HR crisis: Short staffed, staff at risk





On November 29, Doug Ford’s Bill 124 was struck down by Ontario’s Superior Court. As the decision makes clear, for the past three years Bill 124 has suppressed the wages of over a million workers in this province, cancelling their Charter rights.
Bill 124 is wrong in so many ways. It’s unconstitutional. It’s a direct attack on women, because the majority of the affected workers are female. It penalized nurses and health-care professionals at the exact moment they were facing down the COVID pandemic.
In his decision, the judge pointed out the blatant unfairness of Bill 124: “Ontario has not explained why it was necessary to infringe on constitutional rights to impose wage constraints while at the same time providing tax cuts or licence plate sticker refunds more than 10 times larger than the savings from the wage-restraint measure.”
Ford said he will appeal the decision - a cynical delaying tactic that will prolong the injustice for many months. Taxpayers will be stuck with the legal bills, but it’s the human cost of Ford’s decisions that is so devastatingfor nurses, patients, and the health-care system that serves us all.







Canadians are waiting longer than ever before for elective surgeries. Across the country, health care systems are experiencing record backlogs in surgery due to successive waves of the pandemic and shortages of nurses, doctors and other health professionals.
There is an urgent need to ensure Canadians receive care in a timely manner by improving our health policies and systems. But there are also everyday practices and processes we can address right away to help improve delays and backlogs.
“Low-value care” describes tests and treatments that are commonly ordered despite clear evidence that they do not help with patient care – and may even cause harm.
A new report released from the Canadian Institute for Health Information and Choosing Wisely Canada evaluates this problem across 12 different low-value tests and treatments. The report looks at trends across the country before the pandemic, as well as during the first year of COVID-19.
Overall, the report shows that Canada has made good progress, with eight of the 12 areas of tests or treatments declining by 10 per cent or more between 2014 and 2019. But, given that most of these tests and treatments are unlikely to be necessary in the first place, we can do even better – saving our valuable health care resources for care that is truly needed.
What are examples of low-value care in surgery?
Knee arthroscopy is a surgical procedure that’s appropriate for treating common knee problems, such as torn ligaments. But for adults aged 60 and older, this procedure offers little to no benefit compared to safer options like exercise therapy, injections or medications.
The good news is that Canada has reduced the number of low-value knee arthroscopies. The rate of knee arthroscopies has dropped by 46 per cent in adults over 60 between 2014 and 2019. Still, 99 out of every 100,000 older adults are getting the procedure each year, with differences in rates among the provinces.
If all of Canada could achieve the rates of the lowest province, which is currently Newfoundland and Labrador, it is estimated that an additional 7,500 knee arthroscopies could be avoided across the country each year –freeing up significant surgical resources to provide more necessary patient care.
Another example is pre-operative testing. If you are getting cataract surgery or other low-risk procedures, you may be asked to go for additional testing before the operation. Evidence shows that these tests – electrocardiograms, cardiac stress tests, echocardiograms or chest x-rays – rarely change a surgeon’s decision to operate or make surgery safer and may lead to additional unnecessary testing and delays in getting the surgery done.
EDITORIAL: February 9
ADVERTISING: Display – Feb. 24 | Material – Feb. 28
Monthly Focus: Facilities Management and Design/Health Technology/Greening Healthcare/Infection Control: Innovative and efficient healthcare design, the greening of healthcare and facilities management. An update on the impact of technology , including robotics and artificial intelligence on healthcare delivery. Advancements in infection control in hospital settings.
+ INFECTION CONTROL SUPPLEMENT
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 401 Vaughan Ontario L4K 0E3
TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor
Kristie Jones editor@hospitalnews.com
Advertising Representatives Denise Hodgson denise@hospitalnews.com
Publisher Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries accountingteam@mediaclassified.ca Circulation Inquiries info@hospitalnews.com
Director of Print Media Lauren Reid-Sachs
Barb Mildon, RN, PHD, CHE
VP Professional Practice & Research & CNE, Ontario Shores Centre for Mental Health Sciences
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
Senior Graphic Designer Johannah Lorenzo ASSOCIATE
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario.
The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.
When Dawn Ethier looks back at the past decade of her life, it is a blur.
The ordeal of taking several medications, almost a hundred pills per day, constantly having to measure mineral levels in her blood, and several visits to hospital was extremely taxing for the Ottawa police officer and mother of four, who battled with hypoparathyroidism.
“This disease took a lot of time away from me, from my family, from work, from caring about myself,” says Dawn, who is now cured after receiving a ground-breaking transplant at UHN’s Ajmera Transplant Centre.
“For a long time, I didn’t think I was worthy of anything, because I was so ill.”
Dawn had thyroid cancer over 10 years ago. The cancer was treated, but a complication she was left with was hypoparathyroidism – when someone has little or no parathyroid function.
The condition caused severe symptoms and even threatened Dawn’s life. She had cardiac episodes, pulmonary embolisms, seizures, loss of muscle control, and longterm impacts to her mental health.
After a lot of research and conversations with her care team in Ottawa, Dawn was able to connect with Dr. Karen Devon, an Endocrine Surgeon at UHN’s Sprott Department of Surgery, and discuss with her a bold idea – trying a parathyroid transplant.

With only one other case of this exact type of transplant recorded in the scientific literature, this was no small undertaking.
Dr. Devon had to do a lot of homework for a couple of years, including connecting with specialists around the world to discuss this case.
She had unwavering support from the Ajmera Transplant Centre, one of the largest transplant programs in North America, recognized for leading ground-breaking procedures.
Dawn seen here with her youngest daughter, Rebecca, says she is very happy to be able to spend more time with her children now.
Small but mighty: transplant of glands the size of grains of rice gave Dawn Ethier her life back.
The journey was long, through listing and matching with potential donors, one failed transplant attempt in 2021, and managing all of this during a global pandemic. But on May 19, four healthy parathyroid glands were implanted on Dawn’s right forearm and they started functioning a few weeks later.
Through this exciting case, Dr. Devon had her first experience as a transplant surgeon and worked closely with the transplant team at Toronto General Hospital. An important ally was UHN’s Physician-in-Chief, Dr. Kathryn Tinckam, who is also a transplant nephrologist at the Ajmera Transplant Centre.

