EASTERN VASCULAR NEW DATA CHART UNDERREPRESENTATION OF WOMEN AT THE HEAD OF NATIONAL CLINICAL TRIALS
By Bryan Kay
THE UNDERREPRESENTATION of women vascular surgeons in national clinical trial leadership formed the central theme of data coming out of a new study that probed all clinical trials in five main areas of vascular disease between 1997 and 2003.
Delivered before the 2023 Eastern Vascular Society (EVS) annual meeting in Washington, D.C. (Sept. 7–9), investigators revealed that female vascular surgeons constituted 10.3% of all investigators leading clinical trials, with solo female principal investigators (PIs) making up just 9%. Additionally, only 5% of women vascular surgeons were solo PIs on industry-sponsored trials, and women were also less likely to lead interventional compared to non-interventional treatment trials, EVS 2023 heard.
The data were presented by Valentyna Kostiuk, a medical student from Yale School of Medicine in New Haven, Connecticut, who opened her talk with a baseline remark: “Female vascular surgeons constitute about 15% of the workforce, but remain underrepresented in vascular societies and NIH [National Institutes of Health] funding. Additionally, female patients are more likely to be enrolled in clinical trials if they are led by female investigators.”
See page 8
WOMEN'S CHAMPION: FREISCHLAG MARKS OUT VALUE OF DIVERSITY AND SURGEONS AS HOSPITAL LEADERS
By Bryan Kay
See page 8
2 From the Editor Malachi Sheahan III, MD, on sex, lies and carotid stents
6 Appropriate care SVS-ACS tandem marks release of outpatient
11 Grand Rounds Opportunity knocks in Washington, D.C.
13 Midwestern Vascular MVSS President Jeffrey Jim, MD, delivers a love letter to vascular surgery at annual meeting

www.vascularspecialistonline.com
COMPLEX AORTIC
Preventing spinal cord ischemia: Novel techniques for direct segmental artery revascularization show promise, WVS hears

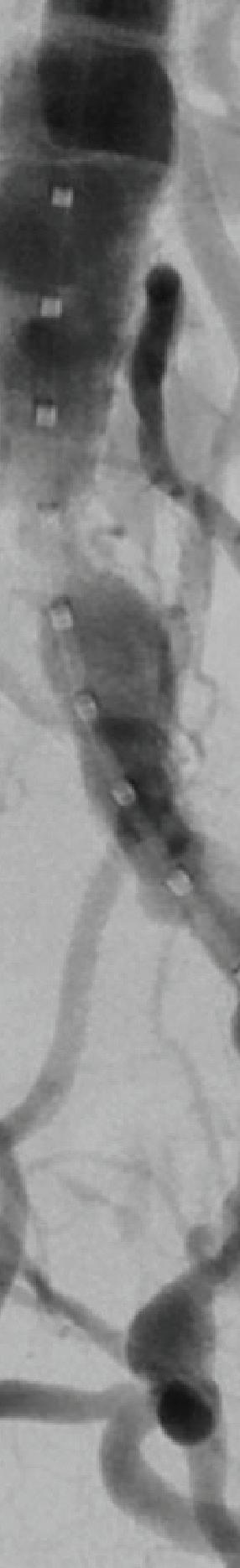
A vascular surgery team from the University of Southern California (USC) demonstrated the feasibility of direct revascularization of segmental arteries to prevent spinal cord ischemia (SCI) using novel endovascular or extraanatomic bypass techniques in high-risk patients with complex thoracoabdominal aortic aneurysms (TAAAs).
By Bryan Kay
This followed a retrospective review of fenestrated or branched endovascular aneurysm repairs (F/BEVARs) over a five-year period, attendees of the recent Western Vascular Society (WVS) annual meeting (Sept. 9–12) were told. The early work, which involves 12 patients undergoing either an endovascular or open approach, was hailed by audience member Benjamin W. Starnes, MD, chief of vascular surgery at University of Washington Medicine in Seattle, who said, “This is a new idea. I applaud the courageousness of our colleagues at USC for pursuing this.”
U SC integrated vascular surgery resident Anand Ganapathy, MD, who presented the study results, told WVS 2023, held in Koloa, Hawaii, that nine patients were treated endovascularly,

See page 4
JULIE A. FREISCHLAG, MD, USED HER turn as honorary guest lecturer at the 2023 Midwestern Vascular Surgical Society (MVSS) annual meeting to make a pitch for vascular surgeons to step up to the plate as hospital and institutional leaders—because that is “who you are,” she told the gathering in Minneapolis, Minnsota (Sept. 7–9).
I would challenge you as vascular surgeons to go and run things,” she said. “Surgeons are really, really good at running things. You make decisions with

OCTOBER 2023 Volume 19 Number 10
THE OFFICIAL NEWSPAPER OF THE ascularV pecialists CHANGE SERVICE REQUESTED 9400 W. Higgins Road, Suite 315 Rosemont, IL 60018 PRESORTED STANDARD MAIL U.S. POSTAGE PAID IM
this issue:
In
Julie A. Freischlag
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William
Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | Professor HansHenning Eckstein, MD | John F. Eidt, MD
| Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS
| Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank
J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Director of Marketing & Communications Bill Maloney
Managing Editor SVS Beth Bales
Manager of Marketing
Kristin Spencer
Communications Specialist
Marlén Gomez
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Roger Greenhalgh

Content Director Urmila Kerslake
Head of Global News Sean Langer
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution Jocelyn Hudson, Will Date, Jamie Bell and Éva Malpass
Design Terry Hawes and Wes Mitchell
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. | Printed by Vomela Commercial Group | ©Copyright 2023 by the Society for Vascular Surgery
FROM THE EDITOR
Sex, lies, and carotid stents
By Malachi Sheahan III, MD
First, a disclaimer. This commentary is woefully short of sex-related content. Not even the wholesome gender-based outcomes stuff. So, if that key term brought your internet search here, feel free to press on with your illicit journeys my friend. Now, let’s get to the lies. In 2008, Christopher White, MD, then chair of the Department of Cardiology at the Ochsner Clinic Foundation, published an editorial accusing vascular surgeons of various crimes and misdemeanors in the nascent debate over carotid stenting (CAS) vs. endarterectomy (CEA). Eloquently titled “Liar, liar, pants on fire,” the article begins, “At the most recent Society of Vascular Surgery [SVS] meeting, held in a secret location, deep in a mountain bunker, shielded against critical and independent thinking, surgeons regaled themselves with tales of science fiction, disguised as scientific data, and told to make the endovascularly challenged among them feel safe and secure from the ‘bogeyman’ of carotid artery stenting.” Now, before everyone can post their Spidermen-pointing-at-each-other memes, I will acknowledge the inherent hypocrisy in calling out another medical editor for utilizing hyperbole and provocative titles. So let’s get to the substance of his argument.
The two abstracts that drew White’s ire utilized national databases and showed that CEA demonstrated dramatic benefits over CAS in terms of stroke, mortality and cost. White points out the limitations of the studies, including the lack of independent neurological evaluations to document stroke. He states, “In reporting the superiority of CEA compared to CAS without any qualification, should we give the authors the benefit of the doubt that they are not sophisticated enough to comprehend the inherent ‘bias’ that invalidates their intended comparison, or have we caught them red-handed in an attempt to purposely deceive their audience?” While bemoaning the lack of a limitations section makes me suspect that White does not know how abstracts work, the request for an exam by an independent neurologist seems fair.
So, surely when he published a study in the same issue of this journal, making the provocative claim that carotid artery stenting is safe in the very elderly (>80 years), he held himself to the same lofty standard? After all, the lead-in phase of CREST had just shown a 12% risk of stroke with CAS in octogenarians. White and colleagues, however, reported only a 1.8% risk of stroke in this same age range, even though half were performed without embolic protection. It seems that independent neurologists don’t grow on trees, though, and White’s group often employed vascular medicine physicians from his institution to perform these evaluations, despite no clear evidence that they are either independent or adequately trained to assess for stroke.
So perhaps White’s group did achieve these outlier results, or perhaps, as he stated in his editorial, the underreporting of complications is a dirty little secret that is “very difficult to prove without an independent audit.”
White also disputes the finding of higher hospital
costs associated with CAS. He states that “the biased data reported in this abstract fly in the face of thousands of reported CAS patients with audited independent data who have had short hospital stays and lower or comparable procedure costs.” I wonder then what he thought of the excellent 2011 analysis by W. Charles Sternbergh, MD, which found that CAS was 40% more costly than CEA and did not provide better clinical outcomes or a reduction in length of stay. I am certain White is aware of this study, as the data came from his own institution.
Over the past 15 years, a plethora of new data has arrived with a series of randomized controlled trials (RCTs). While many used perplexing endpoints (the inclusion of myocardial infarction [MI] seems the logical equivalent of considering ambiance while comparing delivery pizzas), and most were underpowered to detect a statistically significant difference in the risk of stroke, a clear trend emerged. CREST-1 (4.1% vs. 2.3%), ACT-1 (2.8% vs. 1.4%), ICSS (7.7% vs. 4.1%), SAPPHIRE (3.6% vs. 3.1%), SPACE-1 (6.5% vs. 5.1%), EVA-3S (9.2% vs. 3.5%), and ACST-2 (3.6% vs. 2.1%) all demonstrated a persistently increased incidence of 30-day stroke with CAS over CEA. Only CAVATAS was an outlier (7.2% vs. 8.3%), although only 504 patients were randomized.
Although 'The Alliance' may sound like the bad guys from a mid-tier Liam Neeson movie, in reality, they are a collection of neurologists, surgeons and interventionalists
I was certain that White and his fellow stent enthusiasts would be happy that these new data have brought some much-needed clarity. Surely we can all agree that a good degree of caution must be employed when performing transfemoral carotid stent procedures, particularly in asymptomatic patients where the treatment efficacy is razorthin? Well reader, I regret to inform you that I was wrong. Last year, the Centers for Medicare & Medicaid Services (CMS) accepted a formal request from the Multispecialty Carotid Alliance to consider greatly expanding coverage for carotid stent procedures while also removing several safeguards currently in place. Although “The Alliance” may sound like the bad guys from a mid-tier Liam Neeson movie, in reality, they are a collection of neurologists, surgeons and interventionalists, including White, who seemingly formed solely to petition CMS to reconsider percutaneous carotid stent coverage.
Medicare began coverage for CAS procedures in 2001 for those performed within investigational device exempt (IDE) studies. In 2005, this expanded to high-risk patients who are symptomatic with greater than 70% lesions, which is essentially where it stands now. Currently, outside of clinical trials, no asymptomatic patients are covered. The last CMS coverage reconsideration for CAS occurred in 2009. According to the Alliance, special interest groups intervened and successfully restricted access to CAS. These “special interest groups” were the SVS, the American Association of Neurological Surgeons, and the American Academy of Neurology.
The Alliance now requests that CMS expand CAS indications to all asymptomatic lesions >70% and all symptomatic lesions >50%. They also request the removal of all facility standards, calling them obsolete. Privileging and credentialing standards, in their plan, will be up to local hospitals. Similarly, all quality assurance would be left to the local peer-review level, eliminating the requirement for participation in a quality registry. Libertarian principles like these are usually better in theory than practice. Allowing continued on page 4
2 Vascular Specialist | October 2023
AMNIOFIX® and AMNIOEFFECT®: Placental-based sheet allografts provide a protective barrier to support the healing cascade and the development of granulation tissue.


AXIOFILL®: Acellular human placental ECM particulate used in the replacement or supplementation of damaged or inadequate integumental tissue.
1.6x

