FALL 2019
UB Medicine Connecting alumni, friends and community
jacobs School of Medicine and Biomedical Sciences University at Buffalo
UB Innovators Are Thriving
o ol
Sp
e
n ch e T ue al Iss i c
gy
Photos by Nancy J. Parisi
Teresa Quattrin, MD, UB Distinguished Professor and senior associate dean for research integration in the Jacobs School of Medicine and Biomedical Sciences, helps a child suit up as a “Research Ranger”.
Mom Ruth Shakkour, Sophie Shakkour (in turquoise-colored “Research Ranger” gear), and Ella Shakkour (in orange).
Capes, coloring books welcome littlest
‘Research Rangers’
By ellen goldbaum
On a recent sunny morning at Canalside next to the Buffalo River, more than a hundred Western New York children gathered to learn about scientific and medical research. The children, along with their parents, camp counselors and caregivers, were attending Storytime at Canalside, sponsored by Every Person Influences Children (EPIC). EPIC is a member organization of the community advisory board of the UB’s Clinical and Translational Science Institute (CTSI). With the theme of “Summer STEM” (science, technology, engineering and mathematics), the event focused on explaining scientific research to the 13-and-under crowd. Children and adults learned how they could be part of medical breakthroughs in Buffalo, courtesy of UB scientists and staff. The CTSI table featured fun, interactive displays explaining the scientific method. Children received colorful capes identifying them as “research rangers,” as well as informative coloring books called “Sofia Learns About Research,” created by UB’s clinical researchers and designed to educate them and their parents about clinical research and how they can participate. Available in English, Spanish and Arabic versions, in collaboration with the International Institute of Buffalo, the coloring book tells the story of Sofia, a little girl who has asthma. “Our goal is for children and their parents to learn about clinical research and share in the excitement of the clinical research going on in Buffalo right now,” said Teresa Quattrin, MD, UB Distinguished Professor and senior associate dean for research integration in the Jacobs School of Medicine and Biomedical Sciences. “We know from our work in pediatric research how difficult it is to recruit children and other underrepresented populations to clinical research,” she said. “We know it can be a very difficult decision for a parent to consider enrolling their child in a clinical research trial, but there can be such important benefits to enrolling, too. So we decided, why not write a children’s book?” The book was co-written by Quattrin; Renee Cadzow, an anthropologist at D’Youville College and researcher at UB; and Alexandra Marrone, previously a research assistant, now a UB medical student. Illustrations are by Isabella Bannerman, an award-winning cartoonist currently based out of New York City; graphic design is by Tia Canonico. Copies of “Sofia Learns About Research” can be obtained by contacting the CTSI Special Populations team at 716-829-6144 or sofiactsi@buffalo.edu.
T A B L E O F C o n te n t s
UBMedicine
UB MEDICINE MAGAZINE, Fall 2019, Vol. 7, No. 2
Michael E. Cain, MD Vice President for Health Sciences and Dean, Jacobs School of Medicine and Biomedical Sciences Eric C. Alcott Associate Vice President for Advancement, Health Sciences, Senior Associate Dean of Medical Advancement
2 Vital Lines Progress notes
Editorial Director Christine Fontaneda Executive Director of Medical Advancement
26 Doctor Visits Reflections on careers
Editor Stephanie A. Unger
28 Pathways
Contributing Writers Gina Marie Ciappina, Lori Ferguson, Ellen Goldbaum, Dirk Hoffman, Charlotte Hsu, Cory Nealon, Grove Potter, Marcene Robinson, Mark Sommer
People in the news
Copyeditor Tom Putnam
32 Q & A
Photography Joe Casio Sandra Kicman Meredith Forrest Kulwicki Nancy J. Parisi Douglas Levere
UB Medicine is published by the Jacobs School of Medicine and Biomedical Sciences at UB to inform alumni, friends and community about the school’s pivotal role in medical education, research and advanced patient care in Buffalo, Western New York and beyond. Visit us: medicine.buffalo.edu/alumni
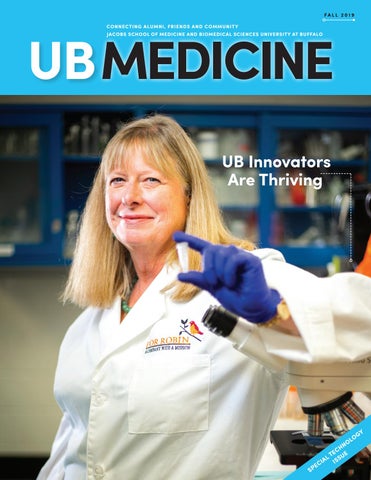
Cover Image Kate Rittenhouse-Olson, PhD, resigned her position as professor in the Jacobs School of Medicine and Biomedical Sciences in 2017 to grow For Robin Inc., a cancer therapeutics company she launched in 2012 with the support of UB. The company, named in memory of her sister, who died of breast cancer, is poised to begin clinical trials. Photo by Douglas Levere
10
Photo by Douglas Levere
Conversations with experts
Lauren Shepard, left, and Ariana Allman creating 3D models of the vascular system in a multidisciplinary effort led by biomedical engineer Ciprian “Chip” Ionita, PhD, and neurosurgeon Adnan Siddiqui, MD, PhD.
Art Direction & Design Karen Lichner Editorial Adviser John J. Bodkin II, MD ’76 Affiliated Teaching Hospitals Erie County Medical Center Roswell Park Comprehensive Cancer Center Veterans Affairs Western New York Healthcare System
6 One-man research catalyst
Kaleida Health Buffalo General Medical Center DeGraff Memorial Hospital Gates Vascular Institute John R. Oishei Children’s Hospital Millard Fillmore Suburban Hospital
8 A scientist’s remarkable resolve
Catholic Health Mercy Hospital of Buffalo Sisters of Charity Hospital
Jeff Harvey, philanthropist and entrepreneur, has partnered with UB to launch two startups based on faculty research discoveries.
Researcher launches For-Robin Inc. cancer therapeutics company in memory of her sister, who died of breast cancer.
10 operating with a net
UB team uses 3D printing to create models of the human vascular system to help surgeons prepare for complex operations.
12 Drug development paradigm shift
Correspondence, including requests to be added to or removed from the mailing list, should be sent to: Editor, UB Medicine, 916 Kimball Tower, Buffalo, NY 14214; or email ubmedicine-news@buffalo.edu
Biotechnology company launched by UB faculty is designed to cut in half the time and money needed for preclinical trials.
FALL 2019
UB Medicine
1
U B M E D v i tal l i n e s
Match Day 2019
Photos by Sandra Kicman
Medical students in the Class of 2019 at the Jacobs School of Medicine and Biomedical Sciences celebrated the next steps in their careers during Match Day, held on March 15 in Statler City’s Golden Ballroom in downtown Buffalo. More than a quarter of the class—42 students—have chosen to stay at UB for advanced training. To learn where all members of the class will train, visit medicine.buffalo.edu and search “Match Day 2019.”
From left, Ayobami Fatunmbi, Danielle Dickson and LaVerne Thompson are all smiles as they anticipate the opening of their envelopes.
From left, Joseph Iluore, Mark Lawlor and Nicholas Kurek celebrate their Match Day residency placements.
Graduation Day 2019
Photos by Sandra Kicman
The Jacobs School of Medicine and Biomedical Sciences held its 173rd commencement ceremonies in May in the Center for the Arts on UB’s North Campus. During the ceremonies, 152 students received medical degrees, including nine MD/MBA degrees; five MD/PhD degrees; two MD/DDS degrees; and one MD/MPH degree. Twenty-nine doctoral, 36 master’s and 154 baccalaureate candidates were eligible to receive degrees in biomedical science fields during the May commencement ceremony.
Steven Fliesler, PhD, Meyer H. Riwchun Endowed Chair Professor, Vice-Chair and Director of Research, Department of Ophthalmology, left; and Sriganesh Ramachandra Rao, who earned his PhD in biochemistry.
2
FALL 2019
UB Medicine
Celebrating graduation is Penpa Bhuti, who will train in internal medicine at Icahn School of Medicine at Mount Sinai.
Chevli Named Chair of Urology K. Kent Chevli, MD, has been appointed professor and chair of the Department of Urology in the Jacobs School of Medicine and Biomedical Sciences and president of the UBMD Urology practice plan. Chevli, president of Western New York Urology Associates and Cancer Care of Western New York, has served as chair of the Great Lakes Health Professional Steering Committee and as director of Kaleida Health’s oncology services. A volunteer faculty member in the Department of Urology since 1997, Chevli completed his residencies in surgery and urology at the University of Louisville School of Medicine. He earned his medical degree from Saint Louis University School of Medicine and an undergraduate degree in chemical engineering from Washington University in St. Louis. In his new role, Chevli is working to develop and strengthen partnerships with other university departments and with industry
sponsors. In collaboration with Stanley Schwartz, MD, PhD, UB Distinguished Professor, Medicine and Pediatrics, and division chief, allergy-immunologyrheumatology, Department of Medicine; and Ravikumar Aalinkeel, PhD, research associate professor of medicine, in the UB Clinical and Translational Science Institute, he is working to provide vital pathological samples to further research on the behavior, diagnosis and treatment of prostate cancer. Chevli is a past recipient of the Department of Urology’s Faculty Teaching Award.
Chevli
Hopkins Receives Norton Medal L. Nelson Hopkins, MD, SUNY Distinguished Professor of Neurosurgery, has been awarded the 2019 Chancellor Charles P. Norton Medal, UB’s highest honor. As one of the founding figures of endovascular treatment for neurovascular disorders, Hopkins has redefined the field of vascular neurosurgery in stroke management and lesion stenting. In the process, he has trained a new generation of neurosurgeons in catheter-based technology for minimally invasive neurosurgery. Hopkins’ innovations in endovascular surgery serve as the benchmark for therapeutic endovascular intervention. An advocate of cross-specialty collaboration, Hopkins fostered the creation of UB’s Toshiba (now Canon) Stroke & Vascular Research Center. He also conceived a new way to organize the multidisciplinary treatment of vascular disease, Jeremy M. Jacobs, left, presenting Norton Medal to Hopkins working with experts from around the world to design the Gates Vascular Institute. Hopkins then recruited the necessary Hopkins has served on the board of directors of the American partners to bring it and the Jacobs Institute — a non-profit Association of Neurological Surgeons (AANS) and on the executive dedicated to accelerating the development of next-generation committee of the Stroke Council of the American Heart Association. technologies in vascular medicine — to life. A past president of the American Academy of Neurological Surgery, He currently is chief scientific officer of the Jacobs Institute, he is a former chair of the scientific and annual meetings of AANS after serving as chair of the UB Department of Neurosurgery and the Congress of Neurological Surgeons, and of the Joint Section from 1989-2013. He joined the UB faculty in 1975. on Cerebrovascular Surgery.
FALL 2019
UB Medicine
3
U B M E D v i tal l i n e s Spring Clinical Day and Reunion Weekend 2019
Alumni came from around the country this spring to celebrate with classmates, friends, faculty and students. More than 400 people joined in the festivities, which included tours of the Jacobs School of Medicine and Biomedical Sciences’ building, Spring Clinical Day and presentation of the Distinguished Alumnus and Volunteer awards, an alumni cocktail party and class dinners. The weekend was sponsored by the UB Medical Alumni Association and the Jacobs School.
Reunion Weekend keynote speaker was Robert J. Gore, MD ’02, Founder and Executive Director, Kings Against Violence Initiative; 2018 CNN Hero; Emergency Department Physician, SUNY Downstate Medical Center and NYC Health+ Hospitals/Kings County, Brooklyn, NY. Pictured, left to right: Sherice Simpson, Class of 2022; Shawn Gibson, Class of 2022; Robert Gore, MD ’02; Shanice Guerrier, Class of 2022; Jarrett White, Class of 2022.
4
FALL 2019
UB Medicine
First row, left to right: Thomas Joly, MD ’89, PhD; Alan Malabanan, MD ’89; Scott Bookner, MD ’89; Daniel Chueh, MD ’89. Second row, left to right: Lee Guterman, MD ’89, PhD; Raghu Ram, MD ’90; Richard E. Ferguson, MD ’89; Young B. Huh, MD ’89; Geoffrey Karl Seidel, MD ’89; Barbara BambachSkomra, MD ’89; Christopher J. Skomra, MD ’89; Sharon Zeigler, MD ’90; Eric R. Southard, MD ’89; A. Kristina E. Hart, MD ’89; Dawn A. Gais, MD ’89; Raul Vazquez, MD ’89 (class chair); Alison R. Moliterno, MD ’89; Kara M. Kelly, MD ’89.
Photos by Joe Cascio
First row, left to right: Darlene Dzik, MD ’94; Maya Srivastava, MD ’94; Priya Srivastava; Idalia Gonzalez, MD ’94; Carol Ann Killian, MD ’94; Donna Gail Ferrero, MD ’94; Stephanie Edwards, MD ’94; Kim Strong Griswold, MD ’94; Tegest Hailu, MD ’94; Petros Ghermay, MD ’94. Back row, left to right: John Dzik, MD ’93; Julie Wood; Christopher Wood, MD ’94; Thomas Burnette, MD ’94; Atif Zafar, MD ’94; James Chmiel, MD ’94.