“I was apprehensive of bringing this idea forward to leadership at the Ajmera Transplant Centre, and I was extremely encouraged by the response, which was to tell me that we have an obligation to help this patient,” says Dr. Devon, who’s also an Assistant Professor with the University of Toronto.
“That was very motivating for me,” she adds.
“This saved my life, it changed everything,” says Dawn, who has come off all the medications she was taking for her disorder, doesn’t need any infusion or regular visits to hospital day units, and has none of the symptoms of hypoparathyroidism.
“My mood, my personality is coming through. I’m no longer exhausted, I’m able to spend more time with my children.
“I can see a future now. This is not going to end up being something that will take me.”
As with other organ transplant candidates, Dawn had to go through extensive testing. Dr Tinckam, who is also a consultant with UHN’s HLA Lab – the largest histocompatibility laboratory in Canada – helped guide the process.
“We test the blood of potential recipients frequently to quantify what percentage of all potential organ donors could be a suitable match. This helps us understand what chances that patient will have of a donor organ becoming available,” explains Dr. Tinckam, who is also Associate Professor of Medicine at U of T.
new study throws cold water on the theory that younger family physicians work less. The study, published in CMAJ (Canadian Medical Association Journal) , found an overall drop in patient visits across all physician cohorts between 1997 and 2018.
Analyzing data from administrative health databases on family physician practice patterns in four provinces –British Columbia, Manitoba, Ontario and Nova Scotia – the researchers found the median number of patient visits (contacts) per physician per year fell by 515 to 1,736 visits. They focused on time in practice (rather than biological age) and found the number of visits peaked at 27–29 years of practice, whereas physicians earlier in practice or at the end of their careers had fewer patient visits. Although the number of visits changed with years in practice and has declined over time for all family physicians, the researchers found no evidence of changes unique to more recent cohorts.
“These findings are important for health workforce planning in primary care sectors across the country and suggest that any intergenerational tension and blame is unfounded and may distract from more important issues in
workforce planning in primary care sectors,” write the authors.
“Intergenerational blame distracts from broader issues in primary care,” says Dr. David Rudoler, Faculty of Health Sciences, Ontario Tech University, Oshawa, Ontario. “Feelings of blame and judgment toward early career family physicians are damaging, particularly when layered with the feeling that family medicine is already undervalued.”
The decline in overall patient visits per family physician coincides with a substantial increase in complexity of care and administrative workloads.
“Whether declines in patient contacts reflect an increase in patient complexity, an increase in administrative burden, increased quality, changes in education or professional norms, different choices about work or different income requirements is not clear; however, observed declines are not unique to current early-career physicians,” write the authors.
They suggest robust workforce planning that considers physician
The report found that between 2015 and 2019, rates of pre-operative testing prior to low-risk surgeries declined by 17 per cent. However, it also shows that one in five patients who undergo low-risk surgery are still being sent for pre-operative testing.
If all of Canada could achieve the rates of the lowest province, which is currently Alberta, it’s estimated another 99,000 preoperative tests could be avoided each year.
With the health care system under extreme pressure, avoiding low-value
care means faster access to care. Policies, processes and professional practices years and decades in the making need to be undone.
Findings from the report suggest that while Canada is making progress in reducing overuse, there’s still plenty of room for improvement.
Differences in rates among provinces and territories suggest that we can all work together and learn about how different health systems tackle this longstanding problem. n H
Wendy Levinson is the Chair of Choosing Wisely Canada. David O’Toole is the President and CEO of the Canadian Institute for Health Information.
age distribution, trends in service volume and changing patient demographics.
In a related commentary, Dr. Tara Kiran, Department of Family and Community Medicine, St. Michael’s Hospital, a site of Unity Health Toronto, and the University of Toronto, makes several suggestions on how to improve access to family physicians.
“Primary care in Canada is in crisis. It affects the rest of the health system and the solution must be bold reform. Primary care should be considered a right and a necessity, similar to public education,” writes Dr. Kiran.
“Increasing the primary care workforce by training more family physicians will likely get us only part of the way to solving the problem given existing shortages and trends. Canada’s health systems need to reimagine how family doctors work and are integrated into the system.”
Shifting to collaborative teambased primary care with skilled office assistants, nurses, nurse practitioners, social workers and pharmacists, and creating neighbourhood-based practices to ensure access for families are some suggestions to increase access to primary care.
“Changes over time in patient visits and continuity of care among graduating cohorts of family physicians in 4 Canadian provinces” and “Keeping the front door open: ensuring access to primary care for all in Canada” were published December 12, 2022. n H
etformin, a commonly prescribed medication for patients with type 2 diabetes, was associated with a 30 per cent reduction in risk of joint replacements, according to a large study published in CMAJ (Canadian Medical Association Journal)
Osteoarthritis is a common chronic condition that usually causes joint pain and can be severe enough to require knee and hip replacements. In the United States, the number of total knee replacement (TKR) and total hip replacement (THR) surgeries is estimated to reach 572 000 per year by 2030. No medications are currently known to prevent or reverse osteoarthritis.
A team of researchers from China, Taiwan and Australia aimed to determine whether metformin use was associated with a lower risk of TKR or THR as evidence to date has been sparse and inconclusive. They analyzed data from 69 706 participants who received a diagnosis of type 2 diabetes in
Taiwan between 2000 and 2012 and compared the risk of TKR and/or THR between people taking metformin and those not taking metformin. The mean age was 63 years and half were women. About 90% of total joint replacements were related to osteoarthritis.
“We found that metformin use in patients with type 2 diabetes mellitus was associated with a significantly reduced risk of joint replacement, suggesting a potential therapeutic effect of metformin in patients with osteoarthritis,” writes Dr. Changhai Ding, Clinical Research Center of Zhujiang Hospital, Southern Medical University, Guangzhou, China, with coauthors.
The authors call for randomized controlled trials to determine if metformin use is effective in patients with osteoarthritis.
“Metformin use and associated risk of total joint replacement in patients with type 2 diabetes: a population-based matched cohort study” was published December 19, 2022. n H
“THESE FINDINGS ARE IMPORTANT FOR HEALTH WORKFORCE PLANNING IN PRIMARY CARE SECTORS ACROSS THE COUNTRY”
By August 2022, most children and adults younger than 60 years in Canada had been exposed to SARS-CoV-2 through a combination of vaccination and infection, according to a large study looking at blood antibodies published in CMAJ (Canadian Medical Association Journal).
The study of almost 14,000 people provides a clear view of the changing antibody landscape during 2.5 years of the COVID-19 pandemic. Over that period, there was a change from virtually all pediatric and adult participants being immunologically naive (and thus susceptible) to SARS-CoV-2 to almost all having been immunologically primed (through vaccination, infection or both). Primed individuals are expected to have swifter immune memory responses to reduce the risk, especially of severe outcomes from SARS-CoV-2.
The study was conducted by the British Columbia Centre for Disease Control (BCCDC), which has a long-es-
tablished seroprevalence protocol for monitoring population susceptibility to emerging or re-emerging respiratory viruses. The BCCDC launched its first SARS-CoV-2 serosurvey among people living in BC’s most populated Lower Mainland region in March 2020 just before the World Health Organization declared the COVID-19 pandemic. Using this survey as the baseline, researchers conducted 7 more analyses up to August 2022.
During the first year of the pandemic, very few people had antibodies to SARS-CoV-2, with less than one per cent seroprevalence during the first three snapshots and less than five per cent by January 2021. With the SARSCoV-2 vaccine rollout, seroprevalence increased dramatically during the first half of 2021 to 56 per cent by May–
June 2021 and 83 per cent by September-October 2021.
Conversely, infection-induced seroprevalence was low (less than 15% in September-October 2021) until Omicron waves occurred, rising to 42 per cent by March 2022 and 61 per cent by July-August 2022. The combined seroprevalence for vaccination or infection was more than 95 per cent by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the commu-
nity,” writes Dr. Danuta Skowronski, the lead investigator based at the BCCDC and University of British Columbia, Vancouver, British Columbia, with coauthors. “The lowest cumulative infection rates were among older adults, which may reflect their greater vaccination rates and social isolation.”
Findings from the United States show similar age-related infection rates. Data among children from other provinces in Canada, however, remain limited.
The authors reinforce continued prioritization of SARS-CoV-2 vaccination for older adults.
“Although everyone may benefit somewhat from additional vaccine doses… the prioritization of older adults, who are still at greatest risk of severe [COVID-19] outcomes, remains most consistent with immunization goals to prevent serious morbidity and preserve health care capacity as the 2022-23 respiratory virus season begins,” they write. n H
Arecently published preclinical study by researchers at Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry, show that vaping may negatively affect pulmonary surfactant in the lungs.
Surfactant, which is made of lipids and proteins, is a critical layer in the lungs that allows people to breathe with minimal effort by reducing surface tension. Without surfactant, it would take more effort to breathe and a person would need mechanical help to do so.
“Vaping continues to be popular but not much is known about what happens with the aerosol when it enters the lungs,” says Dr. Ruud Veldhuizen, Lawson Scientist and Professor at Schulich Medicine & Dentistry. “We realized that the first
thing the vapor aerosol comes in contact with in the lungs is pulmonary surfactant, which is an area our team specializes in.”
The research team was able to study the effects by placing a film of surfactant inside a syringe and, then using a vaping device to push aerosol into the syringe. This allowed the vapor to directly interact with the surfactant. The researchers then mimicked inhaling and exhaling vapor into the syringe 30 times to resemble a standard vaping session.
“In particular we were looking at the surface tension in the surfac-
tant,” explains Emma Graham, Master’s student at Schulich Medicine & Dentistry. “After vaping, we saw high surface tension which suggests the surfactant would not be as effective at supporting proper lung functioning.”
The team also examined different vaping devices, flavours, additives and nicotine to see if there were any difference in effects.
“Nicotine didn’t have any worse effects on surface tension of surfactant compared to other e-liquids, but some flavourings like menthol e-liquid did,” says Graham.
While his team intends to study this further, Veldhuizen says these findings could provide an indication as to why people that vape have a susceptibility to develop lung injury, including those with respiratory viruses such as COVID-19.
“We would like to get this information out there so that people know vaping may be damaging to the lungs,” says Veldhuizen. “As a next step, we hope to further investigate the effects of vaping on the lungs and how we can treat resulting injury.”
The study has been published in the PLOS ONE Journal . These findings build on a body of research about the impacts of vaping through Lawson and Schulich Medicine & Dentistry. Our researchers were the first in the world to report on a potential new type of vaping-related injury in 2019.
n H
THE AUTHORS REINFORCE CONTINUED PRIORITIZATION OF SARS-COV-2 VACCINATION FOR OLDER ADULTS.
“VAPING CONTINUES TO BE POPULAR BUT NOT MUCH IS KNOWN ABOUT WHAT HAPPENS WITH THE AEROSOL WHEN IT ENTERS THE LUNGS.”
Phew! The holidays are over, so at least one stressor is gone… for a while. Maybe you had time off and now it’s back to work with challenging schedules, long shifts, staffing shortages, viruses that continue to evolve and a home life that always needs attention.
You talk to your patients and their families about self-care, to manage stress and anxiety as they navigate the healthcare system. But what about you. What do you do to help yourself?
When I started my nursing career, I was not told how important it was to take care of myself. We all knew the job was physically challenging and could take a toll. But there was always a primary focus on the patient first- which is the reason why we all get into healthcare in the first place. It’s not long before the effects of patients first and self last are felt which can leave you feeling drained and overextended. We now know that there must be a delicate balance of patient and self care.
Survey results released in January 2022 by the Workplace Strategies for Mental Health found that more than one third (35 per cent) of Canadians were feeling burnt out. That number jumped to more than half (53 per cent) in the health and patient care sector.
Within that sector, an astounding two thirds of nurses reported feeling burnt out. Mental health professionals followed closely at 61 per cent and all other segments surveyed in this sector landed well above the Canadian average of 35 per cent reporting burnout.
The impacts are wide ranging and can include chronic health conditions, increased anxiety or decreased mood,
enthusiasm, motivation, compassion, or empathy. When the effects show up in a breakdown of health, it can reinforce a sense of shame or selfblame around not taking better care of ourselves or finding and sustaining a healthier work/rest balance.
Today I work to make healthcare workplaces safer and healthier, not directly with patients or in healthcare settings but I still remind myself, when overwhelmed, about the safety instructions on any airplane. In case of emergency, put your oxygen mask on first before helping anyone else. You can’t provide quality care, if you’re not prepared.
There are any number of articles out there about what you can do to begin caring for yourself first. Eating well, meditation, listening to music, being outdoors, exploring your neighbourhood, getting a massage, getting enough sleep and exercising are all great ideas. But I would be remiss if I didn’t mention reaching out to your HR, wellness or health and safety representative. (In each organization that person or department will be different.)
Because more and more employers are understanding the impact of stress and burnout in employees they are using organizations such as the PSHSA to help build holistic health and safety programs, including psychological health.
There are as many opportunities to improve your wellness and self-care as there are causes for stress, burnout and anxiety. However, advice, no matter how well-intentioned, can be translated into “just another thing I have to do.” Something else – although enjoyable and longed for – added to that ever-growing list. They’re often the first to get dropped when the needs of others must be addressed.
So, in fact, there may not be one answer but several or a combination
of short- and longer-term suggestions that might work for you.
Many of them you have already likely shared with patients, team members, staff and other employees but it’s worth a reminder.
Some self-care best practices*
• Yoga – Don’t know how to get started or concerned about joining others. There are many, many free yoga videos on YouTube. You can even get online yoga classes customized to a particular issue, circumstance, or ailment.
• (Re)start a hobby – Volunteer, reignite an old passion project, start a garden, try journaling, essentially, anything that revives and refreshes you. The good thing is they don’t have to be done every day.
• Explore the practices of meditation and mindfulness.
Self-care is a journey that starts with awareness and understanding. You may need to start slow initially and with less of a commitment. So, you may want to start with something that can be easily incorporated into your schedule and then over time try adding different approaches to see what works for you.
• Get hydrated – Have a glass of water.
• Go for a walk – Even just a short one, around the block. You’ll be surprised how much a change of scenery and the fresh air will help.
• Check out ResilientME – PSHSA’s free, 30-minute self-guided microlearning program focuses on: mental fitness, physical fitness, nutrition, financial fitness, sleep and social connections. It incorporates highly effective strategies and tools designed to increase your capacity for resilience. It can be found at bit.ly/ pshsa-resilience
As with physical health and safety, there are many interventions that can be implemented by employers, policy and decision makers, and JHSC com-
mittees at the organizational level to reduce the risk of psychological strain. The PSHSA has created a guide that can be used to build a psychological health and safety program, or to identify program gaps in any existing one. It provides:
• Information on provincial legislation and national/international standards.
• A review of the traditional workplace psychological health and safety and psychosocial factors and the additional healthcare factors.
• Occupational health and safety hazard mitigation concepts at the organizational level and at the job-position levels.
• Information on psychological health and safety program development and implementation using systematic occupational health and safety and continuous improvement processes.
• Linkages to existing supporting resources and tools for successful implementation where appropriate.
If you are looking for an approach that is specific to your workforce, the PSHSA’s Occupational Stress Injury Resilience Tool is an evidence-based screening tool that can predict resiliency or vulnerability for occupational stress injuries. It provides employers and health and safety decision makers with a better understanding of the occupational stress injuries in the workplace. It allows employers to focus on supports and resources to mitigate their employees’ specific risk of occupational stress injuries. Finally, it provides recommendations to create, update or enhance any wellness program or evaluate the efficacy of an existing program.
It’s a fact, psychologically healthy and safe workplaces, with an open and supportive culture, are better able to attract and retain workers, have higher levels of employee engagement, productivity and performance, and lower rates of absenteeism, short- and longterm disability claims rates, grievances, and conflict.
And the PSHSA team of skilled and experienced health and safety experts are ready to help you create, evaluate, or adjust your health and safety pro-
grams and ensure a safer and healthier workplace.
Finally, if you are inclined to make one or several new year’s resolutions, I hope you will include a commitment to you. The time is now to put your psychological health first on your to-do list. If you are in a position to make organization-wide choices about the psychological health and safety of employees, there is no time like now to make changes or improvements.
But most importantly, do not suffer in silence. Reach out for help. This could be a trusted friend, family member, colleague or one of your many workplace resources. There are always solutions and people ready to help.
For more information about the PSHSA, its resources, training and consulting services, please visit our website at PSHSA.ca (https://bit.ly/PSHSA-Consulting), call 416-250-2131 or email clientexperiences@pshsa.ca. n H
*Suggestions noted in this article are just that, suggestions. They should not be considered medical advice. Always consult a physician before starting any practice that may impact your health.
“We then sequence a part of the DNA of all potential donors to confirm potential immunologic suitability for the recipient.”
She remembers that Dawn didn’t have the best odds. From her lab results, it was estimated that only 2 per cent of potential donors would be a match for her. This raised expectations even higher, especially going through a first failed attempt and waiting for the second chance that came in May.
“It was really a team effort. We all wanted this to work,” Dr. Tinckam recalls.
“After the second transplant, when we saw her PTH and calcium levels coming up, we were absolutely thrilled.”
For Dr. Atul Humar, the Director of the Ajmera Transplant Centre, the success of this case is a testament to the efforts of a stellar multidisciplinary team, that doesn’t shy away from a challenge.
“This is part of our DNA at the Ajmera Transplant Centre and UHN.
We never shy away from trying something new, especially when patients look to us for life-saving and life-altering procedures,” says Dr. Humar, also Professor in the Department of Medicine at U of T.
This case also happened thanks to the support from generous donors to UHN Foundation, and to the support from Trillium Gift of Life Network
(TGLN) at Ontario Health, the organization in charge of organ and tissue donation in Ontario, as it supported logistics for this innovative treatment, including the creation of deceased donor listing for parathyroid glands.
“Thanks to the commitment and dedication of all our partners, more patients will be able to enjoy vastly improved lives as a result of this innovative work,” says Rebecca Cooper, Vice President, Ontario Health (Trillium Gift of Life Network and Ontario Renal Network), who added that ground-breaking medical advances in organ and tissue donation and transplant are only possible through the generosity of donors and their families, reminding Ontarians they can register to donate at BeADonor.ca
With this initial success, Dr. Devon and the team at the Ajmera Transplant Centre are working to study further and expand parathyroid transplant as treatment for severe hypoparathyroidism. n H
We’ve gathered evidence about the current state of digital health interoperability in Canada and the significant opportunities for health system improvement.
Learn about the findings: infoway-inforoute.ca/en/connected-care

HE SUCCESS OF THIS CASE IS A TESTAMENT TO THE EFFORTS OF A STELLAR MULTIDISCIPLINARY TEAM, THAT DOESN’T SHY AWAY FROM A CHALLENGE.
Ahigh reliability organization (HRO) is an organization that succeeds in avoiding catastrophes despite working with hazardous and complex systems, such as air traffic control and nuclear power facilities. Health-care organizations frequently adopt the five key principles of HROs in their efforts to eliminate preventable harm, but studies about the perceptions of health-care workers at the centre of this effort are lacking.
Dr. Trey Coffey is the Medical Officer for Patient Safety at The Hospital for Sick Children (SickKids), and senior author of a study focused on how health-care professionals understand and enact HRO principles. HROs are one of the first things safety professionals learn about during training at the Centre for Quality Improvement and Patient Safety, or C-QuIPS, a joint partnership of teaching hospitals including SickKids.
Trey’s affiliation with C-QuIPS allowed her to connect with experts in HROs, as well as team members with advanced methodological skills, resulting in a paper published in BMJ Quality and Safety.