Advanced Surgical Allograft Products Limb salvage is your goal. Providing surgical solutions is ours. NEW! RCT Outcomes with DHACM Scan to learn more or contact us: 888.543.1917 customerservice@mimedx.com DHACM = Dehydrated Amnion/Chorion Membrane, DFU = Diabetic Foot Ulcer, VLU = Venous Leg Ulcer, SOC = Standard of Care * 2x = based on mean time and 3.8x = based on median time, ^ Per Protocol group VLUs DFUs e defect closur vs. SOC at 16 weeks3,4^
rate of
2x to 3.8x
closure vs. SOC1,2* REFERENCES: 1. Zelen CM, et al. Int Wound J. 2013;10(5):502-507. 2. Zelen CM, et al. Int Wound J. 2015;12(6):724-732. 3. Bianchi C, et al. Int Wound J. 2018;15(1):114-122. 4. Bianchi C, et al. Int Wound J. 2019;16(3):761-767. Patents and patents pending see: www.mimedx.com/patents. AMNIOFIX, AMNIOEFFECT, AXIOFILL, and MIMEDX are trademarks of MIMEDX Group, Inc. ©2023 MIMEDX Group, Inc. All Rights Reserved. www.mimedx.com US-AC-2300002 v2.0
faster defect
EDITORS LETTER SEX, LIES AND CAROTID STENTS
folks to police themselves often leads to things like emotional support leopards on domestic flights. Where the evidence does not support expanding CAS indications, the Alliance is quick to find fault. They refer to the stroke/death outcomes in SPACE, EVA-3S, and ICSS as “unacceptable by 2021 standards.” They criticize the inexperience of the CAS operators and the technology and techniques employed at the time. The Alliance would have us believe that EVA-3S was performed in the 1500s by a bunch of French peasants launching stents at unsuspecting patients with trebuchets.
In critiquing the International Carotid Stenting Study (ICSS), presumably because of its 7.7% CAS stroke rate, the Alliance notes that two operators caused five of the strokes despite enrolling only 11 patients. Even though the operators were suspended, the Alliance points out that the strokes were included in the final analysis. To this, I would reply that these practitioners were only removed because the study was carefully monitoring outcomes. How many more real-world strokes are we going to see if guardrails such as registries are removed, as the Alliance recommends? In their submission to CMS, the Alliance states that there are four modern RCTs comparing CAS to CEA in asymptomatic patients. They opine that all have shown comparable outcomes for periprocedural complications, as well as rates of ipsilateral stroke. In reality, none of the protocols were powered to detect a statistically significant difference in stroke outcomes.
The Asymptomatic Carotid Trial (ACT-1) randomized 1,453 patients out of an intended 1,658. The study reported a stroke rate of 2.8% in the stent group and
continued from page 2
1.4% in CEA group. Stent-Protected Angioplasty vs. Carotid Endarterectomy-2 (SPACE-2) planned to enroll 3,640 patients but only randomized 513. There were three groups: CEA with best medical therapy (BMT), CAS with BMT, and BMT alone. The five-year cumulative incidence of any ischemic or hemorrhagic stroke was 5.3% in the CEA group, 9.8% with CAS, and 6.5% with BMT. The CAS group also demonstrated the highest (4.4%) five-year cumulative ipsilateral ischemic stroke rate (2% CEA, 3.1% BMT). The Asymptomatic Carotid Surgery Trial-2 (ACST2) randomized 3,625 patients. The 30-day stroke rates were higher with CAS (3.6% vs. 2.4%, p=0.06) but did not achieve significance. At five years, the composite risk of ipsilateral stroke or death was 5.5% for CAS and 3.6% for CEA. The Stenting vs. Endarterectomy for Treatment of Carotid-Artery Stenosis (CREST) trial randomized 2,502 patients and did find a significantly higher risk of periprocedural stroke with CAS (4.1% vs. 2.3%, p=0.01). Of course, CREST famously used a combined stroke, MI, and death primary endpoint, which did not demonstrate a significant difference between the modalities. So even
though all four modern asymptomatic carotid trials showed a higher incidence of stroke with CAS, the Alliance assures us not to worry. Why? Well, we are better now. Smarter. We have a greatly improved understanding of the anatomic and clinical characteristics that increase risk for CAS. In fact, they even provide them.
So fans of precision medicine take note: Criterion #1— vasculopathy. Vascu-what now? In fact, of the high-risk characteristics provided by the Alliance, the majority are vague definitions like atherosclerotic arch, complex great vessel anatomy and carotid tortuosity. The Alliance correctly touts the importance of patient selection and operator experience in asymptomatic patients, yet they would like to remove all of the guardrails.
So clearly, to offer safe treatment to patients with asymptomatic carotid disease, the practitioner must be technically experienced as well as a content expert. Where will this expertise be gained? Interest does not translate to competence. Vascular surgeons matriculate into the workforce with documented technical and educational experience in the treatment of carotid disease. For other specialties? Not so much. The words “cerebrovascular” and “carotid” appear a total of zero times in the ACGME Program Requirements for Graduate Medical Education in Interventional Cardiology. If CMS follows the recommendations of the Alliance, only one thing is certain. More transfemoral stents will be placed in asymptomatic carotid lesions in Medicare patients by interventionalists under less regulation. The Alliance states that this is in the best interests of patient care. Who is lying now?
FROM THE COVER: PREVENTING SPINAL CORD ISCHEMIA: NOVEL TECHNIQUES FOR DIRECT SEGMENTAL ARTERY REVASCULARIZATION
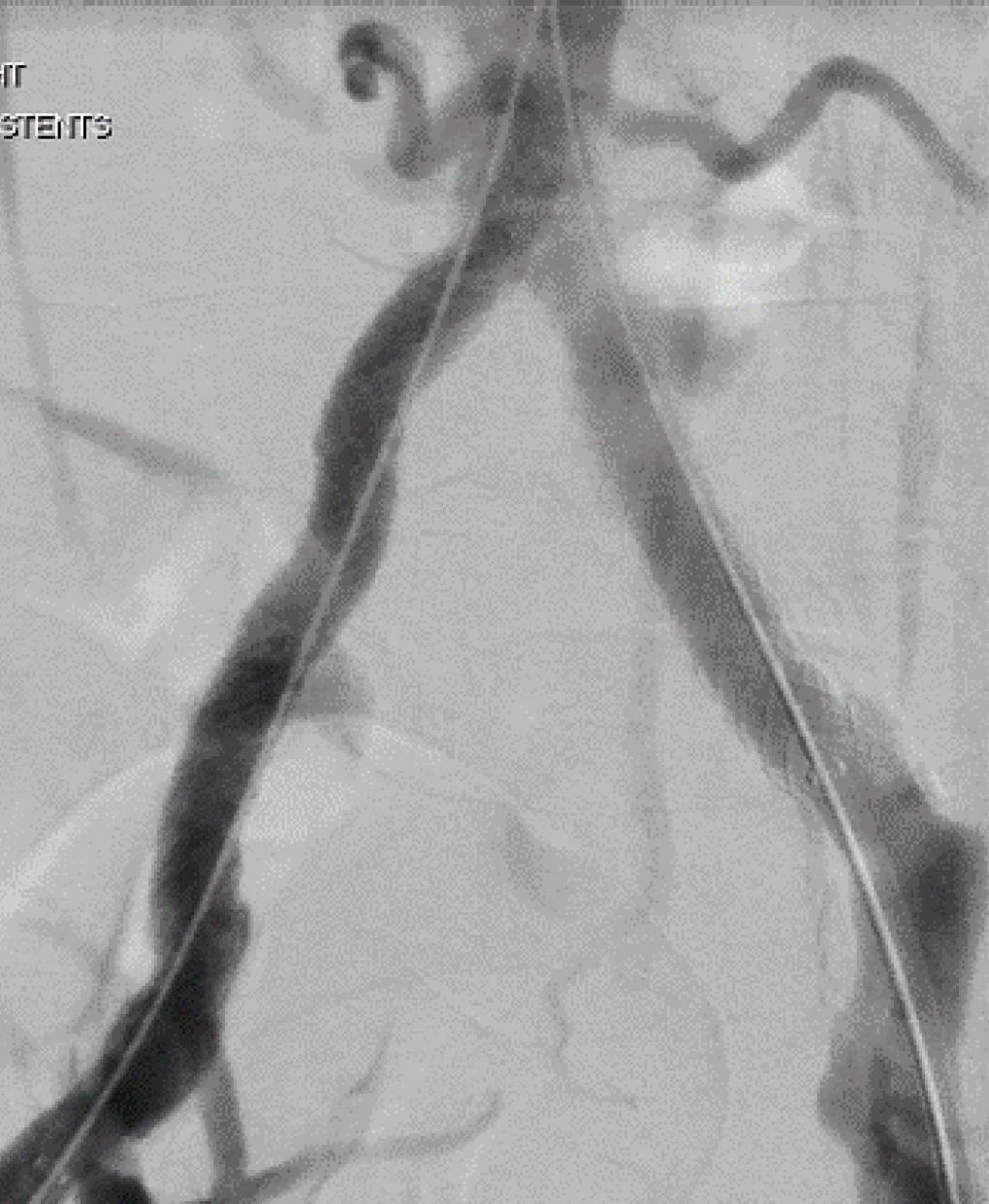
with a total of 11 segmental arteries incorporated. Ganapathy outlined how seven were revascularized using a directional cuff sewn directly onto a physician-modified graft that was extended with self-expanding Viabahn stents; two of the arteries were treated using stented fenestrations; and the remaining two—located along the seal zone—were tackled using unbridged, large fenestrations without covered branched stents. The other three patients received an extra-anatomic bypass.
Extents I and II were the most common type of TAAA among the patient group, Ganapathy continued. Procedural details for endovascular repair of the aneurysms demonstrated an average of 4.3 target vessels (2–6) treated, with a technical success rate of 83%.
Failures (two patients) involved a bridging stent to a renal artery “that was dislocated from the fenestration and not recoverable” and a malalignment of an unstented fenestration to an intercostal artery “maintained with an uncovered stent.”
Nine patients had successful prophylactic spinal drain placement. The three patients who underwent open repair of their segmental arteries received their bypass an average of three days prior to the F/BEVAR procedure.
Ganapathy reported no mortality at 30 days post-procedure. Two patients—one who had a staged extra-anatomic bypass, the other an unstented fenestration—incurred spinal cord ischemia that “resolved completely by discharge.” Both had prophylactic spinal drain placement.
Average follow-up was 472 days. Three of the 14 targeted segmental arteries occluded during follow-up, Ganapathy added. Occluded branches involved one extra-anatomic bypass and two directional cuffs. “They occurred beyond one year without causing spinal cord ischemia,” he said.
G anapathy concluded: “Spinal cord ischemia remains a serious complication of F/BEVAR, despite current mitigation strategies. Our initial experience demonstrates feasibility of endovascular and ex-
tra-anatomic bypass for segmental revascularization in select patients.
“Further work is planned to improve patient selection through anatomic and dynamic assessment of spinal cord perfusion patterns, as well as the safety and efficacy of segmental artery revascularization procedures through a multidisciplinary, collaborative effort across expertise from a growing list of specialists. Our vision is that someday this might serve as another adjunct to the current spinal cord ischemia mitigation protocols.”
K arthikeshwar Kasirajan, MD, a clinical professor of vascular surgery at Stanford University, the designated discussant of the paper at WVS, summarized the study’s headline findings, outlining how the novel techniques had been employed in 3.8% of F/ BEVAR patients reviewed during the study period. Some 11% of the endovascular group and 33% of the open group developed transient paraplegia, he said.
Kasirajan commented: “In my opinion, it should be noted that stent grafts have a lower instance of paraplegia when compared to open repairs in general. This is despite the fact that length of coverage is often more extensive as to require landing
zones that are much more extensive than open repairs. Additionally, during open repairs we can reimplant intercostals. This cannot be done during stent graft [implantation], hence intercostal revascularization may not be the holy grail in the prevention of paraplegia.”
Alan Lumsden, MD, chair of the Department of Cardiovascular Surgery at Houston Methodist in Houston, Texas, congratulated the USC team on the ground-breaking nature of their work, asking Ganapathy and colleagues to drill down on any guidelines they follow to determine which patients should receive the novel approach.

Senior author of the study, Sukgu Han, MD, co-director of the Comprehensive Aortic Center at USC’s Keck Hospital, said: “Patient selection is everything. There’s probably more value from putting this protocol together with people from different specialties, maybe actually in the characterization of the spinal perfusion and individual variability.
“Because, so far, really the only surrogate marker we are looking at, in really very few select patients, is the size and assumption that that carries dominant collateral to the spinal cord.”
4 Vascular Specialist | October 2023
➽
SHOW PROMISE continued from page 1
“How many more real-world strokes are we going to see if guardrails such as registries are removed as the Alliance recommends?”
“Our vision is that someday this might serve as another adjunct to the current spinal cord ischemia mitigation protocols”
ANAND GANAPATHY
Anand Ganapathy
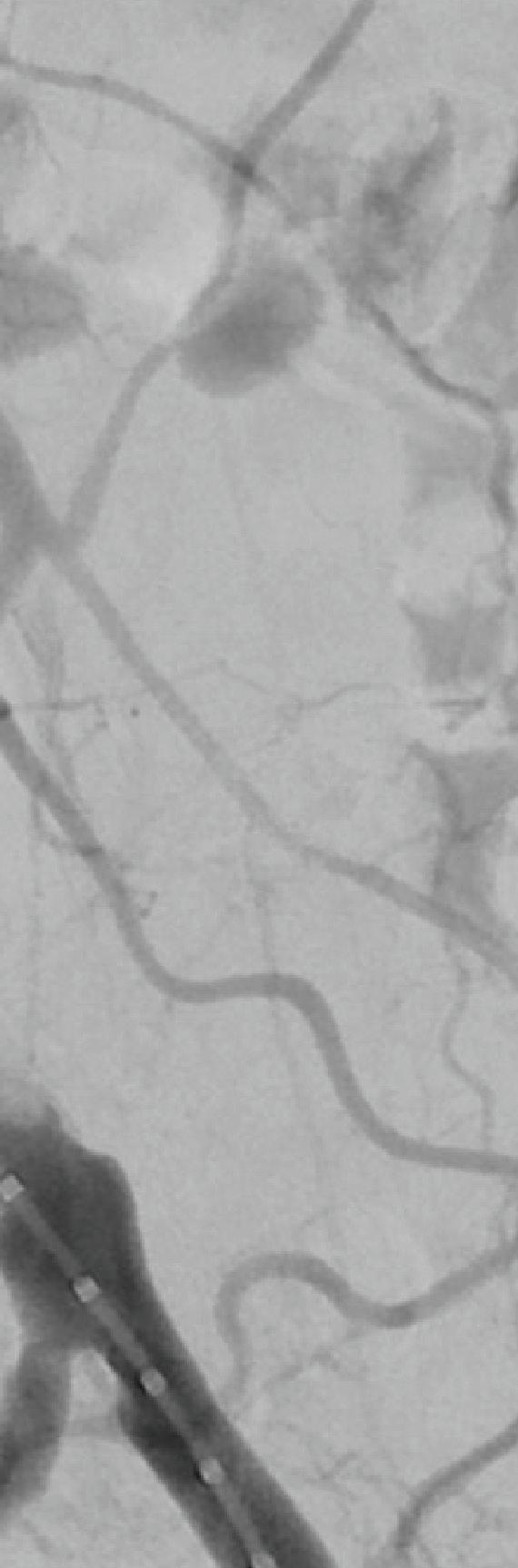
Behind the procedure: Removing in-stent thrombosis with the RevCore
Thrombectomy Catheter
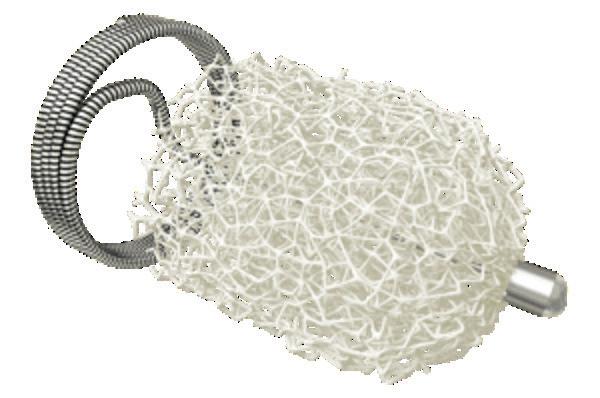
For patients with in-stent thrombosis (IST), one of the most critical unmet needs has been an effective method to remove acute-to-chronic material. Here, Rishi Roy, MD, a vascular surgeon at Advanced Vascular & Vein Associates in Flowood, Mississippi, discusses his experience with the first mechanical thrombectomy device to be able to do so—the RevCore thrombectomy system. RevCore is a minimally invasive, over-the-wire device indicated to treat thromboemboli in the peripheral vasculature, including venous stents. It includes a catheter with an expandable element for venous stent treatment. It also has a reinforced catheter shaft for precise movements and a diameter-control knob for adjusting the element to treat vessels 6mmplus and venous stents from 10–20mm.

Prior to RevCore, how did you treat in-stent thrombosis?
Previously I would take a multimodal approach using suction thrombectomy, along with balloon venoplasty, or even a non-compliant balloon. The goal was to get some lumen gain, to restore some outflow to decompress the limb.
How does this new device work?
RevCore makes it possible to extract thrombotic material from an occluded stent. The diameter of the coring element can be increased or decreased manually to accommodate the size of the vessel . You engage or disengage with the stent, as needed, and you can be more aggressive as you work through the material that caused the occlusion.
How do you size the catheter and capture liberated clot?
When sizing the element in the stent, low and slow is key. There is a tactile feel to the device when “revving,” and it’s important to note resistance level. Some resistance is good—too much means the element is likely oversized and should be decreased by turning the external diameter-control knob to the minus sign on the handle. An important consideration for these cases is to have another device placed in the inferior vena cava (IVC) to capture the cleared material.
When do you know that RevCore worked?
Immediately postprocedure, I can gauge whether the device worked when I visualize blood flow on imaging. Because the device
nal stent diameter, that patient will require close follow-up every six months or so, but they may be able to go for a couple of years between interventions. Fewer interventions also means decreased anesthesia time, operative time, chance of adverse events and morbidity. If we can decrease the number of cases because we’re able to remove IST in a single procedure, that’s a game changer.
A FlowTriever catheter (Inari Medical) was advanced over a stiff wire to the infrarenal segment of the IVC, and two of the catheter’s XL disks were deployed. From the right side, a stiff wire was advanced to the IVC via a Bern catheter (Boston Scientific), followed by an Amplatz wire. The catheter was removed, and then a 16F sheath was placed.
IVUS was performed in the IVC, revealing that the stent extended into the very distal IVC; no stenosis was seen. IVUS of the right common iliac vein (CIV) showed overlapping stents but no stenosis. A venous ultrasound probe inserted to the level of the right EIV showed 50–60% stenosis. IV heparin was administered.
The RevCore catheter was advanced over the Amplatz wire to the right EIV, and the coring element was deployed within the stent in an unexpanded state. The coring element was then slowly enlarged and rotated, loosening the material within the stent. RevCore was then withdrawn and cleaned. A Triever16 Curve catheter (Inari Medical) was advanced and suction thrombectomy performed, removing a combination of subacute and chronic thrombotic material (C). Balloon venoplasty of the stented portion of the right CFV, EIV and CIV was performed with an 18mm noncompliant balloon.
Initial
is new, I have an intensive follow-up protocol and, working with a wound care group, even closer follow-up is possible. I generally see the patient back in four weeks. After that, we see them at three and six months, and then every six months. If over a twoyear period we don’t see recurrent stenosis, and the patient is comfortable, we could get it down to once a year.
What anticoagulation regimen do you give these patients?
I send them out on either a novel oral anticoagulant (NOAC) or Coumadin. You know, people often ask me, “Which do you prefer?” My honest answer is I prefer whatever the patient can afford. Because if they can’t afford a NOAC, then they’re not going to take it, and we’re back at square one.
How do you think
RevCore will change the treatment pathway?
RevCore allows us to consider intervention sooner for patients who are suffering from symptoms related to IST. Some had stents placed when they were in their 20s or 30s, and when these stents are put in, they’re in forever. Now it’s decades later, and they have recurrent IST with chronic material that requires reintervention every threesix-eight months for symptom relief. Now, if we can debulk and get back to the origi-
Case report: Complete thrombus extraction after severe right EIV stent stenosis

