




1999 2023 ISSUE 95 JANUARY 2023 ISSN 2397-138X HAPPY NEW YEAR HAPPY NEW YEAR HAPPY NEW YEAR


THE JING INSTITUTE – SCHOOL OF MASSAGE AND COMPLEMENTARY MEDICINE 28/29 Bond Street, Brighton BN1 1RD • 01273 628942 • info@jingmassage.com jingmassage.com FREE ZOOM FOR THERAPISTS MANUAL THERAPY FOR LOW BACK PAIN Learn the latest research and cutting edge techniques to help improve client pain and mobility. TUESDAY 31 JANUARY 2023 1-2PM Register online: buff.ly/3V2n7tu






















TECHNICAL SHORT LONG PRACTICAL JANUARY 2023 ISSUE 95 ISSN 2397-138X is published by Centor Publishing Ltd 88 Nelson Road Wimbledon, SW19 1HX, UK https://Co-Kinetic.com HOW TO TARGET NICHE MARKETS FOR SEARCH ENGINE OPTIMISATION 42-44 Instagram www.instagram.com/co_kinetic/ Facebook www.facebook.com/CoKinetic Our Green Credentials Paper:100% FSC Recycled Offset Paper Our paper is now offset through the World Land Trust Naked Mailing No polybag used Plant-Based Ink Used in Printing Process Twitter https://twitter.com/co_kinetic LinkedIn https://www.linkedin.com/company/co-kinetic/ YouTube www.co-kinetic.com/youtube CBP006075 More details https://bit.ly/3dAwGwd Publisher/Founder TOR DAVIES tor@co-kinetic.com Business Support SHEENA MOUNTFORD sheena@co-kinetic.com Technical Editor KATHRYN THOMAS BSC MPhil Art Editor DEBBIE ASHER Sub-Editor ALISON SLEIGH PHD Journal Watch Editor BOB BRAMAH MCSP Subscriptions & Advertising info@co-kinetic.com what’s inside 4- 11 JOURNAL WATCH SOCIAL MEDIA SUCCESS FOR PHYSICAL THERAPISTS 45- 50 20-26 THE HYPERMOBILITY CONUNDRUM CLINIC POSTERS 12- 13 DISCLAIMER While every effort has been made to ensure that all information and data in this magazine is correct and compatible with national standards generally accepted at the time of publication, this magazine and any articles published in it are intended as general guidance and information for use by healthcare professionals only, and should not be relied upon as a basis for planning individual medical care or as a substitute for specialist medical advice in each individual case. To the extent permissible by law, the publisher, editors and contributors to this magazine accept no liability to any person for any loss, injury or damage howsoever incurred
indirectly, of the use by any person of any of the contents of the magazine.
Limited consents to certain features contained in this magazine marked (*) being copied for personal use or information only (including distribution
shown. No other unauthorised reproduction, transmission or storage in any electronic retrieval system is permitted of any material contained in this
liability
arising) in connection with the supply or use of any goods or services purchased as a result of any advertisement appearing in this magazine. 14-19 SHOULD WE BE TAKING 'GROWING PAINS' MORE SERIOUSLY? 27-32 EVIDENCE BASE FOR INSTRUMENT ASSISTED MASSAGE MANUAL THERAPY AND LOW BACK PAIN 33-41
(including by negligence) as a consequence, whether directly or
Copyright subsists in all material in the publication. Centor Publishing
to appropriate patients) provided a full reference to the source is
publication in any form. The publishers give no endorsement for and accept no
(howsoever
EFFECT
Ansari A, Nayab M, Saleem S et al. Journal of Bodywork and Movement Therapies
OF SOFT AND PROLONGED GRAECO-ARABIC MASSAGE IN LOW BACK PAIN - A RANDOMIZED CONTROLLED CLINICAL TRIAL.
2022;29:232–238
Forty-eight patients with clinically and radiologically diagnosed low back pain were randomised into test and control groups (both n=24). The massage group received soft and prolonged massage at the lumbo-sacral region every alternate day for 20min for up to 3 weeks using a herbal lotion with mainly anti-inflammatory properties. The massage consisted of superficial stroking (10min) followed by tapping (5min) and finally pounding (5min). The
Co-Kinetic comment
control group received shortwave diathermy with a frequency of 27.2Mhz given on every alternate day up to 20min for 3 weeks. The result was that a pain scale score was reduced by 42.14% in the massage group and 13.94% in the control group. Scores on the Oswestry low back pain disability questionnaire improved by 37.16% in the massage group and 5.93% in the control group.
You can either accept that the results are influenced by a traditional medicine system similar to Ayurvedic and Traditional Chinese Medicine with its accompanying mysticism or look at this as massage v electrotherapy – and massage won. For the record, Graeco-Arabic medicine is primarily based on the ancient methods taught by Hippocrates (who lived in Greece between 460bc and 370bc) and Galen (who lived in Greece and later in Rome between ad129 and 199) with further contributions by Avicenna (an Arabic scholar who lived in Iran between ad980 and 1037). Treatments include diet, herbal and mineral medicine, massage, manipulation and the application of cold, heat or suction cups.
EFFECTIVENESS OF TREATMENTS FOR ACUTE AND SUBACUTE MECHANICAL NON-SPECIFIC LOW BACK PAIN: A SYSTEMATIC REVIEW WITH NETWORK META-ANALYSIS. Gianola S, Bargeri S, Del Castillo G et al. British Journal of Sports Medicine 2022;56:41–50

The purpose of this study was to assess the effectiveness of interventions for acute and subacute non-specific low back pain (NS-LBP) based on pain and disability outcomes. A search of the usual medical databases for randomised clinical trials (RCTs) involving adults with NS-LBP who experienced pain for less than 6 weeks (acute) or between 6 and 12 weeks (subacute) resulted 46 RCTs (n=8765) being included. The risk of bias was low in 9 trials (19.6%), unclear in 20 (43.5%), and high in 17 (36.9%). At immediate-term follow-up, for pain decrease, the most efficacious treatments against an inert therapy were exercise, heat wrap, opioids, manual therapy and NSAIDs. Mild or moderate adverse events were reported in the opioid (65.7%), NSAID (54.3%) and steroid (46.9%) trial arms.
Co-Kinetic comment Bin the drugs, they have side effects. Here you have evidence that movement and a bit of heat and manual therapy work.
A SURVEY OF CANADIAN MASSAGE THERAPISTS EXPERIENCES


OF WORKRELATED PAIN. Barraclough W, Baskwill A, Higgs C et al. International Journal of Therapeutic Massage & Bodywork 2022;15(3):18–26



This starts with a quote from a study by Statistics Canada which reported that healthcare workers make up 3% of all reported injuries in the country. Another quoted report by the Registered Massage Therapists’ Association of Ontario reported that 51% of practitioners would like to work more hours per week; however, 40.3% of those who wished to work more hours chose not to, owing to the physically demanding nature of the work, and a further 13.4% did not take on more work because they feared physical burnout. The data for the present study came from 42-item questionnaires (n=1103) sent to massage therapists ranging in age from 20 to 73 years, 85% of respondents were female. The majority (85%) had experienced, or were experiencing, work-related pain (WRP) at one or more of five pre-identified, primary locations with the hand/wrist, the most common site (65.5%); followed by the fingers/thumb (60.3%), shoulder (55.0%), lower back (50.1%), and neck (49.2%). Females were significantly more likely to report neck and shoulder pain than males, and were significantly more likely to report WRP at a higher number of body locations, with approximately one in five female MTs reporting WRP at all of the five primary sites. On a 10-point pain-severity scale, females reported significantly higher perceived pain than males. WRP was attributed to the gradual onset of musculoskeletal conditions by 60.3% of respondents, with no other choice of cause being reported by more than 11.1%. Furthermore, 48% reported an impact on activities of daily living, 31% reporting a loss of income, 54.6% working in pain, and 30.5% considering changing (or having changed) their profession.
Various work adjustments to WRP were reported, including altered biomechanics, the use of adjustable massage tables and chairs, and the use of a greater rest period between patients. Respondents believed that some WRP stemmed from what they considered to be ‘bad habits’ developed early in their careers, and that improving techniques reduced WRP. Therapists referred to ‘hiking shoulders’, ‘torquing wrists’, or over-using thumbs/fingers as undesirable.
Co-Kinetic comment
There have been a few similar studies recently. This one has lots of stats and none of them look good for practitioners. It seems that manual therapy is great for the patients but not so great for the therapists; however, the ‘bad habits’ section suggests that some of it is self-induced.
Co-Kinetic Journal 2023;95(January):4-11
4
OPEN
CLICK ON RESEARCH TITLES TO GO TO ABSTRACT = OPEN ACCESS
OPEN OPEN OPEN
Journal Watch
EFFECTIVENESS
OF EXERCISE
This is a clinical commentary on a Cochrane review “Exercise therapy for chronic low back pain” by Hayden et al. [Cochrane Database of Systematic Reviews 2021;9:CD009790 (http://bit.ly/3AsaHCK)].

It starts with a very simple question: “Is exercise an effective treatment for adults with chronic low back pain?” It then gives a very simple answer: “Yes”. There is low- to moderatequality evidence that exercise reduces pain and improves function in patients with chronic low back pain compared with no treatment, usual care, and other conservative interventions such as education, manual therapy, and electrotherapy. This effect is clinically significant in the short term (6–12 weeks) but less pronounced 6 months after treatment completion. The review does not recommend a specific exercise regimen to treat chronic low back pain.
The latter point is addressed by stating that current guidelines from the American College of Physicians and the National Institute for Health and Care
THERAPY IN PATIENTS
WITH CHRONIC LOW BACK PAIN. Lindberg B, Leggit JC. American Family Physician 2022;106(4):380–381

Excellence recommend general exercise with other nonpharmacologic therapies as initial treatment for chronic low back pain. The guidelines quote a recent metaanalysis by Owen et al. published in the British Journal of Sports Medicine (Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2020;54:1279–1287). It compared a specific 4-week exercise programme with varying weekly exercise regimens and found that using Pilates, resistance training, aerobic exercise, and motor control exercises (ie. activation of the deep trunk muscles progressing from simple to complex tasks with an emphasis on functional activities) were overall the most effective exercise treatment modalities for chronic low back pain.
Co-Kinetic comment
This is like playing research pass the parcel. You open one paper hoping for specific help with your long-term low back pain patients and find that you have to open another and then another before you get to something you can use. It may be better to skip the unwrapping and go straight to the Owen et al. paper. You can get it free at [http://bit.ly/3UWRmCC]
CLINICAL RELEVANCE OF MASSAGE THERAPY
AND ABDOMINAL HYPOPRESSIVE GYMNASTICS ON CHRONIC NONSPECIFIC LOW BACK PAIN: A RANDOMIZED CONTROLLED TRIAL. Bellido-Fernández L, Jiménez-Rejano JJ, ChillónMartínez R et al. Disability and Rehabilitation 2022;44(16):4233–4240

Sixty patients aged between 20 and 65 years who had been diagnosed with chronic non-specific low back pain, had mechanical pain for at least 12 weeks, and had no severe complications were randomly divided into one of three groups (each n=20). Each group received 8 interventions of 30min treatment time over a 4-week period.
Group 1 received a massage therapy protocol focused on their spine designed for the soft tissue of the thoracic lumbar and cervical system, the entire fascial system, and the vertebral joints. Group 2 performed a series of six static abdominal hypopressive exercises consisting of postural exercises that decrease the pressure in the abdominal, perineal, and thoracic cavities. These exercises lead to direct activation of the transverse abdominal muscle, which strengthens the abdominal girdle and stabilises the spine. The participants repeated each exercise three times in addition to a previous phase of learning and a minimum rest period. Group 3 received four interventions of massage therapy and another four interventions of abdominal hypopressive gymnastics in alternating sessions.
Outcomes were an Oswestry disability index score, pain intensity using the Numerical rating scale, an SF12 Quality of life questionnaire and lumbar mobility using a Schober’s test. The results showed that both the massage and exercise groups had reduced pain levels, increased mobility of the lumbar spine, and improved disability and quality of life scores in the short term. The combined group had an even better quality of life score.
Co-Kinetic comment
The great Dr James Cyriax, aka the father of orthopaedic medicine, said that all pain has a source and that unless you find the source and treat it directly you will not solve the problem. Non-specific back pain is therefore an anathema to the good doctor’s many followers. It is a lazy diagnosis. On the plus side, the interventions had a positive effect. The authors also deserve credit for saying, “the massage considered the ergonomics of the physiotherapist”.
5 Co-Kinetic.com RESEARCH INTO PRACTICE
An experimental group (n=45) received dry cupping therapy, with cups bilaterally positioned parallel to the L1 to L5 vertebrae. The control group (n=45) received sham cupping therapy. The interventions were applied once a week for 8 weeks. Participants were assessed before the first treatment session, then at the mid-point and the end. The sham was that the cups were prepared with small holes <2mm in diameter to release the negative pressure in approximately 3s. On a 0-to-

DRY CUPPING THERAPY IS NOT SUPERIOR TO SHAM CUPPING TO IMPROVE CLINICAL OUTCOMES IN PEOPLE WITH NON-SPECIFIC CHRONIC LOW BACK PAIN: A RANDOMISED TRIAL. Almeida Silva HJ, Barbosa GM, Scattone Silva R et al. Journal of Physiotherapy 2021;67(2):132–139
10 scale, the between-group difference in pain severity at rest was negligible at all of the measurement points. Similar negligible effects were observed on pain severity during fast walking or trunk flexion. Negligible effects were also found on physical function, functional mobility and perceived overall effect. No
Co-Kinetic comment
We didn’t report this when it came out but we have included it now because it acts as a counterpoint to the Traditional Chinese Medicine paper. It’s a bit embarrassing for cupping fans.
THE
Fifty-four subjects with low back pain and decreased length in at least one hamstring were randomised to receive either dry needling (DN) or sham dry needling to the T12 and L1 multifidi. Participants underwent regional (fingertip-to-floor) and remote flexibility (passive knee extension, passive straight leg raise) and pressure pain threshold (PPT) testing of the upper and lower extremity before, immediately after and 1 day after treatment. The DN consisted of needles placed using an inferomedial approach approximately
1cm lateral to the spinous process and guided through the muscle to the lamina. Needles were manipulated in a ‘pistoning’ fashion. For the sham, real needles had their sharp end cut off and smoothed. They were kept in the holders and tapped to stimulate the ‘pistoning’.
The results showed that statistically larger improvements in regional flexibility, but not remote flexibility, were observed immediately post-treatment in those who received DN compared to those receiving sham; however, the
EXERCISE AS EFFECTIVE AS SURGERY
IN
IMPROVING
worthwhile benefits could be confirmed for any of the remaining secondary outcomes. OPEN
EFFECTS OF DRY NEEDLING TO THE THORACOLUMBAR JUNCTION MULTIFIDI ON MEASURES OF REGIONAL AND REMOTE FLEXIBILITY AND PAIN SENSITIVITY: A RANDOMIZED CONTROLLED TRIAL. Clark NG, Hill CJ, Koppenhaver SL et al. Musculoskeletal Science and Practice 2021;53:102366



effect did not carry through to the plus 1 day test. Differences between upper and lower extremity PPT were not significant.
Co-Kinetic comment
This is another paper we did not report when it was first published but it also serves as a counterpoint to the Traditional Chinese Medicine paper. This time the sham is not quite as successful in that there is a short-term effect on flexibility but it doesn’t last. This is not the place for an argument about the difference between acupuncture and DN.

QUALITY
OF LIFE, DISABILITY, AND
PAIN
FOR
LARGE
TO MASSIVE ROTATOR CUFF TEARS: A SYSTEMATIC REVIEW & METAANALYSIS. Fahy K, Galvin R, Lewis J et al. Musculoskeletal Science and Practice 2022;61:102597
OPEN
A search was made of the usual medical databases looking for studies about exercise intervention for adults with large-to-massive rotator cuff tendon tears, which are defined as >5cm and involving two or more tendons. Five trials (n=297 participants; average age, 66.7 years; 55% male) were included in the analysis. Three trials compared exercise to another non-surgical intervention and two trials compared exercise to surgery.

At 12 months a significant improvement in pain was found for the surgical group and a significant improvement in shoulder external rotation ROM favoured the exercise group.
Co-Kinetic comment
There are other measures in this study but, based on the available evidence, exercise is as effective as surgery. A caveat is that the authors complain of very low standards of quality of the evidence, and so in reality the jury is still out. We should probably also stress that the success of most surgical procedures, anywhere in the body, depends on the quality of post-surgery rehab so it’s worth trying the exercise approach first.
EFFECTS OF CRYOTHERAPY AFTER SOFT TISSUE INJURY: A SYSTEMATIC REVIEW.

Mohd Radzi AAA, Mohamad MY. International Journal of Allied Health Sciences 2022;6(2):2625–2631
OPEN
This study aimed to review the effects of cryotherapy on pain reduction and time taken to return to normal activity after soft tissue injury. The Science Direct, PubMed, and Cochrane library were searched. Only 3 articles out of 178 articles fulfilled the inclusion criteria and were included in the systematic review. Significant difference can be seen in terms of pain measured in VAS score when cryotherapy is applied either alone or together with manual therapy. A total of 161 patients who received cryotherapy out of 179 patients from 3 articles reported an average reduction of 2.3 VAS points from their initial score. However, there were no studies that specifically included time taken to return to normal activity as an outcome measure.
Co-Kinetic comment
Cool! [Groan – Ed]
Co-Kinetic Journal 2023;95(January):4-11
6
OPEN
A sports-related concussion (SRC) is most commonly sustained in contact sports. An exercise-induced elevation of core body temperature is associated with increased brain temperature that may accelerate secondary injury processes following SRC, and exacerbate the brain injury. In a recent pilot study, reported here, acute head/ neck cooling of 29 concussed ice hockey players resulted in shorter time to return-to-play. For this study, the clinical trial was extended to include players of 19 male elite Swedish ice hockey teams over five seasons (2016–2021). In the intervention teams, acute head/neck cooling was implemented using a head cap for ≥45min in addition to the standard SRC management used in controls. The primary endpoint was
SHORTER RECOVERY TIME IN CONCUSSED ELITE ICE HOCKEY PLAYERS BY EARLY HEAD-AND-NECK COOLING: A CLINICAL TRIAL. Al-Husseini A, Bakhsheshi MF, Gard A et al. Journal of Neurotrauma 2022;doi:10.1089/neu.2022.0248

time from SRC until return-to-play (RTP). Sixty-one SRCs were included in the intervention group and 71 SRCs in the control group. The median time to RTP was 9 days in the intervention group and 13 days in the control group. The proportion of players out from play for more than the expected recovery time of 14 days was 24.7% in the intervention group, and 43.7% in controls.
Co-Kinetic comment
The authors state a couple of limitations on this study including not having a sham cap for the placebo effect, not knowing for certain that the extent
MANUAL MYOFASCIAL RELEASE AND MUSCLE ENERGY ENHANCES TRUNK FLEXIBILITY AND STRENGTH IN RECREATIONALLY RESISTANCE-TRAINED
WOMEN: CROSS-OVER STUDY. Cunha JCdOM, Monteiro ER, Behm DG et al. Journal of Bodywork and Movement Therapies 2022;doi:https://doi.org/10.1016/j. jbmt.2022.09.011

The purpose of this study was to compare the effects of myofascial release (MFR) and muscle energy technique (MET) on acute outcomes in trunk extensors for active ROM and strength. Seventeen apparently healthy women performed three experimental protocols using a cross-over, randomised counterbalanced format, and within-subjects design. The protocols were: l ROM and strength test after MFR; l flexibility and strength test after MET; and l ROM and strength test without MFR or MET to act as a control.
Active trunk ROM was measured via a sit-and-reach test and trunk extension strength via isometric dorsal dynamometer. A significant increase in ROM was found after MFR and MET, and for strength after MFR compared to baseline values.
Co-Kinetic comment
Both are worth doing. The comment about the subjects being ‘apparently’ healthy is worrying in a medical journal. Couldn’t the authors tell?
of the injuries was similar, and not having blind assessors but maybe it is time we re-thought all the randomised control business because – let’s be honest – many of the studies on interventions using ‘healthy’ athletes tell us little or nothing about how real injured ones will react. This does, so the authors shouldn’t be beating themselves up.
THE EFFECTIVENESS OF FITNESS MASSAGE AFTER PHYSICAL ACTIVITY AND SPORT MASSAGE OF LOWER EXTREMITIES IN IMPROVING RANGE OF MOTION AND JOINT FUNCTION SCALE OF FUTSAL ATHLETES. Graha AS, Ambardini RL. In: Proceedings of the Conference on Interdisciplinary Approach in Sports in conjunction with the 4th Yogyakarta International Seminar on Health, Physical Education, and Sport Science (COIS-YISHPESS 2021). Atlantis Press 2022
As the lengthy title states, this is a report from a conference which discusses the difference between sport massage (SM) and fitness massage after physical activity (FMPA) and the effectiveness of both in improving ROM. It used pre-experimental design of two-group pretest and posttest. Treatment was given three times, which were at 2min, 15min and 30min after the game. Forty samples were drawn from the population of 80 students majoring in sport science of the Faculty of Sport

Co-Kinetic comment
Science of Yogyakarta State University using purposive sampling. The ROM was measured with a goniometer and lower extremity functional scale (LEFS) as instruments. Both treatments improved the ROM and the joint function scale of the lower extremities, and the effectiveness of the SM was 0.60 (60%) and that of the FMPA was 0.63 (63%). The effectiveness of the SM in improving the joint function sale of the lower extremities was (73%), and that of the FMPA was (80%).
Sadly the massage protocols were not described which, given that the objective was to compare one to the other, makes it a bit of a waste of time. However, on the plus side, for those of you involved in futsal (according to both FIFA and UEFA it is the fastest growing indoor sport in the world with 115 nations participating) some interesting injury stats are quoted. The WHO states an injury rate of 235 cases per 1000 games. A five-season retrospective study of the aetiology of injuries in the Spanish national futsal male team showed that the majority of the extrinsic injuries resulting from external trauma took place during official training. The thigh was the most injured site (43.3%); followed by the remaining parts of leg (12.6%), knee (10%), back (9.7%), ankle (6.15%), and foot (5.8%). More than 50% of the injuries were diagnosed as resulting from muscle overload and in the most cases (96.6%) the diagnosis was made after clinical assessment. This does raise the question of how were the other 3.6% diagnosed?