In the following Q&A, Coffey discusses the study, which explored how different professional groups in paediatrics perceive the HRO principles, including what’s working, what isn’t working, and why.
All study participants were from SickKids, where we have a hospital-wide safety program called Caring Safely. Instead of choosing randomly, we used a method called purposive sampling. To achieve the greatest breadth possible within the sample, we selected one critical care area, one surgical care area, and one medical specialty care area. From each of those areas, we included a diverse set of roles
– physicians, nurses, interprofessional staff, quality leads. Then we also intentionally included members of the Caring Safely steering committee.
We found very different levels of understanding between the different principles of high reliability. For example, the principle of “preoccupation with failure” seen in HRO, meaning that even a small deviation from what is expected can represent a significant risk, was in one sense a good “fit” in health care. Participants could readily describe many examples of how we enact this, for example by reporting safety events. On the other hand, the complexity of the health-care environment and constant risk of making a mistake – big or small – can also interfere with doing their job. The other challenge is that in health care we are under constant pressure to be efficient, often with limited resources. Staff described having to constantly balance taking their time to be careful with moving quickly to meet our patients’ needs.
In the process of interviewing study participants, we prompted them by asking if they could recall examples as we named and briefly described each principle. We didn’t provide a fulsome explanation of the principle unless asked. In most cases, they expressed having heard of the principle, and then went into examples.
That would be the principle of “commitment to resilience,” which refers to processes and behaviours that allow us to effectively ‘contain’ a situation when something unexpected happens so that further disruption or safety issues are minimized. This is distinct from the concept of “personal resilience,” which is what participants tended to think of when asked about this principle. Enacting “commitment to resilience” requires proactive activities that prepare teams to do this well, such as simulation and team training. Though we do some of these activities in health care, we typically place the bulk of our attention and resources on reactive work.
in the breadth and depth of HRO implementation in health care. The editorial discussed some reasons why the broader health-care sector has difficulty adopting safety concepts from other industries and asserted some ideas to change this, such as making more of an effort to learn why things usually go well instead of learning why things occasionally go wrong, addressing differences in the degree of staff participation in safety training, as well as tackling larger systemic risks that go beyond the level of one organization.
The differences in how each of the principles were understood were striking. This suggests that we shouldn’t think of, and teach, HRO as one monolithic idea and that we should deepen our focus on each of the five principles individually. I think we also realized that we are all probably making assumptions about how well our colleagues understand these concepts. In the future, this kind of safety program could do more to help leaders and staff understand the principles more deeply, so that they are more equipped to reflect and evolve their approaches to safety.
A big surprise was that Kathleen Sutcliffe, one of the researchers who originally coined the term “HRO” decades ago, co-wrote an editorial in response to our paper, which validated the idea that there are gaps
My immediate plans are to share the learnings here at SickKids and in the network of 145 children’s hospitals, Solutions for Patient Safety, that we work with. Along with other leaders striving to advance safety through programs like Caring Safely, we will consider how to evolve training and support for health-care leaders to better equip them to deepen their practice of high reliability. As we continue this work, I look forward to future opportunities to partner with researchers in the interest of safety. n
DID YOU PROVIDE PARTICIPANTS WITH A DEFINITION OF EACH PRINCIPLE, OR DID YOU WANT THEM TO
DID YOU LEARN ANYTHING THAT WOULD CHANGE YOUR OPINION ABOUT THE USE OF AN HRODr. Trey Coffey is the Medical Officer for Patient Safety at The Hospital for Sick Children
The COVID-19 pandemic forced us to reimagine, reorder, and restructure every sector of society. In almost all instances, technology has been at the heart of our adaptations. Nowhere has this transformation been more pronounced than in the practice of medicine.
As practitioners responded to the pandemic, telehealth and virtual care adoption accelerated dramatically around the globe - to keep patients and healthcare providers safe and to increase access to care.
It was an acceleration that, while challenging at the time, has largely delivered positive results. Many patients have shown their enthusiasm for virtual care, appreciating its flexibility. And as physicians, being able to offer this kind of flexibility is not only a point of pride, but a change that often allows us to practice better medicine. Managing virtual care addresses the universal challenge of a future enabling five key “rights:” the right care, at the right time, in the right setting, by the right physician or clinician, using the right modality (such as phone appointments or video calls).
Many of us are seeing the value of virtual care firsthand. A study from the Canadian Medical Association reinforces what I’ve heard from colleagues who practice in Canada and the U.S. In it, 94 per cent of physicians polled said they currently provide virtual care (including by telephone, video conferencing, email, and other modalities). More importantly, 70 per cent said they believe virtual care improves patient access and enables quality, efficient care.
In response to some of these positive results, we’re seeing more appetite to
invest in virtual care, including in Canada. Each of the provinces and territories have action plans to expand virtual care offerings in their jurisdictions.
These investments in virtual care will play an important role in reducing backlogs for routine procedures and check-up appointments. Streamlining the more routine concerns helps clinicians prioritize the patients with urgent matters.
However, as the medical community and policymakers decide what the
models can use this framework to guide their decision-making on how they use virtual care. Policymakers can do the same, using it to inform coverage and payment decisions, and support the establishment of regulations that work.
The framework includes six value streams, which it then uses to consider the different factors that may influence those value streams, including the type of practice and modality of virtual care (see below).
went from <1% to more than 80% of total visits. Patients were less likely to miss their telepsychiatry appointment because of the improved convenience of conducting a virtual visit.
In using the framework, VCU found ways to reduce wasted time slots. It also gained better insights into health equity questions.Including virtual solutions was found to provide equal levels of care among age groups, despite concerns about older, less tech-savvy patients potentially experiencing more barriers.
future of virtual care should look like, it raises questions around evidence (namely around value, equity, and access). These are not impossible hurdles – and they’re ones worth conquering.
To support clinicians and policymakers alike, the American Medical Association created a framework for measuring the value of virtual care. It considers how virtual care programs may generate benefits for patients, clinicians, and society – all in the context of the post-pandemic “return on health.” Care providers looking to develop and assess new remote care
Measurement across these value streams allows for a better picture of the true value of digitally enabled care. Some health systems are already using it with success. VCU Health in Virginia, for example, used this framework to evaluate the impact of its virtual care model on psychiatry care access. VCU Health Psychiatry practice saw 120% more patients using telehealth (compared to pre-pandemic in-person model), while retaining equitable access. The no-show rate among psychiatry visits declined from 11% pre-pandemic to 6% post- pandemic as virtual visits
Any conversation around virtual healthcare needs to consider how we measure its value in building stronger, integrated and digitally enabled health systems that empower the right care. Effective decisions about the future of virtual care cannot happen in the context of outdated systems or limited measures of success. A part of this investment often overlooked is the standardization of medical coding which enables the interoperability of treatment regardless of care setting. This coding foundation can not only capture all care, but it can use data sets to help to optimize the efficiency of the system itself.
Many measures of virtual care have been short-term or focused on dollars and cents, rather than its potential to be truly transformative for patient and clinician experience. Realizing the full potential of digitally enabled care will require fundamentally rethinking how care models are designed, implemented, and scaled – and how we measure their impact.

Medicine is changing. The future of care delivery must change, too. ■ H
https://www.cma.ca/virtual-care-canada-progress-andpotential-report-virtual-care-task-force. Published February 2022. Accessed December 2022.
orkplaces are central to our lives. For better or worse, many of us spend more time with our colleagues than with our families. Yet we know in any given week, at least 500,000 employed Canadians are unable to work due to mental health problems, and 30% of disability claims are related to mental illness. The pandemic has only made things more challenging, particularly among healthcare workers.
Ensuring good psychological health and safety in the workplace is vitally important to keeping employees en-
ergized, healthy, and at work, ready to deliver exceptional patient care to those who most need it.
Since 1904, Waypoint’s expert staff have been here day in and day out, supporting patients who need acute
or longer-term psychiatric inpatient and outpatient care including forensic mental health services on their recovery journey. In an effort to support our staff, in 2015 the hospital embarked on a three-year initiative to implement
the National Standard for Psychological Health & Safety.
“Healthcare has changed so much over the decades and we knew that we would need a comprehensive plan to support our staff through the many changes on the horizon,” said Nicole Mace, Interim Director, People Experience and Talent. “At the time the pandemic wasn’t even on our radar and I think having this standard embedded in our practice before it hit helped us weather some of the challenges.”
Developed under the leadership of the Mental Health Commission of
our GTA hospitals are combining recruitment efforts to create a special team of critical care nurses who can be deployed to help fill staffing gaps, and provide additional patient care capacity.
North York General Hospital, Michael Garron Hospital, Scarborough Health Network (SHN), and Sunnybrook Health Sciences Centre, received support from the Ministry of Health to launch the pilot project, which will recruit and orient nurses to work across the critical care units of the four partner hospitals.
“Nursing vacancies continue to be one of our greatest challenges across the system and in critical care, in particular, where vacancies continue to be high,” said Susan Woollard, VP, Clinical Services, Quality and Long-Term Care & Chief Nursing Executive, North York General Hospital. “Critical care is one of the safety-nets of our health system and we cannot afford to have this area short staffed. The specialized critical care team across our four hospitals will be one of many solutions we’re implementing to ensure patients have access to life-saving care during this extraordinary time.”
Each hospital will recruit five nurses for the team, for a total of 20, who will receive training and orientation to the critical care units across the four organizations. Staffing levels on the units are monitored daily and when a need arises, members of the team can be assigned to work at whichever hospital needs help.
“We are pleased to collaborate with our fellow partner hospitals who share a one-team vision and approach to caring for patients and their loved ones during their greatest time of need,” said Kevin Edmonson, Director of Michael Garron Hospital’s (MGH) Critical Care and Emergency Departments. “As we navigate increasing pressures and demands on Ontario’s healthcare system, we recognize that it takes the collective efforts of all our inter-professional teams and health system partners to care for our communities and each other. We look forward to the opportunity to expand our exceptional critical care team together with our partners.”
When the nurses are not needed in other hospitals, they will work as a member of the critical care teams in their home institution, where they were recruited initially.

‘This is a tremendous opportunity for nurses to get a wide range of experience working with other teams and hospitals,’ said Ru Taggar, EVP and Chief Nursing and Health Professions Executive, Sunnybrook. ‘An important part of the program is the handson mentoring and career coaching that will be provided for every member of the team. There is also an emphasis on wellness for the team that ensures there’s not only a focus on skill development but also, the emotional well-being of each nurse is a key element of success.’
“Our patients are acutely ill. Proper staffing levels ensure we can provide a level of care for patient conditions that
can change rapidly - in a matter of minutes, in most cases,” said Sam Michael, a frontline nurse at SHN’s Centenary ICU. “The complexity of the patient’s condition also must be considered when determining appropriate staffing levels and how impactful it can be when even one team member is missing. The ICU depends on a full team environment for exceptional, life-saving care.”
Recruitment for the team began in November and interested applicants should refer to the Human Resources department of the participating hospitals. The pilot will run for a period of two years and it is hoped this model could be replicated for other professions. n H
Four hospitals coming together to help address critical care nursing shortages
“WE HAVE WORKED VERY HARD OVER THE YEARS TO EMBED THE INTERCONNECTEDNESS OF MENTAL HEALTH AND EMPLOYEE WELLNESS.”
Canada, the National Standard outlines a systematic approach to develop and sustain a psychologically healthy and safe workplace and focuses on mental illness prevention and mental health promotion. Waypoint’s journey involved the creation of a specialized resource to develop an implementation plan focused on building a foundation while considering pre-existing structures, new programming, education and gradual systems refinement.
Adopting the standard was only the beginning for the hospital. Employee Wellness Coordinator Liz Everett shares “We have worked very hard over the years to embed the inter-connectedness of mental health and employee wellness.”

Since adopting the standard, the hospital has created a psychological health and safety committee, embedded mental health support skills in leadership development through initiatives like Psychological Health & Safety Conversation Kits and Leadership Rounding, worked with the Waypoint Research Institute to study trauma in the workplace, studied staff burnout in partnership with the Yale Center for Emotional Intelligence, and collaboratively led Ontario Health Central region hospitals in collective well-being efforts.
All of this work led the hospital to be recognized as a 2022 Certificate of Merit Recipient for Mental Health at Work®. This nationally recognized award acknowledges the years of hard work that leaders and staff have put into the development and implemen-

tation of the extensive psychological health, safety and wellness program, and recognizes Waypoint as a national leader in psychological supports for staff.
“I couldn’t be more pleased with this recognition for our first year participating in the Excellence Canada awards and share my thanks with everyone involved in the work leading up to the award,” said Dr. Nadiya Sunderji, President and CEO.
As with most things in healthcare, the work never stops and plans for further enhancements are underway, particularly in these challenging times across the sector. Focus groups with staff and managers are inspiring growth opportunities and everyone’s participation is helping the hospital chart our path toward achieving outstanding results focused on mental health, safety and wellness for employees at all levels of the organization.
“With this recognition we know we are on the right track as we stay focused on this important employee support,” said Demetrios Kalantzis, Vice-President, People and Chief Human Resources Officer. “Special thanks to the team involved and everyone who dedicated time to reviewing our program and activities and filling out the substantial application. This is a great example of our commitment to quality improvement as we measure ourselves against industry standards and gain ideas for how we can continue to enhance what we are doing to support efforts towards the next level of certification.” n H
Adoctor at Princess Margaret Cancer Centre is supporting the development of a curriculum to help healthcare professionals navigate the complex and ever-evolving Medical Assistance in Dying (MAID) program.
While MAID was legalized in 2016, the legislation has since been amended and expanded, making it more challenging for physicians, who receive limited training as medical students in how to discuss MAID with patients, and how to implement the legislation.
“From one day to the next, it became something that doctors and nurse practitioners needed to be able to provide to patients who requested it – but nobody learned how to do this in medical or nursing school,” says Dr. Madeline Li, psychiatrist and clinical scientist at the Princess Margaret.
Dr. Li says this created a need for clear training for medical students and providers alike. She hopes the creation of a standardized, national curriculum will ensure every healthcare professional in Canada is trained in how to provide access to patients who request MAID in a safe and appropriate way, and how to navigate difficult conversations.
Dr. Li is one of three co-Leads on the project, along with Dr. Stefanie Green, a family physician in Victoria who is President of the Canadian Association of MAID Assessors and Providers (CAMAP), and Dr. Gord Gubitz, a neurologist with Nova Scotia Health in Halifax.
MAID was first offered to patients with terminal illnesses such as cancer, following a decision by the Supreme Court of Canada that found prohibiting assisted dying infringed on patients’ constitutional rights. Patients had to have a “grievous and irremediable” condition, be in an advanced state of decline, and undergoing intolerable suffering. Two assessors needed to confirm the request, and the patient had to be found to be capable to make the decision.
Last year, the federal government expanded eligibility to include Canadians who aren’t dying imminently, removing the requirement that their death be “reasonably foreseeable.” Pa-
Dr. Madeline Li, a psychologist and clinician scientist at the Princess Margaret Cancer Centre, is co-leading development of the curriculum to help healthcare professionals navigate MAID, which was legalized in Canada in 2016.

