


































































































































































































































































































It's important to start HIV treatment as soon as possible and stick with it. Remember to take your treatment as prescribed and stay engaged in care. Taking care of yourself is a great way to help you live well with HIV.
It's important to start HIV treatment as soon as possible and stick with it. Remember to take your treatment as prescribed and stay engaged in care. Taking care of yourself is a great way to help you live well with HIV.
HIV doesn't have to stop you from being you. Discover helpful tips and support to keep living your authentic life.
HIV doesn't have to stop you from being you. Discover helpful tips and support to keep living your authentic life.
Find more helpful information and resources at HelpStopTheVirus.com
Find more helpful information and resources at HelpStopTheVirus.com
If you're living with viral load to undetectable. little virus in the blood it. Current research prescribed and getting prevents the transmission also known as U=U
If you're living with viral load to undetectable. little virus in the blood it. Current research prescribed and getting prevents the transmission also known as U=U
U=U means undetectable=untransmittable. It helps destigmatize living with HIV, raises awareness that medications can be e ective, and reminds people importance of continuing to take treatment as prescribed.
Stay empowered to live a longer and healthier life.
U=U means undetectable=untransmittable. It helps destigmatize living with HIV, raises awareness that medications can be e ective, and reminds people importance of continuing to take treatment as prescribed. Stay empowered to live a longer and healthier life.
It's important to be healthcare provider and your routine. meet with them.
It's important to be healthcare provider and your routine. meet with them.
Fighting against HIV and AIDS has always been a struggle. Much work remains to end the epidemic. POZ encourages you to get involved in advocacy. Go to poz.com/ advocacy to find the latest news and learn how you can make a difference in the fight.
Opinions still vary on whether criminal law should apply to HIV disclosure, exposure and transmission. However, there is a growing consensus to make laws reflect current science. Go to poz.com/ criminalization for more on how you can get involved in reform efforts.



The science is clear: People who have an undetectable viral load don’t transmit HIV sexually. In addition to keeping people healthy, effective HIV treatment also means HIV prevention. Go to poz.com/undetectable for more.
Brenda Emily was born with HIV.
22 HIV ADVOCACY ON TIKTOK A new generation is using the social media sensation to promote sexual health.
BY CHARLES SANCHEZ28 WARD 86 AT 40 The clinic has pioneered innovations that have been adopted worldwide.
BY LIZ HIGHLEYMANScan the QR code (left) with your smartphone camera or go to poz.com/digital to view the current and past issues online.

3 FROM THE EDITOR Only the Young
4 POZ Q & A
Marvell Terry II has a new role in HIV advocacy: helping to ensure access for all to long-acting injectable HIV treatment.

6 POZ PLANET
16 CARE & TREATMENT
HIV mortality continues to decline, but disparities persist • women with HIV missing from clinical trials • PrEP does not impair kidneys • HIV stigma among Latinos
18 RESEARCH NOTES
HIV vaccine fails in Mosaico trial
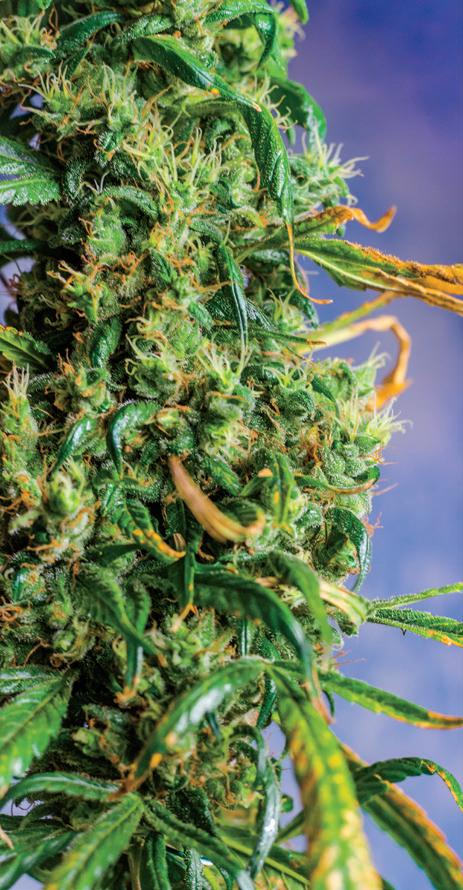
• Sunlenca, approved for people with multidrug-resistant HIV, also works for first-timers • HIV in the brain • cannabis use may impair adherence to HIV treatment
• POZ Stories: Eunice & Kalvin
PEPFAR turns 20 • Tennessee rejects “free money” to prevent HIV • no HIV from hepatitis vaccine • scuba trips not part of HIV research • Beyoncé thanks her uncle lost to AIDS
• Everyday: milestones in the HIV epidemic
12 VOICES
Saturday Night Live sends up HIV treatment ads, and an argument in favor of the HIV Is Not a Crime conference.
14 SPOTLIGHT
Black advocacy
19 BASICS Syphilis
20 NUTRITION & FITNESS
Mushroom and egg toast
• slow down and enjoy your food
32 HEROES
As a new mother living with HIV, Brenda Emily has chosen to breastfeed.

EDITOR-IN-CHIEF
ORIOL R. GUTIERREZ JR.
MANAGING EDITOR
JENNIFER MORTON
DEPUTY EDITOR
TRENT STRAUBE
SCIENCE EDITOR
LIZ HIGHLEYMAN
COPY CHIEF
JOE MEJÍA

EDITORIAL ASSISTANT
LAURA SCHMIDT
ART DIRECTOR
DORIOT KIM
ART PRODUCTION MANAGER
MICHAEL HALLIDAY
CONTRIBUTING WRITERS
SHAWN DECKER, OLIVIA G. FORD, ALICIA GREEN, MARK S. KING, TIM
MURPHY, CHARLES SANCHEZ
CONTRIBUTING ARTISTS
JOAN LOBIS BROWN, LIZ DEFRAIN, ARI MICHELSON, JONATHAN
TIMMES, BILL WADMAN
FOUNDER
SEAN STRUB
LEGACY ADVISER
MEGAN STRUB
ADVISORY BOARD
A. CORNELIUS BAKER, GUILLERMO
CHACÓN, SABINA HIRSHFIELD, PHD, KATHIE HIERS, TIM HORN, PAUL KAWATA, NAINA KHANNA, DANIEL
TIETZ, MITCHELL WARREN
PRESS REQUESTS
NEWS@POZ.COM
SUBSCRIPTIONS
HTTP://ORDER.POZ.COM
UNITED STATES: 212-242-2163
SUBSCRIPTION@POZ.COM
FEEDBACK
EMAIL WEBSITE@POZ.COM OR EDITOR-IN-CHIEF@POZ.COM
SMART + STRONG
PRESIDENT AND COO
IAN E. ANDERSON
EDITORIAL DIRECTOR
ORIOL R. GUTIERREZ JR.
CHIEF TECHNOLOGY OFFICER
CHRISTIAN EVANS
VICE PRESIDENT, INTEGRATED SALES
DIANE ANDERSON
INTEGRATED ADVERTISING MANAGER
JONATHAN GASKELL
INTEGRATED ADVERTISING COORDINATOR
SARAH PURSELL
SALES OFFICE 212-938-2051; SALES@POZ.COM
CDM PUBLISHING, LLC
CEO
JEREMY GRAYZEL
CONTROLLER
JOEL KAPLAN
I‘M OLDER NOW THAN I EVER thought I would be after testing HIV positive in 1992. At 52, I’ve been living with HIV longer than young people—folks under 30—have been alive. That’s a bit of a mind trip for me.
Not only am I feeling older, I’m most certainly behaving so too. Case in point: TikTok. I didn’t really pay attention to the social media platform until fairly recently. That isn’t like me, at least a younger me. I’ve been an early adopter of most technology.
For example, I was very ready for the first iPhone because I could finally have just one device instead of two. Saying goodbye forever to my PalmPilot was a milestone in my relationship with tech. As new tech came along, including social media, I was usually soon on board.
So not getting into TikTok was weird for me. I suppose Vine, the short-lived video app, had something to do with it. TikTok launched about the same time that Vine shuttered. As a result, I took a wait-and-see approach to TikTok. However, young people did the opposite, making TikTok the sensation it is today.
As with previous social media, HIV advocacy has found a way to make an impact on TikTok. In this special issue focusing on youth, we spotlight four advocates using TikTok to promote HIV awareness and sexual health. Go to page 22 to read about Chase Cramer, Johneri’O Scott, Melissa Strype and Oliver Wong.


Encouraging young people to get tested for HIV and get treated if they have the virus is understandably the message of most HIV advocacy for those under 30. Nonetheless, some young people living with HIV are also long-term survivors. Some were born with the virus, while others contracted it early in their lives. When discussing youth, we should include them.
HIV advocate Brenda Emily makes sure that we do. The 26-year-old was born with the virus. She is also the mother of a baby
girl, whom she breastfeeds, which was not supported by her pediatric health care providers—so she got another team. Go to page 32 to read more about her advocacy.
Former POZ magazine cover subject and youth advocate Marvell Terry II has a new role in HIV advocacy. He’s working to ensure that underserved populations have equal access to long-acting injectable HIV treatment. Go to page 4 to learn more.
Serving those most in need is something that Ward 86 in San Francisco has done for a long time. The first dedicated HIV inpatient clinic in the United States marked its 40th anniversary earlier this year. It pioneered innovations in HIV treatment and prevention that have been adopted around the world. Its latest initiative aims to broaden the use of long-acting injectable treatment to a safetynet population. Go to page 28 for details.
The President’s Emergency Plan for AIDS Relief (PEPFAR) also had a big anniversary this year. The U.S. global HIV program marked 20 years of service. Go to page 6 for more about PEPFAR’s accomplishments.
ORIOL R. GUTIERREZ JR. EDITOR-IN-CHIEF editor-in-chief@poz.com
Want to read more from Oriol? Follow him on Twitter @oriolgutierrez and check out blogs.poz.com/oriol.
Ensuring underserved populations have access to long-acting injectable HIV treatment.
FORMER POZ MAGAZINE COVER SUBJECT MARVELL TERRY II HAS a new role in HIV advocacy. He is the new project manager and community engagement lead of the Accelerating Implementation of Multilevelstrategies to Advance Long-Acting Injectables for Underserved Populations (ALAI UP) Project at the Aaron Diamond AIDS Research Center of Columbia University’s Vagelos College of Physicians and Surgeons. Cabenuva (cabotegravir plus rilpivirine) is the first long-acting injectable HIV treatment and is administered by a health care provider monthly or every other month.
Previously, Terry raised awareness and promoted education and resources for Black LGBTQ people in the South with his annual conference, the Saving Ourselves Symposium, now hosted by the Southern AIDS Coalition. He has also worked at the Human Rights Campaign Foundation and the Southern HIV Impact Fund at AIDS United.
Terry recently sat down for a chat about this next step in his career with his friend and colleague DaShawn Usher, currently the director of communities of color and media at GLAAD, an LGBTQ media advocacy organization.
As project manager, I work internally with the leadership team to manage the execution of the ALAI UP Project efficiently and effectively. Externally, I work with eight clinics from across the United States that provide clinical and wraparound services to underserved populations to ensure that this first form of injectable treatment reaches those who need it the most as quickly as possible.
In my community engagement lead role, I work with those eight clinics to ensure that in the pre-implementation phase, clinics are meeting with, listening to and hearing from the community. I work with clinics to ensure that listening sessions are happen-
ing and the voices of underserved populations inform implementation.
Once sites are selected, I work to increase representation of people living with HIV on our project advisory board from those geographic areas in which we are working—and, importantly, I ensure that those newer members feel included and their perspectives are valued.
I also feel a sense of responsibility, working now at a large Ivy League institution with many academics, to ensure we are intentional in our work with the community and to ensure we are effective and efficient.