Patient history
A man in his mid-50s presented with ulceration and swelling in his right foot with the intention to transfer care. Several months prior, a right external iliac vein (EIV) to right common femoral vein (CFV) stent had been placed. A venous duplex ultrasound study showed proximal stent occlusion and non-occlusive venous thrombosis in the left proximal femoral, popliteal, posterior tibial, and gastrocnemius vessels, as well as thrombosed varicosities. Right lower extremity venography and intravascular ultrasound (IVUS) performed two-and-a-half weeks later confirmed 65% stenosis of the left EIV stent (image A). An in-hospital mechanical thrombectomy and balloon angioplasty procedure was planned.
Procedural overview
The patient was positioned supine and ultrasound guidance was used to access the right CFV. A J-wire was advanced into the IVC. An 8F sheath was placed and a venogram showed stenosis within the right EIV stent (B). Similarly, access was gained to the left CFV, and a J-wire was advanced into the IVC. An 11F sheath was placed and a venogram confirmed there was no stenosis in the selected segments.
Additional passes with the Triever16 Curve catheter were conducted along the right iliac segments and within the IVC, removing thrombotic material that had been captured by the FlowTriever XL disks. Thrombus capture with either FlowTriever XL disks or the Protrieve sheath is critical to the RevCore procedure. Blood was returned to the patient using FlowSaver.
A final IVUS showed nearly 100% lumen gain, restoring the right EIV to CFV in-stent diameter to 16.4 mm (D). A final venogram demonstrated appropriate flow through the right CFV, EIV, CIV and IVC, and resolution of the stenosis within the right EIV (E). The FlowTriever disks and all other devices were removed, and manual pressure was held.
Total procedure time: 40 minutes. Estimated blood loss: <50mL. The patient tolerated the procedure well. He was discharged on dabigatran the following day. At four-week follow-up, stent patency was maintained per venous duplex ultrasound, and the patient’s right lower extremity pain and edema had improved. Progress was also seen in a previously non-healing ulceration of the right foot.
He will continue wound care and daily medication and return every six months for repeat imaging.
Conclusion
Use of the novel RevCore system ( F) allowed for thorough extraction of in-stent thrombosis and complete lumen restoration post-thrombectomy, with sustained patency and symptom relief at follow-up. The results show promise for improving quality of life in patients who had exhausted their treatment options previously.
5 www.vascularspecialistonline.com
ADVERTORIAL | SPONSORED BY INARI MEDICAL
Rishi Roy
IVUS confirmed the IST (A). Preprocedure venogram demonstrated instent thrombosis and impaired flow (B). Extracted thrombotic material (C). Postprocedure IVUS confirms stent patency (D). Postprocedural venogram confirms patency (E). RevCore Thrombectomy Catheter with expandable coring element (F)
APPROPRIATE CARE
SVS-ACS VASCULAR VERIFICATION PROGRAM MARKS RELEASE OF NEW STANDARDS FOR OUTPATIENT VASCULAR CENTERS
By Beth Bales and Bryan Kay
THE SOCIETY FOR VASCULAR Surgery (SVS) and the American College of Surgeons (ACS) have released new standards for outpatient vascular centers to help them provide optimal care and treatment of patients receiving vascular surgical and procedural care.
These new standards, outlined in the Optimal Resources for Vascular Surgery & Interventional Care—2023 Vascular-VP Outpatient Standards manual, are part of the Vascular Verification Program (Vascular-VP), launched earlier this year by the SVS and the ACS. These standards provide the requirements necessary for outpatient vascular centers to achieve and maintain verification for their vascular programs.
“Outpatient facility verification by this program demonstrates to patients, referring physicians, regulators and payors that high-quality, high-value vascular care is being delivered. Participants who successfully complete the verification process will
be setting the standard for vascular care in their community,” said William Shutze, MD, chair of the Vascular-VP Outpatient Work Group and a vascular surgeon with Texas Vascular Associates in Plano, Texas. Vascular-VP, which now offers verification for both inpatient and outpatient vascular centers, leverages the strengths and expertise of the SVS and ACS to provide a program that provides an evidence-driven, standardized pathway for instituting and growing a quality improvement and clinical care infrastructure within a center’s vascular program.
The release of this new set of standards within Vascular-VP encourages sites to put the same emphasis on quality in outpatient settings that is applied to inpatient settings, as more surgical services are directed to outpatient centers.
These new Vascular-VP outpatient standards detail elements of vascular surgical care and quality across nine domains,
including institutional commitment; program scope and governance; resources for facilities, equipment, services, and personnel; clinical care; data abstraction and analysis; and quality improvement.

By participating in the Vascular-VP program and complying with these standards, outpatient vascular centers can develop the tools necessary to provide safe, effective, patient-centered, timely, efficient and equitable care to all vascular patients.
Together, the SVS and ACS sought to evaluate and improve the quality of care for vascular patients with the following elements: program-specific standards; infrastructure needed to meet such standards and deliver high-quality,
high-value care; data collection and analysis; and verification site visits to ensure proper implementation and maintenance of these components.
Centers interested in becoming verified and continuing the quality improvement journey of their vascular service are encouraged to apply online at www.facs. org/quality-programs/accreditation-and-verification/ vascular-verification/
The first four hospitals in the U.S. to be verified as part of the inpatient strand of the program were announced in June.
References
1Hull JE, Jennings WC, Cooper RI, Waheed U, Schaefer ME, Narayan R. The pivotal multicenter trial of ultrasound-guided percutaneous arteriovenous fistula creation for hemodialysis access. J Vasc Interv Radiol. February 2018;29(2):149-158.e5.
2Shahverdyan R, Beathard G, Mushtaq N, et al. Comparison of Ellipsys percutaneous and proximal forearm gracz-type surgical arteriovenous fistulas. Am J Kidney Dis. October 2021;78(4):520-529.e1.
3Hull JE, Jennings WC, Cooper RI, Narayan R, Mawla N, Decker MD. Long-term results from the pivotal multicenter trial of ultrasound-guided percutaneous arteriovenous fistula creation for hemodialysis access. J Vasc Interv Radiol Published online June 2, 2022.
4Franco G, Mallios A, Bourquelot P, Jennings W, Boura B. Ultrasound evaluation of percutaneously created arteriovenous fistulae between radial artery and perforating vein at the elbow. J Vasc Access. September 2020;21(5):694-700.
5Mallios A, Bourquelot P, Franco G, et al. Midterm results of percutaneous arteriovenous fistula creation with the Ellipsys vascular access system, technical recommendations, and an algorithm for maintenance. J Vasc Surg December 2020;72(6):2097-2106.
Brief Statement Indications
The Ellipsys™ system is indicated for the creation of a proximal radial artery to perforating vein anastomosis via a retrograde venous access approach in patients with a minimum vessel diameter of 2.0 mm and less than 1.5 mm of separation between the artery and vein at the fistula creation site who have chronic kidney disease requiring dialysis.
Contraindications
The Ellipsys system is contraindicated for use in patients with target vessels that are < 2 mm in diameter. The Ellipsys System is contraindicated for use in patients who have a distance between the target artery and vein > 1.5 mm.
Warnings
• The Ellipsys system has only been studied for the creation of an AV fistula using the proximal radial artery and the adjacent perforating vein. It has not been studied in subjects who are candidates for surgical fistula creation at other locations, including sites distal to this location.
• The Ellipsys system is not intended to treat patients with significant vascular disease or calcification in the target vessels.
• The Ellipsys™ system has only been studied in subjects who had a patent palmar arch and no evidence of ulnar artery insufficiency.
Use only with the Ellipsys™ Power Controller, Model No. AMI-1001.
• The Ellipsys Catheter has been designed to be used with the 6 F Terumo Glidesheath Slender *. If using a different sheath, verify the catheter can be advanced through the sheath without resistance prior to use.
• Use ultrasound imaging to ensure proper placement of the catheter tip in the artery before retracting the sheath, since once the distal tip of the catheter has been advanced into the artery, it cannot be easily removed without creation of the anastomosis. If the distal tip is advanced into the artery at an improper location, complete the procedure and remove the catheter as indicated in the directions for use. It is recommended that a follow-up evaluation of the patient is performed using appropriate clinical standards of care for surgical fistulae to determine if any clinically significant flow develops that require further clinical action.
Precautions
• This product is sterilized by ethylene oxide gas.
Additional procedures are expected to be required to increase and direct blood flow into the AVF target outflow vein and to maintain patency of the AVF. Care should be taken to proactively plan for any fistula maturation procedures when using the device.
• In the Ellipsys study, 99% of subjects required balloon dilatation (PTA) to increase flow to the optimal access vessel and 62% of subjects required embolization coil placement in competing veins to direct blood flow to the optimal access vessel. Prior to the procedure, care should be taken to assess the optimal access vessel for maturation, the additional procedures that may be required to successfully achieve maturation, and appropriate patient follow-up. Please refer to the “Arteriovenous Fistula (AVF) Maturation” section of the labeling for guidance about fistula flow, embolization coil placement, and other procedures to assist fistula maturation and maintenance.
The Ellipsys™ System is intended to only be used by physicians trained in ultrasound guided percutaneous endovascular interventional techniques using appropriate clinical standards for care for fistula maintenance and maturation including balloon dilatation and coil embolization.
• Precautions to prevent or reduce acute or longer-term clotting potential should be considered. Physician experience and discretion will determine the appropriate anticoagulant/antiplatelet therapy for each patient using appropriate clinical standards of care.

Potential Adverse Events

• Potential complications that may be associated with creation and maintenance of an arteriovenous fistula include, but may not be limited to, the following:
• Total occlusion, partial occlusion or stenosis of the anastomosis or adjacent outflow vein
• Stenosis of the central AVF outflow requiring treatment per the treatment center’s standard of care
Failure to achieve fistula maturation
• Incomplete vessel ligation when using embolization coil to direct flow
• Steal Syndrome
• Hematoma
• Infection or other complications
• Need for vessel superficialization or other maturation assistance procedures.
CAUTION: Federal (USA) law restricts this device to sale by or on the order of a physician.
Important Information: Indications, contraindications, warnings, and instructions for use can be found in the product labelling supplied with each device.
6 Vascular Specialist | October 2023
medtronic.com/ellipsys UC202301636 EN ©2022 Medtronic. Medtronic, Medtronic logo, and Engineering the extraordinary are trademarks of Medtronic.
All other brands are trademarks of a Medtronic company. 09/2022
“Participants who successfully complete the verification process will be setting the standard for vascular care in their community”
www.vascularspecialistonline.com THEOFFICIAL NEWSPAPEROF THE StandardPostage Lebanon CHANGE SERVICE REQUESTED 9400 W. Higgins Road, 315 Rosemont, 60018 APRIL 2023 olume Number 02 Guest editorialIntentional mentorship— and why it matters 07&CommentAnalysis Corner Stitch looks back at VESS 2023 and open repair volumes among trainees 12 Diversity Society of Black Vascular Surgeons builds bridges 17 VAM 2023 ‘Early birds’ flock as registration opens, spectrumfullof meeting program comes into focus In this issue: SOCIETY FOR VASCULAR SURGERY (SVS) and the American College of Surgeons (ACS) have launched the “Vas-cular Verification Program (Vascular-VP),” an ACS Quality Program developed in partnership with the SVS. The newly launched inpatient program reviews not just safety processes against standards created by vascular surgeons, but also emphasizes the importance of using clinical data for tracking outcomes and supporting quality improvement specific to vascular care. It covers the perioperative continuum of care, from pre-hospital to post-discharge care. “We created this program to ensure quality and quality improvement in vascular care in both the inpatient and outpatient settings,” said SVS President Michael C. Dalsing, MD. “Our own members asked for this program, particularly for outpatient settings, which may have little or no oversight. They understand the importance of standard policies and procedures embedded wherever care provided to ensure safety and promote quality.” The verification process ensures that an applicant program: Has the appropriate infrastructure for the procedures performed ◆ Follows clinical pathways to ensure care is in line with evidence-based clinical guidelines when available ◆ Monitors outcomes, emphasizing the importance of clinically relevant, risk-adjusted, nationally benchmarked data ◆ Submits all needed information to reviewers who will assess all required aspects of the program for verification ◆ Undergoes a verification visit to ensure all standards are complied with and performs case review to ensure that there are internal quality processes in place to ensure safe and appropriate care of patients afflicted with vascular disease provided The ACS has long-standing experience in wide array of quality verification programs to include See page See page THE OCCASION A SEMINAL MEETING HELD Chicago by former Society for Vascular Surgery (SVS) Presidents John Bergan, MD, and James S.T. (Jimmy) Yao, MD, played a central role in the formation of the world-renowned Charing Cross (CX) International Symposium, which this year marks its 45th edition. The year was 1976, and Roger M. Greenhalgh, MD, CX founder and chairman, had not long returned from tour of the world’s major vascular surgery centers, when he was invited to attend the Bergan and Yao meeting at Northwestern UniSCVS 2023 ORENDOVASCULAR-FIRST -ONLY APPROACH FOR ALL CLTI PATIENTS ‘IS NOT EVIDENCE-BASED CARE’ MICHAEL S. CONTE, MD, ONE of the foremost experts in the field of peripheral arterial disease (PAD), took attendees of the 2023 Society for Clinical Vascular Surgery (SCVS) Annual Symposium in Miami on journey through the decades ev- idence-based limb-threateningrevascularization ischemia, telling those gathered that the recently published “landmark” BEST-CLI trial evidence should lead shift in the current practice landscape, where open bypass surgery “un- der-offered and under-utilized.” Conte, chair, professor and chief of vascular endovascular - gery at the University of California San Francisco (UCSF), was delivering the SCVS 2023 (March 25–29) Distinguished Visiting Professor address, devoting significant portion to the recent publication of the BEST-CLI (Best endovascular versus best surgical therapy patients with critical limb ischemia) randomized-controlled trial (RCT) data, and what its results means for the treatment CLI, or chronic limb-threatening ischemia (CLTI) goingConteforward. posed the ultimate question: What are the take-home messages in the world of CLTI treatment post-publication of the BEST-CLI results? “I think it is really See page A joint effort aimed at ensuring quality vascular care and quality improvement is universal goal has seen eight pilot programs—four inpatient and four outpatient centers—go through the pilot phase of the verification process. By Beth Bales ✓ ✓ ON OCCASION OF 45THANNIVERSARY,CX SYMPOSIUM CHAIRMAN CREDITS CHICAGO VASCULAR SURGICAL TANDEM FOR ENDURING SUCCESS By Bryan Kay By Jocelyn Hudson and Bryan Kay APPROPRIATENESS
WILLIAM SHUTZE
William Shutze
Less invasive, long lasting
Ellipsys™ Vascular Access System

