 Aisha Latifa
Aisha Latifa
Alzheimer’ s disease is a neurodegenerative disease with insidious onset and progressive impairmentofbehavioral andcognitivefunctionsincludingmemory,comprehension,language, attention, reasoning, and judgment. Alzheimer is the most common form of dementia, it may contribute to 60-70% of worldwide cases of dementia, which is currently more than 55 million cases of dementia (WHO, 2023).
Alzheimer has physical, psychological, social, and economic impacts, not only for people living with it, but also for their careers, families, and society at large. There is often a lack of awarenessandunderstandingofAlzheimer,resultinginstigmatizationandbarrierstodiagnosis and care. It’s hoped that our project might improve welfare of the patient with Alzheimer by raising awareness of it.
Therefore, throughthis poster to raiseawareness in societyabout warning signs ofAlzheimer’s disease, we invent ‘OH MY GOD’:
o Obstructed daily life due to memory loss
o Have struggles with words, speak or write
o Misplacing things and hard to retrace steps
o Yield to decreasing or poor judgment
o Getting confused with time or place
o Often have issues with problem solving
o Difficulty completing familiar tasks
References
o Anon., 2023. Alzheimer's Association. [Online]
Available at: https://www.alz.org/alzheimers-dementia/10_signs [Accessed 10 April 2023].
o Greenblat, C., 2023. World Health Organization. [Online]
Available at: https://www.who.int/news-room/fact-sheets/detail/dementia [Accessed 10 April 2023].
o Kumar, A., 2022. Alzheimer's Disease. s.l.:National Library of Medicine.
OH MY GOD! IS IT ALZHEIMER
Alzheimer OMG! IS IT
DO YOU KNOW?
ALZHEIMER IS A BRAIN DISORDER THAT SLOWLY DESTROYS MEMORY AND THINKING SKILLS. THIS ILLNESS GETS WORSE OVER TIME, AND MAINLY AFFECTS OLDER PEOPLE
60-70 %OUT OF 55 MILLION CASES OF WORLDWIDE DEMENTIA IS ALZHEIMER
OOBSTRUCTED

DAILY LIFE DUE TO MEMORY LOSS
MISPLACING THINGS AND HARD TO RETRACE STEPS
HAVE STRUGGLES WITH WORDS, SPEAK AND WRITE
YIELD TO DECREASING OR POOR JUDGMENT
GETTING CONFUSED WITH TIME OR PLACE

H m g Y o d
OFTEN HAVE ISSUES WITH PROBLEM SOLVING DIFFICULTY COMPLETING FAMILIAR TASKS
WARN
INGSIGNS OF ALZHEIMER
AISHA LATIFA
SOURCE
1.2 MILLION CASES IN INDONESIA (2016)
BewareofOsteoporosis,TakeCoverBehindRIBS
PutriUtamiLestari,PutiRaniaEsfandiary,PandhuPradipta NararyaPangemanan,AmeliaPutri Maharani
Background:Osteoporosisisaskeletaldisordercharacterizedbytheweakeningofbone microstructureintegrity.In2018,19.7%oftheIndonesianelderlypopulation(3.6million people)sufferedfromosteoporosis.Globally,anestimated200millionpeoplesufferfrom osteoporosis,whicharedominatedbyhigh-riskgroupssuchasmenopausalelderlywomen.It isalsoestimatedbytheInternationalOsteoporosisFoundationthatosteoporosisfractures countupto8.9millioncasesannually.Fromthosecases,hipfractureisthedeadliest osteoporosisfracturebasedonits20-24%mortality.Someriskfactorsofosteoporosisare non-modifiable,butnumerousmodifiableriskfactors,someofwhicharedietaryintake, physicalactivitylevel,andotherfactorssuchassmokingandalcoholconsumption,canbe intervenedtopreventthisdisease.Awarenessofthoseriskfactorsisanimportantkeyto ensuringthatpreventivemeasuresaretaken,especiallyforthoseinhigh-riskgroups.Someof thosemeasuresincluderegularexercise,intakeofvitaminDandabalanceddiet,bathing oneselfinsunlight,andstoppingtobaccoandalcoholconsumption.
Objectives:Thisposteraimsforcommunityawarenessthrougheducationaboutosteoporosis andpreventivemeasuresthatcanbetakentominimizepossibleriskfactors,especiallyin geriatricpatientsandmenopausalwomen.
Keywords: osteoporosis,education,awareness,preventive,high-riskgroup

Prevent Gout by Avoiding “STOPLABS”
Cecilia Audie Sutedja, Cecilia E.O.L Hutauruk, Bryan Setyoputra, Natasha Theodora [Correspondence E-mail: ceciliaaudie03@gmail.com]
Background
Hyperuricemia is a condition where there is an excess of uric acid in the blood that can lead to a disease called Gout. It’s caused by crystal deposition made of monosodium crystals and secondary to hyperuricemia. It deposits in joints or other tissues and causes a painful condition to the joint. It can also lead to the formation of kidney stones and the development of cardiovascular disease.
According to the World Health Organization (WHO), gout is a major cause of disability and contributes significantly to the burden of non-communicable diseases. Gout affects approximately 4% of adults in the United States, and its prevalence is increasing worldwide. Gout can be caused by a variety of factors including genetics, alcohol, renal impairment to excrete urate, and obesity. However we could avoid gout by avoiding some food such as seafood, tuna, organ meats, pork, lamb, alcohol, beef, and sardines. A study conducted among Koreanpatientsconcludedthatasimpleeducationalinterventioninincreasinggoutknowledge. Therefore, this public poster can hopefully contribute to reducing the burden of diseases at the national level.
Objective
To increase public knowledge and awareness about gout, including its definition, risk factors, and foods to avoid.
Keywords
Gout, hyperuricemia, geriatry, prevention
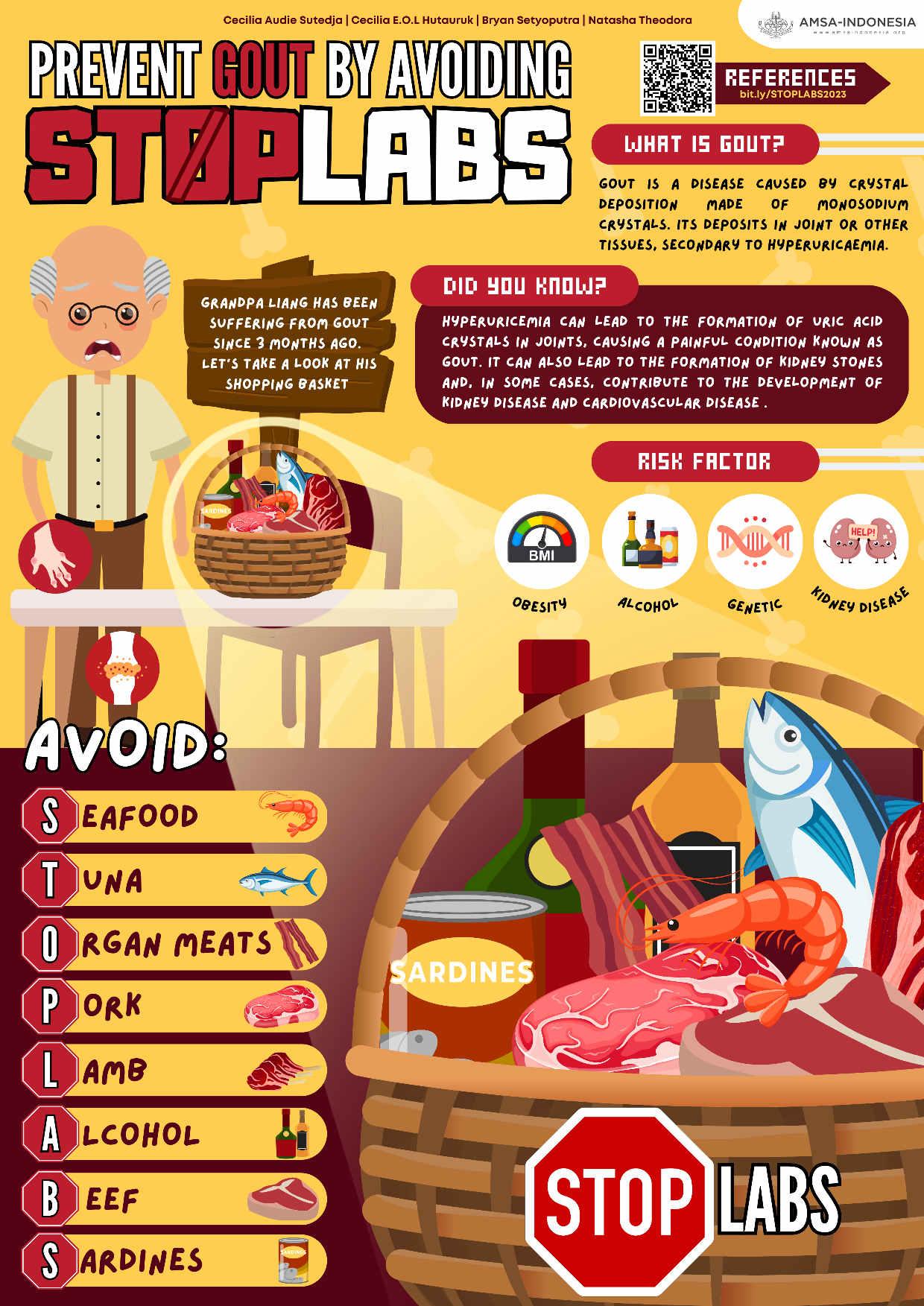
AUTHORS: RachelOlivia,AlmiraGloriana,CelineAurielle

TREATTHEELDERLYWITHCARE Pre-conferenceCompetitionAsianMedicalStudents’conference
FacultyofMedicine UniversityofPelitaHarapan 2023
TREATTHEELDERLYWITHCARE
RachelOlivia,AlmiraGloriana,CelineAurielle
[CorrespondenceE-mail: rachel.doloksaribu@gmail.com]
Background:Theagingprocessoccursduetotheaccumulationofavarietyofmolecularand cellularinjuriesovertime.Asaresult,physicalandmentalabilitiesgraduallydeteriorate, increasingsusceptibilitytoillnesses,andeventuallydeath.Hypertensionhadthehighest prevalenceamongthefivemostcommonillnesses,affecting83.4%ofthepopulation, followedbyosteoarthritis(54.0%),ischemicheartdisease(42.0%),osteoporosis(36.9%), andchronicobstructivepulmonarydisease(27.3%).Unfortunately,severalstudiessuggest that10%ofalladultsover65mayencountermistreatmentinhealthcaresettings.This includesbeating,misuseofrestraints,force-feeding,oranyotherbodilyharm.Itmightalso includeintimidation,threats,oranyotheractionthatcausesemotionalpain.Wecantherefore supporttheelderlyinmaintainingahighqualityoflifebyprovidingattentivecareand fulfillingtheirneeds
Objective:Tostopthemistreatmentoftheelderly,andprovideinformationaboutelderly care.
Keywords: Aging,health,mistreatment,elderlycare,qualityoflife

CLEARYourVisiontoPreventCataract
YongYeeWen,BryanSetyoputra,JeanAndrinaLiem,CelineAurielle
[CorrespondenceE-mail: yongyeewen1804@gmail.com]
Introduction/Background:
Cataractisadiseaseoftheeyeinwhichthenormallyclearlenshasopacifiedwhich obscuresthepassageoflight.Itisagraduallyprogressivedisease.AccordingtotheWorld HealthOrganization(WHO),cataractisresponsibleforapproximatelyhalfofallcasesof blindnessglobally,withanestimated65millionpeoplelivingwiththeconditionworldwide. Itisaleadingcauseofvisualimpairmentandblindness,andithasasignificantimpacton individuals,families,andcommunities.Cataractsnotonlyaffectaperson'sabilitytosee,but theyalsoimpacttheirqualityoflife,independence,andabilitytoperformdailyactivities. Theycanmakeitdifficulttoread,drive,andrecognizefaces,whichcanleadtosocial isolationanddecreasedqualityoflife.Inaddition,untreatedcataractscanleadtoother complications,suchasglaucoma,retinaldetachment,andothereyediseases.
Theawarenessofcataractsinsomeregionsandcommunitiesisrelativelyhigh,and peopleareawareoftheconditionanditseffectsonvision.Incontrast,inotherregions, cataractawarenessisrelativelylow,andmanypeoplemaynotbeawareofthecondition,its symptoms,orhowtopreventortreatit.Thislackofknowledgeoftenleadstothe continuationofbadhabitsthatcanincreasethechanceofdevelopingcataractsorevenmake themworse.
Objectives:
Thisposteraimstoincreasepublicknowledgeaboutcataracts,includingits definition,riskfactors,andprevention.
Keywords: Geriatry,Cataract,Prevention

TaketherightSTEPtopreventfalls!
1FacultyofMedicine,UniversitasTarumanagara
2FacultyofMedicine,UniversitasSamRatulangi
Abstract
Introduction:Globally,fallsareamajorpublichealthproblem.Fallsarethemost commoncauseoftraumaticbraininjuries(TBI).Fallsarethesecondleadingcause of unintentionalinjurydeathsworldwide.Eachyear,3millionolderpeoplearetreatedin emergencydepartmentsforfallinjuriesandatleast300,000olderpeoplearehospitalized forhipfractures(WHO,2021). Objective:Toraiseawarenessregardingtomaintain physicalhealthwithhelpolderadultstoreduceriskofinjury.“STEP”isasimple mnemonicthatwedesigntoraisetheelderly’scommunitycanawarenessandhelp preventfalls,suchasStrengthenyourlegswithexercises,Takeprecautions,Evaluate yourmedications,Practiceproperfootwear. Conclusion:Inthispublicposter,wewantto remembertotakingtherightstepsforfallpreventionisimportantformaintaining independenceandqualityoflifeinyourgoldenyears.Byfollowingthesesimpletipsand rememberingthe"STEP"mnemonic,wecanreduceriskoffallsandstayactive.
Keywords: Falls,TBI,Injury,Elderly
AshiraGraciana1,DanielHuang1,DerrenDavidChristianHomentaRampengan2,NatashaCita ParadhitaKusuma1

TheDementiaAdventure,HelpThemwithSparkles
DanielHuang1,NatashaCitaParadhitaKusuma1,DerrenDavidChristianHomentaRampengan2
1FacultyofMedicine,UniversitasTarumangara
2
FacultyofMedicine,UniversitasSamRatulangi
ABSTRACT
Dementiaisasyndromethatcanbecausedbyanumberofdiseaseswhichovertimedestroy nervecellsanddamagethebrain.Currentlyasthe seventhleadingcauseofdeath andresults fromavarietyofdiseasesandinjuriesthataffectthebrainaffecting 10millionnewcases worldwideeveryyear.Infactupto 40%ofdementiacasesmaybepreventedordelayed.We raisedthisposterwith“TheDementiaAdventure,HelpThemwithSparkles”.Becausecanlead situationiswhatwecanfoundonoursociety,memoryproblemsoccurandthisisnotidealso importanttoadventuretheknowledgeaboutcommonsymptoms.Tohelpthemwithabbreviated SPARKLESthatstandforSocialDancingandwalking,Playmusictherapyandcreativewriting, ArtVisualTherapy,Rekindlingloveofbooks,Keepupthehobbies,Living-friendly environment,Engageregularmedicalcheck-upwithdoctor,Spendtimewithfriendsandfamily. Mostpeoplewithdementiafacedamagethebrainonadailybasisandthiscanworsentheir condition.Howeverwecanandeducatethesocietyaroundelderlythatdementiaisaserious medicalconditionandifnottreated,canbeverydangerous-especiallytothemselves
Keywords: Dementia,Syndrome,Dangerous

Manage Diabetes in your golden years with HEALTH!
ABSTRACT
Introduction: Diabetes is a chronic condition that affects people of all ages leading to several complications including heart disease, kidney disease, and nerve damage. Approximately 1 in 5 adults aged 65 years or older have diabetes worldwide. The number is predicted to rise to 643 million by 2030 and 783 million by 2045.
Objective: This public poster focused on promoting lifestyle changes to prevent diabetes, by promoting lifestyle changes which are abbreviated as "HEALTH":
H - Have a healthy diet: Ahealthy diet can help prevent and manage diabetes in older adults.
E -Exerciseregularly: Exerciseis important for maintaining goodhealth andcan help prevent and manage diabetes.
A - Avoid smoking and alcohol consumption: Smoking and excessive alcohol consumption can worsen diabetes and increase the risk of complications.
L - Limit your sugar intake: Limiting your sugar intake can help prevent blood sugar spikes and reduce the risk of complications.
T - Take your medication as prescribed: Skipping doses or stopping medication without consulting your healthcare provider can lead to complications.
H - Have regular check-ups with your healthcare provider: Regular check-ups with your healthcare provider can help you monitor your diabetes and manage any complications.
Keywords: Diabetes, Lifestyle, Prevention

DASH DIET
Abstract
Hypertension is one of the most common worldwide health problems, the global burden of hypertension is increasing due to an aging population and increasing prevalence of obesity, and is estimated to affect one third of the world's population by 2025. In Indonesia, the prevalence of hypertension in older adults has reached 32,5%. Management strategies for hypertension in elderly is incluiding lifestyle modification. The risk factors of hypertension can be controlled to an extent by utilizing the DASH diet.
Keywords: Hypertension, older adults, management, lifestyle, DASH
DASH DIET
Follow these DASH (Dietary Approaches to Stop
Lean Meats

six 1-ounce servings or fewer a day. One serving is 1 ounce cooked meat, poultry or fish, or 1 egg.


Fruits

4 to 5 servings a day. One serving is one medium fruit, 1/2 cup fresh, frozen or canned fruit, or 1/2 cup fruit juice.




Low-Fat Dairy
2 to 3 servings a day. One serving is 1 cup milk or yogurt, or 1 1/2 ounces cheese.
Grains


6 to 8 servings a day. One serving is one slice bread, 1 ounce dry cereal, or 1/2 cup cooked cereal, rice or pasta.
Nuts, Seeds and legumens
4 to 5 servings a week. One serving is 1/3 cup nuts, 2 tablespoons peanut butter, 2 tablespoons seeds, or 1/2 cup cooked legumes (dried beans or peas).

Vegetables
4 to 5 servings a day. One serving is 1 cup raw leafy green vegetable, 1/2 cup cut-up raw or cooked vegetables, or 1/2 cup vegetable juice.

Source : DASH eating plan. National Heart, Lung, and Blood Institute. Ainun T | Nurul R | Zulaeyha A | Fiardi A
Fight Osteoarthritis be ACTIVE
Introduction: Osteoarthritis is a degenerative joint disease when the cartilage within the joint begins to break down and the underlying bone begins to change, slowly and get worse over time. Osteoarthritis can also cause pain, stiffness and swelling. 43% of people with Osteoarthritis are 65 or older, An estimated 240 million individuals worldwide have symptomatic Osteoarthritis, including 10% of men and 18% of women aged 60 and older. It occurs most commonly in the hands, hips, and knees. Understanding the essence of prevention is crucial for the elderly as it may improve their daily activity and well being.
Objective: To increase public knowledge and awareness of osteoarthritis, its symptoms, the places that can be affected, and its prevention.
Keyword: Osteoarthritis, Elderly, Prevention

Improving Physical Capability in the Elderly with KISS!
ABSTRACT
Introduction: Aging is a natural process, and as we grow older, our physical abilities tend to decline. However, we should not stop being physically active as staying mobile helps improve physical capability and prevent non-communicable diseases.
Objective: This public poster aimed to promote how physical activity can help improve physical capability and encourage overall health and well-being in the elderly, therefore we propose the KISS abbreviation, which consists of:
K eep moving
Regular physical activity can help improve physical capability, reduce the risk of chronic diseases, maintain strong bones, muscles, and joints, improve balance and coordination, and reduce the risk of falls.
I mprove physical capability
Gradually increasing the intensity of simple activities such as walking, swimming, dancing, and gardening can help improve physical capability.
S trength training is important
It helps improve muscle strength and mass, which can help reduce the risk of falls and improve overall physical capability.
S tay safe during activity
Before starting any physical activity, it is important to talk to your doctor, especially if you have any health conditions. Make sure to wear appropriate footwear and clothing, and stay hydrated during physical activity. Stop any activity if you experience pain or discomfort.
Keywords: Aging, Frailty, Physical Activities
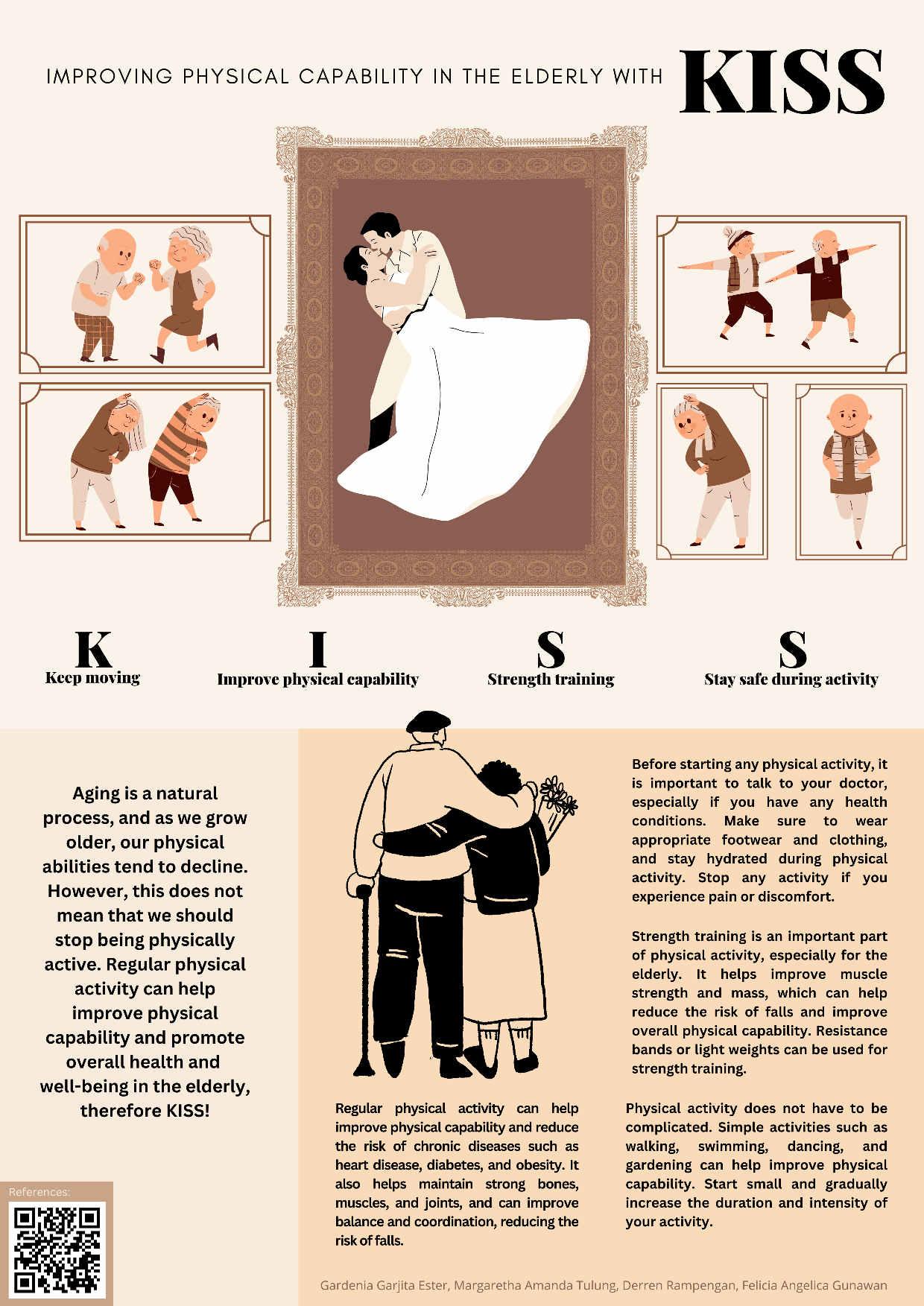
Introduction: Visualimpairmentisasignificantconcernfortheelderlypopulation worldwide.AccordingtotheWorldHealthOrganization,anestimated253millionpeople livewithvisionimpairment,andthisnumberisexpectedtotripleby2050.Age-related maculardegeneration,cataracts,andglaucomaaretheprimaryreasonsforthisimpairmentin theelderly.Thisissueaffectstheirabilitytoperformdailyactivitiesandcanleadtosocial isolationanddepression.Itisvitaltoaddressthisproblemandprovideappropriatesupport andcaretotheelderlypopulation.Moreattentionisneededtopreventtheimpactofvisual impairmentontheelderly'squalityoflife,emphasizingtheneedforawareness,early detection,andinterventionprograms.
Objective: Thispublicposterfocusedonpromotinglifestylechangesinelderlytoprevent visualimpairment,bypromoting,"SEE"
Scheduleregulareyeexams: Regulareyeexamsarecrucialformaintaininghealthy vision,especiallyinelderly.
Eatahealthydiet: Adietrichinfruits,vegetables,wholegrains,andleanproteins canhelpprotecteyesandmaintainhealthyvision.
Eyeexerciseregularly: Regulareyeexercisecanhelpimprovebloodflowtoeyes, whichcankeepthemhealthyandfunctioningproperly.
Keywords:visualimpairment,elderly,lifestyle,prevention
SEEYourWaytoaHealthyVisioninYourGoldenYears
Common Causes
Million People



Degeneration Cataracts


Glaucoma



SEE SEE WHO S S E E E E
chedule Reguler Eye Exam
S Go to your doctor and let them detect any potential problem early and recommen treatment


at a healthy diet E
Foods like salmon, leafy greens, and citrus fruits are particularly good for your eyes.
xercise regularly E

Some exercises that may help include eye yoga and eye stretching.
Remember SEE to take care of your eyes as you age so that you can have a healthy vision and see your golden years


SCAN ME!
 Aletheia H. PrastyoDerren D. C. H. RampenganGionina H alim
Aletheia H. PrastyoDerren D. C. H. RampenganGionina H alim
Afraid of Osteoarthritis? : HANDLE them with CARE!
ABSTRACT
Introduction: Osteoarthritis is one of the types of arthritis, also known as the degenerative joint disease that causes the cartilage within a joint to break down and the underlying bone to change. Osteoarthritis raises concerns as the prevalence of osteoarthritis in Indonesia increases with age, which is 5% for individuals aged <40 years, 30% for individuals aged 40-60 years, and 65% for individuals aged > 61 years.
Objective: This public poster aimed to spread awareness regarding osteoarthritis risk factors, summarized by using the HANDLE abbreviation as well as promote the prevention of osteoarthritis by encouraging a healthier lifestyle using the CARE acronym.
The risk factors of osteoarthritis include:
Have certain metabolic disease
Age
Not control your weight
Descent
Load of stress on the joint
gEenetics
The prevention of osteoarthritis centered on habit modification and consultation for the wellness of the joint, which summarized with:
Consult your doctor
Actively doing physical activity
Reduction of the meal and making diet plans
Eliminate the risk of joint injury
Keywords: Elderly, Degenerative Joint Disease, Healthier Lifestyle