I want to ensure that we not only interrogate the numbers but also reflect on the faces and lives of underserved populations and remember that our work is to serve them where so many other systems have failed them.
Tell us more about ALAI UP.
ALAI UP is part of the Special Projects of National Significance Program funded by the Health Resources Services Administration. ALAI UP is focused on supporting clinics across the United
States to deliver long-acting injectable HIV treatment to make progress toward health equity and ensure that all people with HIV can remain engaged in HIV care and achieve and sustain viral suppression.
I manage a large team of folks at Columbia University’s Vagelos College of Physicians and Surgeons, the New York City Department of Health and Mental Hygiene, City University of New York and the Southeast AIDS Training and Education Center in Nashville.
My role is to make sure that we are on track to use their combined expertise in implementation science, clinical service delivery, capacity building, monitoring and evaluation; [to show] a deep commitment to anti-stigma and anti-racism; and to create tools and resources that are specifically designed to make it possible that this new injectable form of treatment is implemented equitably from day 1—instead of trying to “fix” inequity in its implementation later.
What about this role appeals to you?
I can recall sitting in the 2015 Policy and Advocacy Summit in Baltimore, organized by the National Black Gay Men’s Advocacy Coalition’s Young Black Gay Men’s Leadership Initiative. This meeting convened young Black gay men from around the United States, and I had a role on the organizing committee that year.
A young Black gay man from the South stood up in deep anger because of how long it took pre-exposure prophylaxis (PrEP) to get to the Black community and then to underserved areas of the United States. That moment—the emotion, the pleadingfromBlackgaymen—hasstayed with me for years.
This role appealed to me because we cannot allow this new tool—theoretically available in our tool kit right now and yet still only used by probably less than 1,000 people across the United States—to reach underserved populations as slowly as PrEP did. We must get this right because I believe this injectable formulation is only the first one— and that other, more advanced medications will follow.
What we learn in this project could show that a different path—one that
prioritizes equity—is possible when new groundbreaking medications, or one day even a cure, are here. As a person living with HIV, the role is also personal. We must ensure long-acting injectables for treatment are accessible to everyone, regardless of where you live or the type of insurance you have.
HowdoesitfeeltoliveinNewYorkCity?
I can remember coming to New York to visit you and telling myself I would never want to live here. I did not see it. I am from Memphis, and there were certain aspects of New York that were just foreign to me, like public transportation and the bodegas and the noise.
But after spending some time in Washington, DC, and Atlanta, living in New York seemed increasingly realistic
HIV organizations have a responsibility, I believe, to speak out against the injustices experienced by the individuals who receive care from them. Social injustices impact one’s medical adherence. They impact one’s ability to see a doctor in person and even impact how an individual receives care. Equitable care, or the lack thereof, impacts how I feel about myself emotionally, mentally and physically.
This is the work I do with clinics in my community engagement lead role: to ensure they see, hear and learn about the community in which they are serving to ensure equitable access to treatment. It is time to challenge HIV organizations that put out ally statements during the summer of 2020 during the height of the Black Lives Matter movement
to me. I look forward to leaning into what New York has to offer in the daytime and nighttime, engaging with creatives and blossoming in that area and becoming one of New York’s most eligible unmarried people. [Laughs]
You’re from Memphis, where yet another video was taken of a Black man experiencing police brutality. Tyre Nichols was brutally beaten by five police officers and died as a result. How does this movement respond? I grew up in the ZIP code where it happened. My activism started in Memphis, so it means a lot to me. I often do not know what to do with the rage that comes because of these incidents. I do go to therapy, and I have learned to channel that rage into my work. I do that by ensuring that the systems in which I work see my Black body, learn of my Black experiences and hear my Black voice.
and push them to examine their own practices and make change.
What matters to you in this moment? After COVID-19 and the racial reckoning this country had in 2020—and is still having—what matters to me the most are honest and authentic relationships.
What matters to me is my voice as a Black man and having the ability to cultivate it and not allow systems or institutions to smother or manipulate it.

It is important for me to be as fearless as possible in this season of my life. Much of this will take consistent work, a measured approach, continued therapy and surrounding myself with the right people. Then some of this is simply about me saying yes to opportunities. ■
Follow Marvell Terry II at facebook.com/ marvell.terry and twitter/marvellous2thet. Go to alai-up.org for more about ALAI UP.
“My role is to make sure that we are on track.”
Marvell Terry II


January 28 marked a milestone in U.S. global HIV advocacy: The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) celebrated an “extraordinary 20 years of impact,” as Ambassador John N. Nkengasong, MD, said in a U.S. Department of State announcement.

President George W. Bush, a Republican, announced the launch of PEPFAR during his 2003 State of the Union address. Although effective HIV treatment became available in 1996, the lifesaving meds were not accessible in many countries across the globe, notably those in sub-Saharan Africa, where an HIV diagnosis remained a death sentence. PEPFAR aimed to change that.
“Through PEPFAR, we have saved 25 million lives, and 5.5 million babies have been born HIV-free. Over a million clients have received pre-exposure prophylaxis [PrEP] to prevent HIV infection,” wrote Nkengasong, who serves as the U.S. global AIDS coordinator and special representative for global health diplomacy at the Department of State.
He added, “Where only 50,000 people in sub-Saharan Africa were on HIV treatment in 2003, today, PEPFAR supports lifesaving antiretroviral treatment for over 20 million adults and children in Africa and beyond. The public

health infrastructure PEPFAR built with our partner countries has been leveraged to support responses for COVID-19, Ebola, and other emerging infectious diseases.”
Through PEPFAR, the United States has invested over $100 billion, including financial resources to the Global Fund to Fight AIDS, Tuberculosis and Malaria, according to the State Department.
Historically, PEPFAR has enjoyed bipartisan support. “My administration is committed to continuing to lead the global HIV/AIDS response,” President Joe Biden, a Democrat, said in a White House statement praising PEPFAR.
“I look forward to working with Congress on PEPFAR’s reauthorization this year.”
Writing in a Washington Post opinion piece, Bill Gates, cochair of the Bill and Melinda Gates Foundation, noted that in recent years, many of the systems put in place to fight HIV were redirected to respond to COVID-19, thus helping safeguard people’s health across the globe.
Urging continued support of the program, Gates added, “We must continue to find and treat people living with the virus. This will not be possible without the continued leadership of the United States—which includes the reauthorization of PEPFAR this year.” Trent
Straube




Tennessee’s Republican leadership announced that the state’s health department will turn down free federal funding to help prevent HIV, reported The Commercial Appeal.
“Restricting access to HIV prevention and testing could lead to increased rates of HIV infection, greater health care expenses and sicker communities,” noted amfAR, The Foundation for AIDS Research, in a statement urging the Tennessee Department of Health to reconsider its decision.
Health experts are concerned that other conservative states may also reject HIV funds. In Tennessee’s case, the money was available through grants from the Ending the HIV Epidemic in the United States initiative, which was launched by President Trump and the Centers for Disease Control and Prevention (CDC). Such funding goes through the Tennessee Department of Health and is distributed to nonprofits that provide HIV prevention, testing,
treatment and other services.
The CDC provides as much as $10 million to Tennessee for HIV programs, Greg Millett, the director of public policy for amfAR, told NBC News. It is unclear how much funding will be rejected this year. Calling the decision by Tennessee’s officials “devastating,” Millett added,“If other states follow suit, we’re going to be in trouble.”

Advocates and Democratic lawmakers argue that Tennessee’s decision is based on politics, not science. That’s because some federal funding goes to HIV programs at Planned Parenthood, which provides sexual health services, including abortions, which many conservative leaders oppose.
Nonprofit groups in Tennessee that receive federal HIV grants were notified that the funding would end May 31 and that the state health department “will utilize other state initiatives to support
all HIV prevention and surveillance staff and activities in funded metro health departments, and those contracts will be in place by June 1, 2023,” reported The Commercial Appeal.

Democratic
As NBC reports, about 20,000 people are estimated to be living with HIV in Tennessee. “I can’t understand why the state would give back funds targeted toward health care,” Diane Duke, president and CEO of Friends for Life, a Memphis HIV service provider, told NBC. “It’s outrageous.” Friends for Life is one of the organizations that received notice that its federal funding would end. —TS
The U.S. global AIDS program has saved 25 million lives.
Experts worry that the move is political and that other states may do the same.Rep. John Ray Clemmons, Republican Gov. Bill Lee







We loathe to give conspiracy theories any attention for fear of spreading misinformation, but we must set the facts straight once again about Magic Johnson and HIV: The iconic athlete did not contract HIV from a contaminated hepatitis B vaccine during a study trial conducted by Anthony Fauci, MD.