tients whose death is not reasonably foreseeable must now either be assessed by professionals with expertise in their condition, or have one of their assessors consult with a professional who has the requisite expertise.
The number of MAID deaths has increased in Canada from 1,000 in 2016 to 31,644 in 2021.
“The development of a curriculum is much needed, important work to ensure that healthcare providers in our country who are involved in MAID can have the competencies required to serve their patients,” says Dr. Mark Bonta, head of the MAID program at UHN.
“This was something that was expected because it was legislated, but that expectation didn’t come with any training or skills – and in my experi-
ence overseeing the program at UHN – this isn’t something that’s easy to do, and not something that clinicians are comfortable with.”
Dr. Bonta explains that the team of UHN clinicians who volunteer their time to complete MAID assessments and interventions is made up of 22 physicians and nurse practitioners, which reflects the number of providers who are most comfortable with this field.
He hopes that a formal curriculum, once made available to all clinicians at UHN, will lead to a sizable increase in the number of clinicians comfortable with responding to requests for MAID.
The curriculum, being developed by the CAMAP consists of seven separate modules designed for existing healthcare providers, and all medical students and residents across the country.
The first module aims to normalize the practice in medicine, consisting of legislative background, history, ethics, and the role MAID plays in palliative care. The second module will teach providers how to converse with their patients about MAID, including the discussion of care goals, the severity of pain, and alternative options.
The third and fourth modules, with Dr. Li chairing the fourth, consists of general assessment and eligibility criteria, as well as a deep dive into complex assessments regarding the capacity and vulnerability of the patient. Similarly, modules five and six focus on the steps involved in providing MAID in both straight-forward and complex case scenarios.
Module seven, which is still being developed, is about navigating MAID for patients suffering solely from mental health disorders and mental health co-morbidities. Dr. Li says this module is particularly challenging.
“If you have cancer, and on top of that, you’re depressed, how do you determine which is driving the MAID request?” she says.
The federal government is widening access to MAID to include people with a mental health diagnosis as a sole criterion, effective in March 2023.
“Canada has not assessed or approved any cases like this before, so the question becomes: How do we safely assess patients with a mental health diagnosis for MAID?” Dr. Li says.
There is content embedded throughout all seven modules designed to help providers manage their own mental health in light of such emotionally charged work.
“Given how complex this environment is, the curriculum will really help to create a robust educational tool that will enable providers to administer MAID confidently,” Dr. Bonta says.
“It’s great that the CAMAP community has come together to create the tools to help people provide such a complex service.”
H





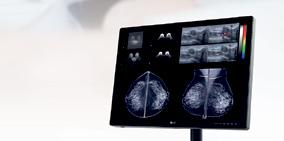
Getting the full picture from your medical imaging is critical to patient care. That’s why LG Medical Displays use the latest innovations to help medical professionals easily distinguish even delicate details with accuracy and efficiency. And with the added convenience of ergonomic design, intuitive hot keys and lighting features, we’ve made our displays more user-friendly. Learn more about all the details that go into an LG Medical Display and request a demo at: lg.com/ca_en/business/digital-showroom/medical-display






For anyone who works in healthcare, it’s a familiar pattern:
Patients struggle to find access to care. Spikes in demand – the most recent driven by the tripledemic convergence of RSV, influenza and COVID-19 – overwhelms health system capacity. Both of these challenges amplify patient frustration, triggering an increasing number of them to verbally and/or physically abuse providers through insults, threats, and physical attacks. These unhealthy working environments are a primary driver of workplace burnout. They also contribute to the exodus of (desperately needed) providers.
Physicians and nurses have always suffered mistreatment at work. More than half of emergency department nurses experience physical or verbal abuse in any given week. In a survey of more than 4,000 doctors and medical learners conducted by the Canadian Medical Association (CMA), 40 per cent said intimidation, harassment, bullying and/ or micro-aggressions happen “often” or “frequently,” with women and racialized providers particularly at risk.

Typically, statistics like these have been greeted with a shrug. “It’s part of the job.” But the pandemic has escalated abuse in every health care setting. In my own practice as an anesthesiologist, I’ve been punched, kicked, scratched and spit on. I have been yelled at and threatened. During the pandemic this aggression has extended beyond the clinical environment, into my personal life. My situation is not unique. The prevalence and severity of abuse directed at health workers continues to expand and escalate.
Last January, new legislation finally came into effect to make intimidation and bullying of health workers a distinct criminal offence. The CMA was instrumental to the passage of Bill C-3, which has so far resulted in three charges in Ontario alone. Convictions can mean up to 10 years of prison time.
Strengthening protections for health professionals – best implemented before abuse happens, but also after the fact – is critical.
Some hospitals have constructed barriers at nursing stations. Video surveillance and “body-worn cameras” are in use at Kingston Health Sciences Centre. In the book Code White: Sounding the Alarm on Violence Against Health Care Workers, a source describes “a safe room where nurses could run to, lock the door, and we have a phone.”
The serious toll of workplace harassment on physician mental health also needs urgent attention: Respondents to our National Physician Health Survey who reported frequent experiences of harassment were twice as likely to score positive for depression than their peers, three times more likely to suffer from burnout and four times more likely to experience moderate or severe anxiety.
The CMA is building a national framework to foster better access, incentivization and accountability for doctors’ psychological and cultural wellbeing, as well as their physical safety.
All of this work must be accompanied, however, by pointed, immediate action to address the roots of aggression towards health professionals – the understaffing and under-resourcing of care.
Harassment of health workers is still focused at the level of individuals instead of the system. We need better ways to identify perpetrators and hold them to account across working environments. We need better shields and better support for the victims of abuse.
But we must also shift the current culture of physicians and other health professionals internalizing these messages, putting pressure on themselves to “just keep going.” We must shift the culture of silence when it comes to unreasonable and unsafe working environment for health workers.
In October, the government of British Columbia announced “a new security model across all health authorities,” including the hiring of 320 in-house protection services officers and 14 violence prevention leads.
“Ensuring our health-care facilities are free of violence will not only help us recruit and retain health-care workers, but it will also improve patient care and continuity,” said Adrian Dix, Minister of Health.
A health system that is truly free of violence, though, is one where we also address worsening access and overwhelmed health systems. We cannot care for patients unless we care for our health workforce. These conversations are complex, but that also means small changes can have major impacts.
At the CMA, we’re committed to doing all we can to break the vicious pattern of staff shortages, staff abuse and staff exodus. Working with colleagues across the health sector, we’re pursuing an agenda of change to transform the system for the future – for providers and our patients. n H



 By Roxane Bélanger
By Roxane Bélanger
An implanted electronic device about the size of a toonie has helped Deberah Witteveen reclaim her life and overcome a debilitating medical condition few people want to discuss.
After coping with chronic fecal incontinence for 25 years, the Brantford, ON resident is no longer afraid to leave her house for fear of having an embarrassing accident. She no longer has to wear an adult diaper 24/7. And she doesn’t have to constantly think about where the nearest bathroom is located, just in case her bowels decide it’s time to go without warning.
“It’s huge. I’m so thankful. I’m so blessed,” the 61-year-old says. “It’s pretty incredible. It’s like something you needed but didn’t know you needed until you got it. It makes a big difference in my life.”
Witteveen’s newfound freedom is the result of a minimally invasive procedure, called sacral neuromodulation (SNM) therapy. The treatment has been available for more than 25 years but is not yet widely offered or commonly discussed with Canadian patients.
Witteveen had a Medtronic InterStim sacral neuromodulator implanted in her upper buttock at Toronto Western Hospital in September 2021. This tiny transmitter can be described like a pacemaker for the bowel or bladder.
The high-tech treatment targets communication problems between the sacral nerves, which control the communication pathways to bowel and bladder function, and a patient’s brain. If there is miscommunication between the brain and the sacral nerves – located near the tip of the tail bone – patients such as Witteveen
can experience fecal or urinary incontinence. To correct the problem, an implanted neuromodulator delivers mild electrical impulses to re-establish proper communication between the brain and the sacral nerves, helping patients regain control over their bodily functions.
“It’s definitely not a well-known treatment and also these conditions aren’t openly talked about,” says urologic surgeon Dr. Dean Elterman, Canada’s foremost authority on the therapy and the main surgeon performing this surgery at Toronto Western University’s urology clinic. “A lot of people are embarrassed about these conditions. They don’t talk to their physician about it. It’s very much a hidden condition. There are a lot of people who suffer in silence.”
Typically, sacral neuromodulation is recommended only after other lines of treatment – such as medication, exercise, or dietary changes – are determined to be ineffective. But because of the stigma surrounding incontinence
Medtronicand a lack of general awareness about sacral neuromodulation, many patients wait years to access the therapy or never access it at all.
There are less than ten hospitals in Canada that perform sacral neuromodulation procedures and the therapy is not available in all provinces and territories. Despite a significant number of people living with chronic urinary and fecal incontinence, less than 500 patients nationwide are implanted per year. * As a specialized centre, Toronto Western treats many of these cases, but the urban location can be a challenge for rural patients.
Dr. Elterman would like to see access to the therapy broadened and increased across the country, with at least one hospital in each province offering sacral neuromodulation to patients.

“The potential number of patients out there who need this therapy is in the tens of thousands in Canada. There’s a tremendous potential to grow,” he says. “It is absolutely life-changing therapy for these people who have to wear diapers and then get their lives back.”
A year after she received her implant, Witteveen says she doesn’t consciously think about the small electrical disk inserted just beneath the skin’s surface at the small of her back that controls her bowel function.
“It just does its own thing,” she says. “There’s no sounds or vibrations. It’s just a feeling. I just know when I have to go to the bathroom.”
The rechargeable battery in Witteveen’s implanted Medtronic InterStim transmitter is expected to last up to 15 years before she will need to have it replaced through another minimally invasive procedure.
After years of seclusion and uncertainty about her own body, she’s grateful to have regained her quality of life.
“My life has been totally changed,” she says. “I don’t have to plan where the bathrooms are. I don’t have to plan my route. I don’t have to pack a diaper bag. I just live my life. It’s the way it’s supposed to be.” n H

Since completing a nursing student placement at St. Michael’s Hospital in December 2020, Conor Goulden knew he wanted to find a permanent spot at the hospital.
“I did a student placement in my fourth year in the Cardiac Intensive Care Unit (CICU), and I remember thinking it didn’t seem possible to work in a workplace and love it so much that you almost feel like crying at the end,” he recalls.
Goulden hoped to find another student placement at St. Michael’s, but due to the COVID-19 pandemic there were no spots at the time. A few months later, he noticed a posting online for a paid clinical extern position that seemed like the perfect fit.
Since last year, the Ontario Ministry of Health has funded a clinical ex-
tern program to support organizations with health human resource challenges resulting from the pandemic. This funding support is slated to continue until March 2023.
Canadian healthcare employers have the highest ever level of job vacancies – with over two-thirds of those positions in nursing roles, according to Statistics Canada. Select hospitals in Ontario, including Unity Health Toronto, were invited to participate to support clinical externships, one of several initiatives the organization has undertaken to address clinical staffing vacancies.
Clinical externs are students who are still in the process of completing their educational programs. Employed as unregulated care providers (UCPs), they can help with specific care tasks, such as assisting patients with activi-
The Master of Health Administration (Community Care) prepares you to effectively manage and lead organizations in the dynamic and growing Community Care sector.
We are conveniently located in Toronto’s epicentre and offer a modular format that allows you to work full-time while completing the program in 16 months.
Learn more at torontomu.ca/mhacc
ties of daily living, supporting ambulation, positioning, feeding and toileting, as well as supporting admission assessments, preparing patients to go for tests, etc.
“Although they can’t do the same kind of work as a fully-trained nurse, externs help with duties that improve the quality of care for patients and play a support role to the unit,” says Julie McShane, Clinical Educator of Nursing Professional Practice at Unity Health. “Externships aren’t necessarily new – some hospitals have used them to provide summer employment to students for many years – but they’ve taken on an expanded importance with the pandemic and health system pressures.”
Once clinical externs have completed their formal education, Unity Health looks for opportunities to hire them into full-time and part-time roles. So far, 44 of the 157 individuals hired as clinical externs have transitioned into registered nurse (RN) and
registered practical nurse (RPN) roles, says Kaleil Mitchell, Project Manager II, Nursing Practice and Education.
Goulden says his externship with the inpatient orthopedics unit at St. Michael’s was an opportunity to supplement his nursing education by being able to observe nursing on a unit more broadly.

“It was like watching a live action documentary of nursing practice on a unit,” he says. “As a nursing student you’re assigned one preceptor, but as an extern some days you would be paired with one nurse, another day two nurses, or some days you’d be assigned an area in the unit.”
“It allowed me to observe how different people do things and you get to observe different skills, especially things like documentation, and it also gave me a chance to lift the fear of simple things, like calling locating to page somebody.”
1st program of its kind in Canada
Located in Toronto’s epicentre
Modular format allows students to work full-time while completing the program in 16 months
With a Master of Health Administration (Community Care), you can help fill the gaps in our healthcare system. There is a critical need for innovative and entrepreneurial leaders who can effectively and ethically lead, manage and/or start organizations that deliver care across diverse populations and locations.
Learn more at torontomu.ca/mhacc

s severe nursing shortages challenge hospitals across Ontario, a program at Unity Health Toronto is paying nurses to become specialized in critical care, helping to advance their careers and fill an urgent need.

