Finding space to breathe
Respiratory Health issue | Reflux, Lung Cancer, Thoracoscopy, IBD Complications, Incidentalomas
MAJOR PARTNER
September 2020 www.mforum.com.au
Dr Divya Sabharwal Avant member
Leading support in your times of need – it’s why more doctors choose Avant Avant is more than an insurer, we provide holistic support for doctors that helps them practise at their best through challenging times. Award-winning defence A 270-strong* team including Australia’s largest health law firm recognised for their expertise, providing members with on-the-ground support in six states and territories.
Advocating for your interests As Australia’s leading medical defence organisation, we use our loud and credible voice to affect positive change to health policy, such as on telehealth and PPE provision during the COVID-19 pandemic.
Financial stability to protect you Avant’s financial stability means we can offer a range of assistance to members and ensure we are here to protect doctors for years to come.
Join today 1800 128 268 avant.org.au IMPORTANT: Professional indemnity insurance products are issued by Avant Insurance Limited, ABN 82 003 707 471, AFSL 238 765. The information provided here is general advice only. You should consider the appropriateness of the advice having regard to your own objectives, financial situation and needs before deciding to purchase or continuing to hold a policy with us. For full details including the terms, conditions, and exclusions that apply, please read and consider the policy wording and Product Disclosure Statement, which is available at avant.org.au or by contacting us on 1800 128 268. *Accurate as at 8/5/2020. MJN-219.4 08/20 (DT-1455)
EDITORIAL BACK TO CONTENTS
Jan Hallam | Managing Editor
Sharing the load
We spend a bit of real estate in this issue exploring the increasingly complex world of public messaging. We are getting a heck of a lot of it, but are we getting it straight? As you will read, trust is the essential ingredient, yet how do we maintain that trust when the messengers start to obfuscate. Politicians are the past masters of the art. While politicians have shown themselves surprisingly (some pundits might think alarmingly) candid over the past six months, it has been in fact their public-servant sidekicks in the limelight. It is the dawn of the celebrity bureaucrat.
It is the dawn of the celebrity bureaucrat.
These previously faceless public servants have spent the better part of their careers avoiding a microphone and a spotlight except for the occasional summons to an estimates committee hearing or a parliamentary inquiry. Both occasions require a fortifying breakfast but never full hair and make-up. Now they are fronting up to daily media conferences, fully exposed as responsible for political decision-making during the pandemic because we are constantly being told that decisions are based on expert advice. It can only be assumed that, as such, messaging will be a much deeper deliberation between the arms of government. Politicians are notoriously flighty with the facts when bad news threatens their electoral stocks, but there is a natural counterbalance – opinion polls and elections. Our democracy doesn’t have the same inbuilt safeguards when it comes to our public service. That’s the point, really. It sails on while politics navigates the rocks. Therefore, we need a vigorous watchdog to keep tabs on transparency and good governance. Still, there is much to celebrate in the new era of the visible bureaucrat. As they become identifiably responsible for the public messaging, we can expect much more from their policy making and their communications. The era of ‘yes minister’ is hopefully a victim of coronavirus and open and frank communication will replace the spin.
SYNDICATION AND REPRODUCTION Contributors should be aware the publishers assert the right to syndicate material appearing in Medical Forum on the MedicalHub.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publishers for copyright permission. DISCLAIMER Medical Forum is published by HealthBooks as an independent publication for health professionals in Western Australia. The support of all advertisers, sponsors and contributors is welcome. Neither the publisher nor any of its servants will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the publisher or its contributors for the promoted product, service or treatment. Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Trades Practices Act 1974 as amended. All advertisements are accepted for publication on condition that the advertiser indemnifies the publisher and its servants against all actions, suits, claims, loss and or damages resulting from anything published on behalf of the advertiser. EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 1
CONTENTS | SEPTEMBER 2020 – RESPIR ATORY HEALTH ISSUE
Inside this issue 10 14 24 18 FEATURES
NEWS & VIEWS
LIFESTYLE
10 Close-Up:
1
50 Doctors Orchestra 51 Wine Review: Schild Estate
Professor Fiona Lake
14 Vaccine Research – Professor Tobi Kollmann
18 The rise of Public Health 24 Contact Tracing
Editorial: Sharing the load – Jan Hallam
6 In the News 7 In Brief 28 Vale Harry Nespolon 30 Foot & Ulcer Clinic
– Dr Craig Drummond
Doctors Dozen... Dr Alison Stubbs from UWA Medical Centre is the winner of the Vasse Felix Doctors Dozen. For your chance to win a dozen bottles of premium wines from Schild Estate, see the review on Page 51 and go to the website to enter www.mforum.com.au (click on the competitions tab)
CONNECT WITH US /medicalforumwa
/MedicalForum_
2 | SEPTEMBER 2020
/medical-forum-wa-magazine
www.mforum.com.au
info@mforum.com.au
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
CONTENTS
PUBLISHERS Karen Walsh – Director Chris Walsh – Director chris@mforum.com.au
Clinicals
ADVERTISING Advertising Manager Gary Sullivan (0403 282 510) mm@mforum.com.au
5
Infective exacerbations of COPD Dr David New
32
Breathe easier Dr Joe Kosterich, Clinical Editor
35
Reflux-induced respiratory disease Dr Michael Prichard
37
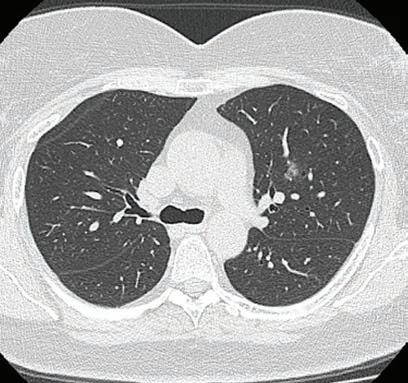
Lung cancer staging Dr Hilman Harryanto
39
Rethinking mental health Dr Jenny Brockis
40
Incidental findings on cardiac CTs. Dr Scott Claxton
45
Video thoracoscopy in empyema Dr Parshotam Gera
47
Oral manifestations of IBD Dr Amanda Phoon Nguyen
48
Smoking in underground metal mines E/Prof Odwyn Jones
EDITORIAL TEAM Managing Editor Ms Jan Hallam (0430 322 066) editor@mforum.com.au Journalist James Knox (08 9203 5222) james@mforum.com.au Clinical Editor Dr Joe Kosterich (0417 998 697) joe@mforum.com.au Clinical Services Directory Editor Karen Walsh (0401 172 626) karen@mforum.com.au GRAPHIC DESIGN Thinking Hats studio@thinkinghats.net.au INDEPENDENT ADVISORY PANEL for Medical Forum John Alvarez (Cardiothoracic Surgeon), Astrid Arellano (Infectious Disease Physician), Peter Bray (Vascular Surgeon), Pip Brennan (Consumer Advocate), Joe Cardaci (Nuclear & General Medicine), Fred Chen (Ophthalmologist), Mark Hands (Cardiologist), Kenji So (Gastroenterologist), Alistair Vickery (General Practitioner: Academic), Olga Ward (General Practitioner: Procedural), Piers Yates (Orthopaedic Surgeon)
Guest Columns
CONTACT MEDICAL FORUM Suite 3/8 Howlett Street, North Perth WA 6006 Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
4
Hey WA – It's OK to be OK! A/Prof Erin Smith
8
Care Can’t Wait Dr Tony Bartone
MAJOR PARTNER
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 3
Hey WA – It's OK to be OK! With Victorian COVID numbers spiking dangerously, A/Prof Erin Smith writes about minimising feelings of ‘survivor guilt’. In the middle of July, in the heart of Perth’s financial district, West Australians were beginning to return to office buildings after months of working from home. Life was starting to get back to normal as coronavirus restrictions in the state eased. But everyone’s pandemic experience is unfolding differently and there is no denying that it has been devastating for many people in WA and around the world. At the worst end of the public health emergency spectrum are the millions of cases and hundreds of thousands of people who have died, as well as their grieving friends and families. At the other end are those who are not only doing well, but sometimes thriving during the pandemic. Mercifully, WA has so far been spared the grim numbers of other states. The West has seen less than 700 cases to date, compared to Victoria which is fast approaching 17,500 and NSW with nearly 4000. Of the 450 COVID-19 deaths in Australia, nine have been in WA. And while Victorians are locked down, most West Australians have now settled into new ways of living and working and are looking forward to building resilience over the next 12 months, learning from collective experiences. Given many of our fellow Australians – and indeed people around the world – are struggling right now: is it OK to be OK in WA? You bet. While mental health advocates and support groups have been rightly promoting that it is “OK to not be OK” during this pandemic, we can’t overlook the importance of reminding people that it is also “OK to be OK”. Cassie Mogilner Holmes, associate professor of behavioural decision making at UCLA, says it’s not only OK – but essential. “It’s actually more important now 4 | SEPTEMBER 2020