Left to right: Daniel Vekhter, MD ’14; Sara Neimanis, MD ’14; Rachel Aliotta-Bloom, MD ’14; Andrew Bloom, MD ’14; Anchara Vivek, MD ’14; Benjamin Verplanke, MD ’14.
Startup Bootcamp! UB students take on surgical problem
O
n July 15, five teams of University at Buffalo students who did not know each other came together in a startup boot camp called UB BLAST to devise solutions to the devastating and costly surgical complication of anastomotic leaks. Such leaks, occurring after some colorectal surgeries, are difficult to detect early. The consequences are severe: an ostomy bag for life, sepsis or even death. The potential market could be worth $2.5 billion. Students had five days to develop a solution and a startup. Along the way, these medical, business and engineering students learned to suture and use robotic instruments, do business plans, conduct patent searches and create a brand complete with a 3D printed logo. They learned from local and international startup gurus and mentors, dedicated UB surgery residents and each other. When they started out, most students didn’t know what an anastomotic leak was. By week’s end, judges evaluated a range of elegant solutions using technologies like smart paper, gold nanoparticles, biomarker assays, radiofrequency ID and hydrogel membranes. The idea came from a program called Business Engineering and Surgical Technologies (BEST) held in Strasbourg, France. Steven Schwaitzberg, MD, professor and chair of surgery in the Jacobs School of Medicine and Biomedical Sciences at UB and the founding director of UB BLAST, was keynote speaker there last summer. While BEST recruits globally, Schwaitzberg realized he had a talented, energetic pool of students to recruit from at UB as well as state-of-the-art facilities in the Jacobs School.
B y E l l e n G ol dba um
“UB’s medical school building in and of itself is an innovation hub,” said Schwaitzberg. During BLAST, students learned procedures in the Amin Tjota, MD, PhD ’91, Melawati Yuwono, MD, and Tjota Family Advanced Procedures Suite, and in UB RISE, the Jacobs School’s full-service medical training and surgical simulation center. RISE stands for Research, Innovation, Structural, Simulation, Education and Engineering. The winning startup was Limitless, which created a device that measures the pH of fluid leaking as a warning sign of a problem. The team, which went on to form — Steven Schwaitzberg, MD, an LLC, has applied for a professor and chair of surgery provisional patent and will now skip the initial rounds of the Henry A. Panasci, Jr. Technology Entrepreneurship Competition and advance straight to the semifinals next March. But the birth of a new startup is only the beginning, says Schwaitzberg. “The story is the struggle. It was the crucible of real life: ‘I need more time. You can’t have more time.’ ‘I need more resources. You don’t have enough money or manpower.’ The final innovations were so much better than we imagined. “The real story is that these kids started out saying ‘I can’t do this in a week’—and then they did.” To read more, go to medicine.buffalo.edu and search “UB BLAST.”
“The final innovations were so much better than we imagined.”
medical student publishes research in prestigous journal Alison Treichel, Class of 2020, is the first UB medical student to receive a Doris Duke Charitable Foundation Clinical Research Mentorship Program award. She took a year out of medical school in 2019 to participate in the full-time clinical research experience. Her manuscript, “Phenotypic distinctions between mosaic forms of tuberous sclerosis complex,” was published in the May 22, 2019 issue of Nature’s journal Genetics in Medicine. Treichel previously took a year out of medical school to serve as a fellow in the Medical Research Scholars Program that places students in National Institutes of Health laboratories and patient care areas to conduct basic, translational or clinical research in areas that match their career interests and goals. “My past two years of research at the National Institutes of Health have been an amazing experience,” Treichel says. “I look forward to returning to Buffalo to finish my fourth year of medical school.”
FALL 2019
UB Medicine
5
{
Innovators Editor’s note: In this issue of UB Medicine, we tell the stories of Innovators in the Jacobs School of Medicine and Biomedical
}
Sciences and describe how they are tapping into an “entrepreneurial ecosystem” at UB and in Buffalo that is designed to help them
move their ideas from the laboratory into clinical practice as rapidly as possible. Because space does not allow us to tell all the Jacobs School success stories, we focus this issue on Innovators who are currently in the process of commercializing their discoveries. These
researchers would be the first to credit UB’s early spin-off companies such as ONY Inc., Athenex, and Empire Genomics with helping UB to establish an entrepreneurial support system that streamlines this complex process. As a result, Jacobs School Innovators—past
and present—are putting UB and Buffalo on the map as a place where creative biomedical endeavors are supported and celebrated. —S.A. Unger
A One-Man Research Catalyst Jeff Harvey, philanthropist and entrepreneur, is on a personal mission
W
hen medical tragedies struck Jeff Harvey’s family, he asked questions, found brilliant scientists at the University at Buffalo who were conducting remarkably pertinent research and started a new company—twice.
When his grandson was diagnosed with Duchenne muscular dystrophy (DMD) in 2008, Harvey—a finance professional who holds a master’s degree in nuclear engineering from the Massachusetts Institute of Technology—was determined to do what he could to help. He read research studies, attended seminars and, being a Buffalo native, he found a scientist in the Jacobs School of Medicine and Biomedical Sciences who was an internationally renowned expert on something called ‘mechanosensitive ion channels.’ “I figured there had to be someone at UB working on this,” Harvey says. “So I literally typed into Google ‘UB muscular dystrophy’ and up came Fred Sachs’ name. It was like ‘Wow!’” What Harvey learned is that Frederick Sachs, PhD, SUNY Distinguished Professor, and his group had found a peptide in tarantula venom called GsMTx4 that closes off mechanosensitive ion channels. They further discovered that closing these channels helps delay the muscle-destroying activity of muscular dystrophy. Harvey approached Sachs and his research partners, Thomas Suchyna, PhD, an assistant professor, and Philip Gottlieb, PhD, an associate professor, both in the Department of Physiology and Biophysics, and proposed forming a company to bring the peptide to market. The company, called Tonus Therapeutics, licensed the GsMTx4 peptide from UB.
6
By Grove Potter
FALL 2019
UB Medicine
No Other Drug Like This Tonus Therapeutics is built upon fundamental, potentially farreaching science that explores the impact of mechanical forces on cell membranes, which is basically a new field in cell science. “Never underestimate the power of luck,” says Sachs, a longtime professor of physiology and biophysics at UB. “When we discovered mechanosensitive ion channels, it was an accident. We were just looking at a chick muscle membrane, and it showed up when we didn’t expect it. There was no data on these things before we discovered them.” When you touch something, signals are sent to the brain to inform you that this contact is taking place. How? Sachs’ discovery of mechanical sensors in cells gave an explanation. “It turns out, every cell in your body is generating mechanical signals,” he explains. “The most familiar are things such as hearing and touch.” Normal cells absorb mechanical forces due to a web of stringlike material under the membrane called dystrophin. In muscular dystrophy patients, a defective gene thwarts the formation of dystrophin and thus removes the protective web from the membrane. Force is then hitting the unsupported membrane and the ion channels open. This allows calcium to flow in and break down the tissue.
Photo by Douglas Levere
From left: Jeff Harvey, Hui Meng, PhD, and Vincent Tutino, PhD, founders of Neurovascular Diagnostics
The peptide that Sachs’s group discovered in spider venom closes the ion channels. “It seemed to me there were a lot of clinical applications for it,” he says, “but no companies were ready to commit to invest in its development as a pharmaceutical.” So when Harvey called, Sachs was ready to pursue a startup company. A retired stock broker, Harvey has found that the drug-development business moves at a slower pace than what he’s accustomed to. “Everything takes longer than you think, and a lot more money,” he observes. Having been drawn to the industry by personal tragedy, the lack of immediate progress has been discouraging at times. “We’re all frustrated and disappointed that somebody didn’t grab this [peptide] four or five years ago and run with it,” Harvey reflects. “We think it’s a very good solution to help these kids.” If the drug is approved, Harvey thinks it can double the lifespan of DMD patients from about 25 years to 40 or 50 years and help them live better lives. “There’s no other drug like this,” he says.
On Track The GsMTx4 peptide is currently undergoing detailed toxicity testing for an investigatory new drug application to the U.S. Food and Drug Administration (FDA). If successful, this will be followed by Phase I/II studies in humans by 2020. Now made by chemical synthesis, GsMTx4 is an orphan drug, a designation that the FDA awards to promising therapies for rare diseases. “Remarkably, we saw no side effects in the mice in the current study, nor in ferrets in a previous study on cardiac disease, despite the fact that mechanosensitive piezo channels—the drug’s target —are ubiquitous in living organisms,” said Sachs. The drug also has a long half-life, so that subcutaneous injection may be needed only once a week. The researchers conclude that GsMTx4 may also complement other therapies, such as anti-inflammatory agents and gene replacement strategies that are being prescribed or studied in DMD.
Another Challenge, Another Company Tragedy had struck Harvey eight years earlier when his wife suffered two brain aneurysms and passed away in 2002. His reaction was the same. He asked big questions and got involved. He joined the board of directors of the Brain Aneurysm Foundation, where he established a fund in his wife’s memory, the Carol W. Harvey Memorial Chair of Research. By chance, a UB research team had received grants from the fund for three consecutive years, and Harvey found their work extremely interesting. That team—Hui Meng, PhD, professor of mechanical and aerospace engineering and neurosurgery, and her PhD student, Vincent Tutino, were developing a low-cost blood test to detect unruptured brain aneurysms. Tutino explains that their research started with a bold hypothesis: that the inflammation caused by a brain aneurysm would create some type of biomarker in the blood that could be detected. By pursing this hypothesis, they discovered differences in Continued on page 31
FALL 2019
UB Medicine
7
Photo by Douglas Levere
Innovators
Kate Rittenhouse-Olson, PhD, founder of For-Robin Inc.
A Scientist’s Remarkable Resolve
Promising cancer drug developed in memory of researcher’s sister
By Charlotte Hsu
T
he name of Kate RittenhouseOlson’s cancer therapeutics company is For-Robin Inc.
It’s an appellation that honors the memory of her sister, a bright young woman who loved flowers, baked a mean chocolate silk pie and gave the teenagers she worked with as a counselor in Pittsford, N.Y., the dose of tough love they needed to get through difficult times in their lives. Robin died of breast cancer in 1986 at the age of 31. At her funeral and after, young people told stories about how Robin’s guidance kept them alive—away from drugs, out of trouble, and hopeful for the future. At the time of Robin’s passing, Rittenhouse-Olson was a postdoctoral researcher in the Jacobs School of Medicine and Biomedical Sciences, and she resolved to learn as much as she could about cancer with the goal of fighting it one day. She subsequently joined the faculty in the Department of Biotechnical and Clinical Laboratory Sciences in the
8
FALL 2019
UB Medicine
Jacobs School, where she worked for several decades and rose to the rank of professor. In 2012, Rittenhouse-Olson’s cancer-research aspirations came to fruition when she became the founding president of For-Robin Inc., a company developing a promising drug designed to stop breast cancer tumors from metastasizing to other parts of the body. The therapy is based on years of research in RittenhouseOlson’s UB lab, including projects funded by approximately $2.7 million in awards from the National Cancer Institute’s Small Business Technology Transfer program. In 2017, Rittenhouse-Olson resigned her faculty position in the Jacobs School to focus full-time on the company.