Only the Ellipsys vascular access system uses a single point of venous access,1 offering the simplest, most minimally invasive option for arteriovenous fistula (AVF) creation.†1,2 It provides an immediate, suture-free, permanently fused anastomosis1 that is clinically proven to improve longevity3-5 and reduce the risk of complications.3,5
medtronic.com/ellipsys
 Distal Tip
† Compared to surgical arteriovenous fistulas.
Distal Tip
† Compared to surgical arteriovenous fistulas.
FROM THE COVER: NEW DATA CHART UNDERREPRESENTATION OF WOMEN AT THE HEAD OF NATIONAL CLINICAL TRIALS
continued from page 1
To evaluate representation, the Yale study group looked at all national PIs, their specialties and their presenting gender. When comparing vascular surgeon PIs to non-vascular surgeon PIs, female investigators constituted 10.3% in the vascular surgeon group compared to 19.9% of investigators in the non-vascular surgical group, Kostiuk said.
They looked at 114 clinical trials focusing on abdominal aortic aneurysms (AAA), analyzing 101: these were led by 125 vascular surgeons, of which 8.8% were women. Similarly, 138 carotid disease trials were identified, with 122 analyzed. This revealed that 38 were led by vascular surgeons, with 13.2% of them women. Another 100 hemodialysis access trials yielded 86 for analysis. These were led by 52 vascular surgeons (9.6% women). In the venous space, 26 thrombectomy and stenting trials showed 30 vascular surgeon as PIs, with 15.4% of them women. Finally, 536 peripheral arterial disease (PAD) trials yielded 432 for analysis, with 169 headed up by vascular surgeons (10.7% women).
“Overall, out of all the investigators, for five major vascular conditions, 10% of them were female investigators,” explained Kostiuk. “On subgroup analysis, we looked at clinical trials led by solo PIs, and 9% of these PIs were women. Additionally, women were less likely to lead clinical trials investigating interventions compared to non-interventional treatments. For industry funding, we identified 11% of investigators as women for non-industry sponsored clinical trials as compared to 8% for industry sponsored trials. Out of this 8%, 5% were solo female investigators.”
Kostiuk concluded by pointing toward the 10.3% figure, which constituted the representation of women vascular surgeons in national clinical trial leadership. “This study identifies a specific issue with diversity and inclusion in our specialty,” she said. “It represents an opportunity for growth and improvement, and also encourages vascular societies and industry sponsors to define pathways for women to lead clinical trials.”
In response to a query from the EVS audience, Kostiuk said the Yale research team will now look to break down whether the numbers are improving over time or remain stagnant. “The numbers are low and could be improved.”
Last month, Vascular Specialist reported on the issues surrounding gender representation at the head of clinical trials and female patient enrollment. One of the starkest portraits of the scene was painted by leading vascular surgical voice Melina R. Kibbe, MD, in an interview.
“We would have fewer untoward side effects, fewer drugs removed from the market by the FDA [Food and Drug Administration], and, ultimately, better outcomes in women,” stated the dean at the University of Virginia School of Medicine in Charlottesville, Virgina, as she reflected on two decades of missed opportunities, the underrepresentation of women as clinical principal investigators (PIs), and women’s under-enrollment as participants in vascular trials.
INTERVIEW
Highlighting original work by women: Peerreview title blazes new trail in vascular surgery
The September issue of Annals of Vascular Surgery featured 37 original, peer-reviewed scientific papers whose lead authors and researchers are women vascular surgeons. Here, editor Caitlin W. Hicks, MD, discusses the mechanics of getting the publication out, coming amid recent trials and tribulations in the vascular space that saw her come under personal attack.
THE WORK HAD BEEN MORE THAN A YEAR IN the making, so to see the final title reach the point of release filled those behind the Annals of Vascular Surgery special issue, “Original Work by Women, with a sense of accomplishment. Hicks said the mere fact the entire edition is fully open access has attracted positive feedback, but, for her, something else stands out as a particular achievement.“The biggest highlight is just the fact we were able to get so many articles with first and last women authors, which given the number of female vascular surgeons is relatively small, and the articles still underwent standard, strict peer review, is probably the most exciting and impactful component,” she tells Vascular Specialist. Solidifying the point, Hicks reveals that somewhere in the region of about 30% of the articles received for inclusion in the issue were rejected.

Reaching the point where such a dedicated women’s issue is possible didn’t occur in a vacuum, Hicks observes. The Medbikini fiasco that kicked off in 2020 lit a fire, she says. “There was sort of an influx of women stepping up to say ‘We’re here,’” she continues. “I think since then, we’ve seen a real presence of women in all aspects of vascular surgery, which is really exciting. This issue doesn’t really come out of the blue. It feeds off of that progress we have made in recent years.”
Strides toward better representation of women vascular surgeons in leadership positions continue to be made, Hicks says, with vascular surgery currently “bottom heavy in the societies because, out of training, we’re seeing 50/50 men vs. women, but 15 years ago it was not that way.”

The Women’s Vascular Summit, started by Linda Harris, MD, out of Buffalo, has also planted roots in recent years. “We continue to push forward and continue to champion the leaders that we have in our women’s group, and then create our own opportunities,” Hicks explains. “What has come out of the [SVS] election findings over the last couple of years has increased focus on the role of women in the vascular surgery space. Linda Harris has had a meeting for a few years now, and that group is going to codify into a women’s vascular society, which I think is exciting.”
Lately, just as the Annals issue was heading for publication, on a personal level Hicks had to confront a backlash to her contributions to the public conversation that followed the NYT exposé on inappropriateness in vascular care.
“I have done a lot of research in this space, and the motivation behind my research is to improve patient care, so when you do things for the right reasons and you get personally attacked, it’s always challenging,” she reflects. “There was definitely a component of ageism in the posts,” adding, “It’s always hard to know, but I do believe if I had been a male I wouldn’t have gotten that type of attack.”—Bryan
Kay
which she was invited to write the introduction.
continued from page 1
very little data, and go do it on a Friday night. You make mistakes; things bleed and clot; and you strive to go fix it. You walk into that operating room every day with high hopes.”
Many CEOs and the types of C-suite operators involved in the likes of mergers and acquisitions, on the other hand, walk into the room with “a whole different thought,” Freischlag said. Often, they assume things are going to fail, and “they may not always tell the truth.
That’s the opposite of the archetypal vascular surgeon, she continued. “What you need to do is get in those rooms and lead those processes, because that is who you are. You make good decisions, are able to own up to your mistakes, and you actually care—about your patients, teams, families and where you are going.”
Freischlag’s lecture was built around the theme of “Daring to do hard things. Detailing snapshots from her own journey—which, in addition to a lofty career trajectory, also included road bumps such as a divorce— she highlighted themes of resilience, diversity, mentorship and bravery in leadership.
She placed a particular emphasis on the importance of diversity in surgery, referencing the recent publication of the special women’s issue of Annals of Vascular Surgery, for
To illustrate the point, Freischlag detailed her first open aneurysm repair, in San Diego in 1987, when she was just 32 years old. The 82-year-old patient, who presented with a 6cm aneurysm, was due to undergo the procedure when Freischlag walked into the room to a less than rapt wider audience. “Her family was aghast,” she recalled. “Who is this kid, they were thinking, although the actual patient herself had no reservations, underwent the operation, and came out the other side, Freischlag said. The tale ended with Freischlag receiving two gifts from the lady and her family: a cross-stitched handkerchief crafted by the patient, along with an inscribed gold bracelet marking out the gratitude of the family. Freischlag cherishes the keepsakes still, explaining: “I was the most diverse vascular surgeon anybody saw doing that work back in the 80s— doing her procedure and trusting me, just like our patients trust us in our clinical trials. It’s really important that that continues to happen in all shapes and forms.”
Meanwhile, inclusive leadership means “you take somebody with you wherever you go. If you haven’t introduced one of your students, residents or fellows to somebody at this meeting, shame on you,” Freischlag implored. “You need to take them by the arm, introduce them to leadership, let them present ... Watching them grow to do it even better than you did is a wonderful feeling, and it makes the world a better place.”
Leadership is a journey, Freischlag added. It is about helping those around you, but, just like in her case, “it isn't always easy.” As the COVID-19 pandemic demonstrated, she said, “you get interrupted.”
8 Vascular Specialist | October 2023
FROM THE COVER: FREISCHLAG MARKS OUT VALUE OF DIVERSITY AND SURGEONS AS HOSPITAL LEADERS
“Female vascular surgeons constitute about 15% of the workforce, but remain underrepresented in vascular societies and NIH funding”
VALENTYNA KOSTIUK
Caitlin W. Hicks





A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the venous arena Editorially independent Subscribe today Available in print and digital formats and through our social channels *Available for US and EU readers only **Available worldwide Visit venousnews.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription**
BRIDGING KNOWLEDGE GAPS AND MEETING NEW DEMANDS OF VASCULAR SURGICAL TRAINING
This month in Corner Stitch, we highlight a trainee-centric study presented at the 2023 Midwestern Vascular Surgical Society (MVSS) annual meeting held in Minneapolis, Minnesota (Sept. 7–9). With the rise of Entrustable Professional Activities (EPAs) and the diminishing number of open aortic cases being performed across the country, this study from the group at Southern Illinois University provides an idea of how we may begin bridging these knowledge gaps and meeting the new educational demands coming to surgical training. For this, Christopher Audu, MD, interviews vascular surgery resident Scot Stanulis, MD, who presented his work on “Video-based self-assessment is an effective method of open surgical education for vascular surgery trainees.”
CA: In your study, your group evaluated open surgical skills using cadavers. Can you share the origin story for this idea? What prompted a cadaveric simulation study?
SS: An important topic in vascular surgery education at the moment, with the advent of integrated residencies and as the proportion of endovascular procedures increases, is that our residents may be exposed to fewer open vascular cases in their training. We wanted to start looking at solutions to this problem, and as we already have a great relationship with our surgical simulation lab, we thought this would be a natural start. The surgical literature, particularly in general surgery, shows promise for integrating more simulation into resident education, and we wanted to see if we could step it up a notch by including complete operations from skin-to-skin, and to see if video recordings, along with faculty and selfassessment, could increase the educational value.
CA: Bravo on taking on a really cool project to meet the need for open skills. How did you go about procuring permission from your anatomy department for this simulation? Is this something any residency can do to improve their resident/fellow open skills?
SS: Luckily, we already have a great relationship with our anatomy department, and many surgical subspecialties at our institution use the
surgical simulation lab for cadavericbased education. For standardization purposes, we needed to request cadavers that had not already underwent dissection in the operative field for a carotid endarterectomy (CEA), and we needed to ensure we could set up a live video-feed with overhead cameras. We were able to work with our simulation lab faculty to solve these pretty quickly. If a residency program does not already have access to cadavers, this would be a bigger obstacle to overcome; however, cadaveric education is an important part of robust simulation education, even outside of our project, and we would recommend any program strive to include some form of cadaveric education in their curriculum.
CA: In the paper you presented, you focused on carotid endarterectomies. What were the areas that the juniors improved in the most? Needle handling? Draping? Steps of the procedure?
SS: For our first exploration in videobased simulation, we chose CEAs for a few reasons: it is a procedure that all our residents had some exposure to; it has well-established, replicable steps, which aids in standardization; and it encompasses a broad range of vascular surgical skills.
In our experience with CEA, we found that the junior residents improved the most in the initial parts of the procedure, including draping and positioning, incision, and initial dissection and exposure. Additionally, there were some specific steps; for example, the PGY1

was able to clamp in the correct order the second time around; and the PGY2 improved at identifying each nerve during dissection. Our senior residents nearly aced our evaluation forms from the first attempt, so there was not much room for improvement—meaning we need to challenge them with more stringent evaluation criteria or a more difficult operation.
CA: That makes sense. What was your observed correlation between areas identified by the resident and those identified by the faculty? Can you infer anything about how a resident is able to assess their own growth?
SS: Residents and faculty were generally congruent on objective measures like “clamping order,” but for subjective measures like “overall proficiency” or even “proper nerve exposure,” we found more of a difference. We did see some improvement in resident self-assessment ability across sessions, but at this point it is clear that a junior resident will need faculty feedback to properly assess their operative performance, at least until they further develop their skill of self-assessment.
CA: That is very interesting. Did the improved residents notice greater autonomy in the operating room (OR) for carotid cases?
SS: At our program, our residents do already get a fair bit of autonomy, and it is hard to say how much that improved from this one experience, particularly as
our experience was blinded and the faculty did not get to see an individual resident’s improvement to then grant more autonomy. However, residents did say that they felt more confident and prepared going into their next CEA, and we do believe that this preparation can make it so residents get more out of their real cases once they have overcome some of the learning process in simulation.
CA: I see. So, one unintended benefit of this is improving resident/trainee confidence, which then translates into OR proficiency. How do you envision the platform being used for other vascular cases? Did your faculty find this a helpful exercise in their assessment of residents?
SS: I think the real benefit for this type of experience is augmenting surgical education in operations that our residents will see less often. Providing residents with confidence and foundational skills in open abdominal cases will be invaluable as we see a trend of residents reporting fewer of these cases in the endovascular era.
Faculty did report that it was useful to see the general weak points of residents so they could better direct teaching in the OR, but our experience was set up more for resident learning, and we did not assess if faculty improved at teaching or assessment.
CA: Right on. I suppose faculty evaluation of their teaching can be a future project. What open vascular operation are you going to do next?
SS: The next operation we will evaluate will be an open abdominal aortic aneurysm (AAA) repair. We chose this because we want to challenge our senior residents more, and see if this model holds up with a more complex operation. Challenges include keeping a larger operative field in the camera view, creating reasonable standardized evaluation forms, and increased time requirements in the simulation lab. If this model works for both a CEA and an open AAA, I don’t see many reasons that would prevent it from being used for a multitude of other open vascular surgery cases.
CHRISTOPHER AUDU is the Vascular Specialist resident/fellow editor. He is a resident at the University of Michigan in Ann Arbor, Michigan.

COMMENT& ANALYSIS CORNER STITCH 10 Vascular Specialist | October 2023
Christopher Audu (top) and Scot Stanulis
“At our program, our residents do already get a fair bit of autonomy, and it is hard to say how much that improved from this one experience, particularly as our experience was blinded and the faculty did not get to see an individual resident’s improvement to then grant more autonomy”
GOVERNMENT GRAND ROUNDS
Opportunity knocks as Congressional ‘busy season’ beckons
By Margaret C. Tracci, MD
WITH THE CONGRESSIONAL “BUSY SEASON” UPON us, the SVS is gearing up for big tasks ahead on the legislative and regulatory fronts. Having stepped into the role of chair of the SVS Advocacy Council this past June, I have to start by highlighting the generosity of our members and the service of surgeon-volunteers who have provided an incredibly strong foundation to build on for the work that lies ahead.
Mark Mattos, MD, and Peter Connolly, MD, led our political advocacy efforts (via the SVS Political Action Committee [PAC] Steering Committee) to achieve a new fundraising record during the last election cycle. This is due to all the donors who have provided invaluable resources to ensure that vascular surgery’s voice is heard on all of the matters important to our members. Already, incoming PAC Chair Yazan Duwayri, MD, is working with the advocacy staff to deploy these funds for maximum impact, including combining forces across specialties where there is common cause. In the upcoming year, we will build on the excellent grassroots efforts of the past year in establishing our “grass-tops”
REACH 535 program and supporting these volunteers in developing lasting relationships with members of Congress.
Some great opportunities are also on the horizon as Congress starts to ask long-overdue questions. A recent “Request for Information” issued in September by the House Ways and Means Committee notes, “Patients across America are facing increasing healthcare facility closures, travel distances and wait times, driven by a shrinking healthcare workforce, healthcare consolidation and patchwork financing models. This access challenge is uniquely difficult for patients and families living in rural and underserved areas in America.”
See the request at vascular.org/RuralHealthCareRFI
This is preaching to the choir—who knows these challenges better than vascular surgeons and patients? The committee “is seeking broad stakeholder input … with an emphasis on solutions to reshape our nation’s healthcare system and bring new access to care in rural and underserved areas.”