“I am certain that I was infected by having unprotected sex with a woman who has the virus,” Johnson wrote in a November 1991 article for Sports Illustrated that The Associated Press references in a recent article. “The problem is that I can’t pinpoint the time, the place or the woman,” he added. “It’s a matter of numbers. Before I was married, I truly lived the bachelor’s life. I’m no Wilt Chamberlain, but as I traveled around NBA cities, I was never at a loss for female companionship.”
To repeat the facts: Magic Johnson did


not contract HIV from a contaminated hepatitis B vaccine. Misinformation about this is deliberately spread online by conspiracy theorists who deny the proven effectiveness of vaccines, specifically the shots that protect against COVID-19. Propagandists also aim to discredit the work of scientists such as Fauci, the recently retired head of the National Institute of Allergy and Infectious Diseases known as America’s doctor. Not only did he lead the country through the COVID-19 pandemic, relaying the latest scientific data and promoting vaccines, but he also guided national health and research efforts through the AIDS epidemic.
Basketball icon Johnson stunned the world on November 1, 1991, when he announced, at the height of his stardom, that he was retiring from the NBA because he was HIV positive.












As an esteemed HIV researcher at Hunter College in New York City, Jeffrey Parsons-Hietikko, PhD, was reimbursed for numerous scuba diving trips (to Cuba, Costa Rica, the Cayman Islands and other locations) that were part of his research, as well as for trips and flights to Denver, Chicago, South Africa and other cities. The research was funded through grants from the National Institutes of Health (NIH).
It turns out, though, that the trips and expenses were for personal use, according to a settlement stemming from a civil fraud lawsuit by Damian Williams, the U.S. attorney for the Southern District of New York.



According to the settlement, Parsons-Hietikko must pay the U.S. government $375,000, and Hunter College, part of The City University of New York (CUNY), must pay $200,000.
While at Hunter, Parsons-Hietikko oversaw the Center for HIV Educational Studies & Training (CHEST), which conducted research on sexual risk behaviors and recreational drug use among men who have sex with men.
According to previous reporting by the New York Post, Parsons-Hietikko drew $37 million in federal grants from 1997 to 2016. He resigned from Hunter in 2019 amid a sexual misconduct scandal.

In November 2021, Johnson marked the 30th anniversary of his public disclosure with press interviews and public statements, tweeting: “God has really blessed me! Today marks 30 years living with HIV so the message resonated with me in such a tremendous way. I thank the Lord for keeping me, giving me strength, and guiding me for 62 years but especially the last 30.”
Over the years, he has used his fame to advocate and educate about HIV issues, and when COVID first struck the nation in March 2020, Johnson publicly urged people to view the coronavirus as a real health threat. —TS


The federal fraud case against him began in 2019 when a whistleblower— now known to be Devin English, who worked for the professor as a researcher—contacted the U.S. attorney’s office and alerted officials about the false claims.
As part of the settlement, Parsons-Hietikko and Hunter College admitted to fraudulently using federal research funds.
“NIH provides funding to academic institutions for the purpose of furthering important research that impacts communities and improves lives,” said U.S. Attorney Williams in the statement. “For years, Jeffrey Parsons-Hietikko obtained these funds under false pretenses, then used them to cover his personal expenses and for other purposes totally unrelated to research. Hunter College improperly used NIH funds to pay undisclosed bonuses to Parsons and for other expenses unrelated to NIH-funded work. When individuals and institutions abuse federal grant money, this Office will hold them accountable.” —TS

This is only a brief summary of important information about BIKTARVY and does not replace talking to your healthcare provider about your condition and your treatment.



BIKTARVY may cause serious side effects, including:
` Worsening of hepatitis B (HBV) infection. Your healthcare provider will test you for HBV. If you have both HIV-1 and HBV, your HBV may suddenly get worse if you stop taking BIKTARVY. Do not stop taking BIKTARVY without first talking to your healthcare provider, as they will need to check your health regularly for several months, and may give you HBV medicine.
BIKTARVY is a complete, 1-pill, once-a-day prescription medicine used to treat HIV-1 in adults and children who weigh at least 55 pounds. It can either be used in people who have never taken HIV-1 medicines before, or people who are replacing their current HIV-1 medicines and whose healthcare provider determines they meet certain requirements.
BIKTARVY does not cure HIV-1 or AIDS. HIV-1 is the virus that causes AIDS.
Do NOT take BIKTARVY if you also take a medicine that contains:
` dofetilide




` rifampin

` any other medicines to treat HIV-1 BEFORE TAKING BIKTARVY
Tell your healthcare provider if you:
` Have or have had any kidney or liver problems, including hepatitis infection.
` Have any other health problems.


` Are pregnant or plan to become pregnant. It is not known if BIKTARVY can harm your unborn baby. Tell your healthcare provider if you become pregnant while taking BIKTARVY.
` Are breastfeeding (nursing) or plan to breastfeed. Do not breastfeed. HIV-1 can be passed to the baby in breast milk.
Tell your healthcare provider about all the medicines you take:

` Keep a list that includes all prescription and over-thecounter medicines, antacids, laxatives, vitamins, and herbal supplements, and show it to your healthcare provider and pharmacist.
` BIKTARVY and other medicines may affect each other. Ask your healthcare provider and pharmacist about medicines that interact with BIKTARVY, and ask if it is safe to take BIKTARVY with all your other medicines.
BIKTARVY may cause serious side effects, including:

` Those in the “Most Important Information About BIKTARVY” section.
` Changes in your immune system. Your immune system may get stronger and begin to fight infections that may have been hidden in your body. Tell your healthcare provider if you have any new symptoms after you start taking BIKTARVY.
` Kidney problems, including kidney failure. Your healthcare provider should do blood and urine tests to check your kidneys. If you develop new or worse kidney problems, they may tell you to stop taking BIKTARVY.
` Too much lactic acid in your blood (lactic acidosis), which is a serious but rare medical emergency that can lead to death. Tell your healthcare provider right away if you get these symptoms: weakness or being more tired than usual, unusual muscle pain, being short of breath or fast breathing, stomach pain with nausea and vomiting, cold or blue hands and feet, feel dizzy or lightheaded, or a fast or abnormal heartbeat.
` Severe liver problems, which in rare cases can lead to death. Tell your healthcare provider right away if you get these symptoms: skin or the white part of your eyes turns yellow, dark “tea-colored” urine, light-colored stools, loss of appetite for several days or longer, nausea, or stomach-area pain.
` The most common side effects of BIKTARVY in clinical studies were diarrhea (6%), nausea (6%), and headache (5%).
These are not all the possible side effects of BIKTARVY. Tell your healthcare provider right away if you have any new symptoms while taking BIKTARVY.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.FDA.gov/medwatch or call 1-800-FDA-1088.
Your healthcare provider will need to do tests to monitor your health before and during treatment with BIKTARVY.
Take BIKTARVY 1 time each day with or without food.
` This is only a brief summary of important information about BIKTARVY. Talk to your healthcare provider or pharmacist to learn more.
` Go to BIKTARVY.com or call 1-800-GILEAD-5
` If you need help paying for your medicine, visit BIKTARVY.com for program information.




















At the 2023 Grammy Awards ceremony, “Break My Soul” singer Beyoncé broke the record for most Grammy wins, with 32. Not only did she become the greatest of all time, but she once again proved to be an ally to the LGBTQ and HIV communities.
While accepting the Grammy for Best Dance/Electronic Music Album for Renaissance, Beyoncé thanked her family and fans and gave a heartfelt shout-out to “the queer community for your love and for inventing this genre” and to her deceased uncle Johnny, whom she said was there in spirit.

Members of the Hive—as Beyoncé’s fans call themselves— and readers of POZ already know why her uncle was particularly relevant to this award. He was gay, and the album Renaissance is a historical homage to the dance music genre so embraced by LGBTQ people.
In 2019, Beyoncé and husband Jay-Z were the Vanguard honorees at the annual media awards ceremony by GLAAD, a national LGBTQ advocacy organization. During that speech, she elaborated on her love of the queer community and her uncle Johnny:
“We’re here to promote love for every human being, and change starts with supporting the people closest to you. So let’s tell them they are loved. Let’s remind them they are
beautiful. Let’s speak out and protect them, and parents, let’s love our kids in their truest form. We’d like to request that we continue to shift the stigmas in this community— especially the stigmas in Black families towards accepting queer Black and brown men and women around the world.
“I want to dedicate this award to my uncle Johnny—the most fabulous gay man I’ve ever met who helped raise me and my sister. He lived his truth. He was brave and unapologetic during a time when this country wasn’t as accepting. Witnessing his battle with HIV was one of the most painful experiences I’ve ever lived. I’m hopeful that his struggle served to open pathways for other young people to live more freely.” —TS
The same device used to take selfies and type out tweets is being repurposed and commercialized for quick access to information needed for monitoring a patient’s health. A fingertip pressed against a phone’s camera lens can measure a heart rate. When the phone is kept by the bedside, its microphone can screen for sleep apnea. Even the speaker is being tapped—to monitor breathing using sonar technology.

In the best of this new world, the data are conveyed remotely to a medical professional for the convenience and comfort of the patient or in some cases to support a clinician without the need for costly hardware.
But the smartphone as a diagnostic tool is a work in progress, experts say. Although doctors and their patients have found some real-world success in deploying the phone as a medical device, the overall potential remains unfulfilled and uncertain.

Smartphones come packed with sen-



sors capable of monitoring a patient’s vital signs. They can help assess people for concussions, watch for atrial fibrillation and conduct mental health wellness checks, to name the uses of a few nascent applications.
Companies and researchers eager to find medical applications for smartphone technology are tapping into modern phones’ built-in cameras and light sensors; microphones;


accelerometers, which detect body movements; gyroscopes; and even speakers. The apps then use artificial intelligence (AI) software to analyze the collected sights and sounds to create an easy connection between patients and physicians.