The hJAA-F11 Antibody For-Robin’s drug is hJAA-F11, an antibody that fights cancer by binding to and blocking the activity of an important carbohydrate found on tumor cells, the ThomsenFriedenreich antigen. Normally, this antigen aids cancer
of hJAA-F11. This validation has been successfully completed and cells in metastasizing. By obstructing this function, hJAA-F11 helps represents third-party confirmation that is important to investors prevent the spread of tumors. and potential pharmaceutical partners. Among other things, The antibody also fights cancer in two other ways: First, it flags the NExT partnership will result in the NCI producing enough tumor cells as dangerous objects for the body to destroy. Second, hJAA-F11 for use in safety testing in animals and in human clinical the antibody can be linked to and deliver a chemotherapeutic agent trials, a process that requires highly specialized facilities capable such as maytansine directly into cancer cells. of producing the pure antibody in large quantities. After the Rittenhouse-Olson’s team has shown that hJAA-F11 can kill successful completion of these milestones, the NCI will assist human breast cancer cells in human tumors grafted into mice, For-Robin in filing an investigational new drug application with while leaving healthy, noncancerous cells unharmed. The Forthe U.S. Food and Drug Administration, a precursor to human Robin lab has recently shown that hJAA-F11 also kills human nonclinical trials. small cell lung cancer and small cell lung cancer engrafted For-Robin estimates that it would have cost the company about into mice. $4 million to complete these activities without the NExT program’s The antibody also shows promise for treating an array of other support. cancers. When For-Robin scientists tested hJAA-F11 on cancerous “If testing and protissues from 1,269 cases duction are successful, the of breast, lung, prostate, NExT program will bring us colon, bladder and ovarian right to the point where we cancer, the drug reacted will be ready to test the drug with about 85 percent of in people fighting cancer,” the specimens, including says Rittenhouse-Olson. “It’s 94 percent of the triplea very selective program, so negative breast cancers. we feel very fortunate to be Rittenhouse-Olson says – Jeff Dunbar, director of Technology Transfer a part of it.” her sister likely died from “Drug discovery is this aggressive form of the an expensive process, disease, which does not and safety testing and respond to three common drug production are some of the hardest parts to get funded,” types of treatments available on the market today. explains Christina Orsi, UB associate vice president for economic “Robin died 33 years ago at a young age, and triple-negative development. “The support from the National Cancer Institute’s cancer is more prevalent in young women like that. For this NExT program is a testament to the promise of For-Robin’s therapy. population, the only thing that really works is hard-core The company’s progress shows how discoveries made in UB labs chemotherapy. Our antibody may be able to give these patients an can benefit society.” additional option.” As For-Robin advances through NExT, the company is seeking to partner with a larger pharmaceutical firm or raise funds from Backed by UB from the Start investors for human clinical trials. UB has backed For-Robin since the company’s early days. In April 2019, For-Robin received an NCI grant that supports a The university assisted the company in filing its successful study that will explore the use of the hJAA-F11 antibody as an aid for patent application and it funded research on hJAA-F11 through the differential diagnosis of lung cancer after indeterminate spots the Bruce Holm Memorial Catalyst Fund and UB Center for are seen on CT scans and chest X-rays. Advanced Technology in Big Data and Health Sciences (UB CAT). UB also provided Rittenhouse-Olson with business coaching as she Driven to Help People transitioned from being an academic into an entrepreneur. “Kate’s commitment to realizing the potential of the hJAA-F11 The memory of her sister, and the desire to help people like her, is discovery to help cancer patients is exemplary of all of UB’s what drives Rittenhouse-Olson. That philosophy—of wanting to aspiring entrepreneurs,” says Jeff Dunbar, director of Technology help—is ingrained in her company as well. Transfer, who has worked extensively with For-Robin since its “I’m really happy to help with Kate’s dream,” says John Fisk, founding. PhD, a senior scientist at For-Robin who earned his doctorate in In 2018, For-Robin marked two major milestones in the microbiology at UB. “She is selfless. Her commitment to her product development of its therapy: It was granted a U.S. patent, and it was and her desire to see this get to the next stage are all driven by her selected to join the National Cancer Institute’s (NCI) Experimental desire to help people, and that is something that I can get behind Therapeutics Program. Referred to as NExT, this highly competitive wholeheartedly.” program facilitates a partnership between the NCI and For-Robin, “Our goal is—and has always been—to bring our product from with the goal of moving the company’s cancer therapy toward the bench to the bedside, to the cancer patient,” says James Olson, clinical trials in humans. PhD, For-Robin vice president, who is a professor of epidemiology and environmental health in UB’s School of Public Health and Health Professions and professor of pharmacology and toxicology A Testament to For-Robin’s Promise in the Jacobs School. “After a successful NExT partnership, we will The first step in the NExT milestone-driven partnership with be ready to move on to the next step, which is human clinical trials.” For-Robin was their validation of the tumor targeting potential
“Kate’s commitment to realizing the potential of the hJAA-F11 discovery to help cancer patients is exemplary of all of UB’s aspiring entrepreneurs.”
FALL 2019
UB Medicine
9
Innovators
Operating with a Net UB team uses 3D printing to create models of vascular system, help prepare surgeons By Gina Marie Ciappina
A
team of biomedical engineers, neurosurgeons and cardiovascular interventionists in the Jacobs School of Medicine and Biomedical Sciences has devised a way to generate 3D prints of the human vascular system, giving surgeons a reliable preview of what they will encounter in the operating room before a scalpel touches skin. Developed by Ciprian “Chip” Ionita, PhD, assistant professor of biomedical engineering and neurosurgery, and Adnan Siddiqui, MD, PhD, professor of neurosurgery, the method that creates 3D prints is being used to better prepare physicians who perform intricate surgeries to treat such conditions as stroke, aneurysms, cardiac arrest and congestive heart failure. “The whole idea of these 3D-printed models is to not only mimic patient anatomy, but to also mimic some of their vascular mechanical properties,” says Ionita, who holds joint appointments in the Jacobs School and in the School of Engineering and Applied Sciences. Before 3D printing, the lifelike models were complicated to make and had to be shipped from Switzerland at a cost of more than $12,000 each. Now, each model costs about $100 and can be customized for individual patients. Ionita and Siddiqui began their 3D-printing research when the UB Clinical and Translational Science Institute and Kaleida Health’s Gates Vascular Institute were co-located in a building that included specially designed “collision spaces” to facilitate collaborations between engineers, physicists and vascular surgeons. “We are now able to optimize our research by meeting every day and working together,” says Ionita, who is also working with engineers at the UB Center of Excellence in Bioinformatics and Life Sciences to enhance the mechanics of the models and make them even more lifelike.
Simulates Elasticity of Arteries The 3D-printed models are built to scale for a patient’s arteries and are often referred to as “phantoms.” The models are warmed up during surgical practice sessions to simulate the gummy elasticity of arteries within a vascular system and to allow the devices, fabricated with shape-memory alloys, to behave the same as human arteries.
10
FALL 2019
UB Medicine
“We are trying to help surgeons who have really difficult cases and have doubts about the approach,” Ionita says. “They have us make a model and then they come to the lab for surgical planning and practicing and to make decisions.” From the moment a patient arrives at the hospital to the completion of post-surgery analysis for research purposes, the entire biomedical team works together to treat his or her condition. The models are also used to educate medical students and to train residents. Ionita says students receive a better education by witnessing the decision-making process, all the way from a patient scan to surgery. “Without ongoing interactions between the researchers and the surgeons, meaningful medical work can’t be done,” he says.
Customized, Economical, Made In-House The 3D printing process starts when a patient receives a diagnosis, Ionita explains. “They give us problems, then we try to solve them.” Next, a scan of the diseased area is taken through 3D medical imaging. A process called segmentation—the selection and isolation of the structure of interest—is collected and analyzed. Once a specific segment is located, engineers create a 3D geometry and put it into secondary software to manipulate before printing the model. The model is then 3D-printed in-house, which can take from 20 minutes to 20 hours, depending on how complex and precise it needs to be and the different types of material being used. Materials can be combined for a single print to get the correct texture, Ionita explains. Rubber silicone mimics blood vessels the best and is used the most for prints.
Photo by Douglas Levere
Biomedical engineer Ciprian “Chip” Ionita, PhD, with 3D prints of the human vascular system
establish an extensive database of brain and Depending on the patient, the print can be heart vascular scans compiled from ongoing used to understand hemodynamics, validate clinical trials. This large database will have medical software, test devices or create a the potential to speed up testing of new surgical plan. devices or procedures. When treating a patient who is very “The whole idea is for us to understand high risk or requires a novel procedure, the more in physician depth how and his or a patient’s her team vascular head to structure Ionita’s lab, interacts where they with the practice on devices and the patientblood flow specific and why, for model to example, one develop a – Ciprian “Chip” Ionita, PhD person fully customized recovers from surgical an aneurysm after six months and another plan. How they want to approach the model patient does not,” says Ionita. determines their steps. If it does not work “At the end of the day, it’s about a patient’s on the model, Ionita says, they adjust the surgeon’s plan and keep track of the changes. specific geometry and vascular mechanics, or the difference between two patients.” “There was a case where a surgeon made Lauren Shepard, Ionita’s student assistant, changes to 70 percent of the steps he was studies how to use the 3D prints to better going to do originally,” Ionita recalls. “Based understand the flow and pressure conditions on his work with the model he decided to use within a patient’s diseased arteries. In one different devices and stiffer wire.” experiment, she is trying to understand how The biomedical engineering team plans to
“The whole idea of these 3D-printed models is to not only mimic patient anatomy, but to also mimic some of their vascular mechanical properties.”
variants in the brain vasculature affect the pressure gradients, or flow. At the bottom of the skull there is a vascular structure called the circle of Willis, which connects the anterior circulation to the posterior circulation. “It is almost like a vascular safety feature to make sure—in case one of the arteries gets blocked—your brain still gets blood supply from the other arteries,” says Ionita. People who have vascular stenosis—a narrowing of the vessel—can be asymptomatic and unaware they have a vascular disease, while others are severely symptomatic. Only 28 percent of people have a full circle of Willis, however, and Ionita’s team is studying how this variation affects the blood in the vessels leading to the brain. The team also is trying to determine the metrics of patients’ risk level when they come into the hospital, which is extremely important for classifications. In the cardiac equivalent of this study, conducted in collaboration with Vijay Iyer, MD, PhD, clinical associate professor of medicine, and Michael Wilson, medical director for cardiac CT at Kaleida Health, researchers examined how catheter-lab measurements of pressure gradients across coronary arteries correlated with measurements in the lab. “This was the first clinical trial of its kind, where they were trying to replicate a study in humans with 3D-printed, patientspecific benchtop models,” Ionita says. “We concluded the study early because we found a significant correlation between the measures of flow from the model to the measures of flow from patients.” Building on the success of this investigation, Ionita and his team are now exploring similar neuro-applications. He predicts that 3D printing will become standard in all medical fields in the near future and reports that radiology departments across the country are adopting 3D printing as a new 3D medical imaging representation. Due to increased acceptance, 3D printing became a reimbursable tool in June 2019, allowing doctors to use it for better diagnosis and treatment planning for high-risk patients. “There is no better tool than 3D printing to replicate patient anatomy,” concludes Ionita. “As a team, we hope to achieve safer surgeries with fewer complications and, ultimately, save lives.”
FALL 2019
UB Medicine
11
Photo by Sandra Kicman
Innovators
Faculty members Randall L. Rasmusson, PhD, left, and Glenna C. Bett, PhD, co-founded Cytocybernetics.
Drug Development Paradigm Shift
UB professors’ technology changes methods for drug screening
By Cory Nealon and Charlotte Hsu
12
N
ew drugs to treat heartburn, allergies, mental disorders and other maladies are constantly under development, but ensuring they do not have unwanted side effects on the heart is difficult. Pharmaceutical companies may spend years and hundreds of millions of dollars only to have a drug fail, often because it disrupts the electrical activity of the heart and causes heart attacks. A company launched by two faculty members in the Jacobs School of Medicine and Biomedical Sciences is quietly upending this paradigm by providing a very welcome alternative to the traditional method for drug screening. The company, called Cytocybernetics, developed new biotechnology called the Cybercyte that is designed to cut in half the time and money needed for preclinical trials. It was co-founded in 2013 by Glenna C. Bett, PhD, vice chair for research and associate professor in the Department of Obstetrics and Gynecology; and Randall L. Rasmusson, PhD, professor in the Department of Physiology and Biophysics. Currently, each drug brought to market costs about $500
FALL 2019
UB Medicine
million in the preclinical trial phase. Cybercyte could cut up to two-thirds of the time and money—more than $300 million per drug and years off the timeline. “Technological innovation has the potential to improve all facets of our lives—everything from our health and well-being, to the creation of new industries, companies and jobs,” says SUNY chancellor Kristina M. Johnson. “Cytocybernetics is well on its way to positively impacting cardiac research, and that is validated by the team recently receiving the highly competitive Small Business Technology Transfer award from the National Heart, Lung, and Blood Institute to advance their product development and commercialization efforts.”
High-throughput screening The Cybercyte—Cytocybernetics’ core technology— uses mathematical modeling and high-speed computer interfaces to deliver an electric current that flows through heart cells grown in the lab. This methodology accurately
models the electrical activity of heart cells within the human body, enabling scientists to test how different drugs influence the function of the cells and, ultimately, the heart. It’s a futuristic technology that blends electronics with biology, reminiscent of Star Trek’s cybernetic Borg. As the Cybercyte interacts with cells, it feeds researchers real-time data showing how the cells are behaving. The company’s technology, developed by Bett, solves some key problems that scientists encounter when evaluating the cardiac safety of new pharmaceuticals. First, the Cybercyte is linked to heart muscle cells grown in the lab. This means the team can investigate how drugs act on whole cells, as opposed to on single proteins within a cell, as researchers did in previous years. Second, the Cybercyte infuses the lab-grown heart muscle cells with a synthetic version of IK1, an electric current that helps regulate the heart’s electrical activity and beat. Without this current, screenings can produce false results—an expensive headache for pharmaceutical firms.
Supported by Buffalo, from the Start Bett credits Buffalo’s tight-knit startup community—including UB— with fueling her company’s growth. The Business and Entrepreneur Partnerships team at UB helped Cytocybernetics secure critical, early stage R&D funding through the UB Center for Advanced Technology in Big Data and Health Sciences (UB CAT) and coordinated acceptance to the START-UP NY program, allowing the company to operate for 10 years without paying various state taxes. These incentives have allowed it to open a research facility on UB’s South Campus and to create internships and hire graduates from UB’s engineering, medicine, management and law programs. In 2015, the company won $500,000 in the 43North startup competition, a highly successful initiative that is part of Gov. Andrew M. Cuomo’s Buffalo Billion Development Investment Plan. That same year, it received two grants that it used to test Cybercyte against current methods to prove its effectiveness to the federal Food and Drug Administration: a $241,933 Small Business Technology Transfer award from the National Institutes of Health; and a $50,000 award from the State University of New York’s Technology Accelerator Fund (TAF). In 2017, the company was awarded $1.5 million by the National Institutes of Health (NIH) to develop an enhanced version of the Cybercyte. The funding—a Phase II Small Business Technology Transfer (STTR) award from the National Heart, Lung, and Blood Institute—enabled the startup to hire more scientists and develop the high-throughput version of its technology.