We are working to answer that, building on the work of the Population Health Task Force with the establishment of an SVS Health Policy Research Consortium to marshal what our researchers have learned about vascular deserts and access challenges in both rural and urban areas, and to enlist our own best minds to fill gaps in the data needed for the strongest, best-informed advocacy.
As the conversation about reform moves forward, from sustainable funding to more efficient and humane delivery, the SVS will also be working to build alliances to help physicians and patients speak with the single voice needed to rise above the cacophony of interested parties. This holds true for reform at the congressional level and certainly for the upcoming task at the Relative Values Scale (RVS) Update Committee
(RUC) of examining how lower-extremity interventions are valued—one in which SVS members can appreciate the foundation of expertise and credibility laid by leaders like Robert Zwolak, MD, Sean Roddy, MD, and Matthew Sideman, MD, and carried forward by Sunita Srivastava, MD, and David Han, MD, on the SVS Coding Committee.
And last, but not least, advocacy looks forward to hearing from SVS members about how we can help you where you are and about your interests and priorities. For instance, we hear from surgeons across the country that prior authorization practices and denials are becoming more onerous, seemingly by the day. The SVS has always worked to analyze and respond to these trends and to work hand-in-hand with members needing support in payer relations. The Society is exploring avenues to most effectively combat barriers to timely, high-quality care. Visit vascular.org/AdvocacyQuestion, or contact svsadvocacy@vascularsociety.org
11 www.vascularspecialistonline.com
MARGARET C. TRACCI is chair of the SVS Advocacy Council.
The SVS will also be working to build alliances to help physicians and patients speak with the single voice needed to rise above the cacophony of interested parties
COMMENT& ANALYSIS VETERANS
There was now 24/7 access postoperatively for the veteran that he or she knew how to use.4
patients cared for by the VA have equal to—if not better—outcomes than those cared for in the civilian world.7
By Amit Chawla, MD
DATA CAN BE GRANULAR AND clarifying. Conversely, data without appropriate context can lack nuance—like a paint-by-numbers portrait using only one crayon.
A recent article published by Becker’s Hospital Review, and promoted by the medical network Doximity, listed the top 10 hospitals with the lowest and highest rate of 30-day readmission based off data from the Centers for Medicare & Medicaid Services’ (CMS) Care Compare Website.1
Eight of the nine hospitals with the highest re-admission rate (I know it was supposed to be 10 but I didn’t write it; blame ChatGPT) are part of the U.S. Department of Veterans Affairs (VA) system.
This information has been in the press lately because facilities in the VA system are now being included in the CMS Overall Hospital Quality Star Ratings. The metric is based off five categories: mortality, safety of care, readmission, patient experience, and timely and effective care. Five stars is the maximum a facility can attain based on its aggregate score.
The dataset from CMS’ Care Compare website encompassed readmissions from July 1, 2018, through June 30, 2021.
However, the data in the article were isolated to July 2020 and June 2021: a heterogenous time pre- and postCOVID-19 vaccine filled with quarantining people who refused to go to the hospital.
In the United Kingdom, deaths at home rose by almost a third in 2020 while in-
PAYMENT CUTS
hospital deaths fell, except those related to COVID-19.2
It is difficult to glean accurate data on readmissions during this time. Furthermore, readmission at VA facilities occur due to manifold reasons: including housing uncertainty, mental health and lack of resources.
The main offender listed in the Becker article was the VA Pittsburgh Healthcare System (VAPHS). What the article doesn’t mention is that since that time, the Pittsburgh VA has implemented the Surgical Safety Net as championed by the Interdisciplinary Medical Preoperative Assessment Consultation and Treatment Clinic Impact team.3 This is a multidisciplinary clinic comprised of Anesthesiology, Care Management and Social Work Services, Office of Primary Care, Physical Medicine and Rehabilitation, and Surgery.4
The team used a prediction model to identify high-risk veterans for readmission after surgery. Members then used a nurse-navigator preoperatively to counsel patients and their families on what to expect perioperatively, as well as calls on post-discharge days two, five, 14 and 30. The Department of Physical Medicine and Rehabilitation (PRM) worked with prehabilitation for the patient. A telehealth team taught the patient and the family to use virtual devices, and provided hotspots if the family had no internet access.
SVS submits comment letter on Medicare fee schedule to CMS
By Beth Bales
IN SEPTEMBER, THE SOCIETY FOR VASCULAR Surgery submitted a detailed comment letter to the Centers for Medicare and Medicaid Services (CMS) in response to a proposed rule that could mean a 3–4% cut in Medicare payments.
The letter responds to CMS’ Calendar Year (CY) 2024 Medicare Physician Fee Schedule Proposed Rule (MPFS). SVS members are urged to address lawmakers on the issues, via grassroots advocacy. Pre-written messages are available at vascular.org/Grassroots
VAPHS dropped its readmission rate from 11.2 in October 2019 to 8.4 in October 2022. This program was selected as the winner for the VA’s 2022 Shark Tank competition. It is in trials at select sites across the country.
This article cherry-picks only readmissions from the list of components for the star system. Other factors, such as mortality and patient experience, have long been analyzed by the VA, especially in relationship to surgery. The American College of Surgeons’ National Surgical Quality Improvement Program for the VA has been used to improve risk-adjusted surgical outcomes.5
The VA has many metrics, such as SAIL (Strategic Analytics for Improvement and Learning Value Model), that it uses to grade its facilities. Started in 2012, SAIL uses 27 quality measures and two measures of overall efficiency and capacity to monitor such factors as acute-care mortality, access to care and employee satisfaction.6
To that very point, Becker’s Hospital Review published an article on July 26 reporting that 67% of the VA facilities eligible received four or five stars in the latest batch of CMS data.8 What a difference 27 days make.
References
1. https://www.beckershospitalreview. com/rankings-and-ratings/10-hospitalswith-highest-lowest-rate-of-unplannedreadmissions.html
2. https://www.ons.gov.uk/ peoplepopulationandcommunity/ birthsdeathsandmarriages/deaths/articles/ deathsathomeincreasedbyathirdin2020 whiledeathsinhospitalsfellexcept forcovid19/2021-05-07
3. https://news.va.gov/120638/castingsurgical-safety-net-reduce-readmissions/
4. https://marketplace.va.gov/innovations/ preventing-post-operative-readmissionswith-surgical-safety-net
5. ha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003; 348:2218–2227.
6. https://www.gao.gov/assets/700/699359.pdf
7. Blegen M, Ko J, Salzman G, et al Comparing Quality of Surgical Care
Between the US Department of Veterans Affairs and Non-Veterans Affairs Settings: A Systematic Review. Journal of the American College of Surgeons. 237 (2): p 352–61.
8. https://www.beckershospitalreview.com/ rankings-and-ratings/67-of-va-hospitalsreceive-4-or-5-star-cms-ratings-for-patientsafety.html
While historically not receiving the best press, the “modern” VA has made great strides with patient outcomes and satisfaction scores.
Many recent articles have found that
Depending on practice setting, vascular surgeons face a 3 to 4% cut based on current Medicare policies proposed in the MPFS rule.
These cuts result from a reduction in the temporary update to the conversion factor under current law and a negative budget-neutrality adjustment stemming in large part from CMS moving forward with implementation of separate payment for add-on code G2211 to account for visit complexity associated with certain office/outpatient evaluation and management visits. The code was initially proposed three years ago, but implementation was delayed as a result of an aggressive advocacy campaign led by surgical societies, including the SVS.
In addition, payment reductions for many vascular surgeons are compounded by the third year of CMS’ phased-in implementation of its clinical labor pricing update, which was finalized in the CY2022 MPFS Final Rule.
“Systemic issues such as the negative impact of the Medi-
AMIT CHAWLA is a member of the SVS Veterans Affairs Vascular Surgeons Committee. Chawla is chief of vascular surgery at Southeastern Louisiana Veterans Healthcare System in New Orleans.

care physician fee schedule’s budget neutrality requirements and the lack of an annual inflationary update will continue to generate significant instability for health care clinicians moving forward, threatening beneficiary access to essential health care services,” the letter includes.
The SVS, in collaboration with medical specialty societies, is continuing to work to mitigate the scheduled cuts and advance policies to stabilize the payment system in the short term and reform the system for the future.
To that end, the SVS supports legislation to provide an inflationary update for the MPFS (H.R. 2474) and is leading the effort that brought forth the introduction of legislation to provide targeted relief for codes most impacted by the clinical labor update policy (H.R. 3674).
The SVS is also seeking further delay of the G2211 code implementation via both regulatory and legislative initiatives. Read the letter to CMS at vascular.org/CMS.9.23
12 Vascular Specialist | October 2023
THE ‘MODERN’ VA HAS MADE GREAT STRIDES WITH PATIENT OUTCOMES AND SATISFACTION SCORES
“ While historically not receiving the best press, the 'modern' VA has made great strides with patient outcomes and satisfaction scores”
AFFAIRS
Amit Chawla
VASCULAR
merely Pollyanna! MVSS
vascular
Outgoing Midwestern Vascular Surgical Society (MVSS) President Jeffrey Jim, MD, used his recent presidential address to call upon vascular surgeons to spread the word far and wide—from Main Street to hospital C-suites—of what marks out vascular surgery as the truly “special” specialty.

JIM STRUCK ON FAMILIAR THEMES DURING THE talk at the 2023 MVSS annual meeting in Minneapolis, Minnesota (Sept. 7–9): the uniqueness of vascular surgery as a comprehensive provider of vascular care; the roots of the “vascular firefighter ” analogy; and the value of the specialty to a hospital system. He prefaced with a slight apologia that the content of his talk might lean pollyannaish, but his core purpose was unwavering: that “vascular surgery is the best”—and here is why...
What do patients do when they need medical help? “Call a medical doctor,” Jim expanded. “When a medical doctor needs help, who do they call? They call a surgeon. When a surgeon needs help, who do they call? A vascular surgeon.”
He delved into the necessity of vascular surgical presence in the context of case mix indexes so complicated, they cannot function without vascular being called in. Vascular surgery is the best, Jim told his audience—“and how can we keep it that way?”
So how should vascular surgeons go about doing so?
“We know [all this],” Jim continued, “but we need to spread the word. For the longest time we have been hiding out—walking in, walking out. We need to own vascular disease in the community.”
If that means heading out into the community to give a rudimentary talk about what vascular disease is, “you need to do it,” he implored. If the setting is a dinner with other healthcare providers, ditto, Jim said. “We need to let them know. We are the ones with the complete toolbox. We need to collaborate and explain what we do and how we can help them.”
Top of mind, too, should be letting leadership figures and hospital administrators in on the vascular story, “because I think we are very undervalued,” he commented. “People barely know what we do.”
It can play out along tired conversation lines, Jim outlined: “Are you in the cath lab? Are you doing open? Are you doing endo?
“We are much more than that,” he emphasized. “We are there to make sure we promote a safe environment, and we let them go ahead and do other service lines. We let them do other cases that otherwise they are not going to be able to do, because we are there to back them up. You need to take ownership and make sure people in your hospital system know that.”
Vascular surgeons also need to become the leaders of quality in vascular care, Jim said. “We may be small in number, but we are really knowledgeable. We happen to have very diverse experience of what we do. We need to look at patient outcomes and experience.”
Cost-effectiveness, too, requires vascular leadership, he pointed out—and independent of specialty. “We can’t just sit there and have arguments with people that we are better because we are vascular surgeons, or you’re not as good because you’re not. We need to talk about who is actually giving better cost-effective care.”
Jim also called out the special nature of vascular surgery
with “essentially the entire internet fed into them.”
Highlighting a pertinent use in daily vascular practice, he illustrated how he uses ChatGPT to circumnavigate CPT code acquisition. When searching for codes via Google, either the search engine gets the code wrong or “you end up on a site behind a paywall,” Ravin said.
in terms of how it plows an innovation trail. In that particular vein, he highlighted the Midwest region of the U.S. as particularly fertile ground.
“I think there is something unique about the healthcare system in the Midwest,” he said. “We have gigantic hospitals. Not that they don’t have big hospitals at UCLA, Stanford, LSU, but we have really big hospitals everywhere. We take care of a lot of surrounding areas, rural areas, and, because of that, I think we have the ability to get high, significant clinical volumes that you might not always get in the big populated city.”
Ergo, the opportunities to advance vascular care by innovation abound.
In his own case, Jim has become known for his special interest in carotid disease and his work with Silk Road to train vascular surgeons in the use of transcarotid revascularization (TCAR). “One of the things I am really proud of is when I go teach the course, I don’t care whether you do the procedure,” he said. “But if you are, I want to make sure you do it right— that’s what vascular surgeons do.”— Bryan Kay
The potential for large language-learning models like ChatGPT to take over tedious writing tasks such as emails and parts of PowerPoint presentations—or even be put to use to help collate Current Procedural Terminology (CPT) code data—was put to attendees of an artificial intelligence (AI) and social media issues session at the recent Eastern Vascular Society (EVS) annual meeting (Sept. 7–9) in Washington, D.C
Reid Ravin, MD, an attending vascular surgeon at ChristianaCare in Newark, Delaware, outlined the advantages of the generative technology, highlighting such AI technology’s ability to understand and generate human language using advanced mathematics and deep neural networks,
In the case of ChatGPT, “the entire internet lives inside of it.” Ravin demonstrated an example: for the past three procedures he carried out, he used the model to list the operations and work them up into a chart alongside a list of their relative value units (RVUs).
He also pointed out Aidoc, an AI-powered triage and notification system, which he said interfaces with electronic medical records to detect patients with specific pathologies.
He also pointed to potential dangers, such as in the case of systems like Aidoc, which could end up “pulling out patients that really don’t need screening—and people who end up getting procedures they don’t need.”— Bryan Kay
OUTGOING WESTERN VASCULAR SOCIETY (WVS) PRESIDENT WEI ZHOU, MD, used her presidential address to put out a call for the vascular specialty to embrace tolerance in order that it thrives amid rising cases of physician burnout and the mounting pressures of practice.
She was speaking during the 2023 WVS annual meeting held in Koloa, Hawaii (Sept. 9–12). “As a specialty we face many challenges,” she told her audience. “Some reflect differences in cultural background, training experience and personal priorities.”
Zhou, an immigrant from China, shared a personal experience, which involved a case in which she suffered illness while at work, dating from her time as an intern. “I tried to stay strong for the team and minimize my illness, scrubbing for a long pancreatic case,” she remembered. Eventually, Zhou threw up into her surgical mask about four hours into the case. As she was walking out of the operating room to clean herself up, she explained, the surgeon on the case declared before the surgical team that Zhou was “pregnant.” “He did not ask, he just assumed that pregnancy is the reason for nausea in a young woman,” she said. “On that day I lost my respect for that surgeon.” Zhou asked the WVS attendees to realize that “we are different,” and “we need to figure out other people’s perspectives.”
“To keep an honest discussion, we also need to explore our own points of view. Oftentimes, we can find more things in common than differences,” she added. That means empathy, Zhou continued.
“We don’t look like each other, sound like each other or act like each other. Being tolerant is not always easy. It requires us to accept our own limitations, look past our differences and accept each other’s flaws—and accept uncertainty.”—Bryan Kay
13 www.vascularspecialistonline.com
MIDWESTERN
Not
president outlines why
surgery is special and how ‘people need to know what we do’
PUTTING ARTIFICIAL INTELLIGENCE TO USE IN VASCULAR PRACTICE
EASTERN VASCULAR
WVS 2023 hears about importance of 'tolerance' in vascular specialty
WESTERN VASCULAR
“We are there to make sure we promote a safe environment, and we let them go ahead and do other service lines. We let them do other cases that otherwise they are not going to be able to do, because we are there to back them up”
JEFFREY JIM
Jeffrey Jim
Determining
By Beth Bales
A VASCULAR SURGEON’S VALUE INCLUDES FAR more than direct revenues from procedures performed, said SVS Robert Tahara, MD, recently. He told surgeons to remember not only these direct revenues, but also the help a surgeon provides other specialties in the hospital, as well as legal savings from “near misses—rarely considered and certainly rarely acknowledged.”
The total will add up to considerably more than the direct revenues usually cited, he told attendees at the 2023 SVS Vascular Annual Meeting (VAM). His presentation was part of the SVS Community Practice Section’s special educational session, “Recognizing, Enhancing and Promoting the Value of the Vascular Surgeon.”
The presentation covered a variety of financial topics, including whether to get a master of business administration degree, a surgeon’s ancillary value, incorporating the use of advanced practice providers and more.
The SVS for many years has sought to determine a vascular surgeon’s true value to his or her institution, Tahara said. An SVS Valuation Work Group produced “The Value of the Modern Vascular Surgeon to the Healthcare System,” report, which includes many of the details he planned to discuss. Tahara recommended surgeons read the report, which was published in February 2021 (visit vascular.org/PowellReport).
In terms of revenues, “Direct revenue is usually the only number physicians ever talk about,” he said. However, indirect (or enabling) revenue, from helping other specialties, and “near-miss” revenue, also are important.
The indirect revenue is that derived “from what we enable other non-vascular services to keep in the institution,” which can lead to increases in the case mix index (CMI). A higher CMI value indicates the hospital has treated more complex, resource-intensive cases, and the hospital may be reimbursed at a higher rate for such cases. “The CMI bump in indirect revenue is poorly accounted for and highly variable,” he said. In analyzing his work at his own facility, his work “added $650,000 a year.”
Tahara also highlighted the “near-miss value, the amount of money that we just saved that hospital by scrubbing in and over-sewing that big rip in the aorta or iliac. I get about one a year,” he said. In one such case, he said, he determined his work saved $300,000 in institutional legal fees, $100,000 in legal fees for him, and $130,000 for the patient.
With wrongful death settlements averaging $1 million, at -
Robert Tahara
torneys estimated that because of this patient’s age, had the “save” not occurred, a settlement in this case would have been $5 million instead.
“This is not a trivial amount of money and never gets accounted for. Your ‘near-miss value’ is never acknowledged, but the value is substantial,” Tahara said.
He recommended all surgeons log every near-miss, to assist when building data packages for compensation negotiations. “At least once a year you save one of these patients,” he told attendees.
CMI and near-miss contributions nearly double a surgeon’s financial value, Tahara said. “Do your homework before negotiating with your hospital about anything,” he told the crowd.
He summarized a vascular surgeon’s financial value: the direct revenue of $886,000; enabling revenue of $640,000; the CMI bump of $650,000; and the total from saved near-miss cases ($450,000 in legal fees plus approximately $1 million for a wrongful death settlement totaling $1.45 million). This brings a vascular surgeon’s full-time equivalent value to more than $3.62 million. “It adds up to almost double what’s quoted in the literature,” he said.
“It is critically important that the value that a vascular surgeon brings to an institution or facility is not unrecognized,” said Robert Molnar, MD, chair of the SVS Community Practice Section. “Vascular surgeons are the hub of the wheel, and we provide the essential base needed for any hospital system to offer multispecialty care.”