than ever to focus on our personal emotional health,” said Holmes. COVID-19 has certainly been a traumatic experience – it has had a profound impact on mental health – about 1000 people have died by suicide in Australia since it began and modelling from the University of Sydney found that suicide deaths could rise by 25% annually. The term survivor guilt is usually used to describe the emotional distress someone feels after surviving a traumatic event when others haven't, like a natural disaster or terrorist attack. It has been identified in veterans, those who survived the Holocaust, 9/11 survivors, and first responders. During COVID-19 we have witnessed the conventional type of survivor guilt associated with surviving the coronavirus when hundreds of thousands haven’t. But not everyone is struggling, and this has resulted in a new type of survivor guilt. This emerging type of guilt is characterised by not feeling ‘impacted enough’ by the pandemic. This type of survivor guilt can be seen in the workplace. The pandemic has forced many organisations to reduce staffing, causing some remaining employees to feel guilty, according to John Hackston, head of thought leadership at the Myers-Briggs Co. Survivor guilt can result in a range of emotions, from shame to a sense of unworthiness or even anger. When emotions are not processed properly, they can impact our physical and mental health and cause depression, anxiety and physical illness. These are not easy days. Many of us are stuck at home trying to make sense of a confusing, contagious virus. And yet, there's so much to be grateful for. As quickly as our communities shut down, new avenues of happiness emerged – whether these took the
form of Zoom catch-ups, driveby birthday parties, or a renewed focus on connection. The fundamental question we're all facing is this: Is it OK to be OK right now – despite the death toll and the number of people sick, the impact on the frontline workers, the pressure on the essential workers who make sure we're all fed and safe, and the growing number of family and friends who are doing it tough? It may sound counter-intuitive, but experts say that seeing the good, despite the bad, is a sign that you have a healthy and balanced approach to this current – and challenging – situation. "If we have to wait for all the conditions to be perfect in order to be happy, we're going to be waiting a long time, perhaps as long as we live," said psychologist Lisa S. Larsen. "Sometimes, we have to look for the best possible solution for a tough situation in order to move forward during a difficult time." Even during hard times, it's common – and OK – to feel two feelings at once. We can be upset by the stress our friends, loved ones, and communities are experiencing and still feel grateful if we're doing OK. We don't have to pick just one emotion. In fact, the ability to feel multiple emotions, and to feel them fully, points to emotional resilience that will help us navigate through uncertain times. And we don’t have to let those emotions turn into feelings of guilt. This is a pandemic – you’ve done nothing wrong. And at the end of the day – it’s OK to be OK! ED: Dr Erin Smith is Associate Professor of Disaster and Emergency Response at the School of Medical and Health Sciences, Edith Cowan University. Figures were accurate at press time.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
GUEST COLUMN
BACK TO CONTENTS
MAJOR PARTNER
Infective exacerbations of COPD What is an exacerbation? The GOLD (Global Initiative for Chronic Obstructive Lung Disease) report, updated in 2019, defines an exacerbation as “an acute event characterized by a worsening of the patient's respiratory symptoms that is beyond normal day-to-day variations and leads to a change in medication.” Respiratory infections (predominantly viral), cause the majority of exacerbations. Other causes include pollution, heart failure or rarely pulmonary embolism or myocardial ischaemia. Role of antibiotics? Antibiotics have the greatest benefit (in morbidity and mortality) in more severe exacerbations (with the greatest evidence in the ICU population). The Anthonisen criteria, endorsed by the GOLD initiative, recommends antibiotics only for a severe exacerbation requiring mechanical ventilation (non-invasive or invasive) or an exacerbation with increased sputum purulence plus either increased dyspnoea or increased sputum volume.
Reproduced with permission from: Shared decision making for antibiotic treatment in exacerbations of COPD in the community [published 2019 April, amended 2019 June]. In: eTG complete [digital]. Melbourne: Therapeutic Guidelines Limited; 2020.
Even in hospitalised patients, the use of antibiotics has not been consistently
shown to demonstrate benefit. A meta-analysis in 2012 showed that antibiotics had no statistically significant effect on mortality and length of hospital stay in inpatients. In the community setting, the same meta-analysis showed low-quality evidence that antibiotics reduced the risk of treatment failure by 25% at one month. However, if the included trials were restricted to currently available drugs (they removed old studies that used chloramphenicol and oxytetracycline) there was no benefit shown. Viral causes should always be considered and empiric oseltamivir be prescribed in flu season. With the advent of COVID, it is likely that this virus will become one of the common causes of viral exacerbations. Hopefully we will have an effective treatment for this virus in the future. If used, antibiotics should be targeted against Haemophilus influenzae, Moraxella catarrhalis, and Streptococcus pneumoniae. Infections with Pseudomonas aeruginosa and Enterobacteriaceae species are rare, often occurring in patients with
Dr David New Consultant Specialist in Infectious Diseases in Microbiology
About the Author Infectious Diseases specialist Dr New has returned to Perth after training in Melbourne. He works at Armadale and RPH and privately at Clinipath Pathology.
underlying bronchiectasis. These patients tend to be sicker with pneumonia and require hospitalisation. Managing expectations: Talking to your patients about what to expect during an exacerbation is very important. The Box below is from the Australian Therapeutic Guidelines. Summary: Overall there is mixed evidence for the benefit of antibiotics in mild cases of COPD exacerbation. It is a difficult situation, and talking to your patients about the expected course of the illness is important. References on request
Shared decision making for exacerbations of COPD in the community To engage in shared decision making with patients and carers: • Ask about the patient or carer’s expectations for management of exacerbations of chronic obstructive pulmonary disease (COPD). • Explain that the duration of a COPD exacerbation is related to the severity of underlying COPD. For patients with mild COPD, symptoms of the exacerbation can last 7 to 10 days. In patients with more severe COPD, symptoms can persist for weeks. • Explain that inhaled bronchodilators and corticosteroids are the standard treatment for exacerbations of COPD. Additional treatment with antibiotics should only be considered if all three of the following clinical features of a bacterial infection are present: • increased sputum volume
• sputum purulence or a change in sputum colour • fever. • Discuss the limited benefits of antibiotic therapy for nonsevere exacerbations of COPD, even when a bacterial cause is likely. • For patients managed in the community with less severe exacerbations, antibiotics do not consistently improve outcomes. Currently used antibiotics do not reduce the rate of treatment failure or prolong time to the next exacerbation. • Discuss the potential harms of antibiotic therapy. • Adverse effects of antibiotics include diarrhoea, rash or more serious hypersensitivity reactions. • Antibiotics disrupt the balance of bacteria in the body (the microbiome). While the consequences of this are not fully understood, it can cause problems
ranging from yeast infections (eg thrush) to more serious infections (eg Clostridium difficile infection). • Antibiotics can cause bacteria in the body to become resistant to antibiotics so that future infections are harder to treat. Multidrug resistant bacteria (known as ‘superbugs’) can be spread between people, affecting other family members and the community. • Ask about the preferences, values and concerns of the patient or carer, and answer any remaining questions. • Make a joint decision about whether to add antibiotics to standard care (inhaled bronchodilators and, where necessary, oral corticosteroids); if a decision is made to use antibiotic therapy, see eTG complete for treatment recommendations. • Discuss criteria for patient follow-up and reassessment.
Main Laboratory: 310 Selby St North, Osborne Park General Enquires: 9371 4200 Patient Results: 9371 4340 For information on our extensive network of Collection Centres, as well as other clinical information please visit our website at
www.clinipathpathology.com.au
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 5
Breathing easier For long-time respiratory clinician-researcher Professor Steve Stick, the opening of the Wal-yan Warlang-up Respiratory Research Centre in August was the culmination of 30 years’ hard work by a phalanx of doctors determine to see WA become a world leader in respiratory research. The centre is a partnership between Perth Children's Hospital Foundation (PCHF), Perth Children's Hospital and Telethon Kids Institute, but Prof Stick said because the researchers had already strong networks, Wal-yan would also collaborate with other research centres particularly in Queensland and Victoria, the US and Europe.
Above: Asthma sufferer Dartanyon Wilson-Finnis will be one of many to benefit from the Wal-yan Centre. Below: Director of the centre, Professor Steve Stick.