The Critical Care Sponsorship Program supports experienced registered nurses (RNs) to become accredited in critical care nursing. Unity Health pays the nurses’ salaries while they are in school at George Brown College or the Michener Institute, and covers their class fees in partnership with Critical Care Services Ontario. The nurse receives both classroom and hands-on clinical education and is then buddied with an existing Intensive Care Unit (ICU) nurse at Unity Health until they’re ready to take on their own patients.
The hospital has doubled down on the number of RNs it supports annually in this career development, with close to 90 nurses annually advancing their skills and becoming specialized in critical care since the start of the pandemic, up from an average of about 30 nurses per year since the program first started in the late 1990s.
“There has never been a more pertinent time to foster the professional development and transition planning for nurses who want to commit their careers to critical care,” says Tasha Osborne, Senior Director of Surgery, Critical Care and Trauma at St. Michael’s.
The program takes 11 to 13 weeks to complete and is designed for RNs with one to two years of experience in acute care nursing. Most who complete the program come from within units at Unity Health, and about 10 per cent are hired from other organizations.
From eLearning to classroom training, PSHSA offers effective solutions to meet your organization’s unique needs.
All workers and employers should have access to the occupational health and safety information and training they need to keep their workplaces safe. That’s why Public Services Health and Safety Association (PSHSA) offers a variety of different courses that address your individual learning needs in the form of:
• Distance learning
• eLearning
• Classroom training
• Blended learning
• Sector-based training
• Paid and free training offers
Our anywhere learning allows PSHSA to enhance prevention activities by delivering solutions in a variety of convenient formats. Not everyone likes the same things, like food, so why would everyone appreciate the same way to learn?
Whether you’re looking for mandatory compliance training such as Joint Health and Safety Committee or WHMIS certification, new training to update your workplace’s health and safety policies like workplace harassment or slips, trips and falls, or to create custom learning with us, PSHSA has you covered.
Not sure where to start on your health and safety journey? Connect with a consultant today at pshsa.ca/consulting
“Having done the course myself, I think it’s the gold standard,” said Chrissy Lefkimmiatis, Patient Care Manager at the St. Joseph’s ICU. “There’s just no better way to prepare a nurse to work in the ICU than to have them go through this course.”
James D’Aloisio, an RN in the Trauma Neurosurgical ICU (TNICU) at St. Michael’s, found the support from the organization especially important. He started at St. Michael’s as a nurse in Orthopedics and was inspired to apply for the course after being redeployed to support critical care pods during the pandemic.
“I could fully commit to my studies and didn’t have to worry about working while I was in school,” he said.
D’Aloisio and his classmates have become irreplaceable in the delivery of critical care services within the highly specialized ICUs at Unity Health, says Liz Butorac, Clinical Leader Manager in the TNICU at St. Michael’s. “Without them, we wouldn’t be able to provide the high quality care we have.”
This is especially important now, with the organization facing a 13 per cent vacancy rate in critical care.
From an organizational standpoint, the program is the best of both worlds,
explains Manson Locke, Vice-President of People and Chief Human Resources Officer. Similar programs also exist to train RNs for other specialized areas such as the operating rooms. The hospital’s leaders are also looking to this approach as they plan solutions to support other specializations that may experience high vacancy rates.
“While attracting new talent is important, what’s of higher value is retaining the talent we have,” he says.
“This program allows us to retain people and put them on a career trajectory they’re looking for, while also filling gaps in some of these highly specialized areas. It’s what makes Unity Health a workplace of endless opportunity. No matter what area of care you’re interested in; we invest in helping people grow.”
And grow they will, Osborne says. In her experience nurses who specialize in critical care often grow into formalized leadership positions within hospitals and in the community.
“A love of the most complex patient care often turns into a love and desire to serve the complexity of the healthcare system,” says Osborne, who was a nurse in a neonatal ICU before
going on to earn a double Masters and pursue hospital leadership. “We’re fostering our next generation of hospital leaders.”
Like D’Aloisio, Brendan Daniel, an RN in the St. Joseph’s ICU who completed this program after starting his career at Unity Health in the hospital’s Interprofessional Resource Team, says
he’s found his passion by working in critical care.

“I love the one-on-one patient ratios, I love the support of the team, and the controlled chaos of an ICU. I have been able to become a preceptor on the unit and take on new opportunities,” he said. “This program has opened doors for me.” n H


Clinical externs also have the ability to build skills in communicating with patients, says McShane.
“Externs have that close contact with the patients they’re assigned to and a bit more time for longer patient interaction, which can be a great help on a unit that’s short staffed,” she says. “It’s also another opportunity to see and to make connections with different areas of the hospital because there are limited opportunities for students in the course of an undergraduate program to see different areas.”
After completing his externship and graduating from his nursing program, Goulden was hired full-time as a RN, first in the cardiovascular (CV) surgery unit and now in the CICU at St. Michael’s.
“I really can say with full confidence and belief that if I didn’t do my clinical externship, I would not




have been fully functional in CV surgery or the CICU,” he says “The externship allowed me to observe and become familiar with a lot of things, like policies, equipment and medication, without being responsible for it. So when I started in these fast paced areas, I felt more comfortable.”
Goulden adds that the nurses on the orthopedics unit where he completed his externship really embodied what it meant to be a teaching hospital.
“During my externship, often the nurses would come and say, ‘I have this neat thing that you probably haven’t seen, come over and have a look’, he says. “Everybody recognizes we’re a teaching hospital genuinely, and everybody wants to teach. That part of the experience has been invaluable to me starting my career.” n H
Here’s a wonderful story of the connection formed between a nurse trained abroad, Alina, who was eager to share her experience with newcomers as a mentor, and another nurse also trained abroad, June, who was dreaming of the day when the recognition process would become more fluid.

By now, we’re all aware of the many challenges the healthcare sector is facing in terms of resources; skilled professionals are rare, and the needs are significant – and Hôpital Montfort, Ontario’s Francophone academic hospital, isn’t spared.
Recently, the College of Nurses of Ontario launched the Supervised Practice Experience Partnership program.

At Montfort, this was something we wanted to explore, but
our needs regarding bilingualism made it so that only a few students were selected on the ten or so pairings identified by the Ministry of Health.
(Since then, Montfort has launched an immersion program, meaning people who speak only French or only English can be considered for some roles without conforming to our language requirements when they’re hired. For more information, visit montfort.ca/ en/immersion.)
I wanted to share with you the first ever experience we had with the Supervised Practice Experience Partnership program at Montfort.
June arrived in Canada with her family four years ago. She then lived in Montreal and worked in a field more or less related to active healthcare, but her heart was still with her former profession, the one that she was practicing in her



MCC 360, a multi-source feedback and coaching program, helps physicians improve their communication, collaboration, and professionalism. The program gives physicians insights into their practice by providing feedback from those who matter most – their patients, colleagues and co-workers – and supports their development with one-on-one coaching.
Organizations across Canada, including hospitals and provincial colleges, are incorporating MCC 360 into their quality assurance programs because of the:
• Insightful report collating qualitative and quantitative feedback collected from patients, colleagues, and co-workers for each physician
• One-on-one coaching options that fit respective organizational needs and help physicians constructively understand the feedback and build an action plan
• Dedicated, bilingual customer service to support the program, administrators and participants
• Research behind MCC 360 and its status as a Health Standards Organization Leading Practice


Eighty percent of participants self-reported in a survey that they made practice changes based on the feedback and coaching. Through the program, physicians also earn CPD credits from the Royal College of Physicians and Surgeons of Canada and the College of Family Physicians of Canada. MCC 360 o ers organizations meaningful, in-practice assessment and support of physicians to further develop their CanMEDS roles, which have been shown to improve patient outcomes. Learn more at www.mcc.ca/mcc360
Alina (left) and June (right) on June’s final integration day.
She jumped on the opportunity offered by Montfort to join a supervised practice program, knowing she could be a nurse once again.
What June didn’t know back when she joined the program was that five or six years ago, Alina, who received her nursing degree in France, went through a very similar process, which took a lot of tenacity and resilience on her part. Alina knew exactly what June was facing and the emotions going through her.
They met at Montfort, and the rest is history.
“Alina wasn’t just my mentor, she was also my French teacher”, says June, laughing.
“She learned quicker than I thought”, remembers Alina, “she really surprised me!”
“I know my capabilities and the limitations related to my program, so I didn’t hesitate to ask Alina and the entire team for help”, explains June.
“I’m really happy I got to contribute to her learning”, adds Alina, who says she is willing to mentor more candidates through the program. “It’s a pleasure for me. I was in their shoes a few years ago, so I understand what it all means for them.”
“This experience helped me regain my confidence and understand my responsibilities as a nurse in a care unit at the hospital”, says June. “It’s different than where I’m from. I was able to familiarize myself with the Canadian healthcare system.”
“Now, I’m trying to get her to come back and work with my team”, adds Alina, laughing. “She’d be a great candidate if she ever decides to come and work at Montfort. I’m really thankful that I got to take June under my wing. It was a pleasure to teach her how we work in unit 4A.”
A few weeks ago, we received a message from June, saying she had just gotten an email from the College, telling her she could sign up and thanking us.
As we like to say, once a nurse, always a nurse. June wanted to be a nurse again, especially in the current circumstances. She was able to find her way back to the profession with the help of Alina.
Thank you, Alina, for being the great mentor – in nursing and in French!
Montfort is proud to have contributed to the integration of a nurse in the healthcare system. n H
Judith Makana is a Professional Practice Advisor at Hôpital Montfort.

Dr. Mireille Norris knows firsthand about the unique disadvantages Black and Indigenous students experience while pursuing careers in medicine.
“I struggled as a Black woman who navigated the medical system,” she says, citing isolation due to the lack of Black representation in the field as well as racism and its resulting sense of unworthiness as just a couple reasons for her challenging path. “I’ve been shouldering a lot more than many of my peers throughout my career, and that has affected my academic productivity.”
With just over two per cent of Canadian physicians identifying as Black and less than one per cent of physicians identifying as Indigenous, similar issues continue to manifest in the newer generation of aspiring Black and Indigenous physicians.
“They really struggled with mentorship, representation, access to research and experiencing discrimination,” says the geriatrician, speaking of the Black medical students she’s encountered in recent years. Reflecting on their circumstances, she says, “I felt that I really needed to build the pipeline.”
After brainstorming with her colleagues and friends Dr. Jill Tinmouth and Dr. Nick Daneman, and after expedited planning and approvals, the Sunnybrook Program to Access Research Knowledge for Black and Indigenous Medical Students – also known as SPARK – was born.
“The idea driving SPARK is to provide various opportunities,” explains Dr. Tinmouth. “We identified strong mentors and research projects, and another key element was to pro-
vide financial support throughout the program.”
SPARK, which is in the midst of its second year, is providing Black and Indigenous medical students with an opportunity to engage in meaningful and fairly-paid research externships at Sunnybrook.

Dr. Norris explains this is a unique opportunity that many Black and Indigenous students typically would not be able to access.
“Residency is very competitive. There’s a disproportionate weight given to research experience. If you have a research opportunity, it reflects well on your resume. The students more likely to access these externships are those with parents and other connections in the medical community, which is not always the case for students who are Black and Indigenous,” says Dr. Norris of medical residency applications.
She adds, students are likely to face financial strain as research externships are often unpaid positions, leaving them with the difficult decision of choosing between an unpaid or low-paying research position and a part-time job to support their education.
In addition to addressing disparities in research access and its accom-
panying financial barriers, SPARK also equips students with networking opportunities by providing participants with three individualized mentors, including a Black or Indigenous physician who will help the student navigate being under-represented in the field.
“Many of the challenges that may go unnoticed to other people can be shared and discussed between myself and an Indigenous physician,” says Sophie Weiss, an Indigenous SPARK participant, of the benefits of having an Indigenous mentor. “It just creates the opportunity to ask questions from another person that’s in a similar position, but who is ahead of you in terms of their career. It can really provide that guidance.”
Passionate about geriatric medicine, Sophie, who is one of just two Indigenous students in her class at the University of Toronto, worked with Dr. Norris and Dr. Barbara Liu to understand how the COVID-19 pandemic has impacted the geriatric fall prevention program.
“I [felt] very in control of my own project, which is really, really excit-
ing,” says Sophie. She notes that one of SPARK’s goals is to support students as leaders in their research projects, which may lead to additional opportunities such as becoming co-authors of a manuscript, thus strengthening their residency applications.
Of her supervisors allowing her to have autonomy over her work, she says, “I felt like they wanted me there, rather than me really hoping they would accept me.”
Amal Ga’al, a fellow SPARK participant who worked with Dr. Daneman on the COVID-19 expansion to outpatients project (COVIDEO), shares the same sentiments as Sophie when reflecting on her project and research mentor.
When prospective SPARK supervisors applied to take part in the program, they had to submit a statement of intent, sharing their personal stories and reasons for wanting to be involved.
For example, in his submission, Dr. Daneman discussed how racial equality was always important to him. He was born in South Africa during the apartheid, but was brought to Canada by his parents as an infant so that he could be raised in a more just society. He grew up idolizing Nelson Mandela and says he’s excited to be a part of SPARK, something that will help contribute to “true, equal opportunity for justice, education, health and happiness.”
“Being able to have supervisors and physicians actually share of themselves and explain why they were excited about the program sets you up with a feeling of not just being accepted, but very much embraced and brought into the fold,” says Amal.
This sense of mutual respect and collaboration, versus the typical supervisor-to-student power imbalance you might find in other research environments, is an intentional part of this innovative program.
“There is an injury that comes from being racialized,” says Dr. Norris. “When you have faculty who say, ‘I see you, I know you, I feel for your struggle,’ it helps bridge that experience and heal the wound.”
Amal, who is a member of U of T’s Black Medical Students Association, says that with the rise of conversations surrounding anti-Black and anti-Indigenous racism, some engagement can seem performative and disingenuous. But both she and Sophie agree that the efforts made by SPARK to enhance their communities have been genuine, self-reflective and welcoming – qualities that Dr. Norris is proud to see in both racialized SPARK supervisors and allies who’ve supported the program.
Dr. Tinmouth echoes this, specifically giving kudos to all those who enthusiastically helped financially.
“We could not have pulled this without the quick support of the organization, the Sunnybrook Depart-
ment of Medicine and the Sunnybrook Research Institute,” she says. “It was remarkable.”
“I think it’s really fantastic the way the Sunnybrook community answered the call,” says Dr. Norris.
While SPARK is aimed at helping students elevate their educational opportunities and medical careers, its impact will be felt beyond the program, through the work that students will go on to do in the community.
“I have a very large interest in Indigenous health, and I plan to do
lots of outreach and really form my future practice around that,” says Sophie.
She also notes that Indigenous people are highly represented in the Toronto patient population but very poorly represented in the physician population – characteristics that she wants to change.
“Representation is so important,” she says. “I know that I can make an impact.”
Amal says she’s still figuring out what her medical career will look like, but she’s grateful that SPARK has exposed her to physicians with all kinds of different paths.
Kaitlin Jingco, a digital communications specialist at Sunnybrook Health Sciences Centre.
CARE Centre for Internationally Educated Nurses (IENs), a government-funded nursing-specific organization, has been supporting newcomer nurses back into practice for 21 years. CARE Centre helps IENs meet Registered Nurse (RN) and Registered Practical Nurse (RPN) licensing requirements.
CARE Centre offers programming for Professional Development with signature courses and workshops. Mentoring opportunities introduce IENs to the Ontario nursing context, helping them increase clinical language proficiency, and offering valuable workplace experience. Observational Job Shadowing (OJS) gives member IENs in-person exposure to the Ontario healthcare workplace through interaction with expert nurses in different sectors. Virtual Mentoring, developed during the COVID-19 pandemic, offers remote mentoring sessions between IENs and expert nurses employed in a variety of roles.
Based on experience as the lead pilot organization, CARE Centre is uniquely positioned to support healthcare organizations in effectively implementing the Supervised Practice Experience Partnership (SPEP), a collaboration between the College of Nurses of Ontario (CNO), Ontario Health and CNO-approved employers.
More recently, CARE Centre actively supported employers and the CNO in the adaptation of the Temporary Licensing option, which enables IENs to meet registration requirements while helping employers solve critical nurse staffing shortages. Contact CARE Centre to find out how to bring global nursing experience to your workplace: www.care4nurses.org
CENTRE FOR INTERNATIONALLY EDUCATED NURSES
Supporting Nurses Back into Practice
Regardless of where her medical career goes, Amal says, “I’m really interested in inequality – how do you address that, and why does poverty exist in society? Why are certain people marginalized?” Looking forward, she says, “I want to be involved in addressing and alleviating some of those issues.”
As for Dr. Norris, Dr. Tinmouth, Dr. Daneman and the rest of the SPARK team, they will continue advocating for Black and Indigenous medical students by continuing to carry out the program in years to come.
“My hope for SPARK is that other hospitals will follow Sunnybrook’s footsteps,” says Dr. Norris.
“SPARK exemplifies transformational actions from the hospital’s leadership team that will bolster the future of Black and Indigenous learners for success in medicine, which will lead to greater representation, fairer opportunities and better care for all.” n H