Registered VAM attendees can view the section’s session, held from 1:30–3 p.m. EDT on Friday, June 16, at vascular.org/OnlinePlanner23
14 Vascular Specialist | October 2023
BRANDING
a vascular surgeon’s value
“It is critically important that the value that a vascular surgeon brings to an institution or facility is not unrecognized. Vascular surgeons are the hub of the wheel and we provide the essential base needed for any hospital system to offer multispecialty care”
ROBERT MOLNAR
SVS WEBINAR COVERS INSIGHTS
LEARNED FROM EXPERIENCES OF MASS-CASUALTY DISASTERS
A mass shooting in Las Vegas. A bombing at the finish line of the Boston Marathon. A shooting at a Fourth of July parade. Beth Bales reports on a recent recounting of surgical life in disaster and crisis scenarios.

HEALTHCARE WORKERS MAY NOT be on the actual front line of disasters, but they’re definitely in the pipeline for the aftermath, when victims flood hospital emergency and operating rooms.
The question is, are those doctors, nurses, surgeons—and the institutions—ready?
Two trauma surgeons relayed their medical centers’ experiences with mass-casualty incidents during an “SVS Presents” webinar in August that focused on disaster preparedness. The webinar looked at mass casualties and how such incidents may affect the vascular surgery community. Moderator April Boyd, MD, PhD, chair of the SVS Education Committee, said SVS members told SVS leadership, in a needs assessment survey, that they want educational programs on leadership, particularly leadership in crisis.
Susan Briggs, MD, is an acute care and
VENOUS DISEASE
trauma surgeon and director of the International Trauma and Disaster Institute at Massachusetts General Hospital in Boston and discussed the 2013 Boston Marathon bombing. Deborah Kuhls, MD, is a trauma surgeon and medical director of University Medical Center’s Trauma Intensive Care Unit. She relayed the experiences at University Medical Center in Las Vegas following the 2017 shooting during the Route 91 Harvest music festival on the Las Vegas Strip.
Three people were killed in the bombing and hundreds were injured, including nearly 20 who lost limbs. In the shooting and its after math, 60 people died and more than 850 were wounded.
“Disaster medical care is not the same
as conventional medical care,” Briggs said. That’s in terms not only of the severity of the injuries but also how likely a patient is going to survive, as well as the available resources.
In the acute phase, providers are working on “minimally acceptable, not maximally acceptable, care due to the large number of victims,” she said, adding, “Both are difficult lessons.
“The key principle in a mass casualty event is that the critical patients with the greatest chance of survival and the least expenditure of time and resources are treated first.”
Vascular surgeons who partner with other physicians and surgeons frequently are invaluable members of a disaster preparedness team, both doctors said. Vascular trainees would be invaluable as well.
“They can work with other surgeons of any specialty,” said Kuhls. “They have special skills.”
Briggs said, “Vascular surgeons are surgeons first. They can help with almost any operation. More and more we’re getting away from titles and functional capabilities and helping each other. We utilized vascular surgeons in almost every case with trauma surgeons.”
In the 2017 Las Vegas shooting, the shooter fired 1,100 rounds of military-grade ammunition in 13 minutes, toward more than 22,000 people at a multi-day concert on the Las Vegas strip.
“We went from zero to 40 patients that were
New varicose vein management guidelines released

he SVS, in collaboration with the American Venous Forum (AVF) and the American Vein and Lymphatic Society (AVLS), has unveiled part two of the clinical practice guidelines for the management of varicose veins of the lower extremities. Building upon the foundation laid by part one, which was published online in October 2022, this latest installment offers evidence-based guidance to healthcare professionals and patients navigating the complexities of varicose vein care.
The new guidelines, endorsed by the Society of Interventional Radiology and the Society for Vascular Medicine, were published in the Journal of Vascular Surgery-Venous and Lymphatic Disorders in September, and are set to become a trusted resource for medical practitioners and individuals seeking effective varicose vein management strategies, according to co-primary author of the guideline writing group, Peter Gloviczki, MD.
SVS clinical practice guidelines are rooted in an evaluation of scientific literature, weighing the likely benefits and potential harms of various treatments.
The guideline writing group utilizes systematic reviews to distill key recommendations from the vast body of available evidence, ensuring that these guidelines remain both current and reliable.
Gloviczki emphasized the trustworthiness of the guidelines, stating, “These guidelines offer the most current and reliable source of information for both patients and healthcare providers.”
The guidelines address critical issues concerning the management of lower-extremity varicose veins, using the PICO
(patients, interventions, comparators and outcomes) framework to provide evidence-based answers to crucial questions.
Part I focused on the role of duplex ultrasound scanning in evaluating varicose veins and treating superficial truncal reflux. Part II delves into several aspects, including the prevention and management of varicose vein patients with compression, treatment with venotonic drugs and nutritional supplements. It also covers the evaluation and treatment of varicose tributaries, superficial thrombophlebitis, venous aneurysms and the management of complications associated with varicose veins and their treatment.
The guidelines place emphasis on incorporating contemporary endovascular venous interventions, both thermal and nonthermal procedures, aligning them with compression therapy and pharmacological treatment for managing varicose veins. The document encompasses a wide range of recommendations spanning parts I and II, ungraded consensus statements, pragmatic implementation notes and best-practice directives. It provides guidance for the appropriate management of patients with symptomatic lower-extremity varicose veins.
“When evaluating patients for varicose veins and conducting duplex ultrasounds, it is important that all physicians use the CEAP (Clinical-EtiologicalAnatomical-Pathophysiological) classification system.
All patients with varicose veins C2 disease should have duplex ultrasound evaluations to evaluate the reflux in the saphenous veins and other superficial veins. This exam should be performed with the patient standing, whenever possible,” said Gloviczki. Marlén Gomez
very critical within five minutes. Some had already died,” said Kuhls.
Because Las Vegas is a tourist destination used to hosting huge events, disaster training in different scenarios, particularly among the trauma centers, occurs at least quarterly, she said.
The shooting taught hospital leaders that “hospitals themselves need to be prepared, and not just individual healthcare workers,” said Kuhls. The Disaster Management Emergency Preparedness Course focuses on the institution as a whole, including how entire hospitals should go about doing drills and being prepared.
Both Briggs and Kuhls relayed other lessons learned during the respective events, which are available on the video recording.
The webinar was a collaborative effort of the SVS Education and Leadership Development committees, plus the Young Surgeons and Women’s sections.
The webinar can be viewed at vascular. org/MassCasualtiesWebinar. SVS members may watch at no charge; non-members will pay $35.
GUIDELINE WEBINAR SET FOR OCT. 10
A virtual roundtable on Oct. 10 will cover the new varicose veins guidelines. Set for 6–7:30 p.m. CDT, the session will address the latest in the diagnostic evaluation of patients with the venous condition using duplex scanning.
The assembled faculty will use case vignettes to design treatment strategies and demonstrate how to put the recommendations from the evidencebased clinical practice guidelines into practice.
Lead author Peter Gloviczki, MD, will introduce the guidelines and provide an overview.

Other topics and presenters are: diagnostic evaluation of vein incompetence, by Mark H. Meissner, MD; compression therapy for varicose veins, by Andrea T. Obi, MD; drug therapy for varicose veins, by Monika L. Gloviczki, MD; percutaneous endovenous ablations of saphenous veins, by Jose Almeida, MD; thrombotic complications of endovenous ablations, by Peter F. Lawrence, MD; and treatment of superficial thrombophlebitis, by Suman M. Wasan, MD.
Learn more and sign up at vascular.org/VVpart2Roundtable
15 www.vascularspecialistonline.com
“Vascular surgeons are surgeons first. They can help with almost any operation”
SUSAN BRIGGS
TRAUMA
T
VASCULAR
Peter Gloviczki
PAD
VASCULAR HEALTH STEP CHALLENGE EMERGES AS BEACON OF AWARENESS AND ACTION

This September, 533 people put their feet to the ground to raise awareness about peripheral arterial disease (PAD) as part of the SVS Foundation’s Vascular Health Step Challenge. The challenge raises funds and awareness, with participants pledging to walk 60 miles throughout the month, a symbolic journey that mirrors the 60,000 miles of blood vessels in the human body.
The annual initiative emphasizes the importance of vascular health and promotes healthy vascular habits. Funds raised during the challenge will support the future of vascular surgery and fulfill the Foundation’s mission.

New this year was the “Pay it Forward” initiative, allowing registrants to cover the $60 sign-up fee for low-in-
SVS Foundation Board of Directors welcomes two new members to its leadership team
come patients, ensuring their participation in the challenge.
The challenge saw a 77% increase in sponsorship compared to 2022. Sponsors include AOTI, Gore, Medtronic, 3M, the Way to My Heart organization, and the Society for Vascular Nursing (SVN).
Participants in the Step Challenge have more than just the goal of a healthier vascular system to strive for; prizes await. Those who achieve the 60-mile target will receive a backpack, and those who raise $600 or more will receive a Stanley drink cup. Team members that meet the $6,000 team goal will be able to sport a Step Challenge cap, and the top individual walker and fundraiser each will receive an outdoor blanket.
THE SVS FOUNDATION’S BOARD OF DIRECTORS announced the appointment of two new board members, Edith Tzeng, MD, and Palma Shaw, MD, at the board’s fall meeting in September. Tzeng was approved as the new chair of the Foundation Development Committee.
Tzeng is the University of Pittsburgh Medical Center chair, professor of surgery and chief of vascular surgery at the Veterans Affairs Medical Center in Pittsburgh, Pennsylvannia. She brings to the board her dedication to advancing vascular surgery research and education, focusing on the problems of blood vessels healing after injury, bypass or angioplasty, and the translational potential of nitric oxide and carbon monoxide for vascular healing.

“I am deeply honored to lead the Development Committee. Together with our dedicated team, we will continue to work diligently to support the Foundation’s mission and to further enhance the future of vascular surgery through research, disease prevention, community outreach and inclusivity,” said Tzeng.
Shaw, recently appointed chair of the Foundation’s Industry Relations Committee, comes to the board following a bylaws change that provides a board seat for that committee chair. She is a professor of surgery at the State University of New York Upstate Medical University program and a member of the division of vascular surgery at Upstate Medical Center in Syracuse, New York. Her clinical expertise includes aortic surgery, peripheral and venous intervention, diabetic foot management and wound care.
“I am thrilled to join the SVS Foundation board as the chair of the Industry Relations Committee. I look forward to working closely with our industry partners to advance the field of vascular surgery and improve patient care,” said Shaw.
 Gomez
Gomez
By Sept. 19, the campaign had already met its walker goal, at that point with 525 registered participants. In 2022, 457 walkers collectively raised over $80,000. Halfway through this year’s challenge, donations raised were at $60,000, and firmly on track to reach its target.— Marlén
Visit vascular.org/Step23
The Foundation’s board is committed to funding the future of vascular health through its four pillars: research and innovation, community vascular care and patient education, disease prevention, and diversity, equity and inclusion.—Marlén Gomez
To support the SVS Foundation’s work, donate today at vascular.org/FoundationDonation

16 Vascular Specialist | October 2023
The American Board of Surgery (ABS) discontinued CME credit self-claiming for Diplomates on July 1, 2023.
Information changes frequently.
for updates and more information at vascular.org/NewCreditProcess.
NEW
CME? SVS has you covered! vascular.org/NewCreditProcess
SVS is in the process of aligning its systems to meet these new requirements and is committed to fully complying with the new process.
Check
CONFUSED ABOUT THE
PROCESS FOR
NEW
BLOOD
Edith Tzeng Palma Shaw
OBITUARY
GEORGE LAVENSON, VIETNAM AND GULF WAR VETERAN, ADVOCATE FOR CAROTID DISEASE SCREENING IN SENIORS, DIES
By Benjamin W, Starnes, MD, Niten Singh, MD, and Todd Rasmussen, MD
George S. Lavenson Jr., lovingly referred to as “Doc” by his many friends, died Saturday, Aug. 19, 2023, on the beautiful island of Maui, Hawaii, where he chose to share a life in majestic Lahaina with his loving wife, Judy. He was 91. George leaves behind four children, Mark, Jim, Patricia and Dean, and three grandchildren, Kelsey, Luke, and Oliver.
As a vascular and general surgeon, George worked tirelessly up until his last days educating and advocating for screening seniors for stroke prevention. When not at his desk researching and writing, George enjoyed reading, cooking, photography, jazz, flying, surfing, cycling, and driving his bright candy-apple red Miata, or cruising on his yellow Harley Davidson motorcycle around the island.
Born in Tacoma, Washington, on Jan. 29, 1932, George graduated from the University of Washington in 1954, and the University of Washington School of Medicine in 1957. He completed his residency in general surgery at Tripler Army Medical Center in Honolulu in 1965. George went on to complete a vascular surgery fellowship at Walter Reed Army Medical Center in 1968 under the mentorship of Col. (retired) Norman Rich.
George served as a surgeon in the Vietnam War with the 24th Evacuation Hospital in Long Binh in 1968 and 1969, and was one of the pioneers of Doppler ultrasound to assess blood flow and viability in injured extremities on the battlefield. As an active-duty Army surgeon at the time, stationed at William Beaumont Army Medical Center in

REGIONAL ROUND-UP
Western Vascular Society presidency passes from Zhou to Fujitani
Roy M. Fujitani, MD, president of the University of California, Irvine (UCI) Medical Center medical staff, took over as Western Vascular Society (WVS) president at the conclusion of the WVS annual meeting recently held in Koloa, Hawaii (Sept. 9–12).