AVOID BONE CRACK IN OSTEOPOROSIS WITH SPIRIT
Gratia Sharon Betosi, Charissa Melody Pali, Tesalonika Kyvenia Wilar, Lingkanwene Tosuraya Divaprinisa Malingkas
AMSA-Universitas Sam Ratulangi
Abstract
Introduction : Every year, over 8.9 million fractures are caused by osteoporosis. In Asia, osteoporosis is severely underdiagnosed and undertreated. Osteoporosis is a bone disease that progress when bone mineral density and bone mass decreases, resulting in remarkable changes in the structure and strength of the bone. Osteoporosis is a “silent” disease because you typically do not have symptoms or feel any pain, and you may not even know you have the disease until you break a bone. As stated in the title of the poster, CRACK stands for several risk factors that contribute to the development of this disease, including Cigarette smoking, histoRy of falls, older Age, alcohol Consumption, and lacK of nutrition. SPIRIT stands for the prevention for osteoporosis, including Sustain a well balance diet, Preventing falls, Intake enough calcium, protein, vitamin D and other nutrients, Remember to mantain your body weight, Improve balance, posture, coordination, and muscle strength with weight bearing exercise, and Tell your doctor if you have osteoporosis risk factors.
Objectives : To enhance public knowledge and awareness about osteoporosis, its risk factors, and how to prevent it.
Keywords : Osteoporosis, Fracture, Bone crack, Prevention
References :
1. International Osteoporosis Foundation. Prevention [Internet]. Switzerland: International Osteoporosis Foundation; 2023 [cited 2023 Mar 30]. Available from: https://www.osteoporosis.foundation/patients/prevention
2. National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis Causes and Symptoms [Internet]. Maryland: National Institutes of Health; 2022 Dec [cited 2023 Mar 30]. Available from: https://www.niams.nih.gov/healthtopics/osteoporosis
3. Cleveland Clinic. Osteoporosis: Symptoms, Causes, Tests & Treatment [Internet]. Ohio: Cleveland Clinic; 2020 Apr 27 [cited 2023 Mar 30]. Available from: https://my.clevelandclinic.org/health/diseases/4443-osteoporosis
4. Pouresmaeili F, Kamalidehghan B, Kamarehei M, Goh YM. A comprehensive overview on osteoporosis and its risk factors. Ther Clin Risk Manag. 2018 Nov 6;14:2029-2049. doi: 10.2147/TCRM.S138000.
5. International Osteoporosis Foundation. EPIDEMIOLOGY OF OSTEOPOROSIS AND FRAGILITY FRACTURES [Internet]. Switzerland: International Osteoporosis Foundation; 2023 [cited 2023 Mar 30]. Available from:
https://www.osteoporosis.foundation/facts-statistics/epidemiology-of-osteoporosisand-fragility-fractures
6. International Osteoporosis Foundation. KEY STATISTICS FOR ASIA [Internet].
Switzerland: International Osteoporosis Foundation; 2023 [cited 2023 Mar 30].
Available from: https://www.osteoporosis.foundation/facts-statistics/key-statistic-forasia
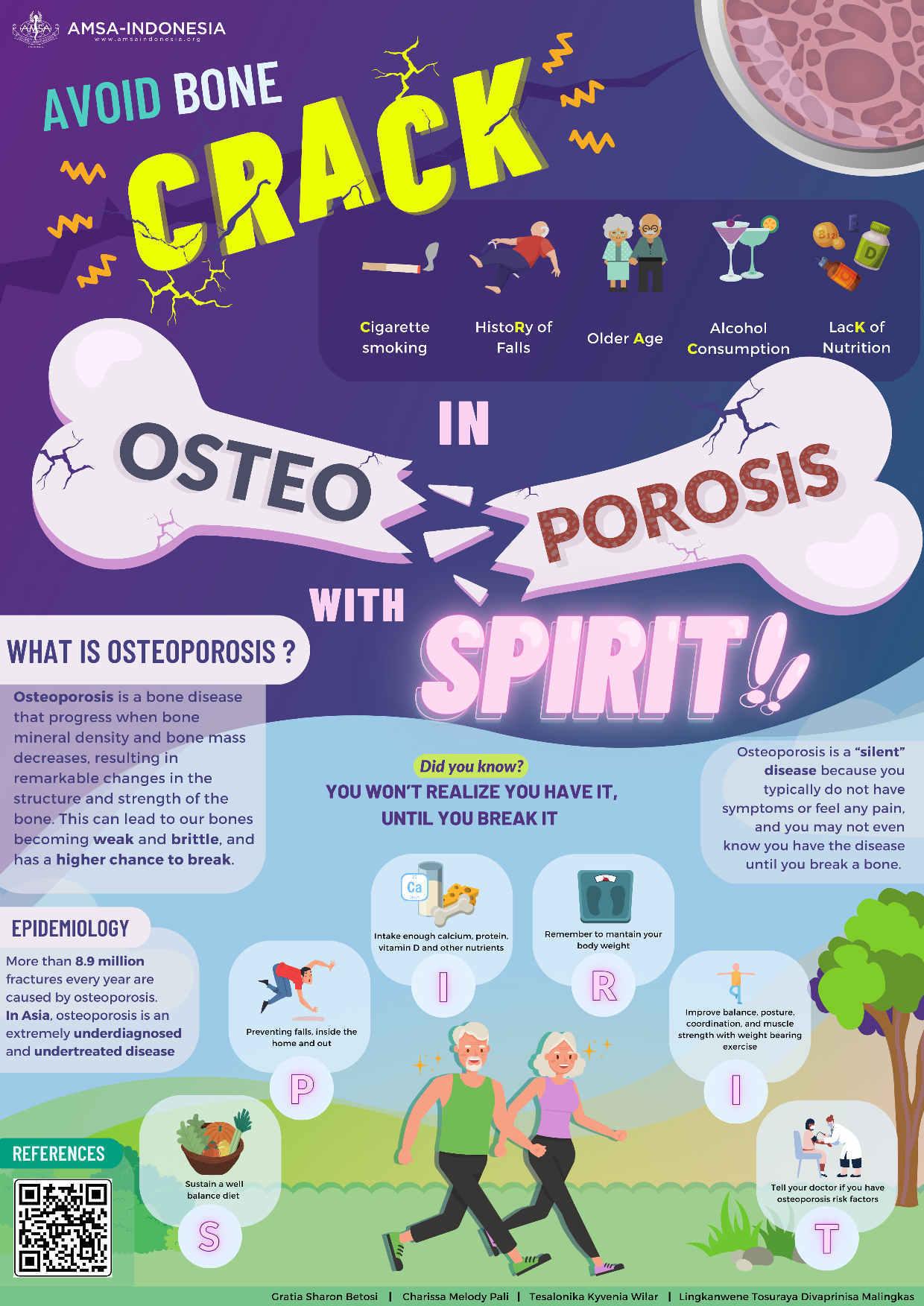
BE SMART to Prevent Stroke in the Elderly
ABSTRACT
Introduction: Stroke is one of the leading causes of disability and death among elders. However, Stroke is largely preventable as simple lifestyle changes can significantly reduce the risk of having a stroke.
Objective: This public poster centered on stroke prevention methods by promoting lifestyle conversion towards healthier habits. We encourage and spread awareness of stroke prevention by using B.E. S.M.A.R.T.
B - Blood pressure control
E - Eat a healthy diet
S - Stay active through exercise
M - Minimize alcohol consumption
A - Avoid smoking
R - Reduce your risk of stroke
T - Take control of your health
Keywords: Lifestyle, Non-Communicable Disease, Stroke

DefeatDementiawithDREAMS!
Introduction: Dementiaisadiseasecharacterizedbylossofmemory,language, problem-solving,andotherthinkingabilitiesthataresevereenoughtointerferewithdailylife. Disordersgroupedunderdementiaarecausedbyabnormalbrainchanges.In2016,1.2million Indonesianssufferedfromdementiaanditispredictedthatthenumberswillescalateto4.2 millionby2050.Thus,thisshowstheimportanceofawarenessofthepublicondementia. However,therehasbeennoeducationalposterfocusingoninformingthepublicaboutthe definition,epidemiology,signsandsymptoms,andevenpreventionofdementiaintheelderly comprehensivelyusingengagingmnemonics.
Objectives: Thisposteraimstoraisepublicawarenessofdementiaalongwithitssymptomsand prevention,especiallyamongtheelderly.Fromthat,publicknowledgeaboutdementiawould increaseevenmorewhichcouldcontributetoadecreaseintheprevalenceofdementiainthe elderly,bothnationallyandglobally.
Keywords: dementia,elderly,memory,prevention

BEWARE!BeatOsteoarthritiswithMOTION
Introduction: Osteoarthritis(OA)isadegenerativehealthproblemthatcausespain,limited physicalfunction,decreasedqualityoflife,anddisability.OAaffects60−70%ofthepopulation over65yearsworldwideandisassociatedwithhightreatmentcosts.OAhasafairlyhigh prevalenceinIndonesia,namely5%attheageof<40years,30%at40-60years,and65%atthe ageof>61years.Fromthesedata,itcanbeunderlinedthatthesusceptibilitytocartilage degradationbecomesveryhighwithincreasingage.Therefore,thereisanurgentneedtoraise publicawarenessregardingtheriskfactors,signsandsymptoms,prevention,andtreatmentsof OA,especiallyintheelderly.However,therehasbeennopublicposterfocusingoneducating peoplecomprehensivelyaboutthedefinition,riskfactors,epidemiology,signsandsymptoms, prevention,andmanagementofOAintheelderlyusingengagingmnemonics.
Objectives: Thisposteraimstoincreasepublicknowledge,especiallyamongtheelderly,about OAandtheimportanceofknowingitsriskfactors,signsandsymptoms,preventions,and treatments.Fromthat,people’sawarenessofOAwouldincreaseevenmorewhichcould contributetoadecreaseinthenumberofOAintheelderly.
Keywords: elderly,prevention,OA,osteoarthritis,treatment
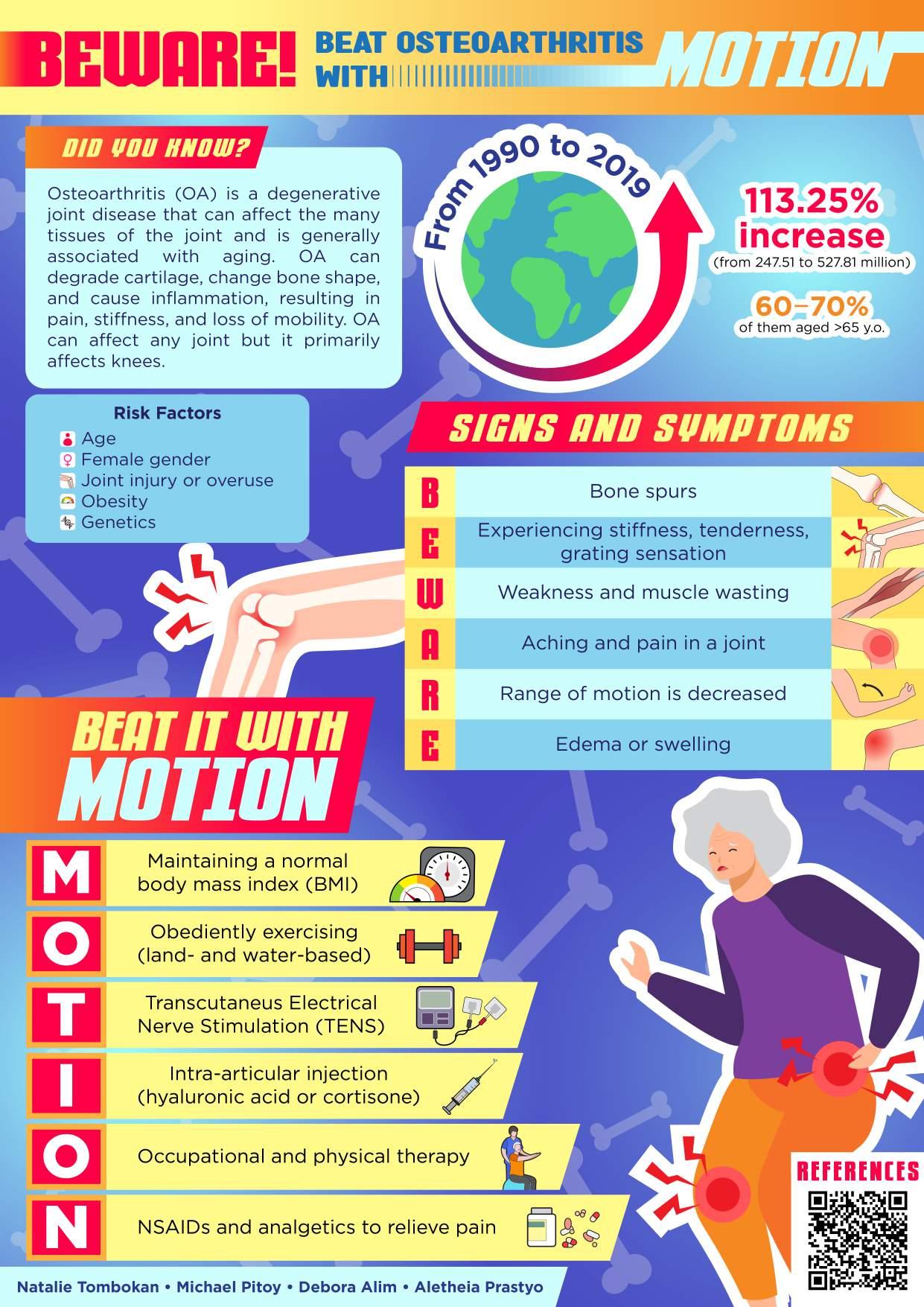
Keep your Mind Sharp with MEMORY!
ABSTRACT
Introduction: Dementia is a term used to describe a group of symptoms affecting memory, thinking, and social abilities that are severe enough to interfere with daily life. The risk of developing dementia increasing with age.An estimated 50 million people living with dementia in 2020, and this number is projected to triple by 2050.
Objective: This public poster focused on promoting lifestyle changes to reduce the risk of developing dementia, by promoting a lifestyle changes abbreviated as "MEMORY"
M - Mind Exercises: Keep your mind active and engaged by doing puzzles, reading books, or learning new skills.
E - Exercise: Regular physical activity can improve brain function and reduce the risk of developing dementia.
M - Manage Stress: Stress can affect brain health. Try relaxation techniques like meditation or deep breathing exercises.
O -Organize:Keepyour environment organizedto avoid confusionanddisorientation. Create a routine and stick to it.
R - Routine Medical Check-ups: Regular check-ups with your healthcare provider can help detect and treat any cognitive decline early on.
Y - Your Diet:Ahealthy diet can help reduce the risk of developing dementia. Include plenty of fruits, vegetables, and whole grains in your diet.
Keywords: Dementia, Lifestyle, Memory, Prevention

Keep Your Heart Healthy with HEART!
ABSTRACT
Introduction: As we age, our risk of developing cardiovascular disease (CVD) increases. According to the data from American Heart Association It is estimated that 70% of people over 70 years old will develop CVD. There are some measurements that can be taken in order to maintain the well-being of the heart and reduce the risk of heart disease.
Objective: This public poster aimed to encourage a healthy lifestyle in order to sustain the wellness of the heart, aligning with the HEART mnemonic.
H - Healthy foods: choose heart-healthy foods like fruits, vegetables, whole grains, lean proteins, and healthy fats.
E - Exercise regularly: move more every day with at least 30 minutes of moderateintensity exercise most days of the week.
A - Avoid smoking: quit smoking to reduce your risk of cardiovascular disease.
R - Reduce stress: manage stress with healthy habits like meditation, yoga, or spending time with loved ones.
T - Take care of your health: stay on top of your health with regular check-ups and screenings.
Keywords: Cardiovascular Disease, Lifestyle, Heart Well-being

Prevent Diabetes with 4 M's!
ABSTRACT
Introduction: Diabetes is affecting about 33% of people aged 65 and older. The majority of older adults with diabetes have type 2 diabetes due to increased insulin resistance and impaired insulin secretion caused by factors such as adiposity, sarcopenia, and physical inactivity. The clinical course of older adults with diabetes is often complicated by concomitant chronic diseases, which can accelerate the progression of diabetic complications and increase the risk of mortality, cardiovascular and microvascular complications, cognitive impairment, frailty, unintentional weight loss, and functional impairment.
Objective: This public poster focused on promoting lifestyle changes in elderly to prevent diabetes, by promoting, "Move, Meals, Monitor, Motivation" or simply "The 4 M's"
Move: Exercise regularly to maintain a healthy weight and improve insulin sensitivity. Low-impact activities like walking, swimming, and chair exercises can be ideal for older adults.
Meals: Choose a balanced diet with plenty of vegetables, fruits, whole grains, lean protein, and healthy fats. Limit processed and sugary foods and drinks.
Monitor: Keep track of your blood sugar levels, blood pressure, and cholesterol. Regular check-ups can help you catch and manage diabetes early.
Motivation: Stay motivated and committed to your health goals. Connect with others for support and accountability.
Keywords: Diabetes, Elderly, Lifestyle, Prevention
PREVENT DIABETES 'S
is a chronic disease that’s common among older adults, affecting an estimated 33% of people aged 65 and older. Older adults with diabetes have an increased risk of complications and mortality.
TAKE


Choose a balanced
diet
M WITH Motivation
THE
M'S
STAY HEALTHY AND PREVENT DIABETES
REMEMBER
4
TO
Monitor
DIABETES? DIABETES?
CONTROL OF YOUR HEALTH AND PREVENT DIABETES WITH THE 4 M'S!
track your blood
levels, and manage diabetes
Move Meals regularly ! Walking, swimming, and chair exercises can be ideal
Keep
sugar
early. Exercise
Stay motivated and committed. Connect with others for support and accountability.
with vegetables, fruits, whole grains, and lean protein.
Background: Patient-CenteredCare(PCC)isanapproachtomultimorbiditygeriatriccarethat placeseldersascapableadultsabletomakeinformeddecisions.Inprovidingholisticgeriatric care,eldersmayfeeluncomfortablewiththeircaregivers.Additionally,morethan30%elders aged45andabovefeellonelyandabout25%eldersaged65andabovearesociallyisolated.So, althoughspecialcareandmedicalinterventionareimportantpartsofgeriatriccare,itis insufficientforholisticPCC.HolisticPCCneedspeersthatcanprovideacomfortablespaceto obtaindailystimulationforhealthyagingandbetterqualityoflife.Thus,anelderlysocialgroup isrecommended.Itaimstobeanoutletforelderstofreelychoosetheirprioritiesandfindpeers.
Objectives: toincreasethecomprehensionofsociety,especially thoselivingwithgeriatrics, regardingsocialgroups'importanceandencouragethemtoimplementtheintervention.
Description: Therearetwomnemonics(PEERSandRELISH).Theinterventionwesuggestto fulfillpatient-centeredholisticcareisPEERS,whichallowsgeriatricstoconnect,provide support,andimprovetheirwell-being,whileminimizingsocialisolation.Activitiesthatcanbe donesogeriatricsmayRELISHarereminiscingmemories,exploring,sharing,conducting spiritualactivities,andhobbies.
Keywords: socialgroup,elderly,loneliness,socialisolation,personalizedcare
REFERENCES
1.WorldHealthOrganization.Integratedcareforolderpeople(ICOPE):guidancefor person-centredassessmentandpathwaysinprimarycare[Internet].Geneva:World HealthOrganization;2019Jan1[cited2023Apr8].Availablefrom: https://www.who.int/publications/i/item/WHO-FWC-ALC-19.1
2.EbrahimiZ,PatelH,WijkH,EkmanI,Olaya-ContrerasP.Asystematicreviewon implementationofperson-centeredcareinterventionsforolderpeopleinout-of-hospital settings.GeriatrNurs.2021Jan-Feb;42(1):213-24.
3.NilsenER,HollisterB,SöderhamnU,DaleB.Whatmatterstoolderadults?Exploring person-centredcareduringandaftertransitionsbetweenhospitalandhome.JClinNurs. 2022Mar;31(5-6):569-81.
4.CordesT,BischoffLL,SchoeneD,SchottN,Voelcker-RehageC,MeixnerC,etal.A multicomponentexerciseinterventiontoimprovephysicalfunctioning,cognitionand psychosocialwell-beinginelderlynursinghomeresidents:astudyprotocolofa randomizedcontrolledtrialinthePROCARE(preventionandoccupationalhealthin long-termcare)project.BMCGeriatrics.2019Dec23;19(1):369.
5.SalomoniF,RasiHA,HosseinzadehS.EmpoweringelderlyIraniansthroughasocial groupworkintervention:atrialstudytoassesstheeffectoftheinterventionon participants'qualityoflife.HealthSocCareCommunity.2018Nov;26(6):917-24.
6.TanakaS,YamagamiT,YamaguchiH.Effectsofagroup-basedphysicalandcognitive interventiononsocialactivityandqualityoflifeforelderlypeoplewithdementiaina geriatrichealthservicefacility:aquasi-randomisedcontrolledtrial.Psychogeriatrics. 2021Jan;21(1):71-9.
7.CuevasPE,DavidsonPM,MejillaJL,RodneyTW.Reminiscencetherapyforolder adultswithalzheimer'sdisease:Aliteraturereview.InternationalJournalofMental HealthNursing.2020;29(3):364–71.
8.LimaS,TeixeiraL,EstevesR,RibeiroF,PereiraF,TeixeiraA,etal.Spiritualityand qualityoflifeinolderadults:Apathanalysismodel.BMCGeriatrics.2020;20(1).
9.EckstromE,NeukamS,KalinL,WrightJ.Physicalactivityandhealthyaging.Clinicsin GeriatricMedicine.2020;36(4):671–83.
10.KuritaS,TsutsumimotoK,DoiT,NakakuboS,KimM,IshiiH,etal.Associationof physicaland/orcognitiveactivitywithcognitiveimpairmentinolderadults.Geriatrics &GerontologyInternational.2020;20(1):31–5.
11.Coelho-JúniorHJ,CalvaniR,PanzaF,AllegriRF,PiccaA,MarzettiEandAlvesVP. Religiosity/spiritualityandmentalhealthinolderadults:asystematicreviewand meta-analysisofobservationalstudies.FrontMed(Lausanne).2022May12;9:877213.

BewareofFRAILTY,EmbraceHEALTHYAging
Introduction:
Frailtyisacommongeriatricsyndromecharacterizedbyage-relateddeclinesinphysiological andfunctionalprocessesacrossorgansystems,increasingsusceptibilitytounfavorable outcomes.Prevalenceoffrailtyintheworldis10.7%whereAsiahasahigherprevalenceof frailtythanEurope.Anotherscaryfactisthatfrailtyincreasestheriskofmorbidityand increasesthelikelihoodofdeathwithinayearbyfivetimes.Frailtysymptomsincludefeeble gripstrength,reducedwalkingspeed,accidentalweightloss,incontinence,lowenergy, mentalproblem,andlowphysicalactivitythatabbreviatedintheposterasFRAILTY.Frailty canbebroughtonbymalnutrition,lowintensityexercise,olderage,smoking,anddiabetes. Frailtyisavoidable,andeveryonecanagehealthily.Therefore,wecouldlowertheriskby followingHEALTHY,namelyahappyenvironment,exercisewell,adequatevitaminintake, lowfatandsodiumdiet,takeawalkunderthesunlight,highfiberandcalciumfoods,and maintainhygiene.Preventionoffrailtycanimprovethewell-beingoftheelderlyandhavea highpotentialtoreducethemortalityrateeachyear.
Objective:
Thisposteraimstospreadawarenesstopreventfrailtyandattainhealthyagingamong geriatricandelderly.
Keywords: frailty,healthyaging,geriatricsyndrome

Don'tLetYourGoldenYearsDimYourVision!: KeepYourGoldenYearsVisionShiningwithEYECARE!
Introduction: Age-relatedeyediseases,suchasage-relatedmaculardegeneration(AMD), cataracts,glaucoma,anddiabeticretinopathy,aresignificantcausesofvisualimpairmentand blindnessinolderadultsworldwide.AMD,inparticular,hasaffectedover196million people,1 andcataractshavebeenreportedtoaffectover90%ofpeopleovertheageof65in low-andmiddle-incomecountries.2 Glaucomahasaffectedover64millionpeople worldwide,3 anddiabeticretinopathyaffectsover93millionpeopleglobally.4 Withthe growingglobalagingpopulation,theseproblemsarestillprevalentandpreventablethrough appropriateinterventions.However,thecurrentpublicunderstandinglackspractical recommendationsforspecificpopulations,particularlytheelderly.5
Objectives: Toincreaseawarenessandunderstandingtheriskfactorsassociatedwiththese eyeconditionsanddevelopingeffectivepreventionandtreatmentstrategiesarecriticalto reducetheburdenofvisualimpairmentandimprovethequalityoflifeforolderadults.
Description: Toachievetheseobjectives,wehaveintroducedatagline,"KeepYourGolden YearsVisionShiningwithEYECARE!"andcreatedaneasy-to-remembermnemonic,"EYE CARE."ThisacronymstandsforEyeexams,6 Year-roundsunprotection,Eatingabalanced diet,7,8 Consistentexercise,9 Avoidingdigitaleyestrain,andREgularlyrestingyoureyes.6-8 Theseapproachesaimtoprovideamorepracticalapproachthatcanbedonewithcontinuous effortandemphasisontheshiningvisionoftheelderly'sgoldenage.Thisposterisaresponse tofillthegapofthelackofeducationforitiscrucialtoincreasepublicawarenessand providepracticalrecommendationstopreventandmanagetheseconditions,whichcan significantlyimprovethequalityoflifeforolderadults.5,6,8
Keyword: age-relatedeyedisease,geriatric,vision,
References
1.JonasJB,CheungCMG,Panda-JonasS.Updatesontheepidemiologyofage-related maculardegeneration.AsiaPacJOphthalmol[Internet].2017Sep14[cited2023Apr 12];6(6):493–7.Availablefrom:https://pubmed.ncbi.nlm.nih.gov/28906084/
2.JolleyE,VirendrakumarB,PenteV,BaldwinM,MailuE,SchmidtE.Evidenceon cataractinlow-andmiddle-incomecountries:anupdatedreviewofreviewsusingthe evidencegapmapsapproach.IntHealth[Internet].2022Apr6[cited2023Apr 12];14(Suppl1):i68–83.Availablefrom: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8986350/
3.AllisonK,PatelD,AlabiO.Epidemiologyofglaucoma:Thepast,present,and predictionsforthefuture.Cureus[Internet].2020Nov24[cited2023Apr 12];12(11):e11686.Availablefrom: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7769798/
4.YauJWY,RogersSL,KawasakiR,LamoureuxEL,KowalskiJW,BekT,etal.Global prevalenceandmajorriskfactorsofdiabeticretinopathy.DiabetesCare[Internet].
2012Feb1[cited2023Apr12];35(3):556–64.Availablefrom: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3322721/
5.DiCarloE,AugustinAJ.Preventionoftheonsetofage-Relatedmacular degeneration.JClinMed[Internet].2021Jul26[cited2023Apr13];10(15):3297. Availablefrom:https://pubmed.ncbi.nlm.nih.gov/34362080/
6.AmericanOptometricAssociation.Adultvision:41to60yearsofage[Internet]. www.aoa.org.2021[cited2023Apr13].Availablefrom: https://www.aoa.org/patients-and-public/good-vision-throughout-life/adult-vision-19-t o-40-years-of-age/adult-vision-41-to-60-years-of-age?sso=y
7.AmericanAcademyofOphthalmology.Sunglasses:ProtectionfromUVeyedamage. [Internet].www.aao.org.2021[cited2023Apr13].Availablefrom: https://www.aao.org/eye-health/tips-prevention/sunglasses-eye-damage-protection
8.CenterforDiseaseControlandPrevention.Healthyagingincludeshealthyvision [Internet].CentersforDiseaseControlandPrevention.2021[cited2023Apr12].
Availablefrom:
https://www.cdc.gov/visionhealth/resources/features/healthy-aging-vision.html
9.OngSR,CrowstonJG,LoprinziPD,RamuluPY.Physicalactivity,visualimpairment, andeyedisease.Eye[Internet].2018Apr3[cited2023Apr13];32(8):1296–303.
Availablefrom:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6085324/

"SMILE and Beat Depression in Your Golden Years!"
Background: Depression is a common mental health disorder affecting all ages worldwide, with an estimated 264 million people affected in 2022. The prevalence of depression increases with age and studies show that 7.5% aged 60 years and above experience depression. In contrast, depression in the elderly is often underdiagnosed and undertreated, which cause negative consequences for overall health and quality of life. Thus, patients should consider a comprehensive treatment to reduce and prevent depression progression. SMILE as an abbreviation aims to be a simple and catchy reminder to beat depression in geriatrics.
1. Seek help from a professional: Depression is responsive to treatment, thus seeking help from a healthcare professional is important.
2. Manage stress levels: Find healthy ways to manage stress, such as meditation, or deep breathing exercises.
3. Increase physical activity: Regular moderate activity can boost mood and reduce depression.
4. Laugh and socialize with others: Spending time with family or social groups can help combat loneliness and social isolation..
5. Eat a healthy, balanced diet: A diet rich in fruits, vegetables, whole grains, and lean proteins can help provide functional nutrients.
Objective: to effectively communicate and provide care applicable by society to beat depression in elderly patients
Keywords: depression, elderly, professional help, intervention
REFERENCES
1. National Institute of Mental Health. (2019). Older Adults and Depression. https://www.nimh.nih.gov/health/publications/older-adults-anddepression/index.shtml
2. Mayo Clinic. (2021). Depression in Older Adults: Symptoms and Causes. https://www.mayoclinic.org/diseases-conditions/depression/indepth/depression/art-20047725
3. Centers for Disease Control and Prevention. (2021). Physical Activity and Health. https://www.cdc.gov/physicalactivity/basics/older_adults/index.htm
4. World Health Organization. Depression [Internet]. Geneva: World Health Organization; 2022 Available from: https://www.who.int/news-room/factsheets/detail/depression
5. World Health Organization. Mental Health of Older Adults [Internet]. Geneva: World Health Organization; 2022. Available from: https://www.who.int/newsroom/fact-sheets/detail/mental-health-of-older-adults