Employers: Join CARE Centre’s Mentoring and Observational Job Shadowing programs to attract IENs
CARE Centre can help navigate the Supervised Practice Experience Partnership (SPEP) and Temporary Licensing with Workplace Integration Initiatives and Preceptor Support
Our Member IENs can help meet your Nurse Staffing Needs
Visit www.care4nurses.org for more information
WHILE SPARK IS AIMED AT HELPING STUDENTS ELEVATE THEIR EDUCATIONAL OPPORTUNITIES AND MEDICAL CAREERS, ITS IMPACT WILL BE FELT BEYOND THE PROGRAM, THROUGH THE WORK THAT STUDENTS WILL GO ON TO DO IN THE COMMUNITY.

 By Tina Novotny
By Tina Novotny
The current crisis in Canadian healthcare has made attracting, registering, integrating, and retaining international healthcare professionals more important than ever. With many hospitals running over capacity, adequate staffing is crucial. Hospitals can create more beds by adding equipment to rooms and wards, but those interventions can’t meet increased patient demand without bedside nurses.
CARE Centre for Internationally Educated Nurses (IENs) has been supporting nurses back into practice for 21 years. CARE Centre is funded by the Government of Ontario, and since 2016, receives funding from Immigration, Refugees and Citizenship Canada to offer a pre-arrival program for nurses to jump-start their registration process. Along with settlement sup-
port, language instruction and exam preparation, CARE Centre offers a variety of professional development (PD) programs to help IENs meet the College of Nurses of Ontario’s (CNO) registration requirements, while working closely with employers to bring more nurses on board.
Some hospitals, like Toronto’s Sunnybrook Health Sciences Centre, run PD sessions on-site for CARE Centre members, such as a recent “Updating Your Health Assessment Skills” workshop. Kimberly Lawrence, interim Advanced Practice Nurse for Interprofessional Practice, Special Projects at Sunnybrook, says that the workshop focused on supporting IENs to revisit and update their existing head-to-toe assessment, and practice this nursing skill in a supportive learning environment.“We wanted to acknowledge
Expand your knowledge. And your career.
that they’re bringing a lot of experience to our organization, and this is a refresher,” Kimberly says.
Join the WeRPN community, and invest in your professional growth
WeRPN’s workshops and e-learning programs provide ongoing professional development so RPNs can respond to the continually changing nursing environment.
Find out how you can expand your expertise at werpn.com/learn
Join our community of engaged, supportive and knowledgeable RPNs committed to excellence in patient care. Half-year memberships available. New Grads get 50% off our annual fee. Flexible payment options available.
Gain an edge on your nursing practice at werpn.com/join
One of CARE Centre’s longest running PD programs is Observational Job Shadowing (OJS), which offers IENs the chance to pair with expert nurses, gaining exposure to the Canadian healthcare workplace, choosing their placement from twenty-one employer partners across Ontario. A recent OJS participant noted, “I feel quite lucky that my first OJS was in the ER Department. It gave me the chance to get a glimpse of the healthcare crisis. It made me face the reality of what I’m getting into. I understood why (obtaining my nursing registration) is a long and arduous task; being there to see things firsthand helped me appreciate why the rules are in place because the quality of care given to patients must never be compromised.”
Employers continue to see the value of the OJS program, with North York General Hospital (NYGH) recently joining after a second nurse employee at their hospital was recognized with CARE Centre’s Joan Lesmond IEN of the Year Award. RN Amina Malik, a nurse educator originally from Pakistan, won the award in 2022, which was presented by 2013 award-winner Edsel Mutia, an RN originally from The Philippines who now works at NYGH in a supervisory capacity.
“As IENs, all of us go through our own professional journey and it may get rough, but no matter how difficult and challenging the days may get, IENs should never forget the reason they became a nurse,” said Malik. “IENs and all nurses should never forget the difference they make in the lives of so many people.”
“Our Internationally Educated Nurses program is an extremely important initiative to expand NYGH’s clinical teams,” says Karyn Popovich, President and CEO of North York General Hospital. “Amina is a shining example of someone who is focused on people-centred care and demonstrates North York General’s core values.”
During the COVID-19 pandemic CARE Centre started a Virtual Mentoring program, a popular option, allowing IENs to connect with expert nurses online, particularly valuable for IENs wanting to return to a specialized area of nursing. CARE Centre continues to find solutions to mitigate the considerable timelines of registration requirements while helping employers solve critical nurse staffing shortages. Growing from an earlier project CARE Centre piloted with University Health Network, CARE Centre collaborates with CNO-approved employers for the Supervised Practice Experience Partnership (SPEP), an initiative by the CNO and Ontario Health. Through
SPEP, IENs participate in a supervised clinical placement for a minimum of 140 hours, earning income while helping to meet evidence of practice and language proficiency conditions with the CNO. CARE Centre also works with IENs and ready employers to assist IENs in obtaining Temporary Licenses with the CNO so they can return to active practice while completing their full registration requirements.
“There have been really beneficial developments of systemic change during these unfortunately unprecedented times. After the predicted wave of baby boom retirements happened, the pandemic worsened the acute nursing shortage,” said CARE Centre Executive Director Dr. Ruth Lee. “IENs are finally being fully recognized as the valuable health human resource they are. They bring global
experience, cultural and language skills and years of nursing expertise to their new jobs in Ontario and across
Canada. The wider healthcare system is finally rallying to give them the support and opportunities they deserve.
We are grateful to our employer partners in working with our team in integrating IENs.” n H

From Leadership courses to tips on better self-care, WeRPN’s in-person and eLearning programs provide ongoing development to expand your nursing knowledge.
In-person workshops are back! Check out our line-up of FREE full day programs*
Scheduled for early 2023, workshops provide nurses with access to informative speakers, topic-specific education, and an opportunity for in-person gathering, creating a Community of Practice to further education, engagement and support.

FEB 6, 2023
Building Resilience with Self-Care
MAR 1, 2023 Advancing Your Career; How to Lead and Influence
MAR 22, 2023 Being Culturally Competent: What does that mean?
For more details on our in-person programs, leadership courses, and monthly WeLearn webinar series, visit werpn.com/learn
In 2003, Dr. Geoff Fernie had what he admits was a wild idea: convert a smallish hole, destined to be a parking garage, underneath University Avenue in Toronto into a massive opening that could house four large research labs. At the time, Dr. Fernie was the Director for the Centre for Studies in Aging at Sunnybrook, while the KITE Research Institute, which was then called the Toronto Rehab Research Institute, was just in its infancy.
When he proposed the concept to the leadership team at Toronto Rehab – the hole would contain four large cylindrical structures where KITE’s growing stable of scientists could conduct their research – they were skeptical.
Fortunately for Dr. Fernie, who spent 15 years as Research Director at KITE and is currently the Creaghan Family Chair in Prevention and Healthcare Technologies, it didn’t take much to convince Mark Rochon, then CEO of Toronto Rehab, that having these labs – simulators that would mimic everything from weather and driving to conditions to help researchers study accidents accurately –was a good idea.
It was then that the Toronto Rehab Research Institute, renamed KITE in 2019, started becoming the world-leading rehabilitation research institute that it is today. The centre’s evolution is also a result of strong leadership, generous funding and smart scientists and clinicians, but the institute wouldn’t be what it is today without Dr. Geoff Fernie.
We spoke with Dr. Fernie, Mark Rochon, research associate Pam Holliday and postdoctoral student-turned-scientist Dr. Alison Novak to find out how KITE – which is an acronym for Knowledge, Innovation, Talent, Everywhere – came to be.
Mark Rochon: I started in late 1998 as CEO of Toronto Rehab, and our research efforts were quite small. There were a number of academic enterprises in post-acute care and rehabilitation, but none of them had sufficient critical mass to really push education and research alongside a clinical mandate. We needed an organization with significant clinical heft to be able to create a world-class research institute.
Before merging, Toronto Rehab was four different organizations: Hillcrest Hospital, the Queen Elizabeth Hospital, Lyndhurst Hospital and the Toronto Rehabilitation Centre. We were all post-acute organizations, none of which were large enough to offer much funding for scientists. One of the major reasons behind the amalgamation was the desire to create an organization with sufficient scale to support the development of a major academic enterprise with a focus on post-acute care.
Geoff: I always loved making things; I loved engineering. When I was in the final summer for my first degree, my advisor sent me to a special school in the south of England in the countryside, Chailey Heritage, that provided a living environment for kids with disabilities and also was a hospital.
I was assigned to look after kids whose moms had taken the drug thalidomide (a drug pregnant women were prescribed to combat morning sickness, which was later found to impact neonatal development). They had lost typically two or four limbs, with a lot of other complications as well. They were about seven years old, and had a lot of courage.
I would get up in the middle of the night to help the nurses change beds and really lived in the thick of it. I tried to work with prostheses for these children and saw some of the operations on them, and thought, “Wow, this is what I want to do.”
I was really taken by the fact that engineering was the only way that these kids were going to get a more reasonable life, so I applied to the PhD in bioengineering program at Strathclyde University, in Scotland. At that time in the U.K., it was necessary, once you got your doctorate, to spend some time in North America, and get what was a BTA, a “Been To America” qualification. Of course, when I came to North America I never went back.
Pam Holliday: Geoff was looking for a research assistant not too long after he arrived in Toronto. He was working at Toronto Western Hospital and they had money to do some projects related to amputee management and care at West Park Hospital, nearby. I actually don’t think I ever had an interview! He was doing rounds when I met him and he kind of tested my balance by, you know, pushing me to see whether I recovered. Then he said, “Yeah that’s good. You’ll do,” and away we went. So that’s how I started working with him on balance in the amputee program, in 1975, and we’ve worked together ever since.
Geoff: The long-term patients at West Park weren’t getting much activity, and there was a lot of incontinence and a lot of falls. I thought these were under-researched areas, and we should do something about them. That’s how we ended up focusing on balance and aging. Then in 1986, I got a visit from the CEO of Sunnybrook, who asked me to help start a Centre for Studies in Aging.
At Sunnybrook, I realized that you aren’t going to solve these problems by treating people after they’ve fallen over. It’s too late. We had to prevent
problems. I needed to build a laboratory that would allow me to study things like falling over in winter, pedestrians having problems on the street with traffic, elderly drivers getting into trouble, people falling down stairs or falling in bathrooms. That’s when I got the invitation to meet with Mark.
Mark: What Geoff brought to Toronto Rehab was a deep history with, and experience in, research and development work that made a real difference to patients and caregivers. He also had a vision for evolving the research enterprise at Toronto Rehab into the organization that you see today. It was great. It was one of the parts of my job that I enjoyed a lot –working with him and helping to create this extraordinary facility.
Mark: In 2001, I negotiated an annual $3-million grant for research purposes with the province of Ontario, and the Toronto Rehab Foundation added to that. We used that money to attract researchers to come to Toronto Rehab and investigate new treatments and technologies that might help people living with life-altering disease or injury.
Geoff: Mark was CEO of Toronto Rehab when I came on – a lovely, incredibly bright and very kind-hearted, enthusiastic guy – and without his support, none of the expansion would have been possible. His leadership was essential for modernizing TRI.
Mark: Together, we created a different focus for the research side of Toronto Rehab that not only looked at the efficacy of various treatment approaches but really asked the question of how we can make lives better for people experiencing life-altering disease, through the application of technology.
We had this idea to create a simulation laboratory as an anchor of the research efforts at TRI that would at-
How Dr. Geoff Fernie helped turn a small rehabilitation institute into a world-leading research centre
tract scientists, grad students and researchers to the facility.
Geoff: I wanted to create a motion base for a very sophisticated simulator and various environments that we could swap onto it – no one had done this before. We needed to be underground and we needed quite a high ceiling for cranes to move equipment around.
Mark: This coincided with the redevelopment of the University Avenue site of Toronto Rehab. And so, we were able to use that construction project to create a space that was purpose-built for the simulation laboratory Geoff wanted, with research spaces on the upper floors of TRI.
Pam: Once we opened up those labs, part of the process was building the science base, the network to use the facilities. So, setting the groundwork for people to come in and collaborate on research projects, collect data and even manage their data elsewhere.
Alison: I started at KITE as a postdoctoral research fellow, working with Geoff. I had done all my doctoral work on understanding stair ambulation and people who have had a stroke, and Geoff had a big vision for understanding and preventing stair falls.
Mark: Geoff’s fingerprints are all over what you see today at KITE. What we were able to do with him was create a different focus for the research enterprise that not only looked at the efficacy of various treatment approaches, and so forth, but really asked questions about how we can make lives better through the application of technology for people experiencing life-altering disease.
Alison: He started off as my postdoctoral research supervisor. And then, as I transitioned into a scientist role at KITE, Geoff was the Institute Director at the time. He informally served as my mentor, as I started out in my research career.