He accepted the mantle from outgoing WVS President Wei Zhou, MD, chief of vascular and endovascular surgery at the University of Arizona in Tucson.

Zhou delivered her presidential address on the importance of tolerance in vascular surgery in order for the profession to continue to thrive.
WVS 2023 also saw Alan Lumsden, MD, present as a presidential guest lecture on why innovation in vascular practice matters.
El Paso, Texas, George presented this first-of-its-kind experience as a study and manuscript from the podium at the International Society of Cardiovascular Surgery (ISCVS) in Philadelphia in June 1971. The paper was accepted two weeks later and published in Archives of Surgery (now JAMA Surgery) later that fall. Traveling to Philadelphia as an Army officer in 1971 and presenting this paper in uniform amidst the intense anti-war sentiments of the country at the time was undoubtedly an act of courage itself, not to mention the groundbreaking clinical results from their downrange experience using Doppler ultrasound.
Later in life, George returned to active duty during the Persian Gulf War with the 44th Evacuation Hospital in Saudi Arabia. Despite his civilian practice and then distance traveled when he lived in Lahaina, George had an unwavering commitment to military surgeons and trainees.
He showed up. George rarely missed the annual December meeting of the Military Vascular Surgery Society in Bethesda, Maryland. He made in-person visits to Walter Reed and the Uniformed Services University to see faculty, residents, and students. And, since Frank Veith, MD, started them at the VEITHsymposium in 2005 or 2006, George never missed sessions that are a tribute to military surgery.
For a decade-plus, as military surgeons were enduring deployments and caring for the injured during the Iraq and Afghanistan wars, George was present to discuss cases, provide his perspectives and, most importantly, his encouragement. Nothing epitomized George’s commitment to military surgery more than his volunteering to participate in the Society for Vascular Surgery Senior Visiting Surgeon Program, which included him spending time at Landstuhl Regional Medical Center in Germany during the height of the wars. After 20 years of service as an Army officer, George never abandoned the needs of military personnel, volunteering his trauma surgical and critical care skills at various times and in various locations.
Most recently, during the COVID-19 pandemic, George volunteered to participate in the Department of Defense’s global pandemic response teleconferences. George joined
SAVS makes travel scholarship applications call for 2024 meeting

The Southern Association for Vascular Surgery (SAVS) has put out a call for applications from medical students and general surgery residents for 20 travel scholarships now available to attend the 2024 SAVS annual meeting.

Applicants must be either a medical student in years 1–3 or a general surgery resident in PGY years 1–3 who are interested in vascular surgery and able to attend the meeting from Jan. 24–27 in Scottsdale, Arizona, the Society announced. Ten of the twenty scholarships are reserved for women and underrepresented minorities

The scholarships are worth $1,000, with the application deadline Oct. 18.
Mock oral examinations designed to prepare candidate members and vascular fellows for the Vascular Qualifying Examination are again taking place at the meeting and set for Jan. 24. The application deadline is Nov. 1 at 11:59 p.m. (EDT).
The meeting will also play host once more to a Simulation Skills Competition. The application deadline is Nov. 1, also at 11:59 PM (EDT).
remotely during the spring of 2020 from his home in Lahaina, astutely pointing out the similarities between COVID-related pulmonary dysfunction and lessons he and his generation had learned from managing Da Nang lung in the combat-injured in Vietnam five decades earlier. George was enthusiastic in conveying his wartime critical care experience, and his perspective as to how today’s Military Health System might optimize management of pulmonary failure amidst the pandemic.
In addition to his years of military service, George had a busy clinical practice in Visalia, California, for 30 years, serving as chair of the Department of Surgery from 1978–1983.
Amongst George’s proudest achievements in civilian medicine was development of a cost-effective stroke prevention screening protocol involving the “LAV Scan” after his own name. George’s innovation and lifelong advocacy for stroke prevention was recognized and honored by the Western Vascular Society as recently as last year. On his deathbed on Aug. 17, George wrote his final statement:
1. Carotid artery disease is the leading immediate cause of strokes.
2. Some 80% of cases in carotid artery disease are asymptomatic prior to the stroke that it causes.
3. The only possible means of reducing strokes in a large epidemiology scale is to find asymptomatic carotid disease so that a stroke can be managed preventively by screening senior populations for asymptomatic carotid disease.
4. Controls for proper application can be applied.
5. How to screen seniors: The only way to find carotid artery disease is to screen seniors, which can be done with a LAV Scan.
George’s presence was a constant for decades and he will be greatly missed. But rest assured George’s legacy lives. Rest in peace George. Mahalo.
Online condolences: www.NormansMortuary.com Donations in George’s honor can be made to The Red Cross Maui Disaster Relief Fund.
Aulivola takes over Midwestern Vascular reins
Bernadette Aulivola, MD, the division director of vascular surgery and endovascular therapy at Loyola University in Maywood, Illinois, took over as president of the Midwestern Vascular Surgical Society (MVSS) at the conclusion of the MVSS annual business meeting held in Minneapolis, Minnesota, on Sept. 8.


Aulivola succeeded Jeffrey Jim, MD, the 2022–23 MVSS president, who is chair of vascular and endovascular surgery at Allina Health Minneapolis Heart Institute in Minneapolis.
Patrick Muck, MD, chief of vascular surgery at Good Samaritan Hospital in Cincinnati, Ohio, who previously was an MVSS councilor, is the new president-elect of the Society for 2023–24.
Ozsvath assumes Eastern Vascular presidency
Kathleen Ozsvath, MD, a vascular surgeon at St. Peters Health Partners in Albany, New York, took over as president of the Eastern Vascular Society (EVS) during the 37th EVS annual meeting that took place in Washington, D.C. from Sept. 7–9.
Ozsvath assumed the mantle following the Society’s business meeting on Sept. 8, before which the 2022–23 EVS President Peter Faries, MD, who is chief of vascular surgery at Mount Sinai in New York, delivered his parting presidential address before the assembled attendees at EVS 2023.
The meeting also featured Michael Marin, MD, as a keynote speaker. He regaled the gathering with his work taking his know-how to those in need in Uganda.
Peter Faries departs the EVS stage in D.C., passing the presidency onto Kathleen Ozsvath
17 www.vascularspecialistonline.com
George Lavenson
Jeffrey Jim hands over to Bernadette Aulivola the MVSS presidential reins in Minneapolis
Roy M. Fujitani is passed the Western Vascular gavel by Wei Zhou after taking over as WVS president
SOCIETY BRIEFS
Prepare to submit research for VAM 2024
Compiled by Beth Bales and Marlén Gomez
Applications open for awards, grant
APPLICATIONS OPEN THIS month for the SVS Excellence in Community Practice Award and the Sub-Section on Outpatient & Office Vascular Care (SOOVC) Research Seed Grant and Presentation Award.
ORGANIZING A VAM TAKES A WHOLE lot of time and a whole lot of longrange planning.
Thus, members of the SVS Postgraduate Education Committee (PGEC) have already evaluated the 90 submitted proposals (an SVS record) for educational sessions at VAM 2024. And Program Committee members, who select the scientific abstracts, are looking ahead to the November opening of the abstract-submission site.
Researchers can submit abstracts for possible inclusion from Nov. 15 through Jan. 10, 2024.
“The science is a critical part of the Vascular Annual Meeting,” said Program Committee Chair Andres Schanzer, MD. “While VAM of course offers opportunities for participants to get together for meetings, exhibits, dinners, catching up with friends and casual events, the scientific and educational sessions continue to be a main highlight. We received the most PGEC submissions in the history of the meeting and hopefully will do the same with the upcoming scientific abstract submissions.”
Many VAM sessions feature abstract presentations, including the large-scale plenary sessions; the International Young Surgeons and International Poster competitions; the International Fast Talk and International Forum scientific sessions; the Vascular and Endovascular Surgery Society (VESS) presentations; the “How I Do It” video session; and the Poster Competition.
VAM 2024 will be held June 19–22 at McCormick Place in Chicago. Educational sessions will run across all four days.

Coding workshop just a few weeks away
THE CHANCE TO LEARN THE NEWEST wrinkles in coding and reimbursement for vascular surgeons is just a few short weeks away. The annual SVS Coding and Reimbursement Workshop will be held Oct. 16 and 17 at the OLC Education and Conference Center, 9400 W. Higgins Road, in Rosemont, Illinois.
The workshop provides a review of current coding and reimbursement information. An optional Evaluation and Management (E/M) Workshop precedes the full workshop from 8 a.m.–12 p.m. CST on Oct. 16.
The Coding and Reimbursement Workshop is 1–5 p.m. on Oct. 16 and from 7:30 a.m.–4:30 p.m. on Oct. 17.
VAM 2024 GALA SET FOR CHICAGO’S MUSEUM OF SCIENCE AND INDUSTRY
DURING THE VASCULAR ANNUAL MEETING THAT CELEBRATES science and research, the SVS Foundation’s annual Gala will take place in a museum that also honors science. “A Night at the Museum—A Celebration of Science” is set for Friday, June 21, 2024 at Chicago’s world-famous Museum of Science and Industry.
Chairs of the 2024 Gala are Michael Dalsing, MD, chair of the SVS Foundation; Bernadette Aulivola, MD, member of the SVS Foundation Board of Directors; and Leigh Ann O’Banion, MD, co-chair of the 2023 Gala.
Tickets for this annual event, which typically sell out quickly, will go on sale in March. Included in the evening are transportation to the museum, live and silent auctions, plated dinner, dancing to a DJ, and much more. “Guests will be able to visit the exhibits on the main floor, which is where the event will be located,” said O’Banion. That includes the museum’s “Yesterday’s Main Street,” the Coal Mine, “Numbers in Nature: A Mirror Maze” and exhibits on “The Great Train Story” (in the Transportation Gallery), “Science Storms,” “Extreme Ice,” “Earth Revealed,” and more. “I practice in Chicago and am no stranger to this fantastic museum,” said Aulivola. “I’m thrilled that we’ve secured this location for our upcoming Gala and I cannot wait to show it off to our Gala attendees. I am certain that this will be an incredibly fun event for all.”

For information contact Catherine Lampi at clampi@vascularsociety.org
Alert! Pay SVS 2024 member dues by Dec. 31.
SVS MEMBERS MUST ACT BEFORE the end of the year to avoid interruption of their 2024 membership benefits. Members can pay their dues on or before Dec. 31 to support the SVS mission and advance vascular health.
Membership renewal includes continued access to all membership benefits, including all Journal of Vascular Surgery publications at reduced or no cost, access to the SVS Education Portal, reduced rates to VAM and more.
Members can pay their dues at
vascular.org/invoices; login is required. While paying their dues, members can also donate to the work of the SVS Foundation.
Additionally, members also can update their SVS profiles, including adding mobile numbers to receive infrequent text alerts on critical society communications, such as dues renewals and election notices when updating their SVS profiles.
For questions, email membership@ vascularsociety.org
The Excellence in Community Practice Award honors members who have exhibited outstanding leadership within his or her community as a practicing vascular surgeon. Criteria include a minimum of 20 years as a practicing vascular surgeon and minimum of five years as an SVS member.
Applicants/nominees must present evidence of leadership in a community-based practice, such as implementation of services or innovations to advance community health, partnerships or collaborations with organizations in the community, and contributions that elevate the stature of the specialty of vascular surgery in the community.
Learn more at vascular.org/ CommunityPracticeAward Applications close Feb. 1.
The SOOVC Presentation Award recognizes vascular surgeons who have completed clinical research projects in an office-based lab (OBL) or ambulatory surgery center (ASC). Three recipients will be selected for the award.
The Research Seed Grant supports research in an OBL or ASC practice, providing vascular surgeons with funds for a data analyst to analyze research data for actionable insights, quality improvement and patient care. Three recipients will be selected, and each will receive a $10,000 grant.
Visit vascular.org/ SOOVCResearchGrant and vascular. org/SOOVCPresentationAward Applications close Jan.15.
MATTHEW CINDRIC, MD, has been named the new chief of vascular surgery at Mon Health Medical Center in Morgantown, West Virginia.
18
Vascular Specialist | October 2023
SPOT LIGHT In memoriam
RAYMOND E. KENNEDY, MD, 34, of Highland Park, New Jersey, a PGY5 integrated vascular resident (and chief resident of vascular surgery) at the Rutgers Robert Wood Johnson Medical School, Aug. 27, in California.
Pictured at the 2023 Gala are Leigh Ann O'Banion (top), and (bottom, left to right) Anna Boniakowski, Bernadette Aulivola, Dawn Coleman and Misty Humphries
CLINICAL&DEVICENEWS
two 42 cm long HAVs to achieve the required bypass length. The Mayo team, led by Todd Rasmussen, MD, reported that the operations to implant the HAV achieved a 100% technical success rate, without any HAV-related major adverse events reported. At a median follow-up of nine months, the secondary patency rate for patients implanted with the HAV was 72%. The limb salvage rate was 86%, corresponding to only a 14% amputation rate.
release reported that the single-arm clinical trial was a success and showed that the HAV in this study had higher rates of patency, and lower rates of amputation and infection, compared to historic synthetic graft benchmarks. Humacyte plans to file a Biologics License Application (BLA) for the treatment of vascular trauma with the FDA during the fourth quarter of 2023.
AN INVESTIGATOR-SPONSORED CLINICAL STUDY conducted at the Mayo Clinic in Rochester, Minnesota, of the investigational Human Acellular Vessel (HAV) in patients with chronic limb-threatening ischemia (CLTI) was presented at the Midwestern Vascular Surgical Society (MVSS) annual meeting in Minneapolis, Minnesota (Sept. 7–9).
Delivered by Sebastian Cifuentes, MD, from the Department of Vascular and Endovascular Surgery at the Mayo Clinic, the researchers concluded that in the clinical study the HAV was a safe, resilient, and effective conduit for arterial bypass and limb salvage.
The presentation reported the outcomes of 29 patients— with a mean age of 71 who had no available vein to use as a bypass graft—who underwent HAV implantation. Of these patients, 97% had previously experienced unsuccessful revascularization procedures on the extremity and 21 (72%) had tissue loss or gangrene. Based on the state of this disease, this patient group had a 30–50% one-year risk of amputation. Notably, surgery in 22 (76%) patients necessitated a tibial artery target, a surgical procedure involving the fusion of
FDA clears AAA-SHAPE trial for IDE approval
SHAPE MEMORY MEDICAL RECENTLY announced that the Food and Drug Administration (FDA) has granted investigational device exemption (IDE) for the company to begin a prospective, multicenter, randomized, open-label trial to determine safety and effectiveness of the Impede-FX RapidFill device to improve abdominal aortic aneurysm (AAA) sac behavior when used with elective endovascular aneurysm repair (EVAR).
A press release details that AAA-SHAPE (Abdominal aortic aneurysm sac healing and prevention of expansion) will enroll 180 patients with infrarenal AAAs across 40 sites in the U.S., Europe, and New Zealand. Study participants will be randomized 2:1, either to EVAR plus sac management with Impede-FX RapidFill (the treatment arm) or to standard EVAR (the control arm). Key endpoints will compare sac diameter and volume change, endoleak rates, secondary interventions, and mortality through five years.
The investigational device, Impede-FX RapidFill, incorporates the novel shape memory polymer, a proprietary, porous, polyurethane scaffold that is crimped for catheter delivery and self-expands upon contact with blood.
“In a complex cohort of patients with CLTI and no autologous options, the HAV is a safe and effective arterial bypass conduit,” Cifuentes reported at MVSS 2023. “This experience using the Food and Drug Administration (FDA) Expanded Access Program provides real-world data that can inform regulatory deliberations and future trials of the HAV. Further studies will evaluate the HAV as a first-line bypass conduit to define patency and limbsalvage potential in less severe cases of CLTI.”
The HAV, a bioengineered tissue, is under investigation as an infection-resistant alternative for revascularization. Designed to be ready off-the-shelf, the HAV has the potential to save valuable time for surgeons and to reduce discomfort and complications for patients. The HAV has accumulated more than 1,000 patient-years of experience worldwide in a series of clinical trials in multiple indications, including vascular trauma repair, arteriovenous access for hemodialysis, and PAD, Humacyte, the company behind the product, reports. The HAV is an investigational product and has not been approved for sale by the FDA or any other regulatory agency.
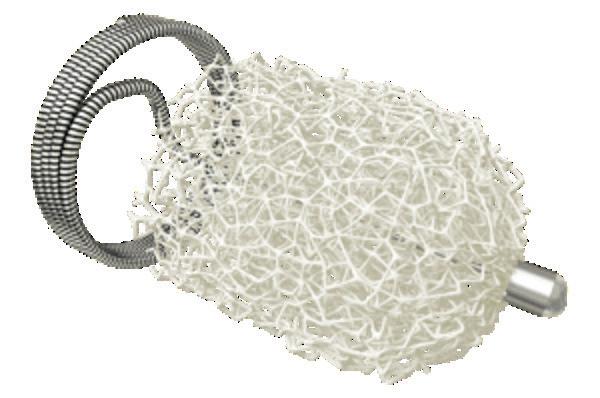
Meanwhile, Humacyte also announced positive top line results from its V005 Phase 2/3 trial of the Human Acellular Vessel (HAV) in vascular trauma repair. A company press
The V005 trial was a single-arm study conducted in the U.S. and Israel in patients with arterial injuries resulting from gun shots, workplace injuries, car accidents, or other traumatic events. Patients enrolled in the study did not have the standard of care, saphenous vein, available to use as a bypass graft. As a result, had the patients not received the HAV, they likely would have been treated with synthetic grafts, ligation of the bleeding artery, and/or amputation.
In AAA-SHAPE, Impede-FX RapidFill is intended to fill the aneurysm blood lumen around a commercially-available EVAR stent graft to promote aneurysm thrombosis and sac shrinkage.
The AAA-SHAPE pivotal trial is preceded by the AAA-SHAPE early feasibility studies which enrolled a combined 35 patients in New Zealand and The Netherlands. This early experience was recently described by Andrew Holden, MD, et al in the Journal of Vascular Surgery: Cases, Innovations, and Techniques
“The AAA-SHAPE early feasibility studies have been key to validating the procedural techniques and best practices that we will leverage in the pivotal trial,” said Marc Schermerhorn, MD, chief of vascular and endovascular surgery at Beth Israel Deaconess Medical Center in Boston, and principal investigator of
GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis
INDICATIONS FOR USE IN THE U.S.: The GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis is indicated for the treatment of de novo or restenotic lesions found in iliac arteries with reference vessel diameters ranging from 5 mm – 13 mm and lesion lengths up to 110 mm, including lesions at the aortic bifurcation.
CONTRAINDICATIONS: Do not use the GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II. Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available.
19 www.vascularspecialistonline.com
Human Acellular Vessel, evaluated in complex cohort of CLTI patients, proves 'safe, effective bypass conduit'
Compiled by Jocelyn Hudson and Bryan Kay
Consult Instructions for Use eifu.goremedical.com
Products listed may not be available in all markets. GORE, VBX, VIABAHN and designs are trademarks of W. L. Gore & Associates. © 2021 W. L. Gore & Associates, Inc. 21100151-EN APRIL 2021
Impede-FX
Sebastian Cifuentes reports results from a recent study of the Human Acellular Vessel in a cohort of CLTI patients
LONG-TERM DURABLE CLINICAL OUTCOMES IN COMPLEX AORTOILIAC OCCLUSIVE DISEASE