SARCOPENIA:AVOIDWHEELCHAIRBYBEINGACTIVE
Background
Sarcopeniaisanon-communicablediseasewhichischaracterizedbylossofmusclemass, strength,andfunctionthatoccursfrequentlyamongtheelderly.Arecentmetaanalysisfound that1–3inevery10individualsaged60andaboveexhibitsymptomsofsarcopenia.Toacertain extent,thisconditionhasimplicationsnotonlyfortheindividual,butalsoforsocietyasawhole. Symptomsofgeriatricsyndrome,suchasfrailty,falls,andanincreasedriskoffracture,are associatedwithsarcopenia.Hence,seniorssufferingwithsarcopeniawilltendtoexperiencea declineinmobility,reducingtheirabilitytoperformdailyactivitiesindependently.Thisinturn willcauseadecreaseinoverallsocietalproductivity.
Objectives
Tointroduceandraiseawarenessregardingsarcopenia,includingitsprevalence,implications, andmethodofprevention,inanefforttominimizeitsoccurrenceasacommonhealthissue.
Keywords: sarcopenia, exercise,geriatric,active

Parkinson’sDisease:ATrapforOlderAdults
Background: AccordingtotheWorldHealthOrganization,Parkinson’sDisease(PD)isa leadingneurologicalcauseofdisabilityanddeath.TheprevalenceofPDhasdoubledover25 years;whatwouldbecomeofthefuture?TheclinicalfeaturesofPDarefatal: tremoror shakinginonesideofthebodywhenresting, rigidityorstiffnessofmuscle, abnormal slowingofmovement, posturalinstability(commonlyabbreviated“TRAP”;simplifiedfor public)andothernonmotorsymptomsthatdecreasequalityoflife(QoL).Moreover,thereis nocureforPD–treatmentsonlyrelievesomesymptoms.Eventually,peoplewithPDare limitedfromdailyactivitiesandparticipation,whichmayleadtomentalillness,functional decline,andevendeath.Hence,itisessentialforthepublictorescueolderadultsfrombeing trappedinPD.
Objectives:
● ToraisepublicawarenessonPDurgencyandsigns&symptoms(simplified“TRAP”) inolderadults.
● TocreateanintegratedcareforPDinolderadultsthroughacatchyandrelevant mnemonic:
○ Recognizeandtrackthesymptoms.
○ Exerciseordophysicaltherapy.
○ Seeaspecialist.
○ Chooseasuitablediet.
○ Utilizecareandsupportservices.
○ Engagewithfamilyandfriends.
● ToincreasethequalityoflifeofolderadultswithPD.
Keywords: Parkinson’sDisease,olderadults,integratedcare

OlderAdultsAreAbletoStandStable
Background: AccordingtotheWorldHealthOrganization,fallingisaleadingcauseof accidentalinjurydeathsworldwide.Fallingcausesmoredisabilitythanallothercauses combined(transportinjuries,drowning,burns,andpoisoning).Inolderadults,thehealth consequencesandfinancialcostsoffallsarerisinggloballyduetodecreasedstrength,vision, balance,andconsciousness.TheIntegratedCareForOlderPeople(ICOPE) guidelinereveals thatoneinthreeolderadultsaged65andaboveworldwidefallseachyear,inwhichmany fallrepeatedly–fallingoncedoublesthechancesoffallingagain.Moreover,thepublictends tofalselybelievefallingisanormalpartofagingandremainsinevitable,whileinreality, olderadultsareabletostandstableifthepublicimplementslong-termcare.
Objectives:
1.Toraisepublicawarenessonfallsurgencyinolderadults.
2.Toengagethepublicincreatinglong-termcare(ICOPE-based)forfallsinolder adultsthroughacatchyandrelevantmnemonic:
● Seeadoctorandfollowtheassessment.
● TakevitaminDsupplements.
● Askadoctorformedicationreview.
● Buildasafeage-friendlyenvironment.
● Let’swearsensiblefootwearandeyewear.
● Exercisetoimprovemultiplephysicalaspects.
3.Todecreasetheincidenceoffallsinolderadultsinthefuture.
Keywords: falls,olderadults,long-termcare
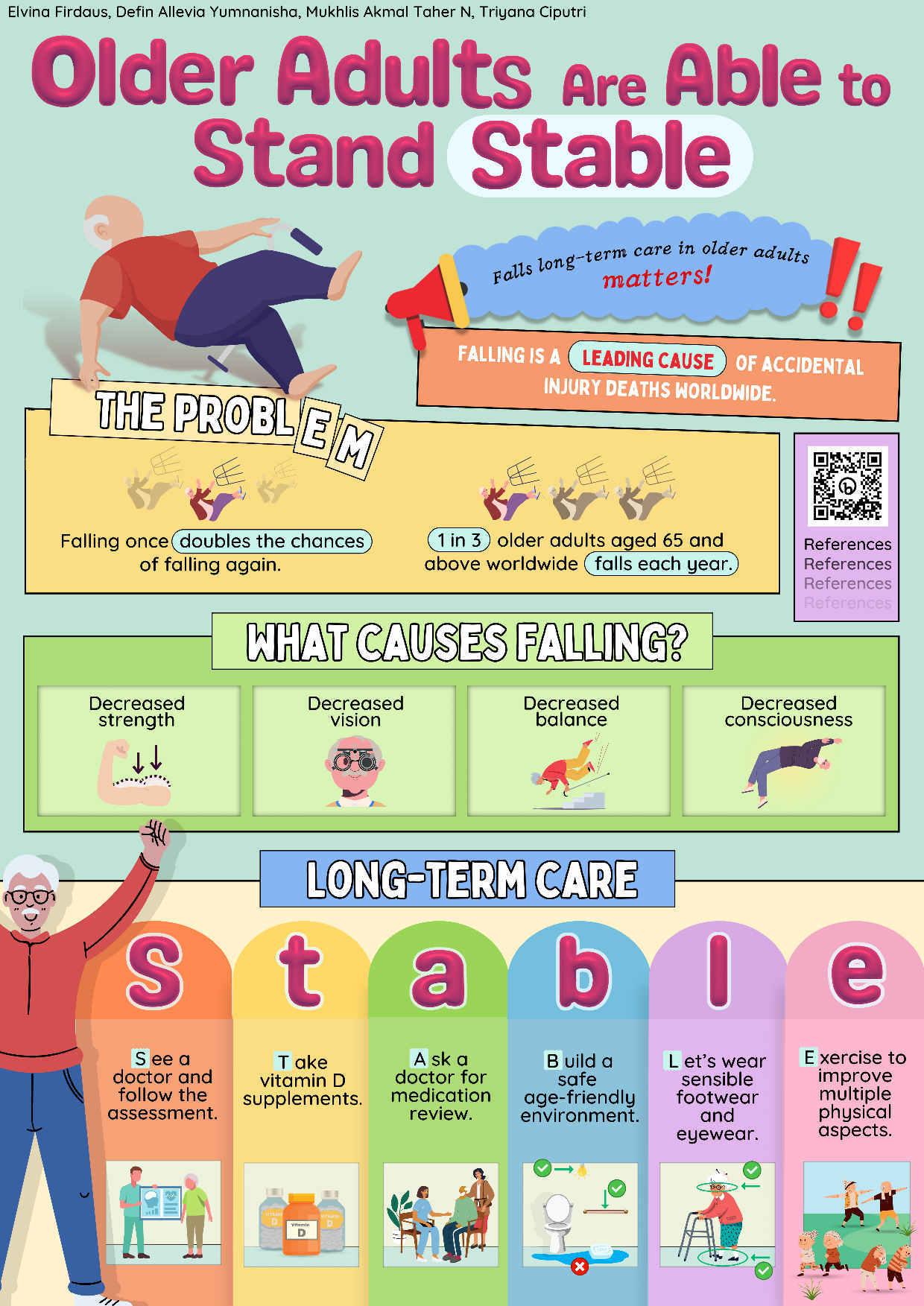
OH,SNAP!LET’SBEACTIVETOPREVENTOSTEOPOROSIS
Osteoporosishasaffectedover200millionpeopleworldwide,andit’sknowntobea“silent disease”sinceitdoesn’tshowanysymptomsuntilaboneisbroken.Theriskfactorsfor osteoporosisaredividedintonon-modifiableandmodifiable.Modifiableriskfactorsincludeage, gender,andfamilyhistory.Basedonworldwidestatistics1in3womenand1in5menagedover 50willexperienceosteoporoticfractureswithmorethan8.9millionfracturecasesannually. Whilethenon-modifiableriskfactorsincludesmoking,nutrientdeficiency,alcoholintakeand physicalinactivity.
Thehighnumberofosteoporosiscasesandthefactthatitoftenoccurswithoutanysymptoms leadsustocreateapublicpostertoraisethepublic’sawarenesstowardsosteoporosis.Moreover, thefactthattherearesomeriskfactorsofosteoporosisthatcanbemodifiedleadsustocreatethe acronym“SNAP”thatthepubliccanremembereasily.Sincemostoftheriskfactorsare modifiable,wecreatedtheacronym“ACTIVE”toinformthepubliconhowtoprevent osteoporosis.
Inconclusion,theconcerningprevalenceofosteoporosisleadsustocreateourpostercontaining theprevalence,riskfactors,andpreventionofosteoporosis.
Keywords: Osteoporosis,Prevention,Riskfactors,Bonemass,Fracture

DERRICK RIZKY AYUNGGA ELSAFIRA RANA RINANDA KARTIKA TAUFANI SUKARNO NI NYOMAN TRIANA WIDHIASTUTI
CONQUERTHEGAMEANDGAINBALANCEWITHEXERGAMING
Introduction: Fallsareoneofthecommonaccidentsthatmostgeriatricsexperienced.Almost 684.000fallshappeneveryyearandabout30-50%offallsresultinminorinjury,while10% resultinmajorinjury.Conventionaltherapiesareavailable,yettheycannotyieldmaximum benefitsinpreventingfalls.However,exergaming,anoveltechnology,isbelievedtoimprove balance,thuspreventingfallsingeriatrics.
Objective: Toraiseawarenesstopublic,especiallygeriatrics,aboutnoveltechnologyfor improvingbalanceandpreventingfalls
Keywords: Exergaming,Falls,Balance
CONQUER THE CONQUER THE CONQUER THE GAME GAME GAME AND AND AND
CONQUER THE CONQUER THE CONQUER THE GAME GAME GAME AND AND AND






GAIN GAIN GAIN BALANCE BALANCE BALANCE WITH WITH WITH EXERGAMING EXERGAMING EXERGAMING
GAIN GAIN GAIN BALANCE BALANCE BALANCE WITH WITH WITH EXERGAMING EXERGAMING EXERGAMING
FALLS WERE NOTED TO BE THE SECOND LEADING CAUSE OF DEATH DUE TO UNINTENTIONAL INJURIES. ACCORDING TO WHO, 684000 FATAL FALLS OCCUR THIS YEAR, AND 60% WAS ACCOUNTED IN SOUTH EAST ASIA
EXERGAMING? EXERGAMING?
TECHNOLOGY-DRIVEN PHYSICAL ACTIVITIES, SUCH AS VIDEO GAME PLAY, THAT REQUIRES PARTICIPANTS TO BE PHYSICALLY ACTIVE OR EXERCISE IN ORDER TO PLAY THE GAME
GAIN YOUR BALANCE GAIN YOUR BALANCE

TRAU A INJURY M M G GAIT IMPAIRMENT A AR OF FALLING FE EEYE IMPAIRMENTS E NARROW FALL RISK LIFESTYLE ACTIVE AND OOSTB YOUR MOOD COORDINATION EXERCISE
DID YOU KNOW?
CONQUER THE GAME THAT REPRESENTS RISK FACTORS
HTTPS://BIT.LY/REFERENCESGAMEBALANCE SCAN ME! REFERENCES
RAISSA MADALINADEWI HUAWE, HASNA LABIBA PANGESTU, TERESA ALMADITA, YEHEZKIAL GIAN PRADIPTA PAHU
CAREGIVER: EVEN A DEMENTIA CAREGIVER NEEDS TO BE CARED
Background
Dementiaisratherageneralterm fortheimpaired abilitytoremember,think,ormakedecisions that interferes with doing daily activities, especially in elders. Patients with dementia have symptoms such as memory loss, difficulty in concentrating, converse, and doing simple tasks, and also will develop mood swings. By 2030, the predicted number of people living with dementia worldwide is estimated at reaching 75.63 million, and its incidence increased exponentially with increasing age.
Objective
Patients with dementia will need someone to take care of them or a caregiver to help them function in their daily life. Sadly, there is a risk of burden being a dementia patients’ caregiver. It may represent lack of social interaction, emotional exhaustion, sleep disturbance, and other medical problems. Yoga therapy can relieve the burden of being a caregiver.
Keywords: dementia, degenerative, geriatric, caregiver, burden

AMessagetoTheSociety:Alzheimer'sDiseasePatientsMATTERforUs!
Alzheimer'sdisease(AD)isastateofprogressivecognitiveandfunctionaldecline characterizedbyabraindisorderthatgraduallyimpairsmemoryandthinking skillsand,atlast,theabilitytocarryoutdailytasks.Elderly Asianpeopleaccount for1in10cases.AsAlzheimer’scasesclimb,expertsprojecttheconditionwill tripleamongAsiansby2030. ADcausesmedicalandpsychological manifestationsincludingpersonalitychanges,memoryloss,hallucinations,and delusionsduetobraindamage.Patientsmayalsobecomecompletelydependent oncaregiversandexperienceseverebrainfunctionlossleadingtodehydration, malnutrition,andinfection,ultimatelyresultingindeath.Community-based supportactionsarerequiredastheoptimalinterventionstoaddressthehigh incidenceofADandtheseverityoftherisksthatmayaffectitspatients.These actionsshouldstrivetoestablishaninterprofessionalcommunityforADpatients toprovideholistic,long-term,andcost-effectiveservices.Community-based supportactionsrequireaspectsof“MATTER”consistingof“Medicate”, “Accompany”,“Talk”,“Train”,“Excurse”,and“ReconcileandRestore”which areabletoimprovethequalityoflifeofADpatientsandtheirfamilies.
Keywords: Alzheimer’sdisease,Intervention,Community-basedsupport
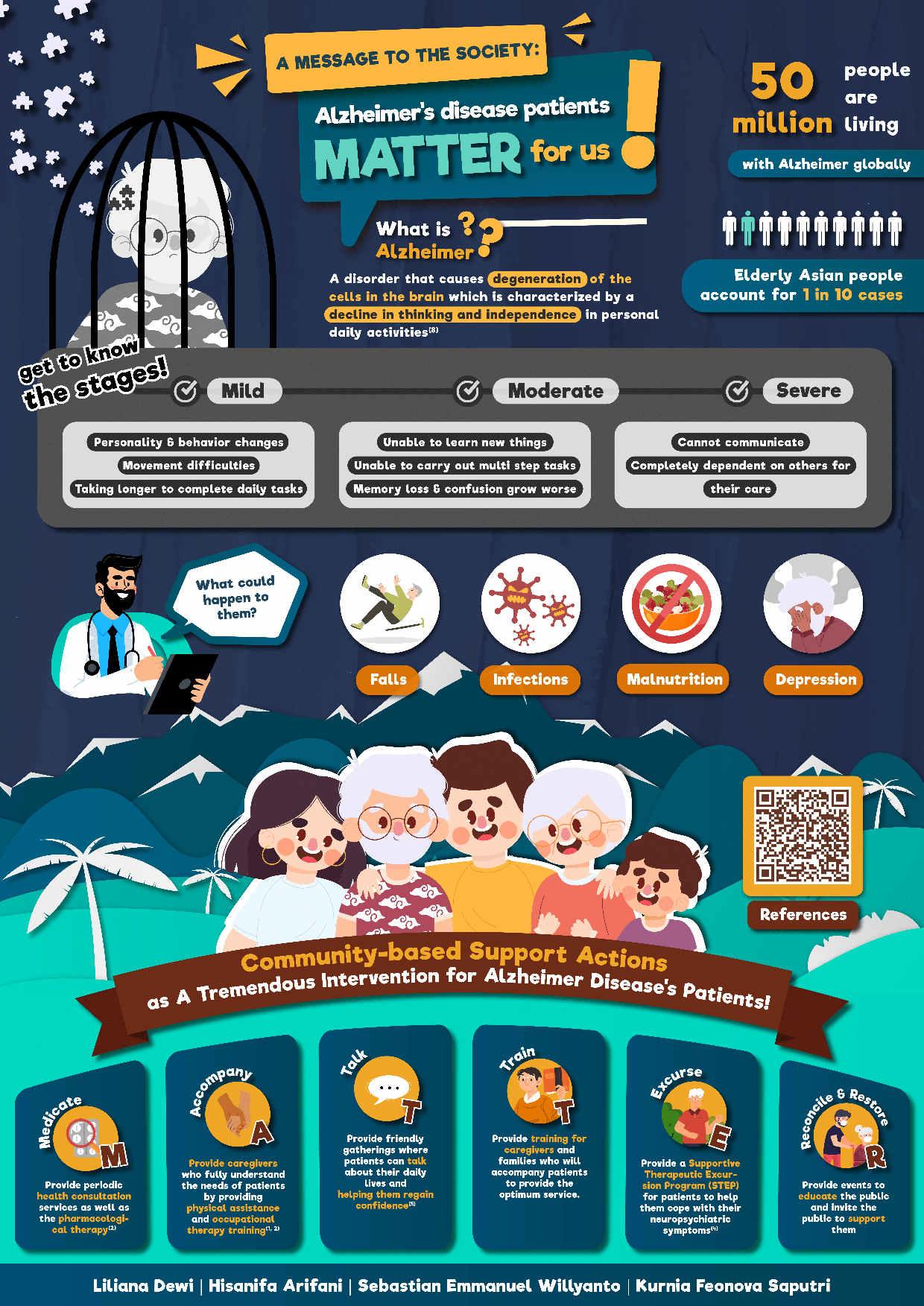
Dementia:M.I.N.D.StheSigns,TreatswithM.E.M.O.R.Y
Introduction/Background:Dementiaisadebilitatingconditionthataffectsmillionsofpeople worldwide.Itisaprogressivedisorderthatcausesadeclineincognitivefunctionand memory,makingitdifficultforindividualstocarryouteverydaytasks.Treatingpeoplewith dementiaisessential,asithelpstoslowdowntheprogressionofthediseaseandimproves thequalityoflifeforboththeindividualandtheircaregivers.Dementiacanbetreatedina varietyofways,includingmedication,therapy,andlifestylechanges.However,itiscrucialto understandthatthereisnocurefordementia,andtreatmentfocusesonmanagingsymptoms andimprovingoverallhealth.Despitetheimportanceoftreatingdementia,manyindividuals withtheconditionarenotreceivingtheappropriatecaretheyneed.Thisissueisparticularly prevalentinIndonesia,whereitisestimatedthatonly10%ofpeoplewithdementiareceive adequatetreatment.Globally,thisnumberisevenmoreconcerning,withonlyaround50%of peoplewithdementiareceivingadiagnosis,andonlyafractionofthemreceivingappropriate treatment.
Objectives:Raiseawarenessabouttheimportanceoftreatingpeoplewithdementiaand provideinformationonhowtotreatthemtoimprovetheirqualityoflife.
Keywords: Dementia,Treatment,Geriatric,Awareness,QualityofLife
References:
1.WorldHealthOrganization.DementiaFactSheet.2021.[cited2023Apr9].Available from: https://www.who.int/news-room/fact-sheets/detail/dementia
2.ArvanitakisZ,ShahRC,BennettDA.DiagnosisandManagementofDementia: Review.JAMA.2019Oct22;322(16):1589-1599.
3.GottesmanRT,SternY.Behavioralandpsychiatricsymptomsofdementiaandrateof declineinAlzheimer'sdisease.FrontPharmacol.2019;10:1062.
4.ParkK,LeeS,YangJ,SongT,HongGRS.Asystematicreviewandmeta-analysison theeffectofreminiscencetherapyforpeoplewithdementia.IntPsychogeriatr.2019 Nov;31(11):1581-1597.
5.ShajiKS,SivakumarPT,RaoGP,PaulN.ClinicalPracticeGuidelinesfor ManagementofDementia.IndianJPsychiatry.2018Feb;60(Suppl3):S312-S328.
















DEMENTIA? M.I.N.D.S The Signs! Treats With M.E.M.O.R.Y What is Dementia? Overall decline in memory and other cognitive skills severe enough to reduce a person's ability to perform everyday activities. Did You Know? 55 Million Only half of people with dementia have been diagnosed Receive Appropriate Treatment and Care. Only 10-25% People Have Dementia Worldwide 50% Memory Issues Impaired Mood Disrupted Visuospatial Perception Notable Concentration Difficulties Struggles With Problem Solving Manage their environment to reduce potential hazards and create a calming atmosphere Engage in meaningful activities and social interaction to stimulate cognitive function Maintain a routine for daily activities to provide structure and reduce confusion Offer simple choices to promote independence and autonomy Reminisce about their past experiences to promote feelings of familiarity and connectedness Yield to their emotions and validate their feelings to build trust and promote a positive relationship M.I.N.D.S the Signs Treat With M.E.M.O.R.Y MIINNDDS S MMORYE Scan This QR-Code for Further Information
HAPPILY AGING WITH HEALTHY JOINT
Background
As peopleage,matrix that makes up jointsin themusculoskeletal systemwilldegenerateand cause diseases, one of which is osteoarthritis. Osteoarthritis is an age-related disease described as progressive breakdown of joint cartilage caused by combination of mechanical stress and individual risk factors. Osteoarthritis is the most common joint disorder worldwide and one of the main cause of pain and disability among geriatric population. The incidence of osteoarthritis keep rising due to the aging of the population and increasing average population weight as one of the main risk factor for osteoarthritis. Among people with osteoarthritis, 43% of them are at the age of 65 or older and 88% are 45 or older, with incidence is highest between 55 and 64 years old.
Objective
Although osteoarthritis isn’t fully preventable, there are ways to minimize the risk of getting it or slow its progression by avoiding injury, living a healthy lifestyle, and doing a routine check-up. Hence, this poster is aimed to promote those ways in a quick and optimal manner. By reading this poster, we hope people, especially the older generation, could be more aware about osteoarthritis and thereby the risk of getting pain and disability from osteoarthritis could be minimized.
Keywords: degenerative, geriatric, osteoarthritis, prevention, progressive
HAPPILY HAPPILY AGING AGING WITH HEALTHY JOINT WITH HEALTHY JOINT
osteoarthritis (OA) osteoarthritis (OA)
is a progressive disease characterised by damage of the joint cartilage between the bones. It is caused by combination of mechanical stress and individual risk factors that gradually breakdown the joint cartilage
Osteoarthritis affects up to 3.6%of the population worldwide and causes moderate to severe disability among 43 million people, especially in theelderly

oasymptoms oasymptoms
Joint pain
Stiffness


Motion restriction
Bony swelling
Joint deformity
Crepitus
Do You Know? Do You Know?
As people age, minerals that makes up joints will degenerate and cause diseases, such as osteoarthritis
OA Risk OA Risk Factors Factors
Elderly Women
Obesity
Joint injury Genetics
Unhealthy lifestyle
a a ii n n g g g g
Avoidjoint injuries from activities with excess weights
Gettheideal bodyweight by consuming healthy diets
Improve endurance andmuscle strength with aerobic exercises
Noticethe symptoms andrisk factors of osteoarthritis
Gotodoctor for screening and full examination

Let's minimize the risk of getting osteoarthritis
Let's minimize the risk of getting osteoarthriti
with
s with
scan here for more info:
Authors: SamuelBobbyC,AllafiaS,SadamAthaE,PutriMahiraS
MANAGE INSOMNIA WITH “CARE” (CBT-I, APPLYING RELAXATION TECHNIQUES, REGULARLY IMPLEMENTING SLEEP HYGIENE, and EMPHASIZING the IMPORTANCE of FAMILY ROLE)
ABSTRACT
Insomnia can be defined as dissatisfaction with sleep either qualitatively or quantitatively Insomnia is the most common sleep disorder that is encountered in geriatric population. Globally, the prevalence of insomnia ranged from 17% to 60% and was much higher in females, ranging from 41.5% to 74.8%. Insomnia has been proven affects the quality of life in elder people but often undertreated.
This poster is aimed to raise people knowledge about how to manage INSOMNIA in elder people with CARE. The word INSOMNIA stands for its symptoms. The elders who suffered from insomnia would have an increase number of errors and accidents, not being able to focus, feeling sleepy at daytime, and often feels tired. Besides that, they would have many worries about sleep, not being able to go back to sleep, easily irritated, and experiencing alteration of sleeping schedule. On the other hand, the word CARE stands for using CBT-I to track sleeping habits, applying relaxation techniques, regularly implementing sleep hygiene, and emphasizing the importance of family role
We hope through this poster, especially those who have elder people at home, would have more awareness and knowledge on how to manage age-related insomnia.
Keyword: Geriatric, CBT-I, Insomnia

GET TO KNOW MORE ABOUT DEMENTIA ABSTRACT
Background:
Dementia is a term for several diseases that affect memory, thinking, and the ability to perform daily activities. It mainly affects older people, but not all people will get it as they age. According to the World Health Organization, now more than 55 million people suffer from dementia worldwide, and every year there are almost 10 million new cases.
Objective:
The purpose of this poster is to increase public awareness about dementia in general so people can recognize it through its symptoms, understand the risk factors that can cause it, and know how to prevent it.
In this poster, we emphasize the importance of preventing dementia by practicing "YOUTH". "YOUTH" stands for:
● Your mind, body, and social life must be active.
● Oversee your dietary habits and get your vitamins.
● Understand your sleep cycle and implement it.
● Treating your body's condition, especially your hearing.
● Halt your smoking and drinking behavior.
With the publication of this poster, we are attempting to increase the public's awareness of dementia, improve knowledge of the disease, and educate people on how to avoid it in order to improve their quality of life.
Keyword: Dementia, Geriatric, Prevention

Mind Your Mental Health: Stay SHARP in Your Golden Years!
Background : Mental health is just as important as physical health, especially in older adults. Aging can bring about various changes in life circumstances, including retirement, chronic health conditions, and loss of loved ones, that can impact mental health and well-being.
Objective : We aim to bring awareness about the importance of maintaining our mental health in order to have a better and healthier life. Our mnemonics “SHARP” consists of the steps to do so:
1. Stay active and engaged: Staying active and engaged in activities such as volunteering and social events can help improve mental health.
2. Have a support system: Having a support system of family, friends, or healthcare professionalscanhelpimprovementalhealth.Don'thesitatetoreachoutforhelpwhen needed.
3. Attend to your physical health: Physical health is closely linked to mental health. Eating a healthy diet, getting enough sleep, and engaging in regular exercise helps.
4. Recognize the signs of mental health issues: Depression and anxiety are common in older adults. It's essential to recognize the signs and symptoms of these conditions and seek professional help.
5. Practice self-care: Self-care practices such as engaging in relaxation techniques, spending time doing hobbies, and practicing gratitude.
Keywords : Maintain, Mental health, Older adults.