The efforts of luminaries such as Prof Lou Landau, Prof Peter Le Soeuf, Prof Pat Holt and Prof Kevin Turner saw a cystic fibrosis research hub develop in the 1980s and that legacy has been developed by those who came after such as Prof Peter Sly and, of course, Prof Stick. The work today, which currently is funded only by philanthropy underwritten by the PCHF, is also focusing on asthma research, with breakthrough studies of the airway epithelium showing enormous promise. The centre is involved in COVID-19 studies with Chile for the efficacy of interferon as a treatment.
PPE critical As Victorian reels from and New South Wales braces for outbreaks of coronavirus, the lack of personal protective equipment is becoming critical. Victorian GP Dr Mukesh Haikerwal called on the Health Minister Greg Hunt to release more PPE from the national stockpile to the frontline, especially N95 masks. Dr Haikwerwal said that despite reassurances that Australia had adequate supplies, 40% of GPs were reporting serious difficulties sourcing them and 75% decided to source their own on the market rather than wait for logistical problems to be sorted out. It was a distraction they could do without. The Royal Australasian College of Physicians released a survey of its members, revealing a significant proportion of them in public hospitals were resorting to buying their own PPE with almost half having limited or no access to N95 grade masks and 11% with no access. The survey found: • 20% of respondents in public hospitals have had to source their own PPE • 22% across all settings say they have either limited (19%) or no 6 | SEPTEMBER 2020
(3%) access to surgical masks • 45% of respondents say they have limited or no access to N95/ P2 masks for their needs, with 11% having no access • 61% of respondents reported having had recent workplace training in the use of PPE.
Hit for HealthEngine The Federal Court has ordered HealthEngine to pay $2.9 million in penalties for engaging in misleading conduct in relation to the sharing of patient personal information to private health insurance brokers and publishing misleading patient reviews and ratings. HealthEngine admitted that between 30 April 2014 and 30 June 2018 it gave nonclinical personal information, such as names, dates of birth, phone numbers, email addresses, of more than 135,000 patients to third party brokers without adequately disclosing this to consumers. HealthEngine earned more than $1.8 million from its arrangements in this period. HealthEngine was also ordered to contact affected consumers and provide details of how they can regain control of their personal information.
In a statement, the company welcomed the conclusion of legal proceedings and emphasised that personal, not clinical, information was provided when consumers specifically requested a call regarding a health insurance comparison. “We did not make it sufficiently clear on the booking form that a third party, not HealthEngine, would be contacting them regarding the comparison and that we would be passing on consumer details for that to occur. This was an error and HealthEngine apologises for it,” CEO Dr Marcus Tan said.
Northam boost The final element of the $42 million Northam Health Service redevelopment has been officially opened. The addition includes operating theatres at double the previous capacity, a refurbished recovery suite and a central sterile services department. A dedicated chemotherapy department has also been established, including a waiting room, reception, consulting room with telehealth capability, and large treatment areas equipped with recliner chairs. The health
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
IN THE NEWS
BACK TO CONTENTS
IN BRIEF service now boasts an expanded emergency department, purposebuilt consultation rooms and indoor and outdoor rehabilitation treatment areas, as well as a new ambulatory care building that provides access to community health services.
believe the pain could be prevented or reduced by using lidocaine.
RPM for Royal Perth
Brakes on eScripts
Philips Healthcare has secured a $6.5 million contract to provide an integrated care management package which will enable RPH (and Bentley) to monitor more than 100 beds from the RPH-based Command Centre. Eventually it will help provide 24/7 clinical support services for all remote patient monitoring and assessment of patient data. The contract with Philips will allow the East Metropolitan Health Service (EMHS) to monitor its high acuity beds enabling early detection and prevention of patient deterioration.
It started with the bang but the Australian Digital Health Agency is now asking GP software companies to remove the electronic prescribing functionality that was only launched in late July. GPs who were early adopters and had updated their software to issue eScript tokens will still be able to use the function. But it’s a “sit-on-your-hands” moment for others. The update will only be available to practices in designated “communities of interest”. The ADHA is also asking GPs outside these designated areas to halt all eScripts until pharmacies are ready to receive the digital tokens.
The project will examine the longterm outcomes of lidocaine infusions for persistent postoperative pain in patients undergoing breast surgery (LOLIPOP).
Lidocaine after surgery
WA eyes EMRs
Consultant anaesthetist and director of research at the Department of Anaesthesia and Pain Medicine at Royal Perth Hospital, C/Professor Tomas Corcoran, was awarded a $4.3 million grant in a joint project with Monash University to study the long-term outcomes of anaesthetic infusions for breast surgery patients to reduce persistent pain after surgery.
The pandemic recovery response will see the WA Government begin the process for a system-wide electronic medical record system. It is injecting $8.1 million to start the planning for a EMRS, which was one of the pillars of the Kruk Sustainable Health Review. Apart from the clinical advantages, planners think it will also create an important foundation for future digital growth and clinical innovation.
Persistent pain after surgery and radiotherapy affects up to half of patients who have undergone breast cancer treatment. Researchers
Medical Forum 2020 readership survey How likely would you be to recommend Medical Forum magazine to a friend or colleague? Very Unlikely Unlikely Neutral Likely Very Likely 0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
UWA PhD student Synat Keam, 32, a medical researcher from UWA’s National Centre for Asbestos Related Diseases has been awarded the Douglas Peter Swift Scholarship for his work exploring immunotherapy and radiotherapy combination treatments of mesothelioma. A/Professor Alistair Cook will supervise Mr Keam’s research. Queensland rural GP Dr Sarah Chalmers is ACRRM’s new president, taking over from Dr Ewen McPhee, who said he was proud to be handing the baton to an ACRRM-trained rural generalist. C/Professor Alan James has been awarded the Thoracic Society of Australia & New Zealand Research Medal for 2020. The SCGH research clinician has been acknowledged for his decades-long work in asthma research. He is also chair of the Busselton Health Study. Dr Andrew Miller has been re-elected AMA WA president while its immediate past president Dr Omar Khorshid has been elected as national AMA president. In its first ever board election, AMA WA announced that members for 2020-23 are: Dr Megge Beacroft, Dr Michael Gannon, Dr Katharine Noonan, Dr Michael Page and Dr Marcus Tan. Thanks were offered to outgoing board members A/Prof Rosanna Capolingua, A/Prof David Mountain and Dr Simon Torvaldsen. Leading global expert on infectious diseases Emeritus Professor Michael Alpers, from Curtin University, is the 2020 recipient of the Australian and New Zealand Association for the Advancement of Science (ANZAAS) Medal.
Almost 70% of readers would recommend Medical Forum to a colleague.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 7
Care Can’t Wait Former past AMA president and GP Dr Tony Bartone writes about the tragedy unfolding in aged care and urges national action. My heart goes out to all Victorians in residential aged care facilities, their families and friends, during this crisis. As a son with an elderly mother in aged care, I understand the heartache, confusion, fear, and concern that so many in the community are going through. But the aged care system in Australia was in crisis long before COVID-19. What we are seeing today is the result of a perfect storm. Our population is ageing and there are long waiting lists for home care packages. In a single year, 16,000 Australians died while waiting for a home care package. People are entering residential aged care older and frailer, while clinical care in homes is limited,
and we have inadequate regulation to mandate adequate staffing numbers. The Royal Commission’s interim report last October laid out in more than 700 pages how the system was failing our older and most vulnerable people. And yet, nothing has been done. I stood beside my colleague, Annie Butler from the Australian Nursing and Midwifery Federation, and called on the Government not to wait for the Royal Commission’s final recommendations to act. The campaign #CareCan’tWait was launched, but we’re still waiting. We called for minimum staffto-resident ratios, along with registered nurse availability 24/7. We called for increased funding to
enable greater availability of home care packages, especially Level 4 packages, to keep older Australians in their communities for longer. And we called for improved funding for GP services in aged care homes. With inadequate numbers and training of staff in aged care, it is no surprise how quickly the virus has spread. The 2017 Pollaers workforce report told us we had a serious workforce and training problem that was only going to get worse because of the increasing older demographics. An ANMF survey showed that fewer than 40% of staff thought their workplace was prepared for a COVID-19 outbreak. Some aged care homes cut staff numbers even further during the pandemic, or did not increase staffing numbers in
Introducing our new onsite sleep centre,
Subiaco Sleep Care Operated by one of Western Australia’s leading sleep services, Sleep Studies Australia, the state-of-the-art facility offers a complete service for the diagnosis and treatment of adult and paediatric sleep disorders. For more information and to order a referral pad, call 1300 651 234 or email reception@sleepstudies.com.au. www.sjog.org.au/subiacosleep
8 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
GUEST COLUMN
GUEST COLUMN
BACK TO CONTENTS
We need to know how many staff members work in multiple aged care homes nationally. Studies from other countries have shown that adequate staffing and limiting the movement of workers between multiple sites are key in preventing the spread of COVID-19 in aged care homes. All aged care staff must have complete sets of PPE and they must be trained and regularly practise how and when to use it.
anticipation for the pandemic. Inconsistent messaging and guidelines across the jurisdictions were causing confusion. Clearly, communication and appropriate direction from the Aged Care Quality and Safety Commission (ACQSC) was failing. While the situation in Victoria is dire, if we act urgently, we still have the chance to keep residents safe and well, and ensure that what is
happening in Victoria now does not happen elsewhere. We cannot work in silos. All sections of government, aged care providers, and the healthcare system must work together to improve quality of care, transparency and accountability. Right now, aged care homes need more staff, especially registered nurses. This cannot be stressed enough.