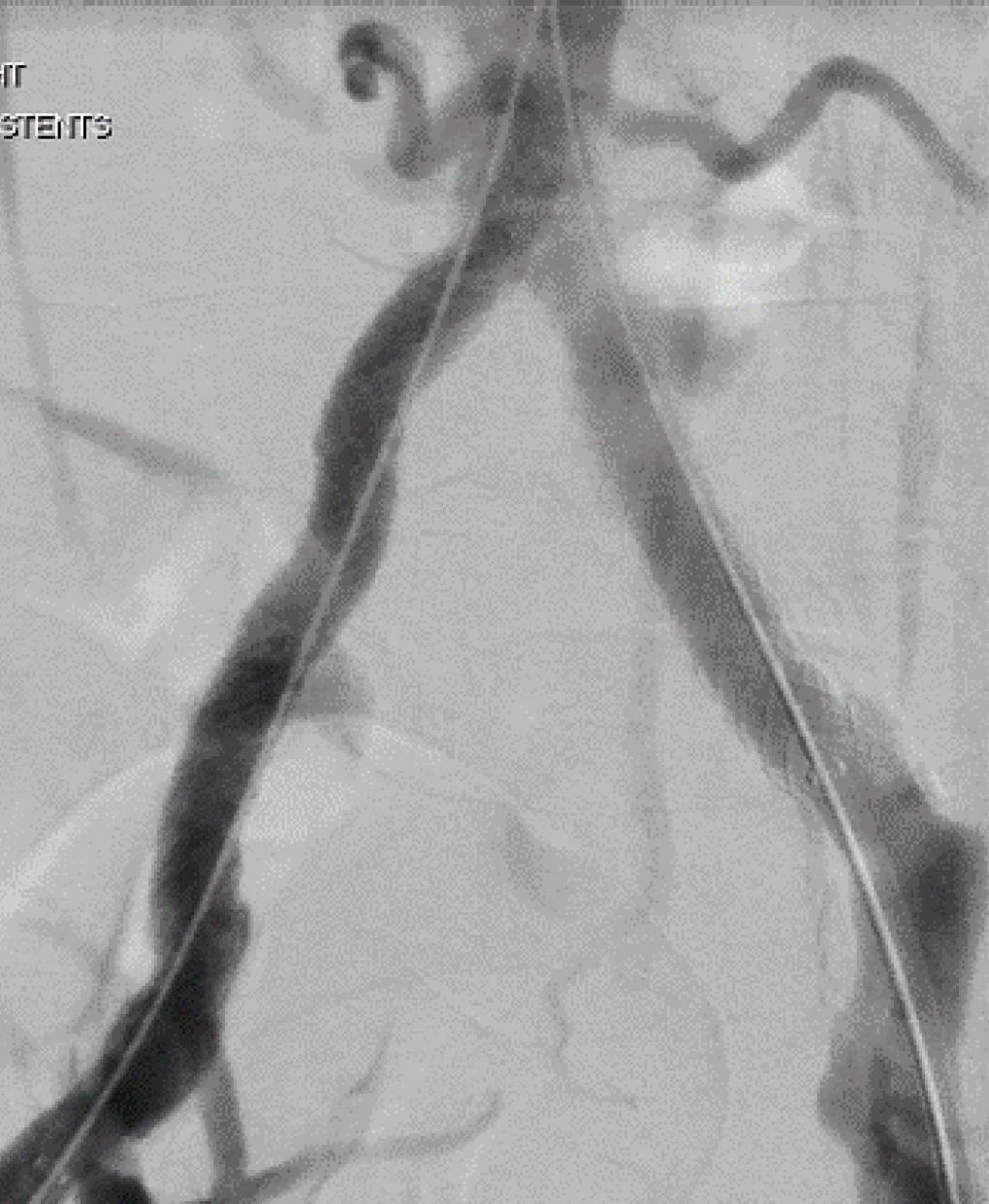
Sustained clinical effectiveness through five years1:








freedom from target lesion revascularization per subject 8.% primary patency per lesion .%



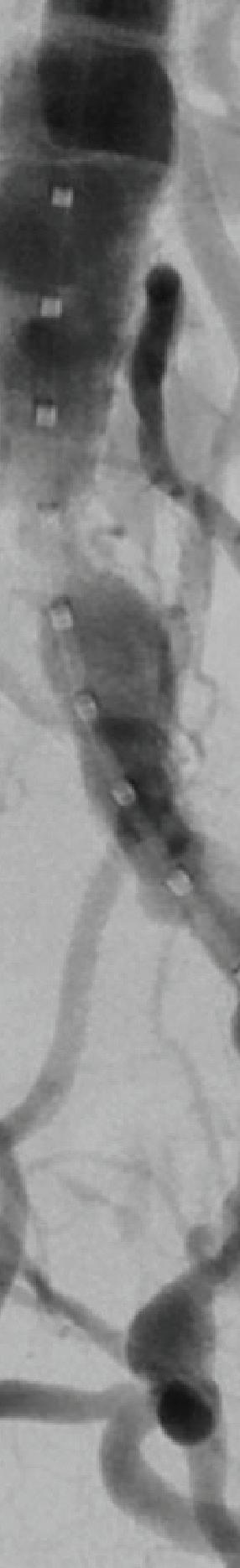
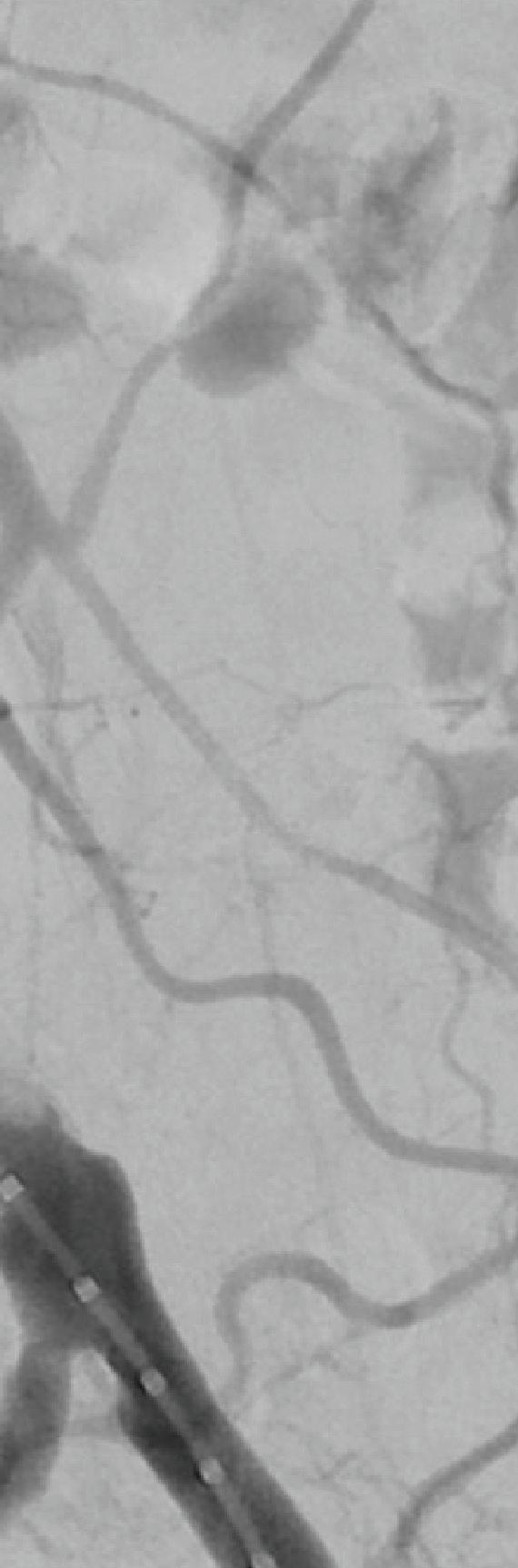

W. L. Gore & Associates, Inc. Flagstaff, Arizona 86004 goremedical.com
Please see accompanying prescribing information in this journal.
Products listed may not be available in all markets.
GORE, Together, improving life, VBX, VIABAHN and designs are trademarks of W. L. Gore & Associates.































© 2023 W. L. Gore & Associates, Inc. 23938719-EN APRIL 2023
See the data

After Before
1. Holden A, Takele E, Hill A, et al. Long-term follow-up of subjects with iliac occlusive disease treated with the Viabahn VBX Balloon-Expandable Endoprosthesis. Journal of Endovascular Therapy. In press.
GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis














 Distal Tip
† Compared to surgical arteriovenous fistulas.
Distal Tip
† Compared to surgical arteriovenous fistulas.










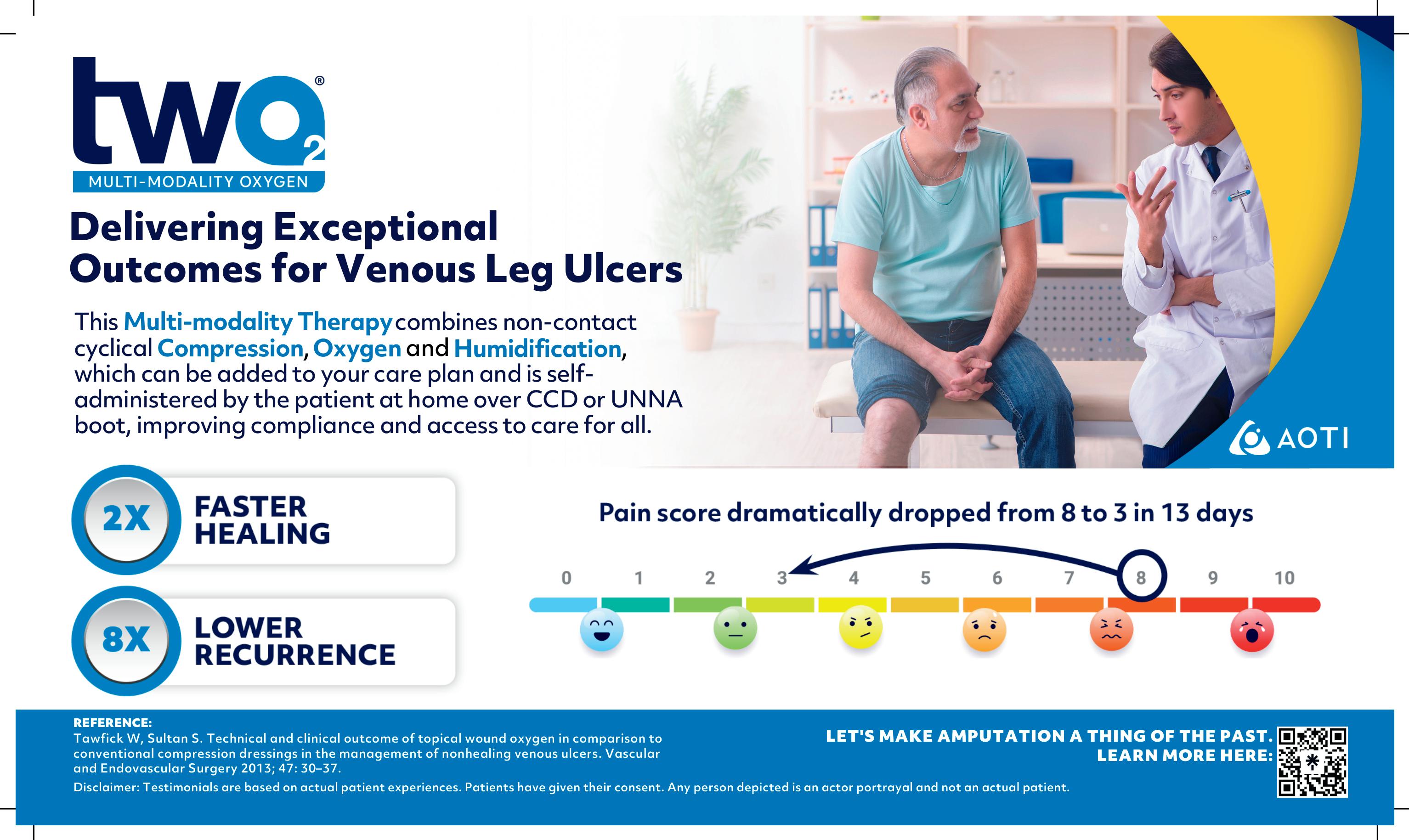









 Gomez
Gomez