BANISH ALZHEIMER’S
BY KEEP YOUR MINDSET
Background: Dementia is often considered part of the normal aging process for many when it is not. Based on the World Health Organization (WHO), Alzheimer's disease is the most common type of dementia (60%-70%) that’s suffered by 55 million worldwide. Each year, there are around 10 million new cases of dementia. However, what many do not aware of is that Alzheimer's can be prevented or delayed.
Objective: To spread information on Alzheimer's disease in hopes to help reduce its prevalence by increasing public awareness of Alzheimer's disease.
Description: Alzheimer's caused by the death of cells in the brain, causing memory loss and decreased cognitive ability. Meanwhile, the symptoms of Alzheimer’s are memory loss, difficulty completing daily tasks, confusion with time and place, misplacing things, andchanges in mood and personality. Therefore, this poster presents MINDSET to banish Alzheimer’s disease.
Impact: Based on the Alzheimer's Association International Conference 2021, decent health promotion on Alzheimer's may help reduce dementia rates by 6.2 million cases in 2050. One of the efficient ways to this approach is by spreading public posters about Alzheimer's disease.
Conclusion: Decent knowledgeandawarenessthroughcontinuinghealthpromotionmayhelpprevent and delay Alzheimer's later.
Keywords: Alzheimer's disease, Dementia, prevention, health promotion, public poster
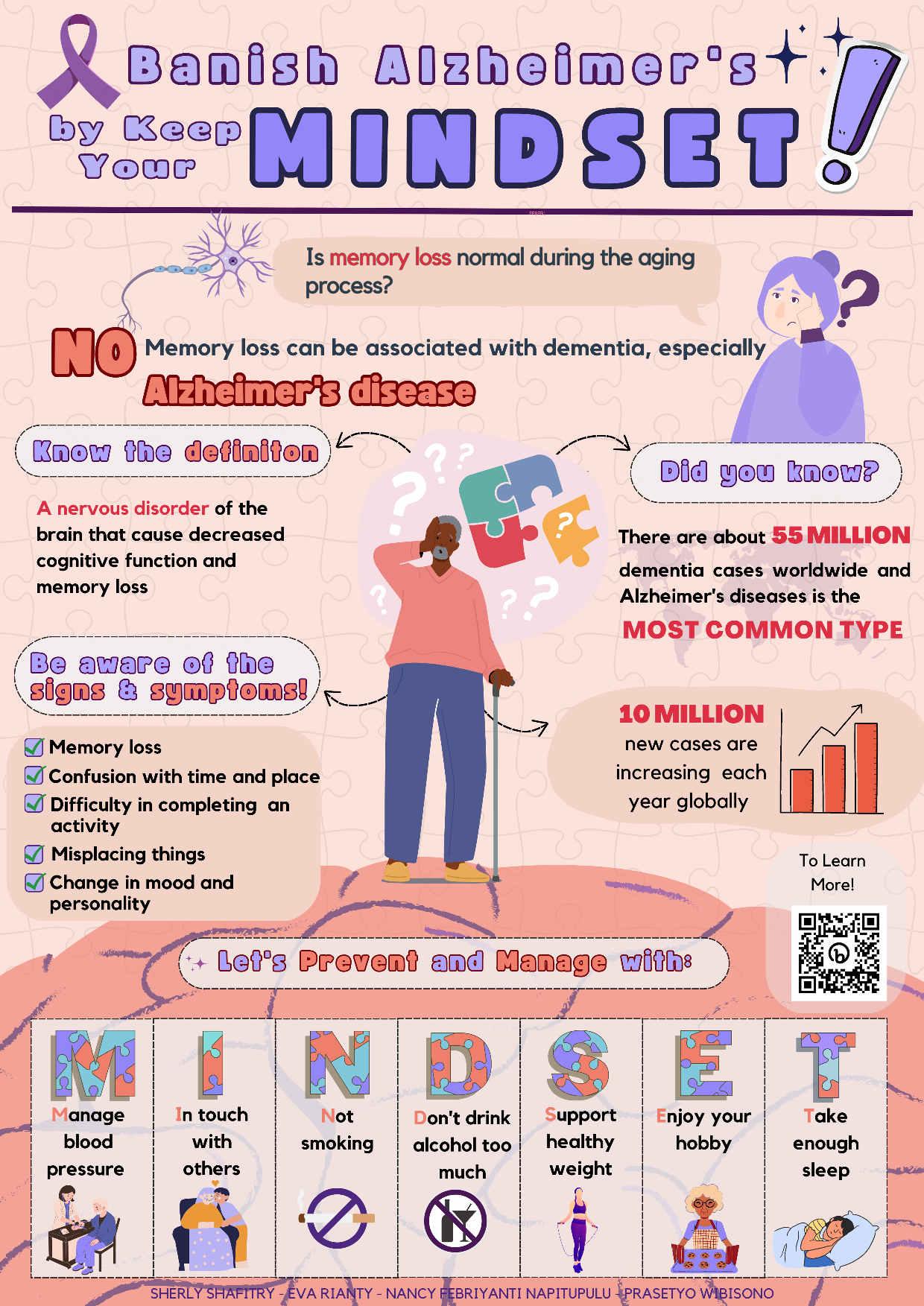
Remember MEMORY to Prevent Alzheimer
Background :
Alzheimer’sdiseaseisabraindisorderthatslowlydestroysmemoryandthinkingskills.Theglobal prevalence of this disease has been estimated as high as 44 million. If it remains untreated, this disease could eventually disrupt someone’s ability to carry out the simplest tasks, such as responding to verbal requests. That’s why we need to prevent Alzheimer in elderly people.
Objective :
To make society, especially the elderly people and their caregivers know more about Alzheimer, mainly about its prevention and symptoms.
Description of Poster :
First of all, we include the definition of Alzheimer's disease to make sure the reader of our poster knows what Alzheimer is. Then, there is the prevalence of Alzheimer and how the disease changes the brain's appearances to make the reader more aware about this disease. We also include early signs of Alzheimer so that the reader knows whether they might have Alzheimer or not. Lastly, the most important one is things that we can do to prevent Alzheimer. In this poster, we use purple as the theme color because it’s identical to Alzheimer and some puzzle pieces that are falling apart. Those puzzle pieces represent the memory of people with Alzheimer that are starting to fade.
Keyword : Alzheimer, Elderly, Memory, Prevention

Introduction: Integrated Care for Older People (ICOPE) is WHO's guidance for health care professionals to address the declining physical and mental capabilities of geriatrics, adopting an integrated, person-centred approach. Several geriatric problems and recommended approach are informed in ICOPE module 1, include visual impairment. Globally, at least 2,2 billion people have impaired near or distant vision. The majority of people with vision impairment and blindness are over the age of 50. Therefore, older people should be screened regularly for visual impairment in primary care and receive timely comprehensive eye care. The title of this poster is “Manage A Long Term Care of Visual Impairment in Geriatric with A MATRIC”. A MATRIC stands for Ask the visual problems, MAnage the visual impairments, TReat the associated conditions Ideally, Create a suitable environment. Comic pixel design, tiny square shape pixels with cartoonish and retro vibe in it, is applied in this poster. This design can evoke sense of nostalgia and playful. It help the audience to understand long term care based on ICOPE guideline.
Objective: To enhance the knowledge about how to prevent, slow or reverse declines in visual impairment aspect based on ICOPE guidelines and resulting improvement in quality of life.
Keywords: ICOPE, Geriatric, Long term care, Preventive, Rehabilitative

Let’sFindanANCIENTWaytoFightDementia
Introduction: Dementiaisasyndromecharacterizedbythecognitivedeclineandimpairment. AccordingtotheWorldHealthOrganizationin2023,morethan55millionpeoplehave dementiaworldwide.Everyyear,therearenearly10millionnewcases.Dementiaisoneofthe majorcausesofdisabilityanddependencyamonggeriatricglobally.Researchsuggeststhat physicalandemotionalhealthishighlyimportanttopreventtheearlyonsetofdementia.
Objective: ToenhancepublicawarenessaboutdementiaandfindanANCIENTwaytofightit.
Description: OurposterisinspiredbythethemeANCIENT.Itisalsomatchwithour mnemonic“ANCIENT”tofightdementiawhichis Aerobicexercise, Nutritionalandhealthy diet, Cognitiveexercise, Intellectualactivities, Engageonsocialinteraction, Notobaccouse, Treatcardiovascularriskfactors.
Impact: Byfirstglance,wehopethispostercanraisepublicawareness.Ifpeoplehavethewill anddothehealthylifestylesincenow,theprevalenceofdementiacanbehighlyreduce.
Conclusion: Dementiaisanacquiredlossofcognitioninmultiplecognitivedomainsthat severelyaffectsocialoroccupationalfunction.Wehopeourpostercanhelpeducatethepublic andfightdementiainanANCIENTwayandresultinginahigherqualityoflife.
Keywords: Prevention,Dementia,Geriatric
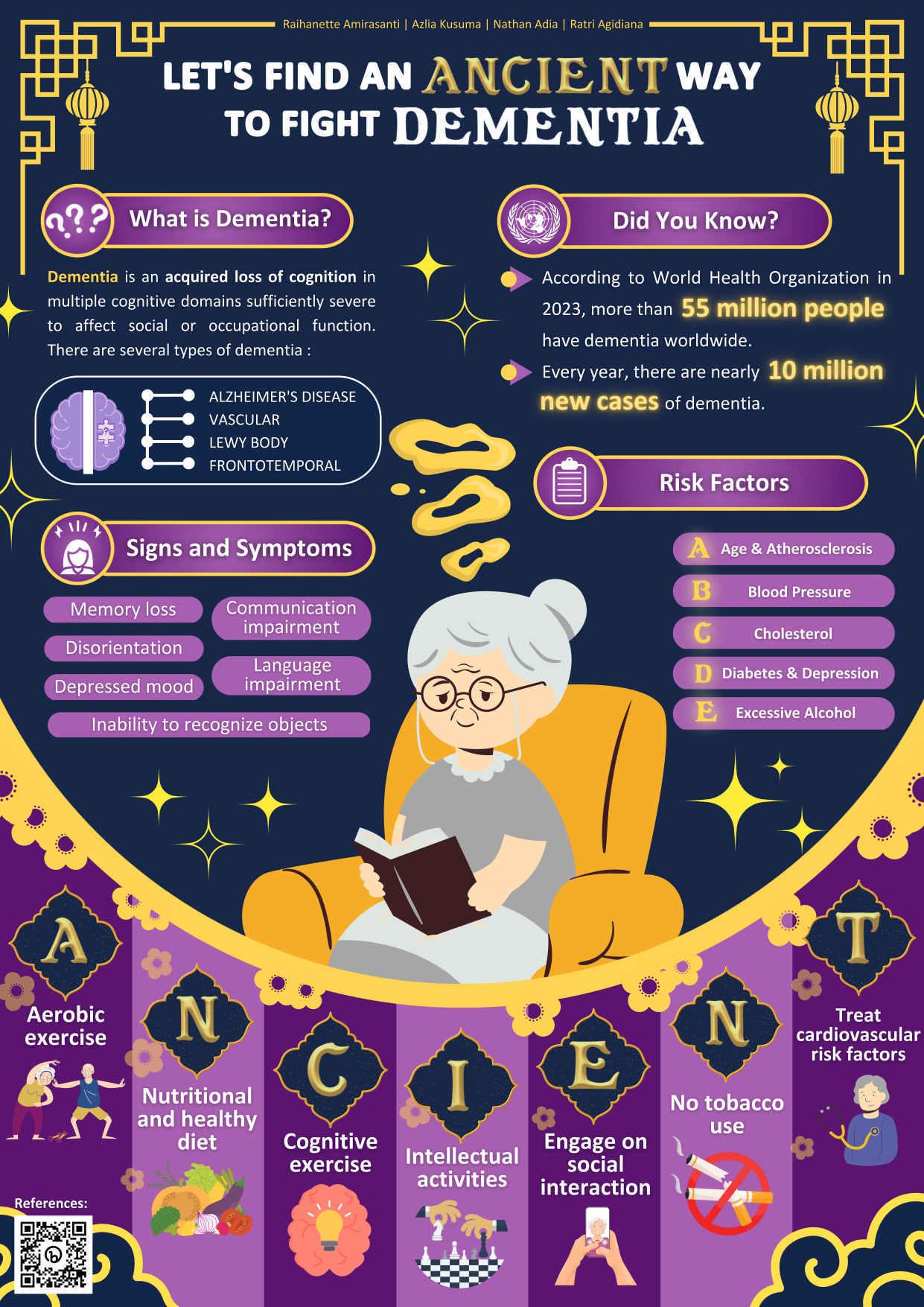
Abstract
Background/Introduction
Geriatricmedicineneedsamultidisciplinaryapproachinsomanyaspects.Througheffective communicationamongpatientsandcaregivers,optimalresultswouldbeabletobeachieved whentryingtoreducepatientsymptomsfromcertaindiseases.Webelievethat patient-centredapproachesingeriatricmedicineisoneofthebestformsofmedication neededtobedoneforgeriatricpatients.Afternarroweddownthepossiblediseasesthat’s mostcommonforgeriatricpatients,wedecidedtorollwithParkinson’sDisease.Itisknown thatParkinson’sDiseaseiscommonlyfoundinelderlypeople.Itisalsooneofthemost commonneurodegenerativedisorders,henceitiscrucialthatweapplythesepatient centred-approachestofurtherenhancethepossibilityofrecoveryforthesepatients.
Objective
Publicposter“We’retheChangerforParkinsonSurvivor”aimstoachievebetterandmore effectivemultidisciplinarypatient-centredcareapproachinordertooptimiseknowledgeand therapiesinaprogressivediseasesuchasParkinson’sDisease,especiallyinelderlypeople. Byapplyingthe“CHANGER”approach,ourhopeistohelpcliniciansandfamiliestochange thewayelderlypatientsaretreatedtosurvivefromParkinsondiseaseanditscomplicationsin aclearandsimpleway.
Keywords
parkinson’sdisease,geriatriccare,patient-centredcare

LET’S COUNTER OBESITY IN THE ELDERLY WITH TROPIC
Background : Obesity are defined as abnormal or excessive fat accumulation that presents a risk to health. It’s a complex disease involving an excessive amount of body fat. Obesity isn't just a cosmetic concern. It's a medical problem that increases the risk of other diseases and health problems, such as heart disease, diabetes, high blood pressure and certain cancers. Then, categories of obese can be defined as BMI ≥ 30 kg/m2 regardless of age range. The prevalence of central obesity at the national level for the elderly is 18.8% which was recorded from the age group 55-64 years 23.1%, 65-74 years 18.9%, and >75 years 15.8%.
Objective : To increase awareness and prevention of obesity in the elderly. Then, to know about the definition, complications and risk factors for all readers especially elderly about obesity so they can implement Tropic programs to prevent obesity in the elderly.
Keywords : Obesity, Elderly, Preventive
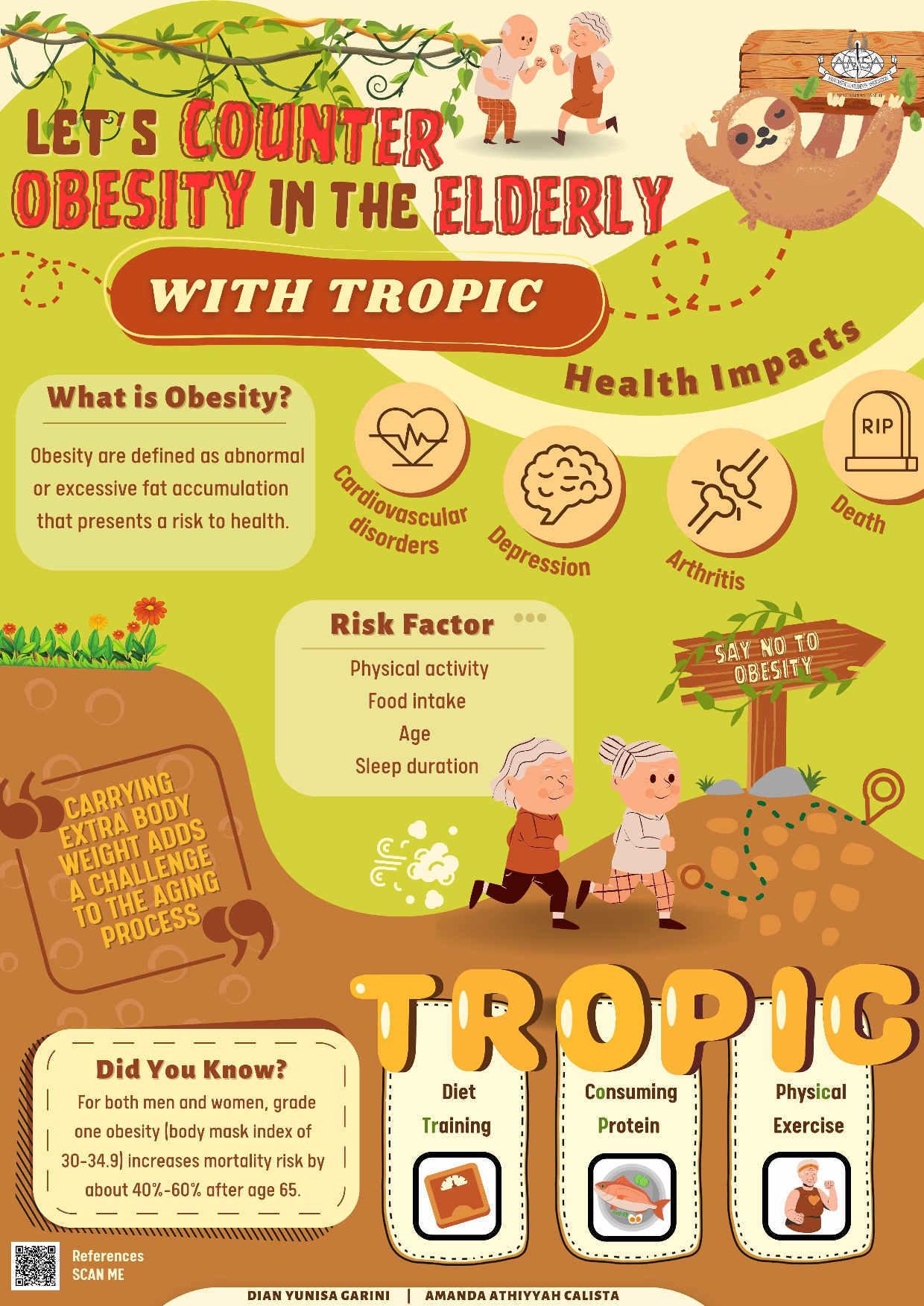
ALZHEIMER’SDISEASEandWHYSHOULDWECAREaboutTHEM
Alzheimer'sisaneurodegenerativediseaseintheelderlypopulationworldwide.Theimpact ofAlzheimer'sdiseaseistremendous.Alzheimer'spatientsexperiencedecreasedcognitive functionandabilitytododailyactivities,thus,requiringintensivecareandsupportfromtheir families.Therefore,itneedsconcernforsociety.InIndonesia,theelderlypopulationis projectedtoreach28millionor10.5%ofthetotalpopulationin2021.Hence,Alzheimer’s patientsareestimatedtoriseaboutfourtimesby2050.
ThegrowingelderlypopulationleadstomorecasesofAlzheimer'sdisease,highlightingthe needforsupportandcare.Neglectingtoprovideadequatecarecouldworsenthedisease's progression.Toenhancethequalityoflife,itisessentialtodecreasetheprevalenceof Alzheimer's'latestage'indications,suchasmaintaininggoodphysicalandmentalhealth throughregularexercise,healthydiet,andstressreduction.
Therefore,ourposterfocusesonthestagesofAlzheimer'sdiseaseandsolutionstoreduceits riskwitheasy-to-understandpicturesandwords.Theaimistoraiseawarenessofthe importanceofearlydetectionandstepstoreducetheriskofAlzheimer'sdisease.Jointefforts areexpectedtoimprovethequalityoflifeofgeriatricsworldwidebyreducingtheimpactof Alzheimer'sdisease.
Keywords:Alzheimer,qualityoflife,care,health,awareness

Abstract
Introduction/Background : Osteoarthritis is a degenerative joint disease that limits the body part movements such as the knee. The incidence of symptomatic knee osteoarthritis is roughly 240 cases per 100,000 people per year. This number rises as high as 40% among people who are older than 70 years old. There are several signs and symptoms of OA including pain, stiffness, swelling, and decreased range of motion (ROM). Thus, serious treatments such as drugs, surgery, and exercises are needed. Aquatic exercises are beneficial for older patients with OA. The waves and buoyancy of water support the weight of the body, reducing the impacts on joints and the intensity of continuous pain. Furthermore, this treatment will relieve stress, reduce stiffness, and increase muscle strength for better prognosis. In conclusion, aquatic exercise can be the initial treatment for OA patients in the future. Therefore, we came up with SPLASH as a breakthrough intervention for OA patients.
Objective : This poster aims to improve public education and become a healthcare intervention promotion of OA through public posters.
Keywords : Aquatic exercises, Osteoarthritis, Pain.
REFERENCES
1. UW Medicine Orthopaedics and Sport Medicine. Water Exercises Pool and Arthritis.
2. CDC. Osteoarthritis (OA). Centers for Disease Control and Prevention. 2020.
3. Lu M, Su Y, Zhang Y, Zhang Z, Wang W, He Z, et al. Effectiveness of aquatic exercise for treatment of knee osteoarthritis. Z Rheumatol. 2015 Aug 19;74(6):543–52.
4. Dong R, Wu Y, Xu S, Zhang L, Ying J, Jin H, et al. Is aquatic exercise more effective than land-based exercise for knee osteoarthritis? Medicine. 2018 Dec;97(52):e13823.
5. Song JA, Oh JW. Effects of Aquatic Exercises for Patients with Osteoarthritis: Systematic Review with Meta-Analysis. Healthcare. 2022 Mar 16;10(3):560.
Osteoarthritis
Osteoarthritis

degenerative joint disease that limits the body part movement, such as the knee.
degenerative joint disease that limits the body part movement, such as the knee.
AQUATIC EXERCISE

Aquatic exercise is a treatment that uses waves and buoyancy of water to
support the weight of the body to reduce the impacts on joints and the intensity of continuous pain.
WHY AQUATIC EXERCISE FOR OA?

COMMON STEPS
UBMERGE YOUR LEGS UBMERGE YOUR LEGS S
RISK FACTORS
Older Age
Joint Injury
Gender (Women)
Race (Asians have lower risk)
Family History
INCIDENCE RATE
OSITION KNEE
STRAIGHT OSITION KNEE STRAIGHT P
THE BENEFITS of aquatic exercise
IFT YOUR KNEE TOWARDS CHEST L
IFT YOUR KNEE TOWARDS CHEST
BDUCT YOUR KNEEBDUCT YOUR KNEE A
WITCH TO THE OTHER KNEE WITCH TO THE OTHER KNEE S
H
Release joint stiffness
Release joint stiffness
Prevent further damage
Prevent further damage
Build muscle strength
Build muscle strength
Increase joint movement (Range of Motion)
Increase joint movement (Range of Motion)
Preserve flexibility
Preserve flexibility
AVE REGULAR DOCTOR APPOINTMENT AVE REGULAR DOCTOR APPOINTMENT
Rizqi Hidayatullah - Noura Alisha - Cindy Fayola - Sulthan Alkatiri
REFERENCES
cases
240
per 100.000 people every year
among people older than 70 Water resistance to strengthen muscle & prevent atrophy Water buoyancy lifts joints’ weight & reduce pain
40% higher
PRE-CONFERENCE COMPETITION
ASIAN MEDICAL STUDENTS’ CONFERENCE 2023 : TAIWAN
Geriatrics: Care for the Future
DON’T LET YOUR MUSCLE WEAK, FIGHT SARCOPENIA WITH MOVE!
Background:Sarcopeniais an age-related syndromecharacterized by progressiveand involuntary loss of skeletal muscle mass and strength. According to the database, sarcopenia affects 16% elderly worldwide with a risk of adverse outcomes such as physical disability, poor quality of life, and death.
Objective: We aim to spread awareness and engage the public on how to prevent sarcopenia.
Description: Therefore, we made WEAK and MOVE as the mnemonic to make the public memorize it easily.
WEAK is the mnemonic for sign and symptoms, which stands for:
W → Walk slower
E → Endurance loss to do daily activities
A → Alighting of muscle mass
K → Kinetic imbalance
MOVE is the mnemonic for prevention, which stands for:
M → Muscle strengthening activities
O → Optimization of daily physical activities
V → Visit medical professionals for a routine check-ups
E → Enhance protein, vitamin D, and omega 3 intake
Impact: We hope for a better quality of life in the older society, especially in this era and in the future where life expectancy is predicted to increase in many countries.
Conclusion: Sarcopenia is characterized by geriatric muscle weakness. It can be prevented with long-term care for muscle.
Keywords: Geriatrics, Move, Muscle, Sarcopenia

LET’SREMEMBERTOPREVENTALZHEIMER
Background: Alzheimerisaleadingcausefordementiainthegeriatricpopulationwithan estimatednumberof55.2million.Itisadegenerativebraindiseasethatmainlyimpacts memoryandcognitiveskills,whichcanseverelyimpactthequalityoflife.Moreover,its treatmentisverycostlywithitseconomicburdenbeing$231billionin2022.
TherearelotsoffactorsthatcanincreasetheriskofgettingAlzheimer,mainlypeopleover 65yearsold,sedentarylifestyle,orpeoplewithcomorbiditiessuchashypertensionand diabetesmellituswhichmeansthatmanypeoplearevulnerabletothedisease.
Objective: ToeducateandtoraisetheawarenessofpeopleaboutAlzheimer'sandthe dangeritposes,alsotheimportanceoflivingahealthylifestyletopreventit.Therefore,we createdamnemonic"REMEMBER"whichconsistsofseveralwaystopreventAlzheimer thatstandsfor Readbooksorplaymusicalinstruments, Enhancehealthydiet, Managestress andsleepwell, Evadesmokingandsedentarybehaviour, Meditation, Bloodpressureand bodyweightshouldbemaintainedtonormal, Exercisefrequently,and Regularlydobrain exercise.Withthismnemonic,hopefullymorepeoplewillbeabletoliveahealthierlifestyle foranenjoyablelifeinthefuture.
Keywords : Alzheimer,Dementia,Prevention
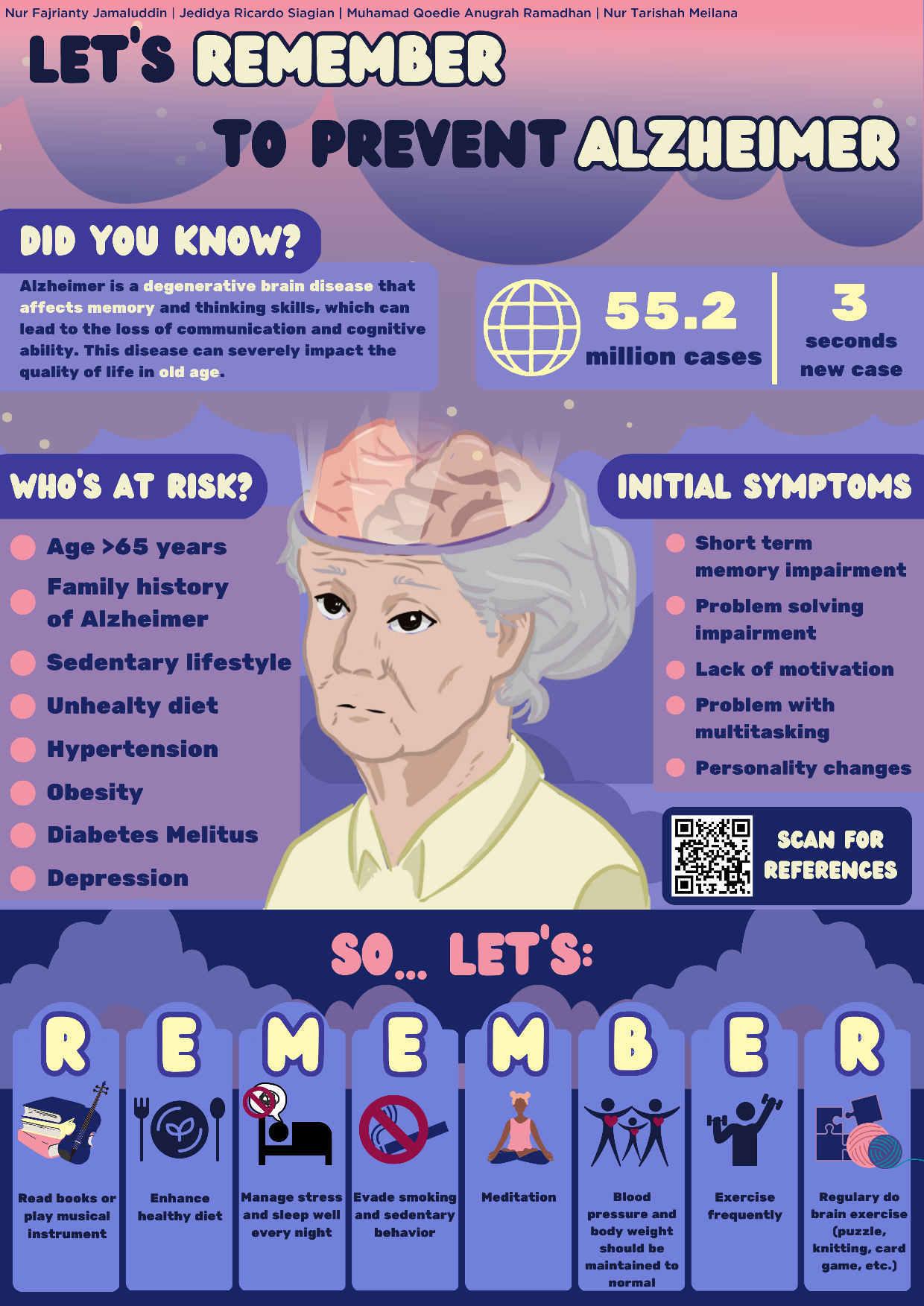 RochelleDeMelloWahyudi,DerrenD.C.H.Rampengan,ArnoldKeane
RochelleDeMelloWahyudi,DerrenD.C.H.Rampengan,ArnoldKeane
Introduction: Age-relatedhearingloss,knownaspresbycusis,isawidespreadissuethat affectsasubstantialnumberofolderadults.AccordingtotheNationalInstituteonDeafness andOtherCommunicationDisorders,disablinghearinglossaffects25%ofthoseaged65-74 and50%ofthoseover75yearsold.1 Thisconditionnotonlyaffectscommunicationbutcan alsoleadtosocialisolation,cognitivedecline,andreducedqualityoflife.2,3 Despiteitshigh prevalence,age-relatedhearinglossoftenreceiveslittleattentionandisneglected,indicating aneedtoincreaseawarenessandunderstandingofthecondition.4 Therefore,itiscrucialto understandtherisksofhearinglossandtakepreventivemeasurestoreducetheimpactof hearinglossontheelderlypopulation'soverallhealthandqualityoflife
Objectives: Toincreaseawarenessandunderstandingofage-relatedhearingloss,particularly invulnerableolderadults,andpromotemeasurestoprotectagainsttheconditionandmitigate itsimpactonhealthandqualityoflife
Description: Toachievethestudyobjectives,weusedthetagline"HEARYourBest:Protect YourHearingHealth!"andcreatedamnemonic,"HEAR,"tomakethemessagemore memorableandeasytorecall.Theacronymstandsfor Haveyourhearingcheckedregularly5 , Engageinear-protectivepractices6 , Assistivedevicesinhearing7,and Regularlycleanyour ears8.Theapproachaimedtoeducatetheelderlyonthedebilitatingconsequencesof age-relatedhearinglossandtopromotepreventivemeasurestheycantaketoprotecttheir hearinghealth.Despitethehighprevalenceofage-relatedhearingloss,thereisalackof publicpostersfocusingonconcise,actionablestepstopreventormanagethecondition.Our studysoughttoaddressthisgapbydevelopinganeasy-to-rememberapproachthatcouldhelp increasepublicknowledgeandawarenessofpresbycusisandpromotepreventivemeasures.
Keyword: presbycusis,geriatric,hearing,age-relatedhearingloss
References
1.NIDCDEpidemiologyandStatisticsProgram.QuickStatisticsAboutHearing [Internet].NIDCD.2021[cited2023Apr12].Availablefrom: https://www.nidcd.nih.gov/health/statistics/quick-statistics-hearing#6
2.DavisA,McMahonCM,Pichora-FullerKM,RussS,LinF,OlusanyaBO,etal. Agingandhearinghealth:thelife-courseapproach.Gerontologist[Internet].2016 Mar18[cited2023Apr13];56(Suppl2):S256–67.Availablefrom: https://academic.oup.com/gerontologist/article/56/Suppl_2/S256/2605334
3.DaltonDS,CruickshanksKJ,KleinBEK,KleinR,WileyTL,NondahlDM.The impactofhearinglossonqualityoflifeinolderadults.Gerontologist[Internet].2003 [cited2023Apr13];43(5):661–8.Availablefrom: https://www.ncbi.nlm.nih.gov/pubmed/14570962
HEARtoMaintainYourHearingHealth
4.Li-KorotkyHS.Age-RelatedHearingLoss:QualityofCareforQualityofLife. Gerontologist[Internet].2012Mar1[cited2023Apr12];52(2):265–71.Available from: https://academic.oup.com/gerontologist/article/52/2/265/616546
5.AmericanSpeech-Language-HearingAssociation.Hearingscreening[Internet]. ASHA.org.2009[cited2023Apr12].Availablefrom: https://www.asha.org/public/hearing/Hearing-Screening/
6.NIH.Noise-inducedhearingloss[Internet].NIDCD.2018[cited2023Apr12]. Availablefrom:https://www.nidcd.nih.gov/health/noise-induced-hearing-loss
7.HornsbyBWY.TheEffectsofHearingAidUseonListeningEffortandMental FatigueAssociatedWithSustainedSpeechProcessingDemands.EarHear[Internet]. 2013Sep[cited2023Apr12];34(5):523–34.Availablefrom: https://pubmed.ncbi.nlm.nih.gov/23426091/
8.CentersforDiseaseControlandPrevention.Loudnoisecancausehearingloss [Internet].CDC.gov.2020[cited2023Apr12].Availablefrom: https://www.cdc.gov/nceh/hearing_loss/default.html