7 Co-Kinetic.com RESEARCH INTO PRACTICE
OPEN
OPEN
EVALUATION
OF THE

EFFECTS
ON POSTURAL STABILITY IN ACTIVE YOUNG WOMEN. Güler Ö, Bingöl AD, Neşe Şahin F et al. International Journal of Applied Exercise Physiology 2020;9(10):44–49
MENSTRUAL CYCLE
OF
The menstrual cycle can be divided into three different phases: the follicular phase (days 1 to ~13, which includes the early menstrual phase), ovulation (~day 14) and the luteal phase (~days 15–28). Postural stability is defined as being able to hold the body centre of gravity within the centre of support to prevent falls and complete desired movements and it is speculated that this together with the systemic hormonal changes that affect tissues such as ligaments, tendons and muscles contribute to an increased injury risk. Hence, the purpose of this study was to evaluate the stability of physically active women during different phases of the menstrual cycle. The phases were estimated from the first day of menstruation with tests on the 2nd or 3rd day (menstrual phase), 14th day (ovulation) and 21st day (mid-luteal phase) of the cycle.
For a limit of stability (LOS) test performed with the Biodex SD System (Biodex, Shirley, NY), a statistical difference was found between the three phases. LOS values decreased in the ovulation phase compared to other phases. No difference was determined between anterior-posterior oscillation, mediolateral oscillation, and postural stability index scores and menstrual phases.
Co-Kinetic comment
If, as these results suggest, menstrual cycle affects balance this is bound to have an impact on injury risk in sports. The big question is therefore what can be done about it? The authors suggest exercises to improve balance performance. There is a PhD out there for someone wishing to find out if it makes a difference.
This study was aimed at looking for risk factors such as characteristics of the participant, environment, structures, and experiences that demonstrate a significant predisposition to burnout. The World Health Organization defines burnout not as a medical diagnosis but as an occupational phenomenon and a ‘syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed’. The most widely used measure of burnout, the Maslach Burnout Inventory, assesses burnout in three constructs: emotional exhaustion, depersonalisation, and personal accomplishment.
The usual medical databases revealed 46 studies (8717 participants). The risk of bias assessment
MENSTRUAL CYCLE AND SPORTING PERFORMANCE PERCEPTIONS OF ELITE VOLLEYBALL PLAYERS.
Ergin E, Kartal A. International Journal of Applied Exercise Physiology 2020;9(10):57–64
This study aimed to investigate menstrual cycle and sporting performance perceptions of elite volleyball players. The subjects were 130 volleyball players who play in the Turkish Leagues, 45% of whom were internationals. They completed a questionnaire consisting of 25 questions about general and sporting performance before, during and after the menstrual cycle. The results showed that 61.5% of the participants described their general menstruation states as regular and 84.6% of them stated that they had menstrual problems due to sports. In addition, 58.5% of the volleyball players feel bad before menstruation, whereas 52.3% feel good during menstruation. The menstrual periods of 46.2% of the participants sometimes affect their sports/training participation and 99.2% participate in competitions during this period. They listed their problems as irritability (36.2 %) and anger (47.7%); 45.4% think that menstruation sometimes affects their sporting performance, whereas 35.4% consider it does not.
Co-Kinetic comment
This is a great partner study for the one we have reported on balance during menstruation. For those of you involved in women’s sport there is lots of information on training load and the effects on daily activity (not just sport), not the least of which is that nearly 70% of the participants often or occasionally take medication during menstruation which in itself may affect performance.


determined all were of fair or poor quality. Fifty-three risk factors were identified, with 4 being classified as unavoidable and 49 determined as avoidable. The avoidable risk factors were further categorised as: structural/ organisational (32%), psychological/ emotional (19%), environmental (19%), or sociodemographic (13%).
The unavoidable risk factors were: years of professional experience, gender, age, and fewer years of employment. The avoidable ones are too many to list here but some of the major ones are lack of management and supervisor support; boredom or lack of challenge; inadequate staff or
material resources; and poor communication.
Co-Kinetic comment
A number of previous studies consistently suggest that work as a physical therapist is associated with burnout. Everyone in our industry should be aware of the risk factors and note that the vast majority of them are avoidable. Note also that the majority are in the control of management. The paper is published in the journal Physiotherapy so all our Chartered Society of Physiotherapy readers can access it and the rest may be able to get it via Science Direct. Share it with your colleagues. Those of you in management positions should have risk factors framed, put on your desk and you should address them every day.
Co-Kinetic Journal 2023;95(January):4-11

8
OPEN OPEN
RISK FACTORS ASSOCIATED WITH PHYSICAL THERAPIST BURNOUT: A SYSTEMATIC REVIEW. Burri SD, Smyrk KM, Melegy MS et al. Physiotherapy 2022;116:9–24
OPEN
OPEN
MEDICAL SERVICES FOR SPORTS INJURIES AND ILLNESSES IN THE BEIJING 2022 OLYMPIC WINTER GAMES. Han PD, Gao D, Liu J et al. World Journal of Emergency Medicine 2022;13(6):459–466


The daily number of injuries and illnesses among athletes reported by Beijing 2022 medical staff in the polyclinic, medical venues and ambulance were recorded. Incidence was calculated as the number of injuries or illnesses occurring during competition or training, respectively, with incidence presented as injuries/ illnesses per 100 athlete-days. In total, 2897 athletes from 91 nations experienced injury or illness. Medical staff reported 326 injuries and 80 illnesses, equalling 11.3 injuries and 2.8 illnesses per 100 athletes over the 17-day period. Altogether, 11% of the athletes incurred at least one injury and nearly 3% incurred at least one illness.
The number of injured athletes was highest in the skating sports (n=104), followed by alpine skiing (n=53), ice track (n=37), freestyle skiing (n=36), and ice hockey (n=35), and was the lowest in the Nordic skiing disciplines (n=20). Of the 326 injuries, 14 (4.3%) led to an estimated absence from training or competition of more than 1 week. A total of 52 injured athletes were transferred to hospitals for further care. The number of athletes with illness (n=80) was the highest for skating (n=33) and Nordic skiing (n=22). A total of 50 illnesses (62.5%) were admitted to the department of dentistry/ ophthalmology/otolaryngology, and the most common cause of illness was

‘other causes’, including pre-existing illness and medicine (n=52, 65%). These findings were similar to the findings during the Olympic Winter Games in 2014 and 2018 despite 2022 still being in the pandemic period.
Co-Kinetic comment Summary papers like this are published after every games. The shear numbers of cases dealt with in a short time is always impressive. If you want to be at the heart of the organisation of the greatest sporting event on the planet and directly contributing to its success, the volunteer portal for Les Jeux Olympiques et Paralympiques de Paris 2024 opens in March 2023 but you can register interest now and receive a newsletter via http://bit.ly/3GIMOf2. They need 45000 people to make it work. It could be you.
Bonne chance.
ICE MASSAGE ON THE CALF IMPROVES 4-KM RUNNING TIME TRIAL PERFORMANCE IN A NORMOTHERMIC ENVIRONMENT. Franco-Alvarenga PE, Cechetti MDS, Barcelos D et al. Research Quarterly for Exercise and Sport 2022:1–7
After familiarisations, 14 recreationally endurance-trained men (age, 21.3±1.2 years; body weight, 67.5±9.2kg; height, 173.0±5.0cm) underwent two 4km time trials on a 400m track in normothermic conditions with or without ice massage before the trial. The time of running, ratings
of perceived exertion (RPE), and pain perception were recorded every 400m throughout the trials. The local cooling with ice massage increased the mean speed (~5.2%) and decreased the time to complete the 4km (~5.5%). Accordingly, ice massage also reduced the exercise-derived pain perception,
although no effect has been found in the RPE during the trials.
Co-Kinetic comment
Just when we are moving away from the use of ice in acute injury management (POLICE to PEACE AND LOVE), it pops up as a pre-match technique. It just won’t be frozen out, will it?
EFFECTS
OF
ACUPUNCTURE, MOXIBUSTION, CUPPING, AND

MASSAGE ON SPORTS INJURIES: A NARRATIVE REVIEW. Zhang H, Zhao M, Wu Z et al. Evidence-Based Complementary and Alternative Medicine 2022;2022:9467002
This is a review of the evidence of four techniques used in Traditional Chinese Medicine.
The results of the World Health Organization’s latest global traditional medicine survey show that acupuncture therapy is recognised by 113 countries worldwide, ranking it first in traditional medical treatment methods. This review includes a table of 14 studies that show that it works for sprains, strains and assorted pains. In summary, it alleviates fatigue, relieves pain, promotes recovery of tissue function, reduces the use of drugs, and has almost no side effects, and so is a viable therapy option for patients and athletes.
Moxibustion is a traditional Chinese method that uses heat generated by burning moxa (mugwort) to stimulate acupoints. Put aside all the stuff about

qi, meridians and balancing yin and yang and it is basically a heat source. Consider it to be the same as infrared or continuous ultrasound. Less scientific support is given for this than for acupuncture with only five studies in the accompanying table. They include it as a treatment for osteoarthritis pain and ligament injury.
Five studies are also cited in support of Chinese massage (tui na), which is a combination of massage, acupressure and other forms of body manipulation. Cited studies are for knee arthritis and plantar heel pain.
Cupping, like the previous techniques is often applied above acupressure points. It has become popular since the Olympic swimmer Michael Phelps appeared at the 2016 games (his fifth) with the tell-tale marks
along his back. The fact that he won four golds to add to his total of 28 Olympic medals helped. For the record that was 23 gold, 3 silver and 2 bronze (even superheroes can have an off day). The table for cupping comprises four studies for low back pain and one for heel pain.
Co-Kinetic comment
OPEN
In the world of evidence-based medicine there is plenty of it here to be quoted to justify the intervention. Whether or not any of it is any good is a different question and you would have to go to the individual papers to make that call; however, let’s not forget that the best evidence is an athlete returning to sports. Does it really matter how they get there as long as they do? As an aside, how annoying is it that when you put a word such as ‘tui na’ into a search engine the first thing that comes up is ‘Buy Tunnia at Low prices’. Stop it please!
9 Co-Kinetic.com
OPEN
EVALUATION OF THE QUALITY OF INFORMATION AVAILABLE ON THE INTERNET REGARDING CHRONIC ANKLE INSTABILITY. Yoon SJ, Kim JB, Jung KJ et al. Medicina 2022;58(10):131

A study quoted in this paper found that almost 90% of patients in Korea search the Internet to obtain information regarding their disease and its treatment. Furthermore, patients who obtain accurate medical information through the Internet tend to enter into good patient–physician relationships, which leads to better treatment outcomes. Therefore, qualitative analyses of the quality of such websites is necessary to ensure that they provide accurate medical information to patients.
The key term ‘chronic ankle instability’ was searched on the three most commonly used search engines in Korea. The top 150 website results were classified into university hospital, private hospital, commercial, non-commercial, and unspecified websites by a single investigator. The websites were rated according to the quality of information using the DISCERN instrument, accuracy score, and exhaustivity score. DISCERN is a brief questionnaire which provides users with a valid and reliable way of assessing the quality of written information on treatment choices for a health problem. The
SURVEY OF PELVIC AND KNEE JOINTS PROPRIOCEPTION AND TYPES OF BALANCE IN ATHLETES AND NON-ATHLETES

FOLLOWING THE FATIGUE PROTOCOL. Moghaddam AM, Ebrahimi Y, Baloochi R et al. Journal of Research in Exercise Rehabilitation 2022;doi:10.22084/ RSR.2021.24483.1583

This study looks at the relationship between core muscle fatigue and joint proprioception with a consideration that this may affect injury incidence.

Thirty men (15 athletes and 15 non-athletes) as a pretest, preformed pelvic and knee proprioception and balance (static and dynamic) tests. In the second session, individuals participated in core muscle fatigue protocol and immediately underwent proprioception and balance tests in fatigue conditions. The findings showed that there was a significant difference between the effect of core muscle fatigue in pelvic proprioception at an angle of 30°, knee proprioception at an angle of 60°, and dynamic balance among athletes and non-athletes. This difference was not significant in static balance.
Co-Kinetic comment
We have not heard much about the importance of ‘the core’ for a while. Is it making a comeback? The suggestion here is that fatigue = changes in the proprioception mechanism = greater injury risk. Another exercise (or set of them) for coaches to embed into their sessions?
results showed that of the 150 websites, 96 were included in the analysis. University and private hospital websites had significantly higher DISCERN, accuracy, and exhaustivity scores compared to the other websites.
Co-Kinetic comment
The Internet is the greatest invention made by man. Discuss. On the one hand, all the information in the world is at your fingertips. On the other, it is full of utter rubbish and the waste tip is bottomless so it’s not surprising that a tool to sort out the wheat from the chaff is useful. The importance of this paper therefore is not that good information on chronic ankle instability has been found but that it brings the tool to your attention. You can download a copy of DISCERN at http://www.discern.org.uk/index.php
SPORT-SPECIFIC REHABILITATION, BUT NOT PRP INJECTIONS, MIGHT REDUCE THE RE-INJURY RATE OF MUSCLE INJURIES IN PROFESSIONAL SOCCER PLAYERS: A RETROSPECTIVE COHORT STUDY. Bezuglov E, Khaitin V, Shoshorina M et al. Journal of Functional Morphology and Kinesiology 2022;7(4):72
Muscle injuries in professional soccer players (n=79; height, 182.1±5.9cm; weight, 76.8±5.8kg; BMI, 23.1±1.4kg/ m2) from three elite soccer clubs from the Russian Premier League were recorded during the 2018–2019 season. The injuries were graded based on MRI, using the British Athletics muscle injury classification. Treatment protocols included the POLICE regimen, short courses of NSAID administration, and a specific rehabilitation programme. The sample group of players (n=34) were given platelet-rich plasma (PRP) injections. The average treatment duration with PRP injection was significantly longer than conventional

Co-Kinetic comment
treatment without PRP, 21.5±15.7 days and 15.3±11.1 days, respectively. Soccer-specific rehabilitation and obtaining MRI/US before the treatment was associated with significantly reduced injury recurrence rate. There was no significant difference between the PRP injection protocol applied to any muscle and the treatment duration in respect of grade 2A–2B muscle injuries. The total duration of treatment of type 2A–2B injuries was 15 days among all players. In the group receiving local injections of PRP, the total duration of treatment was 18 days; in the group without PRP injections, the treatment duration was 14 days.
The word ‘might’ is in the title and there are a few mights and maybes in any conclusions drawn from this because it is not clear what criteria were used to choose the players that received the PRP and there were three different protocols for its injection but there is plenty of food for thought. It’s all in the rehab!
10
Co-Kinetic Journal 2023;95(January):4-11
OPEN OPEN
DETERMINE
DORSIFLEXION RANGE OF MOTION, FUNCTIONAL STATUS AND NAVICULAR POSITION IN PATIENTS WITH PLANTAR FASCIITIS. Chouhan D, Joshi S, Kaushik V et al. Indian Journal of Physiotherapy and Occupational Therapy 2022;16(4):7–13
Forty subjects with plantar fasciitis (aged 25–60) were randomly divided into an experimental group receiving tibialis posterior strengthening along with conventional therapy and a control group receiving only conventional therapy. All reported pain in their first few steps in the morning, a numerical pain rating scale of 5 to 10, plantar heel pain for more than 3 months, pain on palpation along the proximal plantar fascia, a positive Windlass test, reduced dorsiflexion of ankle joint, and a navicular drop >1cm.
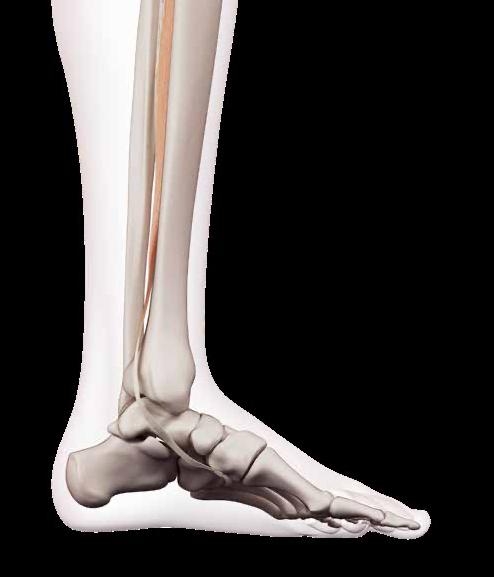
Patients in both groups received iontophoresis with 0.4% dexamethasone drug for 10min, 3 sessions per week for 4 weeks, stretching of calf and plantar surface, self-release of the plantar fascia with tennis ball, intrinsic foot muscle strengthening exercises (heel raises and toe curls). In addition, the treatment group strengthened their tibialis posterior muscle via ankle inversion using elastic bands and emphasising eccentric control, side-lying ankle inversion using ankle weight, emphasising eccentric phase control and single-leg stance balance activities with neutral foot positions twice a day for 4 weeks. Both groups improved but the tibialis strengthening group had the better result.

Co-Kinetic comment
They threw the kitchen sink at this. The authors state that improving overpronation decreased the risk of planter fasciitis. Given that the tibialis posterior is the primary stabiliser of the medial longitudinal arch working it twice a day for 4 weeks is bound to have an effect.
PHYSICAL THERAPY INTERVENTIONS FOR THE MANAGEMENT OF BICEPS TENDINOPATHY: AN INTERNATIONAL DELPHI STUDY. McDevitt AW, Cleland JA, Addison S et al. International Journal of Sports Physical Therapy 2022;17(4):677–694



The purpose of this study was to establish consensus on conservative, non-surgical physical therapy interventions for individuals with long head of biceps tendinopathy using the Delphi method approach.
Twenty-nine experts on shoulder pain were systematically identified as clinicians and/or researchers who had international and nationally recognised training and experience in the physical therapy (PT) management of shoulder pathology or experience in research related to specific PT interventions used to treat individuals with shoulder pain and/or pathology. Once recruited, they rated their agreement with a list of proposed treatment interventions and suggested additional interventions. Agreement was measured using a four-point Likert scale. Descriptive statistics including median and percentage agreement were used to measure agreement. Consensus was defined as an a priori cut-off of ≥75% agreement.
At the conclusion of the study, 61 interventions were designated as recommended based on consensus among experts and 9 interventions were not recommended based on the same criteria; 15 interventions did not achieve consensus. The themes of the interventions revolved around tendon loading techniques, progressive resistance exercises, open and closed kinetic chain exercises and task-specific functional activities (such as reaching, lifting and overhead activity), and occupation and sport-specific activities. In addition there was consensus on stretching/flexibility exercises, non-thrust manipulation and patient education.
Co-Kinetic comment
Not much of a consensus with 61 interventions.
CAN AMERICAN ORTHOPAEDIC FOOT AND ANKLE SOCIETY (AOFAS) SCORE PREVENT UNNECESSARY MRI IN ISOLATED ANKLE LIGAMENT INJURIES? Kandemir V, Akar MS, Yiğit Ş et al. Journal of Orthopaedic Surgery 2022;30(3):10225536221131374
The aim of this study was to validate an algorithm to be used to eliminate unnecessary MRI scans. The American Orthopaedic Foot and Ankle Society (AOFAS) scale was originally published in 1994 in Foot and Ankle International. It incorporates both subjective and objective information. Patients report their pain, and therapists assess function and alignment. Scores rank ankle trauma from 0 to 100, with healthy ankles receiving 100 points. The score may be used to assess the ankle, subtalar, talonavicular and calcaneocuboid joint levels and may be useful for fractures, arthroplasty, arthrodesis and instability procedures.
For this study, ankle MRI images of 328 patients who had reported ankle trauma followed by persistent problems were taken and compared to their AOFAS scores. As determined by MRI, 21.3% (n=70) of patients had ligament damage and 78.7% (n=258) of patients had no ligament damage. There was a statistically significant difference in terms of AOFAS between the group with ligament damage and the group without ligament damage. Following a receiver operating characteristic (ROC) analysis, the AOFAS threshold value for MRI request was determined as 80.5 (84.3% sensitivity and 72.3% specificity). Based on the determined threshold value, 73 patients who had unnecessary MRI would have been eliminated, thus reducing the number of MRIs by 42.6%.
Co-Kinetic comment
THE USE OF INSTRUMENT-ASSISTED SOFTTISSUE MOBILIZATION FOR MANUAL MEDICINE: AIDING HAND HEALTH IN CLINICAL PRACTICE. Pianese L, Bordoni B. Cureus 2022;14(8):e28623

This informative essay looks at the use of instrumentassisted soft tissue mobilisation (IASTM) tools from the prospective of protection of the clinician’s hands. It points out that such tools were used by the ancient Greeks, Romans and Chinese. They offer a mechanical advantage minimising the forces going through a therapist, especially at the thumbs.
Co-Kinetic comment
In many ways this is a companion piece to the Canadian Massage Association survey and quotes similar stats from an Australian study. To hammer home the message of using tools to prevent hand damage it includes a gory picture of surgery to a trapezius-metacarpal joint. All fair enough, but the Greeks, Romans and Chinese who originated instrument use

Co-Kinetic.com RESEARCH INTO PRACTICE
TO
THE EFFECTIVENESS OF TIBIALIS POSTERIOR STRENGTHENING ALONG WITH CONVENTIONAL THERAPY ON ANKLE
You can get a free
OPEN OPEN OPEN OPEN
download of the AOFAS from http://bit.ly/3hZvJmy
FACTS
Low back pain is the leading cause of disability worldwide. Treatments can often be costly, time-consuming and may not work. Unhelpful or misleading beliefs about your back pain can cause greater levels of pain, disability and have a damaging impact on your quality of life.
FICTION Here are the 10 most common unhelpful beliefs about low back pain:
It’s always a serious medical condition Gets worse in later life













Pain means tissue damage
Scans and investigations always needed
If it hurts when moving, it’s a signal to stop

It is caused by poor posture
Once any serious pathology has been ruled out, scientifc evidence has shown that understanding these helpful facts below, can bring about a positive mindset change to help you cope better with your back pain:
Scan the QR code to order A1-A3 sized posters

Results from scans or imaging don’t determine your prognosis and won’t improve the outcome of your current back pain Graduated exercise and movement in all directions are safe and healthy for your spine

Your posture and the alignment of your spine while standing, sitting or lifting does not predict low back pain or how long it lasts
For more details talk to your local healthcare professional.
A weak core does not cause low back pain. Although it is good to have strong trunk muscles, it is also helpful to relax them when they aren’t needed Spine movement and loading are safe and build structural resilience when done progressively Painful fare-ups are often related to changes in activity, stress and mood rather than tissue damage
Effective care for low back pain can be relatively cheap and safe and includes education, and optimising physical and mental strength.
Lovingly
planning individual
©Co-Kinetic 2023
produced by The information contained in this poster is intended as general guidance and information only and should not be relied upon as a basis for
medical care or as a substitute for specialist medical advice in each individual case.

























Lovingly produced by ASK US FOR OUR BACK PAIN RESOURCES The information contained in this poster is intended as general guidance and information only and should not be relied upon as a basis for planning individual medical care or as a substitute for specialist medical advice in each individual case. ©Co-Kinetic 2023 General Back Pain Resources 10 Facts About Back Pain Acute Back Pain Chronic Low Back Pain Sciatica Understanding Chronic Pain Back Pain in Women Back Pain Triggers and Causes Could My Back Pain Be….? Massage for Low Back Pain Self-Treatment for Back Pain Who Should I See for My Back Pain? Yoga Stretches for Back Pain Back Pain and Sleep Resources Back Pain and Sleep Newsletter 8 Bed Time Stretches Morning Stretch Routine for Back Pain Sleeping Positions for Back Pain Back Pain and Golf Resources Golfer’s Back Newsletter Golf Injury Cheat Sheet 5 Strategies for Sidestepping a Golfing Injury Golfer’s Back Exercise Handout ASK US FOR MORE DETAILS Back Pain Exercise Handouts We also have a wide range of exercise handouts for all types of back pain. 1 2 3 4 5 6 7 8 9 10 11 Morning Stretch Routine for Back Pain HIP FLEXOR STRETCH REACH LEGS TWO ARMS Repeat each exercise 3-5 times holding each one for 5-10 seconds l If an exercise causes pain, stop and move onto the next exercise Perform single leg exercises on both legs f BackPain Sleeping Positi Side Lying Y r Fr t SleepingPositiFlatOnBack Ge ingInand OutofBed Back Pain and Pregnancy Resources Pregnancy and Back Pain Newsletter 7 Tips to Relieve Pregnancy Back Pain Pregnancy Back Stretches Pregnancy Back Pain Exercises Back Care with Baby Scan the QR code to order A1-A3 sized posters
‘Growing Pains’
Osgood–Schlatter disease (OSD) is a condition of knee pain in 1 in 10 adolescents. Recent research has shown that it has a greater impact and that its effects can be longer lasting than was previously thought. However, little research has been done on how best to manage it. This article summarises the available evidence and the current thinking about the management of OSD so that you can most effectively help your patients through this condition.
Osgood–Schlatter, also known as Osgood–Schlatter ‘disease’ (OSD), is one of the most common knee-pain conditions in adolescents. It is reported to affect 1 in 10 of the general population; more often in boys between the ages of 12 and 15 years, and also in girls between the ages of 8 and 12 years. Although OSD is more common in boys, as more girls are becoming involved in sports the gender gap is narrowing (1*). OSD prevalence is highest in active adolescents, with early sport specialisation associated with a fourfold greater relative risk of developing OSD (2*). OSD results in knee pain, often severe enough to cause limping. It may be accompanied by swelling or deformity, and frequently results in long-term symptoms with functional impairment. Pain is exacerbated on descending stairs, after prolonged periods of sitting with the knee immobile, while kneeling, and during sports activities. Pain is aggravated by activities that load the quadriceps muscle (and indirectly the tendon attachment), for example, jumping, landing, and running (1*). Although the aetiology is not fully understood, OSD is considered to be an apophyseal
By Kathryn Thomas BSc MPhil
injury of the tibial tuberosity at the site of the patellar tendon attachment. Before maturity of the apophysis, the apophyseal cartilage is thought to be weak and thus susceptible to injury. Apart from pain, characteristics of OSD include cartilage swelling and tendon changes involving thickening of the patellar tendon and increased Doppler activity (3,4*,5*). In football, the statically dominant leg has been shown to be more prone to develop OSD. In other sports (including track and field, basketball, martial arts and handball), however, either leg could be affected by OSD. Age at onset, growth rate, BMI and muscle imbalance is not significantly predisposing. Interestingly previous heel pain (Sever’s disease) is strongly associated with the presence of OSD. It is not clear why or what the pathophysiological connection is apart from possibly exposure to similar levels of physical activity (6*).
Traditionally OSD is reported as a self-limiting growth-related condition that resolves spontaneously within 12 to 24 months with the maturation of the tibial tuberosity, and no residual symptoms in the majority


(~90%) of cases (7). However, there is little data to support this claim. A healing period of even 1–2 years can be a lifetime for an adolescent, especially one that is a competitive athlete. More studies are documenting the fact that adolescents are suffering from long-term symptoms and even adults may present with residual symptoms or sequelae from OSD (8*,9,10*,11). Çakmak et al. also reported on the potential for OSD symptoms to persist into adulthood, thus contradicting the common assumption OSD is innocuous as previously assumed (12). This is problematic, as it may lead clinicians to underestimate the potential burden and impact of experiencing long-standing pain during adolescence. A recent survey of healthcare professionals stated they expected that the majority of patients would return to sport, symptom free within 6 months (13). Thus, children and adolescents complaining of ‘growing pains’ need to be better managed to ensure a favourable long-term outcome. Amusingly, the number of available review articles covering OSD treatment options is even larger than the number of available original studies or clinical trials. Although the problem is starting
All references marked with an asterisk are open access and links are provided in the reference list.
14
THE PREVALENCE OF OSGOOD–SCHLATTER DISEASE (OSD) IS HIGHEST IN ACTIVE ADOLESCENTS
to be recognised, evidence-based guidelines do not exist, which results in treatment recommendations being based on clinicians’ experience and anecdotal evidence (1*,14*). This article will address the concerns of long-term pain and disability following OSD, and what options might exist to better manage our youth. In the best cases, OSD may resolve quickly with no residual symptoms, but this may not be the case for all patients.