The government must ensure that hospital outreach teams can go into the community, and particularly aged care homes, to ensure adequate clinical care is provided. Local hospitals need to develop strong and robust levels of communication and awareness of their catchment facilities, including the local GPs who serve those facilities. Finally, the government should urgently implement systemic improvements in the sector already identified by the Royal Commission. Australia’s older people deserve action, not inaction. Their care cannot wait. ED: This is an edited extract of Dr Bartone's blog.
Proudly Developing Commercial Projects Since 1980 08 9262 7400
zirconprojects.com.au
enquirires@zirconprojects.com.au
BC 5975
Featuring Hamilton Hill – Medical Centre
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 9
BACK TO CONTENTS
CLOSE-UP
Yes, she’s that Fiona Working on the frontline with COVID-19 patients, Professor Fiona Lake tells Ara Jansen that patient care is both the biggest honour and challenge in medicine.
When you’re a WA doctor named Fiona, you might have to get used to being ‘the other Dr Fiona’. No, not Dr Fiona Wood, who worked tirelessly with burns victims after the 2002 bombing in Kuta. And not Dr Fiona Stanley either, for whom the Fiona Stanley Hospital is named. Still, when people walk past Dr Fiona Lake in the street and casually say “Hey Fiona, thanks for your work in Bali” she has learnt to acknowledge the compliment. ‘Don’t worry’, one of the other Fionas advised, ‘accept the praise, graciously’. But all that has changed over the past couple of months because while Dr Fiona Lake might have had the lesser celebrity public profile of the three, her professional profile is undisputed, as is her work in the area of respiratory health as a consultant in the Department of Respiratory Medicine at Sir Charles Gairdner Hospital. 10 | SEPTEMBER 2020
Fiona was on call on the weekend in late February this year when Charlie’s received its first COVID-19 cases from the Diamond Princess cruise ship. Along with Dr Chris Kosky and Dr Anna Tai, the trio volunteered to be the frontline physicians to respond to the pandemic. They assessed and facilitated the care of patients who presented with fever or flu-like symptoms, even if the underlying disease process wasn’t a respiratory one. To minimise staff to patient contact, these doctors provided primary patient care around the clock, until they were proven COVID negative. As part of their Stars of COVID-19 campaign, a recent post by the WA branch of the Australasian College of Health Service Management MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
CLOSE-UP (ACHSM) said the trio “stepped forwarded at a time of enormous unpredictability and anxiety. Behaving in a calm and measured fashion, they provided leadership and reassurance to all staff and the best possible care to patients”.
Qualities shine They also said Professor Lake demonstrated great leadership, kindness and empathy towards patient care. “We became the COVID team and there was an enormous amount of learning very quickly,” explains Fiona. “It was also extremely rewarding and challenging and a very novel process in a hospital. “It required a lot of collaboration and, I think, that has changed the way we practise, hopefully, forever.
“This pandemic has definitely driven some innovation, particularly around things like telehealth, which is something we have been talking about for years and, within a couple of weeks, people were using it. “I hope we can take all of the learnings and try not to go backwards. The way we communicate has changed. There are still people to see face-to-face, but when we can’t or don’t need to, then video calls in whatever form they take can make care so much more flexible.” Fiona is now part of a statewide committee set up for the management of COVID-19 in the community. Since studying medicine at the University of WA, Fiona has held
varying positions at universities and hospitals in Perth, mixing teaching and education with hands-on clinical work. Those positions have included being associate dean at UWA’s Faculty of Medicine and Dentistry and establishing the Education Centre within the faculty, a consultant respiratory physician at Royal Perth Hospital and the Winthrop Professor of Medicine at SCGH.
People first When it was time to head off to university, Fiona wasn’t sure what she wanted to do. After a year in Canada as an exchange student, she agreed to see what first year medicine looked like. She got involved with a student initiative in community health where she would visit a patient at home, accompanying a social worker and a nursing student. It was this experience that got Fiona excited about medicine. She started thinking obstetrics and gynecology was going to be her specialty because, oddly, there weren’t many women doing it in the late 1970s. Internal medicine was fascinating to her and in the end it was people like Bill Musk and Gerard Ryan, alongside a number of others, and the work they were doing in the area of respiratory and occupational health that sent Fiona towards a new specialty. “It was at the time when asbestos cases were in court and doctors were standing up for patients,” says Fiona. “To me the area seemed to have less well-off patients and there was a sense of social justice about it. I certainly felt aligned to that. “I have had a very blessed and fabulous life. I really like the patient work, which is at the core of what I do. I have worked in academia, education and in leadership roles. In the end it has been the patient care that gives me the most pleasure. “It’s the care and that kind of intellectual stimulation, the challenge and the art that come with trying to understand a patient’s fears and hopes, meet their needs and translate that into care. “It’s an extraordinary privilege to meet people from all walks of life and from parts of society you never see and how they cope with life and hear their stories.
Fiona in Hornstradir, Iceland. Opposite: Her photo taken at the recent BLM rally in Perth.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
continued on Page 12
SEPTEMBER 2020 | 11
Yes, she’s that Fiona continued from Page 11
Shared care “A lot of people think that doctors in hospitals don’t have good relationships with their patients, if any at all. For me, I’m with my patients for an intense period in their lives. They are usually very unwell and I work very closely with them. “Human beings are wonderful and capable of the worst and the best. I don’t have a faith but I see people who do and it helps them. It’s fascinating that they have a kind of framework that they use. I’ve never lost my wonder in human beings. I think all doctors start out with a level of compassion but we learn so much more from our patients.” Fiona says as a young doctor being asked by a patient how long they had to live was probably one of the hardest questions she had to learn to answer. At the time she had no idea what to say or how. But it caused her to make a vow: she would never fear any question someone asked. Decades on she has kept that promise and says she either tries to help someone or admits she doesn’t know and gets help. “The biggest thing I have learnt is
that as doctors we talk too much. If you give someone too much information they can’t make good decisions and often they make bad ones. You have to be quiet and listen and give them information, then listen again and then you become much better at picking up the clues.” Fiona says it’s imperative to recognise when something isn’t done well or didn’t go well and strive to do it differently at the next opportunity. “I feel like one of the biggest misconceptions about COVID, in the community and the media, is that the ICU is the place to go and that can solve your problems, when in fact it might kill you. It’s an exceedingly difficult conversation to have with someone when they are sick, that ICU may not be the best place because they have a high chance of dying and, if they survive, they may not have the same level of independence as they had before getting sick.”
teachers, supervisors and workshop facilitators. Fiona ran countless workshops around Australia and delivered the program in Vietnam, Myanmar, Taiwan, Saudi Arabia and Ireland. “I always thought this was a way to influence a large number of doctors rather than just one at a time. Plus, a great teacher will only interact with a small number of students, but if we train up many doctors to be great teachers, the impact is huge.” While she has spent short stints working in the US, UK and Canada, Perth is firmly home to Fiona and where she has always worked. Her husband, a doctor, has recently retired and they have a son. Alongside internal medicine, the natural world also gives Fiona enormous pleasure. She likes nothing more than a good long hike, as evidenced by holidays on foot in Iceland and France. There are also walks with her dog Jezza, a vizsla or Hungarian pointer.
Rewards of teaching
When walking a piece of the Cape to Cape in the South West, Fiona found a paper nautilus (or an argonaut) which is a kind of egg case for an octopus.