Some of these products have sought Food and Drug Administration clearance to be marketed as medical devices. That way, if patients must pay to use the software, health insurers are more likely to cover at least part of the cost.
Other products are designated as exempt from this regulatory process, placed in the same clinical classification as a Band-Aid. But the agency is still adjusting how it handles AI and machine-learning-based medical devices to reflect software’s adaptive nature.
Ensuring accuracy and clinical validation is crucial to securing buy-in from health care providers.
 —Hannah Norman and Kaiser Health News
—Hannah Norman and Kaiser Health News

September 2006 was the start of a journey that changed us forever. We’d been married for 21 years and were trying to figure out why Kalvin was having health issues. I was also having health issues, but they were going unnoticed. Kalvin went to many doctors and specialists. They all had the same answer—let me refer you to another doctor. He was put in the hospital in January with PCP (pneumocystis pneumonia) and kidney failure and given two blood transfusions. He was diagnosed with AIDS and AIDS-associated dementia in February. I was also tested and was diagnosed with HIV in April. We started slowly learning all we
could about HIV and started sharing the information. We knew something had to be done because we had no clue this could happen to us.
Fast-forward 16 years and we are now both HIV advocates doing what we can to show people that HIV sets no limitations on transmission. We’ve volunteered with Positive Women’s Network–USA, the Positive Organizing Project and many other organizations.
What three adjectives describe you? Caring, helpful, enthusiastic.
What is your greatest achievement? Being visible as a couple showing people that love can triumph over HIV.
What keeps you up at night? Knowing that people believe HIV is a gay disease. This is what fuels the transmission of the virus. HIV is a people disease—all genders, every age group and every sexual orientation are contracting HIV.
If you could change one thing about living with HIV, what would it be? Truthfully educating people about HIV and how it is transmitted.
What is the best advice you ever
received?
If you want to see things change, don’t wait for others; make it happen yourself.
What person in the HIV/AIDS community do you most admire? Too many to name. All the advocates and activists who paved the way for us to do what we are doing.
What drives you to do this work? Knowing we can and are making a difference in the minds and attitudes of people.
If you had to evacuate your house immediately, what is the one thing you would grab on the way out? Each other!
If you could be any animal, what would you be? And why?
A black jaguar. They are very rare. Only 11% of jaguars have the dark pigment color. They are very solitary, secluded and selective about who can see them.
Read other POZ Stories or share your own at poz.com/stories.
April 4
Filmmaker, educator, poet and activist MARLON RIGGS dies of AIDS-related complications at age 37. (1994)
6

NATIONAL YOUTH HIV & AIDS AWARENESS DAY

May 10
Tony Kushner’s ANGELS IN AMERICA: MILLENNIUM APPROACHES opens on Broadway. (1993) 18

HIV VACCINE AWARENESS DAY
18
NATIONAL TRANSGENDER HIV TESTING DAY 19

A revival of 1985’s offBroadway drama THE NORMAL HEART by Larry Kramer opens on Broadway. (2011)

19
NATIONAL ASIAN & PACIFIC ISLANDER HIV/AIDS AWARENESS DAY 29
Vienna holds its first LIFE BALL, which becomes one of the world’s biggest annual AIDS charity events. The last Life Ball was held in 2019. (1993)

In a blog post titled “Saturday Night Live’s Problematic Send-Up of HIV Medication Ads,” POZ contributing writer Shawn Decker spells out what he believes the long-running NBC variety show got wrong. Below is an edited excerpt.
THE 2023 SEASON DEBUT OF Saturday Night Live (SNL) was hosted by Aubrey Plaza, star of The White Lotus (season 2) and Parks and Recreation. The episode featured a send-up of the recently ubiquitous TV ads for HIV medications. You know them. They’ve played during football games, cooking shows and even during Christmas movies. No matter where you’ve been or what you’ve watched, you’ve seen these ads for HIV medications. They are so relentless that, right now, I think people are more familiar with the folks living with HIV in those commercials than they are with the current cast members of SNL. Kenan Thompson, of course, is a notable exception.

I still watch SNL. Well, on and off. When it’s good, it’s a fun watch. When it’s not, I’m ready. See, I’ve got a Spidey sense for when a sketch is looking to spin in the mud for five or 10 minutes. Like, if a character is a screamer who hasn’t been suitably introduced or written into a funny scenario, I’ll scan them without a second thought. I watch SNL the way Simon Cowell watches contestants on America’s Got Talent—
with a scowl and a raised eyebrow that doubts I will be sufficiently entertained.
One of the areas in which the writers at SNL are the most consistent, unfortunately, is when it comes to sexually transmitted infections (STIs). “I have herpes” or something to that effect is regularly used as a punch line with no setup. So I should have been a little more on guard when the send-up of the HIV ads began.
Foolishly, I thought it would be about how omnipresent the ads are. One of the reasons why they’re doing the sketch is because everyone has seen the source material. The skit is set at a gay club with Aubrey Plaza as the director of an HIV ad. A guy in the ad keeps ad-libbing that he’s straight, and Plaza’s character keeps imploring the actor not to ad-lib.
But he keeps doing it. To his logic, he’s straight, and he’s trying to bring that into his character. Clearly, the joke is he’s an actor taking a gig that he’s not entirely comfortable with. There’s comedy in that concept, clearly, but it wasn’t mined in favor of the hilarity that is homophobia. One of the last of the beleaguered troubadour’s ad-libs
was: “I got HIV the same way Magic Johnson did—from a basketball.”
We haven’t seen so many not-hot takes on Johnson’s HIV status since the early ’90s. For instance, former UFC fighter and current professional blabbermouth Brendan Schaub recently “joked” about not wanting to be near Magic Johnson, alluding to his HIV status.
A recent story from POZ.com debunks conspiracy theories: “Magic Johnson Did NOT Contract HIV From a Hepatitis Vaccine.” My point is, the general public is already still tragically uneducated when it comes to HIV.
Admittedly, I loved hearing one of the cast members in the skit say that taking his HIV medications helps him keep his viral load undetectable, and I think the constant bombardment of HIV ads is doing a good job in educating the general public about Undetectable Equals Untransmittable (U=U).
It’s not going to change anytime soon, but I hope that someday the SNL staff will resist the urge to punch down when it comes to STIs and those of us who are living with them or loving someone who is. ■
In a blog post titled “Why HINAC Is the HIV Event We Desperately Need,” POZ contributing writer Mark S. King urges anyone interested in learning more about HIV criminalization to attend. Below is an edited excerpt.
THE ISSUE OF HIV CRIMINALization used to intimidate me because I didn’t understand state laws, much less how to change them.
Thank God I got a scholarship to the Sero Project’s first HIV Is Not a Crime Training Academy (HINAC) in 2014. It opened my eyes and introduced me to dedicated, kick-ass activists, most of them living with HIV, who showed me how they were already rolling back dangerous statutes that are prosecuting and jailing people for no other reason than their HIV status. And yes, this grotesque injustice is going on right here in the United States.
The next HINAC is taking place from June 4 to 7. I urge anyone with any level of knowledge of this issue or who wants to get an education about it to consider attending. Trust me when I tell you that HINAC is a life-changing experience, focused on real education and interaction, where you will meet people whom you will know and admire for the rest of your life. Yes. Really.
My favorite part of HINAC is how it is very deliberately unlike any other conference you might have attended. There
is no swanky host hotel. There are no Big Pharma gift bags or ballroom-sized catered lunches. Instead, HINAC is held on the campus of a university, where we all stay in dorm rooms and eat in the cafeteria. If that sounds like roughing it to you, maybe it is. Give in. You’ll love it.
Look, I’m as bougie as the next privileged gay guy, but I have been to every in-person HINAC and always had a blast. You won’t be clicking through Netflix selections in your hotel room. You’ll be laughing with, and learning from, all your new friends in the middle of a college campus.
Most people know HIV criminalization from biased news stories of people who didn’t disclose their HIV status to partners—stories that usually don’t mention that the person living with HIV was undetectable or used other protection or otherwise did not expose their partner to HIV or the very complicated issue of HIV disclosure—but it’s so much more than that.
If you’re living with HIV and get arrested for something unrelated to your status, criminal charges could be heightened simply because of the virus in your body.

And get this. Right now, Tennessee is going through an HIV funding nightmare because the state is cutting off its own federal funding from the Ending the Epidemic initiative just so it can limit money to Planned Parenthood, which provides HIV services, and other similar groups. The state is willing to walk away from millions and millions of dollars in HIV funding just to make a political statement.
What does this have to do with HIV criminalization? The county in Tennessee that will suffer the greatest loss of funding is Shelby County. And Shelby County is also the place where the largest number of people living with HIV have been prosecuted. It’s all connected. Go figure.
There’s so much more to say, but you can find out more about criminalization and HINAC on the Sero Project’s website (SeroProject.com) and Facebook page (Facebook.com/TheSeroProject).
This year, HINAC will be held at Emory & Henry College in Emory, Virginia. Sero’s presenting partner organizations are THRIVE SS, U.S. PLHIV Caucus, Positively Trans and the Positive Women’s Network–USA. ■


Since 1999, National Black HIV/AIDS Awareness Day (NBHAAD) has been observed each February 7. Although African Americans make up only 13% of the U.S. population, they account for 42% of HIV cases. This year’s NBHAAD theme, “Together, We Can Make HIV Black History,” emphasized the collective effort required to remedy this inequity and underscored that February is also Black History Month.
On NBHAAD 2023, advocates staged actions, tested via mobile units and paid tribute to fellow advocates. By lucky coincidence, on the eve of NBHAAD (during an unrelated event), Tony-winning Broadway actor (most recently for Hadestown) and long-term survivor André De Shields, a self-described Afro Queer man, was honored for his longtime HIV advocacy by friends and fellow thespians at a GMHC cabaret and auction event held at Joe’s Pub in New York City.
1. A week in advance of GMHC’s 10th Annual Cabaret & Howard Ashman Award, journalist Frank DiLella interviewed honoree André De Shields for NY1. A Tony and Emmy winner, De Shields has been living with HIV for more than 40 years. 2. Award-winning composer Marc Shaiman serenaded De Shields at the February 6 event. De Shields received the Howard Ashman Award for his advocacy of people living with and affected by HIV and AIDS. 3. Members of CAN Community Health’s Phoenix team were on hand to test folks for HIV at Peoria, Arizona’s Multicultural Music Fest and Black History Celebration. 4. Iris House, which serves women, families and underserved populations affected by HIV, observed NBHAAD by honoring Black advocates at its Harlem headquarters and offering free HIV testing.


5. On NBHAAD, Emmy and Tony winner Billy Porter shared a clip of an interview he did with Drew Barrymore last year about overcoming his shame about his HIV status and urged folks to get tested.