“This award strengthens the notion of Western New York being an important region for early phase drug development.” — Glenna C. Bett, PhD
“Technologies stemmed from university research stimulate economic growth. We are pleased to have awarded a TAF investment to help Drs. Bett and Rasmusson prepare the Cybercyte for commercial production and verify its value in drug safety screening, positioning the company to apply for STTR funding,” says Grace Wang, PhD, SUNY senior vice chancellor and vice chancellor for research and economic development.
Expansion to Neurologic Applications In 2018, Cytocybernetics received a $250,000 Small Business Innovation Research (SBIR) award from the National Institute of Mental Health (NIMH) to move into a new market: neuronal drug development. The new SBIR funding enables the company to expand beyond cardiac applications and develop the Cybercyte for use with brain cells, called neurons. If successful, this advancement will allow researchers to use the Cybercyte to study how drugs being developed for neurological disorders—such as epilepsy and Parkinson’s disease—affect electrical activity within individual brain cells. “This will enable neuroscientists to determine specific details of how drugs interact with neurons and affect their electrical behavior,” says Bett. “Whereas our work with heart cells is focused on drug safety screening, our work with neurons will target an earlier but equally important step in the drug development pipeline: studying how a drug works, and enabling scientists to more fully characterize early stage candidate drugs with potential in neuroscience.” The new award from NIMH resulted in two new jobs at Cytocybernetics, adding to the firm’s current total of seven full-time employees, not including Bett, who serves as CEO of Cytocybernetics, and Rasmusson, who is president. “This award strengthens the notion of Western New York being an important region for early phase drug development,” Bett says. “Dr. Mark Nowak, who joined Cytocybernetics as our lead scientist in 2015, will be overseeing our research on neuronal applications for the Cybercyte. He graduated from UB in 1992 with his PhD, went to Caltech, then worked in drug discovery in California before coming back to Buffalo to be part of the burgeoning health tech innovation culture here.”
Entrepreneurial Ecosystem Is Thriving In recent years, UB and its partners have worked to expand the region’s entrepreneurial ecosystem, devoting new resources to promoting the growth of startups. Cytocybernetics exemplifies how these investments—ranging from increased mentoring for faculty entrepreneurs to new sources of funding for research, development and commercialization—are paying off for Western New York. “The work of Dr. Bett and Dr. Rasmusson exemplifies how university research benefits society,” says Venu Govindaraju, PhD, UB vice president for research and economic development. “Cytocybernetics’ innovations have the potential to greatly improve the drug discovery process. The company is also creating jobs in Western New York, contributing to the region’s economic development. Cytocybernetics exemplifies how the university is working to commercialize UB technologies, driving growth and helping to transform the region into a national health sciences hub.”
FALL 2019
UB Medicine
13
Photo by Douglas Levere
Innovators
Barry S. Willer, PhD, left, and John J. Leddy, MD ’85, are developers of the Buffalo Concussion Treadmill Test, which is now in wide use around the world.
Treatment of Adolescents with Concussion By Ellen Goldbaum
A landmark study based on breakthrough research
M
uch to the frustration of physicians and athletes alike, there has been no proven treatment for concussion, especially among adolescents, who typically take the longest to recover. That may now change. In a study that overturns conventional approaches to treatment, researchers in the Jacobs School of Medicine and Biomedical Sciences and colleagues have found that adolescent athletes who sustain concussions while playing a sport recover more quickly when they undergo a supervised aerobic exercise regimen. They reported their findings in a paper published earlier this year in JAMA Pediatrics. An accompanying editorial in the journal called it “a landmark study.” The paper describes the first randomized clinical trial of a treatment in the acute phase after a sportrelated concussion. The goal was to evaluate prescribed, progressive sub-symptom threshold exercise—physical activity that doesn’t exacerbate symptoms—as a treatment within the first week of a concussion in adolescents after a few days of rest. The researchers followed 103 participants ages 13-18, with nearly the same number of males and females.
14
FALL 2019
UB Medicine
After sustaining a sport-related concussion, all were seen within 10 days at one of the UBMD Orthopaedics and Sports Medicine clinics in Western New York or at the Pan Am Clinic in Winnipeg. Patients who followed the aerobic exercise program took on average 13 days to recover while those in the control group, who performed stretching exercises, took 17 days. Most patients did not attend the clinic until five days after their injury; therefore, what seems like a small difference— getting better four days faster—in fact equated to improving 30 percent faster from the time of their first visit to the doctor. In addition, fewer patients in the exercise program took longer than four weeks to recover than did patients in the control group.
Contradicts Conventional Approaches “This research provides the strongest evidence yet that a prescribed, individualized aerobic exercise program that keeps the heart rate below the point where symptoms worsen is the best way to treat concussion in adolescents,” says first author John J. Leddy, MD ’85, clinical professor of orthopaedics in the Jacobs School, and director of the UB
Global Health spotlight
“We prescribed exercise at 80 percent Concussion Management Clinic at UBMD of that threshold,” Leddy explains, “so each Orthopaedics and Sports Medicine. patient’s exercise ‘dose’ was individually “Until now, nothing else has been proven in any way effective for treating concussion,” tailored.” Patients were randomly assigned to the says senior author Barry S. Willer, PhD, aerobic exercise group (52) or to a stretching professor of psychiatry in the Jacobs group (51). Patients in both groups were sent School, and director of research in the UB home with a heart rate monitor so they could Concussion Management Clinic. “This is the make sure they stayed below the threshold best evidence so far for a treatment while exercising. that works.” Both groups performed their assigned Leddy and Willer are internationally exercise for about 20 minutes each day and known for their research into the best ways were required to report compliance and to diagnose and treat concussion, especially daily symptoms online. Those in the aerobic among adolescents, who are the most group either walked on a treadmill, rode vulnerable age group for concussions. They have led the emerging body of research findings that show that a patient’s degree of exercise intolerance in the first week after injury, i.e., the lower the threshold of activity at which symptoms increase, is a key clinical indicator of how severe – Barry S. Willer, PhD the concussion may be. The findings of their latest study directly contradict the conventional approach to concussion, which often consists of nearly a stationary bike, or walked either inside total rest and eliminating most physical and or outdoors. Aside from the prescribed mental activities, including schoolwork. exercise, patients were advised to refrain “Telling a teenager to go home and from contact sports, gym class or team basically do nothing is depressing,” says practice. They were given advice about Willer. “It can actually increase their getting schoolwork done and told to avoid physical and psychological symptoms, excessive use of electronic devices, since that and we see that particularly among girls. can also aggravate symptoms. But with our approach, we’re saying, sure, Each patient’s condition was re-evaluated you can return to school and you should weekly, and as symptoms improved, start doing these exercises. Their chins are the “dose” of exercise or stretching was up, Mom and Dad are happy and so is the increased, according to the weekly treadmill student.” test results. Recovery was rigorously defined, requiring agreement among three Buffalo Concussion independent criteria: the patient’s reporting Treadmill Test a normal (minimal) level of symptoms, a To determine how much exercise patients normal physical examination by a medical could sustain without exacerbating doctor, and the return of normal exercise symptoms, the researchers had each one tolerance on the Buffalo Concussion undergo the Buffalo Concussion Treadmill Treadmill Test. The physicians were Test to determine at what level their blinded as to the group assignment of each symptoms worsen. The test, developed by participant. Leddy and Willer in 2004, is now in wide use One surprising finding was that only around the world. two participants out of 52 (4 percent) in the As the patient walks on a treadmill, aerobic exercise group took longer than the incline is gradually increased and the four weeks to recover, compared to seven heart rate is recorded at the point where out of 51 (14 percent) in the stretching group. concussion symptoms intensify. This did not reach statistical significance,
{ } “Reducing the number of concussed adolescents who have delayed recovery has major implications.”
but the scientific literature suggests, by contrast, that between 15 and 30 percent of adolescents who do not receive any treatment will be symptomatic past four weeks. “Reducing the number of concussed adolescents who have delayed recovery has major implications,” Willer says, noting that delayed recovery creates more difficulty with schoolwork, can lead to depression and puts additional demands on the health care system and its costs.
Expanding Access to This Treatment Michael J. Ellis, MD, co-author and medical director of the Pan Am Concussion Program in the Department of Surgery and Pediatrics at the University of Manitoba, says that for years, his clinic has been successfully using the Buffalo Concussion Treadmill Test and a medically supervised sub-symptomthreshold aerobic exercise program to treat professional, collegiate and elite adolescent athletes. Expanding access to this treatment is now critical, he says. “The results of this study suggest that we must build greater capacity within our health care systems to allow patients access to multidisciplinary concussion programs and clinics that have the medical expertise to carry out early targeted rehabilitation of acute concussion.” In the future, the UB group plans to investigate if the treatment is also effective in adults with concussion. Recently, they were awarded a grant from the U. S. Department of Defense to evaluate the feasibility of implementing this protocol with concussed soldiers. In addition to Leddy, Willer and Ellis, co-authors are Mohammad N. Haider, MD, of the Department of Orthopaedics in the Jacobs School; Scott R. Darling, MD and Michael S. Freitas of UBMD Orthopaedics and Sports Medicine; Heidi N. Suffoletto, MD, of the Department of Emergency Medicine in the Jacobs School and UBMD Orthopaedics and Sports Medicine; Rebekah Mannix, MD, of Boston Children’s Hospital; and Jeff Leiter, PhD, and Dean M. Cordingley of the Pan Am Clinic Foundation. The research was funded by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health and the National Center for Advancing Translational Sciences of the National Institutes of Health.
FALL 2019
UB Medicine
15
Innovators
Device Takes Aim at Joint Replacement Infections Photo by Sandra Kicman
Electrical stimulation creates an antibacterial environment By Cory Nealon and Dirk Hoffman
Y
Mark Ehrensberger, PhD
ou probably know someone with a knee or hip replacement. If not, chances are you will, as demand for these surgeries is expected to continue growing. While widely successful, not all joint replacements go as planned. Infections are a serious problem, often requiring costly and painful follow-up surgery. But this could become much less common thanks to the efforts of a multidisciplinary research team at the University at Buffalo that has developed and patented a new infection control strategy that delivers low magnitude voltage-controlled electrical stimulation to a joint replacement or any metal inserted into the body. The electric signal modifies the interfacial electrochemical processes at the metal implant surface to create an antibacterial environment that stops infections before they become problematic. The initial groundwork for this innovative therapy was generated through a multidisciplinary collaboration between Mark Ehrensberger, PhD, associate professor of biomedical engineering and director of the Kenneth A. Krackow, MD, Orthopaedic Research Laboratory, and Anthony A. Campagnari, PhD, professor of microbiology and immunology and senior associate dean for research and graduate education in the Jacobs School of Medicine and Biomedical Sciences. The team showed that the electrical stimulation can prevent and eradicate problematic infections and, importantly, that the technology was synergistic with traditional antibiotic therapy. Garwood Medical Devices LLC, the Buffalo-based startup company that licensed the technology from UB, is developing the Biofilm Disruption Device (BDD) to apply this therapeutic electrical stimulation in a clinical setting. The BDD system includes two electrode skin patches, a machine that generates the electrical stimulation, and a small percutaneous probe that delivers the stimulation directly to the joint replacement.
16
FALL 2019
UB Medicine
The probe is inserted into the body until it reaches the implant or metal hardware. The electrical stimulation then modulates electrochemical processes at the surface of the implant, which produces a surrounding microenvironment that promotes the killing of bacteria. The advancement is important, says Wayne D. Bacon, president and chief executive officer of Garwood, because infections affect roughly one of every 100 knee replacements and there is no simple and effective way to treat them. Often, infections prompt the need for replacement surgeries, which cost at a minimum tens of thousands of dollars. And some studies suggest the rate of infections following joint replacements will increase. “The Biofilm Disruption Device is an elegant and minimally invasive solution to a growing problem that causes pain and suffering in hospitals across the nation. It also could save the health care system billions of dollars,” says Ehrensberger. Garwood is developing the technology with assistance from UB’s Buffalo Institute for Genomics and Data Analytics. Garwood also has been working with UB’s New York State Center of Excellence in Materials Informatics, the UB Center for Advanced Technology in Big Data and Health Sciences and the UB Center for Computational Research. Additional testing of BDD is underway, with the goal of providing the necessary information to win approval from the U.S. Food and Drug Administration when Garwood files its formal application in 2020, Bacon says. In parallel with the commercialization efforts, Ehrensberger and Campagnari are continuing to work with Albert H. Titus, PhD, professor and chair of biomedical engineering, and Thomas R. Duquin, MD, clinical assistant professor of orthopaedics, on a project funded by the Office of Naval Research that seeks to further optimize the electrical stimulation parameters for preventing and treating orthopaedic implant-related infections.