The Reality of a Poor Prognosis Following OSD
Research by Krause et al. in the 1990s stated that at long-term follow-up (mean, 9 years) as many as 1 in 4 patients had ongoing symptoms into adulthood (15). Although the severity and impact on sport and lifestyle were not documented, 60% of subjects were unable to kneel without discomfort. A more recent retrospective study (8*) indicated that at a median 4-year follow-up, 60% of OSD patients still experienced knee pain, with an average duration of symptoms being 90 months. Of those still experiencing knee pain, 43% suffered from daily pain. More than half of the subjects reported that the pain reduced their sports participation. The knee injury and osteoarthritis outcome score sports/recreation (KOOS) subscale scores were significantly lower in those with knee pain than in those without pain. The lower self-reported function and HRQoL–EQ-5D-3L-Y (health-related quality of life – youth version EuroQol 5 dimensions 3 levels) score in those with continued pain may be a consequence of impaired physical activity due to knee pain (16*). College-aged men (mean, 20 years old) with a history of physiciandiagnosed unilateral OSD have a greater disability compared with agematched subjects without a history of OSD (8*). Research has shown that 79% of the patients still complained of persistent but not impairing pain on kneeling or knee contact at a 4-year


follow-up. However, within this study, 28% of all patients reported having switched their sport activity to other disciplines due to OSD (9).
Kaya et al. found that as many as 50% of adolescents continue to show ultrasound (US) findings consistent with OSD at 24-month follow-up (17). In addition to this, these adolescents demonstrated functional limitations in objective measures of lower limb strength, power and endurance performance at the same follow-up. It is concerning that such functional deficits and resulting disability may persist into adulthood (17).
Interestingly, subjects who stated themselves as ‘recovered’ at followup (ie. no longer experiencing pain), reported mean KOOS and EQ-5D-Y index scores lower than documented for controls without a history of knee pain (18). Again this suggests a potential longer-term disability with functional deficits in patients with a history of OSD (5*,8*,17). A high rate of dropout in sports is seen following OSD. It has been reported that more than 70% of patients with OSD are restricted from sports for more than 10 months on average, and 1 in 3 adolescents when returning to sport after 3 months of being symptom free experience a recurrence (19). There may be a need for greater focus on ongoing management, and rehabilitation as well as a graduated return to sport.
Would Imaging Help the Management of OSD?
The majority of clinicians are confident in making an OSD diagnosis based on patient history and clinical examination without the use of imaging (13). The majority of imaging studies have focused on using imaging to characterise the pathophysiology – despite the fact that the pathology for OSD still
remains controversial. Originally, OSD was attributed to the avulsion of the tibial tuberosity due to forceful patellar tendon contractions. Since then studies have demonstrated that fragmentation may be a normal part of maturation and not necessarily pathologic. Many studies have reported soft tissue changes, such as in the patellar tendon, as being characteristic of OSD. The De Flaviis classification of OSD was developed using US equipment, but the interrater and intrarater reliability is yet to be examined. Baseline De Flaviis categorisation (using US) has been shown to be associated with a worse prognosis for pain, whereas those without identifiable changes (cartilage swelling, bony change, and/ or associated tendinopathy/bursitis) at baseline demonstrate a significantly better prognosis (5*).
PHYSICAL THERAPY
OSD IS CONSIDERED TO BE AN APOPHYSEAL INJURY OF THE TIBIAL TUBEROSITY AT THE SITE OF THE PATELLAR TENDON ATTACHMENT
EVIDENCE SHOWS
Treatment Options Without Scientifc Guidelines
It is possible that owing to the previously assumed innocuous nature of OSD, there is a scarcity of research evaluating interventions to reduce symptoms, improve function and speed up or sustain recovery. Randomised controlled trials are confined to investigating injections and surgical management. No randomised controlled clinical trials have evaluated other management strategies (2*).
From a recent survey of clinicians, the most common treatments were patient education (99%) and exercise therapy (92%). There was some heterogeneity across pain medication prescriptions (31% for and 34% against). Factors which may influence a clinician’s decision to allow a return
treatment strategies have been proposed (1*,22*):
1. a decrease in physical activity (2*,23);
2 application of cold;
3. use of knee orthoses to apply support or pressure to the patellar tendon thus reducing the tractional load on the insertion;
4. physical therapy (24);
5. warm-up and cool-down exercises before and after training and competition; and
6. stretching of the leg extensor musculature to reduce the tension generated by the extensor apparatus (1*,24,25,26*).
Regarding the final point above, care should be taken not to stretch excessively, as it is essential to
are speculative based on patient symptoms and the understanding of the pathophysiology or have been extrapolated from other knee conditions [including anterior cruciate ligament (ACL) injury rehab or patellofemoral pain syndrome (PFPS)]. A recent cohort study by Rathleff et al. reported high rates of successful outcomes among OSD patients (80% at 12 weeks and 90% after 12 months), with 16% having returned to sport after 12 weeks, and 67% after 6 months (2*). This was after a 12-week intervention that included:

1. an activity ladder, designed to manage patellar tendon loading and pain (see the ‘Activity ladder’ on p3 of Appendix 1 “Quit knee pain –Osgood Schlatter” (https://bit.ly/3G8DMYc) from Rathleff et al. (2*));
2. knee-strengthening exercises; and 3. graduated return to sport.
The intervention was structured into 2 blocks: see ‘Table 2: Building blocks of the intervention’ (http://bit.ly/3X271Su) in Rathleff et al. (2*)). Weeks 0–4 included an initial load management strategy with a temporary reduction in sport participation. During this time, subjects were instructed to refrain from pain-aggravating activities and sport participation. Yet knee exercises were performed, including static holds and bridging to avoid loss of muscle strength. The load-based activity ladder and pain monitoring were used as guidance and support at this time
During weeks 5–12, adolescents performed a progressive homebased knee-strengthening exercise programme while still following the activity ladder, and progressing towards a return to sport. Three exercises progressed with increasing difficulty. Subjects were not allowed to move onto level 3 (slow running) on the activity ladder until they were able to perform a squat with a pain rating below 3. The exercises included wall squats that progressed as pain allowed to a 90° knee-flexion wall squat. Then a standing squat progressing to a 90° knee-flexion posture and finally a lunge. Consultation with physical
THAT ADOLESCENTS ARE SUFFERING FROM LONG-TERM SYMPTOMS OF OSD AND EVEN ADULTS MAY PRESENT WITH RESIDUAL SYMPTOMS OR SEQUELAE
therapists during the 12 weeks focused on educating the adolescents and their parents on understanding the benefits of progressive loading and avoiding painful setbacks. Greater detail about the education programme and exercise progression (sets, repetitions, holds) is available in the Appendices of Rathleff et al. “Activity modification and knee strengthening for OsgoodSchlatter disease: a prospective cohort study” (http://bit.ly/3X271Su). This study illustrated that active intervention improved pain and knee function as well as realising a successful return to sport over 12 months. Thus, targeted strength training can offset some of the long-term negative impacts previously documented (2*). Adolescents with OSD have shown approximately 30% lower isometric knee extension strength compared to their pain-free peers (18), and strength deficits may persist after the resolution of symptoms (17). The intervention increased strength to the same level as adolescents without knee pain (18). Strength training should prepare adolescents for return to sport, as they are then better prepared to withstand the physical demands. Treatments such as stretching, rest, and other passive modalities although recommended (22*,25) neglect this objective.
Rathleff et al. highlighted that despite the majority of adolescents reporting that they were improved, one-third still experienced pain and were affected in their sport participation (2*). In addition to this, at 12-month follow-up less than 50% reported that they would be satisfied to live with their current symptoms. It may be prudent to consider this a long-standing condition, which may in some cases need ongoing management (2*). More studies like this are needed to add to the body of evidence and possibly offer a longerterm intervention, follow-up and/or maintenance programme to prevent symptoms continuing into adulthood. Active intervention like physical or exercise therapy may offer an alternative to passive approaches.

Knee rehabilitation and prevention programmes generally cover a component of activity progression combined with progressive
LOAD
strengthening. Within that conditioning element, neuromuscular-training programmes (proven effective through clinical trials) play a vital role. Neuromuscular training may include plyometrics, balance, agility, flexibility and strengthening. Should we not raise the question then why, in the management and prevention of recurrence of OSD, these proven interventions are not considered?
It has been suggested that excessive tractional loads should not be applied through the patellar tendon onto the anterior tibial tuberosity in children aged 9 to 15 years (22*). Any underlying muscle imbalances that favour higher tension (stiffness) in the patellar tendon should be addressed. This may be of particular concern when added to sports activities with acyclic and explosive components. Muscle rebalancing through lengthening (flexibility) and strengthening programmes that contribute to reducing tension at the patellar tendon insertion might be an interesting strategy towards managing OSD (22*). Furthermore, some authors recommend core stabilisation exercises may benefit knee pain and dysfunction. Core stability exercises have become one of the more favoured components in ACL injury-prevention programmes. During physical activities, the knee joint biomechanics are affected by the dynamic motion of the trunk and hip joint. Deficits in neuromuscular control in the trunk and hip joint have been shown to increase ACL injury risk. It has been demonstrated that core stability can predict ACL injury and that hip abduction and external-rotation muscle strength can predict noncontact knee injury in athletes (27*). Simple core muscle training results in changes to neuromuscular control in the trunk and lower limbs, thus increasing trunk and pelvic stability and thereby reducing the risk of a knee injury (27*). These proven benefits should be extrapolated and studied in intervention programmes for OSD in
the future.
EXERCISES
Additionally, it has been seen that trunk muscle activity precedes the dynamic movement of the extremities, implying that the abdominal muscles may engage to provide a stable foundation for production, absorption and force control during the motion to the extremities. Subsequently, insufficient core stability may lead to less efficient movements and possibly musculoskeletal injury. Reduced core stability, tested in runners, has been linked to increased peak torque in knee flexion during the stance phase of running (28*). This, in turn, increases vertical loading and places the individual at risk of injury, specifically in the development of PFPS. Emphasising core stability
17 PHYSICAL THERAPY
AN INITIAL
MANAGEMENT STRATEGY FOLLOWED BY KNEE-STRENGTHENING
HAS SHOWN HIGH RATES OF SUCCESS
OSD IS NO LONGER SIMPLY A ‘REST AND RECOVER’ CONDITION
athletes involved in jumping activities is advocated (27*,28*). Despite these potential benefits, more studies are needed to clarify which type of treatment would be most appropriate for adolescents. As confirmed by Neuhaus et al., no clinical trial comparing specific exercises with sham or usual care treatment exists (1*).
Other treatment modalities could be considered. Extracorporeal shock wave therapy has been proven to effectively reduce tendon pain owing to its analgesic effects and to promote remodelling and repair of soft tissues (29). Magnetic field therapy may effectively enhance cartilage and bone repair by increasing the bone matrix (10*). Again no clinical trial has
been conducted to assess efficacy in adolescents with OSD.
Surgery should only be considered when other types of treatment have previously failed or when bone fragments (intra- or extra-tendon) remain after complete ossification (22*). Surgery may be necessary if nondisplacement fractures are present. Different surgical techniques and approaches have been proposed, each with advantages and disadvantages (22*).
Where Does That Leave Us?
The scarcity of literature pertaining to OSD, particularly in the clinical management of patients is concerning. Future research is required not only to investigate the pathology of the condition but also (and more importantly) any possible preventive measures and long-term management protocols. It is true that investigating and understanding the multiple factors related to this condition is key; however, at this time it is necessary for research to delve much deeper into the treatment options, both at the preventive and recovery level.
For symptom relief, a combination of training load reduction or relative rest, and limitation of movement patterns that generate pain may contribute to the improvement. Progressive muscle strengthening combined with a progressive return to activity appears to produce positive outcomes. Addressing muscle imbalances through exercise therapy and preparing the body for the loads anticipated on return to sport makes ‘rehabilitation sense’. The evidence is telling us that OSD is not simply a ‘rest and recover’ condition. We would be doing our youth an injustice if we did not structure more effective ways of managing OSD.
References
1. Neuhaus C, Appenzeller-Herzog C, Faude O. A systematic review on conservative treatment options for OSGOOD-Schlatter disease. Physical Therapy in Sport 2021;49:178–187 Open access http://bit.ly/3A8oT4z
2. Rathleff MS, Winiarski L, Krommes K et al. Activity modification and knee strengthening for Osgood-Schlatter disease: a prospective cohort study. Orthopaedic
Journal of Sports Medicine 2020;8(4):232596712091110 Open access http://bit.ly/3X271Su
3. Nakase J, Aiba T, Goshima K et al. Relationship between the skeletal maturation of the distal attachment of the patellar tendon and physical features in preadolescent male football players. Knee Surgery, Sports Traumatology, Arthroscopy 2014;22(1):195–199

4. Yanagisawa S, Osawa T, Saito K et al. Assessment of Osgood-Schlatter disease and the skeletal maturation of the distal attachment of the patellar tendon in preadolescent males. Orthopaedic Journal of Sports Medicine 2014;2(7):232596711454208 Open access http://bit.ly/3AdfN6y
5. Holden S, Olesen JL, Winiarski LM et al. Is the prognosis of Osgood-Schlatter poorer than anticipated? A prospective cohort study with 24-month follow-up. Orthopaedic Journal of Sports Medicine 2021;9:232596712110222 Open access http://bit.ly/3TBcM71
6. Schultz M, Tol JL, Veltman L et al. Osgood-Schlatter disease in youth elite football: minimal time-loss and no association with clinical and ultrasonographic factors. Physical Therapy in Sport 2022;55:98–105 Open access http://bit.ly/3Gep2qN
7. Circi E, Atalay Y, Beyzadeoglu T. Treatment of Osgood–Schlatter disease: review of the literature. Musculoskeletal Surgery 2017;101:195–200
8. Ross MD, Villard D. Disability levels of college-aged men with a history of Osgood-Schlatter disease. The Journal of Strength and Conditioning Research 2003;17(4):659–663 Open access http://bit.ly/3WTIzTz
9. Rathleff MS, Rathleff CR, Olesen JL et al. Is knee pain during adolescence a selflimiting condition? American Journal of Sports Medicine 2016;44(5):1165–1171

10. Lee DW, Kim MJ, Kim WJ et al. Correlation between magnetic resonance imaging characteristics of the patellar tendon and clinical scores in OsgoodSchlatter disease. Knee Surgery & Related Research 2016;28(1):62–67 Open access http://bit.ly/3EwemT6
11. Circi E, Beyzadeoglu T. Results of arthroscopic treatment in unresolved Osgood-Schlatter disease in athletes. International Orthopaedics 2017;41(2):351–366
12. Çakmak S, Tekin L, Akarsu S. Long-term outcome of Osgood-Schlatter disease: not always favorable. Rheumatology International 2014;34(1):135–136
13. Lyng KD, Rathleff MS, Dean BJF et al. Current management strategies in Osgood Schlatter: a cross-sectional mixed-method study. Scandinavian Journal of Medicine & Science in Sports 2020;30:1985–1991
14. Cairns G, Owen T, Kluzek S et al. Therapeutic interventions in children and adolescents with patellar tendon related pain: a systematic review. BMJ
18
Open Sport & Exercise Medicine
2018;4(1):e000383 Open access http://bit.ly/3TxL22T
15. Krause BL, Williams JP, Catterall A. Natural history of Osgood-Schlatter disease. Journal of Pediatric Orthopedics 1990;10(1):65–68
16. Guldhammer C, Rathleff MS, Jensen HP et al. Long-term prognosis and impact of Osgood-Schlatter disease 4 years after diagnosis: a retrospective study. Orthopaedic Journal of Sports Medicine 2019;7(10):232596711987813 Open access http://bit.ly/3hH4wVy
17. Kaya DO, Toprak U, Baltaci G et al. Long-term functional and sonographic outcomes in Osgood–Schlatter disease. Knee Surgery, Sports Traumatology, Arthroscopy 2013;21(5):1131–1139
18. Rathleff MS, Winiarski L, Krommes K et al. Pain, sports participation, and physical function in adolescents with patellofemoral pain and OsgoodSchlatter disease: a matched crosssectional study. Journal of Orthopaedic & Sports Physical Therapy 2020;50(3):149–157
19. Kujala UM, Kvist M, Heinonen O. Osgood-Schlatter’s disease in adolescent athletes. American Journal of Sports Medicine 1985;13(4):236–241
20. Sailly M, Whiteley R, Johnson A. Doppler ultrasound and tibial tuberosity maturation status predicts pain in adolescent male athletes with Osgood-Schlatter’s disease: a case series with comparison group and clinical
KEY POINTS
interpretation. British Journal of Sports Medicine 2013;47(2):93–97 Open access http://bit.ly/3AbmBS0
21. Hirano A, Fukubayashi T, Ishii T et al. Magnetic resonance imaging of OsgoodSchlatter disease: the course of the disease. Skeletal Radiology 2002;31(6):334–342
22. Corbi F, Matas S, Álvarez-Herms J et al. Osgood-Schlatter disease: appearance, diagnosis and treatment: a narrative review. Healthcare 2022;10(6):1011 Open access http://bit.ly/3WTJiUN
23. Nührenbörger C, Gaulrapp H. OsgoodSchlatter disease. Sports Orthopaedics and Traumatology 2018;34(4):393–395
24. Bezuglov EN, Tikhonova AA, Chubarovskiy PhV et al. Conservative treatment of Osgood-Schlatter disease among young professional soccer players. International Orthopaedics 2020;44(9):1737–1743
25. Ladenhauf HN, Seitlinger G, Green DW. Osgood–Schlatter disease: a 2020 update of a common knee condition in children. Current Opinion in Pediatrics 2020;32(1):107–112
26. Launay F. Sports-related overuse injuries in children. Orthopaedics & Traumatology: Surgery & Research 2015;101(1 Suppl):S139–147 Open access http://bit.ly/3EwywN8
27. Sasaki S, Tsuda E, Yamamoto Y et al. Core-muscle training and neuromuscular control of the lower limb and trunk. Journal of Athletic Training 2019;54(9):959–969
Open access http://bit.ly/3EEdwEh
28. Chaudhari AMW, Van Horn MR, Monfort SM et al. Reducing core stability
l Osgood–Schlatter disease (OSD) is a sport- and growth-associated knee pathology seen in adolescents.
l OSD is a relevant problem in young athletes, predominantly treated conservatively with a ‘wait and see’ philosophy.
l Research has revealed that adolescents can experience symptoms well beyond the expected 12–24-month recovery timeline.
l Pain, strength deficits and functional disability originating from OSD can persist into adulthood.
l Many adolescents have had to stop their sport, or change their sporting code because of persistent symptoms or recurrence of injury.
l Reviews have highlighted the poor prognosis of OSD and the severe lack of clinical trials investigating treatment protocols.
l Only one study exists that implements an intervention of progressive lower limb strengthening exercises combined with activity modification and a graduated return to sport, and shows positive outcomes in OSD.
l Core muscle strengthening improves neuromuscular control of the trunk and lower limbs reducing the risk of knee injuries, this may be extrapolated to OSD.
l Core muscle training is proven essential in anterior cruciate ligament injury prevention and rehabilitation and could benefit adolescents with OSD.
l A pro-active management strategy of exercise therapy, education, activity modification and graduated return to sport, with a long-term maintenance plan, may be required to ensure a positive outcome.
influences lower extremity biomechanics in novice runners. Medicine & Science in Sports and Exercise 2020;52(6):1347–1353 Open access http://bit.ly/3O161dv
29. Lohrer H, Nauck T, Schöll J et al. [Einsatz der extrakorporalen Stoßwellentherapie bei therapieresistentem M. Schlatter.] Sportverletzung Sportschaden 2012;26(4):218–222.
RELATED CONTENT
l Osteoarthritis of the Knee: A Practical Treatment Approach [Article] http://bit.ly/3hCalDF
l Patellofemoral Pain Syndrome: A Practical Treatment Approach [Article] http://bit.ly/3WSSSqK

DISCUSSIONS
l What is your current belief and treatment plan for adolescents presenting with OSD?
l Do you believe you have seen knee pain and functional disability in young adults that may be persisting from OSD and why?
l Would you agree that not managing ‘growing pains’ seriously could negatively impact an adolescent’s pain beliefs and influence their biopsychosocial pain model?
THE AUTHOR
Kathryn Thomas BSc Physio, MPhil Sports Physiotherapy is a physiotherapist with a Master’s degree in Sports Physiotherapy from the Institute of Sports Science and University of Cape Town, South Africa. She graduated both her honours and Master’s degrees Cum Laude, and with Deans awards. After graduating in 2000 Kathryn worked in sports practices focusing on musculoskeletal injuries and rehabilitation. She was contracted to work with the Dolphins Cricket team (county/provincial team) and The Sharks rugby teams (Super rugby). Kathryn has also worked and supervised physios at the annual Comrades Marathon and Amashova cycle races for many years. She has worked with elite athletes from different sporting disciplines such as hockey, athletics, swimming and tennis. She was a competitive athlete holding national and provincial colours for swimming, biathlon, athletics, and surf lifesaving, and has a passion for sports and exercise physiology. She has presented research at the annual American College of Sports Medicine congress in Baltimore, and at South African Sports Medicine Association in 2000 and 2011. She is Co-Kinetic’s technical editor and has taken on responsibility for writing our new clinical review updates for practitioners.
Email: kittyjoythomas@gmail.com

19 PHYSICAL THERAPY
All references marked with an asterisk are open access and links are provided in the reference list
TheHypermobility Conundrum
Joint hypermobility includes a complex range of conditions. This article clarifies the different categories and definitions used in this field and describes how to make a proper assessment of a patient with hypermobility to allow the best personalised management (including onward referral if necessary) for a successful outcome.
By Kathryn Thomas BSc MPhil
The ability to move one’s joints beyond the normal range of motion (ROM) would be defined as joint hypermobility (JH). Depending on the definition or classification of JH, and on race, age and sex, an estimated prevalence of 2–57% exists (1*). In some activities and sporting disciplines, where high flexibility is required, JH may be seen as advantageous. However, not all hypermobility disorders are asymptomatic. Some present with chronic or recurrent pain, joint instability, fatigue and disability. In some cases, there may be additional musculoskeletal complaints, impaired function, decreased ability to perform daily activities, increased psychological problems and poor health-related quality of life (2*,3).