6. For NBHAAD, the Elton John AIDS Foundation interviewed Dafina Ward, JD, executive director of the Southern AIDS Coalition, who discussed how historical inequality has contributed to high rates of HIV in the South, especially among African Americans.

7. New York City Council Member Pierina Sanchez (bottom, far right) joined advocates at City Hall on NBHAAD to rally support for a bill that would require the city’s health department to ramp up rapid testing for sexually transmitted infections, prioritizing communities in boroughs with higher infection rates.
8. Members of Positively U Inc.’s Winter Haven, Forida team tested Polk County residents on NBHAAD. In honor of Black History Month, they did so at the Larry Jackson Branch Library, named after the civil rights leader and attorney.


9. The HIV Modernization Movement of Indiana, which seeks to update antiquated HIV criminal and public health laws, raised awareness of racial disparites concerning HIV at the Indiana Statehouse on NBHAAD.

10. On NBHAAD, Health Stop St. Louis’s HIV prevention team promoted the importance of doing equitable HIV work within the Black community.

Mortality among people with HIV continues to decline over time as antiretroviral treatment and access to care have improved, but gender and racial disparities persist. Researchers analyzed all-cause mortality and premature death among more than 6,500 people with HIV who received care at the Vanderbilt Comprehensive Care Clinic in Nashville between January 1998 and December 2018. A total of 956 people (15%) died during the course of the study. People who received care during 2014 to 2018, when treatment was more effective and easier to take, had a 78% lower risk of death than those treated during 1998 to 2003, after effective combination therapy first became available. Overall, women had an increased risk of death compared with men. Black women had the highest premature mortality—that is, the largest number of years of potential life lost—followed by Black men, white women and white men.

“Despite marked improvement over time, sex disparities in mortality as well as sex and race disparities in years of potential life lost remained among people with HIV in this cohort,” Rachael Pellegrino, MD, MPH, of Vanderbilt University Medical Center, and colleagues concluded.
Another study looked at differences in initial antiretroviral therapy prescription for nearly 43,000 people entering HIV care in the United States. Here, too, the researchers compared two time periods: 2007 (when the first integrase inhibitor was approved) to 2015 and 2016 to 2019. The overall probability of receiving a prescription for antiretroviral therapy did not differ significantly according to race/ethnicity. During the earlier period, Black and Latino people were significantly less likely to receive an integrase inhibitor, but this gap closed after treatment guidelines made these drugs the sole preferred option for first-line therapy.
Women living with HIV are underrepresented in late-stage clinical trials of new treatments, and the disparity is particularly stark for Black women. Women account for 19% of people newly diagnosed with HIV and nearly one quarter of people living with HIV in the United States. About 60% of newly diagnosed women are Black, while white and Latina women each account for around 20%.









women account Researchers with the Food and in Phase III antiretroviral trials submitted to the agency in various countries
respectively, among men. But in U.S. trials, only 11% were women, of whom 34% were white and 62% were Black. The researchers calculated that, overall, women were not adequately represented in clinical trials relative to their share of the HIV population. But when this was broken down by race, there was a disparity for Black women but not for white women.


not women. trial is because may work or men versus women. have found that women may not trials for a of reasons, including lack of awareness, responto access.
women were

Researchers with the Food and Drug Administration looked at women’s participation in Phase III antiretroviral therapy trials submitted to the agency since 2010. The analysis included 18 studies conducted in various countries that together enrolled more than 13,000 previously untreated participants, including about 5,300 in the United States. Overall, 15% were women; 45% of the women were white and 36% were Black, compared with 69% and 18%,
Representative trial participation is important because therapies may work differently or have different side effects in men versus women. Previous studies have found that women may not join trials for a variety of reasons, including lack of awareness, family responsibilities and barriers to access. “Additional research into innovative approaches to recruit and retain females in clinical trials should continue,” the study authors concluded.
tive to the authors concluded
Tenofovir disoproxil fumarate/emtricitabine (TDF/FTC; Truvada or generic equivalents) for pre-exposure prophylaxis (PrEP) is generally safe for the kidneys, according to a recent study.

Jean-Michel Molina, MD, and colleagues with the French ANRS-PREVENIR Study Group assessed the impact of different PrEP dosing regimens on kidney function. The analysis included 1,235 participants, mostly gay and bisexual men, in the PREVENIR trial, which compared daily PrEP versus on-demand PrEP before and after sex. Because of TDF’s known effect on the kidneys, the trial was limited to people with adequate kidney function at baseline. For this analysis, they were divided into three groups: daily use (40%), on-demand use (39%) and those who switched (21%); the three groups took a median of 6.0, 1.7 and 4.0 pills per week, respectively.
The researchers looked at estimated glomerular filtration rate (eGFR), a measure of how fast the kidneys filter toxins such as creatinine out of the blood. Over a median follow-up period of about two years, eGFR declined slightly in the daily and switch groups but rose slightly in the on-demand group, but the researchers did not consider these small changes to be clinically important. Only five people, distributed across the groups, saw an eGFR decline of 25% or more.
“In our study, the renal safety of PrEP with tenofovir disoproxil fumarate/emtricitabine was good, whatever the dosing regimen,” the study authors concluded. “On-demand PrEP dosing had a smaller impact on eGFR evolution than daily PrEP, but the difference was not clinically relevant.”
Latino people living with HIV experience stigma and health care discrimination that could contribute to health disparities. Latinos are disproportionately affected by HIV, accounting for about a quarter of all people living with the virus and 29% of new cases in the United States while making up 19% of the population.
Researchers with the Centers for Disease Control and Prevention analyzed data collected during 2018 to 2020 from 2,690 HIV-positive Latino adults, mostly men, who participated in the Medical Monitoring Project, an annual study of experiences and outcomes among people living with HIV. Stigma was measured using a 10-item scale that included personalized stigma, disclosure concerns, negative self-image and public attitudes. The survey also asked about seven types of health care discrimination.

Self-reported stigma was common. Up to 78% of those who experienced stigma had concerns about disclosure. Latina women reported more stigma than Latino men, and stigma scores were higher for those who identified their race as American Indian, Native American or Black. Nearly one quarter of participants said they had experienced health care discrimination during the past year. More than 60% of those reporting discrimination said health care providers didn’t listen to them, and 48% felt they were not treated with courtesy or respect. Here, Latina women were less likely than Latino men to report discrimination, and those who identified as Black reported more discrimination.
“HIV stigma and discrimination are human rights issues associated with adverse HIV outcomes,” the study authors wrote. “Eliminating stigma and discrimination, which are barriers to HIV care and treatment, is a national priority.”

Another large clinical trial has been halted after Johnson & Johnson’s experimental HIV vaccine was found to be safe but not effective against HIV. The Phase III Mosaico study enrolled 3,900 cisgender gay and bisexual men and transgender women in North and South America and Europe. Participants received four doses of a vaccine called Ad26.Mos4.HIV that uses an adenovirus vector to deliver antigens from multiple HIV strains plus two doses of a second vaccine containing gp140 proteins. An interim data review found that the number of people who acquired HIV was statistically equivalent in the vaccine and placebo groups. The results were not surprising, as a parallel trial dubbed Imbokodo was halted in 2021 after interim results showed that a similar vaccine regimen did not protect young women in Africa. The news adds to a long string of disappointments in HIV vaccine research. Mosaico was the last large trial testing a traditional vaccine for HIV prevention. Most experts now think more sophisticated approaches will be needed.

Sunlenca (lenacapavir), a long-acting medication recently approved for treatment-experienced people with multidrug-resistant HIV, also works well for people starting antiretroviral therapy for the first time. Sunlenca, from Gilead Sciences, is the first approved HIV capsid inhibitor. It remains active against HIV that has developed resistance to other drugs, and its long half-life allows it to be administered once every six months. The Phase II CALIBRATE trial enrolled 183 previously untreated participants. They were randomly allocated to four groups, receiving daily Sunlenca pills or twice-yearly injections in combination with other antiretrovirals or else a standard oral regimen. At 54 weeks, 85% to 90% of those who took Sunlenca plus tenofovir alafenamide or bictegravir had an undetectable viral load. Treatment was generally well tolerated. The most common side effect was mild to moderate injection site reactions. This new long-acting injectable is a welcome option, but it still needs an equally durable partner to construct a complete twice-yearly regimen.
HIV may lie dormant in a distinct viral reservoir in the brain and spinal cord, which could present another barrier to a cure. Antiretroviral therapy can keep HIV in check as long as treatment continues, but the virus inserts its genetic blueprints into human DNA and establishes a long-lasting reservoir in resting CD4 T cells in blood and lymph tissue. Now, a study suggests that HIV may establish multiple reservoirs. Researchers compared genetic sequences of rebounding virus in blood and cerebrospinal fluid (CSF) from 11 people soon after treatment interruption. About half experienced pleocytosis, or transient entry of white blood cells into the central nervous system. Some of them had differing viral sequences in the blood and CSF, suggesting they arose from distinct populations of latently infected cells. In contrast, resurgent virus in the blood and CSF was similar in those who did not experience pleocytosis. These findings suggest that HIV cure strategies may need to reach latent virus in the brain as well as in T cells in the blood and lymph system.
Older people living with HIV who recently used cannabis are about twice as likely as nonusers to sometimes miss doses of their antiretroviral medications, according to a recent study. Many people with HIV use marijuana to improve appetite, manage pain or relieve depression or anxiety. Researchers looked at the link between cannabis use and treatment adherence among 1,011 participants ages 40 or older in a long-term study of HIV-positive adults. All were on antiretroviral therapy, and most had an undetectable viral load. Within this group, 18% reported current cannabis use (during the past month), 6% reported intermittent use (during the past year but not the last month) and 76% had not used cannabis within the past year or ever. Current cannabis users were 53% more likely to report less than perfect adherence than nonusers. Among people who missed at least one dose during the past week, 21% were current cannabis users, 19% were intermittent users and 10% were nonusers. When the data were broken out by sex, the association was statistically significant for men but not for women.
SYPHILIS IS A SEXUALLY transmitted infection caused by Treponema pallidum bacteria. It can be cured with antibiotics, but if left untreated, it can cause severe complications, including heart damage and neurological problems.
Gay and bisexual men have the highest rate of syphilis, but it is increasing among heterosexual men and women, and congenital syphilis in newborns is on the rise. HIV-positive people with syphilis lesions are more likely to transmit HIV, and HIV-negative people with syphilis sores are more likely to acquire the virus. People living with HIV— especially those with a low CD4 count— may develop more severe syphilis and may not respond as well to treatment.
Syphilis has been dubbed “the great imitator” because its symptoms can resemble those of many other conditions.
Primary syphilis typically starts as a painless sore known as a chancre. These appear most often on the penis, vulva, vagina, anus or mouth—the sites where the bacteria enter the body. The initial sore usually heals without treatment, but the person remains infected.
Secondary syphilis usually develops within several weeks after the initial chancre has healed. The most common symptom is pox-like lesions that can appear anywhere on the body, including the palms of the hands and soles of the feet. Other symptoms may include fever, swollen lymph nodes, sore throat,
fatigue, hair loss, headache and muscle aches. Symptoms typically resolve within several weeks, but the bacteria remain in the body.
Latent syphilis is an asymptomatic stage that can last for years. People with latent syphilis are less likely to transmit the bacteria, but treatment is recommended to prevent serious late-stage complications.