Ward Off Dementia With EXERGAMES”
Introduction/Background:
ABSTRACT
Dementia is a syndrome resulting from brain damage that impair several higher cortical functions, including memory, thinking, orientation, comprehension, arithmetic, learning, language and judgment. This is not a natural part of aging.
Dementia refers to a syndrome characterized by progressive decline in cognitive function. As the disorder progresses, patients become increasingly dependent on others to carry out routine daily activities.
Objectives:
Dementia is a serious problem not only for the person with dementia, but also for caregivers and families. It is very important that everyone knows more about dementia. This poster aims to raise people's awareness about how to prevent dementia through Exergame. Exergaming is an innovative method of training in a virtual reality or gaming environment that helps people with dementia become physically active while receiving cognitive stimulation. We also present EXERGAMES for dementia risk prevention including:
EX : Exercise actively with constant interval.
ER : Engage on regular social and mental activities.
GA : Gain a better sleep quality.
ME : Mediterranean healthy plate diet.
S : Support for informal care and caregivers.
We hope this poster will educate people about dementia and help those prone to dementia improve public health well-being without dementia.
“
Keywords: Dementia, Brain, Exergame
References:
Active ageing - world health organization [Internet]. [cited 2023Apr13]. Available from: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHO-ActiveAgeing-Framework.pdf
Bansal N, Parle M. Dementia: An overview. Journal of Pharmaceutical Technology, Research and Management. 2014;2(1):29–45.
Dementia [Internet]. World Health Organization. World Health Organization; [cited 2023Apr13].
Available from: https://www.who.int/news-room/fact-sheets/detail/dementia
Van Santen J, Dröes R-M, Holstege M, Henkemans OB, van Rijn A, de Vries R, et al. Effects of exergaming in people with dementia: Results of a systematic literature review. Journal of Alzheimer's Disease. 2018;63(2):741–60.
What is dementia? - alzheimer's society [Internet]. [cited 2023Apr13]. Available from: https://www.alzheimers.org.uk/sites/default/files/201810/400%20What%20is%20dementia.pdf
wHAT IS wHAT IS DEMENTIA? DEMENTIA?





Dementia is a term for several diseases that affect memory, thinking, and the ability to perform daily activities. This illness gets worse over time.
DID YOU KNOW? DID YOU KNOW?
Dementia affects over 46 million individuals in worldwide. The number of dementia patient is expected to increase to 131.5 million by 2050.


EXERGAME FOR EXERGAME FOR FUTURISTIC CARE FUTURISTIC CARE









Exergame is a combination of exercise and game. It helps to improve physical and mental activity to prevent dementia.




YESNO




warning sign OF warning sign OF dementia dementia






Memory loss Changes in mood and behavior




Disorientation to time and place






Withdrawal from social activities


"INNOVATIVE, "INNOVATIVE, "INNOVATIVE, FUN, AND FUN, AND FUN, AND RELATIVELY RELATIVELY RELATIVELY SAFE" SAFE" SAFE"

Exercise

Actively with Constant Interval Engage on Regular Social and Mental Activities



Gain a Better Sleep Quality



Mediterranean Healthy Plate Diet
Support for Informal Care and Caregivers
Muhammad Alif
| Angelie N. Sungkar | Ghina Tsurayya | Teuku
Naufal
Fais Duta
REFERENCES REFERENCES





















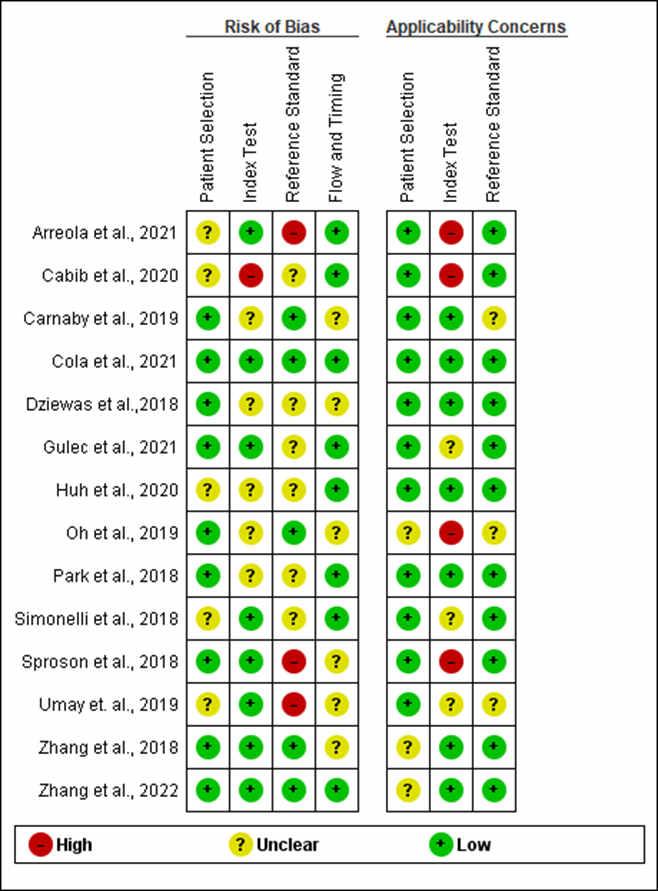


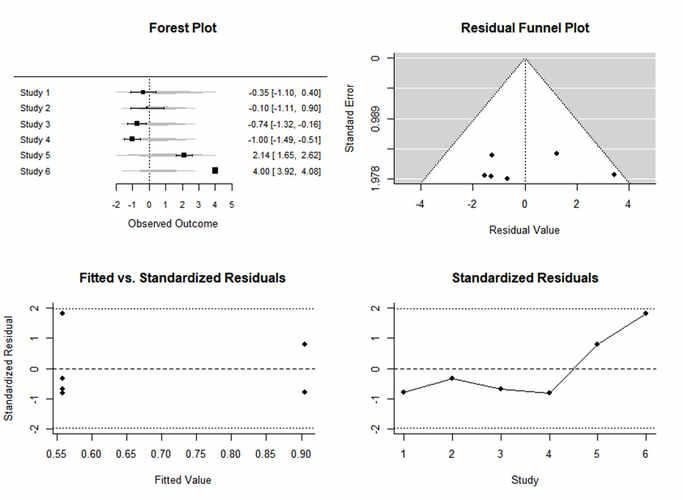





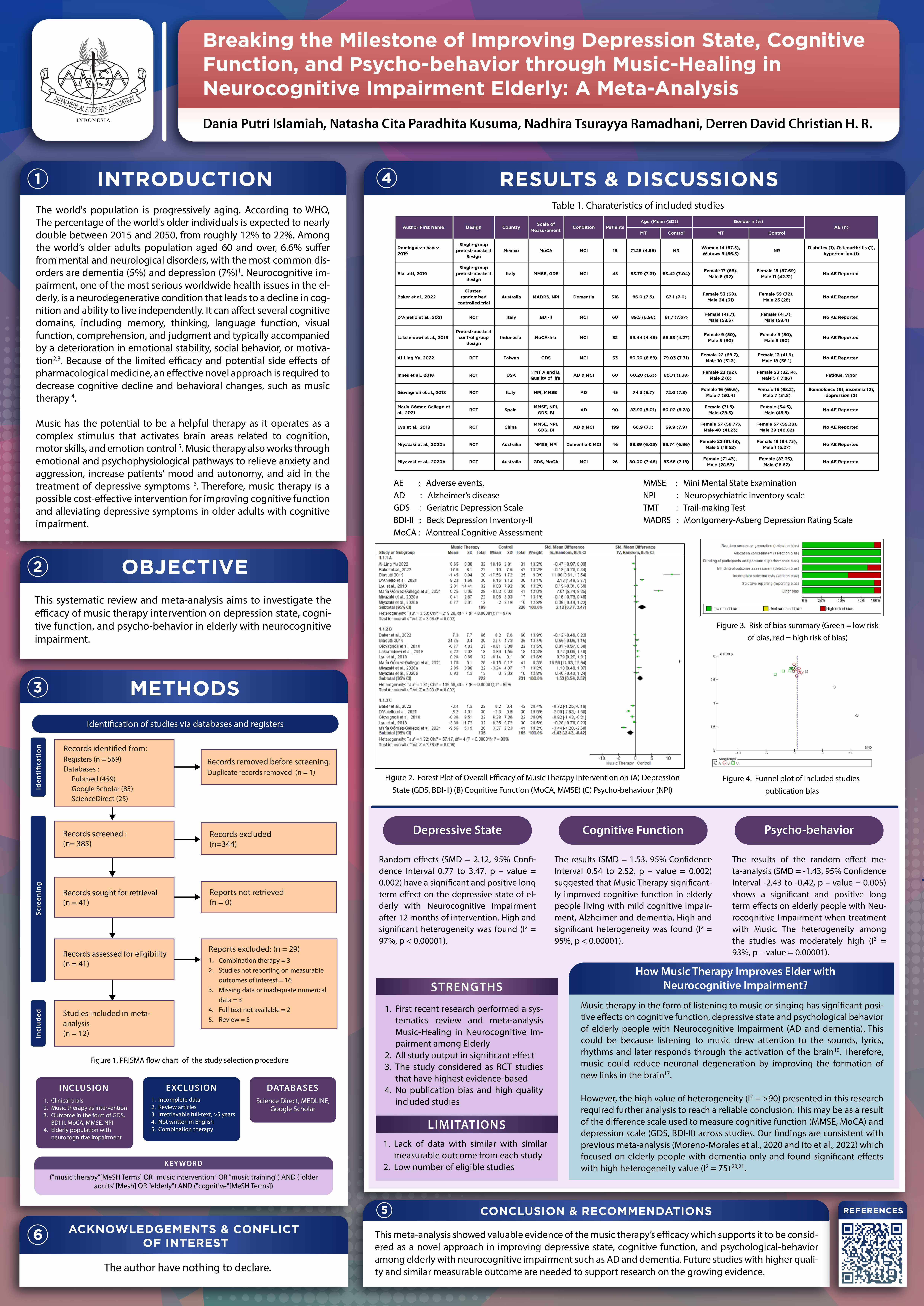
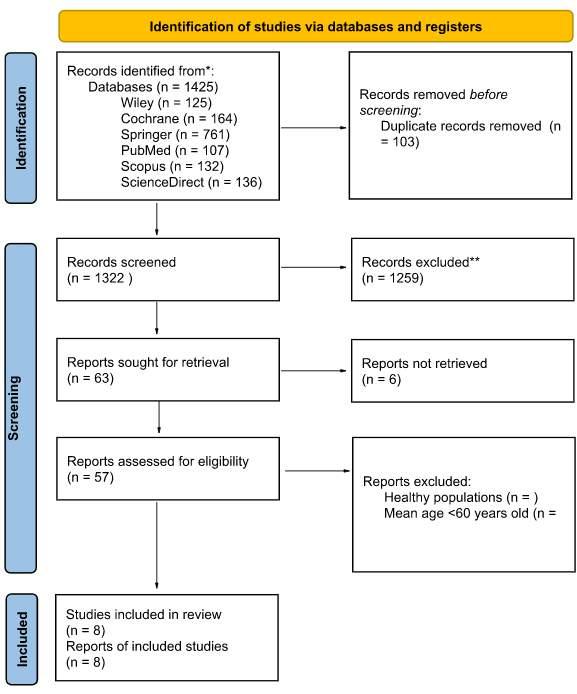
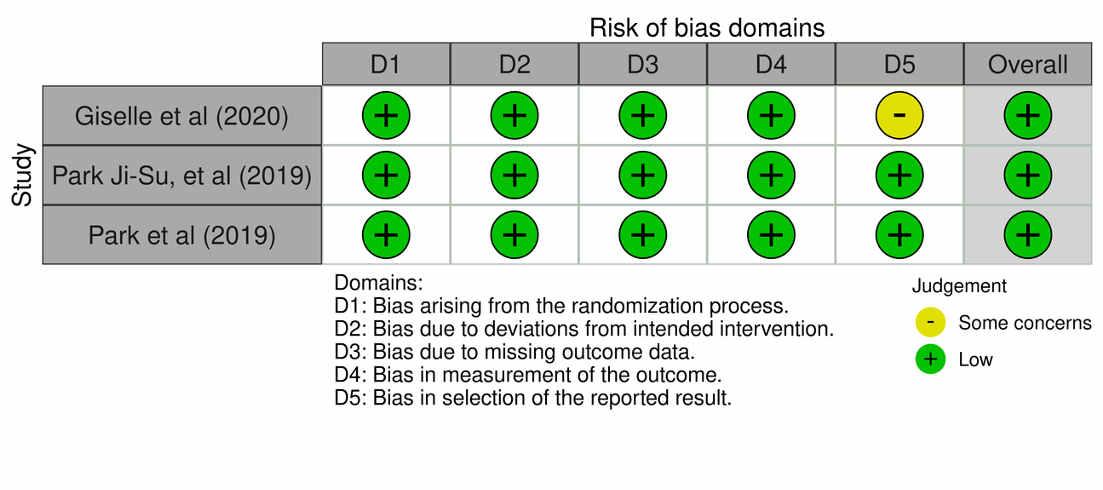



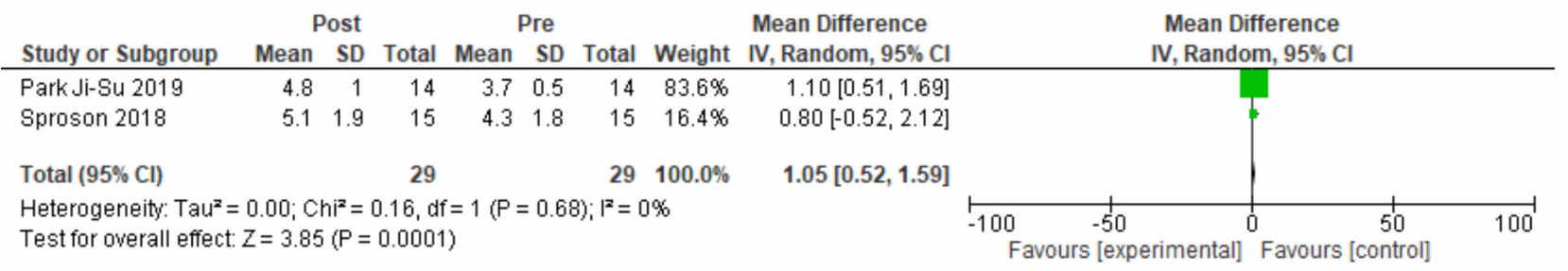


 Introduction
Defin Allevia Yumnanisha, Mukhlis Akmal Taher N, Elvina Firdaus, Kelvin Kohar
Introduction
Defin Allevia Yumnanisha, Mukhlis Akmal Taher N, Elvina Firdaus, Kelvin Kohar




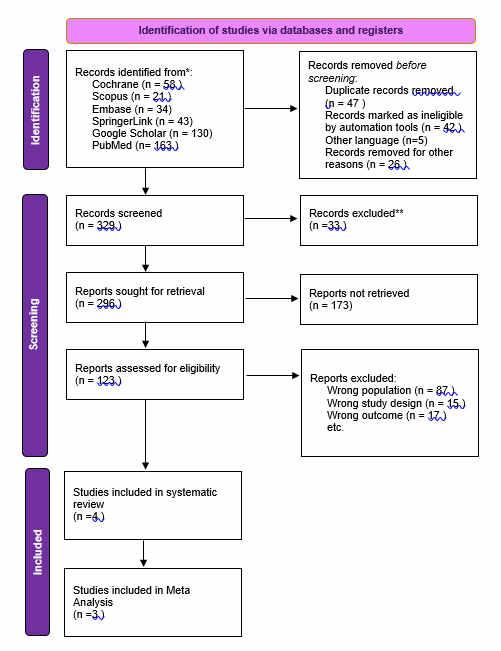

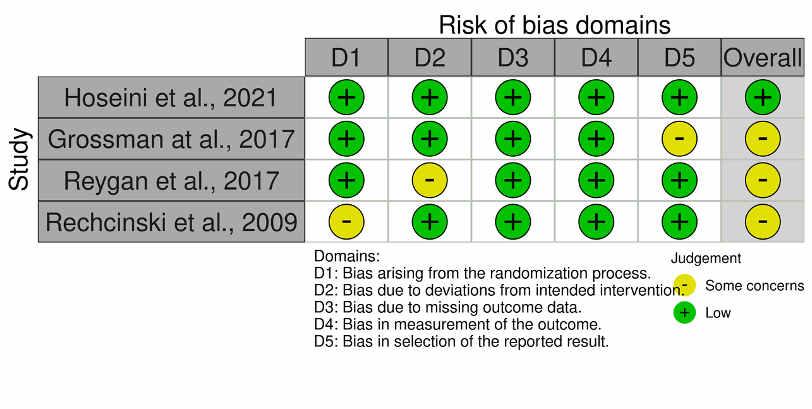











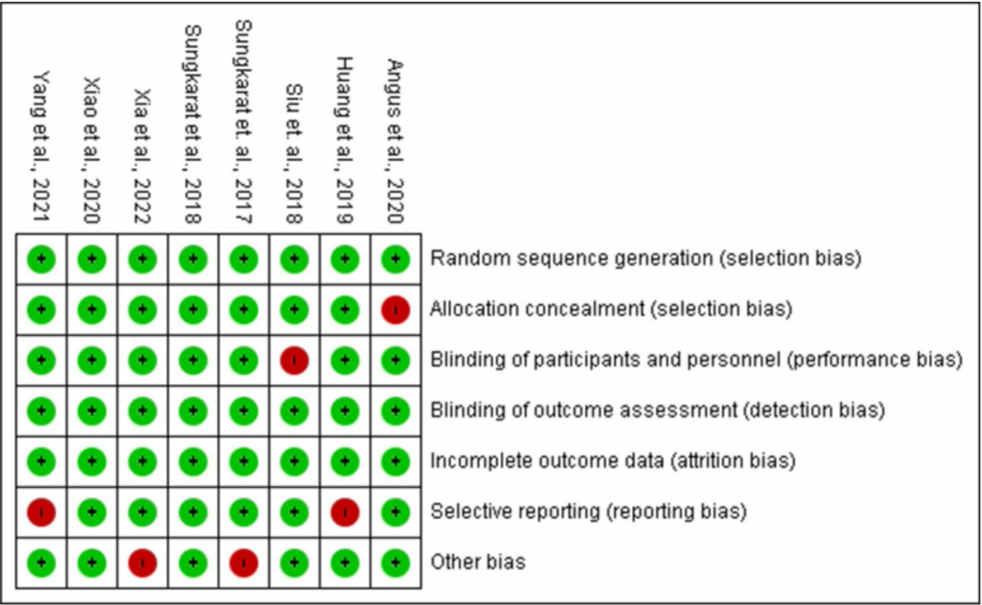







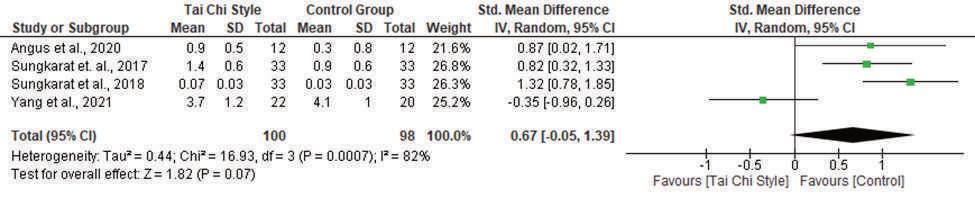

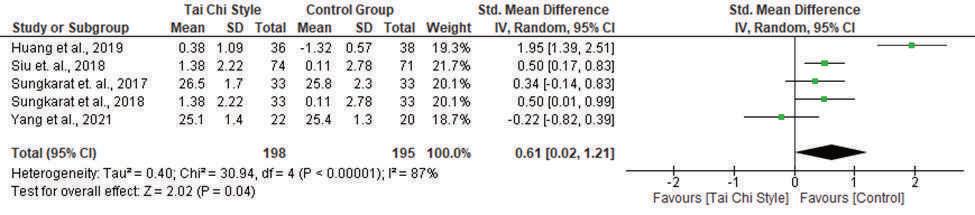
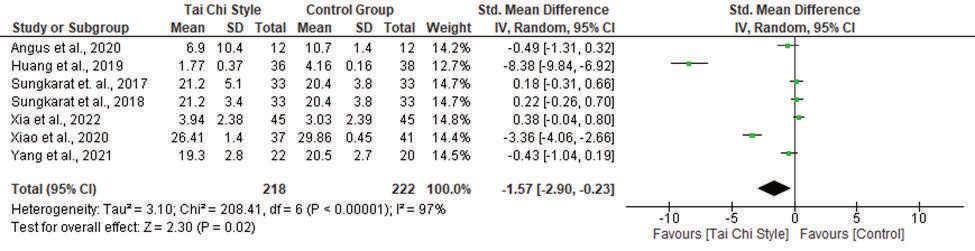