While it has been her biggest joy, working with patients hasn’t been the only area of medicine Fiona has been involved in. She co-created a successful and awarded program called Teaching on the Run, which helps doctors become better
The discovery of a near perfect shell on the beach sent her off on a fascinating reading journey about Jeanne Villepreux-Power a pioneering French marine biologist who in 1832 was the first person to create aquariums and studied
Looking for Safe, Secure, Convenient & Affordable storage units? Storage units for sale or lease Ideal for archiving
Discrete and private
Suitable for private and valuable possessions – e.g. artworks, antiques, memorabilia, jewellery etc
Fire rated units with individual fire and security alarms
Eco-friendly design that moderates internal temperature and humidity levels (ideal to protect valuables and documents)
Conveniently located in Osborne Park
Sizes ranging from 23sqm to 57sqm (57m3 to 189m3)
Contact Robert Luca 0413 270 058 or email: rob@luca.net.au ww.multistorage.com.au 12 | SEPTEMBER 2020
Smarter
Safer
Stronger
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
CLOSE-UP
CLOSE-UP
BACK TO CONTENTS
“Medicine is competitive and full of big egos but what you see is not the whole story. I think a lot of people feel the need to push themselves hard, work long hours and keep up with others, but struggle inside. I think it’s important to help doctors go in whatever direction they want and not feel pressured. I’d like to help them do that.” Growing up in Fiona’s family home, justice and equality were important. Then, as life moves on, you get buried in work and donate money instead of time. While somewhat controversial, Fiona said it felt important for her to go to Perth’s Black Lives Matter rally. She took her camera to immortalise the event, showing off another talent.
Fiona with Jezza.
marine life in them. Her work proved that the paper nautilus produced their own shells rather than acquiring them, like a hermit crab.
wanting to be “one of those people who hang around until they are ancient”. Armed with plenty to offer, she’s aware that moving on allows “a lot of fantastic young people” the space to move and develop.
Joy of discovery For Fiona, her curiosity about finding something interesting is what sends her off on a trail of discovery, most likely applied with the same vigour she uses to uncover a tricky diagnosis. At 63, while she is far from ready to retire, Fiona is also conscious of not
“I’ve recently started a leadership position in education at Charlie’s which is exciting and gives us an opportunity to look at what COVID taught us and how we can learn and work differently. I also think mentoring and supporting young people is particularly important work.
“I felt it was too important not to go. We calculated the area and how many people might be in it while socially distancing and reckoned it was safe. I went to land rights rallies as a student and this felt as important. I was thrilled to see it was run by passionate, young, articulate Aboriginal people. “Sadly, many Aboriginal people present at the hospital for an extended stay during some point in their lives and we have to make sure that their experience is as positive as possible. In our care I hope we can make a small difference.”
Read this story on mforum.com.au
WE HELP YOU GET ON TOP OF BUSINESS SO YOU CAN GET ON WITH CARING FOR THE COMMUNITY Talk to the ANZ Health Banking Specialist Team that understands your needs. Visit anz.com/health or contact your local State Health Director, Megan Carter, on 0411 140 781.
© Australia and New Zealand Banking Group Limited (ANZ) ABN 11 005 357 522.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 13
BACK TO CONTENTS
FEATURE
A universal sentinel Telethon Kids researchers are looking beyond magic bullets and aiming for long-term benefits for our most vulnerable.
Jan Hallam reports.
Before the SARS COV2 pandemic, vaccine research and development were studied and measured affairs. Underpinning them were two words – safe and effective. While there are grim health imperatives driving many of the vaccine projects around the world, the vaccine ‘race’ itself has entered a particularly worrying political stage with the availability of a Russian vaccine that many scientists consider is undercooked, and governments of wealthy nations speculating billions of dollars on promising vaccine candidates. The stakes are high. For Professor Tobi Kollmann and his partner, Dr Nelly Amenyogbe, who have been brought to Perth by the Telethon Kids Institute and the Perth Children's Hospital Foundation to open the first paediatric research centre for the Human Vaccines Project, sometimes the greatest vaccine prizes are right under our noses. In May this year, the team published a paper that showed the century old Bacillus Calmette-Guérin (BCG) vaccine for TB, when repurposed, helped kickstart newborns’ immune systems in their vulnerable first days of life when sepsis is a deadly threat.
Supercharging Their research found that there was a dramatic and rapid increase in neutrophils (firstly in mice) and then in human newborns in West Africa and Papua New Guinea within three days of the vaccine being administered. “It’s been known for a long time that neutrophils play an important role in managing sepsis, but until now nobody understood the role of BCG in initiating this critical process,” Dr Amenyogbe said at the time. “It was actually thought to be biologically implausible, however, we’ve not only shown how BCG is involved, but that it kicks off this process almost instantly following vaccination – far more quickly than anticipated.” It was a thrilling find and one close to Prof Kollmann’s heart. Forty years ago, Swedish-born, Denmark-raised anthropologist-medico 14 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
FEATURE Dr Peter Aaby began working in Guinea Bissau, an impoverished nation in West Africa where infant mortality was extremely high.
medical establishment almost destroyed him. This kind of thinking in medicine is our biggest obstacle for progress.
He became a close friend of Tobi Kollmann’s.
“What we have just published now, we have known for many years. BCG is one of the safest vaccines, it is one of the most commonly administered vaccines in the world and it cost pennies.
Aaby observed and later published a paper on the non-specific benefits of some vaccines and of BCG in particular. “He noticed that giving BCG to low birthweight infants within the first two days of their lives reduced death by 50%,” Prof Kollmann said. “It was an observational study, not a randomised controlled trial in the wilds of Guinea Bissau, but Peter published his observations anyway because they seemed too important not to.
Loud critics “He was howled down by the medical establishment. In their view, BCG was for TB, and TB doesn’t kill newborns. How could it save the life of newborns in less than three days when the BCG microbacterium grows so slowly? “Our paper has shown that BCG rapidly increases the growth factor G-CSF which stimulates the bone marrow to produce granulocytes and stem cells and release them into the blood stream within hours of administering the vaccine. “Peter’s observations were right but the dogmatic thinking of the
“So, the only thing we need to do to make this benefit available to all newborns in the world is to give it to every newborn at birth. Timing is critical and what’s standing in the way in many parts of the world is red tape from WHO protocols about the number of doses required per vial. “If the WHO changes that policy, we can save 500,000 babies every single year. Our research has given the WHO the scientific proof it requires.”
BCG & COVID The same BCG vaccine has also found itself in the COVID-19 research frenzy as Prof Kollmann and Dr Amenyogbe are involved in the BRACE trial which began in the early stages of the pandemic. It aims to determine if it can offer any protection against the virus, particularly among health care workers. The trial is being conducted across three sites – Melbourne, Adelaide and Perth.
However, both sounded warnings that while the effect was rapid and offered robust protection against newborn sepsis, it was relatively short-lived and their studies indicated that the protection did not occur in adult mice at any rate. This trial-and-error is very much a part of the COVID landscape, but Prof Kollmann added that it is how medicine has been practised “forever”. “Scientists are using whatever biological information they have, based on existing data, to guide them to make the best possible decisions, for example, administering steroids,” he said. “If you see somebody dying from COVID because they're likely having a hyper-immune response, those are reasonable guesses. The impact of these drugs may be marginal, where the sickest of the sickest may benefit, but you're not going to change anything dramatically.” Tobi Kollmann’s world has been a lab for the better part of his career, but it started in a similar way to his friend Peter Aaby – where observation sparked inquiry.
Sliding doors As a young medical student in Germany in the early 1980s, he planned a visit to his brother, who was a doctor working in Ethiopia. It was while walking past a newsstand at Frankfurt airport that his world tipped on its axis. The cover of Newsweek on his outward journey was a haunting collage of the faces of the AIDS epidemic in New York – men, women, white, black, the disease did not discriminate. “That was the first thing that struck me, this was not a homosexual disease,” he said. “I spent the next three months working with my brother in a little town called Dilla on the track between Addis Ababa and Nairobi. It was a market town where a lot of trucks stopped on their way to somewhere else. There was a lot of sex trafficking and in my time there I saw just about every STD in the book and, of course, there was a lot of HIV. “There was also a lot of young children between the ages of two
Prof Tobi Kollmann with Telethon Kids Director, Prof Jonathan Carapetis. Opposite: Prof Kollman with Dr Nelly Amenyogbe.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
continued on Page 17
SEPTEMBER 2020 | 15
Page removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act. --https://medicinesaustralia.com.au/code-of-conduct/aboutthe-code/ https://www.tga.gov.au/legislation-legislative-instruments
BACK TO CONTENTS
FEATURE
A universal sentinel continued from Page 15 and five dying and nobody could really understand why. “Returning back to university, I was transiting through Frankfurt again and passed the same newsstand. This time the cover of Newsweek had the face of a young girl from New York. She had prominent ‘chipmunk’ cheeks, the same facial features of the dying children in Ethiopia. The girl on the cover had AIDS. “I bought the magazine and read the article which described the work of Dr Arye Rubinstein, who was working in the Bronx and discovered that AIDS could be transmitted from mother to child. “I was beside myself. I immediately wrote to him, telling him I had just returned from Africa where I saw kids who I thought could potentially have had AIDS. In those days it was letter writing, so six weeks later I got a reply inviting me to come to New York.