The biggest thing that Geoff did for me specifically was set me up for success in terms of developing my research program and aligning me with his contacts. A lot of my work is to redefine or to provide evidence to support building codes and building development, and as a mentor Geoff was exceptional at identifying where my expertise would be critical to their processes and just supporting me, as a new scientist, to get involved in those circles and in that industry.
Pam: Our research has always been not just understanding what’s going on – the biomechanics of what happens to balance, for instance – but simultaneously looking at what we can do about it. What are we going to get out of this? Are we going to change the way we do therapies? Do we have a new product? An improved way to make an artificial limb? Or can we change policies, regulations, codes, those kinds of things?
Geoff: We get feedback all the time about the results of research we’ve been conducting. We’ve changed building codes in Canada and we’re about to change more of them. We produce more publications at KITE than anywhere in the world. And not only do we write more, we actually have more impact than any other rehab research facility – the research that we do actually changes things. So I don’t think there’s a week that goes by without me feeling good about something we’ve accomplished.
Mark: Toronto Rehab is about knitting together research, education and care in a way that will improve not only what happens to individuals who come through here but the extent to which we can transfer what we’ve learned and our knowledge to other providers. Geoff’s legacy is one that’s really related to the positive outcomes people experience in their lives: helping people live their lives to the fullest following life-altering disease or illness. n H
WE’VE CHANGED BUILDING CODES IN CANADA AND WE’RE ABOUT TO CHANGE MORE OF THEM. WE PRODUCE MORE PUBLICATIONS AT KITE THAN ANYWHERE IN THE WORLD. AND NOT ONLY DO WE WRITE MORE, WE ACTUALLY HAVE MORE IMPACT THAN ANY OTHER REHAB RESEARCH FACILITY – THE RESEARCH THAT WE DO ACTUALLY CHANGES THINGS. – DR. GEOFF FERNIE
Sheila Leano-Cunanan says nursing is in her blood.
“Through my mom, I saw nursing as being a hard job, dealing with so many different people and circumstances, and also rewarding to help those who are in need and to serve humanity,” she says.
Fifteen years ago, Leano-Cunanan followed in her mother’s footsteps and became a nurse working in the paediatrics and Neonatal Intensive Care (NICU) units of a tertiary hospital in the Philippines, where she was born and raised. Five years into her career, she immigrated to Canada, but it was clear it would be a long process to get her license to practice nursing in Ontario.
She worked as a Personal Support Worker (PSW) while continuing to study, completing courses towards her nursing licensure and becoming a firsttime mother.
In 2020, Leano-Cunanan learned about a program for internationally-educated nurses that would allow her to reach her goal – and ultimately find herself coming full-circle, working at Unity Health Toronto’s paediatrics and NICU units.
Statistics Canada recently reported that vacancies in the health-care sector are at record highs, with over two-thirds of those positions in nursing roles. The Supervised Practice Experience Partnership (SPEP) program is an initiative launched by the College of Nurses of Ontario (CNO) and Ontario Health to help address the health human resource needs of the province.
The SPEP program provides paid, supervised work placements for Internationally Educated Nursing (IEN) interns going through the registration process to become nurses. These placements, created in collaboration with hospitals and other CNO-approved practice settings in Ontario, are meant to help candidates complete their evidence of practice and, in some
STATISTICS CANADA RECENTLY REPORTED THAT VACANCIES IN THE HEALTH-CARE SECTOR ARE AT RECORD HIGHS, WITH OVER TWO-THIRDS OF THOSE POSITIONS IN NURSING ROLES.
cases, language proficiency registration requirements.
At Unity Health Toronto, the program requires IEN interns to complete 335 hours of supervised practice over a three-month period. IEN interns may be seeking registration as a Registered Nurse (RN) or Registered Practical Nurse (RPN). The SPEP program is one of several initiatives the organization is undertaking to fill clinical staffing vacancies.
So far, Unity Health has been able to employ 17 of the internationally educated nursing interns who have completed their placements in the organization.
“It’s a long journey that internationally educated nurses have to go through to be licensed in Ontario,” says Julie McShane, Clinical Educator of Nursing Professional Practice and coordinator of the SPEP program at Unity Health. “It takes a lot of time and there are a number of hurdles they have to overcome.”
“This evidence of practice is really the last piece they have to meet to be licensed here in Ontario, so we want them to have the best experience possible. This has meant collaboration with our unit managers, human resources team, clinical educators and practice team.”
McShane says Unity Health has incorporated a somewhat unique approach to try to match IEN intern candidates with their past clinical area of expertise or one they have a strong interest in. The hope is that interns enjoy their experience with the organization and decide to apply to fill vacant positions.
Originally from India, Navdeep Kaur, an RPN intern candidate in the program, says she was excited to be placed on the Cardiology unit at St. Michael’s Hospital, as she wanted to follow in the footsteps of one of her college professors.

“I worked in a charitable hospital back home for two years where they
don’t have much of a budget,” she says. “At first, before getting to know how health care works here, my confidence was close to zero but my preceptor was so sweet and worked with me and explained how to do things and now I feel I’m at 100 per cent.”
McShane says the involvement of preceptors has been a critical part of the program. Preceptors are paired with an IEN intern for a specific time period to assist and support learning experiences and orient the IEN intern to the practice placement.
Amita Ganeshan, an RPN on the 2L Medicine unit at St. Joseph’s Health Centre, says her passion for teaching drove her to volunteer to be a preceptor to an IEN intern on her unit.
“I focused on trying to give information about the nursing culture at St. Joseph’s and orienting our intern to the unit,” Ganeshan says. “We sat down together from the beginning so I could understand her nursing experience and skills from back home, and I let her know she should feel empowered to speak up and ask questions at any time.”
“Now she’s licensed and was able to get a job on our unit!”
For Leano-Cunanan, her nursing journey in Ontario has brought her to the same clinical care area where she began her career in the Philippines.
She completed her internship placement on the paediatrics and NICU units at St. Joseph’s and was hired there as an RN.
She says the camaraderie and team work she witnessed on the paediatrics and NICU units made her internship enjoyable and has made her grateful to join the team.
“At certain times through this journey, I sometimes thought about giving up on nursing because of the pressures of life, being an immigrant, trying to provide for my family,” Leano-Cunanan says. “To others going through the same thing I would say, if nursing is your passion, just never give up and be strong for your dreams.” n H
Prior to October 1, 2013, Windsor Regional Hospital and Hôtel-Dieu Grace Hospital each operated an acute care hospital servicing Windsor/ Essex, Ontario and the Erie-St. Clair region for various tertiary and quaternary services. In addition, Windsor Regional Hospital operated non-acute services at a standalone campus. However, as a result of previous health services restructurings, neither hospital would be considered a full-service general hospital. Each operated various speciality services which unfortunately resulted in hundreds of patients having to be transferred between acute care campuses annually.

In 2008, both hospital corporations were faced with needing to create master site plans for future planning of both services and facilities. During this planning, it became obvious that the current two acute care organization structure was unsustainable. After extensive community consultation, a decision was made that the benefits of one acute care organization was needed for patients and future growth. This resulted in working with the Ministry of Health on planning for a new acute hospital for Windsor/Essex. Also, more importantly, it resulted in the Boards of Directors of both Windsor Regional Hospital and Hôtel-Dieu Grace Hospital agreeing to have Windsor Regional Hospital take responsibility for all acute care services, and Hôtel-Dieu Grace Hospital taking responsibility for sub-acute services at the standalone campus.
Many assumed that we had two full-service hospitals prior to 2013. We did not. Windsor Regional Hospital and Hôtel-Dieu Grace Hospital each operated many unique services requiring patients to flow back and forth for clinical care. However, that was difficult at times due to, among other things, demands within each organi-
zation at any given time. Since 2013, the fact we have now one acute care organization has been beneficial to the patients we serve even though moving to one combined site is still the goal. Due to aging facilities, we have faced floods, equipment issues and heating/ cooling disruptions to name a few. Having one acute care organization, one medical advisory committee, one administration and one board of directors during these disruptions or even facing day to day issues has resulted in a more efficient decision-making process and in many situations minimal, if any, disruption to patient care. In addition, there have been many patient care enhancements as we standardize patient delivery at both acute campuses and plan for a new acute care hospital for Windsor/Essex.
This consolidation of acute care services allowed Windsor Regional Hospital’s team to be in a much better position to face what our community, region and country faced during COVID-19. Looking back at the benefits of this consolidation in 2013 many have concluded we would have struggled mightily during the pandemic if not already in place. Instead, our team was able to plan effectively and proactively while also reacting quickly to the changing landscape locally, provincially and across Canada. This resulted in Windsor Regional Hospital being able to support hundreds of
patients from the GTA and also from outside of Ontario within hours of any request being made.
This leads us to the present and future. The creation of Ontario Health and dividing the province into five regions and the adoption of Ontario Health teams hopefully is a move towards a more regionalized operating structure to not only meet the demands we all face today, but the ones we will meet in the future. Hospitals can lead the way in these discussions. Again, this will help support day-today decision making for the benefit of patients let alone being able to address disruptions in services or facing issues such as outbreaks and pandemics of the future. n H
THE CREATION OF ONTARIO HEALTH AND DIVIDING THE PROVINCE INTO FIVE REGIONS AND THE ADOPTION OF ONTARIO HEALTH TEAMS HOPEFULLY IS A MOVE TOWARDS A MORE REGIONALIZED OPERATING STRUCTURE TO NOT ONLY MEET THE DEMANDS WE ALL FACE TODAY, BUT THE ONES WE WILL MEET IN THE FUTURE.
Drs. Heather Ross and Joseph Cafazzo are the winners of UHN’s 19th annual Inventor of the Year Award.

The researchers are being recognized for their discovery leading to the commercialization of the Medly platform, a fit-in-your pocket companion for heart care powered by software and artificial intelligence developed at UHN.
Medly is also the basis of UHN new venture Medly Therapeutics, poised to bring heart care benefits to patients around the world.
Dr. Heather Ross is the Division Head of Cardiology at the Peter Munk Cardiac Centre (PMCC), the Scientific Lead for the Ted Rogers Centre for Heart Research at PMCC, the Loretta A. Rogers Chair in Heart Function and the Pfizer Chair in Cardiovascular Research. Dr. Joseph Cafazzo is the Executive Director, Biomedical Engineering, the Centre for Digital Therapeutics, and Healthcare Human Factors (HHF) at UHN, and is the Wolfond Chair in Digital Health.
“Their pioneering digital health innovations are changing the face of heart health for patients nationwide,” says Dr. Brad Wouters, Executive Vice President of Science and Research at UHN. “Commercialization of the Medly platform is an example of translating world-class research into precision medicine – for the benefit of cardiac patients, as well as for individuals living other chronic diseases.”
Sponsored by Commercialization at UHN, the Inventor of the Year Award recognizes an individual or team whose invention has made a substantial and noteworthy commercialization contribution leading to A Healthier World.
Drs. Ross and Cafazzo worked closely with Commercialization at UHN to pivot the Medly technology into a foundational platform for UHN spinoff Medly Therapeutics. The process included the selection of a seasoned entrepreneur-in-residence (EIR) to lead company formation efforts. Commercialization at UHN continues to steward ongoing augmentations to Medly’s core technology.
The journey leading to the development and commercialization of
Medly would not have been possible without important contributions from members of TeamUHN and the University of Toronto, including Emily Seto, Shumit Saha, Bo Wang, Michael McDonald, Amika Shah, Kenneth R Chapman, Philip Segal, as well as UHN’s Centre for Digital Therapeutics team, the Ted Rogers Centre for Heart Research, PMCC and HHF. Drs. Ross and Cafazzo are also grateful for the vast philanthropic support from donors to UHN Foundation who have enabled the development of the Medly platform.
According to Dr. Ross, nearly one million Canadians are living with heart failure (HF) and one-in-five people over the age of 40 will experience HF. Challenges in treating HF include timing patient treatment with HF episodes, a lack of real-time, actionable patient data and limited patient involvement along the journey to better health.
To counteract these challenges, Drs. Ross and Cafazzo devised Medly to be an innovative digital self-management solution with 24/7 monitoring technology, making it accessible and easy to use for patients wherever they might be.
The Medly technology has proven to be effective clinically at UHN and
other sites, supporting more than 800 patients with chronic heart failure (CHF) at the PMCC. It has also led to a 50 per cent reduction in HF-related hospitalizations and a 24 per cent reduction in other hospitalizations, with patients reporting greater self-management support, confidence and peace of mind, and a better relationship with their care team.
“In delivering health care today, we are often still overly focused on treating patients once they become acutely ill and end up in hospital,” says Dr. Ross. “Leveraging the incredible power of big data, artificial intelligence and predictive analytics, Medly provides a more proactive, scalable and affordable solution to manage the epidemic of heart failure – and research is continually ongoing to enhance it.
“Working with the team at Commercialization UHN to scale Medly nationally and beyond will allow this technology to reach more patients than ever before.”
Dr. Cafazzo says, “innovative digital therapeutic solutions like Medly give patients an incredibly advanced capacity to manage their care at home, right at their fingertips, while still staying connected to their healthcare team.
“By detecting changes in a patient’s health status, Medly also allows care providers to intervene earlier, before the patient needs to be re-hospitalized for a serious complication such as heart failure, which can be an im-
mense added comfort to patients living with complex chronic conditions,” Dr. Cafazzo adds.
Commercialization at UHN is thrilled to recognize the world-class science, collaboration and commercialization of this groundbreaking digital health technology. It is exciting to see another UHN and Toronto ecosystem technology making bold strides towards improving health and reaching more patients in need.
Congratulations Drs. Ross and Cafazzo and teams!
Based on core technology invented at UHN, Medly includes an application that can be used on hand-held devices such as smart phones, home medical devices and wearables to help individuals self-manage heart disease. Every day, patients enter key details such as their weight, blood pressure and heart rate and answer questions about their symptoms. Using a sophisticated, expert system and machine learning algorithms, Medly assesses health risks in real-time and notifies the patient’s care team of any signs of deteriorating health. The app then triggers alerts to the health care team, which are presented alongside the patient’s list of medications, lab results, graphs and contact information. Medly allows care providers to intervene proactively, before the patient would otherwise recognize a need to visit a clinic or hospital. The team is now working to incorporate additional features into the Medly platform, including an automated solution to optimize medication dosages based on data from patient visits.
Medly’s technology is currently being channeled into Medly Therapeutics, a new venture partnership between Commercialization at UHN and Toronto Innovation Acceleration Partners (TIAP), scaling the technology for maximum patient impact.
For more information about the Medly platform, visit: www.medly.ca
For more information, including past winners of the Inventor of the Year Award, please visit: www.uhncommercialization.ca n H
PROVEN CLINICALLY EFFECTIVE(L to R) Dr. Brad Wouters, UHN’s Executive Vice President of Science and Research, Dr. Heather Ross, Dr. Joseph Cafazzo and Mark Taylor, Director of Commercialization at UHN. Photo credit: UHN StRIDe Team
Dr. Marla Beauchamp feels fortunate to be leading a first-of-its-kind study looking at how technology can help older adults with their mobility – a vital health indicator. Called McMaster Monitoring My Mobility – or MacM3 for short – the AGE-WELL-funded study is now underway and recruiting as many as 2,000 participants ages 65 to 80.
Before Dr. Beauchamp became an AGE-WELL researcher and associate professor, CRC (tier 2), Mobility, Aging, and Chronic Disease, at McMaster University in Hamilton, Ontario, she earned a master’s degree in physical therapy at the University of Toronto. As part of her studies, she did a placement working with older people. It marked an important step in a career
devoted to supporting healthy aging. Her pursuit is personal to a degree.