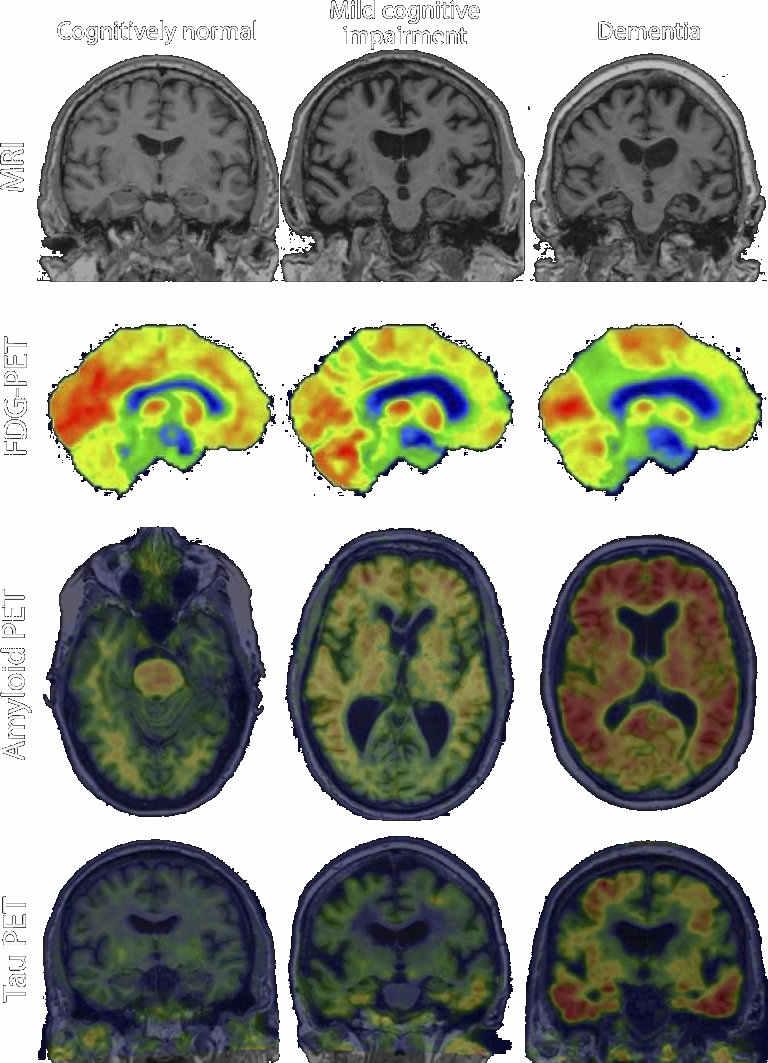











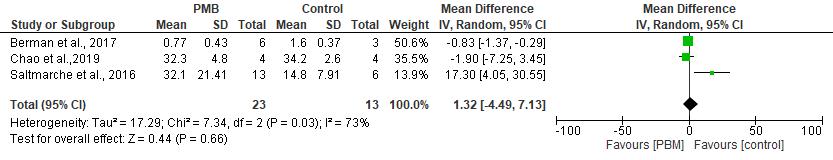



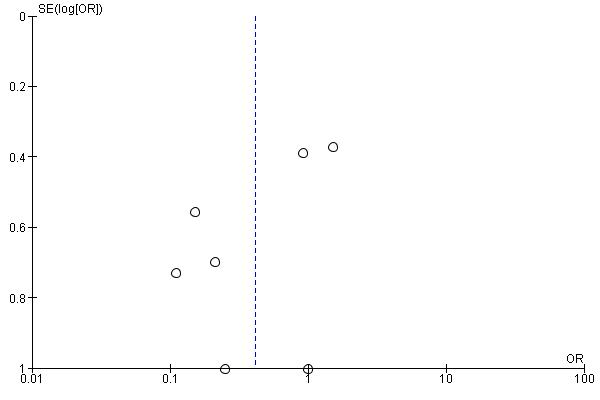

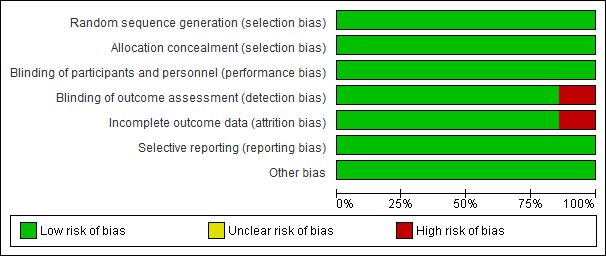

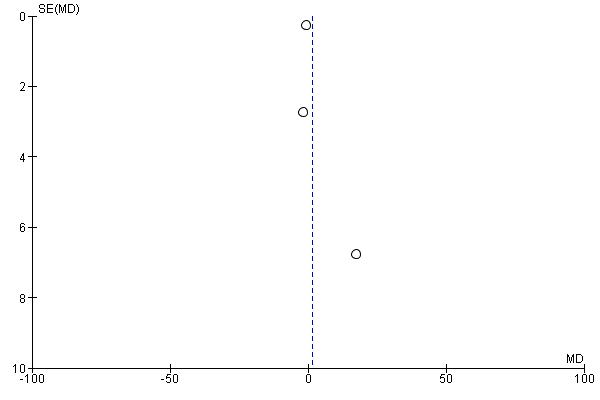



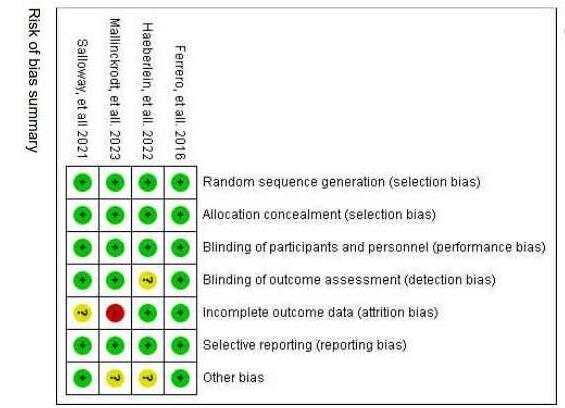










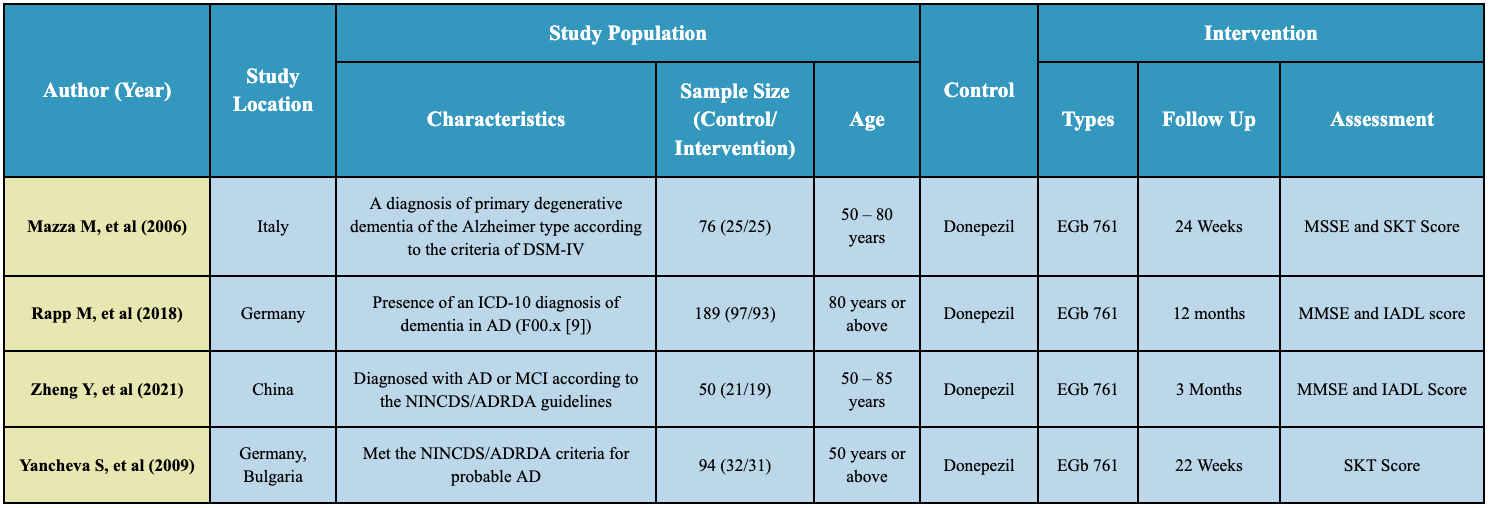

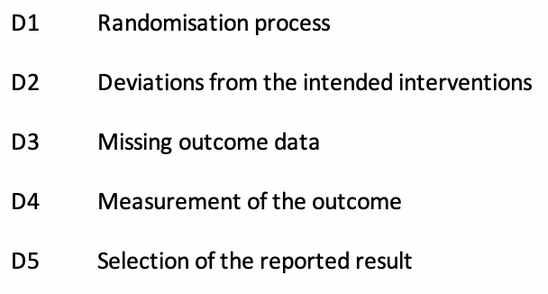




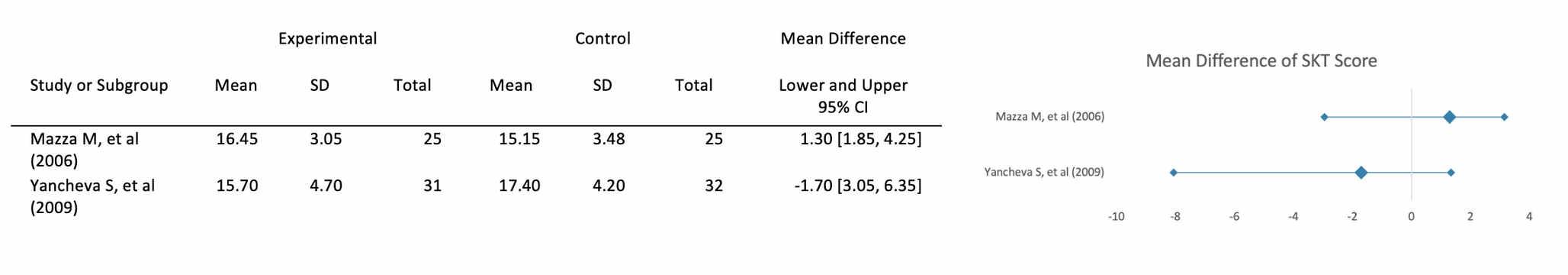


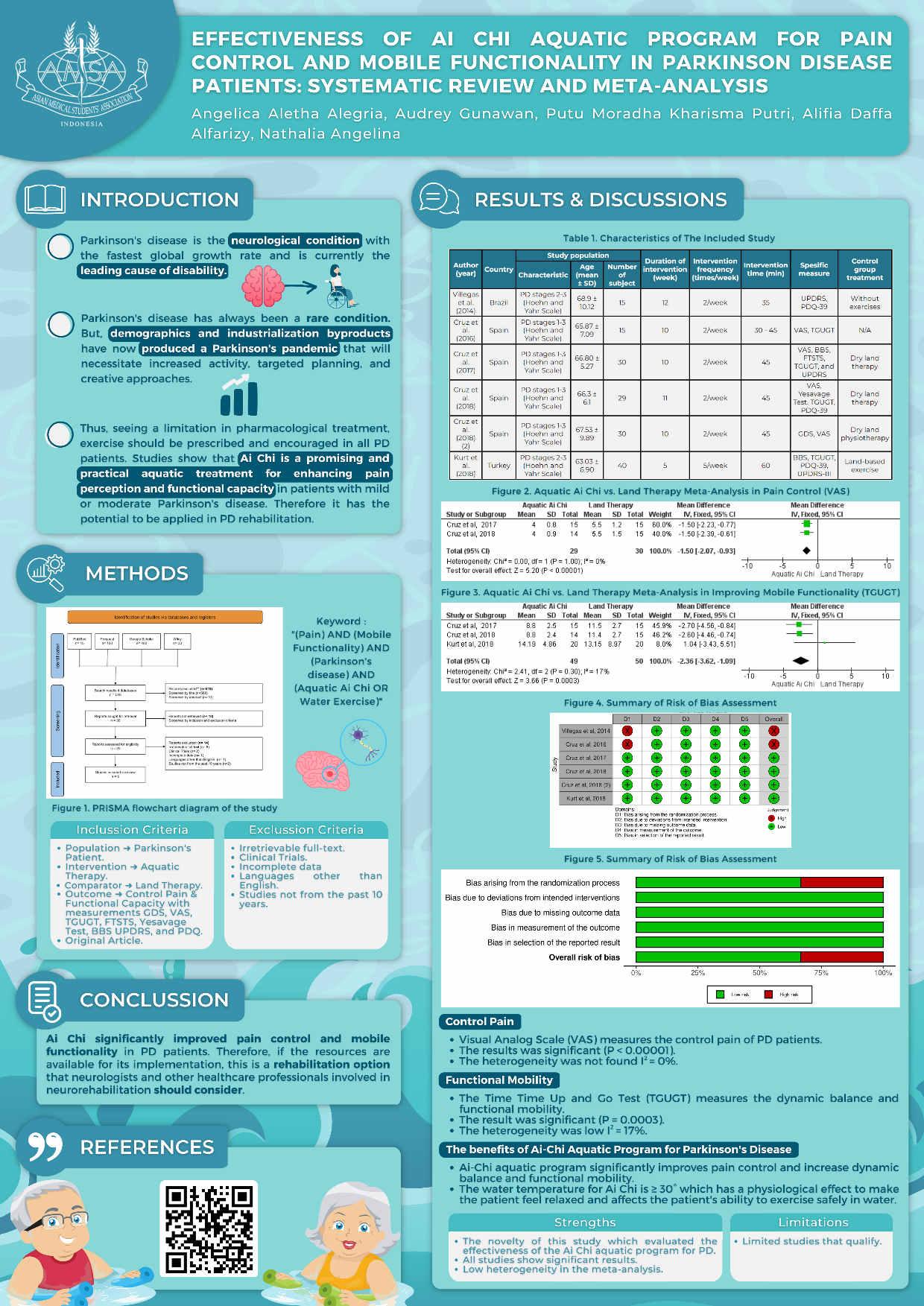
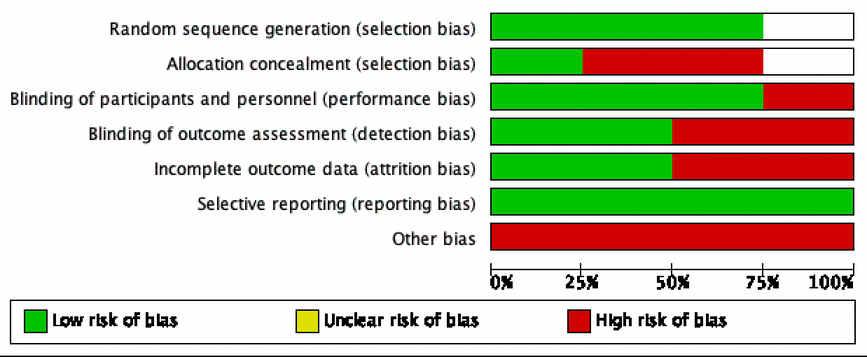

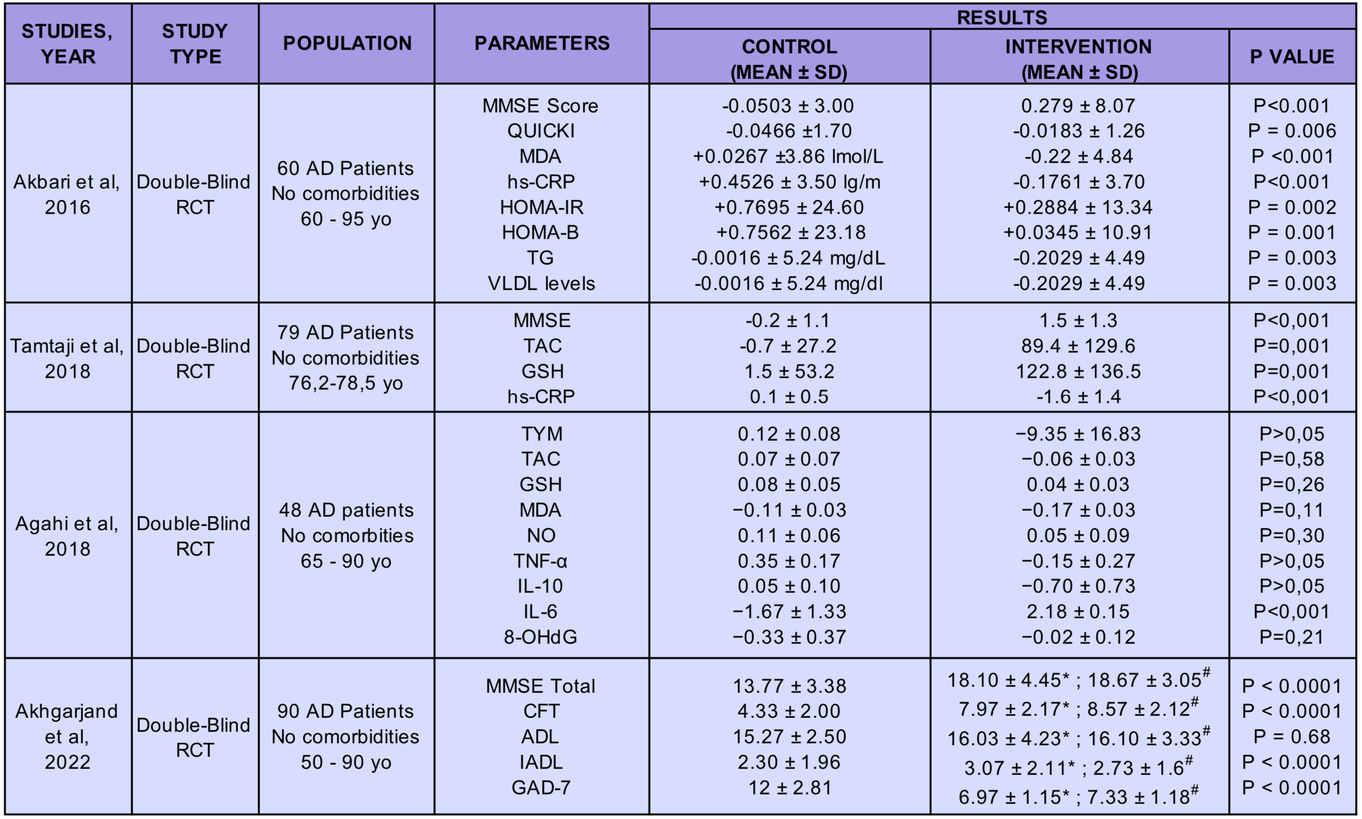










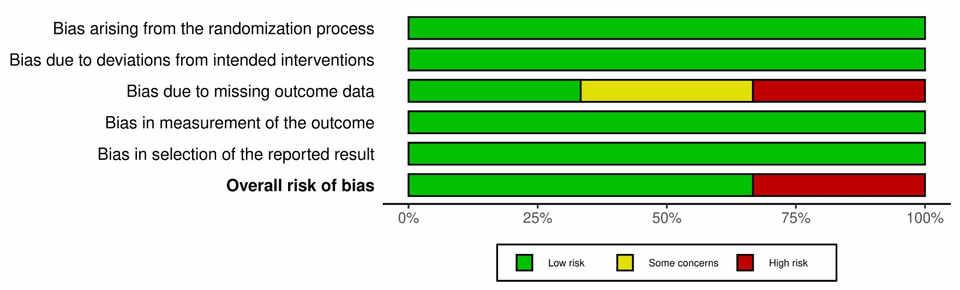

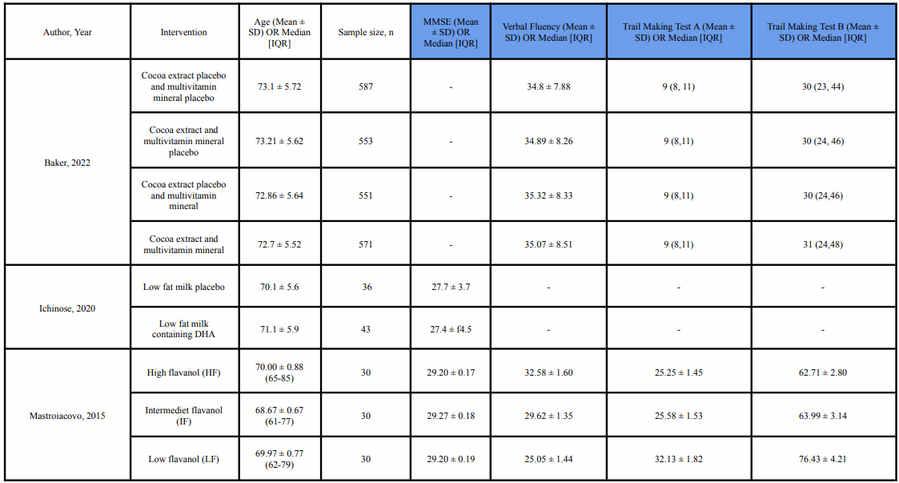








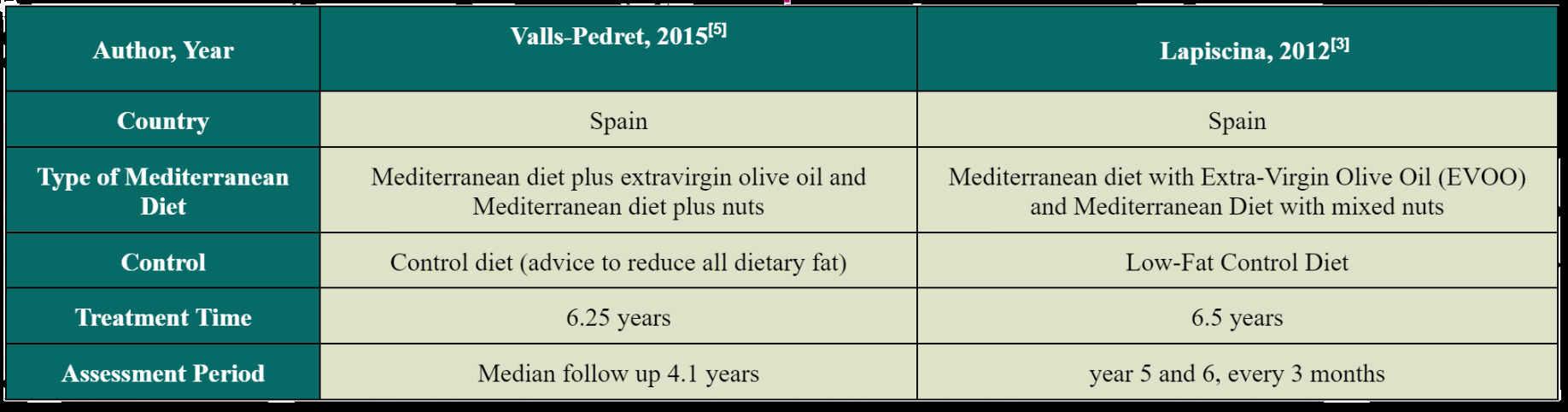







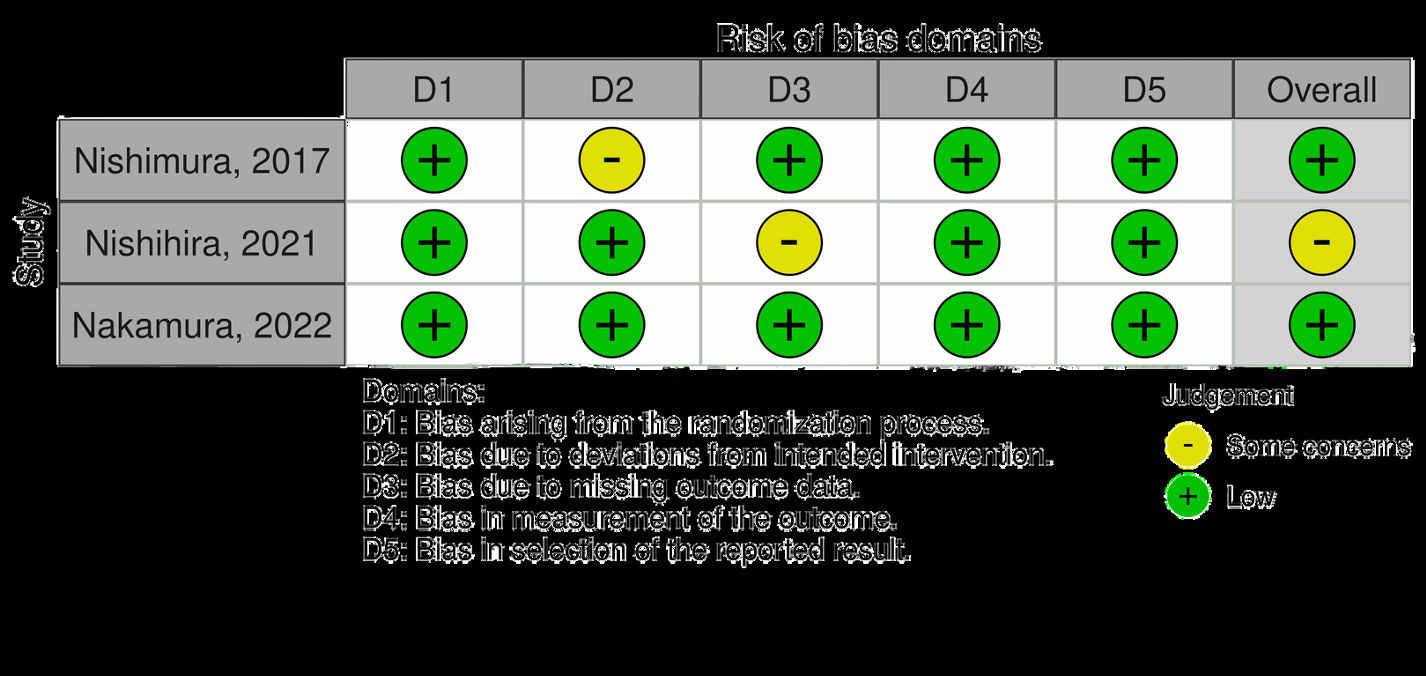



 Takbir Sabda Akhiru Ramadhan, Namira Kirana Djatmiko, Lise Putri Sesotyaningati, Kirafara Ghaitsa
Takbir Sabda Akhiru Ramadhan, Namira Kirana Djatmiko, Lise Putri Sesotyaningati, Kirafara Ghaitsa

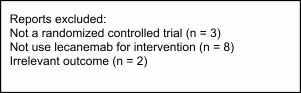


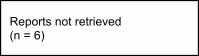
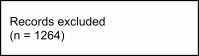



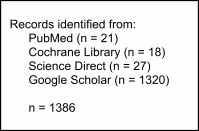
 Figure 1: PRISMA 2020 flow diagram
Figure 2: Risk of Bias Asessment for RCT
Figure 1: PRISMA 2020 flow diagram
Figure 2: Risk of Bias Asessment for RCT