Pocket dynamo “I got to the Bronx on a Friday afternoon and walked into the lab and there in front of me stood a man who was almost half my size, wearing a yamulke and greeting me in German. He and his family had left Berlin before the Holocaust. “He invited me into this special little clinic and there on the examination table was the little girl on the cover of the magazine. It was surreal. I examined her, took some blood from her, played with her. “Being there in that lab, something happened to me. I went to a German medical school where what wasn’t written in the textbooks was dark matter. The buildings on the far side of the faculty were the research labs. I used to think, ‘what a joke, that’s not real medicine’. “When Arye Rubinstein told me that no one really knew what caused AIDS but he was doing research to find out, as I'm saying this to you right now, I have the same shivers as I did at that moment. It just clicked inside of me. “Rubinstein looked at me as said ‘without research there is no
change’. In that moment I felt it was my life that had changed. Research became central.” For the next five years, paediatric AIDS was Prof Kollmann’s focus until another shiver went down his spine. “I am not a very sociable person, so I was in the lab on a Saturday evening, it was 1994. I was the only one in the building, all the other lights were out and I was looking at a paper from the Paediatric AIDS Foundation. It was such a focused moment visually and spiritually. What was going to be my next move?
Most in need “I knew it had to be ethically and morally right, so, I thought, who is suffering the most in the world? The answer was newborns and their risk of dying from infection.” It led him to Seattle to work with Prof Chris Wilson, who was later to join the Gates Foundation’s Discovery program.
“Having that network of experts on your side is an incredibly enriching experience. We know already the basic rules that we identified in our previous work. All we need right now is the money – $100 million – and it sounds a lot, but if you think about the impact it will have, wow, this is doable.” Prof Tobi Kollmann knows that there are doubters but if a breakthrough is to come, he believes it will be here in Perth.
Can-do attitude “West Australia, maybe Australia I don't know, but WA and especially Telethon Kids and Jonathan Carapetis are committed to building bridges to deliver solutions to lowcare settings. The local folks here put their money where their mouth is because they believe in this. “For me, that is unprecedented. I have never experienced that anywhere in the world before. To me, this has been transformative and both my wife and I feel privileged to be here.”
Read this story on mforum.com.au
“He is still my mentor but he's tough. There have been some tearful moments with him, but he allowed me freedom to explore.” The ‘newborn immunity initiative’ of the Human Vaccines Project (HVP) has led to the other side of the world to Telethon Kids Institute and the quest for a vaccine that will supercharge an infant’s immune system to fight the diseases of the future. “The goal is to enrol 25,000 mothers and follow them through pregnancy and assess their vaccine status and then the newborn and infant vaccines,” he said. “There will be data-driven processes and machine learning and AI to tell us what is actually happening and not just what we think is happening.” The scope of the HVP is immense and is matched by its financial requirements but as Prof Kollmann suggests, few projects have the capacity – “technologically, informatically, conceptually, on every level” – to achieve the goal of saving hundreds of thousands of lives a year.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
Support your patients with their diagnosis of dementia
Specialised support services available through:
» Home Care Packages » CHSP » NDIS
Call us today 1300 66 77 88 alzheimerswa.org.au
SEPTEMBER 2020 | 17
The rise of Public Health Public health may have once been the quiet achiever of the health system, but COVID-19 has changed all that.
James Knox reports.
Cigarettes, alcohol, illicit drugs, prescription opioids, suicide, mental illness and sexually transmitted diseases all share an unfortunate commonality: they are, in widely varying degrees, bad for us. This simplistic summation may seem obvious but if you dig a little deeper, you will find public health policy at the root of this schema. The role of public health, now more than ever, has come to the fore of the collective consciousness thanks to the coronavirus pandemic, with constant reminders of what we should and should not be doing and what we are not permitted to do. Australia and particularly New Zealand’s success in avoiding the worst of the pandemic is in large part due to the population’s trust in public health, trust of those elected to act in the best interests of their constituents and trust that they follow the best advice from specialists. Yet, as can be seen in countries such as the United States and Brazil, which seemingly are unable to control the spread of the virus, another commonality is shared: wholesale undermining of public health. The failure of these countries to manage the pandemic highlights the dangers of politicising and ultimately delegitimising public health, which is why countries such as Australia and New Zealand need to be especially careful now 18 | SEPTEMBER 2020
in the way they deliver messages to maintain the trust of their populations. That is easier said than done.
Managing the message It may be reductionist to say public health is all about the messaging, even though its success is heavily reliant on effectively communicating consistent messages, particularly in a pandemic such as COVID-19, that requires direct and immediate results. The Chief Health Officer of Western Australia, Dr Andrew Robertson, and his department are responsible for ensuring the messages are successfully delivered to the state.
“This was crucial in establishing credibility and building public trust, particularly with the rapid implementation of restrictions when Australia first started recording COVID-19 cases. “As we contemplated health systems under a huge amount of pressure, communication became a crucially important intervention to ensure that all members of the WA community worked together to protect themselves and others to avoid the emergency department, hospital ward, or intensive care units,” he explained. “The messaging needed to get the balance right on communicating the risk of a virus that initially was not present in WA, reassuring the public, and reinforcing the potential urgency of the challenges we might face in the months ahead.”
Balancing act
“I would say within the context of the COVID-19 pandemic, or any outbreak for that matter, consistent public health messaging is a critically important public health intervention,” Dr Robertson told Medical Forum. Although reducing the spread of the virus has been the main objective of the messaging, Dr Robertson explained this was shaped by national messaging, as well as correcting mistaken statements, emphasising shared vulnerability, and being open about areas of uncertainty and complexity.
While communicating a harmonised, inclusive, and tangible message that is understandable for most of population is the objective, the difficulty is in reaching those who are not in the ‘most’ category. “Clear, simple and consistent public health messaging is critical. To address some of the difficulties in that task, we have worked to understand the needs of specific groups who might experience barriers to accessing information, and this includes providing information in multiple and accessible formats. “For example, we have a collection
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
FEATURE
BACK TO CONTENTS
FEATURE
of resources for Aboriginal and Torres Strait Islander people, and resources available in different languages and interpreters on hand to serve our culturally and linguistically diverse population.
Trust the source “However, without the public’s trust, public health messaging will not achieve the desired response in terms of motivating citizen behaviour to comply with measures to reduce the spread of the virus. “The WA community, including our elected officials, has maintained a high level of public trust in the health response and has subsequently listened to the advice, particularly when restrictions needed to be imposed around social distancing, mass gatherings and other public health measures. “As a result, WA has maintained consistently low numbers of new COVID-19 cases and succeeded in limiting the spread of the virus. This has allowed us to ease restrictions in a way that supports our economy, with minimal risk to the community’s health.”
Politicisation of public health However, trust is not iron clad and can be easily eroded with partisan interference as witnessed in the US and Brazil where the severity of COVID-19 has been downplayed, public health apparatus have been undermined and a disproportionate spike of cases the result. According to Dr Robertson,
politicians have deferred to the advice and evidence from public health specialists in Australia. “All Governments have worked closely with their public health officials to get the advice required to guide their decisions and to support the operational requirements needed to implement those decisions. “As the Chief Health Officer, and public health regulator, I must ensure that I fulfil the legislative responsibilities pursuant to the Public Health Act to ensure the law protecting the health of the community is properly administered. As such, I am required to be independent and nonpartisan. “We only have to look to other countries with uncontrolled COVID-19 outbreaks to observe the impacts of a fractured relationship between politicians and public health experts. “A strong relationship between politicians and public health experts is crucial to ensure a united front and consistent, evidence-based public health messaging nationally. All this works to establish and maintain public trust to ensure the uptake of preventative strategies. “Fostering a strong, collaborative and respectful relationship between politicians and public health experts also ensures all sides are working towards a common goal. This is important in ensuring that, when public health recommendations
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
are made using the highest quality scientific data, politicians will give due consideration to this advice in their decision-making.