Tertiary syphilis occurs in up to one third of people who remain untreated, usually 10 to 30 years after initial infection. The bacteria can damage organs throughout the body, including the brain, nerves, eyes, ears, heart, blood vessels, liver, bones and joints.
Neurosyphilis occurs when the bacteria infect the nervous system. Neurosyphilis, ocular syphilis (affecting the eyes) and otosyphilis (affecting the ears) can occur at any stage of infection. Neurological damage may lead to numbness, paralysis, blindness, deafness, cognitive impairment and dementia.
Congenital syphilis occurs when a mother passes the bacteria to her baby during pregnancy or delivery. Congenital syphilis can cause miscarriages, stillbirth and premature birth. Many infants don’t have any symptoms at birth, but if left untreated, they can develop serious complications including bone or teeth deformities, neurological problems, blindness and deafness.
Syphilis is usually passed from person to person through direct contact
with active sores during vaginal, anal or oral sex. The bacteria are present in semen and vaginal fluid. It’s important to avoid contact with sores during sex and to avoid having sex if you have active lesions. Condoms can reduce the risk, but they’re not fully protective because sores can occur in areas not covered by a condom. Recent research shows that taking doxycycline as post-exposure prophylaxis after sex—known as doxy PEP—reduces the risk for syphilis in people at high risk.
Get tested if you have symptoms suggestive of syphilis or if a sex partner has tested positive. The Centers for Disease Control and Prevention recommends regular testing—even if asymptomatic—for sexually active gay and bisexual men, people with HIV and those using HIV pre-exposure prophylaxis (PrEP). Pregnant people should be tested during their first prenatal visit.
Syphilis can be treated at any stage. The standard treatment is injectable benzathine penicillin. A single injection in the buttocks is usually enough to treat primary or secondary syphilis. People with late-stage syphilis should receive weekly penicillin injections for three weeks. Neurosyphilis and eye and ear manifestations require more intensive treatment. Follow-up blood tests should be done after treatment to make sure it was successful. And remember: Syphilis does not confer immunity, so it is possible to get it again. ■
If left untreated, syphilis can lead to severe health problems and even death.

Even though we all seem to lead busy lives, it’s important to slow down to eat your food. Instead of eating as quickly as possible, give your stomach time to tell your brain it’s full.


THIS QUICK RECIPE CAN MAKE A GREAT BREAKFAST or a satisfying lunch. Mushrooms are rich in vitamins and minerals—like selenium, an important antioxidant for metabolic health—and eggs pack a nice hit of protein.
SERVINGS: 4 / INGREDIENTS: 9 / PREP: 20 MINUTES
INGREDIENTS
1 tablespoon olive oil



2 cloves garlic, sliced
2 cups portobello mushrooms, diced
1 cup cherry tomatoes, halved
1 tablespoon fresh oregano, chopped 4 slices of whole grain bread, toasted (use white bread if on bland, low-fiber diets)
¼ cup soft goat or cream cheese, divided 4 soft-boiled eggs



Salt and pepper, to taste

1. In a wide skillet with a tight-fitting lid, heat the olive oil over medium-high heat. Add the garlic and cook for 3 minutes or until fragrant and beginning to turn golden.
2. Add mushrooms, cherry tomatoes, chopped oregano and a sprinkling of salt and pepper. Cover and cook for 5 minutes. Uncover and stir, and cook for another 2 minutes. Taste for seasoning. Turn off the heat, and let sit until ready to serve.
3. Evenly spread 1 tablespoon of goat or cream cheese on each of the slices of toast. Top with the mushroom mixture and then the soft-boiled egg. Serve immediately.
CHEF TIPS
For a tasty touch of England, add a tablespoon of Worcestershire sauce to the mushrooms along with the other ingredients. If portobellos are not available, quarter some baby bella, cremini or button mushrooms.
NUTRITION FACTS (per serving)
Calories: 242; fat: 14 g; saturated fat: 5 g; polyunsaturated fat: 2 g; monounsaturated fat: 6 g; carbohydrates: 19 g; sugar: 5 g; fiber: 4 g; protein: 11 g; sodium: 411 mg
©2023 Fred Hutchinson Cancer Research Center, a 501(c)(3) nonprofit organization. Used with permission.




To eat more slowly, try eating with your opposite hand. As strange as it may seem, it works. If you have issues with overeating or scarfing down your food too quickly, this technique will help you slow down while eating and help you feel fuller faster.

on at



IAS 2023, the 12th IAS Conference on HIV Science, will take place in Brisbane, Australia, and virtually from 23 to 26 July.






















A NEW GENERATION IS USING THE SOCIAL MEDIA SENSATION TO PROMOTE SEXUAL HEALTH.





















Khartoon Weiss, the global head of agency and accounts at TikTok, defines the app as an entertainment platform rather than a social network. TikTok users can while away hours watching short videos of dance challenges, lip synchs, makeup tutorials, workout tips, recipes, pranks and more.
TikTok is not without controversy. The app was launched by the Chinese company ByteDance, and by law, the Chinese government can compel any company to share any user data it collects.

In December, Chris Wray, director of the Federal Bureau of Investigation, told the House Committee on Homeland Security during a hearing that the FBI had security concerns, including the possibility that the Chinese government was using the app to gather private information about its users. And in February, Texas Governor Greg Abbott called for a ban of the app on all government devices, citing security risks.

Despite the big white balloons of controversy, TikTok continues to delight its users, especially young people. Some of them are also using the platform to spread awareness of HIV and sexual health via compelling content that employs humor and music to draw viewers and spark important conversations. Below are four such advocates.
@oliverwongcomedy
Los Angeles
Oliver Wong’s TikTok features clips from his hilarious standup, stories about his life in Southern California, racism challenges and a smidge of groovy dancing, but his most viewed videos are about HIV. The Taiwanese native came to the states seven years ago to attend film school and tested HIV positive two years ago. Two months after his diagnosis, he started chronicling his HIV journey on TikTok.
In a video that has garnered over 556,000 views, Wong talks about how he discovered he was living with HIV. “Within two to six weeks of your initial HIV infection,” he says in the video, “you develop flu-like symptoms. So I believe I was infected in November of 2020.” He goes on to describe the symptoms he started feeling a month or so later, which he thought might have been due to COVID. It wasn’t until February 2021 when he went to get tested for sexually transmitted infections (STIs), which he does regularly, that he found out he had HIV.

Wong was using TikTok before he was living with HIV. “As a stand-up comedian,” he says, “one of my jobs is to be as honest and sincere as I can be onstage so people can relate to me. Once I got HIV, I was like, I don’t want to hide. I don’t want to be funny onstage [without disclosing], there is a secret inside of me, which is HIV.” Because he already exposes so much of his life—his parents, his Asian-ness, his sexuality—in his stand-up and on social media, it was only natural that he add HIV to the mix. “I started to write jokes about HIV, and then I started to talk about it onstage,” he says, “and then after a month or two, I started to translate those jokes to TikTok.”
Wong, who also works as a director of straight adult films, has found that using TikTok has helped him deal with his diagnosis. “It’s really a therapeutic experience for me to make peace with my status as an HIV-positive person,” he says. “I think by talking about it in public, it really helps me to accept the fact that I’m dealing with this new reality.”

As for making jokes about HIV? Wong says it’s a soft way to get people to pay attention. “Humor lets people ease into a heavy topic such as HIV,” he says. “By making HIV a topic so light and digestible, I believe most people would be able to listen more. Most people associate HIV with death, which is not the case anymore—with modern medical advances— so I think using humor to talk about it can reverse people’s assumptions.”
@jscotttv
Atlanta
Johneri’O Scott didn’t start using TikTok until August 2022, but he already has over 45,000 followers and 583,000 likes for his videos.


“I thought, Let me do things that educate and inspire and empower people,” Scott says. “Let me put myself, my life, as a living testament for those who may be feeling like they just contracted HIV and they’re going to die.” He wants to let people know the truth about HIV.
Scott was diagnosed with HIV in 2014, but he knew he couldn’t let the diagnosis stop him. “I just had to educate myself because the stigma [and misinformation] around HIV was so thick, like if you have HIV, you’re going to get AIDS. If you have HIV, you’re going to die.” After educating him-
HERE’S NO DENYING THE GROWING POWER and influence of TikTok. With 1 billion active users globally, the short-form video app has been steadily gaining users since its launch in 2016, with a notable surge in the past few years amid the COVID-19 pandemic.
self about the virus, finding support groups and community and asking a lot of questions, he wanted to help educate others. “That’s when I fell in love with education of HIV and STDs [sexually transmitted diseases, or sexually transmitted infections (STIs)],” he says, “and just how many lives I’ve touched since coming out with my own story.”
Scott’s empowering TikTok videos tell the truth about HIV, shedding light on topics such as Undetectable Equals Untransmittable (U=U), pre-exposure prophylaxis (PrEP), HIV and STI testing and





more. In a video that has earned 2.9 million views, he humorously outlines how to tell whether your man has an STD. “Honey, if he’s pre-cummin’ way before you get started in bed, then guess what? Run! It may be an STD!”