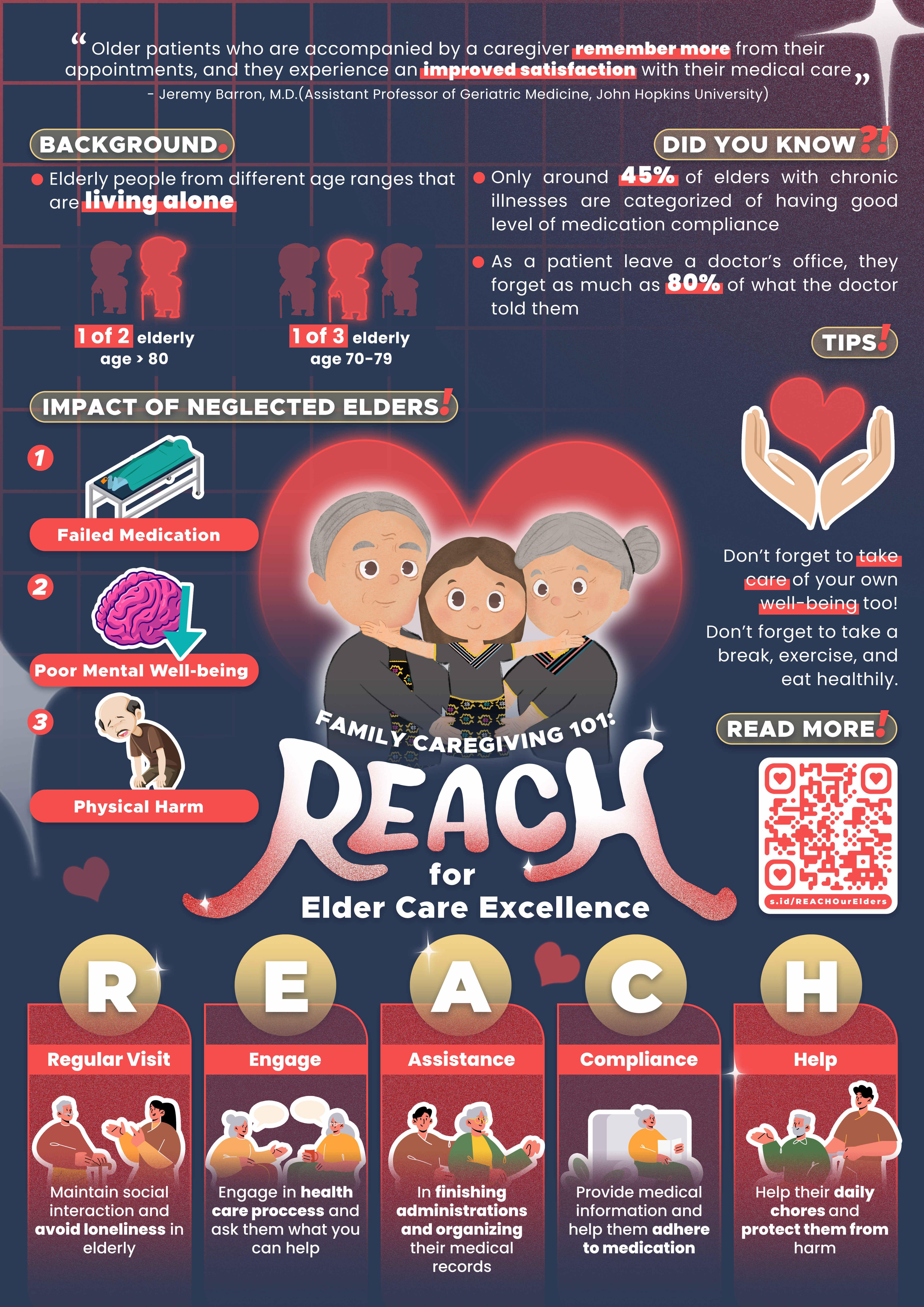

































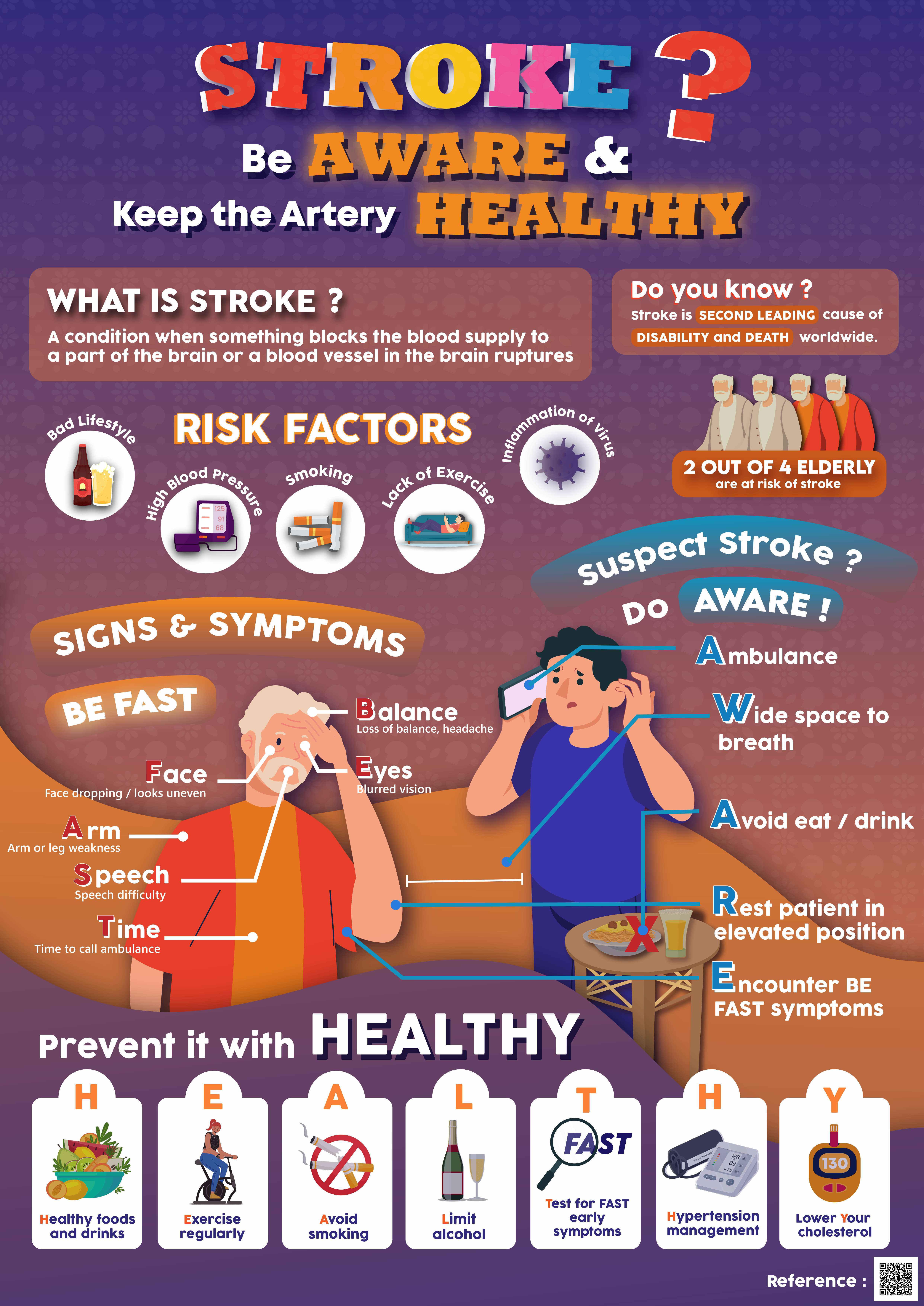





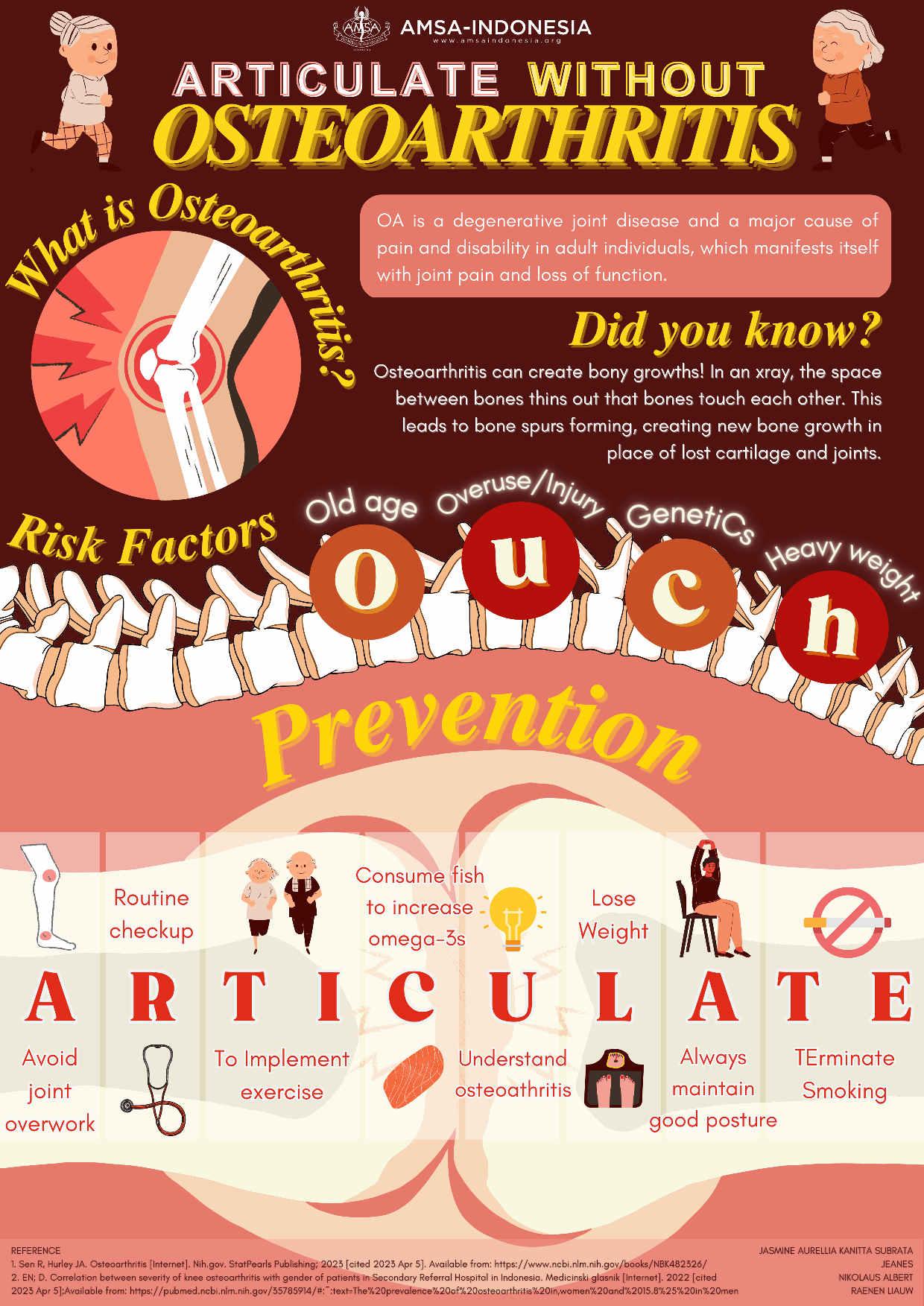

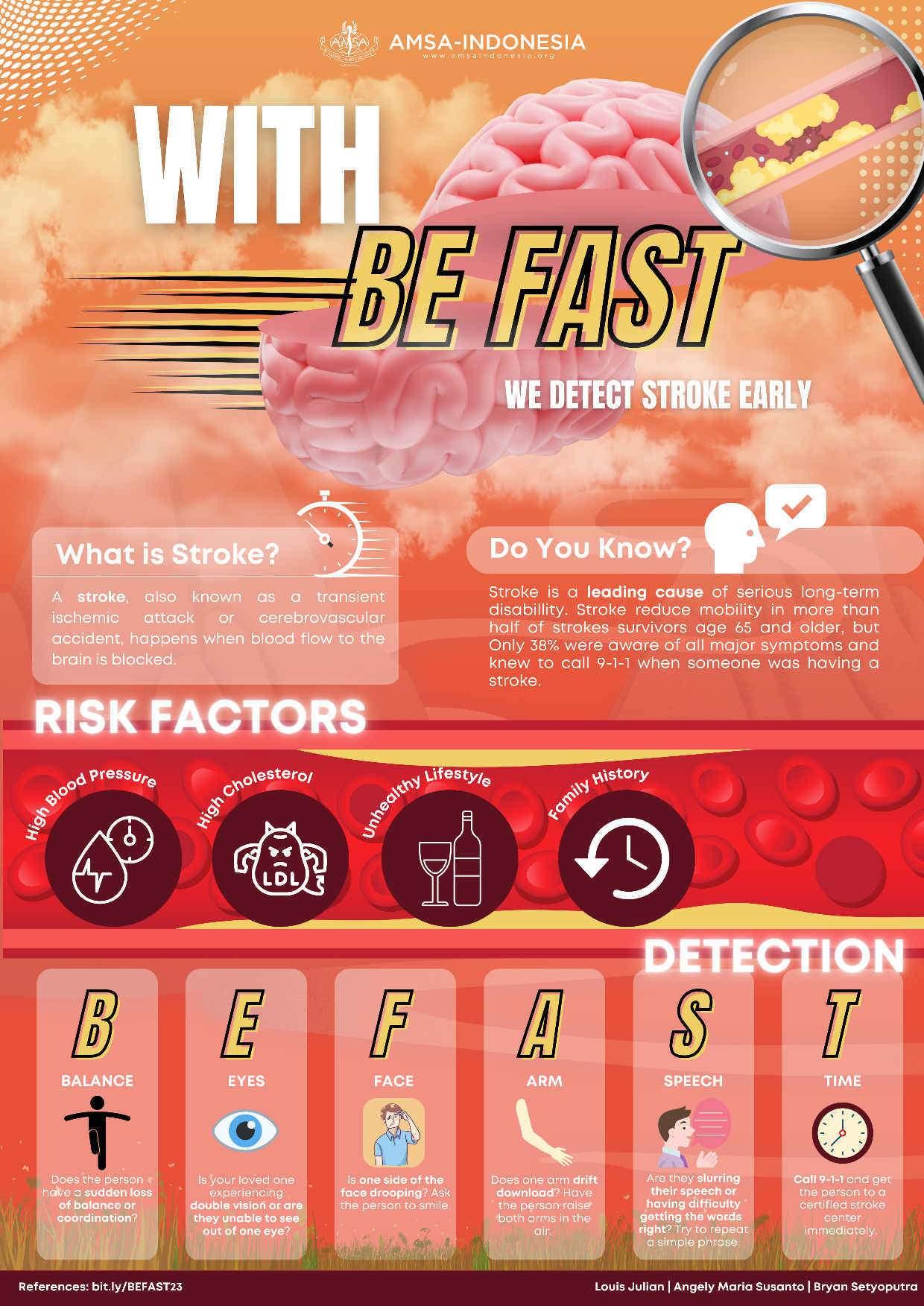

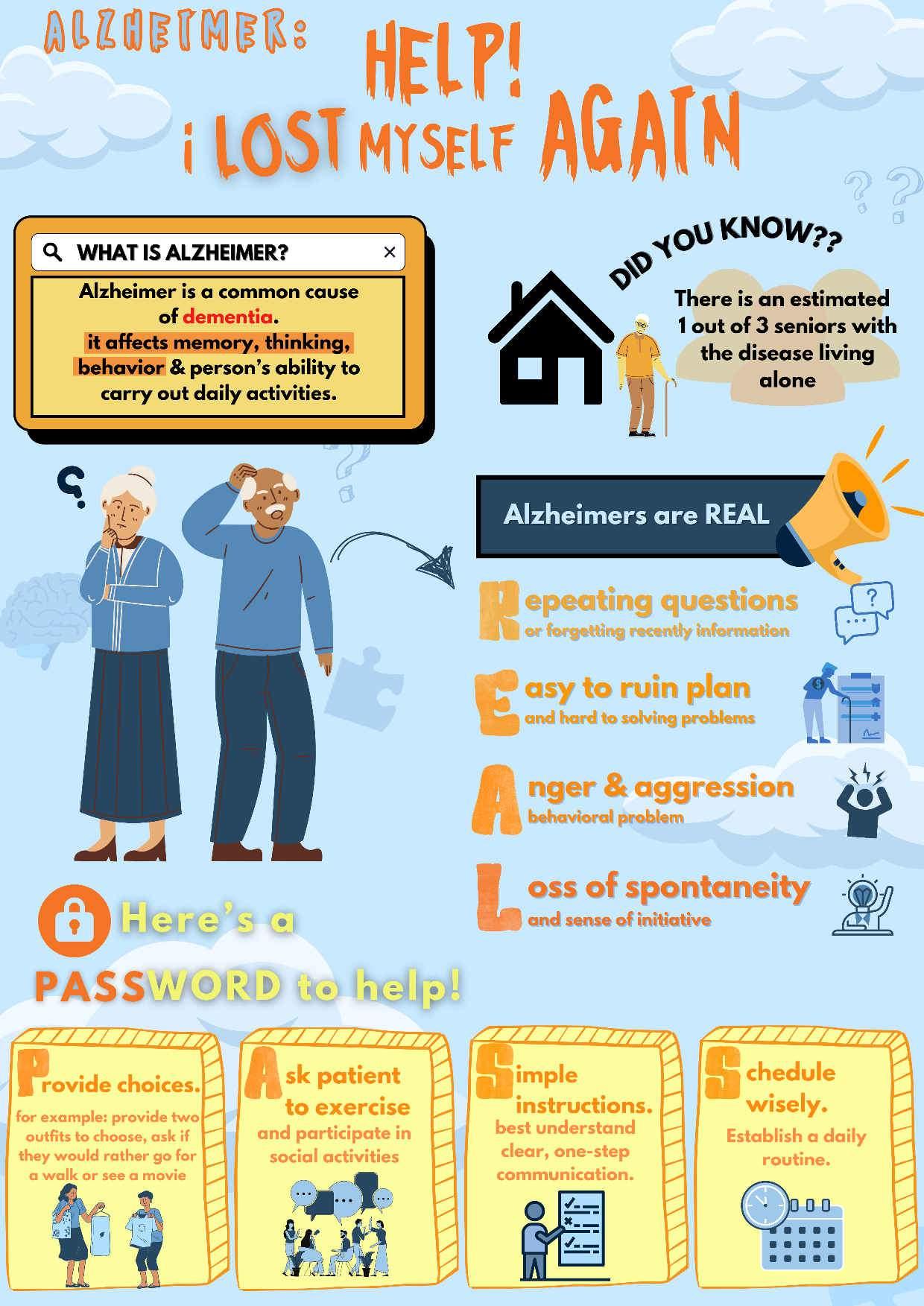











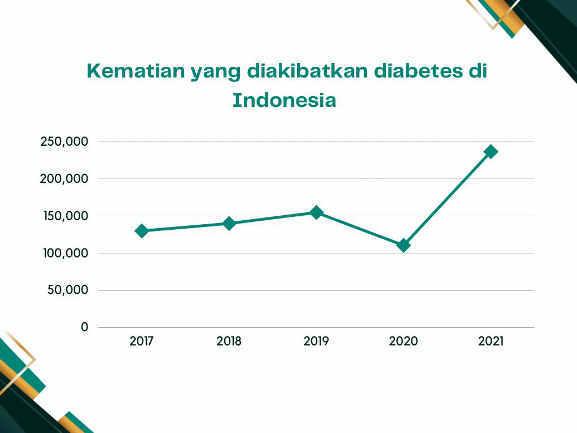


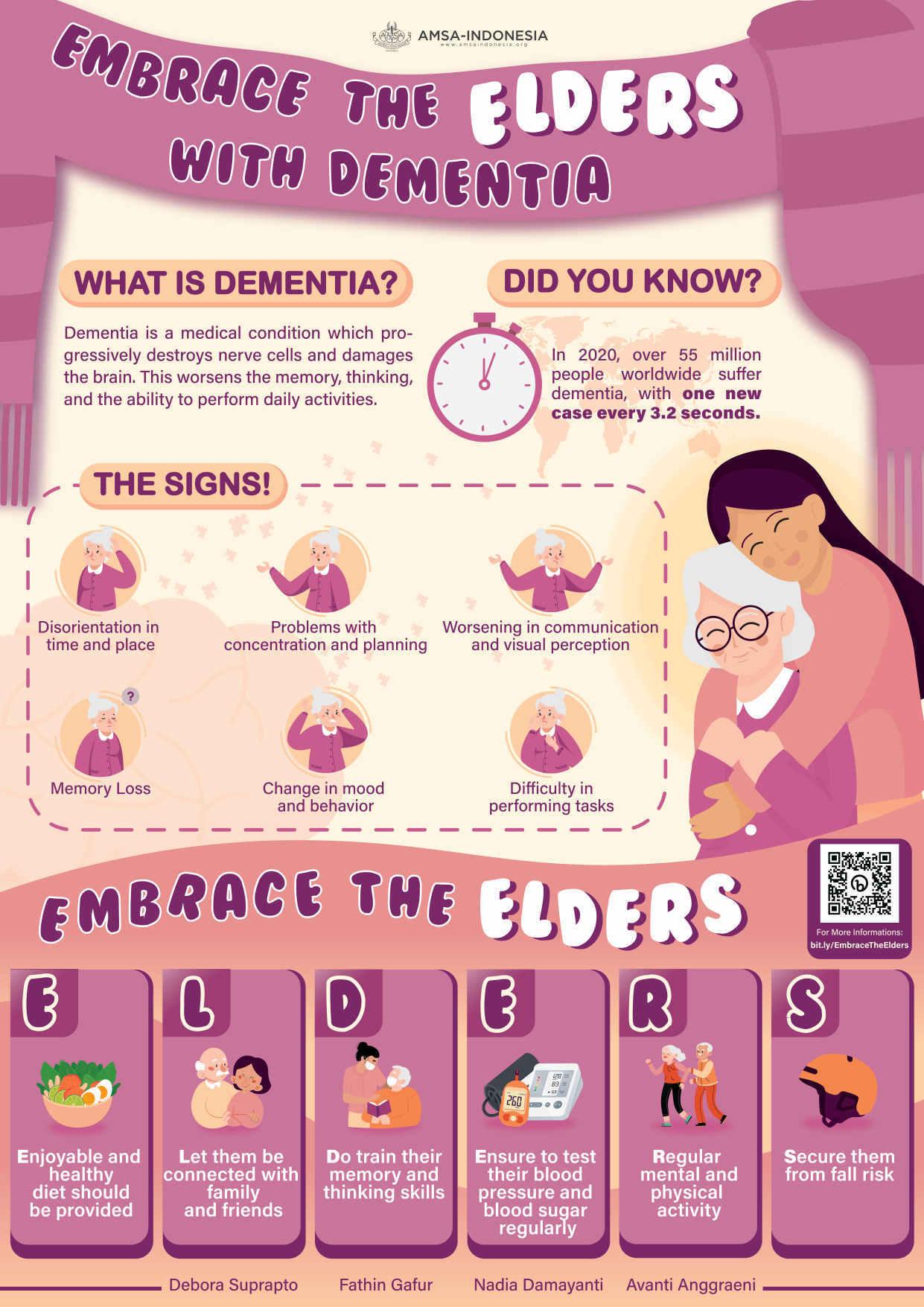









 Aisha Latifa
Aisha Latifa



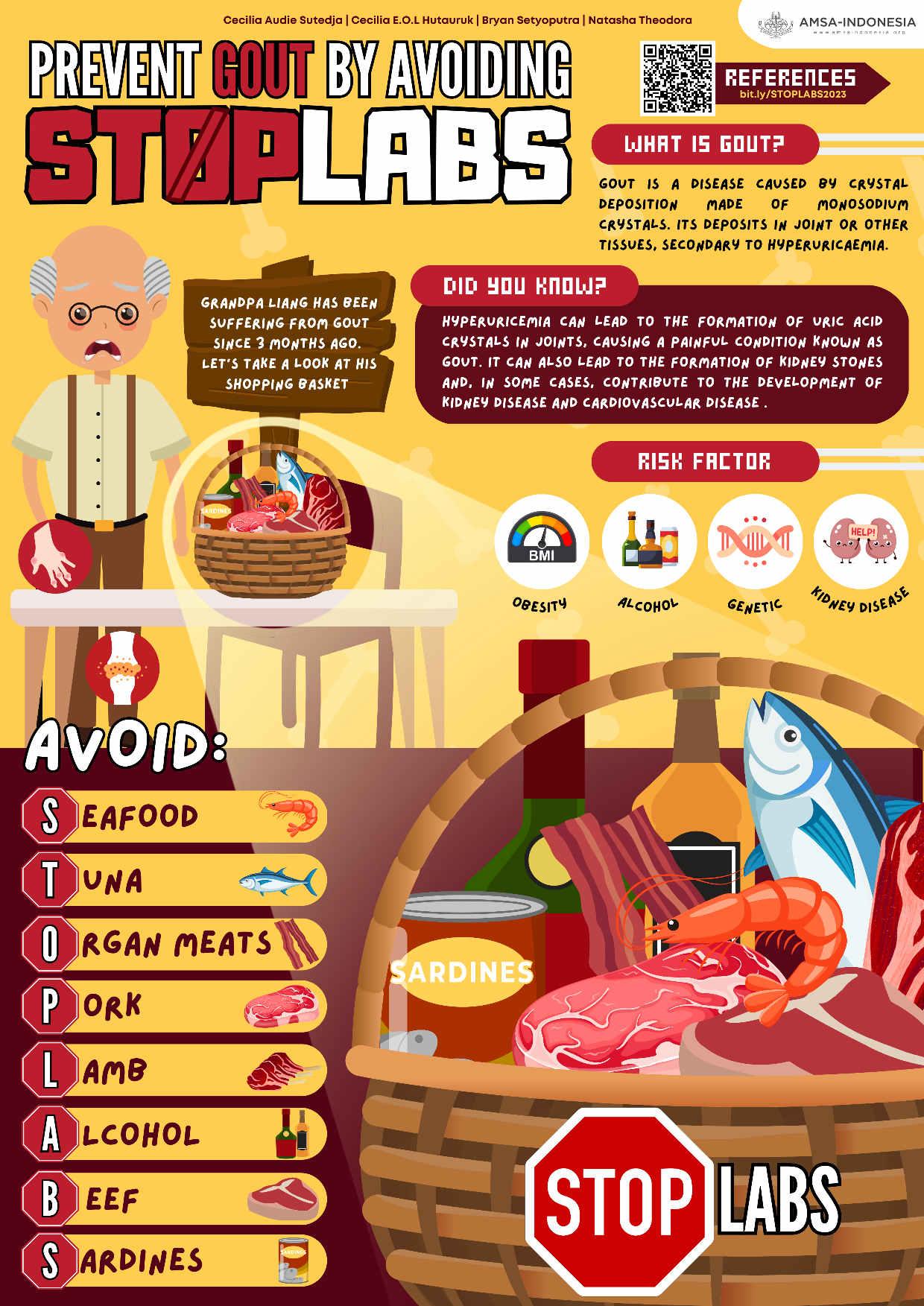



















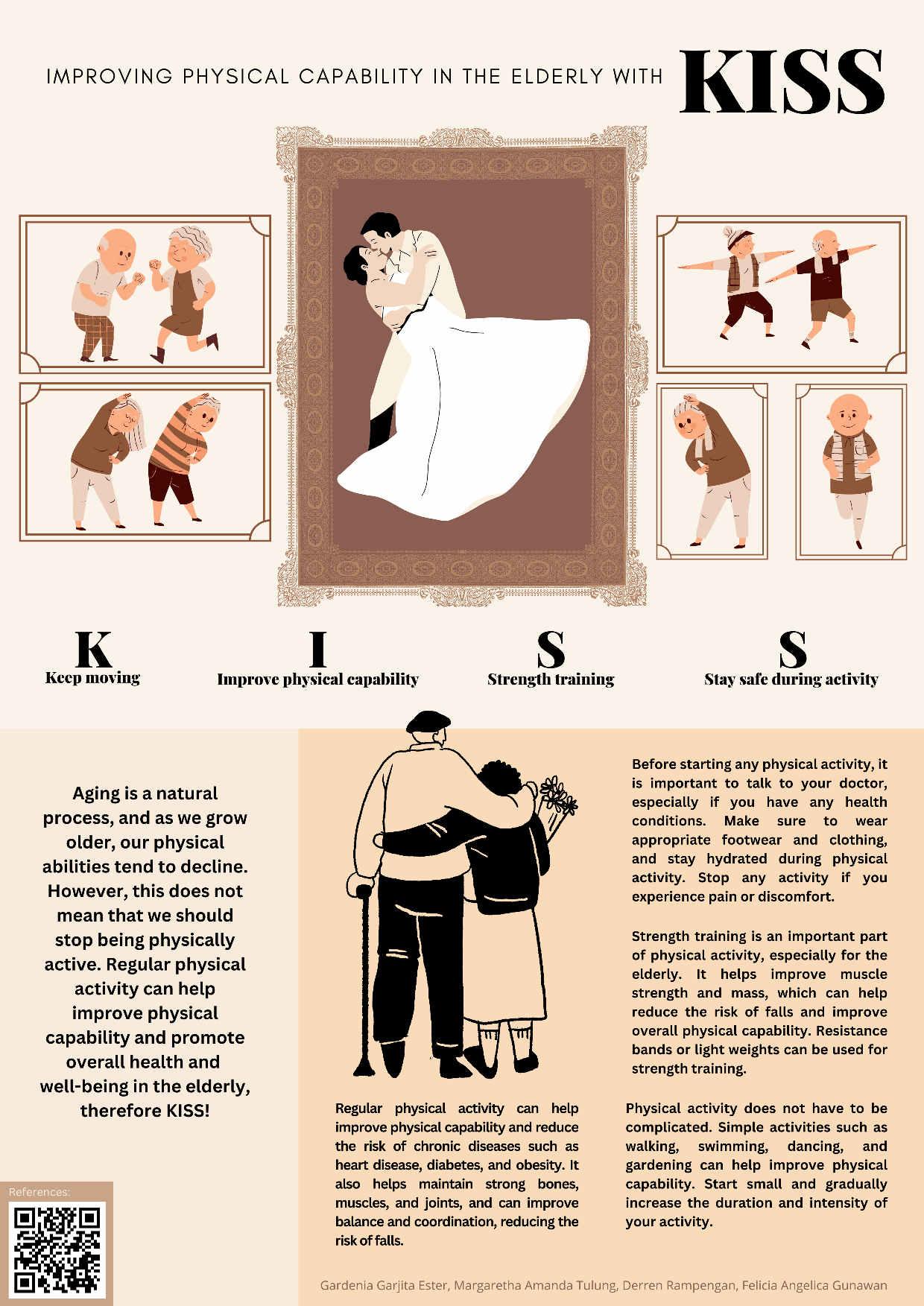











 Aletheia H. PrastyoDerren D. C. H. RampenganGionina H alim
Aletheia H. PrastyoDerren D. C. H. RampenganGionina H alim