False facts When the wheels come off the public health bandwagon, the outcomes can be catastrophic, such as with the anti-vaccination movement, based on the infamous research of Andrew Wakefield who fraudulently claimed causality of autism with the measles, mumps and rubella vaccine. Since his discredited paper was published in 1998, anti-vaxxers have disseminated this ‘evidence’ to support their propaganda claiming harmful effects of vaccines. Public health may be the domain of governments to communicate health messages to most of their populations, however, there are cohorts of sceptical, susceptible, and gullible people who just cannot be reached by mainstream public health and are prime targets for messaging from ‘advocates’, ‘influencers’, and ‘experts’, such as Mr Wakefield, willing to broadcast alternative narratives, light on facts and heavy on speculation. Mr Wakefield is now using the coronavirus pandemic to persuade whoever will listen to his counterfactual narrative that COVID-19 vaccines, once developed, will be dangerous and people should be suspicious of them. continued on Page 20
SEPTEMBER 2020 | 19
continued from Page 19
Communicating risk If anti-vaxxers can teach us anything, the lesson is, regardless of the message, some people will accept it, while others will not. “The spread of falsehoods is not a new phenomenon,” said Dr Robertson. “I can appreciate they have gained unprecedented emphasis in recent years through digital media, which often has no editorial oversight. “Countering false claims requires an across-the-board response, which brings me back to the importance of clear, coordinated, transparent and evidence-based public health messaging. If this is put in place from the start and public trust is developed and maintained, this makes it significantly easier to lessen and dilute the impact of falsehoods. “From a department perspective, the DoH WA acts as the lead agency to advise the Department of Premier and Cabinet on the health aspects of a whole-ofgovernment response. This ensures one point of truth to strengthen the COVID-19 messaging, rather than information splintered across a variety of sources.”
Mixed messages While it is expected that sovereign countries will lead their own public health policy, the pandemic has emphasised how differing those approaches can be, even for neighbouring countries such as in Scandinavia, where Sweden took a different approach to its neighbours. Although Australia does not share a border with Sweden, can its decisions affect Australia?
20 | SEPTEMBER 2020
According to Dr Robertson, absolutely. “As a global epidemic, there are important lessons to be learnt from other countries which have taken different approaches to us in terms of limiting the virus. “These lessons have been both good and bad, with some countries controlling the outbreaks well, such as South Korea and New Zealand, while other countries have struggled, with surging infection rates, catastrophic death tolls, the collapse of health systems and strict and long-term lockdowns. “Our public health messaging is based on the best available evidence, with WA’s success in controlling the spread of COVID-19 being world-leading. If anything, this strengthens our own messaging,” he said. Dr Robertson emphasised the role of the Australian Health Protection Principal Committee (AHPPC), the key decision-making committee for health emergencies in Australia. “The AHPPC includes membership from all state and territory Chief Health Officers, including myself, and is chaired by the Australian Chief Medical Officer. “The AHPPC began working closely together at the beginning of the pandemic and continues to meet daily to discuss new evidence and issues, which requires consensus from the committee, and provide public health advice to the National Cabinet. “The AHPPC works with states and territories to develop and adopt national health protection policies and guidelines to ensure
An important aspect to public health is clearly and concisely communicating risk to change behaviour, which may sound simple yet is anything but, particularly within the ever-changing environment of a pandemic. “It does take a bit of time for knowledge to filter through to the general public and as soon as it does, things change. The real challenge of the pandemic is just how quickly things are changing [and our understanding of COVID-19] so information can go out of date so quickly, Dr Carissa Bonner explained to Medical Forum. Dr Bonner is a behavioural scientist and research fellow at The University of Sydney who specialises in evidence-based decision making and risk communication strategies to address problems in public health. Although the understanding of COVID-19 is still growing, there are some knowns that are stable, and it is these aspects which are important to convey continually to the public, according to Dr Bonner. “We know that the threat is real and that can be a consistent message. We know the main ways to prevent [transmission] have not really changed: social distancing, basic hygiene, and handwashing. And now, in Australia, the really important thing for people to know
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
Dr Carissa Bonner Image – Copyright: @ The University of Sydney / Stefanie ZIngsheim
The rise of Public Health
a coordinated COVID-19 response through the alignment of plans. Again, this additional level of scientific oversight serves to strengthen our own evidencebased messaging,” he said.
BACK TO CONTENTS
FEATURE
BACK TO CONTENTS
FEATURE is when and where to get tested so that we can keep it under control.
presented to the public before the COVID-19 pandemic.
“Although the evidence is changing all the time, the basic messages we need to convey are quite consistent, which is something that all levels of government can do consistently.”
“People understand that some things get politicised, but other things will be delivered directly and truthfully. We have a track record of honestly conveying health messages to the public for the most part,” she said.
Confidence in message So far, the Australian population has accepted the federal and state governments responses, according to Dr Bonner’s research. “Confidence in state governments is about 75% and the federal government 65%, which compared to countries such as France and the US, is very high.” Dr Bonner emphasised that this research was conducted in April, was not totally representative of the Australian population, and was currently published on a preprint server. “Overall, most people trust the government in Australia and is in a good position for public health communication. Although there is a lot of media coverage about the anti-vaccination movement, especially since COVID-19, this is still a small minority of people who believe those things.” Dr Bonner and her colleagues recruited more than 4300 participants from across Australia into a prospective, longitudinal online survey to investigate the prevalence of beliefs in COVID-19 misinformation. “We were particularly interested in whether people, theoretically, would take up a vaccine. We have been following this over time and it is now more than 80% [of respondents in favour] even though the threats that have gone down in some states, particularly Western Australia,” explained Dr Bonner. Australians’ high confidence in their elected officials could be attributed to how health messages had been
“Australia has been a leader in public health initiatives such as tobacco regulation. As a country, we are quite accepting of that sort of intervention at a government level.” While most of the government communications have been effective, not all were totally appropriate, Dr Bonner said. “The promotion of the COVIDsafe app to get restrictions lifted quickly was problematic because the lifting of restrictions was completely independent of the app. There has been media about how the app has been relatively ineffective as well, so that was one example where the government was not quite so open. “For the most part, though, I think they have done a pretty good job of being open about the uncertainty.”
Media matters Regardless of the message, mass media plays an important role in disseminating public health information. “A lot of people still get their information about this pandemic from public TV, which is surprising to some younger people who don't use it so much,” Dr Bonner said. “Yet the mass media campaigns have been quite effective for getting the basic messages through to most but not all parts of our community. For example, we know younger people are more likely to agree with misinformation, and are less likely to engage in traditional news media.” Yet not all media plays with a
straight bat, with various outlets in Australia profiting from sensationalist coverage of the pandemic, at the expense of public health messaging. However, the real threat to public health messaging lies in the mainstays of misinformation – unregulated social media and digital applications such as Facebook, YouTube, Twitter and WhatsApp. “We know that a lot of the conspiracy beliefs are spread through social media. It is a tricky international issue with attributing responsibility to owners of the apps. “They do seem to be taking responsibility by marking content when they think something is not reliable information and directing people to government websites. They are stepping up a bit during the pandemic,” she said. Although misinformation and conspiracy theories have swirled around public health for decades long before the rise of the internet, social media has provided previously unattainable access to publishing. “It is easier for small groups to have a big influence if they know how to use social media, which seems to be the case with anti-vaccination groups. They are already campaigning against a vaccine before one is even available. And they seem to have been doing that quite effectively.” As part of the COVID-19 misinformation and beliefs study, Dr Bonner and her co-researchers asked participants in June about conspiracies surrounding the pandemic, finding relatively small numbers believing such ideas as 5G being causal to the spread of the virus. But there is broader confusion about specific treatments such as ibuprofen, hot temperatures and UV light, which had 20% of the sample querying. “We have found associations between things such as trust in government and misinformation. It is particularly an issue of health literacy. People who have less skills to access and understand reliable health information do seem to be more inclined to believe some of the less helpful information. If we are aware of that, we can at least address it and focus communications to those groups.” continued on Page 23
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 21
Why Mount Hospital... Not only is Mount the leading provider of Cardiothoracic Services in Western Australia, for over 30 years Mount has been home to leaders in respiratory and sleep health on site at Perth Respiratory & Sleep Clinic. Perth Respiratory & Sleep Clinic offers an integrated breadth of services in: • Lung Cancer.
• Respiratory Health.
• Cardiothoracics.
• On Site Sleep Clinic.
To find out more please visit: www.perthsleep.com.au or phone 08 9481 2244.