One of the risks of being so visible on TikTok is that some viewer comments can be harsh, but Scott takes it in stride. “I know I’m comfortable with myself,” he says, “when they be like, ‘He’s lying—he don’t have HIV’ or ‘He’s just putting on a front,’ I just keep strolling, because you don’t really know me, and I don’t really know you.” He just continues





doing his work: producing informative TikTok videos and encouraging regular HIV and STI testing. “When it comes to your sexual health,” he says, “you have to be really selfish.”
Melissa Strype, 34 (she/her)
@thebiglissa
Los Angeles

In one of Melissa Strype’s TikTok videos, which has over 109,000 views, she’s strolling down the aisle of a national






office supply chain rapping, “Get to know your groin! How it smells! Take a whiff, make a note! Write it down! What’s going down down there? I said, ‘What’s going down down there?!’”













Strype has been working in the sexual health arena for years, but her videos have opened up a new avenue for education. “I’ve been creating these comedic music videos about sexual health topics,

and the topics are requested by my audience. So many young people are like, ‘Can we do one about consent?’ ‘Can we do one about this STI?’ ‘Can we do one about pubic hair?’”


Strype is not shy about any topic. She’s tackled smegma, sharts, queefs and condoms, and she believes using comedy is key. “If we can laugh about these really sensitive, scary, embarrassing topics, we’re open to thinking about things in new ways,” she says, “If we’re able to laugh, we’re opening ourselves up to having important conversations.”
Strype’s TikTok is a starting point. “There’s a lot of great people doing work online talking about these issues in a more complex way,” she says, “and what I try and do is really distill it down to a silly little thing that kind of gets caught in people’s heads but that is going to make them laugh. But laughing to the point where they’re like, ‘OK, yeah, I get the overall message that she’s saying, and I’m going to see how that applies to my life.’”

“My whole goal of doing this work online is to exude empowerment for folks,” Strype says. She hopes that her use of comedy and music will inspire viewers to have conversations. “I hope they might say, ‘I really enjoyed that. Let me think about this. I feel like I can go to my doctor.’ ‘I can talk to my partner.’ ‘I can talk to my parent about this kind of stuff.’”
Chase Cramer, 27 (he/him, they/them)
“I pretty much went viral from showing cum on the walls,” Chase Cramer says. The trans man is talking about their presence on TikTok, which centers on LGBTQ-inclusive sexual education. Cramer, who has over 225,000 followers, uses the platform to discuss HIV and STI testing, PrEP, sex toys and adult bookstores as well as more personal issues, like their pregnancy scares, hair loss and dealing with transphobes.
Cramer started making videos on TikTok about three years ago in their native New York. “I was working as a public health educator, traveling to various high schools with a nonprofit,” they say. Cramer taught topics like HIV or birth control—whatever aspect of reproductive health the teacher wanted taught.
“When COVID hit, I launched a social media for the nonprofit. I started a TikTok for them, and it went viral,” Cramer says, “It was doing really well. I reached the outreach numbers for the entire five-year grant in one month,
without spending a single company dollar.”
Unfortunately, Cramer says, their work at the nonprofit was discounted and downplayed. They were furloughed and took a job at an adult store. “I started ‘Sex Tour Story Time,’ which is how I started my social media.” The store had an arcade of adult video viewing booths, and Cramer would talk about the wild things that took place at the store and the people who came in.
Cramer would also tour other arcades. “I was like, ‘Hey! This is what arcades are,’” Cramer says. “There’s no need to be afraid of them. Here are some of the social rules I’ve learned. Like, some guys are on Grindr, but some of them, like the older guys, might leave a penny outside the door to let you know they’re available.”
Due to challenges finding enough work during the COVID lockdown, Cramer moved to Phoenix and startedworkingasaphlebotomist and social outreach educator. They used the TikTok platform to educate people and tackle topics some folks might be afraid to ask about.
“When I was an educator, I felt so limited by the education I could provide because it was all scripted, and there are so many laws around what’s deemed appropriate to teach teenagers,” Cramer says. Through their TikTok, Cramer has been able to educate much more freely. “These topics that are considered taboo or inappropriate,” they say, “that’s the fire that lighted in me to start doing social media.”
“My journey with TikTok has been a long and rough one,” they say, “as the guidelines have constantly changed. For the longest time, I couldn’t say the words condom or lube without my videos being taken down.” Cramer has also experienced people reporting their videos simply because they are trans. “I had some very conservative, MAGA Republican, Proud Boy kind of hate. Sometimes I’ve had to take breaks for months at a time.”
Cramer always returns, though, because they believe in the work. “I don’t get paid for most of the work that I do on TikTok,” they say, “Our sex ed [in the United States] is just so not realistic to the realities of sex. Our sex ed is: This is a condom,’ ‘This is HIV,’ ‘This is STIs,’ ‘You could get pregnant; here’s birth control.’ You can’t talk to teens about pleasure because that’s inappropriate.”
Cramer acknowledges that they still have to jump over hurdles when it comes to nonprofit work and the challenges of TikTok, but this platform allows them to push the envelope further and bring up more of the realities of sex. After all, Cramer says, “one of the most basic and probably the most universal human experiences is an orgasm.” ■
“THESE TOPICS THAT ARE CONSIDERED TABOO OR INAPPROPRIATE—THAT’S THE FIRE THAT LIGHTED IN ME TO START DOING SOCIAL MEDIA.”

 BY LIZ HIGHLEYMAN
BY LIZ HIGHLEYMAN
ARD 86, THE FIRST DEDICATED HIV INPATIENT clinic in the United States, marked its 40th anniversary with a celebration at Zuckerberg San Francisco General Hospital (ZSFGH) on January 25. A key element of the so-called San Francisco model of comprehensive community-based care, the clinic has pioneered innovations in HIV treatment and prevention that have been adopted nationwide and around the world.
“Treatment has dramatically changed the lives of our patients,” said Diane Havlir, MD, chief of ZSFGH’s HIV, Infectious Diseases and Global Medicine Division, at the event. “But two things about Ward 86 have not changed. Number one, it is patient-centered. And second, we are constantly figuring out better ways to deliver all the scientific advances in HIV to our patients. I tell people that Ward 86 is the Silicon Valley of innovation for AIDS care.”
The Ward 86 outpatient clinic opened its doors in January 1983, followed by the opening that July of Ward 5A, ZSFGH’s designated inpatient ward for people with AIDS.
“Between the outpatient and the inpatient units, we launched a number of research initiatives and clinical care programs to improve the care of those living with HIV, not just in San Francisco but to provide models for HIV care around the country and internationally,” Ward 86 medical director Monica Gandhi, MD, MPH, told POZ.
Former National Institute of Allergy and Infectious Diseases director Anthony Fauci, MD,
who stepped down from his position this past December, offered his congratulations in a video address.
“Ward 86 has a special place in HIV’s history dating back to the early dark days when San Francisco was the epicenter of the HIV epidemic in this country and previously healthy young individuals were dying despite our best efforts to provide the supportive treatments available to us at that time,” he said. “What has become known as the San Francisco model became renowned as the best approach to HIV patient care in the world.”
Ward 86 has been at the forefront of the innovations in care and treatment that turned an inevitably fatal disease into a chronic, manageable condition.
“The research over the years at Ward 86 has been stellar, from some of the earliest and most important clinical trials to implementation research, notably for people experiencing homelessness and other hard-to-reach individuals,” Fauci recalled.
Ward 86 investigators helped lead some of the major clinical trials of experimental HIV treatments, including the first trial of AZT (Retrovir) and studies of protease inhibitors and combination antiretroviral therapy, which began to turn the epidemic around in the mid-1990s.
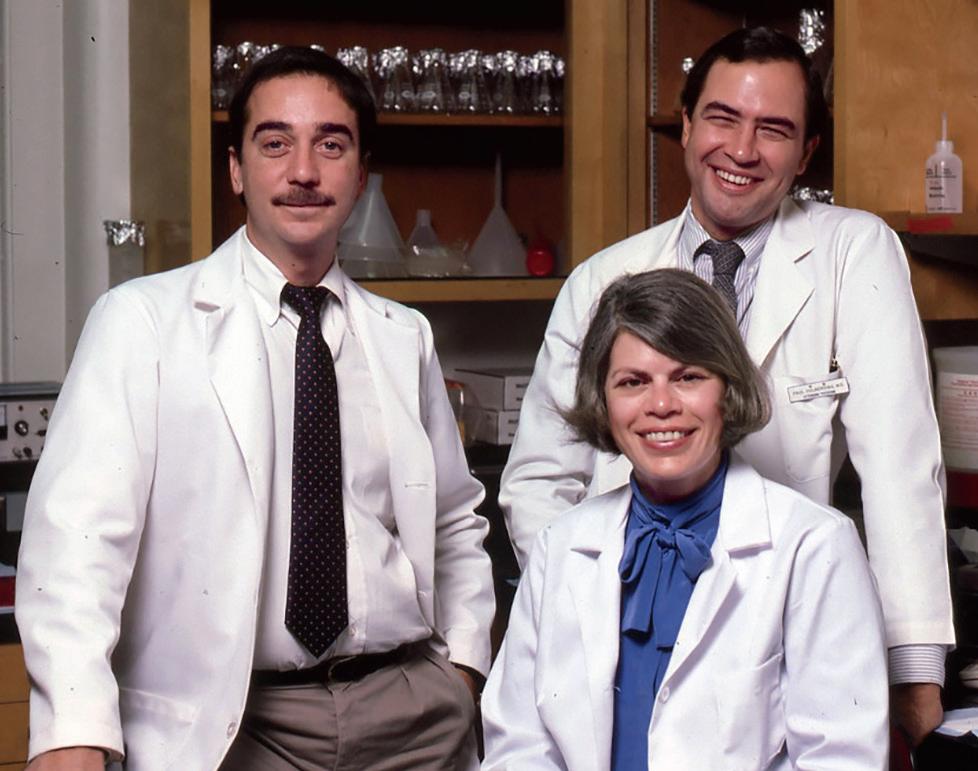
In 2010, even before the START trial definitively showed that early treatment initiation leads to better outcomes, Ward 86 and other San Francisco Department of Public Health (SF DPH) providers were the first to recommend antiretroviral treatment for all people diagnosed with HIV, regardless of CD4 T-cell count—two years before national guidelines did the same.
In 2013, Ward 86 created its RAPID ART program, which helps people start treatment as soon as possible after diagnosis to avoid falling through the cracks while waiting for test results or follow-up appointments.
Ward 86 also continues to play a role in HIV cure research. Steven Deeks, MD, and colleagues have been studying a cohort of elite controllers, people who are able to naturally control the virus without antiretrovirals, in an effort to learn how to achieve long-term remission.