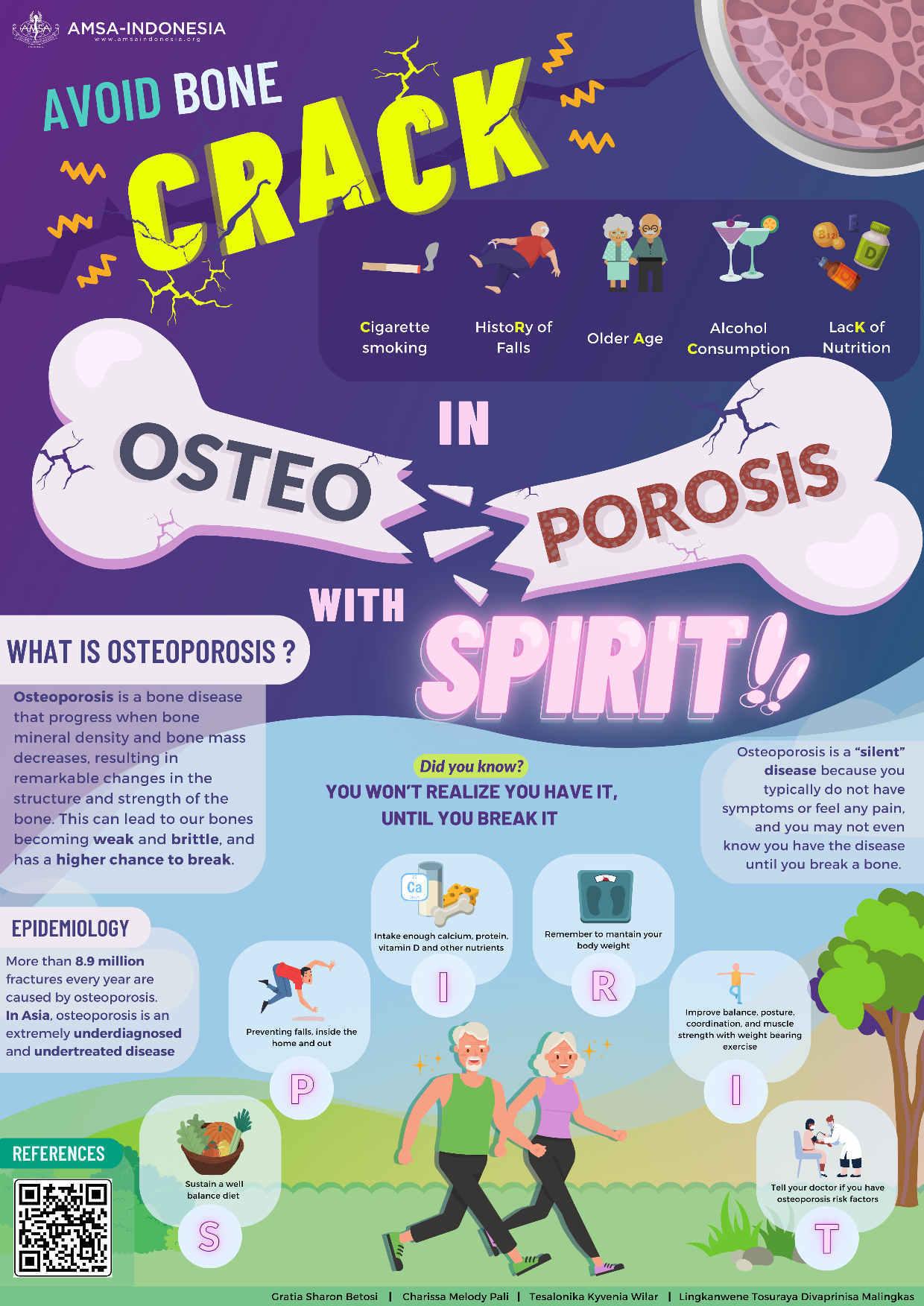


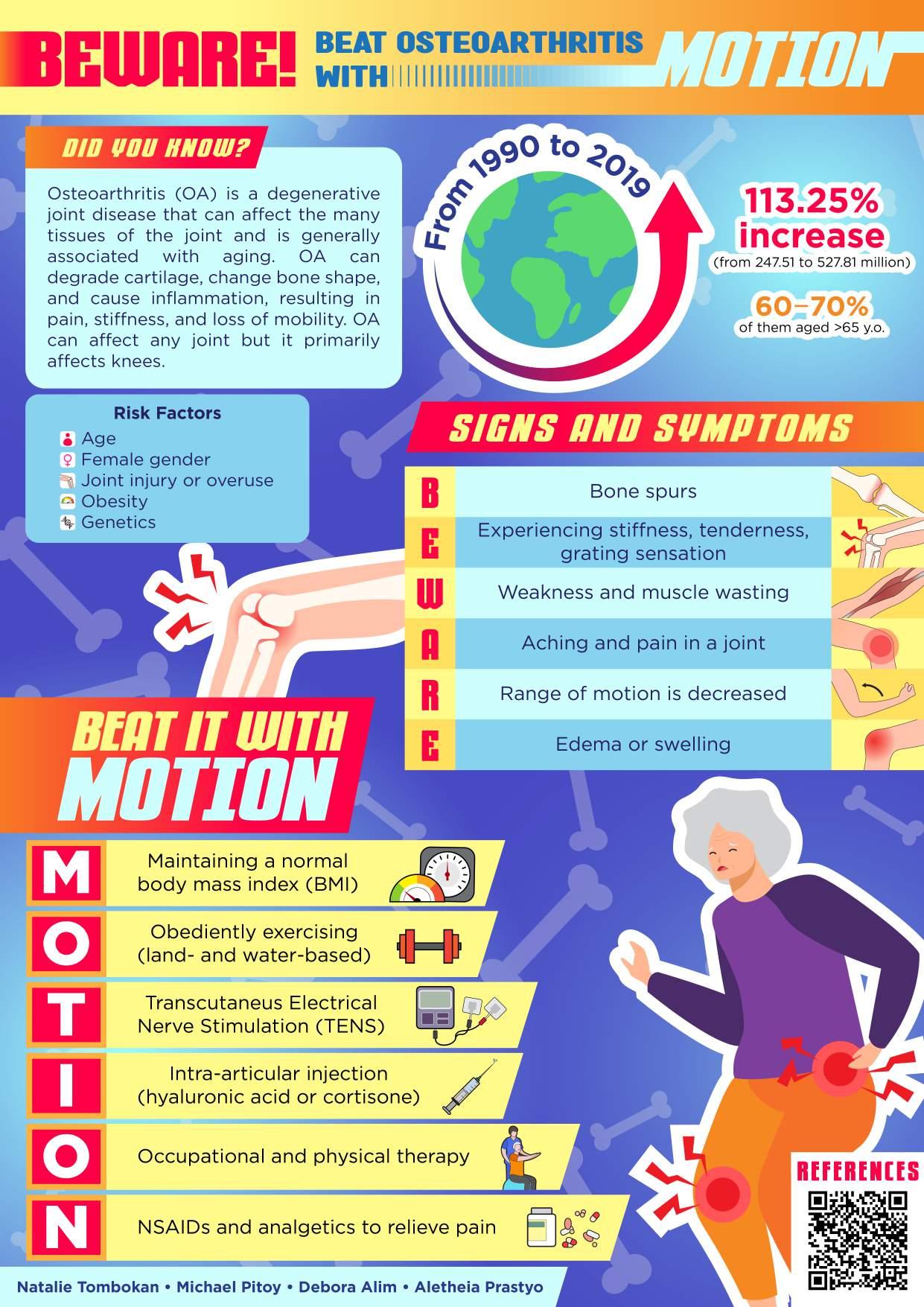










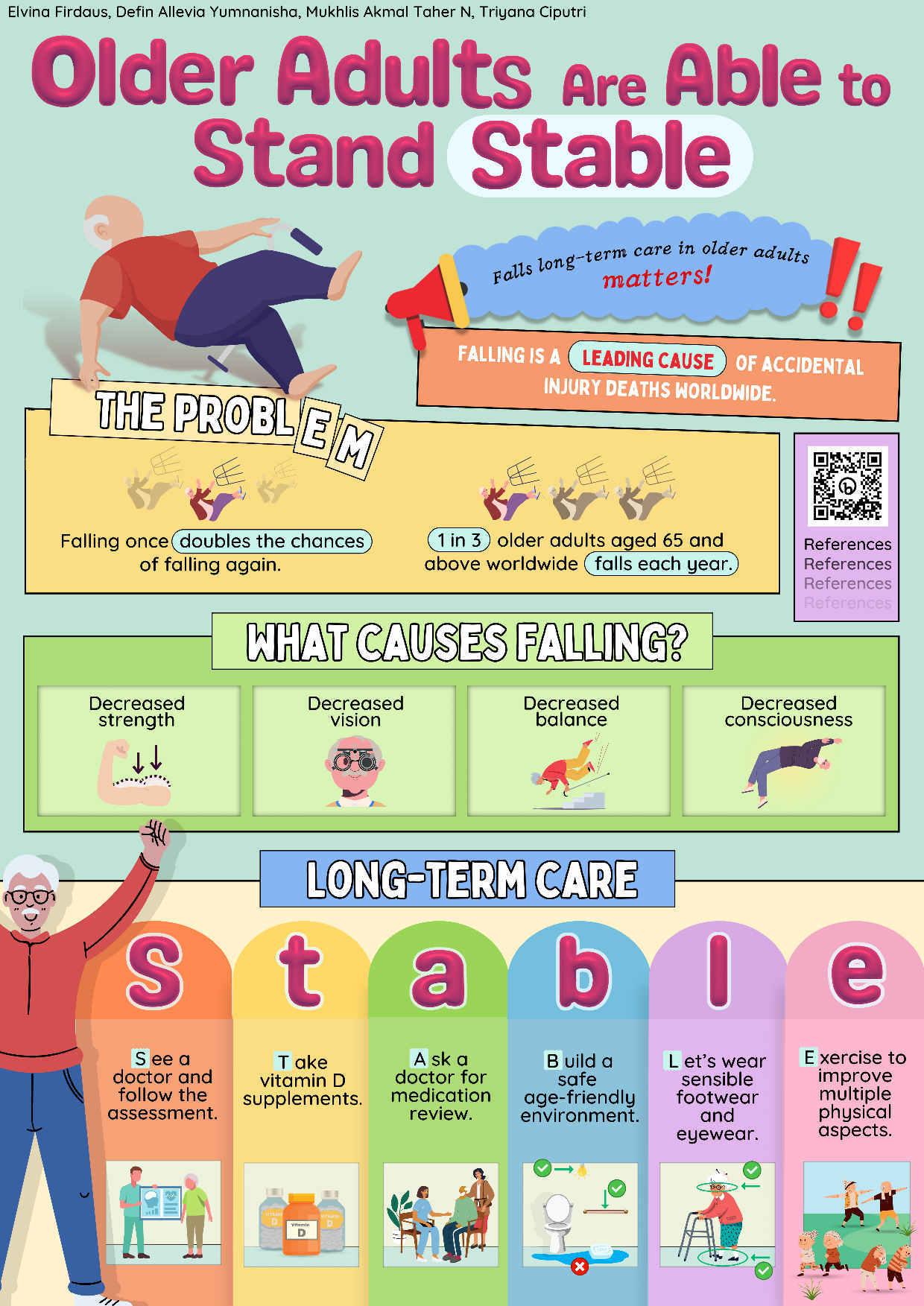






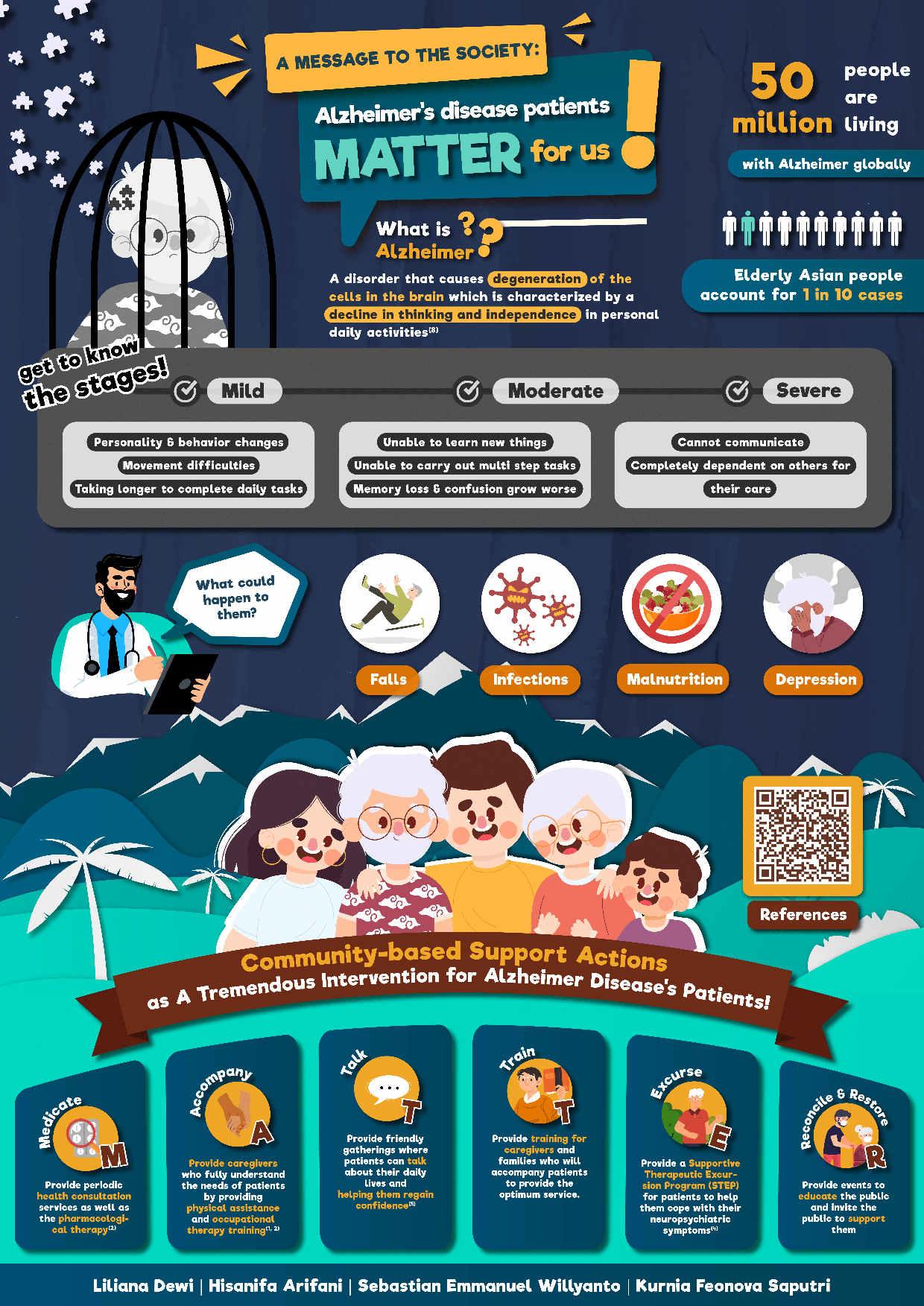












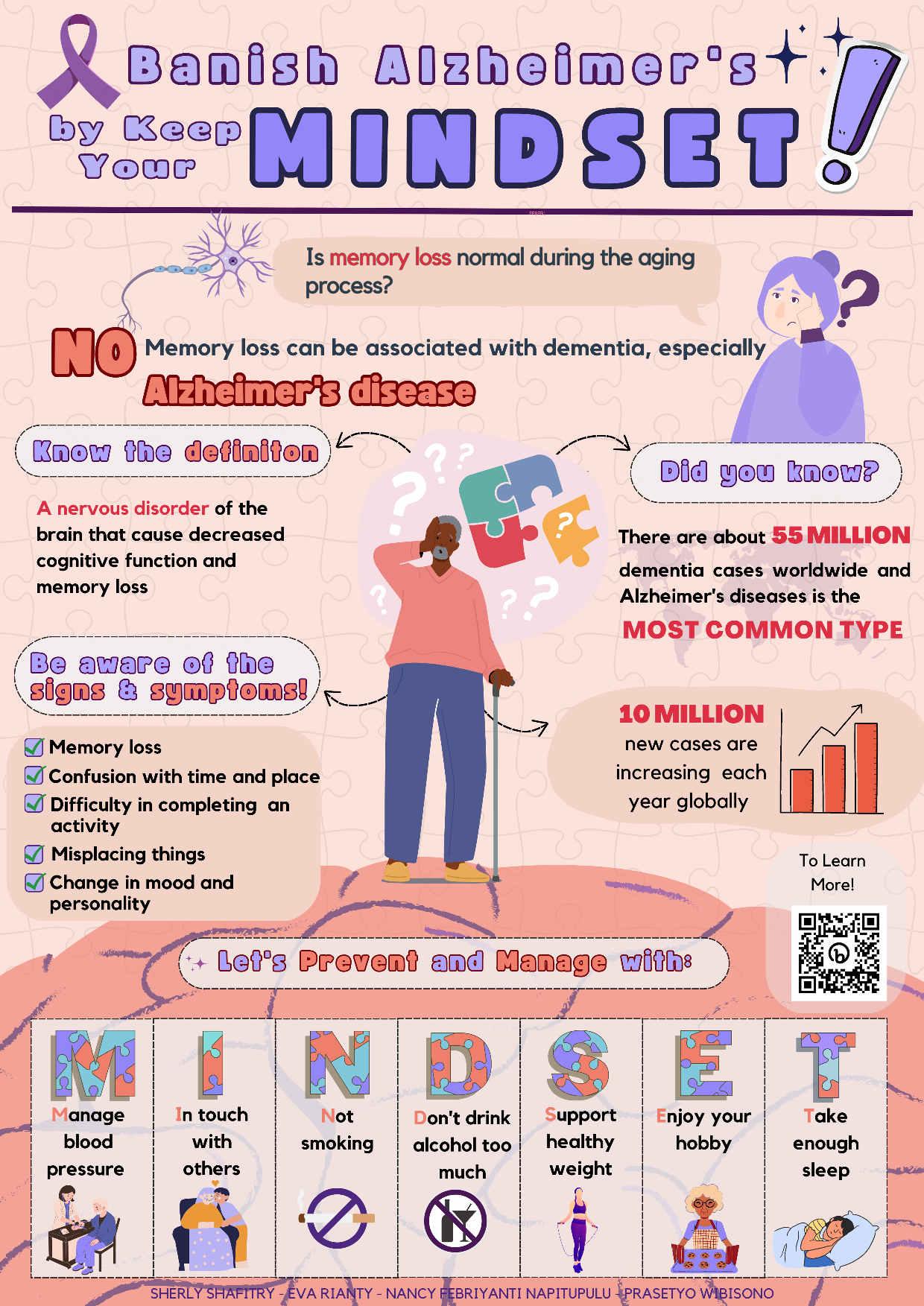


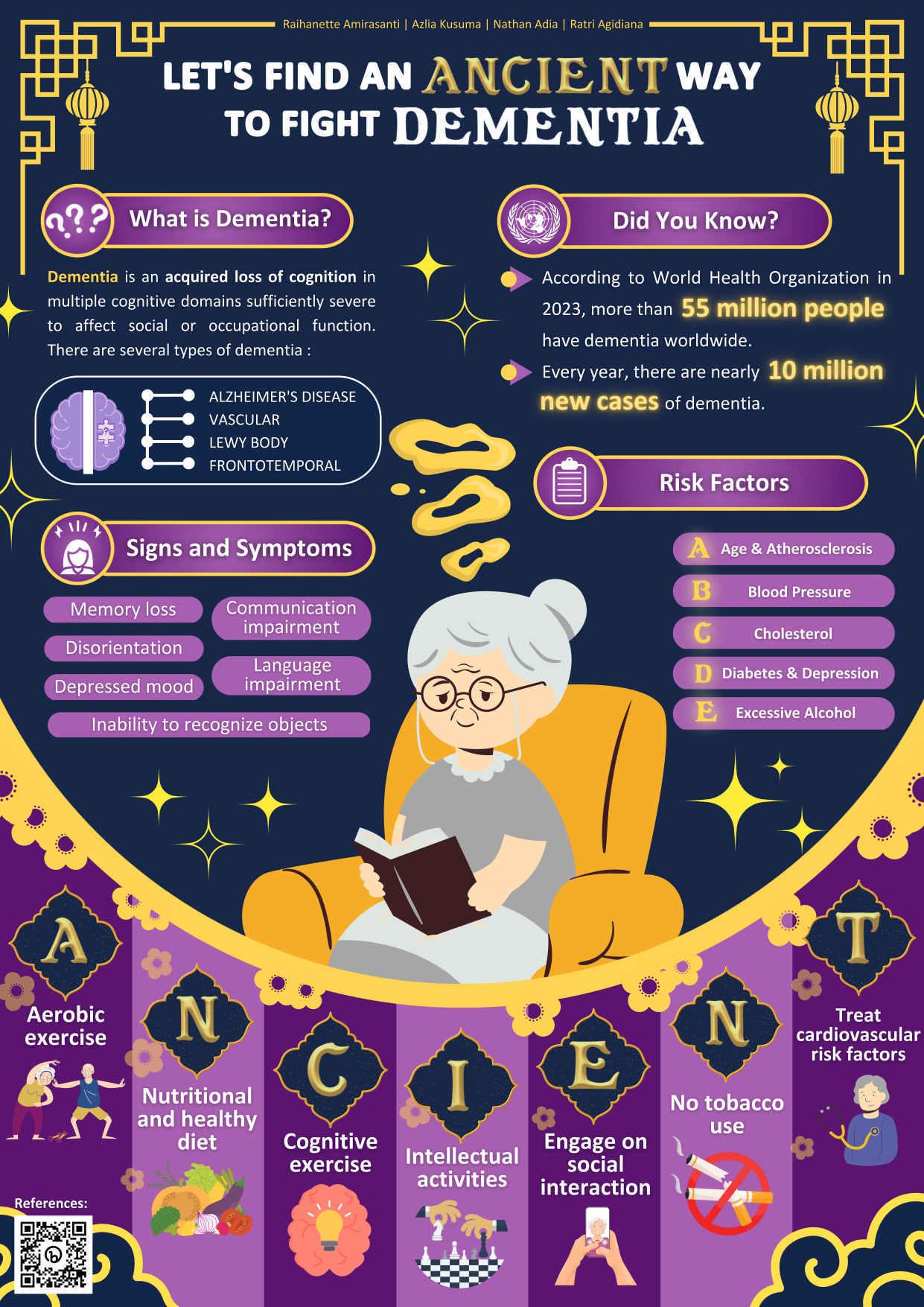

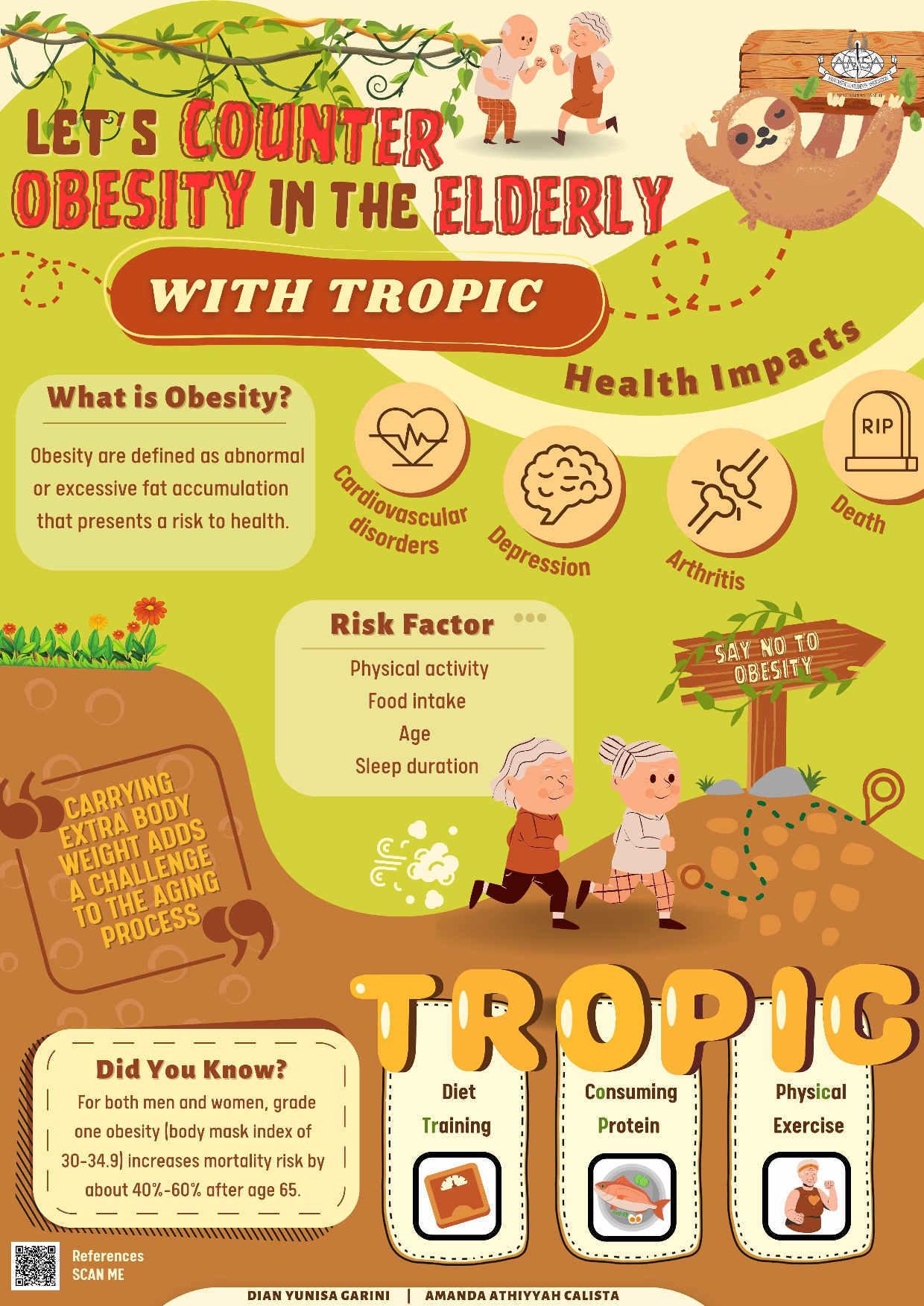





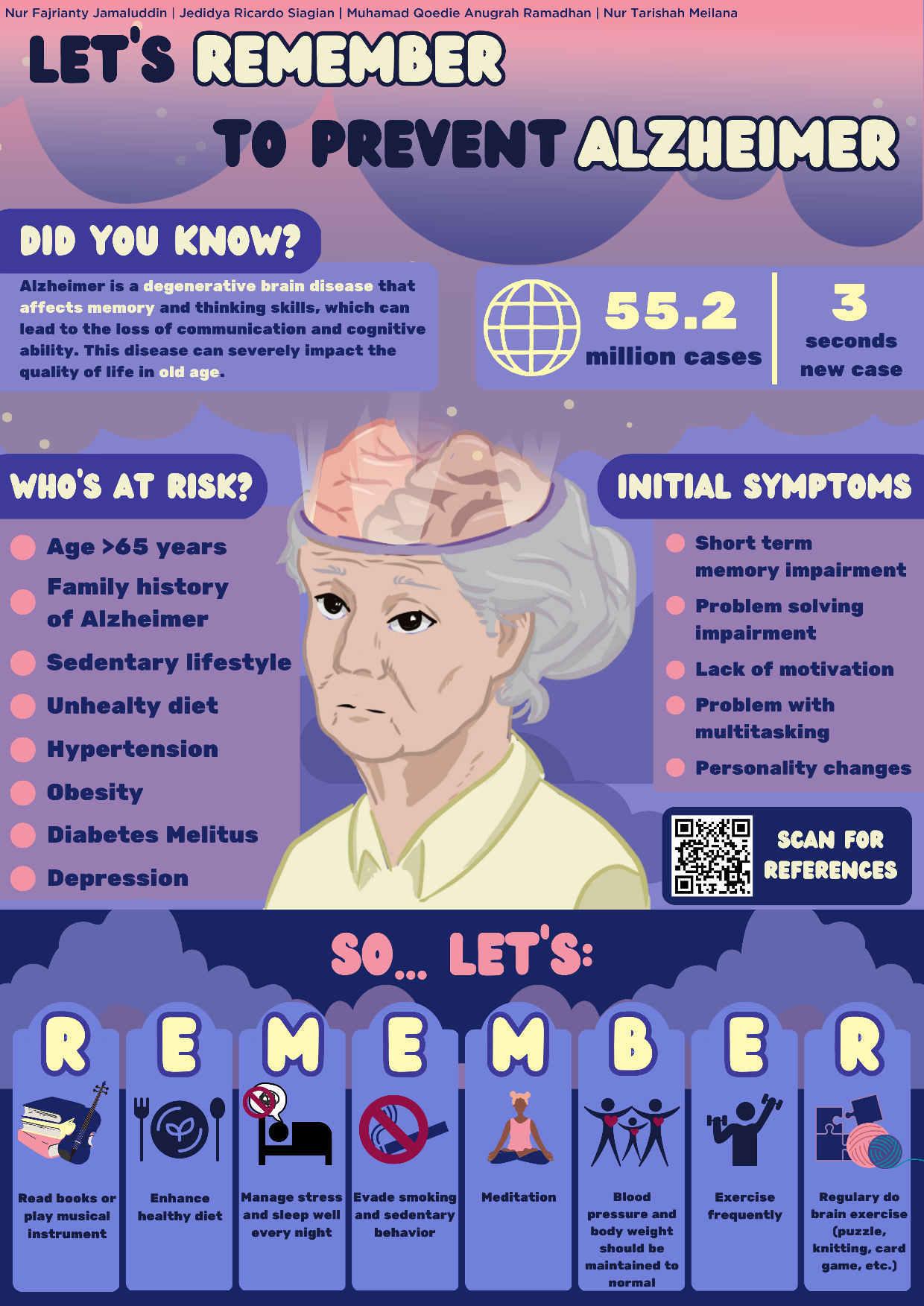 RochelleDeMelloWahyudi,DerrenD.C.H.Rampengan,ArnoldKeane
RochelleDeMelloWahyudi,DerrenD.C.H.Rampengan,ArnoldKeane