Historically, hypermobility syndrome was defined as ‘the occurrence of symptoms in otherwise healthy hypermobile individuals’. Specialists in genetics and
dermatology ascribed the term ‘Ehlers–Danlos syndromes’ (EDSs), whereas the rheumatology field coined the term ‘joint hypermobility syndrome’ (JHS), and others referred to the symptomatic clinical entity as ‘hypermobility spectrum disorder’ (HSD) (4*). Specialists from different fields recognised the overlap and possible confusion in diagnosing, naming and thus managing these conditions. Recent consensus has agreed upon terminology attributed to specific diagnoses of generalised hypermobility spectrum disorder (G-HSD) and hypermobile Ehlers–Danlos syndrome (hEDS) (4*).
Owing to its prevalence and the existence of some emerging evidence, one can consider the shoulder in HSD patients as an example of a management strategy. Four out of five patients with HSD experience shoulder joint symptoms which may have a profound impact on daily life (1*,2*,3). In patients with HSD and
multidirectional shoulder instability, recent studies have shown imbalanced electromyographic scapular muscle activity, altered scapular kinematics and increased humeral head translation (5). Clinical trials focused on treatments for shoulder instability for HSD patients have not been conducted, and there is no gold standard of treatment (6*,7). Management for persistent shoulder complaints, such as rotator cuff tendinopathy, impingement syndrome and anterior or multidirectional glenohumeral instability focuses on improving the scapular stabilising muscles and rotator cuff muscle function. This is achieved through exercise interventions (8*,9).
Many clinicians are hesitant to use high-load strengthening exercises when dealing with shoulder laxity, instability or HSD owing to uncertainty about safety and efficacy. Current guidelines actually recommend against high-load strengthening (10*,11*), and therefore low-load strengthening and closed-chain exercises dominate the exercise regimens.
However, high-load strengthening exercises are proven to be particularly effective at increasing tendon stiffness and global muscle strength (12*). Given that patients with HSD often
Co-Kinetic Journal 2023;95(January):20-26 20
PEOPLE WITH JOINT-HYPERMOBILITY-RELATED DISORDERS CAN PRESENT ALONG A SPECTRUM OF PHENOTYPES
present with strength impairments in the shoulder and decreased tissue stiffness, one might anticipate that they would benefit from highload strengthening (13*). A recent randomised controlled trial showed that high-load shoulder strengthening was statistically superior to low-load strengthening exercises for selfreported shoulder pain and function in the short-term (16 weeks) in HSD patients (11*).
People with JH-related disorders can present along a spectrum from asymptomatic, to symptomatic with a few or many musculoskeletal complaints, to symptoms involving multiple systems including but not limited to the cardiovascular, gastrointestinal, urogynaecological, dermatological and psychological systems. Early recognition and treatment are key to effective management. A biopsychosocial and patient-empowerment approach to functional restoration is recommended. Based on the above, this article endeavours to give some clarity to the clinical identification of the hypermobility spectrum. Simple ways in which you can differentiate HSD from other hypermobility, laxity or instability conditions as well as an outline of the latest evidence regarding management will be discussed.
efniti ns l ssifc ti ns and Clarity
Laxity, JH and instability, although used interchangeably, are not synonymous (14*).
l Laxity – is an objective measure describing the passive movement of a joint beyond the normal limit during an accessory motion. This may be a glide or spin. It may be assessed or measured manually for example the Lachman’s test of the knee, or a shoulder or ankle anterior drawer test. It can also be tested using a mechanical device.
l Hypermobility – is an objective measure describing the active or passive movement of a joint beyond normal physiological limits around its axes of motion. Hyperextension or recurvatum of the knee is an example. It is proposed that JH is multidimensional in causes including
bone morphology/shape, the increased surface area of articulation and dysplastic or excessively compliant passive restraints.
l Functional instability – is a selfreported or subjective observation by a patient mistrusting or feeling insecure about their joint remaining intact even under low-load/force conditions. They might describe their joint as going out of place, giving way, subluxing or even dislocating. Functional instability or ‘confidence in the joint’ may be assessed by questionnaire.
Signs of hypermobility and laxity, if asymptomatic, may be clinically irrelevant. Similarly in the absence of functional instability (a symptom except where dislocation is evident) may be deemed ‘normal’. In some individuals, it may be an asset to their activities or sporting endeavours. Consider a gymnast or ballerina, despite their hypermobility and laxity, they do not report joint subluxations or dislocations during their routines or activities of daily life. Their joints are not considered unstable and do not require management. In this scenario, inadequate passive stabilisers (fascia, joint capsule and ligaments) may be disguised. Adequate stability by the active system (muscles and tendons) combined with adequate proprioception and kinesthesis ensure that the physiological and accessory motions are controlled. Affected joints may become symptomatic when the active system fails, which may occur owing to injury or deconditioning (14*).
The presentation and distribution of JH may vary widely across individuals, and age, sex and race. It may be monoarticular (affecting a single joint), pauciarticular/ oligoarticular (affecting a few joints), polyarticular (affecting several joints often either central or peripheral, upper or lower limbs), or be generalised JH (GJH) (present in all four limbs and the axial skeleton). Hypermobility may be inherited with no identifiable genetic variant or inherited as part of a syndrome such as the EDSs and other connective tissue heritable disorders. Otherwise, JH may be acquired from trauma, injury, joint
disease or training. For example, a baseball player’s throwing or dominant arm may have greater shoulder ROM compared to his non-dominant arm. Likewise, a fast bowler in cricket may have developed greater shoulder mobility and back extension over the years of playing the sport.
Many people with hypermobile joints remain asymptomatic throughout their life. Thus a healthy individual without any associated symptoms or complications may be described as having ‘asymptomatic JH’. Researchers and clinicians don’t fully understand the determinants that cause JH to become symptomatic. It seems that there may be a threshold for multiple risk factors either at the joint or within proximity of the hypermobile joint that results in the onset of pain and symptoms. Risk factors may include muscle weakness, insufficient musculotendinous length, reduced mobility, muscle hypertonicity, obesity and altered movement patterns (14*). Hence, hypermobility combined with pain, recurrent subluxations and musculoskeletal overload injuries may be categorised as ‘symptomatic JH’. This typically results in decreased functional capacity, reduced strength, suboptimal muscle activation and poor musculoskeletal control (14*).
hypermobile joints often have complaints beyond the confines of the joint or even the musculoskeletal system. Two-thirds of these patients have functional multisystemic symptoms, including (but not limited to) physical and cognitive fatigue, anxiety and depression, gastrointestinal dysfunction, orthostatic intolerance, postural orthostatic tachycardia syndrome (POTS), and urogynecological problems (14*). See ‘Figure 1: Phenotypic ramifications of joint
PHYSICAL THERAPY Co-Kinetic.com
SIGNS OF HYPERMOBILITY AND LAXITY, IF ASYMPTOMATIC, MAY BE CLINICALLY IRRELEVANT
SYMPTOMATIC HYPERMOBILE
hypermobility’ (http://bit.ly/3EuIBKg) in Castori et al. for a useful summary of JH manifestations (4*). There is an association between many of these conditions and GJH, but the associated underlying pathology remains unknown.
‘Figure 1: Phenotypic presentation of joint hypermobility’ (http://bit.ly/3TCPkWV) in Nicholson et al. is a useful illustration where JH can be compared with ‘the tip of an iceberg’ (14*). The tip above the water surface is the most obvious feature that stands out during clinical assessment. Most individuals remain asymptomatic, but some patients develop symptoms. Careful consideration for further investigations and referral to a specialist may be required for those patients presenting with orthopaedic deformities, skin alterations and tissue fragility, where ruling out a heritable connective tissue disorder would be important.
As suggested from the iceberg image mentioned above, further screening is warranted for a patient with hypermobility who also demonstrates several orthopaedic deformities, skin abnormalities and vascular fragility to ensure proper medical follow-up and avoid more severe complications. Pathologies that could relate to this presentation include disorders of connective tissue such as Marfan syndrome, EDSs, osteogenesis imperfecta and Stickler syndrome. Several other chromosomal disorders (such as Down syndrome) and metabolic disorders (such as homocystinuria and hyperlysinemia) may also need to be excluded (14*). Features to be aware of during the assessment include:
Marfan syndrome, vascular EDS, familial thoracic aortic aneurysm.
2. Skin fragility and altered skin structure
l soft and velvety skin surface; l stretchy skin; l skin hyperextensibility; l atrophic scarring; l the presence of multiple scars; l delayed wound healing; and l wound dehiscence.
3. Orthopaedic deformities
l pectus deformity; l congenital club feet; l short or tall stature; l congenital scoliosis; l bilateral congenital hip dysplasia and/or hip dislocations; l increased arm span-to-length ratio; and l arachnodactyly (14*).
The recently (2017) revised EDS classification states for persons with otherwise unclassified JH, the term ‘hypermobile-EDS’ (hEDS) should be restricted to those with features suggestive of a systemic and/or Mendelian connective tissue disorder (4*). Of the 13 types of EDSs, hEDS is the most common accounting for greater than 95% of all EDS presentations (15*). The conditions G-HSD and hEDS share many clinical characteristics, including: l GJH l joint instability l widespread chronic pain.
So to be clear how can you classify JH, Castor et al. (4*) have proposed that JH can be classified into three categories as follows.
Five exercises targeting scapular and rotator cuff muscles. A1–A2: side-lying external rotation (ER) in neutral; B1–B2: prone horizontal abduction; C1–C2: prone ER in 90° of shoulder abduction; D1–D2: supine scapular protraction; and E1–E2: seated shoulder elevation in the scapular plane.
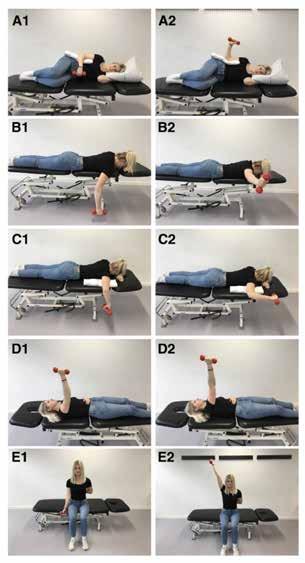
1: The exercise programme
1. Tissue fragility (patient history and observation may allude to this factor)
l recurrent fractures (bone fragility); l soft tissue fragility (abdominal hernia, bladder, uterine, or bowel prolapse);
l organ fragility (rupture of hollow organs); and
l vascular fragility – the most important to recognise – easy bruising, bleeding tendency, vascular aneurysms, dilatations, or dissections; associated with
1. Subjects with asymptomatic, nonsyndromic/isolated localised JH (LJH; affecting a single small or large joint), peripheral JH (PJH; affecting mostly hands and feet only, no large or axial joint involvement), or generalised JH (GJH; involving peripheral small and large joints and axial joints). Asymptomatic JH may have a familial pedigree and, theoretically, might also occur as an isolated trait in healthy relatives of patients with a full-blown hEDS.
2. Individuals with a well-defined syndrome with JH, also comprising hEDS.
Co-Kinetic Journal 2023;95(January):20-26
22
Figure
Liaghat B, Skou ST, Jørgensen U et al. Heavy shoulder strengthening exercise in people with hypermobility spectrum disorder (HSD) and long-lasting shoulder symptoms: a feasibility study. Pilot Feasability Stud to Pilot and Feasability Studies 2020;6:97 (23*). Reproduced under the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/).
PATIENTS WITH
JOINTS OFTEN HAVE COMPLAINTS BEYOND THE CONFINES OF THE JOINT OR EVEN THE MUSCULOSKELETAL SYSTEM
3. Individuals with symptomatic JH but not satisfying the criteria/ diagnosis for a syndrome, the term ‘hypermobility spectrum disorder(s)’ (HSDs) is proposed.
HSDs are a group of clinically relevant conditions related to JH. The phenotypic domains of HSDs are usually limited to the musculoskeletal system and thus are distinguishable from hEDS and the other syndromes with JH. In this HSD patient category there is a limited extension to other organs and tissues. Therefore, HSD classification is mostly intended as an alternative label for patients with symptomatic JH who do not meet the criteria for hEDS or any other rare EDS condition.
So, from a classification perspective, the diagnosis of hEDS is established by the presence of a positive Beighton score (ie. GJH) plus two or more systemic involvements,
musculoskeletal criteria, and positive family history (as specifically defined in the new nosology) (4*,15*). Currently, the hEDS diagnostic criteria are not valid for children and adolescents as multiple multisystemic features are not appropriate in assessing children. Thus, should an individual, particularly a child, be diagnosed as having HSD, but has a family history of hEDS, then a ‘relaxed’ follow-up in clinical genetics services may be scheduled because of a potential future revision of the diagnosis to hEDS or another JHrelated syndrome (4*).
In keeping with the previously defined types of JH, four different HSDs may be identified (4*).
1. Generalised (joint) HSD (G-HSD): GJH objectively assessed (commonly by the Beighton score, see below) plus one or more secondary musculoskeletal manifestations including trauma, chronic pain, disturbed
proprioception or neuromuscular control, and altered posture or movement patterns.
2. Peripheral (joint) HSD (P-HSD): JH limited to hands and feet plus one or more secondary musculoskeletal manifestations as previously identified above.

3. Localised (joint) HSD (L-HSD): JH at single joints or group of joints plus one or more secondary musculoskeletal manifestations regionally related to the hypermobile joint(s).
4. Historical (joint) HSD (H-HSD): selfreported (historical) GJH (by the five-point questionnaire, see below) with negative Beighton score plus one or more secondary musculoskeletal manifestations. In these cases, physical examination is aimed at excluding other types of HSD as well as other rheumatologic conditions.
See ‘Table 1: Phenotypes belonging to the “spectrum”’ (http://bit.ly/3EuIBKg
Table 1: Mechano-biological description of the progressive heavy shoulder strengthening programme (HEAVY) Liaghat B, Skou ST, Søndergaard J et al. A randomised controlled trial of heavy shoulder strengthening exercise in patients with hy permobility spectrum disorder or hypermobile Ehlers–Danlos syndrome and long-lasting shoulder complaints: study protocol for the Shoulder-MOBILEX study. Trials 2020;21:992 (24*). Reproduced under the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/). X1, load magnitude, repetition maximum (RM); X2, number of repetitions; X3, number of sets; X4, rest in-between sets; X5, number of sessions per week; X6, duration of the experimental period; X7, fractional and temporal distribution of the contraction modes per repitition and duration of one repetition; X8, rest in-between repetitions; X9, time under tension (s); X10, volitional muscular failure; X11, range of motion (ROM); X12, recovery time in between exercise sessions; X13, predefined anatomical exercise form
23 Co-Kinetic.com
Week X1 X2 X3 X4 X5 X6 X7 X8 X9 X10 X11 X12 X13 1 50% 10 RM 10 3 60s 3 per week 1 week 3s shortening 0s 60s No Full ROM 48h Yes 0s isometric 3s lengthening 2 70% 10 RM 10 3 60s 3 per week 1 week 3s shortening 0s 60s No Full ROM 48h Yes 0s
3s
3 90% 10 RM 10 3 60s 3 per week 1 week 3s
0s 60s No Full
48h
0s
3s
4 10 RM 10 3 60s 3 per week 6 weeks 3s
0s 60s Yes
48h
0s
3s
10 8 RM 8 4 90s 3 per week 6 weeks 3s shortening 0s 48s Yes Full ROM 48h
0s
3s
16 70% 8 RM 8 4 90s 3 per
isometric
lengthening
shortening
ROM
Yes
isometric
lengthening
shortening
Full ROM
Yes
isometric
lengthening
Yes
isometric
lengthening
week 1 week 3s shortening 0s 48s No Full ROM 48h Yes 0s isometric 3s lengthening
PHYSICAL THERAPY
in Castori et al. for a useful summary of the classification of the different domains of JH (4*).
In most cases, the Beighton score functions well as a screening tool (Video 1). However, in those who experience symptoms associated with JH, more extensive assessment to determine the joint(s) and plane(s) of movement affected together with patient-specific and objective functional assessments will facilitate a targeted management approach (16*). For example, a patient who describes shoulder instability and tests positive to all three upper limb hypermobility assessment tool (ULHAT) shoulder tests and demonstrates functional movement impairments may best be managed with exercises that improve strength and control in more than one anatomical plane.
For more information about screening JH see ‘Assessing Joint Hypermobility’ (http://bit.ly/3twpJEk) by the Ehlers–Danos Society (17*).


The ‘Supplementary Table: Summary of the test items in the Beighton score, upper limb hypermobility assessment tool, lower limb assessment score and 5-part hypermobility questionnaire’ (https://
bit.ly/3BaOXfS) in Nicholson et al. is a summary of the test items mentioned above (14*). In addition to these tests, it is strongly advised to include multiple objective tests when assessing EDS or HSD patients, for example, muscle strength and endurance, physical function, balance and movement patterns or coordination (13*). Disability in HSD and hEDS is often due to pain, fatigue or psychosocial distress and therefore each of these factors should be explored in the history. Childhood symptoms, such as clumsiness and poor coordination/ frequent falls are also important to explore (18).
If patients with HSD and hEDS complain of POTS-related symptoms (for example chest pain, syncope or dizziness when moving from sitting to standing, brain fog and fatigue) a ‘stand test’ can substitute for the formal tilt-table test. The stand test involves recording the patient’s heart rate after 5 minutes of resting supine, then at 2, 5, and 10 minutes of standing still (without fidgeting). Ideally, blood pressure is monitored to rule out orthostatic hypotension. A rise of ≥ eats per minute in adu ts and ≥4 eats per minute in chi dren is the threshold for the diagnosis of POTS (18).
Management
‘Syndromic hypermobility’ encompasses HSD and heritable connective tissue disorders such as hEDS which are characterised by excessive joint ROM and pain. Being able to make the correct diagnosis is invaluable for directing subsequent clinical management – the focus being on the patient’s individual symptom presentation. The treating therapist, after completing the assessment and diagnosis, needs to consider the degree of complexity and severity of problems and the subsequent strategies and/ or need for a multidisciplinary team approach (eg. referral for genetic screening or specialist physician if EDS is suspected). It is possible that those diagnosed with G-HSD are undermanaged because of the perception that their condition is less severe than hEDS. Conservative
interventions such as exercise therapy are the cornerstone of management, yet their effectiveness is unclear. Despite the growing body of literature, few high-quality singular intervention studies have been reported (18). Research has shown that early recognition, knowledgeable therapists, effective communication and working as a team result in successful physiotherapy outcomes (19).
An empowerment model of management suggests conditionspecific education and goal-orientated functional rehabilitation. It is believed that patients who fully understand their condition, what triggers or reactions they have and self-care strategies can more effectively manage pain and disability, as well as recover more efficiently from a flare-up or injury. Patient-centred goal setting will also help direct and motivate therapy in these patients (6*).
Strategies for joint protection and avoiding activities or movements that excessively stress the joint should be learnt by the patients and their caregivers. Therefore understanding body mechanics and ergonomics will facilitate this. For functional or recreational activities external joint support such as braces and splints can help protect both large and small joints. Apart from physical restriction, one of the benefits of bracing may be proprioceptive input through cutaneous sensory input. In addition to this, adaptive utensils and tool modifications may decrease stress on joints and thus reduce pain (18).
Exercise therapy is a key management component, as it addresses physical impairments. Strength training and proprioception have been shown to be effective in reducing pain, improving movement control and thus quality of life. Both concentric and eccentric strength can be reduced in those with syndromic hypermobility. Although hypermobile people have been shown to strengthen at the same rate as non-hypermobile people, they may need to start exercise therapy at a lower level (20). Closed-chain exercises and augmented or external feedback using biofeedback may be helpful owing to decreased proprioception. Patients
Co-Kinetic Journal 2023;95(January):20-26 24
The
Joint Hypermobility
https://bit.ly/3XM799e FURTHER SCREENING IS WARRANTED FOR A PATIENT WITH HYPERMOBILITY WHO ALSO DEMONSTRATES SEVERAL ORTHOPAEDIC DEFORMITIES, SKIN ABNORMALITIES AND VASCULAR FRAGILITY
Video 1:
Beighton Score | Generalized
(Laxity) (Courtesty of YouTube user Physiotutors)
have reported that a ‘hands-on’ approach to help guide the movement or exercise was beneficial (19). To avoid irritating unstable joints and often irritable surrounding muscles and tendons, the implementation of strengthening programmes should be slow and progressive. Patients’ muscle activation may respond differently to non-hypermobile people possibly resulting in symptom flare-ups. Patients with HSD and hEDS often report having tight muscles (19). Overstretching the joints of patients with hypermobility is discouraged, but the use of massage or foam rollers to release muscle spasms may be beneficial. Focused stretching with the joint maintained in a stable or supported position can be helpful to reduce symptoms and address muscle imbalances (21).
A recent study by Spanhove et al. showed home-based exercise programmes led to significant improvements in shoulder function in patients with EDS and HSD (22). However, the authors felt that a multidisciplinary, supervised approach might be more effective for altering kinesiophobia in this patient population. In patients with HSD, many clinicians choose lowload strengthening exercise, with a reluctancy to use high-load exercises. This may be due to concerns over safety, subluxations or dislocations and flare-ups, combined with the fact the current guidelines recommend against high-load strengthening (10*). For patients with HSD and shoulder pain and/or shoulder instability a supervised, progressive high-load shoulder strengthening exercise programme (full-range, open kinetic chain) (Fig. 1) has been proven to provide greater selfreported improvements in shoulder function than less supervised and less progressive low-load exercises (neutral to midrange) at 16 weeks (Table 1). In this study more than twothirds of patients receiving high-load strengthening exercises improved shoulder function above the threshold for minimal important difference. In addition to this 64% reported an important improvement in physical symptoms post-intervention. There

were no serious adverse events, but HEAVY (versus LIGHT) was associated with more transient muscle soreness (56% versus 37%) and headaches (40% versus 20%). With four out of five patients with HSD experiencing symptoms in the shoulder joint, it is encouraging that this may be an option for managing their shoulder pain.
When prescribing exercise, therapists should be aware of the load on the cardiovascular system which may already be compromised, depending on systemic involvement. These patients may have a reduced exercise tolerance and suffer from post-exercise malaise and symptom flare-ups. Patients with hypermobility should know their first-line management for POTS: (i) increasing fluids and salt, (ii) avoiding triggers such as hot environments and eating large carbohydrate meals. These patients should be taught anti-syncope manoeuvres such as fist clenching and shifting weight when standing for long periods of time. To aid venous return compression garments can be worn. Therapy can begin with recumbent exercises, lower extremity and core strengthening to facilitate venous return before gradually progressing to upright exercise (25). Thus recognition of the systemic issues commonly associated with HSD and hEDS by clinicians is instrumental in promoting the best possible (and safest) treatment outcomes.
Pain education, learning to self-manage and understanding the biopsychosocial complexities of pain is critical in disease management because many of these patients suffer from chronic pain and flare-ups. This must involve the children and their parents/care-giver when applicable. Pain self-care may include the use of ice, heat, bracing and pacing, learning to correct body mechanics and slow and steady progression of activities. Relaxation and coping skills, deep breathing exercises, massage and good quality sleep can reduce symptoms (18).
There is very limited evidence regarding
The risk of knee pain in overweight adolescents with hypermobility was further increased by >10-fold (26*). Thus weight management through a healthy diet and physical activity is critical to managing symptoms.
A tailored physical activity programme, including cardiovascular and strengthening activities, should meet the individual’s interests and capabilities. Walking, swimming and Pilates have been reported as
Co-Kinetic.com
PHYSICAL THERAPY
HAVING A CORRECT DIAGNOSIS IS INVALUABLE FOR DIRECTING CLINICAL MANAGEMENT


beneficial forms of physical activity (19).
Summary
People of all ages, races, sexes and family histories are likely to present with hypermobility-related disorders to health professionals. Many of these people may have complaints involving multiple body systems, not just the musculoskeletal system. The new classification of hEDS and HSD hopefully clarifies any confusion. The heterogeneous presentation of multisystem signs and symptoms means that management must be individualised. Most pertinent to management is that thorough history-taking and clinical assessment must combine with equally thorough clinical reasoning, informed by patient expectations and goals. Early recognition and treatment provided by health professionals who are knowledgeable is key to effective management. Management must include a biopsychosocial assessment and a functional restoration approach to treatment. It is critical to include patient and family education such that they can actively engage in self-management and injury prevention. Since research is sparse and just beginning to provide evidence regarding optimal interventions, therapists need to integrate existing research and clinical expertise with patient preference to maximise the benefit for each individual.
KEY POINTS
l Joint hypermobility (JH) presents on a spectrum from an asymptomatic physiological phenomenon, to one that comprises both musculoskeletal and other systemic symptoms.
l Althoughs JH is often asymptomatic, symptomatic forms require specialised assessment, management, and follow-up.
l Using standardised terminology about JH will assist researchers and clinicians to compare findings, make a diagnosis, and plan their management strategy.
l Hypermobile Ehlers–Danlos syndrome (hEDS) is the most common form of the Ehlers–Danlos syndromes, and includes both musculoskeletal, systemic symptoms and a family history or genetic component.
l Hypermobility spectrum disorder (HSD) is reserved for individuals with symptomatic JH that do not meet the criteria for hEDS.
l Early recognition and treatment of hypermobility-related disorders is key to effective management.
l A biopsychosocial, empowerment model of functional rehabilitation is recommended.
l Exercise therapy and physical activity are the cornerstones of treatment.
l Supervised exercise programmes may be more effective than homebased therapy alone.
l Emerging evidence suggests the use of high-load open-chain strengthening exercises for improving shoulder pain and function in HSD and hEDS patients is safe and effective.
DISCUSSIONS
l Have you been fastidious in considering EDS criteria (systemic involvement) when presented with a symptomatic hypermobile patient (for example shoulder pain with increased ROM)?
l If NO, do you believe this was due to a lack of clarity in definitions and screening tools available for practitioners?
l When treating a hypermobile joint what exercises or physical activity do you find most effective and facilitates patient compliance?
THE AUTHOR
Owing to space limitations in the print version, the references that accompany this article are available at the following https://bit.ly/3Vv3FGA
t n s Sc si il S ts si t e is a physiotherapist with a Master’s degree in Sports Physiotherapy from the Institute of Sports Science and ni e sit e n S ut ic S e du ted t e n u s nd ste s de ees u ude nd with Deans awards. After graduating in 2000 Kathryn worked in sports practices focusing on musculoskeletal injuries and rehabilitation. She was contracted to work with the Dolphins Cricket team (county/provincial team) and The Sharks rugby teams (Super rugby). Kathryn has also worked and supervised physios at the annual Comrades Marathon and Amashova cycle races for many years. She has worked with elite athletes di e ent s tin disci lines suc s c e t letics s i in and tennis. She was a competitive athlete holding national and provincial c l u s s i in i t l n t letics nd su li es in nd s passion for sports and exercise physiology. She has presented research at t e nnu l e ic n lle e S ts edicine c n ess in lti e and at South African Sports Medicine Association in 2000 and 2011. She is Co-Kinetic’s technical editor and has taken on responsibility for writing our new clinical review updates for practitioners.
Email: kittyjoythomas@gmail.com
Co-Kinetic Journal 2023;95(January):20-26
Hypermobility Conundrum
References
1. Juul-Kristensen B, Østengaard L, Hansen S et al. Generalised joint hypermobility and shoulder joint hypermobility, – risk of upper body musculoskeletal symptoms and reduced quality of life in the general population. BMC Musculoskeletal Disorders 2017;18:226 Open access http://bit.ly/3TzkePN
2. Liaghat B, Pedersen JR, Young JJ et al. Joint hypermobility in athletes is associated with shoulder injuries: a systematic review and meta-analysis. BMC Musculoskeletal Disorders 2021;22:389 Open access http://bit.ly/3TG05Yu
3. Scheper MC, Juul-Kristensen B, Rombaut L et al. Disability in adolescents and adults diagnosed with hypermobility-related disorders: a meta-analysis. Archives of Physical Medicine and Rehabilitation 2016;97:2174–2187
4. Castori M, Tinkle B, Levy H et al. A framework for the classification of joint hypermobility and related conditions. American Journal of Medical Genetics. t Se in s in edic l Genetics 2017;175:148–157 Open access http:// bit.ly/3EuIBKg
5. Spanhove V, Calders P, Berckmans K et al. Electromyographic muscle activity and three-dimensional scapular kinematics in patients with multidirectional shoulder instability: a study in the hypermobile type of the Ehlers-Danlos syndrome and the hypermobility spectrum disorders. Arthritis Care & Research 2022;74:833–840
6. Engelbert RHH, Juul-Kristensen B, Pacey V et al. The evidence-based rationale for physical therapy treatment of children, adolescents, and adults diagnosed with joint hypermobility syndrome/hypermobile Ehlers Danlos syndrome. American Journal edic l Genetics t Se in s in Medical Genetics 2017;175:158–167 Open access http://bit.ly/3GkT4cN
7. Palmer S, Bailey S, Barker L et al. The effectiveness of therapeutic exercise for joint hypermobility syndrome: a systematic review. Physiotherapy 2014;100:220–227
8. Ingwersen KG, Jensen SL, Sørensen L et al. Three months of progressive high-load versus traditional low-load strength training among patients with rotator cuff tendinopathy: primary results from the double-blind
randomized controlled RoCTEx trial. Orthopaedic Journal of Sports Medicine 2017;5:232596711772329 Open access http://bit.ly/3UDxAvZ
9. Warby SA, Ford JJ, Hahne AJ et al. Comparison of 2 exercise rehabilitation programs for multidirectional instability of the glenohumeral joint: a randomized controlled trial. American Journal of Sports Medicine 2018;46:87–97
10. Treatment of hypermobility – prevention of pain and injuries (webpage). The Danish Rheumatism Association 2015 Open access http://bit.ly/3TA6GDK
11. Liaghat B, Skou ST, Søndergaard J et al. Short-term effectiveness of high-load compared with low-load strengthening exercise on self-reported function in patients with hypermobile shoulders: a randomised controlled trial. British Journal of Sports Medicine 2022;56:1269–1276 Open access http://bit.ly/3EwsBrf
12. Laudner KG, Metz B, Thomas DQ. Anterior glenohumeral laxity and stiffness after a shoulder-strengthening program in collegiate cheerleaders. Journal of Athletic Training 2013;48:25–30 Open access http://bit.ly/3fYVKSE
13. Coussens M, Lapauw B, Banica T et al. Muscle strength, muscle mass and physical impairment in women with hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorder. Journal of Musculoskeletal & Neuronal Interactions 2022;22:5–14 Open access http://bit.ly/3UWtmPH
14. Nicholson LL, Simmonds J, Pacey V et al. International perspectives on joint hypermobility. Journal of Clinical Rheumatology 2022;28:314–320 Open access http://bit.ly/3TCPkWV
15. Malfait F, Francomano C, Byers P et al. The 2017 international classification of the Ehlers–Danlos syndromes. American Journal of Medical Genetics. t Se in s in edic l Genetics 2017;175:8–26 Open access http://bit.ly/3ErryI3
16. Malek S, Reinhold EJ, Pearce GS. The Beighton score as a measure of generalised joint hypermobility. Rheumatology International 2021;41:1707–1716 Open access http://bit.ly/3TAaUeH
17. Assessing joint hypermobility
[webpage]. The Ehlers–Danos Society 2022 https://bit.ly/3uhUddW
18. Simmonds JV. Masterclass: hypermobility and hypermobility related disorders. Musculoskeletal Science & Practice 2022;57:102465
19. Simmonds JV, Herbland A, Hakim A et al. Exercise beliefs and behaviours of individuals with joint hypermobility syndrome/Ehlers–Danlos syndrome – hypermobility type. Disability and Rehabilitation 2019;41:445–55
20. To M, Alexander CM. Are people with joint hypermobility syndrome slow to strengthen? Archives of Physical Medicine and Rehabilitation 2019;100:1243–1250
21. Simmonds JV, Keer RJ. Hypermobility and the hypermobility syndrome. Manual Therapy 2007;12:298–309