In a video address that he started at Ward 86 in 1993, Deeks recalled “one of the low points” when it had become
clear that available treatments were not working. In 1995, he and colleagues at the University of California San Francisco (UCSF) and the University of Pittsburgh tried an idea “that sounded completely crazy and still does”: giving activist Jeff Getty a baboon bone marrow transplant, which led to insights about the role of inflammation in HIV disease.
“Everywhere I went, people wanted to figure out what was the ‘magic sauce’ that made everything so unique at Ward 86,” Deeks said. “I always thought it was this amazing collaboration between patients and providers and the academic community and all the virologists and immunologists at UCSF and all the resources that were available. It all came together on Ward 86 at that time and since then.”
As Fauci noted, the population affected by HIV in San Francisco has changed over the years.
In 2008, Ward 86 opened a women’s clinic. It launched the SALUD clinic for Spanish-speaking clients in 2016. The following year saw the debut of the Golden Compass program, which provides comprehensive care for HIVpositive people over age 50. According to SF DPH’s latest HIV epidemiology annual report, 73% of city residents living with HIV are 50 or older. And Ward 86 does not limit

itself to HIV treatment; it also runs a pre-exposure prophylaxis (PrEP) clinic for HIV prevention.
Today, Ward 86 serves some of the city’s most disadvantaged people living with or at risk for HIV. Many are living in poverty, 96% rely on Medicaid or Medicare, a third lack stable housing and rates of mental illness and substance use are high.
“The model of HV care at Ward 86 evolved as the epidemic unfolded and has continued to adapt to the many changes seen in more recent years,” Paul Volberding, MD, who founded Ward 86 with Donald Abrams, MD, and the late Constance Wofsy, MD, told POZ. “From the start, it brought needed services of many forms to a single site in a coordinated, compassionate and effective manner that is truly responsive to patient needs.”
In 2019, Ward 86 launched the POPUP program to provide specialized HIV care for homeless and marginally housed people. According to the city’s latest epidemiology report, 24% of individuals newly diagnosed with HIV inSanFranciscoin2021werehomeless. What’s more, HIV-positive people experiencing homelessness are least likely to have an undetectable viral load, at just 27%.
The latest Ward 86 initiative is SPLASH (Special Program on LongActing Antiretrovirals to Stop HIV), which aims to broaden the use of long-acting injectable treatment to a safety-net population. (See sidebar, “A Long-Acting Lifeline.”)
“IknowfrommytimeinDCthatpeople always ask what’s happening in San Francisco, and what they were really asking is what’s happening at Ward 86,” said San Francisco Director of Health Grant Colfax, MD, who formerly served as director of the Office of National AIDS Policy during the Obama administration. “We are here today because of our doctors, our nurses, our community partners and activists who push the bureaucracy to do more and, of course, most importantly, the patients. We’ve all championed the importance of getting to zero as we continually advance our mission with compassion and equity.” ■
IN 2021, THE FOOD AND DRUG ADMINISTRAtion (FDA) approved the first long-acting injectable regimen, Cabenuva (cabotegravir plus rilpivirine), which is administered by a health care provider once monthly or every other month. So far, it is approved only for people who already have an undetectable viral load and wish to switch to a more convenient regimen.
But Cabenuva may also be a feasible option for people starting treatment for the first time and those who have been unable to achieve and maintain viral suppression due to challenges with treatment adherence. Ward 86 is now implementing this approach with SPLASH, the Special Program on Long-Acting Antiretrovirals to Stop HIV. The program offers a range of support, including case managers, phone or text reminders of upcoming injection visits, follow-up for those who miss appointments and even street-based nursing services.
“By trying to use these novel agents in patients with concomitant life challenges, we hope to get individuals suppressed on therapy who have never been suppressed before and change the trajectory of the HIV epidemic,” Ward 86 medical director Monica Gandhi, MD, MPH, told POZ.
Gandhi and her team evaluated outcomes among 133 people who switched to Cabenuva from an oral antiretroviral regimen. Two thirds were homeless or lacked stable housing, and many were dealing with substance use and mental health problems. A majority (76 people) already had an undetectable viral load on their current medications; all of them maintained viral suppression after switching to the injections. The more exciting finding, Gandhi reported at this year’s Conference on Retroviruses and Opportunistic Infections, was that outcomes were nearly as good for the 57 people who started with a detectable viral load and in some cases advanced immune deficiency: All but two achieved viral suppression.
Use of Cabenuva for people without current viral suppression goes beyond the FDA-approved indication, and it might not be an option for those who don’t have the same level of intensive support provided by Ward 86. But for some, it could offer a lifeline.
“We’re seeing phenomenal results,” says Ward 86 nurse manager Jon Oskarsson, RN, MN. “People who had not in a long time or ever been able to suppress their HIV now are suppressed. It can be a tool for people who are living with a ton of complexity in their lives.”
Life is pretty normal these days for 26-year-old Brenda Emily. The central Pennsylvania resident and her boyfriend became parents to a baby girl, Emmy, in late 2022, whom Emily breastfeeds— something her pediatric team didn’t want her to do. “They said to me, ‘You can’t do that—we’ll call child services on you,’” she says. “I told them it was safe because I’m on HIV medications and undetectable. Then, I got a new pediatric team.”


Emily is living with HIV as well as moderate cerebral palsy. But unlike most people under 30 with the virus, she contracted it not via sex but in the womb. Her biological mother and father died of AIDS-related illness. She was raised by adoptive parents who, upon her biological dad’s death when she was 6, finally explained what he had died of and why she had to take meds.
“After that, I wasn’t allowed to talk about it,” she says. “I was told to hide it and never bring it up.”
However, once a family member leaked the news in town, Emily suffered yet more stigma as a schoolkid. “I had a few supportive friends, but there were also bullies who would mock me.”

Plus, the HIV meds Emily took as a child—which are now outmoded—caused hollowness in her face and limbs. “Not only did many people know I had HIV, but I actually looked like I was dying.”

All that made coming of age tough. “Sexuality didn’t exist for me,” she says. “I was convinced that if they touched me, I’d kill them—or that they wouldn’t want me anyway.”
Then, at age 21, she joined a support group for folks with HIV. She was the only woman among gay men, but the group motivated her to disclose her status, which she did on Facebook in 2015. “I felt free,” she says. “Like I could breathe.”
Around then, she learned about Undetectable Equals Untransmittable (or U=U, the fact that people with undetectable viral loads don’t transmit HIV to sexual partners). She also entered a clinical trial for cosmetic facial fillers and finally got on an easy-to-take HIV regimen—all of which were healing. And she plunged into activism. She has done numerous interviews about growing up with HIV and is involved with the Boston-based young adult group Next Step.

“My life felt controlled by HIV for so long,” she says. “Today, I’m starting to get to know my whole self. I’m strong and determined.” Enough to tell those on her pediatric team that they were wrong about breastfeeding. And she was right. Recently, the Centers for Disease Control and Prevention announced that even though the chance of a mother on meds passing HIV to her child via breastfeeding is not technically zero (it’s less than 1%), pediatric care teams should support mothers who choose to do so.
“I’ve learned that everyone matters, but no one matters more than you,” she says. “And I mean that in the most humble way!” ■
Negative attitudes or behaviors toward people living with or at risk for HIV are known as HIV-related stigma. Stigma can lead to isolation and depression. It can prevent people from getting tested or accessing care and treatment. POZ wants to know your thoughts on HIV-related stigma.
1 What do you think causes HIV-related stigma?
(Check all that apply.)
❑ Lack of education or awareness about HIV
❑ Misconceptions about how HIV is transmitted
❑ Religious or cultural beliefs
❑ Fear of contracting HIV
❑ Other (Please specify.): ___________________
❑ None of the above
2 What do you think can be done to reduce HIVrelated stigma? (Check all that apply.)
❑ Promote education and awareness about HIV
❑ Advocate for the rights of people living with HIV
❑ Enact laws or policies that protect people living with HIV
❑ Engage in conversations and challenge negative attitudes
❑ Other (Please specify.): ___________________
3 Have you ever participated in activities or initiatives to combat HIV-related stigma?
❑ Yes ❑ No
4 Do you think HIV and people living with HIV are adequately reflected in the media?
❑ Yes ❑ No
5 How often have you witnessed or encountered HIV-related stigma in the past year?

❑ Often ❑ Rarely
❑ Sometimes ❑ Never
6 Has HIV-related stigma prevented you from getting tested for HIV or seeking care, treatment or support in the past year?
❑ Yes ❑ No
7 Are you living with HIV?
❑ Yes ❑ No (Skip to question 12.)
8 Are you comfortable telling other people you are living with HIV?
❑ Always ❑ Sometimes
❑ Usually ❑ Never
9 Has HIV-related stigma ever adversely affected your relationships with family or friends?
❑ Yes ❑ No
10 Has HIV-related stigma ever adversely affected your dating life or sexual relationships?
❑ Yes ❑ No
11 Has HIV-related stigma ever adversely affected your career?
❑ Yes ❑ No
12 What year were you born?__ __ __ __
13 What is your gender?
❑ Male ❑ Female
❑ Transgender ❑ Other
14 What is your sexual orientation?
❑ Straight ❑ Bisexual
❑ Gay/lesbian ❑ Other
15 What is your ethnicity? (Check all that apply.)
❑ American Indian or Alaska Native
❑ Arab or Middle Eastern
❑ Asian
❑ Black or African American
❑ Hispanic or Latino
❑ Native Hawaiian or other Pacific Islander
❑ White
❑ Other (Please specify.): ___________________
16 What is your current level of education?
❑ Some high school ❑ Some college
❑ High school graduate ❑ Bachelor’s degree or higher
17 What is your annual household income?
❑ Less than $15,000 ❑ $50,000–$74,999
❑ $15,000–$34,999 ❑ $75,000–$99,999
❑ $35,000–$49,999 ❑ $100,000 or more
18 What is your ZIP code? __ __ __ __ __

Register Today!
September 6-9, 2023
Marriott Marquis
Washington DC USCHA.life • #2023USCHA