“I was very close to my grandparents, so that’s part of it,” she says. “I also appreciate the wealth of experience that older people share. I think about how they’ve contributed their whole lives – and wonder how we can help people to live independently for longer. I saw how important that was to my grandparents and it’s what interested me about physiotherapy and rehabilitation. It is the lens that I bring to my research.”
For the MacM3 study, Dr. Beauchamp and her co-leads from disciplines spanning geography, social science and mathematics, have created a smartwatch app that participants wear for 10-day intervals every four months throughout the two-year study.
Continued on page 36
Dr. Marla Beauchamp, School of Rehabilitation Science, McMaster University, leads the first-of-its-kind mobility study.

Home care is about trust. It is feeling comfortable with a provider coming into the home of someone you care for and, possibly, assisting with the most intimate care.
Bayshore’s home care services are extensive, varied, and personalized for each individual. Whether it’s just a little assistance for daily tasks or round-the-clock care, Bayshore’s caregivers can help your loved ones to live their best life while remaining at home.

Information collected includes step count, mode of travel, distance travelled and activity intensity. Everything is encrypted for privacy. This is in conjunction with GPS and additional health measures, such as in-person assessments, quarterly phone calls and monthly diaries.
Currently, there is no wearable that comprehensively monitors mobility and that is valid for predicting important health outcomes in older adults. Problems with everyday mobility, such as walking, getting in and out of a car, and driving, are common with aging and can negatively affect health and wellbeing. During consultations with older adults and caregivers, there was a clear interest in using wearable tracking devices to self-monitor mobility.
To date, study participants are from the Hamilton area. Recruitment will soon begin in Toronto through a partnership with the McMaster Institute for Research on Aging | Dixon Hall Centre.
With the data gathered in the study, machine learning and advanced statistical methods will be used to identify trajectories of change in mobility over time and how these trajectories relate to health outcomes, such as falls. With input from older adults and caregivers, the ultimate goal is to develop a mobility self-monitoring tool that can help prevent or delay mobility problems in later life through early detection and treatment.
The MacM3 study addresses a gap in mobility research. “While there have been studies looking at how fast people can get in and out of a chair and how fast someone walks, current mobility research doesn’t address how mobility is something to take charge of as a central strategy for managing your health,” says Dr. Beauchamp. “We go to a doctor who takes measurements, like blood pressure and BMI, yet there’s no measurement of mobility – something that we value so much.
It’s an indicator of our overall wellbeing and a future predictor of falls and hospitalization. Examining someone’s mobility is an opportunity for early intervention and information sharing.”
Irene Schieberl is one of the study participants. The 80-year-old Hamilton resident was keen to take part.
“I have participated in a few different studies conducted by McMaster,” she says. “I would like to help the senior population in any way I can to keep us healthy and in our homes as long as possible because that’s less expensive for the health-care system. This is a way for me to give back.”
Schieberl also thought it was a good chance to understand more about her own mobility. She has a life-long passion for dancing, everything from tap to Hawaiian and jazz, and performing
– something she hasn’t been able to do throughout the COVID pandemic. “I needed a way to get motivated and to improve my strength and stamina,” the mother of two explains. “During my exercise pre-tests at the McMaster Innovation Park, I was able to see how good my balance, endurance and strength were and get a benchmark for my current mobility.”
For Michael Kasoian, being involved in the study and wearing a smartwatch to track his movements is a way to monitor how his mobility will change over the next 24 months. The retired elementary school principal who lives in Burlington considers himself to be a very healthy 73-year-old –one who keeps fit by playing pickleball, walking and golfing. “When you get to be my age, you know things are going

to change,” he says. “I am interested in anything that can keep me as active as I can be.”
Over the course of the study, participants will send in monthly postcards to report falls, wear their smartwatches and an optional activity device on their thighs, and do a fitness test that will compare where they started physically and where they ended up two years later. They are asked to live normally throughout the study, keeping their normal level of activity and maintaining their current diets to get the most accurate assessment of their progress.
Before recruiting participants and equipping them with wearable devices, Dr. Beauchamp and colleagues worked with talented software developers to develop the specific technology that would gather the data and analyze it. The result was the Ivy app to collect the information through a smartwatch, and an app called Clover, which downloads and processes that data. “We had to develop the software and heavily test it – all during COVID,” she explains. “Before we actually started our study, there was a lot of preparation that went into it.”
Dr. Beauchamp credits the support received from AGE-WELL (Canada’s technology and aging network) with getting things moving by providing core research funding. “It was a perfect fit, not just for the funding, but for the opportunity to work with a partner,” she says. “It has been phenomenal. Everyone involved in MacM3 is really excited about it.”
Dr. Beauchamp also acknowledged the McMaster Institute for Research on Aging (MIRA) as co-funder of MacM3.
She adds: “I’m lucky to have found an area of research that I am really passionate about. What I do doesn’t feel like work. It just feels like something I want to do and was meant to do.”
To join the MacM3 study or learn more, visit: https://macm3.com/ n H
Michele Sponagle is an editor, writer and content manager. AGE-WELL is a federally funded Network of Centres of Excellence. The pan-Canadian network brings together researchers, older adults, caregivers, partner organizations and future leaders to accelerate the delivery of technologybased solutions for healthy aging. agewell-nce.ca
“WHILE THERE HAVE BEEN STUDIES LOOKING AT HOW FAST PEOPLE CAN GET IN AND OUT OF A CHAIR AND HOW FAST SOMEONE WALKS, CURRENT MOBILITY RESEARCH DOESN’T ADDRESS HOW MOBILITY IS SOMETHING TO TAKE CHARGE OF AS A CENTRAL STRATEGY FOR MANAGING YOUR HEALTH,”
Keep residents connected to the people and things they love the most. With Managed Wi-Fi, TELUS Business makes it easy to connect residents to their own personal area network. Our property-wide Wi-Fi is secure and reliable, our technology is easy to learn and use, and we offer bilingual 24/7 technical support for residents and employees.

Vincent Terstappen and Shirley Chandler are on a mission to make healthcare knowledge more accessible through the use of plain language. They offer a goldmine of tips and resources for AHS staff, physicians and volunteers as well as oversee MyHealth.Alberta.ca, a trusted source of easy-to-understand information on health conditions, healthy living, medicines, tests and treatments.
Don’t ever doubt the value of plain language when it comes to healthcare.
Consider this bit of medical bafflegab: “Ingest two capsular units of acetylsalicylic acid and implement a vocal communication my way in the ante meridiem.”
If your doctor were to utter such words, you’d tell them to get the marbles out of their mouth, and try again with something simpler like: “Take two aspirins and call me in the morning.”
A passion for clarity and a love of language keep health literacy consultants Shirley Chandler, Vincent Terstappen and Heather Ball on their grammatical toes daily for Alberta

Health Services. They’re the team who oversee content for MyHealth. Alberta.ca, the website Albertans rely upon as a trusted source of easy-to-understand information on health conditions, healthy living, medicines, tests and treatments.
“I love making things understandable and easier for people to read so that they know what’s going on,” says Chandler. “I’m a Registered Nurse and I like finding ways to explain things better. It’s always been a passion of mine.
“I’ve experienced it myself, and I’ve also seen it in others, where you tell them something and they nod and say ‘yes’ or they sit there with this stone look on their face – and you know you haven’t reached them. You know they don’t get what you’re saying.”
With a background in population health and communications, Terstappen says he believes presenting health information in a more understandable way not only preserves, but has the potential to improve the well-being of all Albertans.
“At MyHealth.Alberta.ca, we get lots of content from subject-matter experts across Alberta who work in, what some might call “the nuance”. They’re so smart. They’re so deep in their areas and we get this amazing health information from them.
“Then we take a look at it to say: ‘How can we present this in a more straightforward way that makes sense to someone who’s just pulling this up to read on their smartphone in the middle of their busy day?”
According to the International Plain Language Federation: “A communication is in plain language if its wording, structure, and design are so clear that the intended audience can easily find what they need, understand what they find, and use that information.”
Plain language also advances AHS’ goal of providing Patient & Family Centred Care, which promotes the respect and dignity of the patient, the sharing of information in an affirming and useful way, collaboration, and empowers the patient to participate more in their healthcare journey.
“We want to give people some information they can take away and use,” adds Chandler. “When it comes
to healthcare, you’re not just trying to get a better deal on a car – your life is involved there.”

Keep a personal tone with an active voice to reach more readers, she suggests. Don’t tell people what they shouldn’t do, let them know what they can do, to keep healthy.
• is easy to read
• can be read quickly
• is easy to understand the first time it’s read
• allows the reader to easily find the information they need and use it
• gets rid of jargon
• your audience and the purpose of the content
• how to organize content that best communicates your message
• design
– layout and adequate white space
– typography (font, font size) that is easy to read
Bulleted lists with headings also allow people to skim and absorb information easier.
“By giving lots of subheadings, we’re organizing content in a flow that makes sense, and really supporting people to scan and browse,” says Terstappen, who adds that the ques-
– graphics to present information in an accessible and engaging way
• expression – tone, word choice
• evaluation – editing and user testing
• Aim for a Grade 5 to 8 reading level (use the SMOG test for readability)
• Use “you”, “your child”, and “your family”
• Use simple, common words and contractions
• Keep sentences and paragraphs short
tion-and-answer format is also a triedand-true way to reach the reader.
“We structure a lot of our health content as question-and-answer. For example, the question may be: ‘What should I do if I get this test result?’
The answer will begin: ‘If you get this test result, you should…’ This kind
• Use Arabic numbers (1, 2, 3), try to avoid Roman numerals and don’t spell out numbers unless at the beginning of a sentence
• It’s OK to use medical or complex words, but explain them in plain language
• Words with two syllables or less tend to be plainer than words with three or more syllables
• Avoid jargon
• Write like you’re talking to the reader
• Use inclusive, people-first and gender-neutral language, and a conversational tone
For more information, visit Plain Language Association International.
of language allows the reader to see themselves. When we edit, one of the big changes that we often make is to make sure we’re really speaking directly to the person, like Shirley says, in an active voice.”
Acronyms, jargon, medicalese and colloquialisms are also to be avoided, wherever possible.
“Not everybody was born and raised in the same type of household or culture,” says Chandler. “Diversity and inclusion, gender and culture sensitivity are huge in what we do – and it’s becoming increasingly so.”
As the small but mighty health literacy team reaches out to others who share their passion, interest is growing in their work, and they’re winning over new converts to the joy of simplicity.
“A dream of ours is to develop a community of practice within Alberta Health Services for everybody who’s interested in plain language and health literacy. This dream is becoming a reality in that AHS has started an initiative to bring together various portfolios who support health literacy and who may be working in this area.” n H
HCP is a voluntary group plan designed for your part -time, casual, contract and temporary employees and retirees. HR teams communicate the opportunity to eligible employees and HCP takes care of the rest.
HCP is a voluntary group plan designed for your part -time, casual, contract and temporary employees and retirees. HR teams communicate the opportunity to eligible employees and HCP takes care of the rest.



Your Employees Need Benefits. We provide an option you can offer them, guaranteed, no medical questions asked, designed specifically for hospital staff.
Your Employees Need Benefits. We provide an option you can offer them, guaranteed, no medical questions asked, designed specifically for hospital staff.
No Fee to Participate. We provide all the necessary material to you, all you need to do is hand it out!
No Fee to Participate. We provide all the necessary material to you, all you need to do is hand it out!
Getting Started is Easy. We walk you through the implementation, every step of the way, and we have the flexibility to accommodate unique groups.
Gettting Started is Easy. We walk you through the implementation, every step of the way, and we have the flexibility to accommodate unique groups. To learn m more, contact us today!
To learn more, contact us today!
1.866.768.1477 x2214
1.866.768.1477 x2214
jatkinson@healthcareproviders.ca
jatkinson@healthcareproviders.ca