22. Spanhove V, de Wandele I, Malfait F et al. Home-based exercise therapy for treating shoulder instability in patients with hypermobile Ehlers-Danlos syndrome/hypermobility spectrum disorders. A randomized trial. Disability and Rehabilitation 2022;1–11
23. Liaghat B, Skou ST, Jørgensen U et al. Heavy shoulder strengthening exercise in people with hypermobility spectrum disorder (HSD) and long-lasting shoulder symptoms: a feasibility study. Pilot and Feasibility Studies 2020;6:97 Open access http://bit.ly/3UzRWWF
24. Liaghat B, Skou ST, Søndergaard J et al. A randomised controlled trial of heavy shoulder strengthening exercise in patients with hypermobility spectrum disorder or hypermobile Ehlers-Danlos syndrome and longlasting shoulder complaints: study protocol for the Shoulder-MOBILEX study. Trials 2020;21:992 Open access http://bit.ly/3AeAH54
25. Gall N, Kavi L, Lobo MD (eds). Postural tachycardia syndrome: a concise and practical guide to management and associated conditions. Springer 2020. ISBN 9783030541644. Buy from Amazon (Print £112.11 Kindle £69.34) https://amzn.to/3hZn4AO
26. Tobias JH, Deere K, Palmer S et al. Joint hypermobility is a risk factor for musculoskeletal pain during adolescence: findings of a prospective cohort study. Arthritis and Rheumatism 2013;65:1107–
1115 Open access http://bit.ly/3ACfVgj
ThePHYSICAL THERAPY 26i Co-Kinetic.com
EVIDENCE BASE FOR INSTRUMENTASSISTED MASSAGE
Commonly occurring soft tissue injuries are associated with excessive tension, overload or repetitive overuse. Be it an acute injury or a chronic overloading stress, no one is immune from injury forever. Inflammation follows an injury and promotes new cell proliferation, during which fibrosis and scar formation ensues. Soft tissue dysfunction and pain can result from reduced tissue elasticity and adhesion development. Within soft tissues, excessive scar tissue can limit perfusion, restricting oxygen and nutrient supply, ultimately interfering with collagen synthesis and regeneration. Subsequently, this can lead to incomplete functional recovery and increased risk of reinjury.
Manual therapy is used to reduce pain, restore mobility, improve movement efficiency and improve motor control. Traditionally, manual therapy includes skilled techniques such as joint mobilisation and manipulation, soft tissue massage, and active, passive and assisted functional movement. Sports massage is pervasive within elite sport and increasingly common at age-group and amateur level. Therapeutic massage is believed to benefit athletes by enhancing performance and improving recovery. It may also promote rest and recovery through biomechanical, physiological and psychological mechanisms. Regardless of this belief, there is limited scientific data supporting improvements in performance and injury prevention with
it or not, our patients now have access to a range of massage therapy tools and if they wish to have a go at doing it themselves, they can. This article discusses the evidence that is available (or not) behind the use of these tools and will enable you, if you wish, to instruct your patients on how and when to use these tools for themselves so that they can benefit most and not practise usage that could be detrimental to their activity or health.
By Kathryn Thomas BSc MPhil
massage (1*,2*). Heterogeneity within the literature makes it challenging to give conclusive answers about the performance benefits of massage. Conversely, sports massage is proven to reduce or prevent delayed-onset muscle soreness (DOMS), which will aid in recovery (2*). Studies have shown that a combination of massage, cold water immersion and the use of pneumatic compression devices are effective in reducing symptoms of DOMS. In some research, active recovery has been shown to be superior to massage in decreasing blood lactate and facilitating recovery (2*). Although active recovery, compression garments and cryotherapy (cold water immersion and contrast water therapy) are beneficial, massage is a ‘powerful’ technique for
assisting recovery from DOMS and fatigue (3*).

Massage has also been proven (in small but significant amounts) to improve flexibility. Flexibility, based on increased range of motion (ROM) at a joint, may be of vital importance for certain individuals depending on their needs, for example a ballerina or gymnast. Bear in mind, though, that too much flexibility in specific sports, such as running, may be detrimental and can increase injury risk (2*).
Research has shown that athletes believe that the benefits of massage include reducing stiffness, improving performance and recovery (4*).
Massage increases plasma endorphin levels, so whether its perceived benefit is due to this or a placebo effect from ‘hands-on’ therapy, the positive
All references marked with an asterisk are open access and links are provided in the reference list.
27 Co-Kinetic.com MANUAL THERAPY
Like
ATHLETES BELIEVE IN THE BENEFITS OF MASSAGE AND IN RECENT YEARS HAVE STARTED TO BUY THE TOOLS SO THEY CAN DO IT FOR THEMSELVES
influence on an athlete’s psychology may be the true value.
Massage is often viewed as a costly, time-consuming luxury; additionally, limited access to a professional therapist can further reduce availability of this therapy. These challenges have been met in recent years by athletes, and the general public, buying into ‘time-saving’, ‘money saving’, ‘convenient’ (anytime, anywhere) tools hoping to achieve the same benefits of traditional massage. The solution seems to have come in the form of ‘self-massage’ with the aid of foam rollers and massage devices/ instruments. The benefits of manual therapy are believed to go beyond the skilled treatment technique to the virtues of touch and physical connection that impact healing. So, can self-massage really do the job, same-same or better, than a massage therapist and could people be doing more harm than good if not using their devices correctly? These devices may be something that frustrate or distress you in practice, potentially losing bookings; however, their use may be something that will have to be accepted – even embraced – to enhance your work in the future. This article will discuss the three most common self-massage devices including percussive massage guns (Theragun® or Hypervolt), foam rolling and instrument-assisted massage tools.

Foam Rolling
Across a variety of sporting disciplines and at home for painful necks and backs, foam rolling (FR) has become common practice. In the sporting arena, FR is regarded as valuable for improving training efficacy and/or competition by accelerating recovery. It may also be promoted to reduce pain and stiffness through massage principles of mobilising and stretching soft tissues such as muscles. As a ‘self-massage’ tool, FR targets specific muscle groups as they are rolled and compressed using the device. Common tools include the foam roller, which come in different sizes and foam densities, as well as various roller massage bars or sticks. Used by both elite and recreational athletes as well as the general public, its popularity stems from its affordability, ease of use, and time-efficiency (‘can do it anytime, anywhere’) combined with its perceived benefit of enhancing performance and recovery.
Mode of Action
The potential effects of FR have been ascribed to mechanical mechanisms comprising a reduction in tissue adhesion and altered tissue stiffness. The enhanced analgesic effects and muscle recovery of FR are thought to stem from neurological pathways, facilitating pain-modulatory systems. FR has also shown physiological responses including increased blood flow and parasympathetic circulation. Improved perceptions of wellbeing and recovery using FR may be a combination of a psychological component, together with increases in plasma endorphins, an activation of the parasympathetic system and/or placebo effect (5,6*,7*,8*).
Clinical Application
The practice of FR is deemed to aid recovery following an intensive bout of physical activity and improve athletic performance. There is, however, no consensus on its benefits, whether it is used before activity (pre-rolling warm-up) or after a bout of exercise (post-rolling recovery). Short-term improvements in flexibility, when using pre-rolling as a pre-exercise warm-up, have shown the largest average effect, with a Hedges’ g of 0.34 which indicates that 62% of the population will benefit from increased flexibility (8*). This small ‘pre-rolling’ short-term benefit in flexibility may be achieved without negatively affecting muscle performance (8*). Research has shown that to achieve the greatest improvement in ROM, FR prescriptions involving 1–3 sets of repetitive rolling over the length of the body part, with a total rolling duration of 30–120 seconds per set is advised (9). If power output is a critical requirement in subsequent exercise or performance, prolonged FR (ie. 5 minutes or more) should be discouraged. Studies show that vertical jump performance remains unchanged after 1 minute of FR, but it is decreased after 5 minutes of FR (5). One should be mindful of this when prescribing FR within a warm-up routine.
Exercise-induced decreases in sprint, jump and strength performance can be lessened with post-rolling. Postrolling has shown accelerated recovery of sprint and strength performance in 62% (Hedges’ g of 0.34) and 58% (Hedges’ g of 0.21) of the population tested, respectively (8*). FR after exercise can facilitate recovery more rapidly than passive recovery (8*).
FR has been shown to be most effective for reducing muscle pain (Hedges’ g of 0.47) (8*). Negative consequences can result from muscle soreness including altered muscle function, reduced athletic performance and reduced training intensity (7*). Enhancing lactate clearance and counteracting DOMS is effective using FR (7*). The type of foam roller, whether it is smooth surfaced, multilevel or a GRID roller all seem to positively influence the recovery rate, with the multilevel and GRID rollers
Co-Kinetic Journal 2023;95(January):27-32 28
ROLLING
PERCUSSIVE MASSAGE DEVICES MAY BE EFFECTIVE IN REDUCING THE EFFECTS OF DOMS AND INCREASING ROM WHEN USED APPROPRIATELY
FOAM
HAS BEEN SHOWN TO BE MOST EFFECTIVE FOR REDUCING MUSCLE PAIN
providing a slightly greater effect (10*,11).
Vibrating foam rollers (VFRs) have recently been developed, which combine the designs of traditional foam rollers and provide local vibration that targets a specific muscle group. Greater improvements in ROM and reduced pain perception using VFR compared with non-vibrating FR have been shown in studies in both healthy active individuals and those with exercise-induced muscle damage (DOMS) (12,13*).
Safety and side effects
A low or zero attrition rate seen in clinical trials indicates an almost complete absence of negative side effects when using FR. Concerns have been raised, however, over the lack of specificity when doing FR – all underlying tissue is mechanically stressed, potentially leading to damage of nerve tissue, receptors, vessels and bones. Care should be taken by athletes and coaches, as well as individuals with diabetes, varices or osteoporosis who may be at greater risk (14).
Conclusion
Pre-rolling may be an effective strategy for short-term improvements in flexibility, without decreasing muscle performance, as well as improving sprint performance. Post-rolling may improve recovery based on performance measures including speed and strength. This may be significant and relevant to an athlete. FR may be endorsed by its positive effects on relieving muscle soreness. The exact mechanism is not fully understood, nor are there measurable physiological benefits with FR. Despite this, the psychological aspect that an individual feels less pain plays an important role in most sports or daily life.
There are vast differences in FR intervention protocols (eg. devices, duration) combined with different exercises, outcome measures, and population groups in the research making it difficult to compare the results. No consensus on optimal FR intervention (ie. in terms of treatment time, pressure, and cadence, etc.) has
resulted from the heterogeneity of study designs. The existing literature does provide some evidence to support the use of FR in sports practice.
Percussive Massage Devices
Hand-held percussive massage treatment has gained popularity in the therapeutic and athletic/sporting arena in recent years. Percussion devices provided by different manufacturers (for example the Theragun® by Therabody and the Hypervolt by Hyperice; Fig. 1) are recommended for therapist use as well as self-massage. Different devices are made to vibrate at different frequencies, up to 53 hertz. A choice of several attachments can be fixed to the device depending on the tissue being treated (ie. soft tissue versus bony tissue). The research on percussive massage application is very limited. It is presumed that using such devices will combine the beneficial elements of conventional massage and vibration therapy. Percussive massage devices are believed to reduce pain, increase blood flow, improve scar tissue, decrease lactate, reduce muscle spasm, increase lymphatic flow, inhibit the Golgi reflex, increase ROM, and improve recovery.

Mode of Action
Following the mechanisms of conventional massage, percussive massage devices are considered to increase ROM through biomechanical (ie. a reduction in muscle compliance), physiological (ie. increased blood flow), neurological (ie. reduction in perception of pain), and psychological (ie. increased relaxation) changes (15*). As assumed with FR and stretching, thixotropic effects may further explain the increase in ROM following percussive massage treatment (16). Similar to FR, percussive massage treatment induces pressure and friction to the treated muscle, skin and fascia, which may lead to reduced resistance to movement by impacting fluid viscosity (16). Vibration therapy increases in ROM have been accredited to a decrease in pain perception (12). Thus, it can be assumed that the changes in ROM achieved with percussive massage

(a) (b)
Figure 1: Image of (a) Theragun® 4th Gen (Therabody; http://bit.ly/3OlTwsZ (b) Hypervolt 2 (Hyperice; http://bit.ly/3Oue9TZ
treatment may be explained by a decrease in muscle stiffness, as well as by changes in pain perception.
Clinical Application
In general there is limited scientific evidence supporting the use of percussive massage devices, even more so in sports performance. Traditional sports massage is proven to provide benefits including improvement in DOMS and acute increases in ROM. However, sports massage is not proven to provide improvements in sports performance (strength, jump, sprint and endurance) (2*). Increases in ROM have been shown when performing whole-body vibration therapy (by standing on a plate) or using a vibrating foam roller for specific muscle groups (12,15*). Compared to conventional massage, vibration therapy has been shown to enhance strength parameters (17). Extrapolating and/or combining the benefits of massage and vibration therapy to percussive massage devices may not be so simple.
Research specific to hand-held percussive massage devices has shown that a 5-minute application during a dynamic warm-up had no effect on performance measured by vertical jump height (18*). These findings are similar to that seen with conventional massage (2*), but differ from the findings on vibration therapy (12), where an increase in strength has been found.
Within a resistance training setting, percussive massage, performed between consecutive sets of bench presses, did not show differences in movement velocity (an optimal indicator of an athlete’s state of physical fatigue indicative of altered neuromuscular qualities). There was,

Co-Kinetic.com MANUAL THERAPY 29
however, an improvement in response to muscular endurance, with a greater number of repetitions per set (19*).
Percussive massage has shown a potential effect in reducing stiffness, restoring muscle compliance and promoting muscle recovery between
proven to reduce the effects of DOMS, potentially facilitating muscle recovery (20*). This is in contradiction to foam roller self-massage performed between sets of lower extremity exercises which may actually hinder performance and increase perceived exertion (21*).
A study by Konrad et al. has shown that following a single, 5-minute percussive massage treatment to the calf muscle, dorsiflexion ROM can be significantly increased (+5.4°) (15*). During this study, no changes in maximum voluntary contraction torque of the plantar flexors was shown. Therefore, percussive massage treatment used in a warmup regimen to optimise flexibility, without losing muscle performance, can be recommended (15*). There are emerging studies showing similar results with increased ROM to the knee and hip following 5 minutes of percussive massage.
Daily percussive massage (5 minutes daily for 1 week) applied across the hamstrings and lower back have shown to significantly reduce pain and increase lower back flexibility. This was, however, a single case study and further research in this area is needed (22*).
Safety and Side Effects
Percussive massage guns should not be used directly over an area of muscle strain or ligament sprain and they should not be used in the vicinity of a broken bone. The vigorous massage action may cause further inflammation, tissue damage or tissue disruption. Haematoma/bruising is commonly reported as a side effect from excessive massage gun use.
Rhabdomyolysis is a serious and potentially life-threatening syndrome credited to the breakdown of damaged skeletal muscle and the release of their contents (specifically myoglobin, potassium and proteases) into the bloodstream (23*). Although there are many causes or risk factors associated with rhabdomyolysis, this should be considered when using a percussive massage device. Safety and education of the public (or user) is imperative – more is not always better. Monitoring proper use, indications and
contraindications can reduce risk of serious side effects.
Conclusion
Hand-held percussive massage devices, such as the Hypervolt, Theragun™ or other muscle gun brands, may be effective in reducing the effects of DOMS and increasing ROM. These devices may not influence performance, as current research shows they are unable to increase muscle activation and force output. It is recommended that individuals can use percussive massage devices as part of a structured warm-up to acutely increase ROM and reduce fatigue without negatively affecting performance. These devices may be useful in a rehabilitation setting to reduce perceived pain and release tight or restricted fascia while simultaneously increasing ROM. This is, however, speculative at present and more research on specific musculoskeletal injuries is required.
Instrument-Assisted Soft Tissue Mobilisation
Tools used to facilitate massage and tissue mobilisation are referred to as ‘instrument-assisted soft tissue mobilisation’ (IASTM). This is a skilled manual therapy intervention used for the detection and treatment of soft tissues. A proposed description is that IASTM is:
“a skilled intervention that includes the use of specialised tools to manipulate the skin, myofascia, muscles, and tendons by various direct compressive stroke techniques” (24*).

A variety of instruments are available, usually made of stainless steel; however, titanium, plastic, quartz, stone and jade can be used. Bevelled edges and contours allow the instrument to conform to different anatomical areas and allow for deeper penetration (25). There are many companies manufacturing IASTM tools such as Graston Technique®, HawkGrips®, RockTape®, Técnica Gavilán®, ERGON®, Functional and Kinetic Treatment with Rehab (FAKTR)®, Adhesion Breakers®, augmented soft tissue mobilisation

Co-Kinetic Journal 2023;95(January):27-32

30
ABOUT THE SAFE USE OF PERCUSSIVE MASSAGE DEVICES IS IMPERATIVE, AS INCORRECT USE CAN CAUSE SERIOUS SIDE EFFECTS Figure 2: (a) GT1 (Graston Technique®; http://bit.ly/3Xfx74K); (b) HG6 – large multi-curve (HawkGrips®; http://bit.ly/3XhsR4I) (c) RockBlades (RockTape®; http://bit.ly/3AweOP2); (d) IASTM tools (ERGON®; http://bit.ly/3tKKJHD); and (e) FAKTR F-1 instrument (FAKTR®; http://bit.ly/3gjuQ7Y) (a) (b) (c) (d) (e)
EDUCATION
or ASTYM®, and Fascial Abrasion Technique™. Each company has its own treatment approach with slightly different instrument designs (Fig. 2).
The ergonomic design of the instrument allows the clinician or user to apply the appropriate pressure throughout the affected area. This mechanical advantage allows deeper tissue penetration, without the compressive forces on the clinician’s thumb, hand and wrist, which can be painful. Soft tissue irregularities, such as tissue restrictions or adhesions, may be more easily detected using these tools as a result of the increased vibratory perception in the hand holding the instrument (26*).
Mode of Action
These instruments are believed to effectively break down fascial restrictions, adhesions and scar tissue. The deep tissue pressure of IASTM application causes an inflammatory response at a cellular level, initiated through micro trauma to the treated area. This results in an increase in fibroblast proliferation, collagen synthesis, maturation and remodelling of unorganised collagen fibre matrix (24*,25). Superficially, the instrument creates skin deformation which stimulates mechanosensitive neurons resulting in a neurophysiological effect, improving local tactile sense and a decrease in pain pressure threshold (27*). Increases in tissue perfusion and the proportion of arteriole-sized blood vessels in the treated area are seen as a vascular response (27*). The mechanism of IASTM is illustrated in ‘Figure 2: Mechanism of instrument assisted soft tissue mobilization on soft tissue injury’ (http://bit.ly/3Oou99T) in Kim et al. (27*).
Clinical Application
When combined with a rehabilitation programme, IASTM treatment can result in positive changes in soft tissue function following tendon injury, including Achilles, patellar and lateral elbow tendinopathy.
l In basketball players with patellar tendinopathy, one session of IASTM per week for 4 weeks resulted in a 23–44% increase in lower extremity functional (LEF) scores (28*).
l In patients with Achilles tendinopathy, significant improvement in LEF scores and more than doubling their walking distance, resulted from one to two sessions of IASTM per week for 8 weeks (27*).
By treating their restrictions, soft tissues extensibility improves with IASTM, and friction from the instrument generates heat which decreases tissue viscosity. Applying two sessions of IASTM per week for 3–4 weeks can significantly improve hamstring and shoulder ROM in athletes (27*). Individuals are at risk of both acute injuries and overuse syndromes when they have restricted joint ROM and reduce flexibility. Whether regular IASTM would translate into injury prevention in the future is unclear at present. The extent of structural and functional changes in tendons or muscles induced by IASTM is not fully understood, nor its effect on future injuries or injury prevention (27*).
The effects of IASTM on pain reduction has been proven in studies involving patients with musculoskeletal conditions as well as across sports including volleyball, triathlon, football and distance running. One to two sessions of IASTM per week applied over 4–6 weeks has been shown to significantly reduce pain and – in some cases completely resolve – the painful symptom (27*).
No single modality, including IASTM, should be administered in isolation during rehabilitation. Functional movements and strengthening to facilitate adaptation and remodelling of tissues should be combined with soft tissue mobilisation techniques. IASTM application should follow the steps described in ‘Table 1: Instrument-assisted soft tissue mobilization (IASTM) treatment program for soft tissue recovery’ (http://bit.ly/3tIrOgC) in Kim et al. (27*).
Safety and Side Effects
Bruising and soreness are the most common side effects that may appear from IASTM, which can be managed using cryotherapy.
Be aware that bruising, together with bleeding, occurs more readily in longer-standing soft tissue injuries. Relative contradictions for the use of IASTM include cancer, kidney dysfunction, pregnancy, rheumatoid arthritis, varicose veins, osteoporosis, lymphedema, fracture, chronic regional pain syndrome, and use of certain medications (eg. anticoagulants, steroids, or nonsteroidal anti-inflammatory drugs) (27*). Absolute contradictions include open wounds, unhealed suture sites, thrombophlebitis, uncontrolled hypertension, skin infection, haematoma, myositis ossificans and unstable fractures (27*).
Conclusion
Owing to its perceived simplicity, practicality and short treatment duration, IASTM has become increasingly popular. For therapists, it also eases the strain on hands, wrists and thumb joints. For individuals at home, they are able to apply a deep tissue self-massage (whether they are doing more harm than good is debatable). IASTM can be effective in improving soft tissue function and ROM in acute or chronic soft tissue injuries, as well as reducing pain. This may be a helpful tool in the field of sports rehabilitation and athletic training. Future research into the mechanisms of IASTM and its effects on tissues other than tendons, including ligaments and muscles, is needed.
Summary
Innovations in manual therapy, including FR, percussive massage devices and IASTM, extrapolate their benefit primarily from sports massage promoting pain relief, increased flexibility and faster recovery. They are popularised for allowing ‘selfmassage’. Apart from perceived ease of use and affordability, these tools may have become more popular over the past 2 years during the COVID-19 pandemic lockdowns. Whether you choose to resent them as they impact on your practice or whether you embrace them, advising or educating your patients on best practice, is your choice. You may already use some

Co-Kinetic.com 31 MANUAL THERAPY
of these tools yourself in clinical practice. Regardless, it is important to note when and where it is best to use the massage devices,
KEY POINTS
considering safety, performance and understanding the general lack of evidence supporting their use across all musculoskeletal injuries.
l The benefits of innovations in manual therapy, including foam rolling (FR), percussive massage devices and instrument-assisted soft tissue mobilisation, have been extrapolated primarily from sports massage where they promote pain relief, flexibility and faster recovery.
l The tools have been popularised for allowing ‘self-massage’, with people buying into the ‘time-saving,’ ‘money saving,’ ‘convenience’ (anytime, anywhere) aspects of the tools hoping to achieve the same benefits of traditional massage.
l FR during warm-up is an effective strategy for short-term improvements in flexibility, without decreasing muscle performance, as well as improving sprint performance.
l Post-exercise FR may enhance recovery and relieve muscle soreness (DOMS).

l There is no consensus on an optimal FR intervention protocol.
l Percussive massage devices may be effective in reducing effects of DOMS and increasing ROM. As part of a structured warm-up, to acutely increase ROM and reduce fatigue, these devices may be effective without negatively impacting performance.
l These devices may not positively influence performance, as current research shows they are unable to increase muscle activation and force output.
l IASTM can be effective in improving soft tissue function and ROM in acute or chronic soft tissue injuries, while reducing pain.
l For therapists, the tools ease the strain on hands, wrists and thumb joints. For individuals at home, they allow the application of a deep tissue self-massage.
l These devices may be used with a lack of specificity where all underlying tissue is mechanically stressed, potentially leading to damage of nerve tissue, receptors, vessels or bones.
l Bruising, haematomas and soreness are common side effects from these treatment tools.
References
Owing to space limitations in the print version, the references that accompany this article are available at the following link https://bit.ly/3XZZynR
RELATED CONTENT
l DIY Sports Recovery [Article] http://bit.ly/3ozbaOV
l Is Massage an Effective Sports Recovery Strategy? [Article] http://bit.ly/3GmAJJ5
DISCUSSIONS
l How do you feel about prescribing and/or guiding your patients through using foam rolling, percussive massage devices or other massage tools at home?
l Do you use IASTM tools in your clinical practice? If so, how effective are they and do patients respond positively to ‘non-hands-on’ treatments?
l Do you feel there is a risk of further injury or harm when patients choose to self-massage with any of these devices?
THE AUTHOR
Kathryn Thomas BSc Physio, MPhil Sports Physiotherapy is a physiotherapist with a Master’s degree in Sports Physiotherapy from the Institute of Sports Science and University of Cape Town, South Africa. She graduated both her honours and Master’s degrees Cum Laude, and with Deans awards. After graduating in 2000 Kathryn worked in sports practices focusing on musculoskeletal injuries and rehabilitation. She was contracted to work with the Dolphins Cricket team (county/provincial team) and The Sharks rugby teams (Super rugby). Kathryn has also worked and supervised physios at the annual Comrades Marathon and Amashova cycle races for many years. She has worked with elite athletes from different sporting disciplines such as hockey, athletics, swimming and tennis. She was a competitive athlete holding national and provincial colours for swimming, biathlon, athletics, and surf lifesaving, and has a passion for sports and exercise physiology. She has presented research at the annual American College of Sports Medicine congress in Baltimore, and at South African Sports Medicine Association in 2000 and 2011. She is Co-Kinetic’s technical editor and has taken on responsibility for writing our new clinical review updates for practitioners.