UB Dental startup builds on laboratory studies By Marcene Robinson
P
raveen Arany, PhD, DDS, and Daniel Chan would have never guessed that a friendship forged over badminton would lead to the formation of an emerging biotechnology startup. The pair, who coached together at Rally Niagara Badminton Club for years, are the co-founders of OptiMed Technology, whose products are based on research conducted in Arany’s lab. The company utilizes nanotechnology to develop toothpaste and 3D-printed denture material that treats gum overgrowth and fungal infections. OptiMed Technology recently received a $25,000 grant from the UB Center for Advanced Technology in Big Data and Health Sciences (UB CAT), part of the university’s Office of Business and Entrepreneur Partnerships, to advance the development of its initial products. “The mouth is more than a simple portal to the body. There is a growing appreciation for the impact good oral care has on overall health, in large part based on seminal work done in our school,” says Arany, assistant professor in the Department of Oral Biology in the UB School of Dental Medicine, and chief scientific and strategy officer for OptiMed Technology.
A Startup Is Born When Arany began searching for ways to help patients access a novel oral stomatitis treatment using light therapy developed in his lab, he raised the issue to Chan over a game of badminton. An entrepreneur who has founded and sold several businesses, Chan suggested commercialization as a potential avenue. “The part that excites me is that we could
Photo by Douglas Levere
3D-Printed Dentures, and More
From left: OptiMed Technology co-founders Robert Bachellor, Praveen Arany and Daniel Chan.
help restore quality of life for the patient,” says Chan, managing partner for the company and a graduate student in the UB School of Management. “Connecting science, research and entrepreneurship will lead to innovations that improve quality of life for everyday people.” With the encouragement of Frank Scannapieco, DMD, PhD, chair of the Department of Oral Biology, the pair quickly went to work, securing a spot in the state’s START-UP NY economic development program and building support from connections within the health care and pharmaceutical fields. Today, OptiMed Technology operates out of Foster Hall on UB’s South Campus with a team of 10 scientists, engineers and advisors. Its first product is digoDent, a toothpaste that treats drug-induced gingival overgrowth (DIGO), the development of irreversible scar tissue in the gums that can cause them to cover the teeth, interfering with chewing, speaking and oral hygiene. The condition, which affects more than one million people each year, can cause bad breath, pain, anxiety and even the loss of teeth. DIGO is a side effect of several commonly prescribed drugs such as immunosuppressants, anti-seizure medications, and high blood pressure (calcium channel blocker) medications. Current treatment is limited to surgery to remove scar tissue. However, these procedures are expensive—costing between $500 and $1,500—and DIGO can reoccur within months. OptiMed Technology is working with the UB Center for Dental Studies to develop and test the product for launch in 2020. At the center, they are collaborating with Edward Bednarczyk, PharmD, chair and
clinical associate professor of pharmacy practice; Alferd Reiman, RPh, clinical assistant professor of pharmacy practice; and Sebastiano Ciancio, DDS, chair of periodontics and endodontics, UB School of Dental Medicine.
3D-Printed Dentures The company is also planning to develop MycoDent to commercialize Arany’s 3D-printed dentures. The dentures combat denture-related stomatitis, fungal infections that cause inflammation, redness and swelling in the mouth and affect nearly two-thirds of the denture-wearing population in the U.S. MycoDent is a specially formulated biomaterial that contains polymer microspheres that can be filled with antifungal medication. The microspheres are designed to protect the drug during the heat printing process and allow the release of medication as they gradually degrade. The product can be combined with acrylamide, the current go-to material for dentures, to create antifungal dentures through 3D printing or relining traditional dentures. Unlike current treatment options, such as antiseptic mouthwashes, baking soda and microwave disinfection, dentures containing MycoDent could help prevent infection while the dentures are in use. 3D-printed dentures also allow clinicians to rapidly create customized dentures chairside, a vast improvement over conventional manufacturing that can vary from a few days to weeks. “Besides the technological innovation, these approaches should improve access to oral care that is currently quite inadequate for a significant portion of our population” says Arany.
FALL 2019
UB Medicine
17
Photo by Sandra Kicman
Zhen Yan, PhD, SUNY Distinguished Professor, Department of Physiology and Biophysics, and founder of ASDDR.
By Ellen Goldbaum
Epigenetic Approach to Treating Autism New start-up targets genes involved in neuronal communication
Of all the challenges that come with a diagnosis
of autism spectrum disorder (ASD), the social difficulties are among the most devastating. Currently, there is no treatment for this primary symptom of ASD. New, early stage research in the Jacobs School of Medicine and Biomedical Sciences reveals the first evidence that it may be possible to use a single compound to alleviate the behavioral symptoms by targeting sets of genes involved in the disease. The research, published in March 2018 in Nature Neuroscience, demonstrated that brief treatment with a very low dose of romidepsin, a Food and Drug Administration-approved anti-cancer drug, restored social deficits in animal models of autism in a sustained fashion. The three-day treatment reversed social deficits in mice deficient in a gene called Shank3, an important risk factor for ASD. This effect lasted for three weeks, spanning the juvenile-
18
FALL 2019
UB Medicine
to late- adolescent period, a critical developmental stage for social and communication skills. That is equivalent to several years in humans, suggesting the effects of a similar treatment could potentially be long-lasting, the researchers say.
Profound, Prolonged Effect “We have discovered a small-molecule compound that shows a profound and prolonged effect on autism-like social deficits in the Shank3 model of ASD without obvious side effects, while many currently used compounds for treating a variety of psychiatric diseases have failed to exhibit the therapeutic efficacy for this core symptom of autism,” says Zhen Yan, PhD, SUNY Distinguished Professor, Department of Physiology and Biophysics in the Jacobs School of Medicine and Biomedical Sciences, and senior author on the paper. “Although the preclinical results for our compound are promising,” she adds, “further testing needs to be done to
examine whether it can elicit similar therapeutic effects on social deficits in humans with autism.” The recent study, funded by the Nancy Lurie Marks Foundation and the National Institutes of Health, builds on Yan’s previous research from 2015. That work revealed how the loss of Shank3 disrupts neuronal communications by affecting the function of the NMDA (n-methyl-D-aspartate) receptor, a critical player in regulating cognition and emotion, leading to deficits in social preference that are common in ASD. In the new research, Yan and her team found they could reverse those social deficits with a very low dose of romidepsin, which, they found, restores gene expression and function using an epigenetic mechanism, where gene changes are caused by influences other than DNA sequences. Yan notes that human genetics studies have suggested that epigenetic abnormalities likely play a major role in ASD. To pursue these promising findings, Yan has founded a startup company called ASDDR, which was awarded a Small Business Technology Transfer grant from the National Institutes of Health in 2017 for more than $770,000.
material in the nucleus, so gene expression can be regulated. Since many genes are altered in autism, the UB scientists knew a histone modifier might be effective.
Rescuing Gene Expression In particular, Yan and her team were interested in histone deacetylase (HDAC), a family of histone modifiers that are critically involved in the remodeling of chromatin structure and the transcriptional regulation of targeted genes. “In the autism model, HDAC2 is abnormally high, which makes the chromatin in the nucleus very tight, preventing genetic material from accessing the transcriptional machinery it needs to be expressed,” Yan explains. “Once HDAC2 is upregulated, it diminishes genes that should not be suppressed, and leads to behavioral changes, such as the — Zhen Yan, PhD autism-like social deficits.” But the anti-cancer drug romidepsin, a highly potent HDAC inhibitor, turned down the effects of HDAC2, allowing genes involved in neuronal signaling to be expressed normally. “The HDAC inhibitor loosens up the densely packed chromatin so that the transcriptional machinery gains access to the promoter area of the genes—thus they can be expressed,” Yan says. The rescue effect on gene expression was widespread. When Yan and her co-authors conducted genome-wide screening at the Genomics and Bioinformatics Core at UB’s New York State Center of Excellence in Bioinformatics and Life Sciences, they found that romidepsin restored the majority of the more than 200 genes that were suppressed in the autism animal model they used. “The advantage of being able to adjust a set of genes identified as key autism risk factors may explain the strong and long-lasting efficacy of this therapeutic agent for autism,” Yan explains. She and her colleagues will continue their focus on discovering and developing better therapeutic agents for autism. Co-authors of the study from Yan’s laboratory in the Department of Physiology and Biophysics are Luye Qin, PhD, research assistant professor; Kaijie Ma, research scientist; Zi-Jun Wang, PhD, postdoctoral fellow; Emmanuel Matas, PhD, former postdoctoral fellow; and Jing Wei, PhD, former postdoctoral fellow. Co-author Zihua Hu, PhD, is a bioinformatics computational scientist at UB’s New York State Center of Excellence in Bioinformatics and Life Sciences.
“Although the preclinical results for our compound are promising, further testing needs to be done to examine whether it can elicit similar therapeutic effects on social deficits in humans with autism.”
Key to Treating Social Deficits Many of the mutations in ASD, Yan explains, result from chromatin remodeling factors, which are involved in dynamically changing the structure of chromatin, the complex of genetic material in the cell nucleus that condenses into chromosomes. “The extensive overlap in risk genes for autism and cancer, many of which are chromatin remodeling factors, supports the idea of repurposing epigenetic drugs used in cancer treatment as targeted treatments for autism,” Yan explains. She and her colleagues knew that chromatin regulators—which control how genetic material gains access to a cell’s transcriptional machinery—were key to treating the social deficits in ASD, but the challenge was to know how to affect key risk factors at once. “Autism involves the disruption of so many genes,” Yan notes. “To rescue the social deficits, a compound has to affect a number of genes that are involved in neuronal communication.” To do so, the team turned to a type of epigenetic enzyme called histone modifiers. They alter the structure of chromatin by modifying proteins called histones that help organize genetic
FALL 2019
UB Medicine
19
Photo by Douglas Levere
Neonatologist Munmun Rawat, MD, right, and Jack Grossman, a biomedical engineering student who collaborated on the project.
“Kangaroo Care” for Preemies
By Ellen Goldbaum
When it comes to parents bonding with newborns, skin-to-skin contact, also known as “kangaroo care,” is always best. In the newborn intensive care unit (NICU) providers now encourage parents to engage in kangaroo care, even with babies weighing less than two pounds. The evidence-based benefits include improving the baby’s ability to breathe, regulating body temperature and promoting weight gain. It also provides long-term advantages to the baby’s cognitive and motor development while benefiting parents and boosting the mother’s ability to lactate. As a neonatologist, Munmun Rawat, MD, was determined to provide as much kangaroo care to her baby as she could. When her baby was born premature at 28 weeks and had to spend 62 days in the NICU, she knew that didn’t have to be a barrier. “My baby was just 1,200 grams (about 2.6 pounds), but as soon as he could be held, I ‘kangarooed’ him throughout the day, holding him on my chest,” says Rawat, an assistant professor of pediatrics in the Jacobs School of Medicine and Biomedical Sciences. “When I slept at night, my husband held him on his chest. Our son was ‘kangarooed’ for 12 out of 24 hours a day,” she says. The baby, despite his premature birth, is now thriving and turned three in August. But it bothered Rawat, a neonatologist at the John R. Oishei Children’s Hospital and a physician with UBMD Pediatrics, that
20
FALL 2019
UB Medicine
babies deemed too unstable to be held have to miss out on this integral experience. “So it triggered the thought, ‘if we can’t bring baby to the mother, why not bring mother to the baby?’” Working with students and faculty in the Department of Biomedical Engineering, a joint department between UB’s School of Engineering and Applied Sciences and the Jacobs School, Rawat began developing a concept to replicate kangaroo care for babies who are too fragile to be held. She decided to develop an incubator mattress that mimics the rhythm of mom and dad’s breathing, transmits their heart beat and even their voices. The team created a necklace made of sensors for the parents, which gathers data about their breathing patterns. Those data are programmed into the mattress, which then inflates and deflates in accordance with those breathing data. Another mechanical pump in the mattress replicates the vibration of the parent’s heartbeat. A small, fabric doll that the mother can sleep with gathers her personal odors, which help to familiarize the infant with parents, even without direct bodily contact. To date, the UB team has developed a prototype and soon will begin working on a technology disclosure. In addition to Munmun Rawat, MD, the UB research team includes faculty mentor Anirban Dutta, PhD, assistant professor of biomedical engineering and director of UB’s Neuroengineering and Informatics for Rehabilitation Laboratory; and biomedical engineering students Dominick Calavano, Michelle Ford and Jack Grossman.
Surgical Residents Launch Startup By Dirk Hoffman
A team of Jacobs School of Medicine and Biomedical Sciences entrepreneurs is launching a new company to solve problems that surgeons experience firsthand. SurgIno is the brainchild of four general surgery residents: Tatiana V. Boyko, MD, Stephen Chiang, MD, Jinwei Hu, MD, and Thomas J. Langan IV, MD, MBA. The startup is developing Tensure, a medical device that measures the tension of tissues as they pull away when surgeons close an abdominal incision. The idea literally took root while Boyko was in an operating room. Usually, surgeons must estimate the tension based on experience, and Boyko saw the potential to improve care for patients by providing a more precise assessment. When tension is high at the site of a closed incision, patients are at risk of developing immediate closure failure or a future hernia. SurgIno’s Tensure device has small hooks that attach to a patient’s fascia, connective tissue located beneath the skin that encloses muscles and organs. When a surgeon is ready to close an incision, Tensure can be placed at the surgery site to make measurements. If surgeons decide the tissue tension is too high, they can opt to perform a procedure such as a mesh repair that helps to reinforce the seam. “We came up with a device that works very easily and uses a gauge to measure the amount of tension present,” says Boyko. “Although
a simple device, it’s implications are enormous,” she says, adding that it has the potential to reduce complications from common abdominal surgeries such as C-sections and hernia repairs. Tensure is SurgIno’s first device, but the start-up has a portfolio of products and innovations from local Buffalo surgeons that it would eventually like to roll out. Resources at UB are helping the company get off the ground. All four co-founders took advantage of UB’s Surgery Plus Program, which enabled them to obtain additional degrees and do research in business, bioinformatics or biomedical engineering during their residency. Steven D. Schwaitzberg, MD, professor and chair of surgery, implemented the Surgery Plus Program when he came to UB in 2015 from Harvard Medical School. “Dr. Schwaitzberg brought along a lot of ideas about innovation,” Hu says. “It makes UB’s surgery residency program quite unique.” Boyko adds: “We were able to do this because we have this protected time so we can focus on projects like this. Without the Surgery Plus Program, we wouldn’t have been able to form our startup.” In February, SurgIno filed a provisional patent for Tensure. To learn more about SurgIno and the Surgery Plus Program, go to medicine.buffalo.edu and search “SurgIno.”