Email: kittyjoythomas@gmail.com
Co-Kinetic Journal 2023;95(January):27-32
32
WHEN COMBINED WITH A REHABILITATION PROGRAMME, IASTM TREATMENT CAN RESULT IN POSITIVE CHANGES IN SOFT TISSUE FUNCTION FOLLOWING TENDON INJURY
EVIDENCE BASE FOR INSTRUMENT-ASSISTED MASSAGE
References
1. Gasibat Q, Suwehli W. Determining the benefits of massage mechanisms: a review of literature. Rehabilitation Science 2017;2:58–67 Open access http://bit.ly/3rGqwTB
2. Davis HL, Alabed S, Chico TJA. Effect of sports massage on performance and recovery: a systematic review and metaanalysis. BMJ Open Sport & Exercise Medicine 2020;6:e000614 Open access http://bit.ly/3rEDW2p
3. Dupuy O, Douzi W, Theurot D et al. An evidence-based approach for choosing post-exercise recovery techniques to reduce markers of muscle damage, soreness, fatigue, and inflammation: a systematic review with meta-analysis. Frontiers in Physiology 2018;9:403 Open access http://bit.ly/3Gg7wiT
4. Schilz M, Leach L. Knowledge and perception of athletes on sport massage therapy (SMT). International Journal of Therapeutic Massage & Bodywork 2020;13:13–21 Open access http://bit.ly/3DqK3JT
5. Phillips J, Diggin D, King DL et al. Effect of varying self-myofascial release duration on subsequent athletic performance. Journal of Strength and Conditioning Research 2021;35
6. Cheatham SW, Kolber MJ, Cain M et al. The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. International Journal of Sports Physical Therapy 2015;10:827–838 Open access http://bit.ly/2ZXNSIQ
7. Pearcey GEP, Bradbury-Squires DJ, Kawamoto J-E et al. Foam rolling for delayed-onset muscle soreness and recovery of dynamic performance measures. Journal of Athletic Training 2015;50:5–13 Open access http://bit.ly/32SEp6H
8. Wiewelhove T, Döweling A, Schneider C et al. A meta-analysis of the effects of foam rolling on performance and recovery. Frontiers in Physiology 2019;10:376 Open access http://bit.ly/3IsJwuA
9. Behm DG, Alizadeh S, Hadjizadeh Anvar S et al. Foam rolling prescription: a clinical commentary. Journal of Strength and Conditioning Research 2020;34:3301–3308
10. Adamczyk JG, Gryko K, Boguszewski D. Does the type of foam roller influence the recovery rate, thermal response and DOMS prevention? PLoS One 2020;15:e0235195
Open access http://bit.ly/3IBcGbl
11. Cheatham SW, Stull KR. Roller massage: comparison of three different surface type pattern foam rollers on passive knee range of motion and pain perception. Journal of Bodywork and Movement Therapies 2019;23:555–560
12. Cheatham SW, Stull KR, Kolber MJ. Comparison of a vibration roller and a nonvibration roller intervention on knee range of motion and pressure pain threshold: a randomized controlled trial. Journal of Sport Rehabilitation 2019;28:39–45
13. Romero-Moraleda B, González-García J, Cuéllar-Rayo Á et al. Effects of vibration and non-vibration foam rolling on recovery after exercise with induced muscle damage. Journal of Sports Science & Medicine 2019;18:172–180 Open access http://bit.ly/3DwsisJ

14. Freiwald J, Baumgart C, Kühnemann M et al. Foam-rolling in sport and therapy – potential benefits and risks. Sports Orthopaedics and Traumatology 2016;32:267–275
15. Konrad A, Glashüttner C, Reiner M et al. The acute effects of a percussive massage treatment with a Hypervolt device on plantar flexor muscles’ range of motion and performance. Journal of Sports Science & Medicine 2020;19:690–694 Open access http://bit.ly/3rK7bkm
16. Behm DG, Wilke J. Do self-myofascial release devices release myofascia? Rolling mechanisms: a narrative review. Sports Medicine 2019;49:1173–1181
17. Lee CL, Chu IH, Lyu BJ et al. Comparison of vibration rolling, nonvibration rolling, and static stretching as a warm-up exercise on flexibility, joint proprioception, muscle strength, and balance in young adults. Journal of Sports Sciences 2018;36:2575–2582
18. Kujala R, Davis C, Young L. The effect of handheld percussion treatment on vertical jump height [abstract]. International Journal of Exercise Science: Conference Proceedings 2019;8 Open access http://bit.ly/3gg9bNZ
19. García-Sillero M, Jurado-Castro JM, Benítez-Porres J et al. Acute effects of a percussive massage treatment on movement velocity during resistance training. International Journal of Environmental Research and Public Health 2021;18:7726 Open access http://bit.ly/302TCBg
20. García-Sillero M, Benítez-Porres J, García-Romero J et al. Comparison of interventional strategies to improve recovery after eccentric exercise-induced muscle fatigue. International Journal of Environmental Research and Public Health 2021;18:647 Open access http://bit.ly/31whxtu
21. Kerautret Y, Guillot A, Di Rienzo F. Evaluating the effects of embedded selfmassage practice on strength performance: a randomized crossover pilot trial. PLoS One 2021;16:e0248031 Open access http://bit.ly/3dnrThC
22. Patel R, Patel A. Effect of Theragun on the improvement of back flexibility: a case study. IOSR Journal of Dental and Medical Sciences 2020;19:15–16 Open access http://bit.ly/3tIVMAZ
23. Chen J, Zhang F, Chen H et al. Rhabdomyolysis after the use of percussion massage gun: a case report. Physical Therapy & Rehabilitation Journal 2021;101:pzaa199 Open access http://bit. ly/3lEPAqf
24. Cheatham SW, Baker R, Kreiswirth E. Instrument assisted soft-tissue mobilization: a commentary on clinical practice guidelines for rehabilitation professionals. International Journal of Sports Physical Therapy 2019;14:670–682 Open access http://bit.ly/31E8J4g
25. Lambert M, Hitchcock R, Lavallee K et al. The effects of instrument-assisted soft tissue mobilization compared to other interventions on pain and function: a systematic review. Physical Therapy Reviews 2017;22:76–85
26. Ge W, Roth E, Sansone A. A quasiexperimental study on the effects of instrument assisted soft tissue mobilization on mechanosensitive neurons. Journal of Physical Therapy Science 2017;29:654–657 Open access http://bit.ly/3rGtozK
27. Kim J, Sung DJ, Lee J. Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: mechanisms and practical application. Journal of Exercise Rehabilitation 2017;13:12–22 Open access http://bit.ly/3y3rWZE
28. Kim DH, Kim TH, Jung DY et al. Effects of the Graston technique and selfmyofascial release on the range of motion of a knee joint. Journal of the Korean Society of Physical Medicine 2014;9:455–463 [in Korean] Open access http://bit.ly/3UMr45W
Co-Kinetic.com 32i MANUAL THERAPY
Name the Pain!
Okay dear readers, it’s musculoskeletal quiz time. Sit back, relax, put your phones away (no cheating now) and see if you know the answers to the following questions:
1. What is the most common musculoskeletal problem worldwide?
2. Which musculoskeletal problem is the leading cause of activity limitation and absenteeism from work?
3. Which musculoskeletal problem causes 40% of absence from sickness in the NHS?
4. Which musculoskeletal condition is so topical it even affects Superheroes?
Yep – the answer to all the above is our old friend low back pain (1*). Low back pain even affected Spiderman in the movie No Way Home where at the height of the big action climax, the plot stops in its tracks so the two main characters can have a long back-andforth (ha ha) about their ageing spines.
Low back pain is now such an issue that it is considered a major global health problem. To add insult to injury (literally), low back pain has even teamed up with our other topical global health issue, Covid 19, to wreak even more havoc. Studies show that low back pain increased during the lockdowns experienced over the last few years (2*).
Considering the scale of the problem, one would think that humankind would have devoted a large part of our brilliant brain power to devising effective treatments for this debilitating condition. Yet although in 2022 you can check your washing machine cycle via your smartphone, your chances for effective treatment of low back pain are still abysmally slim. Musculoskeletal medicine often seems stuck in the dark ages, with the internet full of misleading and unhelpful information and your local GP having neither the time, knowledge nor energy to engage with this problem that often has a multifactorial cause.
Our Wrongheaded View of Low Back Pain: Why Your Back Isn’t ‘Out’ and Your Disc Hasn’t ‘Slipped’
One of the reasons that treatment
MANUAL THERAPY AND LOW BACK PAIN

Back pain is the most common musculoskeletal condition worldwide and current research has revolutionised how we think about it. However, the old ‘beliefs’, which can actually be very detrimental, are slow to die out. Reading this article will bring your knowledge of back pain up to date and show you how to integrate your manual therapy and massage skills into the biopsychosocial model of treatment to obtain the best possible results for your back pain patients.
By Rachel Fairweather BA, AOS, LMT
for low back pain is so woefully inadequate is that many medical and therapeutic approaches are working on an outdated model of the causes of musculoskeletal pain.
Medics, the public and many manual therapists have been indoctrinated consciously or unconsciously with a predominantly structural paradigm to explain musculoskeletal pain. In short, in this simplistic view, tissues get damaged, or a joint or bony structure gets misaligned, and an ensuing pain sensation is reported to the brain. So, muscles and ligaments tear and fray, discs herniate thus pressing on nerves, and joints wear down producing problematic bony spurs and uneven surfaces. Furthermore, improper alignment of our bones and joints leads to nasty painful symptoms. Anteriorly or posteriorly tipped pelvises, unequal length legs and bones that are ‘out’ need to be
put back into proper position to relieve pain. Right? Wrong.
The biggest newsflash in pain biology research over the past decade is this:
The amount of pain you experience does not necessarily relate to the amount of tissue damage sustained. There can be tissue damage without pain and pain without tissue damage.
Yes, that’s right. You can be riddled with bulging discs, rotator cuff tears and crumbly joints but be in no pain whatsoever. Conversely you can have real, excruciating, and debilitating pain without a single iota of damage to any of your muscles, ligaments or joints.
We will now consider a few ‘strange but true’ facts from research studies.
All references marked with an asterisk are open access and links are provided in the reference list
33 Co-Kinetic.com MANUAL THERAPY
MASSAGE HAS A POSITIVE EFFECT FOR LOW BACK PAIN, ESPECIALLY WHEN COMBINED WITH SELF-CARE AND EXERCISE
THERE CAN BE TISSUE DAMAGE WITHOUT PAIN AND PAIN WITHOUT TISSUE DAMAGE
1 Tissue Damage Without Pain Seems to Be Reasonably Common
Studies have shown that 52% percent of those with no low back pain have bulging discs and 27% a disc protrusion (3*). Another study found that 32% of asymptomatic subjects had ‘abnormal’ lumbar spines when examined by MRI (4*).
2 Findings from MRIs and X-rays Are NOT Related to the Pain Experienced in Musculoskeletal Complaints
Studies have shown that the MRI scans of the spine of patients with sciatic pain exhibit no relationship between symptoms and degree of disc displacement or nerve root entrapment, leading the authors to conclude, “magnetic resonance imaging is unable to distinguish sciatic patients in terms of the severity of their symptoms” (5).
Other studies comparing MRI scans of both those in pain and asymptomatic subjects found that many people (32%) had crumbly, funny looking, discs a-bulging, and bone-spur-ravaged ‘abnormal’ lumbar
spines. Which according to the doctors should mean they were in terrible pain. Except they weren’t. On the other hand, 47% of the sample had prize winning ‘normal’ lumbar spines. Which obviously meant they were pain free, right? Err, no. They were all back pain sufferers. Epic fail for the orthopaedic approach there (4*).
This knowledge has now filtered its way through to primary care. NICE (National Institute for Health and Care Excellence) guidelines recommend that your GP does NOT routinely carry out MRI scans on patients with low back pain. Although this is a positive move with orthodox medicine moving away from a structural approach it is one generally scorned by the uninformed public (“Can you believe the GP didn’t even offer me an X-ray?”).
3 Structural Deviations Are Generally of Little Consequence
The widely accepted view in manual therapy that postural and structural deviations can lead to musculoskeletal pain is based on scanty evidence. Lederman convincingly presents a body of research substantiating the fact that there is no relationship between postural and structural factors such as leg length difference, pelvic asymmetry, spinal curves and low back pain (6). He concludes:
“The lack of association between postural structural factors and low back pain has also important implications for what we aim to achieve and for our choice of techniques and exercise used to manage the condition. We can no longer justify the use of manual techniques to readjust, correct or balance-out the misaligned structure.”
4 Pain Without Tissue Damage
Just as there can be tissue damage without pain, there can also
be pain without tissue damage or structural abnormalities. Most of low back pain (85–90%) is now classified as ‘non-specific’; ie. there is no identifiable structural cause such as herniated discs, spondylitis, or irritated facet joints. This feature of pain without tissue damage is particularly true in chronic or persistent pain conditions and is known as ‘central sensitisation’.
Central sensitisation is where the central nervous system can “change, distort or amplify the experience of pain in a manner that no longer reflects the noxious stimuli from the periphery”(7). In other words, the spinal cord and brain can act like a faulty amplifier that turns up the volume of the pain – the client is in (real) pain even though there is no longer any injury or damage. This persistent pain sensitisation has been shown to be a feature in many of the client conditions that are staples of the massage therapist’s clinic including chronic low back pain (8).
Central sensitisation is somewhat like the oversensitive car alarm that keeps getting triggered even though there is no danger or damage to the car. In cases of central sensitisation, we need to make sure as bodywork therapists that we are addressing the faulty and over sensitised alarm system and not just focussing on the tissues.
No Brain, No Pain!
So, if the pain condition is not always coming from damage to the tissues, what exactly is going on? It is now clear that all pain is a perception of the brain rather than always being an accurate representation of what is happening at the tissue level. Thus, the sensation of pain can be heavily mediated by a variety of factors including emotional state, previous experience, expectations, sense of control over the pain condition and other social and contextual factors.
This reconceptualisation of the root of chronic pain has vindicated the paradigm known as the biopsychosocial model (a bit of a
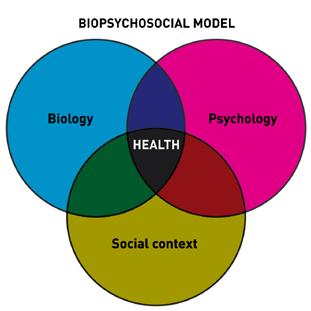
34 Co-Kinetic Journal 2023;95(January):33-41
“The brain decides whether something hurts or not – 100 % of the time with no exceptions” Lorimer Mosely (9)
Figure 1: Biopsychosocial model of pain
mouthful and hence commonly abbreviated to BPS) as first proposed by the psychiatrist George Engel way back in the late 1970s (10). The biopsychosocial model (Fig. 1) sees pain as a combination of biological, psychological, and social factors. This paradigm contrasts strongly with the still prevailing biomedical view that sees pain as a result only of biological factors such as disease, abnormalities of structure or tissue damage.
Recent advances in brain imaging studies have shown that pain is indeed heavily influenced by our brains, vindicating not only the biopsychosocial model but the central tenet of Eastern medicine, most folk medicines, and complementary therapy. Psychosocial factors including beliefs, feelings, emotional state and sense of control over our circumstances have a much larger role than previously believed in whether we experience pain or not. The BPS model is now becoming widely accepted in medical and scientific circles as the most relevant model for the treatment of chronic pain (11).
Implications for the Massage and Manual Therapist
So as the dedicated manual therapist, what are our chances for the successful treatment of both acute and chronic low back pain? Both clinical experience and research suggest that massage can be extremely effective in the treatment of chronic musculoskeletal pain conditions. Several systematic reviews have found that massage has a positive effect for low back pain, especially when combined with selfcare and exercise (12,13*). Current NICE guidelines recommend massage for low back pain when combined with exercise.
However, for effective results, it is vital that we manual therapists grasp the fundamental concept that pain is not just about an ‘issue in the tissues’, any more than it is due to our clients anteriorly tipped pelvis, barely visible scoliosis, or minimal ‘leg length’ difference. Manual therapists can no longer justify techniques that are mainly aimed at correcting errant structures while blithely ignoring the elephant in the room that is our client’s

stress levels, nasty divorce or the fact that their back pain worsened during the existential threat of the pandemic. It may well be the fact that successful manual therapy interventions work more through reducing central sensitisation than healing damaged tissues or correcting errant pelvises.
The methodology for the manual therapist needs to go beyond that of a purely hands-on approach to one that places the biopsychosocial model of pain firmly central in our model of treatment. This can be challenging to therapists who often see the ‘verbal’ portions of treatment (assessment and prescribing selfcare) as an afterthought, rather than significant opportunities to assist healing.
Effective therapy for low back pain relies not just on the therapist’s beloved magic hands but the application of other interpersonal skills during the assessment and self-care phases of client contact. The assessment process and choosing of appropriate self-care are both extensive skill sets in themselves and are significant areas for the therapist to attend to in order to improve their success in treating low back pain.
Top Tips for the Manual Therapist Working Within a Biopsychosocial Model
Our own clinical experience suggests that the manual therapist has a far greater chance of achieving success in treating chronic pain if the following factors are considered.
receive (15*); as one reviewer put it, “Successful interactions between patients and their practitioners lie at the heart of medicine” (16*).
This is just as true for our work with musculoskeletal pain, as studies have shown that positive therapeutic alliance ratings between physical therapists and patients are associated with improvements of outcomes in low back pain and increased treatment satisfaction for clients with musculoskeletal problems (14*,17*). Really? Can our client’s bad back be improving just because they like us? Is being smiley more important than soft tissue release? Research suggests it is certainly a factor and points to the importance of the practitioner–client bond as part of a competent and truly holistic healing process.
Thorough and Holistic Assessment Process
Taking time to take time with your clients in the assessment process will pay off handsomely in terms of results. Kaptchuk et al. found that the quality and length of the initial interaction with a practitioner was strongly correlated with improvement measures (18*). Clients receiving placebo acupuncture for irritable bowel syndrome were randomly divided into three groups: ‘waiting list condition’, ‘limited interaction’ and ‘augmented interaction’. In the waiting list group, the patients had no interaction with the practitioner. In the ‘limited interaction’ the acupuncturist introduced himself and said that ‘he knew what to do’, after which the
Strong
Therapeutic Relationship Between Practitioner and Client
Whether you are a medical doctor, physical or manual therapist, talk therapist or acupuncturist, a key component of facilitating wellness in your client is this therapeutic relationship or alliance (Fig. 2). This refers to the sense of “collaboration, warmth, and support between the client and therapist” (14*). Research shows that if you have a good relationship with your doctor, this means that you are likely to have an improved healthcare outcome regardless of what treatment you

35 Co-Kinetic.com
MANUAL THERAPY
Figure 2: A strong therapeutic relationship between practitioner and client improves healthcare outcomes
FINDINGS FROM SCANS ARE OFTEN NOT RELATED TO
IN MUSCULOSKELETAL COMPLAINTS
conversation ceased and the treatment began. In the ‘augmented interaction’ the patient and the practitioner had a 45-minute conversation before the treatment began where the practitioner expressed empathy, asked the patient about the symptoms, and told the patient that he had very positive experiences with treating these symptoms.
The results showed how powerful the interaction with the therapist is independent of what happens in the actual treatment. Patients in the ‘augmented interaction’ group had a significantly greater improvement and more pain relief when compared with the group exposed to the ‘limited interaction’ of the confident but somewhat abrupt practitioner. The latter, in turn, had significantly more improvement than the waiting list group with no human interaction other than the sham acupuncture.
n uence s c s ci l ct s in the Pain Condition Make sure that your assessment process considers any potential psychological or social factors that may be contributing to the client’s pain experience. Yellow flags are indicators of psychosocial factors that may be involved in perpetuating the pain issue. In acute situations, unaddressed yellow flags may mean that the pain is more likely to become chronic. In existing chronic pain conditions, these elements can be a barrier to recovery.
Identifying yellow flags can help focus treatment by emphasising self-care and education measures in addition to the hands-on work. As we have seen, in cases where there are many psychosocial factors at work, the issues are not just ‘in the tissues’.
A great way for remembering the major yellow flags is the ‘ABCDEF and W’ soundbite (19*). Gentle and open questions around the areas below will help you to tease out the role that psychosocial factors may be playing in perpetuating your clients pain condition.
A ttitudes – What is the client’s attitude towards the current problem? Is the client optimistic that they will get better with appropriate help and are they expecting to return to normal activities? Or is the client fearful and catastrophising about the future?
B eliefs – Unhelpful beliefs about the pain can be absorbed from friends, the media or misinformed professionals. The most common misguided belief is that the patient feels they have something serious causing their problem such as cancer or arthritis. Others include the fear that the condition will lead to permanent disability, that they should rest or not work.
Enquiring into the stress of dealing with legal issues can be very revealing.
D iagnosis – There is an emerging body of evidence that what clinicians say to clients may help to create chronic pain situations. For example, complicated diagnoses, terrifying visuals of crumbling spines or popped discs are likely to make the client feel hopeless, out of control and reliant on an expert. Ask the client what they have been told and what it means to them. Try and steer the client towards more accurate and empowering information that emphasises their own role in returning to health
E motions – Clients with high levels of stress or other emotional difficulties such as ongoing depression and/or anxiety states are more likely to have chronic pain issues. It is important that these are not overlooked in the quest to find the soft tissue issues or structural causes of the pain.

F amily – It is interesting to ask about the role of the immediate family; both under-supportive and overprotective attitudes can play a role.
C
ompensation – Is the patient awaiting payment for an accident or work-related injury? This can lead to perpetuation of the pain condition that is not conscious or deliberate.
W ork – Understanding your client’s work situation can be very helpful. On the one hand, the lack of a meaningful occupation can exacerbate pain states leading Gifford to state that “getting people back to work or keeping them in work if at all possible, should be a major goal of physiotherapy” (19*). On the other hand, many clients can end up trapped in jobs where they feel unsupported, bored or bullied which also leads to persistence of pain conditions. The self-employed are not exempt and are often the worse culprits for driving themselves into the ground and then getting felled by bad backs, chronic headaches or repetitive strain injury. Ring any bells anyone?! In these situations, encouraging the client to take a holiday or proactive measures to reduce workload can be very helpful.
Language
Be aware of how you talk to your client and the ideas you are planting as the ‘expert’. Labels such as herniated disc, arthritis or scoliosis can sow the seeds of permanent disability and pain into your client’s psyche by exacerbating
36 Co-Kinetic Journal 2023;95(January):33-41
Figure 3: Acronym for the Jing method multimodal approach to treating musculoskeletal pain.
THE PAIN EXPERIENCED
the tendency to catastrophise. Be realistic but reassuring about the potential route out of pain.
Self-Care Measures
Many clients in pain feel totally disempowered. Giving exercises or other recommendations to help them feel back in control is key to recovery. Prescribing effective self-care is a skill in itself and it is important to realise that self-care is not just about rehabilitation or physio-style exercises. The intelligent manual therapist will be looking to a biopsychosocial model for clues for effective self-care including teaching basic breathing exercises or meditation techniques. A case of more therapy and less resistance-band exercises!
Cross-Referral
For some clients, catastrophising and other fear-related beliefs can be helped with simple reassurance and education. Others may need a referral to a talk therapist – CBT in particular has been found to be helpful in painrelated conditions.
Education, Education, Education Help put your client back in the driving seat. Educate them about the biopsychosocial model and the multifactorial causes of musculoskeletal pain and reduce their fear of feeling out of control or dependent on the expert.
Reduction of Nociceptive Input with Massage Techniques
Manual therapy techniques are probably best directed towards reducing any potential nociceptive input that may be contributing to maintaining central sensitisation (rather than attempting to correct perceived structural abnormalities). In our own clinical practice we use a combined approach with fascial work, precise trigger point therapy, acupressure and stretching. Research has shown that trigger points contribute to central sensitisation – for example in whiplash, myofascial trigger points serve to perpetuate lowered pain thresholds in uninjured tissues. Additionally, it appears that lowered pain thresholds associated with central sensitisation
can be immediately reversed, even when associated with long-standing chronic neck pain.
Summary of the Jing Method Multimodal Approach to Treating Musculoskeletal Pain: HFMAST
Over the past 30 years of clinical practice, we have developed a multimodal soft tissue approach to treating all chronic musculoskeletal pain. In addition to a targeted consultation, the techniques that form the cornerstone of the Jing method can be summarised by the acronym HFMAST (Fig. 3) (20).
H – The use of heat or cold.
F – The use of fascial techniques, both direct and indirect methods.
M – Treating muscles with precise trigger point therapy, specifically treating ALL the muscles around an affected joint to release trigger points.
A – Acupressure, treating relevant acupressure points.

S – Stretching, using stretching techniques such as static, proprioceptive neuromuscular facilitation or active isolated stretching.
T – Teaching the client self-help strategies that lie within the massage therapist’s scope of practice. This would include, for example, self trigger point treatment, simple breathing techniques, stretching or mobilisation exercises.
Significantly we recommend that all these techniques are integrated within a 50-minute treatment and that practitioners work on a treatment approach of 1–6 weekly sessions with the aim of reducing pain and increasing function by week 3, thereafter lengthening time between treatments.
Massage and Manual Therapy Techniques: The Jing Method Low Back Pain Protocol
Our book and online courses outline a comprehensive protocol for working
Figure 4: Crossed-hand stretches
with all types of non-specific low back pain. Significantly, as outlined above, our approach involves the use of different modalities combined within treatment as exemplified in the HFMAST approach.