Photo by Sandra Kicman
Left to right, general surgery residents and innovators Thomas Langan IV, MD, Tatiana Boyko, MD, Stephen Chiang, MD, Jinwei Hu, MD
F ALL 2 0 1 9
U B M edicine
21
From left: Grant Glatfelter, PhD candidate; Anthony Jones, PhD candidate; Jennie Lipinski, master’s student; Margarita Dubocovich PhD, SUNY Distinguished Professor, senior associate dean for diversity and inclusion; Carleara Weiss, PhD, postdoctoral fellow; and Tanzania Bussey, undergraduate student.
a DiversityMakes Difference
The value of a physician workforce that reflects its community
By Grove Potter Photos by Sandra Kicman
22
As an accomplished African-American student, Shawn Gibson received acceptance letters from numerous medical schools. For a variety of reasons, he and his family chose the Jacobs School of Medicine and Biomedical Sciences. “At first I really wanted to go back home to New York City for medical school,” says Gibson, Class of 2022, “but everything just pointed here. It’s a very family-friendly environment.” Medical schools today are motivated to increase the percentage of underrepresented students, residents and faculty in order to more accurately reflect the diversity of their communities. One of the most compelling factors behind this drive is that patients are known to have better outcomes when treated by physicians who look like them— a factor not lost on the Liaison Committee on Medical Education (LCME), the accrediting body for medical schools in the U.S. and Canada. In 2009, the LCME charged medical schools with increasing diversity. While the directive did not set specific targets to meet, it did require schools to have a “missionappropriate” diversity policy and to commit to recruiting and retaining underrepresented students.
FALL 2019
UB Medicine
Medical schools, including UB, have in turn understood that having a diverse student body requires that concomitant efforts be made to diversify faculty, administrators and residents, as well. “Students, faculty and residents from diverse backgrounds have a lot of opportunities today,” says SUNY Distinguished Professor Margarita L. Dubocovich, PhD, senior associate dean for diversity and inclusion, who heads the Office of Diversity and Cultural Inclusion in the Jacobs School. “Many medical students whom we accept decide to go other places, and we see the same thing with the graduate students. It is very competitive nationwide.”
Building the Pipeline By 2050, and possibly sooner, it is predicted that half the population in the United States will be made up of people who are underrepresented in the physician workforce. “It’s imperative that we have a physician workforce that reflects this diversity,” Ducobovich says. Faced with that challenge, medical schools across the country are working to address this disparity. UB has been
a leader in this effort, dating back to 1990 when it began sponsoring one of New York State’s largest Post-Baccalaureate Programs. Operated in partnership with the Associated Medical Schools of New York, the Post-Baccalaureate Program is designed to expand the pool of underrepresented, economically and educationally disadvantaged students in medical school. Underrepresented students who narrowly miss out on medical school admission can be selected to attend a one-year program to hone study skills. If they complete that year and retake the MCAT exam if needed, they are accepted to one of 10 participating New York State medical schools that nominated them to join the UB PostBaccalaureate Program. Each year, UB admits 19 to 24 students into the program. Numerous programs aimed at supporting biomedical sciences’ careers for underrepresented students have also been established in the Jacobs School, foremost of which are the expansive Collaborative Learning and Integrated Mentoring in the Biosciences (CLIMB) programs created and administered by Dubocovich. CLIMB UP is an umbrella summer program that gives undergraduate students from across the country an opportunity to work in UB faculty labs, performing research and learning about graduate and professional career options. CLIMB PRO, one of four summer program, hosts undergraduates who have a strong interest in pursuing an MD or an MD/PhD. CLIMB HI supports mentoring and fosters professional development for graduate students enrolled in PhD or MD/PhD programs across seven schools at UB and Roswell Park Comprehensive Cancer Center. CLIMB Pathways offers career and professional development for master’s students, and CLIMB-NS provides opportunities and mentoring for postdoctoral associates. “The CLIMB programs welcome everyone, yet 62 percent of the participants in CLIMB UP are underrepresented students, which reflects our focused and integrated recruiting efforts,” Dubocovich explains. UB’s efforts are having success. Underrepresented medical students (African American, Hispanic and Latino, and Native American) made up 18 percent of the class of 2018. For the entire school, 15.2 percent of the students were underrepresented, which is above the national average of about 13.5 percent. “When we created the CLIMB UP program in 2009, we had three students, and this summer we had 36 students,” Dubocovich reports. “The program receives 200 applications a year.” Of the 244 students who have gone through the program, 25 have enrolled in graduate programs at UB, including five who have entered the medical school.
The Residency Challenge Increasing the number of residents and fellows is a steeper challenge. There are more institutions competing for graduates from underrepresented groups. In 2017 and 2018, 830 institutions sponsored approximately 11,200 Accreditation Council of Graduate Medical Education (ACGME) residency and fellowship programs, enrolling 135,000 active full-time and part-time residents and fellows. In 2018, among first-year residents and fellows, 6.8 percent were from underrepresented groups. Among Jacobs School residents and fellows—from which future faculty members can be recruited—a total 7.8 percent were from underrepresented groups, slightly below the national average of between 9 and 12 percent. Current efforts to increase faculty diversity in the medical school centers on recruiting from a pool of underrepresented-in-medicine
David Milling, MD ’93, left, senior associate dean for student and academic affairs and associate professor of medicine; and Roseanne Berger, MD, senior associate dean for graduate medical education and associate professor of family medicine.
residents to steadily reach the national average of 9 percent. “Residents are especially important because, under supervision of faculty, they provide direct care to patients for, on average, three to six years of training, and they are role models for medical students,” says Roseanne Berger, MD, senior associate dean for graduate medical education and associate professor of family medicine. “While they are at UB, we have an opportunity to demonstrate why Buffalo is a good place to advance their careers and become part of the community—to retain them as faculty members. In my mind, the residents are a lynchpin to increasing diversity.” Recruiting residents is a challenge for all institutions. The Jacobs School enrolls about 250 residents and fellows each year. Some programs have established a track record of success in recruiting physicians who are underrepresented in medicine. “This year almost 40 percent of the incoming class in family medicine was underrepresented, and obstetrics and gynecology consistently attracts residents from underrepresented groups,” Berger reports. “My hypothesis is that the students resonate with the commitment to care for people in the community and envision themselves working well with current residents and faculty members.” The concept of service is a particularly strong characteristic among the underrepresented candidates, Berger notes. At a recent reunion of alumni from the UB Post-Baccalaureate Program, former medical students and residents were asked to speak about what motivated them to become physicians. “Many are first-generation college students who described how they are driven by a wish to give back to the communities that helped them and the students who follow in their footsteps.” Berger says. “They may have different career goals, but they all expressed this desire to serve.”
A Huge Lesson A growing body of data indicates that increasing diversity enriches all facets of a university—that students, residents and faculty benefit from learning and working in a more diverse environment. This environment, however, must include training in cultural competency if it’s to reach its full potential in service to education, research and patient care.
FALL 2019
UB Medicine
23
Photo by Sandra Kicman
Prospective biomedical sciences student Rosie Salomon, left, shadowed Shawn Gibson, Class of 2022, president of UB’s chapter of the Student National Medical Association at the 2019 Second Look Weekend event. Salomon began classes this fall at the Jacobs School of Medicine and Biomedical Sciences.
“Clinicians are trained to look at data and evidence-based medicine and apply it fairly to everyone,” Berger says. “But we’re all subject to unconscious bias that is culturally driven, and it’s been shown to influence clinical decision making and interfere with trust in doctor-patient relationships. However, it’s also been shown that when physicians are sensitized to the risk of unconscious bias and learn how to recognize and address cultural differences and beliefs, communication and behavior changes.” Kim Strong Griswold MD ’94, MPH, RN, professor of family medicine, psychiatry, and public health and health professions, sees every day the benefits of a diverse, inclusive medical school in her work with Buffalo’s underserved patient populations. “If you’re not from the U.S., you may not understand that having regular physical checkups from a doctor is good and can help your health improve,” says Griswold, who devotes much of her practice to working with refugees. “You may not understand that taking your medicines as prescribed is good. For example, some patients, rather than taking their pills everyday as prescribed, spread them out so they last longer.” Clear communication is essential to providing good care, yet communicating with patients with different backgrounds requires skills that most people have not developed and so need to be trained in, notes Griswold. She explains that some cultural miscommunications are widely held—rooted in history—and that never learning about them can have negative health consequences. “Years ago, I had an African American patient who had hypertension, yet he was reluctant to do anything about it,” Griswold recalls. “Eventually he agreed to start on a medication. When I talked to him about it, I said, ‘Now this may not work. Sometimes we have to change meds or add something and experiment a little.’ The word ‘experiment’ was a red flag to him, although he didn’t say anything.
24
FALL 2019
UB Medicine
The next time I saw him, I asked him if he had taken the medications, and he said, ‘No, and I’ll tell you why. Are you experimenting on me?’ He didn’t mention the *Tuskegee study, but that was on his mind. So we had a very good talk. That was a huge lesson for me, and it’s the kind of thing you have to learn.”
Science and Sensitivity David Milling, MD ’93, senior associate dean for student and academic affairs and associate professor of medicine in the Jacobs School, understands the need for cultural sensitivity when offering medical care. Originally from Jamaica, he earned undergraduate and pharmacy degrees at UB, then worked at Buffalo General Medical Center for four years before entering medical school at UB. “It’s one thing for people to train in medicine so they can take excellent care of patients from a scientific perspective—and there are many people who are really good at that—but if those physicians are unable to recognize and address cultural barriers their patients face, then they have lost an opportunity to provide optimal care.” Learning the subtleties of cultural differences can often best be learned from peers, Milling notes, which is one of the most valuable and enduring aspects of a diverse school. “The cross pollination that takes place in medical school among students who are different in terms of gender, sexual identity, race and religion, helps to inform everyone about what’s important to those individuals. Over time, this prepares students to more sensitively—and effectively— navigate the multifaceted needs of the patients they will be caring for.”
Health in the Neighborhood Linda Pessar, MD, director of the Center for Medical Humanities in the Jacobs School and clinical professor of psychiatry emerita,
offers first-year medical students an elective called Health in the Neighborhood. The course, which fills up quickly, gives students an opportunity to learn about social determinants of health and health-care disparities by spending time in an underdeveloped black neighborhood. It pairs students with families in the community so they can better understand day-to-day aspects of their lives and, most especially, their experiences with the health-care system. In addition to interacting with families in the community, the students attend seminars in which they have readings and discussions about bias and its consequences to health care. If a medical school is diverse, courses such as this will be just the beginning of the cultural exposure students receive, Pessar says. “If you attend a school that has a diverse medical student population and residency population, you meet people who are not like you, and you talk about your culture and you talk about cultural differences. If you’ve never spoken in detail to a black person or a Hispanic person or a Muslim person, how do you know anything about them? How can you approach patients in anything but a flatfooted way if you can’t begin to imagine their lives? “And most medical school graduates today will work in multispecialty groups or work for hospital systems, where they will treat people with very diverse backgrounds,” Pessar continues. “If they haven’t had this early exposure, they will feel ill at ease because they won’t understand the patient population they serve, and we know this has a deleterious effect on health-care outcomes.”
Second Look, First Choice For Gibson, a first-generation college student, Second Look Weekend was the deciding factor in his choosing to attend medical school at UB. The event was launched last year by Karole Collier, Class
of 2021, president of the Student National Medical Association (SNMA), a national organization committed to supporting current and future underrepresented minority medical students with the goal of increasing the number of culturally competent and socially conscious physicians. Collier collaborated with the Office of Admissions to invite all admitted underrepresented students and their families to Buffalo for three days to get a closer look at the Jacobs School and the community. The gathering builds camaraderie among the students and opens their eyes to all that is available. One highlight is a dinner at which several physicians from the community, who are themselves from underrepresented populations, speak to the students. “These are doctors we can relate to, who look just like us—Hispanic doctors, Native American doctors, black doctors,” Gibson says. “At first, you don’t think that there are doctors of color in the community, but at that event we saw a lot, and it makes a difference.” Gibson followed Collier as SNMA president and organized this year’s Second Look Weekend. The event’s success is measured by its results, and this year all the students who attended have selected UB. “UB does a really, really good job welcoming underrepresented students,” Gibson says. “I have to credit the office of admissions and SMNA for that. Every single Wednesday there are interviews, and the SNMA has partnered with the Office of Admissions to introduce incoming underrepresented students to the school.” That is all part of building a superb medical school, Ducobovich emphasizes. “Diversity is an integral part of excellence. You cannot have excellence without diversity and inclusion.” *In the Tuskegee Syphilis Study in the 1930s and 40s, Black men were not treated for the disease when medicine became available. It is cited as a highly unethical experiment.
Linda Pessar, MD, director of the Center for Medical Humanities in the Jacobs School of Medicine and Biomedical Sciences and clinical professor of psychiatry emerita, left, with Barbara Smith, at a Health in the Neighborhood event held at Hopewell Baptist Church in Buffalo.
F ALL 2 0 1 9
U B M edicine
25
U B M E D docto r v i s i t s
“This is a very exciting time to be studying addiction, since the field is still relatively new.”
Jennifer Martin, PhD, and her mentor David Dietz, PhD, chair of the Department of Pharmacology and Toxicology
Exploring How Heroin Changes Brain Cells Jennifer Martin, PhD ’19, neuroscientist and role model
Jennifer Martin recently completed her doctorate in pharmacology and toxicology in the Jacobs School of Medicine and Biomedical Sciences, and along the way she garnered national recognition for her research on how heroin changes cells in the brain. In 2018, Martin, who is Mohawk and part of the Six Nations community, received a prestigious award from the National Institutes of Health that supports a defined pathway across career stages for outstanding graduate students from backgrounds underrepresented in neuroscience research. The Blueprint Diversity Specialized Predoctoral to Postdoctoral Advancement in Neuroscience (D-SPAN) Award helps talented graduate students transition to postdoctoral positions in neuroscience research, and provides career development opportunities in support of their becoming independent researchers. Martin is grateful for the many opportunities her aptitude and education have given her, but concedes that “the road to a doctorate is long and difficult.” When asked to elaborate, she explains that the biggest challenge to being a female and minority in the sciences is a lack of role models. “It can be hard to picture yourself succeeding in a field where you don’t see many people like you in high positions. But my family has always instilled in me the idea that I can break the mold and be the person who helps to bring more underrepresented individuals into science by being an example.” By Lori Fer g uson and S. A. Ung er
26
FALL 2019
UB Medicine
A Buffalo native, Martin earned a bachelor of science in chemistry from St. John Fisher College in Rochester. While earning her doctorate at UB, she worked in the laboratory of David Dietz, PhD, chair of the Department of Pharmacology and Toxicology, who is internationally recognized for research on how molecular and behavioral plasticity in the brain mediates an individual’s susceptibility to drug abuse and relapse. Martin’s doctoral dissertation explored the role of neuronal and glial cells in the brain’s reward pathway to regulate opiate-induced plasticity. “Glial cells arise from neural stem cells and thus hold the potential for self-renewal,” she says. “If we can gain a greater understanding of how these cells change as a consequence of exposure to opioids, then we can encourage them to repair themselves, thereby preventing addiction relapse.” Today, Martin is a postdoctoral researcher at UB in the laboratory of SUNY Distinguished Professor Zhen Yan, PhD, Department of Physiology and Biophysics, where she is exploring another aspect of glial cells: their role in stress-induced depression. “This condition is often comorbid with addiction, so it’s a fascinating follow-on to my doctoral research.” Martin says that Dietz was instrumental in helping her to become a successful student and scientist, and explains that she also was supported through her membership in UB’s Collaborative Learning and Integrated Mentoring in the Biosciences (CLIMB) program. “There are people in this program who want you to succeed, and they will do anything to help you achieve your goals,” she says. “This is a very exciting time to be studying addiction, since the field is still relatively new. Being part of a generation that is setting the groundwork in the field is thrilling.”
Photos by Sandra Kicman Photos by Sandra Kicman
“I see the devastation that these diseases bring to patients in my retinal degeneration clinics and this informs our long-term goal.”
Gene Therapies for Macular Degeneration Jack Sullivan, MD, PhD, ophthalmic researcher By S. A. Unger
Age-related macular degeneration (AMD) is a serious and presently incurable eye disease that affects more than 10 million Americans. A leading cause of vision loss, its prevalence
increases over age 55. Both the dry and wet forms of the disease are caused by deterioration of the central (macula) portion of the retina, the inside back layer of the eye responsible for capturing the images we see and sending them to the brain through the optic nerve. Because it affects the macula, the disease can severely impair central vision. At present, the effects of the disease can only be mitigated—something John (Jack) Sullivan, MD, PhD, professor of ophthalmology in the Jacobs School of Medicine and Biomedical Sciences, hopes to change. Sullivan is driving advances in gene-based therapeutics to develop promising new approaches to treating retinal and macular degenerations. To accomplish this, he and his team are developing innovative ribonucleic acid (RNA) therapies that target and shut down (suppress) genes that stress and kill retinal cells. By relieving stresses, they expect to preserve both retinal cell vitality and central vision. The molecular agents he is developing (ribozymes and RNAi), may be used to suppress the functioning (expression) of mutated or even normal genes in order to slow down AMD progression. In a further development, Sullivan and his team have developed an RNA drug discovery technology platform that has the potential to significantly accelerate RNA therapeutics for use against diseases
that occur both within and outside the eye. (RNA therapeutics are an emerging class of drugs called biologics.) “Our approach is multidisciplinary and includes such fields as biophysics, bioengineering, molecular genetics and bioinformatics, as well as novel technology and instrumentation designs,” says Sullivan. “I see the devastation that these diseases bring to patients in my retinal degeneration clinics and this informs our long-term goal to translate RNA drug discovery into human clinical trials for people who suffer from visual loss due to these disease states.” The promise of Sullivan’s research is compelling, and families affected by these diseases are responding. UB alumnus George Stevens and his wife, Roberta, have committed $1 million in a bequest gift to support the Department of Ophthalmology and research into AMD. Aleksandra Thon, whose late father suffered from AMD, has pledged $76,000 to establish the LMA Thon Endowment with the Foundation of Jewish Philanthropies to support research at UB, including Sullivan’s. “These generous contributions provide resources to accelerate innovation and provide gap funding whenever needed to ensure that our research continues uninterrupted,” says Sullivan. “My team and I are very grateful for those who support our research and discovery. Giving to UB helps to advance medical breakthroughs that benefit patients in our community and around the world. The challenge is real, and the time is now.” Sullivan completed his MD and PhD training at the Mount Sinai School of Medicine, his ophthalmology residency at Washington University School of Medicine, and his fellowship in retinal and macular degenerative diseases at the University of Michigan. FALL 2019
UB Medicine
27
U B M E D p at h w a y s
Distinguished Alumni and Volunteer Awards The 2019 Distinguished Alumni Awards for the Jacobs School of Medicine and Biomedical Sciences were presented during Reunion Weekend, May 3-4. The event, sponsored by the UB Medical Alumni Association in conjunction with the school, was attended by family and friends of the awardees, as well as alumni, faculty and students.
John A. Ulatowski, MD ’84, PhD ’80, MBA 2019 Distinguished Medical Alumnus John A. Ulatowski, MD ’84, PhD ’80, MBA, is an internationally recognized leader in anesthesiology/critical care medicine, neurology and neurosurgery. He has been on faculty at Johns Hopkins University since 1991. In 2004, Ulatowski became the Mark C. Rogers Professor and director of the department of Anesthesiology and Critical Care Medicine (ACCM), as well as anesthesiologist-in-chief for Johns Hopkins Hospital. Under his oversight, ACCM emerged as an institutional leader in patient safety, culminating in the department’s founding leadership of the Armstrong Institute for Patient Safety. Ulatowski’s research interests focus on the regulatory mechanisms of cerebral blood flow and oxygen delivery to the brain, pain management and sedation, and patient safety and performance improvement in the OR and ICU environments. From 2011 to 2018, Ulatowski served as vice president of Johns Hopkins Medicine International (JHI). In this role, he oversaw delivery of medical care to international patients coming to the Johns Hopkins Health System in the U.S. He also led efforts to increase medical care and medical program development at institutions affiliated with JHI around the world. At Johns Hopkins, Ulatowski is credited with creating a new educational platform for residencies and fellowships in all specialties in anesthesia; expanding research programs; introducing new care models to clinical practice that were later adopted by outside institutions; implementing electronic medical records for perioperative environments; and facilitating telemedicine initiatives in the adult and pediatric ICUs to improve patient care. Ulatowski received a bachelor of science degree in biology from Niagara University. He then attended the University at Buffalo, where he earned a doctorate in physiology and a medical degree. After completing his internship and residency in neurology at the University of Maryland Hospital, he began a second residency in anesthesiology at Johns Hopkins in 1988. He followed this with combined fellowships in neuroanesthesia and neurocritical care. In 2000, he earned an MBA degree from Loyola College of Maryland.
28
FALL 2019
UB Medicine
Elizabeth Repasky, PhD ’81 2019 Distinguished Biomedical Alumna Elizabeth Repasky, PhD ’81, is Distinguished Professor of Oncology, the William Huebsch Professor of Immunology, and program leader for the Cell Stress and Biophysical Therapies Program at Roswell Park Comprehensive Cancer Center. A leading expert in the field of thermal medicine, Repasky focuses her research on stress and its physiological consequences in order to better understand how to manipulate stress to improve the efficacy of cancer therapies, including radiation, chemotherapies and immunotherapies. In recent years, she has pursued investigations into the impact of body temperature and thermal stress on immunotherapy, which have led to Phase 1 and Phase 2 clinical trials at Roswell Park. A native of Western Pennsylvania, Repasky earned a bachelor of arts in biology from Seton Hill University and a PhD in anatomical sciences from the Jacobs School of Medicine and Biomedical Sciences. She completed a postdoctoral fellowship at the California Institute of Technology. Repasky is the recipient of the 2018 J. Eugene Robinson Award and the William C Dewey Award for mentorship, both from the Society for Thermal Medicine. She has also been awarded Seton Hill University’s Distinguished Alumna Leadership Award, the Thomas B. Tomasi Hope Award for her research discoveries, and several mentorship and teaching awards, including the 2018 Graduate Student Association Award for Faculty Excellence in Mentoring and Teaching. The author or co-author of 190 research publications, Repasky has been consistently funded by the National Institutes of Health (NIH), and she is currently the principal investigator on four NIH grants. She also has obtained several patents associated with her work, served as thesis advisor to 23 doctoral students, and trained 17 postdoctoral fellows.
Ranjit Singh, MB BChir, MBA ’04 Distinguished Resident
Thomas J. Guttuso Sr., MD ’60 2019 Lifetime Achievement Award
Ranjit Singh, MB BChir, MBA ’04, is a recognized leader in the field of patient safety in primary care. He has served on numerous patient safety committees, nationally and internationally, including those at the Centers for Disease Control, National Quality Forum, and World Health Organization. His work has been funded through federal grants, with partners across diverse disciplines. For more than 20 years, Singh has worked to make patient safety an integral part of medical education and practice. His research applies systems engineering and information technology to prevent errors and improve safety. He is especially dedicated to preventing avoidable harm from medications among older adults. His current research focuses on deprescribing— identifying and discontinuing medications that pose significant risk without commensurate benefit. Currently, Singh is co-director of the National Institute of Health’s Research Career Development Program (K12) in Implementation Science, training the next generation of clinician-researchers in scientific methods that help translate research findings into real-world settings. This includes implementing patient-care guidelines as well as de-implementing unsafe or ineffective treatments that are still being used. Singh earned both a master’s degree in management sciences and a medical degree from the University of Cambridge, England, after which he came to UB for residency training in family medicine. In 2004, he earned an MBA from UB. Singh has served on faculty in the UB Department of Family Medicine since 2000 and holds secondary faculty appointments in the Department of Biomedical Informatics and in the School of Management’s Department of Management Science and Systems.
Kim Strong Griswold, MD ’94 2019 Distinguished Volunteer of the Year Kim Strong Griswold, MD ’94, MPH, RN, FAAFP, is professor of family medicine, psychiatry, and public health and health professions. For 25 years, Griswold has dedicated her clinical practice to working with mentally ill adults and with immigrant and refugee populations seeking asylum. She also serves as a role model to UB medical students and residents by providing care to underserved communities overseas. As faculty advisor to the student-led Human Rights Initiative in the Jacobs School, Griswold has been instrumental in establishing and sustaining this unique learning experience for UB medical students.
The 2019 Lifetime Achievement Award was presented posthumously to Thomas J. Guttuso Sr., MD. A 1960 graduate of the Jacobs School of Medicine and Biomedical Sciences, Guttuso was dedicated to his alma mater, serving it in numerous capacities over a span of decades. A respected ophthalmologist and school administrator, Guttuso was chair of ophthalmology at Erie County Medical Center (ECMC) in the late 1970s and early ’80s and led a successful effort to form a single, unified UB-sponsored ophthalmology program. This was accomplished by incorporating what were then three strong clinical sites—at Women and Children’s Hospital of Buffalo, the Buffalo VA Medical Center and ECMC. Guttuso then served as program director for the new Department of Ophthalmology from 1985 to 1988. Guttuso also served the Jacobs School as director of medical student admissions for 20 years and assistant dean for admissions. In 2014, he served as president of the Medical Alumni Association (MAA). In this capacity, he worked to further strengthen the relationship the MAA has with the Jacobs School administration and with the Office of Medical Advancement and Alumni Engagement. During his tenure, the MAA saw a significant increase in the Alumni Scholarship Fund, as well as enhanced relationships with alumni and students. Guttuso received numerous honors for his contributions to the medical school, including the Distinguished Medical Alumnus Award in 1995 and the Dean’s Award in 2001.