Below I have presented a shortened version of this protocol with some of the key areas that need to be addressed – for the full protocol please see Chapter 12 of our text Massage Fusion: The Jing Method for the Treatment of Chronic Pain (20) or our online low back course (available from www.jingmassage.com)
Heat Application and Preparatory Work
Heat: before working on the affected area, apply moist heat in the form of a heating pad over the low back and buttock area. Heat can also be applied using large hot stones – use two stones either side of the back and a large one on the sacrum.
Fascial Techniques
Crossed-hand stretches: these can be performed in many areas on the low back – for example, with one hand on the sacrum and one over the spine, or over the quadratus lumborum area on both sides. Place your crossed hands adjacent to one another in the area to be released – they should be a few inches apart at this point. Sink down until you have a sense of being on the deep fascial layers that runs around
37 MANUAL THERAPY Co-Kinetic.com
RECENT BRAIN IMAGING STUDIES SUPPORT THE USE OF THE BIOPSYCHOSOCIAL MODEL OF PAIN
and through the muscles. Then put a stretch on this tissue so you have a sense of tension between your two hands, like a piece of material being stretched to a barrier. If you tune in with your sense of listening touch, after a while you will start to feel the sensation of the tissue starting to move
beneath your hands. Make sure you maintain the stretch and ‘follow’ the tissues until you feel the sense of tissue release described in the fascial chapter – this whole process takes around 3–5 minutes so you will need to be patient! Repeat the crossed-hand stretches on anywhere that is needed (Fig. 4).
Muscle Techniques and Treatment of Trigger Points Broad Work to the Low Back
Single forearm massage: working with the forearms is a great way to save your hands and is a wonderful sensation for your client. Stand in horse position at side of table, knees bent, spine relaxed but straight. Shift your weight onto the leg nearest the low back area. Use the soft medial part of your forearm to work into your client’s low back, making sure your wrist is floppy and not tense. Shift weight onto your upper leg for a light return stroke. Continue gradually working deeper into the musculature layer by layer. Cross to the opposite side of the table to work the other side (Fig. 5).
Apply more heat: this is also a great time to apply more heat with some dynamic hot stone work. Use any hot stone techniques you know to work into the low back tissues (Fig. 6).

Find and release relevant trigger points: remember the object in this section is to find and release the key trigger points that are the primary cause of the client’s pain pattern. Key trigger points should be treated 2–3 times within the session. You will be
treating all the muscles around the joint for trigger points.
Treating Erector Spinae
Stand at the head of table in tai chi stance: starting from the upper back, muscle strip the entire muscle using your thumbs or supported fingers. You are feeling for taut bands and trigger points as you do this work and listening to any communication from your client that you have hit a relevant trigger point. Treat any trigger points you find with static pressure for 8 to 12 seconds until pain releases (you will need to communicate with your client to assess this). You should go back and treat any key trigger points relevant to the client’s pain pattern for 2 to 3 times per session. Start next to the spine and work from the head to the sacrum in strips (like methodically ‘mowing the lawn’). You will need at least three strips to cover the whole width of the erector spine group (Figs 7 and 8).
Forearm or other power effleurage: to finish use deep forearm effleurage or other power effleurage strokes, really focussing on opening up the low back and quadratus lumborum region.
Treating the Quadratus Lumborum (QL)




There are several steps to treating trigger points in this muscle effectively:
1 Treat transverse process attachments of QL.
To treat the transverse process attachments of QL your focus needs to be underneath the erector spinae group which lies
38
Co-Kinetic Journal 2023;95(January):33-41
Figure 7: Trigger point work to erector spinae
Figure 8: Trigger point work to erector spinae
Figure 9: Treating transverse processes of the quadratus lumborum (QL)
Figure 5: Single forearm massage
Figure 6: Applying heat with hot stone techniques
superficial to this muscle. To treat the transverse process attachments, stand face on at the side of table and apply pressure at a 45° angle between the iliac crest and 12th rib. Hold static pressure and treat any trigger points you find for 8–12 seconds. Explore this small space by orienting your fingers slightly towards the 12th rib or iliac crest. Your focus is underneath the bulk of the
erector spinae towards the midline.
Always use static pressure first. If the muscle is not too tender you can add some slight cross fibre friction working in one direction only (Fig. 9).
2 Treat 12th rib attachment.
Turn your body so you are in tai chi stance facing the head. Use thumbs to hook underneath and treat the insertion point of QL on the 12th rib. Use static pressure first, treating any trigger points, then use cross fibre friction if appropriate (Fig. 10).
3 Muscle strip the entire QL muscle.
Turn your body so you are facing the feet in tai chi stance. Muscle strip the side of the QL using thumbs or supported fingers, working towards the iliac crest (Fig. 11).
4 Treat the inferior attachment point on iliac crest.
Now treat the lower portion of QL which attaches under the iliac crest. Make sure you push your thumbs under the bone and work from lateral to medial with static pressure and cross fibre friction (Fig. 12).
Deep effleurage to QL with palm of hand from superior to inferior: in forward tai chi stance work down the side of the QL with the heel of the hand, gently pushing into the iliac crest at the end to stretch out the muscle.
Treating Gluteal Muscles and Lateral Rotators






Opening up the gluteal muscles and lateral rotators: over the drape, in horse or forward tai chi stance, lean the soft part of your forearm into the glutes. Make sure you have a broad contact area with the whole of the forearm – you are not digging into the tissues with your elbow. Wait in this place and hold for the muscles to release. Your pressure is straight down towards the table. Repeat so that the whole gluteal area is covered (Fig. 13).
Fingertip friction to edge of sacrum: using supported thumbs or fingers,

gluteal region
TRIGGER
39 MANUAL THERAPY Co-Kinetic.com
Figure 10: Treating 12th rib attachment of QL
Figure 13: Opening up the gluteal muscles
Figure 11: Muscle stripping of the QL
Figure 12: Treating the iliac crest attachment of the QL
Figure 14: Fingertip friction to the edge of the sacrum
Figure 15: Treating trigger points in
POINTS CONTRIBUTE TO CENTRAL SENSITISATION
work the edge of the sacrum with cross fibre friction in one direction only. This addresses any trigger points that may be found near the attachments of gluteus maximus. Cross to the other side of the table to work the other side of the sacrum (Fig. 14).
Treating Trigger points in the gluteal region: now search for and treat trigger points over the entire gluteal region. As the glutes are very thick, use a ‘listening forearm’ to explore the region first. Start about an inch down from the iliac crest, sinking into the glutes with your forearm and identifying any tight areas. When you find these, treat as trigger points, and wait for a release. Work out towards the side of the hip, then place your forearm on the next line down and work out in a similar manner. Repeat until the entire gluteal region is covered. Make sure you address the inferior aspect near the ischial tuberosity where trigger points are likely to lurk (Fig. 15).
For more specific trigger point work: go back to any tight areas and use supported thumb or fingers to treat trigger points. You can also do cross fibre friction in one direction only: work with the fibre then cross fibre (Fig. 16).
Treating the Piriformis
Soft tissue release of the piriformis: extend this manoeuvre into a soft tissue release stretch of the piriformis. Use the heel of your hand or a soft
fist into the piriformis area and lock into the muscle while stretching the leg away from the midline (pulling a pint). Hold for 2 seconds, release the stretch and repeat, treating the entire region with this ‘lock and stretch’ technique. If you need to do more specific work you can use a supported thumb and lock and stretch in the same way. Always do broad work first before specific work (Fig. 17).
Practise this stroke in rhythm: l lock l stretch (count: 1,2) l release l replace l repeat.
Finish with deep forearm effleurage: to the gluteal region or broad release work over drape.



Supine
Mobilisations: either kneeling on the table or in standing tai chi stance, fold your clients knees to their chest and gently rock their low back with small rocking movements towards and away from the head. Your hands rest lightly on their knees. Use a rate of about one rock per second. If the client has a very sore low back do about 5–10 mobilisations then check in about comfort levels (Fig. 18).
References

1. The global burden of low back pain
[website]. International Association for the Study of Pain 2021, July 9 Open access https://bit.ly/3h1RlP5
2. Papalia GF, Petrucci G, Russo F et al. COVID-19 pandemic increases the impact of low back pain: a systematic review and metanalysis. International Journal of Environmental Research and Public Health 2022;19(8):4599 Open access https://bit.ly/3Fspd0W
3. Jensen MC, Brant-Zawadzki MN, Obuchowski N et al. Magnetic resonance imaging of the lumbar spine in people without back pain. The New England Journal of Medicine 1994;331:69–73 Open access https://bit.ly/3P8Affg
4. Savage RA, Whitehouse GH, Roberts N. The relationship between the magnetic resonance imaging appearance of the lumbar spine and low back pain, age and occupation in males. European Spine Journal 1997;6(2):106–114 Open access https://bit.ly/3UIXWvS
5. Karppinen J, Malmivaara A, Tervonen O et al. Severity of symptoms and signs in relation to magnetic resonance imaging findings among sciatic patients. Spine 2001;26(7):E149–154
6. Lederman E. The fall of the posturalstructural-biomechanical model in manual and physical therapies: exemplified by lower back pain. Journal of Bodywork and Movement Therapies 2011;15(2):131–138
7. Lederman E. Therapeutic stretching: towards a functional approach. Churchill Livingstone 2013. ISBN 978-0702043185 (Print £35.10 Kindle £34.99) Buy from Amazon https://amzn.to/3F9uPvI
8. Roussel NA, Nijs J, Meeus M et al. Central sensitization and altered central pain processing in chronic low back pain: fact or myth? Clinical Journal of Pain 2013;29(7):625–638
9. Lorimer Moseley G. Painful yarns. Dancing Giraffe Press 2008. ISBN 978-0980358803 (Print £22.00

40 Co-Kinetic Journal 2023;95(January):33-41
Figure 17: Soft tissue release of the piriformis
Figure 18: Supine mobilisations of the low back
Figure 16: Specific trigger point work to the gluteal muscles
Kindle £5.9) Buy from Amazon https:// amzn.to/3P3IM2K
10. Engel GL. The clinical application of the biopsychosocial model. The American Journal of Psychiatry 1980;137(5):535–544
11. Gatchel RJ, Peng YB, Peters ML et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychological Bulletin 2007;133(4):581–624
12. Furlan AD, Imamura M, Dryden T et al. Massage for low back pain: an updated systematic review within the framework of the Cochrane Back Review Group. Spine 2009;34(16):1669–1684
13. Kumar S, Beaton K, Hughes T. The effectiveness of massage therapy for the


KEY POINTS
treatment of nonspecific low back pain: a systematic review of systematic reviews. International Journal of General Medicine 2013;6:733–741 Open access https://bit.ly/3W905lp
14. Ferreira PH, Ferreira ML, Maher CG et al. The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Physical Therapy 2013;93(4):470–478 Open access https://bit.ly/3VCpDYq
15. Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physicianpatient interactions on the outcomes of chronic disease. Medical Care 1989;27(3 Suppl):S110–127 Open access https://bit.ly/3h0BmRA
16. Kelley JM, Kraft-Todd G, Schapira L et
l Back pain is the most common musculoskeletal problem worldwide.
l Treatment is often inadequate as many medical and therapeutic approaches are working on an outdated model of the causes of back pain.
l Tissue damage without pain is reasonably common.
l Findings from scans are not often related to the degree of pain experienced.
l 85–90% of low back pain is now classified as ‘non-specific’; ie. there is no identifiable structural cause.
l Central sensitisation is a condition of the nervous system that is associated with the development and maintenance of chronic pain.
l Recent brain imaging studies support the use of the biopsychosocial (BPS) model of pain.
l Psychosocial factors have a much larger role than previously believed in how we experience pain.
l Effective therapy for low back pain relies not just on the therapist’s hands but the application of other interpersonal skills during the assessment and self-care phases of client contact.
RELATED CONTENT
l Low Back Pain: Moving Back To Basics [Article] https://bit.ly/3Wv7mwj

l How to Unpick Postural Locks [Article] https://bit.ly/3qDYDY5
l Low Back Pain During Pregnancy: Physiological versus Pathological Back Pain [Article] https://bit.ly/3pQm2rl
l Classification Systems: A Review of Low Back Pain Care [Article] https://bit.ly/2BSZKKn
l Low Back Pain: The 10 Minute Assessment [Article] https://bit.ly/3R2nxyE
DISCUSSIONS
l Discuss the ways in which a structural model of low back pain is now considered outdated.
l What is your understanding of the biopsychosocial model of pain? Can you think of some examples of clients whose pain may be affected by psychosocial factors?
l In what ways can you adapt your assessment and self-care for clients to work more from a biopsychosocial approach?
al. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2014;9(4):e94207 Open access https://bit.ly/3VRymWg
17. Hall AM, Ferreira PH, Maher CG et al. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Physical Therapy 2010;90(8):1099–1110 Open access https://bit.ly/3VBLdME
18. Kaptchuk TJ, Kelley JM, Conboy LA et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 2008;336(7651):999–1003 Open access https://bit.ly/3VC8uhg
19. Gifford L. Perspectives on the biopsychosocial model - part 2: the shopping basket approach. In Touch, The Journal of the Organisation of Chartered Physiotherapists in Private Practice 2002;99(Spring Issue):11–22 Open access https://bit.ly/3utXN4M
20. Fairweather R, Mari MS. Massage fusion: the Jing method for the treatment of chronic pain. Handspring Publishing 2014. ISBN 978-1909141230 (Print £35.00 Kindle £33.25) Buy from Amazon https://amzn.to/3iHQnIn2
THE AUTHOR
Rachel Fairweather BA, AOS, LMT is author of the best-selling book for passionate massage therapists – Massage Fusion: The Jing Method for the treatment of chronic pain.
She is also the dynamic co-founder and Director of Jing Advanced Massage Training (www.jingmassage.com), a company providing degree level, hands-on and online training for all who are passionate about massage.
Rachel has over 30 years experience in the industry working as an advanced therapist and trainer, first in New York and now throughout the UK. Due to her extensive experience, undeniable passion and intense dedication, Rachel is a soughtafter international guest lecturer, writes regularly for professional trade magazines, and has twice received awards for outstanding achievement in her field.
Rachel holds a degree in Psychology, a Postgraduate Diploma in Social Work, an AOS in Massage Therapy and is a New York licensed massage therapist.
Email: info@jingmassage.com Website: www.jingmassage.com Twitter: https://twitter.com/JingMassage Facebook: https://www.facebook.com/ JingMassageTraining
41 MANUAL THERAPY Co-Kinetic.com
How to Target Niche Markets for Search Engine Optimisation

We all know by now that simply having a website for our business is not going to bring clients flocking to our doors. However, it is a necessary good start. The next thing to do is to optimise your website and web pages so that it can be not only found by search engines but also score the appropriate points to be ranked high up in the results list. After all, when do you ever scroll on to the second page of search results? This article is an introduction to how web pages can be optimised to rank highly in the results of niche searches – ie. people looking for very specific information about certain conditions or treatments in their local area. These are exactly the kind of people we want to find our websites because they are already half way to becoming a customer, so what’s not to love?
By Chris Dann, founder of Market Your Clinic Online
Optimising Webpages
For Niche Searches
Although the majority of people looking for a physical therapist will search online for the type of therapist they’re looking for, eg. physiotherapist, osteopath, etc, many will search for the individual condition they are looking for help with, eg. ‘sports injury clinic’, ‘running injury’, ‘treatment for carpal tunnel’ and so on. Some people might also search for the sort of treatment they are looking for, eg. ‘shockwave treatment near me’ or ‘kinesio taping’.
Although most websites are generally naturally optimised for our primary service (eg. physiotherapist), we stand to gain many more potential patients if we also appear in these niche searches of people who are looking for a particular treatment that we offer, or a particular condition that we treat. This is particularly true if we have a specialism, such as pre-/post-natal physiotherapy, neurophysiotherapy, and so on.
Although fewer people overall are searching in this way (there are far fewer people searching for ‘prenatal physiotherapy’ than simply for
‘physiotherapy’, for example), there are big advantages to appearing high up in Google results lists for these niche searches. Firstly, the potential patient is already very clear about what they want, so are far more likely to go with a local specialist than they are to shop around, and secondly there are far fewer therapists optimising for these niche searches in the first place, so we face far less competition to rank highly for them in the search results if we optimise our web pages correctly.
Data-Driven Optimisation
Although we can simply create content around anything we feel we would like to treat and hope for the best, we can use our efforts far more efficiently if we have some data around the searches people are making.
Firstly, we need to know what niche searches patients are making There is no point creating content to optimise our website for ‘tendonitis’ when very few people are using this term to search for local treatment, and over 50 times as many people are searching for treatment for ‘plantar fasciitis’ (as is the case).
Some conditions rank relatively high in results lists on national (known as informational) searches but much lower on results lists for people actually searching for treatment. ‘Tennis elbow’,
for example, ranks relatively high in searches for general information but significantly lower when compared to other conditions on results lists for people actually searching for local treatment. Of course, if you are a recognised expert in a particular niche and your patients are willing to travel a significant distance to see you, the national search volumes become more relevant.
Using this data firstly to choose the most fertile conditions or treatments to optimise for, we also need to know the language people use to search for treatment. For example, people searching for ‘sports injury’ treatment almost exclusively search for a ’sports injury clinic’, whereas people with back pain or fibromyalgia search far more often for a ‘specialist’, and those with plantar fasciitis search for simply ‘treatment’.
We can use this data to inform the way we word our pages. A webpage called ‘Back Pain Specialist in Bristol’ will, all other things being equal, get more traffic than one called ‘Back Pain Treatment in Bristol’, and so on, and knowing these nuances is both important and powerful.
Creating Niche Pages
Now that we know the conditions or treatments we want to optimise for and
Co-Kinetic Journal 2023;95(January):42-44 42
FIRSTLY, WE NEED TO KNOW WHAT NICHE SEARCHES PATIENTS ARE MAKING
the words people are actually typing into search engines to look for them, we are ready to create niche-specific pages, or blog posts, to target those terms. Search engine optimisation (SEO) is, of course, a very big area and there is much that goes into creating a webpage about a condition or treatment that successfully ranks highly in the list of search results. However, we can give some general principles.
First of all we need to remember that we are writing pages to target users who are looking for local treatment, ie. people typing in ‘back pain Bristol’, ‘back pain near me’, and so on (Fig. 1) (Box 1). So the webpage should not only discuss the condition or treatment, but also make it very clear that treatment is available from your clinic, and the location of that clinic. Google will then be far more likely to return that page in the search results when it recognises that it is local treatment that the user is searching for. Of course, this is good practice in any case from the point of view of conversion (the process of encouraging people to move from simply browsing your website to becoming paying clients), as we should be adding frequent calls to action on the page inviting the user to download a helpful resource, book an appointment and pointing out the location of our clinic and any other selling points we have (such as easy parking, evening appointments and so on).
Secondly, we then aim to explain the condition and its treatment in a target of approximately 1000–1500 words. A mistake many practitioners make here is to dive straight into their own treatment without answering wider questions the searcher might have. For a condition page, begin by discussing the condition and treatment options in very general terms. For example, a back pain page might include a brief discussion of treatment options including everything from painkillers to surgery. We then move on to how our particular treatment fits into this scheme and how it works, before moving on to Why choose us? material.
Exactly what to discuss on the page will depend on the condition. Here again, search data gives us a very
Box
1:
Terms that send Google into local mode
With search terms such as ‘specialist’ and ‘clinic’ we have an advantage, as these are local trigger terms which generally send Google into local mode and return a map with local results in the same way as if we had specified a location or typed ‘near me’.
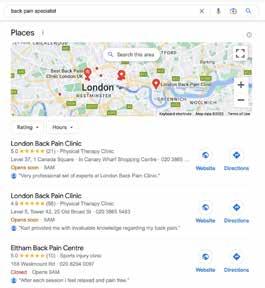
large helping hand. When we look at informational search data, we find the concerns and questions people have around any given condition or treatment. For example, the largest informational search volumes around ‘hip pain’ are ‘injections’ and ‘yoga’ (Fig. 2). Although these are not services we necessarily offer, by including sections on the page such as Do I need an injection for my hip pain? or Can yoga help with my hip pain? we are far more likely to be in step with the questions that the searcher is actually asking, and therefore far more likely to convert them into a booking.
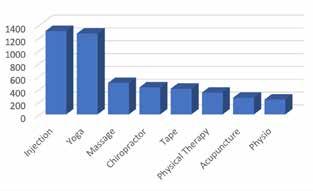
Lastly, ensure that it is clear to the user and to Google that you – a qualified medical professional – are the one putting your name to this information. This has been important since Google’s so-called Medic update in 2018, aimed at preventing people from finding medical advice online from those not qualified to give it, and selfdiagnosing or self-treating incorrectly. You can do this by simply creating an About the author or Medical review section at the end of the page, stating who you are, your qualifications and title, and a link to your practitioner page if you have one (Fig. 3).


The Role of Local Authority Authority is the missing piece of the jigsaw puzzle which is so frequently overlooked in SEO.
In a hypothetical situation, let’s say that there are several local clinics, all of which have identical websites and are the same distance away from the person making the search. How will Google decide which one to put at the top of the search results? The answer is authority, or in simple terms how important or popular Google considers you to be (Fig. 4).
A variety of factors contribute to
ENTREPRENEUR THERAPIST 43 Co-Kinetic.com
Figure 2: UK Monthly Searches for ‘hip pain’ plus another term
Figure 3: With any medical information it is crucial to demonstrate to Google that it has been written or reviewed by a qualified professional
Figure 4: Your domain authority is a large factor in your SEO rankings
Figure 1: Adding a location, the words ‘near me’, or certain terms such as ‘specialists’ put Google into local mode and return a map with local results
Case Study
In Spring 2022, we created condition pages for an osteopathic clinic to target searches for back pain, sciatica, scoliosis and sports injury.
After creating targeted pages for these conditions in March, we measured local SEO rankings over the next 3 months to see the difference. We saw a jump in the results rankings of the niche search terms that we were targeting into the top spots on Google, where previously the listings hand been buried down on page 3 or 4 or not listed at all before the optimisation. Most striking was a jump from 38th place to 1st place for ‘back pain near me’, a key search phrase.
The clinic in question already had a reasonable domain authority, which allows condition page creation to move the SEO needle more strikingly than for low-authority domains. However, the authority of your website should generally increase over time as you continue to publish useful content, and keep building your reputation and inbound links locally.
A physical therapy SEO specialist can help you decide on the best strategy for your clinic, which may include condition page creation, blogs and other content creation, and proactive authority building.
building authority. Originally, authority was based simply on the quantity of inbound links to your website, so a website with 500 other websites linking to it was considered higher authority than a website with only 50. This led to a proliferation of paid ‘spam links’, and Google has since become more and more sophisticated.
Links are still important, but Google is looking for relevance, either in terms of location (eg. a link from the local press), or subject (eg. a link from a running magazine to your running injury page) and is more likely to discount irrelevant links, or even penalise for them if it considers your link profile to look overly ‘spammy’.
Building quality inbound links to your site takes time and effort, and involves forming genuine relationships with other local organisations who will be prepared to refer to you or to link to your site. The key is to always be offering value and something of use. This might be in the form of useful blog posts, advice sheets and factsheets, discounts to relevant organisations, sponsoring local events, or giving your time for free – say for a talk at a local running club – in exchange for a link back from their site. Good link building is inseparable with relationship and profile-building in general. It requires proactivity, and the attitude of giving in order to get.
One great way to do this is to offer free events and webinars – such as the talk in the example above – to anyone who’s interested. This serves to raise
your profile as the local expert who runs free events to help others, widens your net for potential patients – as people are far more likely to share and talk about your free event than about your clinic – and creates great link-building potential, as it is in the interest of local media, blogs, etc, to get the word out about your event, all with a link back to your site.
This is exactly why the Co-Kinetic Clinic Growth subscription gives you all the tools, including the presentation itself, to help you organise and run these type of events as their importance cannot be overstated when it comes to both generating new customers and also building an authoritative SEO presence.
Evidence-Based Marketing Course
Co-Kinetic have asked me to write an SEO course module for their upcoming Evidence-Based Marketing (EBM) course, due to launch in the first quarter of 2023. This full EBM course will be a 14 week, hands-on, online course involving teaching as well as having time set aside for implementation, and will take you through the whole process of building an audience, nurturing trust and then culminating in running an event, designed specifically to generate new customers. You will be supported throughout the course with ready-touse content at every level.

This article forms the basis of SEO modules to be included in this course. In those modules I’ll take you through
Case Study Results
Search term Ranking in Google search results list March 2022 June 2022 (pre-SEO) (post-SEO)
Back pain near me 38 1 Sciatica treatment near me 50+ 3
Back pain West Hampstead 11 2
Back pain Hampstead 47 5
Scoliosis physical therapy near me 50+ 7
Scoliosis treatment near me 50+ 10 Back pain 50+ 14
You can see the full case study at https://bit.ly/3BiN94s
SEO of your website from the ground up, the latest developments in how SEO will work in 2023, and search data for various conditions and therapies so you know not only how to optimise your website, but the most fruitful terms to optimise it for. We will provide you with articles and content which we will then help you optimise for your chosen specialities/skill set. To register your interest for the course visit https://bit.ly/3uBNpYB.
RELATED CONTENT
l How to Use Content to Make Your Business More Findable on the Web [Article] https://bit.ly/3Bo6ykq
l Practical Ways to Use Content to Promote Yourself and Your Business [Article] https://bit.ly/373sGS6
l Physical Therapy Marketing Strategies: Being Seen, Being Found and Being Heard [Article] https://bit.ly/3kFxogi
l How to Get More Patients Without Being Salesy [Article] https://bit.ly/2sRgRvr
THE
AUTHOR
Chris Dann is the founder of Market Your Clinic Online and is unreasonably passionate about digital healthcare marketing. He builds websites, carries out SEO optimisation, has written for Osteopathy Today, works with Physio First and Co-Kinetic and is the author of the Manual Therapy SEO Reference Guide. When not promoting clinics, he enjoys the gym, modern art, playing guitar and eating hamburgers.
Email: chris@marketyourcliniconline.com Website: https://www.marketyourcliniconline.com/ LinkedIn: https://www.linkedin.com/in/cpjdann/ Facebook: https://www.facebook.com/ marketyourcliniconline
44
Co-Kinetic Journal 2023;95(January):42-44
Social Media Success for Physical Therapists
 By Tor Davies, physiotherapistturned Co-Kinetic founder
By Tor Davies, physiotherapistturned Co-Kinetic founder
The Problem
Social media causes a significant problem for most of the health professionals that I encounter, if for no other reason than the fact that it haemorrhages valuable time which could be spent on a whole host of much more productive business growth (or even personal) activities.