Griswold conducts research related to psychiatry, cultural care and public health. She is a co-investigator on a project to increase the primary care workforce size, leadership potential, diversity and commitment to patientcentered medical home models of practice in underserved areas throughout the region, state and nation. A highly regarded teacher, Griswold is devoted to educating premed and medical students and training family medicine residents to provide complete inpatient management of adult patients, with a special focus on care for vulnerable populations. Griswold earned a bachelor of arts degree in drama and English from Bard College; a nursing degree from Upstate Medical Center; a master’s degree in public health from Yale University; and a medical degree from UB. She is a graduate of the Royal College of Physicians Educator Program. Over the course of her career, she has received multiple teaching and humanism awards from students and residents and has been inducted into the Richard Sarkin Memorial Chapter of the Gold Humanism Honor Society. FALL 2019
UB Medicine
29
U B M E D p at h w a y s
Pinkel Receives Honorary Doctorate Donald Pinkel, MD ’51, pioneering pediatric oncologist, and the first director of the St. Jude’s Children’s Research Hospital in Memphis, was conferred a SUNY Honorary Doctorate in Science in absentia at this year’s Jacobs School commencement. Pinkel is worldrenowned for developing the first curative drug treatment for acute Pinkel lymphoblastic leukemia (ALL) — the most common type of cancer in children and a disease once considered virtually untreatable. For his seminal achievements, he was honored in 1972 with the Lasker Award, often referred to as “America’s Nobel Prize.” Pinkel also was instrumental in developing the public health initiative that led to the formation of a supplemental food program for women and children that was adopted by the U.S. Department of Agriculture. Now known as the
Women, Infant, Children (WIC) Program, this initiative is recognized as one of the nation’s most successful and costeffective nutrition interventions. After graduating from the Jacobs School of Medicine and Biomedical Sciences, Pinkel began his career in pediatrics as an intern, resident and chief resident at the Children’s Hospital of Buffalo, now the John R. Oishei Children’s Hospital. While there, he developed his interest in hematology and oncology, starting the hospital’s first oncology service and clinic. Throughout his career, he integrated clinical care and basic research protocols. He is a passionate advocate for children and a trailblazer in the research and treatment of a once-incurable disease. His groundbreaking work has enhanced not only the lives of patients with ALL, but of those with other childhood cancers and several adult malignancies as well. In 2000, Pinkel was named Distinguished Medical Alumnus for the Jacob’s School.
Jacobs Faculty Earn SUNY Chancellor’s Awards Congratulations to the following Jacobs School of Medicine and Biomedical Sciences’ faculty who were honored through the SUNY Distinguished program and the SUNY Chancellor’s Awards for Excellence program in 2018-19. Anthony Campagnari, PhD ’84, senior associate dean for research and graduate education, and professor of microbiology and immunology, and Campagnari medicine, named SUNY Distinguished Professor.
Duffey
30
Michael E. Duffey, PhD, professor of physiology and biophysics, and medicine, recipient of the Chancellor’s Award for Excellence in Teaching.
FALL 2019
Elkin
Peter L. Elkin, MD, professor and chair of biomedical informatics, and professor of internal medicine, recipient of the Chancellor’s Award for Excellence in Faculty Service. M. Laura Feltri, MD, professor of biochemistry and neurology, recipient of the Chancellor’s Award for Excellence in Scholarship and Creative Activities.
Feltri
UB Medicine
Steven D. Schwaitzberg, MD, professor and chair of surgery, recipient of the Chancellor’s Award for Excellence in Faculty Service. Schwaitzberg
A One-Man Research Catalyst gene expression within the neutrophils (a type of white blood cell) of people who have intracranial aneurysms. In 2016, Harvey launched Neurovascular Diagnostics with Meng and Tutino. “The test we’re developing is important because today the way you determine if you have an unruptured brain aneurysm is to have an MRA [magnetic resonance angiogram], which can cost between $2,000 to $3,000, something insurance companies may not pay for because patients often do not have any symptoms,” explains Harvey, who is chief financial officer of the company. “Also, brain aneurysms can be genetic. One doctor said my children should be tested every five years. To spend $4,000 to $6,000 every five years to have this tested, that’s a lot of money. A $200 blood test would be much better, and if it’s positive then you can get an MRA.” UB is providing direct support to Neurovascular Diagnostics and has also connected the firm to numerous resources designed to accelerate commercialization. The Business and Entrepreneur Partnerships team in the Office of the Vice President for Research and Economic Development helped Neurovascular Diagnostics secure a Small Business Innovation Research (SBIR) award from the federal government by introducing the firm to InteliSpark, an Ithaca-based consulting firm that assists startups in competing for SBIR and Small Business Technology Transfer —Frederick Sachs, PhD (STTR) funding. The UB Center for Advanced Technology in Big Data and Health Sciences (UB CAT) provided seed funding for R&D, supplementing a $45,000 award from the Brain Aneurysm Foundation. UB’s Career Experience Program, which funds internships in the life sciences and advanced manufacturing sectors, placed a UB student with Neurovascular Diagnostics for a semester. Both the Career Experience Program and UB CAT are funded by Empire State Development’s Division of Science, Technology and Innovation (NYSTAR).
Photo by Sandra Kicman
Continued from Page 7
Frederick Sachs, PhD, Suny Distinguished Professor, with his tarantula friend.
going to be a lot easier for Neurovascular to receive FDA approval.” Since its launch, Tonus Therapeutics, like Neurovascular Diagnostics, has received comprehensive support from UB’s Business and Entrepreneur Partnerships team, which will continue to work with both firms into the future. This support includes business consultation, funding, commercialization services, regulatory guidance, marketplace potential research and access to specialized equipment and lab space. “Incredible innovations happen here every day,” says Christina P. Orsi, associate vice president for economic development at UB. “We are seeking more interested business experts like Jeff Harvey to engage with our researchers to help bring those innovations to life through new products and services.” Harvey—as an investor who is deeply motivated by what his own family has faced—is today an inspiration for patients and families who suffer from Duchenne muscular dystrophy and brain aneurysms, two medical conditions in great need of breakthrough treatments and early diagnostics. He is as determined as ever to put his resources and intelligence toward seeing these developments become a reality by partnering with world-class biomedical researchers who, it turns out, work at a premiere researchintensive university in his hometown. To learn more about UB’s Business and Entrepreneur Partnerships, visit www.buffalo.edu/partnerships.
“Never underestimate the power of luck. When we discovered mechanosensitive ion channels, it was an accident. . . . There was no data on these things before we discovered them.”
Hometown Advantage Harvey is optimistic that the blood test will receive approval from the FDA. “Neurovascular Diagnostics is developing a blood test, whereas Tonus is developing a therapy that would go into humans,” he says. “So, I think it’s
FALL 2019
UB Medicine
31
ub med Q & A Telemedicine for Integrated Treatment of HCV/Substance Abuse —A Conversation with Andrew Talal, MD, MPH, a pioneer in the approach
Andrew H. Talal MD, MPH, a leading expert in liver disease, has pioneered the use of telemedicine to treat hepatitis C virus (HCV) patients who are in opioid treatment programs. A professor of medicine in the Jacobs School of Medicine and Biomedical Sciences, Talal is founding director of the UBMD Internal Medicine Center for Clinical Care and Research in Liver Disease. Recently, he was invited by the National Academy of Medicine to discuss the success of his telemedicine program that integrates treatment of substance abuse and HCV. UB Medicine talked with Talal about his innovative work.
Q: Why are best practices in HCV/substance abuse so urgently needed today?
A: HCV infection is closely tied to the opioid epidemic, and injecting drugs is the primary transmission route. HCV causes more deaths than 60 other reportable infectious diseases combined, and the incidence is expected to grow rapidly in the next decade, especially among opioid users. Yet, this population rarely receives treatment.
Q: A:
What are the outcomes for your telemedicine program?
Outcomes from our early pilot studies show that telemedicine is a highly effective way to reach and treat this vulnerable population. In 2018, I published reports in Clinical Infectious Diseases and in Telemedicine and E-Health on the use of telemedicine to treat HCV in patients on methadone. Both studies found that telemedicine had excellent clinical effectiveness and that patients preferred it to being referred to a conventional off-site provider. They appreciated the one-stop shopping and being treated in the comfortable, familiar location of the opioid treatment program. It was especially well-accepted by patients from underrepresented groups who had concerns about privacy and confidentiality.
“Privacy, stigmatization and lack of easy access to HCV specialists are all barriers.”
Q: A:
Has the concern for privacy been a major barrier to treatment?
Privacy, stigmatization and lack of easy access to HCV specialists are all barriers. The conventional method of treatment delivery—referral to an offsite location—has discouraged many individuals from initiating or completing treatment. Now that we have all-oral treatments with improved efficacy and almost no side effects, more patients should be lining up to be treated.
Q: What other barriers does the telemedicine approach overcome? A: There is a limited number of providers. The ability to link patients to providers via telemedicine removes geography as a barrier to implementation of high-quality specialty care. Also, many of these patients suffer from mental health conditions, and they are more likely to be affected by poverty and a lack of social support—factors that may deter them from seeking treatment in conventional clinical settings.
Q: Are you optimistic about the future of telemedicine as an effective way to address A:
HCV in substance users?
Yes—but issues around reimbursement have to be resolved first. In order for it to reach its full potential, telemedicine should be reimbursed at the same rate as a visit to a doctor’s office. Equitable reimbursement is required to ensure financial sustainability, and is an area we need to pursue to enable more widespread adoption.
—S. A. Unger
Talal
32
FALL 2019
UB Medicine
Honored
Grateful Rebecca Kish, a 2019 Western New York Medical Scholarship recipient
By S.A. Unger
“Beyond grateful” is how Rebecca Kish, Class of 2021, describes what she felt when she learned that she had been named a 2019 recipient of the Western New York Medical Scholarship, which will cover the majority of her medical school tuition. The Western New York Medical Scholarship Fund, now in its fifth year, provides four-year scholarships to local students to attend the Jacobs School of Medicine and Biomedical Sciences. The goal is to train and retain more doctors in the eight counties of Western New York, stemming a steady decline in the number of physicians who practice here. Scholarship recipients are awarded about $30,000 annually and must pledge to practice in Western New York for five years upon finishing medical school and resident training. The highly selective criteria require recipients to have excelled academically, to have graduated from a high school in the eight-county region of Western New York and to have demonstrated financial need. Kish, a native of Buffalo, was raised by her mother, a single parent, in a cottage near the beach in Angola. When health issues arose in the family, it was difficult to find specialists close to home. “This was one of the first things that spurred my interest in becoming a doctor,” Kish recalls. “Everyone should have access to quality health care.” When Kish was young, her mother returned to school to become a physical therapist assistant, assuming steep debt. Kish realized her mother would not be able to help finance her education and that she had to make her way on her own. Fortunately, her academic achievements earned her a Provost scholarship at UB and, upon graduation, she was admitted to UB medical school. The accomplishment was bittersweet once she realized she would have to assume over $300,000 in debt over the next four years to cover her education and living expenses. “Now, by alleviating my debt, the Western New York Medical scholarship allows me to stay in my hometown and give back to the community I love,” says Kish. “Because of this I will have the opportunity to pursue the avenues of medicine that I am truly passionate about without having debt guide my choices.” This summer, Kish began her third-year of medical school with renewed appreciation. “I can focus on becoming the best physician possible, and not have to worry about my financial situation upon graduating,” she says. “And I am so honored to know that the community supports my education.” To learn more about the Western New York Medical Scholarship Fund, email Eric Alcott, senior associate dean and executive director of medical philanthropy and alumni engagement, at ealcott@buffalo.edu, or call (716) 829-2773.
Photo by Meredith Forrest Kulwicki
AND
Nonprofit Org. U.S. Postage
UB Medicine University at Buffalo 916 Kimball Tower Buffalo, NY 14214-8028
PAID Buffalo, NY Permit No. 311
My Bold Moment “Someone I didn’t know gave me this scholarship money and My Bold Moment it taught me to pay it forward. In the grand scheme of things, that’s “I was always attracted what I’m here for.and That’s why I to primary care chose medicine—to community health. Ihelp wantothers.” to effectCheema, change,third-year not only in Amandip Jacobs medical treatment but in the School of Medicine and Biomedical patient-and-family journey.” Sciences student Dennis Kuo associate professor and division chief, general pediatrics
Bold moments are what make us great. Moments when theory becomes reality. When we stand up for what we believe in. And when we work together toward the greater good. The Boldly Buffalo campaign provides countless opportunities for faculty and students to lead the way in research and practice. To learn how you can help create a better world, visit buffalo.edu/campaign.