Added to the fact that fewer than 1 in 20 practitioners can say that it materially boosts customer numbers, it makes it extremely questionable why so many people spend so much time on it.
Most physical or manual therapists I meet fall into one of the following three camps when it comes to social media.
1. Do nothing and hope it will eventually go away.
2. Post sporadically, without knowing exactly why they’re doing it.
3. Post a lot, but most of it being poor quality posts.
The end result tends to be the same for everyone – zero engagement, zero business generation and a lot of wasted time, effort and money, because even if you’re not paying anyone else to do it, YOUR TIME IS NOT FREE, meaning it’s a real cost to you.
Let’s be honest, social media is a time-sucking vortex for pretty much everyone (me included). According to data from our time/cost calculator on our website, the average post (that’s
In this article we tear away the cloak of secrecy that social media often seems to hide behind and break down what’s important and what’s not, when it comes to your social media business pages. We look at what social media can help you to achieve, but also what is realistic to expect from your efforts and highlight seven key areas for you to focus on. If you don’t approach social media with a strategy, you will carotid-arterystyle haemorrhage precious time, for absolutely nothing in return. Even if you hate social media and feel it has no place in business, this article is worth a read. This article has been written as supporting material for my Social Success for Physical Therapists course which will launch in January 2023 (more details at the end).
just ONE post) takes 40 minutes to create and schedule. There’s coming up with the idea, finding royaltyfree images (or paying for a photo library subscription), creating the post image, writing the post copy and then scheduling it to be posted. It’s a lot of work.
For most people, you could treat a new patient (and write up the notes) in the time it takes to create a new social media post, and most practitioners I know would rather be doing that any day compared to creating social media content. So, sorry to be blunt but WTF???
Even if you only post 2 or 3 posts a week, that’s still costing you between £100 and £200 a week in time (use our calculator at https://bit.ly/3UStcbC to see exactly what it’s costing you both monthly and annually).
I’m willing to bet just about anything that there’s not a single other business activity that people spend
so much time on that delivers such a poor return on investment. Can you suggest a worse one?
And if you’re one of those people who spins out a self- or businesspromoting post in 5 minutes and is sitting there right now, feeling rather smug, just hold your horses my friend, we’ll talk more about that in a minute.
But first, let’s talk about ‘engagement’ because that’s what drives which content is shown to whom, and that is determined by the ‘Almighty Algorithms’.
45 Co-Kinetic.com
ENTREPRENEUR THERAPIST
EXECUTING A WELLSTRUCTURED SOCIAL MEDIA STRATEGY CAN DELIVER A WHOLE HOST OF GREAT MARKETING BENEFITS
Image credit: Antlii
ALGORITHMS GOVERN WHO IS SHOWN WHAT CONTENT ON EACH SOCIAL MEDIA NETWORK
Engagement
Every social network has its own proprietary algorithm which is a closely guarded secret and, for the most part, everyone (except perhaps Mark Zuckerburg and friends) is taking educated guesses at understanding them.
We explore this in more detail in my upcoming Social Success for Physical Therapists course (See Overview of the Course box at the end) but for the purposes of this article, here’s what you need to know. In short, the algorithms govern who is shown what content, on each respective social network.
Engagement is essentially defined as a click, a reaction, a comment, a tag or the ‘first prize’ – a conversation. It’s an umbrella term for a measure of how much people are interacting with your social content.
The more engagement a post gets, the more people (who are similar to or exhibit similar behaviour to the audience that’s already engaging in it)
are shown the post.
As a consumer of content, the goal of the algorithm is to serve you the most relevant content possible, with the best chance of keeping you scrolling down your feed, and ultimately, hopefully spending money (because if people don’t spend money, advertisers will stop advertising and the social networks will be forced to take a long hard look at their business models or risk going out of business).
The more people that engage with your posts, the more people will be shown them (although this is by very small increments), and this goes for both your followers but also people with similar interests to your followers – this is called ‘organic reach’ – it’s happening organically (naturally) without you having to pay for it. But don’t get too excited, unfortunately it’s not all party, party, party.
The trouble is that the number of people who will be shown your post in the first place is, well, very, very small, and yes this includes your own followers. It’s estimated that as few as 1–5% of your followers, will ever be shown one of your posts, and if they do happen to engage with it, it’s more likely that they will also be shown your future content, which means your posts will generally circulate within the same small group of people all the time.
So you need to be very clear in the understanding that if you think that just because you publish a post on your social network’s business page all your followers will automatically see it, this
is wrong – because actually they won’t.
This is also why it’s physically impossible to ‘bombard’ people with too many posts, the algorithm simply won’t let it happen, because if you get bored and you stop scrolling, that’s no use to them. The job of the algorithm is to keep putting content in front of you that will firstly keep you on the social network and secondly encourage you to engage with it, and as you can imagine, you’re up against A LOT of competition. For example, on average, there are 4.75 billion items shared by Facebook users each day and an average of 1,500 posts that are eligible to appear in a Facebook user’s feed each day, so that algorithm has to do some major filtering!
To make it harder, algorithms are constantly changing and evolving, attempting to work out their kinks (because they’re not perfect either) and make the user experience better and better, which means it’s a constant battle to experiment with content, analyse results and try new strategies. And I don’t need to tell you that most small business owners do not have the will, resources or the capacity to be able to do this.
Box 1: Social Media Statistics
l 4.6 billion people are on social media (58% of the world’s population)
l Facebook is still the most widely used social network with 2.94 billion users worldwide
l 84% of people aged 18–29 are on the social networks; 81% of those aged 30–49; 75% of those aged 50–65; and 45% of those aged 65+
l 75% of internet users use social media to research brands
l 71% of users who have had a positive experience with a brand on social media are likely to recommend that brand to friends and family
l 55% of people learn about new businesses on social media

l 78% of people are willing to buy from a company after having a positive experience with them on the social networks
Sources: Oberlo (1) and Sprout Social (2)

The alternative is to throw money at it and pay to promote your content to get it in front of fresh and relevant audiences, and this is something that can be incredibly useful when it comes to growing your email list (without doubt the single most important marketing activity that every small business should be doing). But at the same time, it also needs to be done with strategy, which is something we talk about in practical terms in the Social Success for Physical Therapists course. It’s all about figuring out the 20% of inputs you need to fulfil, in order to get the 80% of the outputs.
In my opinion and my own personal experience, there are dramatically diminishing returns in investing heavily in trying to achieve organic engagement with your social media. It is the holy grail, and unless you have the strength, resilience and courage of Indiana Jones, or the budget of companies like Disney, or Amazon, it’s just not a fight worth fighting.
46 Co-Kinetic Journal 2023;95(January):45-50
So Why Bother with Social Media at All?
You’re probably asking yourself, why on earth is someone who provides social media as a subscription service (ie. me), being so damning about social media?
Well, even if you can fit what you know about marketing on a postage stamp, you’ll probably be aware that, on the flip side, there is also a very compelling case for (and strong evidence to support), that executing a well-structured social media strategy can deliver a whole host of great marketing benefits.
Here are a few.
1. Most of your clients will be on at least one of the social networks.

2. People are increasingly looking for businesses on the social networks.
3. Social platforms and social media can help you:
l connect with your customers and prospects and learn what they’re looking for;
l increase awareness about your brand and the services you provide;
l grow an audience (with incomparable targeting
accuracy);
l build your email list (again with great specificity);
l generate sales;
l establish authority and credibility;
l strengthen relationships and build trust; and
l get customer feedback.
There are some stats in Box 1 to support these claims.
My main issue is the disproportionate amount of time people invest in trying to achieve these goals. In my view, all small businesses should be focusing on getting the main boxes ticked as quickly and as cost-effectively as possible, and then get on with doing your real job.
So what are the social media goals that small businesses should be aiming for?


Small Business Social Media Goals
We drill into each of the following goals in much greater detail in our Social Success course but here’s a quick summary of those main goals.
Box 2: 12 Qualities of Good Social Media Content
We aim to deliver as many of these qualities as we can, with each of the social media campaigns we create under the Co-Kinetic subscription: 1. Offers value to the reader/follower 2. Is engaging and encourages conversation 3. Incorporates a range of different formats including video/live video 4. Helps you build an audience 5. Utilises hashtags (and correctly) – this is more relevant in some social networks
6. Is specific, ie. targeted to a specific audience 7. Includes content that’s both personal (conversational) and workthemed 8. Uses content that people interact with like polls, quizzes, giveaways, freebies 9. Incorporates humour to make it entertaining 10. Helps to educate
Builds authority and credibility 12. Fits with your personal and professional ethos
FYI that’s exactly the framework we use to create the Co-Kinetic social media content we produce, so if you want a shortcut to this process, there’s one right there (more details at https://www.co-kinetic.com/social-media)
7 Goals of Your Social Media Investment


1. Deliver an authoritative, regularly updated social media presence 2. Publish the most engaging content possible, as cost-effectively as you can 3. Be guided by a clear strategy 4. Be consistent in your efforts 5. Invest in proactive and reactive engagement 6. Set realistic goals and measure/analyse 7. Use social media to build an audience
Deliver an Authoritative, Regularly Updated Social Media Presence

The primary goal of any business-related social media profile is to represent you and your business as authoritative, professional and current. As the stats in Box 1 demonstrate, people do look for businesses on the social networks, so it basically becomes the equivalent of an informal version of your website. It gives you the opportunity to demonstrate authority and knowledge and to connect with both existing clients as well as prospective ones. It’s like an informal complement to your more formal, official website. A constant supply of fresh, educational, authoritative content keeps you looking up to date and relevant. Pepper this with the odd personal post (which will always get better engagement because the social networks prioritise personal interactions) and it’s job done.
Publish the Most Engaging Content
Possible, as Cost-Effectively as Possible
Time and money are of the essence with every small business, and there’s no way with the best will
47 ENTREPRENEUR THERAPIST Co-Kinetic.com
11.
in the world that most have enough of either resource to create a regular, consistent supply of social media, with the best chance of optimising for organic engagement ‘by hand’, and this is exactly why I created my subscription offer (Box 2). It is hands down the most cost- and time-effective solution bar none.

The Co-Kinetic subscription is certainly not the only social media offering out there, I’m sure there are many options to choose from, but I’m fairly confident in guaranteeing that we’re the only peerreviewed and data-led solution (our inbuilt social media scheduling tool is posting thousands of posts a month, all of which we collect engagement data for). This makes it a hugely valuable source of information when it comes to developing new content. Our campaigns include a wide range of different media types (animations, videos, memes, infographics, value-added education resources, etc) with the added benefit of a range of posts linking to pre-built email lead collection pages designed to help you build your email list, all of which we take care of for you (and one of the most powerful ways to use the social networks to help you build
And the fact that all the social media content is pre-loaded into an inbuilt social media scheduling tool, means it’s not only the quickest solution out there, but also the simplest solution for people with a dislike for technology. As far as I’m aware there isn’t an equivalent social media offering that can compare, and especially not for the price, which is
the equivalent of around one patient treatment a month for most physical therapists. We discuss more about content types in the next section.
Be Guided by a Clear Strategy Strategy comes in everywhere, from choosing the right distribution of content types, posting at the optimal times, posting consistently enough (this is an important algorithm trigger) and not drowning your page in yawn, yawn self-promotional content. There’s also the issue of which social networks to post on (and why), and the role that both organic and paid social media can play in helping you get an ROI from your efforts. All of these aspects are important to understand when deciding on a social media approach, and we cover them in detail in our Social Success course.
Be Consistent in Your Efforts
Consistency is one of the key markers the algorithms look for when deciding whether to widen the exposure of your content or not. If you post 25 posts one month and then only one the next month, in the algorithm’s view you can’t be relied upon to post consistently good content, so they won’t stick their algorithmic necks out to promote your content. You have to post a consistent number of posts, on a regular basis.
Invest in Proactive and Reactive Engagement
Basically this means making sure you reply when people engage with your content (that’s the reactive engagement part) and the proactive engagement means getting involved in relevant social media groups and pages, where your prospective customers are and sharing helpful information, resources and tips. It’s super-important that this isn’t ‘salesy’ engagement, the focus must be for the benefit of the community you’re engaging with. This is one of the most effective ways of growing your organic engagement and if you know where to focus your efforts, this
is where you should invest what small amount of time you have (more in the course).
Set Realistic Goals and





Measure/Analyse
Social media analytics is a minefield. There’s so much data it’s hard to focus on what’s important, which is why we’ve created a spreadsheet template with a difference in our Social Success course. At the end of the day engagement relative to your audience size and the reach of your posts is probably the most important thing to track, so you can use it to watch the trends in your content over time. In the course we’ll look at some of the most popular, fan-busting profiles, and you might be surprised to see that when everything is made relative, even though those profiles are getting thousands of engagements, there’s actually a consistent pattern when you compare them relative to each other.
Use Your Social Networks to Build an Audience
By this I’m referring to a well-targeted, local audience of people with the greatest chance of requiring your services or visiting your clinic. One of the most underused and yet valuable powers of the social networks, is to help you build targeted audiences of people with specific interests by using high value pieces of content that benefits your audience, while at the same time helping you to grow your email list.
Combine this with a regular, consistent email nurture programme (regular emails that add value to your email list and DO NOT sell), is (or should be) the backbone of your marketing plan. Followers on social networks are an audience, but as we’ve seen by how few of them are shown your social media posts, they’re not an audience you’re in control of. An email list, on the other hand, is an audience you can control communications with. Remember, you’re not going to spam them, you’re going to focus on nurture emails, which add value. Their primary purpose is for the good of the reader. Then when you do need to call them
48
Co-Kinetic Journal 2023;95(January):45-50
ENGAGEMENT IS THE SECRET SAUCE TO ATTRACTING ATTENTION FROM THE ALLPOWERFUL ALGORITHMS
into sales action, they’re primed and warm and feeling good enough about your business to want to engage.
Without an audience, you have a very limited capacity to sell. You can’t invite them to attend education events, you can’t sell vouchers, you can’t make offers, you can’t promote a clinic membership scheme, you can’t tell them about new equipment or services you’re offering, or the new therapist that’s joined you. Basically without an email audience, you have no route to market. In reality, the health of your email list is a key indicator of the health of a business.
Each of these 7 components above represent core modules in our Social Success course and we cover them in much more detail there.
And lastly, for this article at least, let’s quickly talk content – what content works and more importantly what content doesn’t.
Engagement-driving content
As we’ve learnt, engagement is the secret sauce to attracting attention from the all-powerful algorithms, and with regards to what content works the best, and what content works the worst, the clue is in the name (Box 3).
Social networks are called ‘social’ networks for a very good reason, they’re motivated and driven by two-way communications. What’s the definition of the adjective social? “Relating to, devoted to, or characterised by friendly companionship or relations”.


So here’s a little experiment, go and review the last 20 posts on your most frequently ‘posted to business page’ social feed and assign each of them to one of the 6 categories below. Be honest with yourself, even if it looks bad (because you’re only cheating yourself if you’re not), if it mentions you, your business or your services in any way, it goes straight into category 6, no questions asked.
Social Media Content Categories
Note that we’re talking about content ‘categories’ here, not media types – it could be a video, a reel, an image, an animation – that doesn’t matter, what matters is the message/intention of
the post.
1. Entertainment/fun/humour (absolutely absent of self-promotion/ sales pitches), eg. memes, jokes, funny videos – pure entertainment posts.
2. Inspiration, eg. quotes, motivational, etc.
3. Education/value-adding, eg. helpful resources, blog posts, links to helpful sites, infographics, educational animations, relevant news etc – absolutely no sales pitch or business promotion included.
4. Email lead generation-focused, eg. designed to collect email address, it could be to offer a high value piece of content, a competition, a prize draw, any kind of activity that encourages a sign-up by email.
5. Connection/engagement-driven/ interactive – something that promotes the opportunity to have conversation or creates a social connection – quizzes could be included here or equally posts which specifically encouraging someone to engage (comment/tag/share, etc).
6. Self/business promotional –something about you, your team, services you offer, classes you run, discount offers, testimonials – something that is specifically designed to promote you/your business and/or drive sales.
In reality, a post can be a combination of several of these ‘categories’ –you could have a funny entertaining post/meme, with a serious message, or a useful educational download.
But the point is that 90% of your content should
Box 3: Co-Kinetic’s ENGAGED formula
We design our social media campaigns around our ENGAGED formula:
E N G A G E D
Entertains and educates
Nurtures conversation and trust
Grows your influence and authority
Attracts customers
Galvanises action
Enriches lives
And most importantly it’s
Driven by data
ENTREPRENEUR THERAPIST Co-Kinetic.com
IT’S WORTH HAVING A GOOD, REPUTATIONBOOSTING SOCIAL MEDIA PROFILE, BUT IT’S NOT WORTH SPENDING ANYTHING MORE THAN AN HOUR OR TWO A MONTH ON IT
49
be falling in categories 1–5, and the reality is probably more likely that 90% of your posts currently fall into category 6. Now consider what is friendly or companionable about one-directional self-promotional posts? How many of your posts seek to entertain, engage in conversation, or add value through education?
We all have those so-called friends who all they do is talk about themselves. They never ask after you or your family (or dog in my case!), your business or things that are important to you. After a while you get wise to it, and you probably start going out of your way to avoid those people. Well, that’s basically what a social media page packed full of selfpromotional posts is like. It’s a one-way conversation that’s going nowhere but down.
The Final Word (for Now)
Hopefully this article has brought some clarity about what you’re looking to achieve through your social media
pages. The crux of it all, is that it’s worth having a good, reputation-boosting social media profile, but it’s not worth spending anything more than an hour or two a month (at the absolute most), to achieve, because if it’s anything more than that, you won’t get a return on your investment. It is 100% worth using paid social media to build targeted email lists, and if this was all you created a social media profile to achieve, you could do a lot worse! If you’re interested in learning more about the Social Success course when it goes live, you can register your interest here:
References
1. Mohsin M. 10 Social media statistics you need to know in 2022 (webpage). Oberlo 2022, 12 September Open access https://bit.ly/3Y9afV2




2. Cover L. 7 Statistics that prove the importance of social media marketing in business (webpage). Sprout Social 2021, 17 June Open access https://bit.ly/3FGYVbD
3. Memon M. 46 Expert tips for boosting organic social growth (webpage). Databox 2020, 28 October Open access https://bit.ly/3W5gV4F
RELATED CONTENT
Should I Use Social Media for my Physical Therapy Business? If So, Why and How? [Article] https://bit.ly/3sLpe7J
Why nobody ever engages with your Facebook posts, why it's impossible to ‘bombard’ your page followers with too many posts, and what the Jan 2018 Facebook news feed changes mean to your business Facebook page https://bit.ly/2CQqcc5
l 25 Ways To Grow Your Email List [Article] https://bit.ly/3jR6NKR
THE AUTHOR
l Setting the scene
l Is social media worth it?
l The algorithm and why it matters
l Organic versus paid engagement
l Setting your goals
l Defining your strategy
l What makes ENGAGING content
l Strategies for increasing organic reach
l Measuring your progress
l Why and how to build an audience using paid social media
l FAQs – which networks, how often, hashtags, authenticity, getting the right content mix, optimising your profile

The taught component of the course will be around 2–3 hours in length, delivered by me (Tor Davies, physio-turned Co-Kinetic founder), with an additional 2 hours required for practical implementation. It will cost in the region of £50–99 (to be decided) and as always, there will be a discount for existing subscribers (inc. SMA members).
Tor Davies began her professional life training as a physiotherapist at Addenbrookes Hospital, Cambridge, UK. She went on to complete a BSc in Sport & Exercise Science at the University of Birmingham while also achieving a WTA international tennis ranking. After graduation she worked in marketing with a London agency and then moved into medical journalism where her passion for publishing was born. At 27 she established sportEX medicine, a quarterly journal for physical and manual therapists. With a passion for technology as well as publishing, Tor’s leadership grew sportEX into the Co-Kinetic journal and website which included a more collaborative, royalty-based form of publishing as well as a wider content remit. Tor’s focus is on providing resources to help therapists develop their professional authority and brand, and grow their own businesses while working more efficiently and effectively, a topic that she speaks regularly on at global conferences.
Join us on Facebook: www.facebook.com/CoKinetic/ Connect with Tor: www.facebook.com/cokinetic.tor

Co-Kinetic Journal 2023;95(January):45-50

50
Physical
JANUARYLAUNCHING2023 Register your interest https://bit.ly/3uBNpYB
Overview of the Social Success for
Therapists Course
SOCIAL SUCCESS FOR PHYSICAL THERAPISTS

IF YOU:
Feel confused or overwhelmed by social media
Get little or no engagement from your social media posts
Have no idea what you should be doing but... Know you’re spending way too much time and getting zero ROI from your efforts
I EXPLAIN:
Why getting engagement on your posts is so hard and ways to overcome that
How to build a dynamic social media profile that demonstrates expertise and relevancy, as well as delivers value to your social media followers
How to use our ENGAGED content formula to create the right kind of professional content that attracts the attention of the all-important platform algorithms
Ways in which you can nurture and ‘massage’ these algorithms to increase exposure to your content, in turn increasing engagement and followers
The two sides of the social media coin, without which your social efforts will always fail
Course Presenter Tor Davies

While Tor trained as a physical therapist, she has been an entrepreneur now for more than two decades. Her focus is providing resources to help practitioners and therapists develop their businesses and to work more efficiently, a topic that she speaks on regularly at global conferences. The marketing practices and principles that Tor advocates, will help you turn a business that is only just surviving into one that thrives in just a matter of weeks.
Don’t know how to build an audience, or promote your business through social media without being salesy

Feel like your social media efforts are mostly a complete waste of time
...then this is the course for you.
Using proactive and reactive engagement to build targeted audiences

How to use paid social effectively FAQs around what networks to post to (and why), when and how often And finally how to generate new clients using social media.
This is a four module course with a heavy emphasis in module 3 and 4 on practical application so you can walk away and create a social media presence that not only you can be proud of but which engages, adds value, entertains and educates your followers.
Be the first to hear when the course launches by registering your interest at the following link
NEW
https://bit.ly/3uBNpYB
COURSE LAUNCHINGJAN 2023 REGISTER HERE
Market Your Clinic Online
Free Web Review
Understand your website and SEO opportunities with a Free Web Review. You might want to talk through some specifc ideas – like a website redesign or how to rank higher on Google – ask some questions, or just see what we could suggest. We’ll also produce some reports on your current website and SEO which are yours to keep.

There’s no obligation, just a half-hour on Zoom to discuss the best ways to market your business.
Free SEO Book
BOOK A REVIEW
https://bit.ly/3ddHSlU
Do you know what your patients are searching for online? We do. The Manual Therapy SEO Reference Guide breaks down search volumes for MSK conditions and treatments so you can create content which targets the searches people are making in real life. Buy on Amazon.co.uk or download the digital version for free from our website.

Who Are We?
https://bit.ly/3ddHSlU

At Market Your Clinic Online we are experts in websites and digital marketing services for physical therapy and Allied Health. Our marketing advice has been published in Osteopathy Today and we also work with Physio First to provide web and marketing advice to their members.
We specialise in small-to-medium practices who need quality services from a company who understands their needs and challenges. We’ve released how-to guides and case studies of our successes, and also publish the Manual Therapy SEO Reference Guide.
We pride ourselves in being honest and approachable, and in producing topquality work that you can rely on. We’re always happy to talk, so don’t hesitate to get in touch.
Marketyourclinconline.com
DOWNLOAD HERE
We’ve gone NAKED!


In a bid to further reduce the carbon impact of our journal we’ve taken two new steps:
1. Our paper is now offset through the World Land Trust
2. We’ve scrapped our starch-based polybag and gone ‘naked’ (lost the polybag)
The old polybag, while a step in the right direction, only breaks down in open air. f it nds its wa into and much of its en ironmenta a ue is ost.
For other enquiries: Email: info@co-kinetic.com
PLEASE RETURN TO: Co-Kinetic, 88 Nelson Road, London, SW19 1HX, UK
IF UNDELIVERED
INCORRECT ADDRESS DETAILS?
Please log in to your Account on https://co-kinetic.com and update your address. If you receive your journal through an Association or Group subscription, please inform the administrator of that Association directly.
CBP006075






































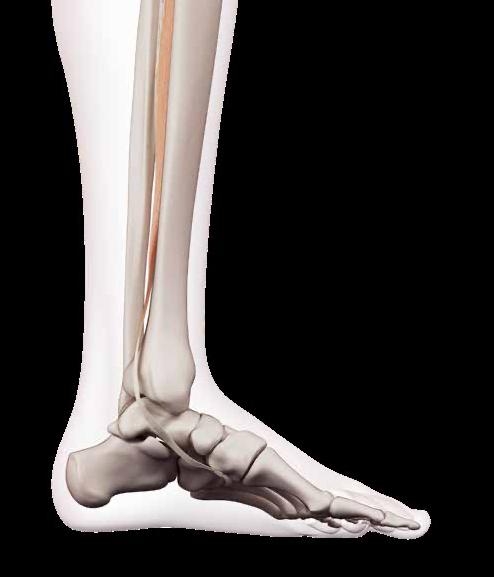


























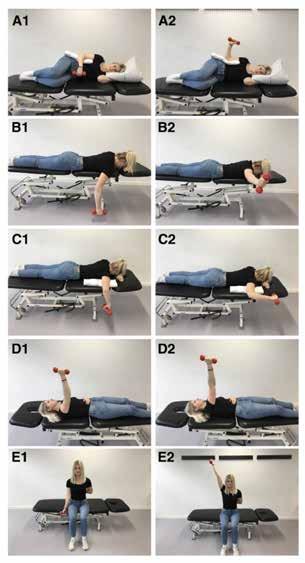
















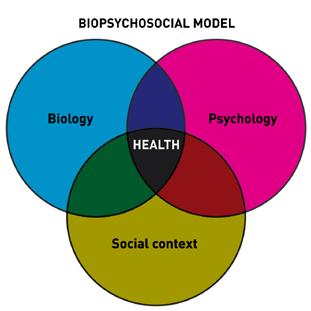






















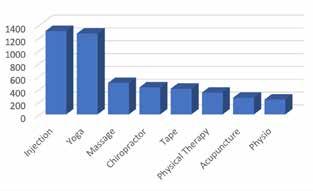



 By Tor Davies, physiotherapistturned Co-Kinetic founder
By Tor Davies, physiotherapistturned Co-Kinetic founder