Introducing:
Dr Michael Prichard
Respiratory Physician
Dr Prichard consults at Mount Hospital and sees patients for all respiratory and sleep issues and has a special interest in: • Obstructive sleep apnea
• Occupational lung disease
• Airway disease
• Other sleep disease
• Respiratory infection
Introducing:
Dr Lokesh Yagnik
Interventional Pulmonologist
Dr. Yagnik consults at Mount Hospital and sees patients for all respiratory issues and has a special interest in: • Lung nodule evaluation
• Fiducial marker placement
• Lung cancer diagnostics and staging
• Severe emphysema for lung volume reduction
• Central airway obstruction • Mediastinal adenopathy management
Find out why Mount Hospital is excelling in quality patient care. Mount Hospital Ph: 08 9327 1100 | mounthospital.com.au | 22 | SEPTEMBER 2020
Mount Hospital by Healthscope
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
FEATURE
The rise of Public Health continued from Page 21
Cultural context These groups also tended to be schooled from different health care systems and cultural backgrounds, highlighting the difficulty in interpreting public health information when English is their second language. “From a public health perspective, we can identify groups in the community that maybe more susceptible to misinformation ensure we're countering it with reliable information that specifically addresses these beliefs,” Dr Bonner. “There hasn’t been fantastic communication in first languages. “Public health information needs to be simple yet clear – both understandable and actionable. We can do that by following basic principles such as not using confusing terms like social distancing when what you actually mean is to stay 1.5m away from other people. Just being clear and direct about what exactly it is that you need people to do and use the simplest language you can. “The second step is translating that message into different languages to ensure everyone is getting understandable information on which they can act. These messages need to be tested with end users to ensure they make sense.”
More to the puzzle Although public health is evidencedriven, evidence is only one piece of the puzzle in delivering messages and implementing policy, according to Professor David Preen. “You can have the best evidence in the world but if it doesn't translate to actually influencing those who are making decisions, for example, how we are going to deal with COVID-19, this can be an issue.” Prof Preen is the Chair in Public Health at the UWA School of Population and Global Health and specialises in the adoption
and implementation of empirical research evidence in policy decision making to inform evidence-based public health policy. Prof Preen used the Australian response to COVID-19 as an example of a functional, evidence-based public health apparatus, with state and federal governments expediently informing policy and coordinating interventions based on the advice of public health specialists. “Essentially, there is a pipeline between evidence generation and advocacy based on evidence and that is all considered in decision making,” he said. “Australia has one of the best health systems in the world, in my view, with public health being a foundational element. If you have the infrastructure and platforms in place, even when something as unexpected as COVID emerges, the ability to respond quickly in a crisis is much better. “Look at countries where there is less coordination, less robust systems in place, less communication or consistent communication between frontline healthcare services, healthcare provision, policy makers, and the community and they have largely not fared as well as Australia in respect to a response to the pandemic and flattening the curve,” explained Prof Preen
Structurally sound Evidence is crucial for informing policy. When combined with the relevant expertise in the public health system this enables quality health care delivery, Prof Preen explained. “In Western Australia, similar to most other states, our Health Department has a dedicated Public and Aboriginal Health division that comprises a range of directorates responsible for areas such as communicable disease control, environmental health, health promotion, disease surveillance, epidemiology, disaster surveillance, and regulatory change,” he said. “All are working cohesively on public health with experts who are medically trained and researchers who are able to generate or digest evidence to feed that through to the
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
heads of those divisions, who from my experience, are very receptive to sound scientific evidence. “We have experts informing the state and federal health ministers, the premier, the chief medical officer, and the prime minister who have that machinery behind them and their decisions. “This means that the best recommendations can be put forward in a fairly short space of time.”
Swift and slow Not all public health recommendations lead to rapid adoption of policy, such as anti-smoking campaigns and regulations, which took decades to enact, Prof Preen said. “People might be surprised, now, to know that it took decades for governments and regulators to start taking smoking seriously, yet the scientific evidence was being generated from the 1950s onwards. While, WA and Australia have led the world in anti-smoking legislation, most major legislative reforms did not occur until the 1990s onwards. Many nations still do not have such reforms in place even today.”
Messaging fatigue Persistence and consistent messaging are key to delivering public health messages – one does not need to look far to see the nowfamiliar ‘stop the spread’ marketing materials. However, Prof Preen cautions that with the success of these efforts, so, too, comes message fatigue. “We can have evidence-based health promotion campaigns that tick every box, and have a fantastic connection and coordination between evidence and policy but once people have heard the same message, time and time again, they do not necessarily pay attention to the same degree. “In the instance of COVID messaging, it needs to continue, especially in the absence of vaccination or complete suppression and the messaging needs to evolve and adapt so that it stays at the forefront of people's minds and not remain static.”
Read this story on mforum.com.au
SEPTEMBER 2020 | 23
BACK TO CONTENTS
FEATURE
Tracing the source WA’s contact tracers have a steady hand on the COVID tiller at home, while lending much needed support to Victorian colleagues.
James Knox reports.
Western Australia has, so far, been successful in controlling COVID-19 cases, largely due to West Australians’ compliance with public health measures, the state’s relative isolation, lack of population density and the vital role of contact tracing. Victoria is another story. Behind the headlines, politicians and health bureaucrats are finely tuned teams of investigators meticulously tracing each contact of a confirmed COVID-19 case. Contact tracing may have become part of the vernacular in these COVID-19 times, however, it has been part of public health practice for centuries, with the first recorded contact tracing being performed by physician Andrea Gratiolo in 1576 to trace the contacts of a symptomless woman accused of spreading the bubonic plague in northern Italy. Gratiolo meticulously investigated the woman’s movements and interviewed people she had been in close contact with and found none was infected with the black death. Although Gratiolo’s contact tracing may seem like the rational thing to do, at the time it was unheard of, particularly when consensus of the 24 | SEPTEMBER 2020
plague’s causality was thought to be God’s punishment for sinners. From Gratiolo’s nascent efforts, contact tracing has become an essential practice in investigating the transmission of infectious diseases. While technology and infectious disease epidemiology has made contact tracing more effective and efficient, the practicalities are much the same as they were four centuries ago – it comes down to a conversation between two people.
What is contact tracing? In essence, contact tracing is investigative work seeking the source or index case of an outbreak and methodically identifying all possible contacts of a positive case, interviewing them and ascertaining, in granular detail, their interactions, then contacting and assessing each possible contact and, depending on their infection risk, having them placed in quarantine. To understand how the process works in WA, Medical Forum spoke with the Clinical Lead of Public Health Operations for COVID-19 at the WA Department of Health, Dr Ben Scalley. Every time a positive case of COVID-19 is identified, the contact
tracing team at WA DoH is notified and the process of contact tracing begins. While COVID-19 has presented contact tracers with a novel disease to trace, the fundamental processes of tracking cases and contacts is the same as used elsewhere in public health system and was used during last year’s measles outbreak. According to Dr Scalley, once a case of COVID-19 is confirmed, the team looks at the movements of each case in detail and the people with whom they have been in contact. These contacts may be obvious – from the household, workplace, or social networks – to the less obvious such as those who use shared facilities including bathrooms. “When a close contact is established, they are notified and put into quarantine for 14 days from the time of their exposure. We then monitor them for symptoms so that if they become unwell, they are isolated at home, stopping the chain of transmission,” he said. The radical change for the tracing team during COVID-19 is its size. From a core team of 25 it has increased to 170 at the peak of the pandemic. The team is primarily
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
FEATURE nurses and doctors who have received specialised training.
goes into each of the cases we've had so far.”
Elements of the team are currently helping the Department of Health and Human Services in Victoria to contact trace during its coronavirus outbreak.
Dr Scalley said the confirmed cases were often easier calls to make as they have already been tested and have assimilated their new normal. Whereas the contacts of confirmed cases are usually unaware they have been in close contact with someone who was infectious.
Dr Scalley attributes success in flattening the curve here in WA to the population taking the disease seriously, which has made his team’s work all the easier. “The good thing is that people within the state have taken to the social distancing measures. People have taken quarantine seriously when they return from overseas, they have removed themselves and self-isolated if they have not been feeling well, or when they were found to be a close contact of a confirmed case. “All these measures have meant that contact tracing in WA has been a lot easier.” Dr Sculley said each investigation, typically, can take days, especially if people were unaware they were infectious or did not quarantine. “Often the conversation initially might be up to two hours longer and might require clarifications. If someone asked you what your exact movements were a week ago, it might take a little while to recall. And then talking to all the different contacts, that might take a number of hours,” he said. “There’s a lot of skill in prompting people with the right questions, such as asking them to look through their financial records to confirm where they may have been. “Then we're checking in on the confirmed cases every day until they are no longer infectious and all of the quarantined contacts for 14 days. There's a lot of work that
“That is quite a hard conversation to have, telling someone to essentially take a break from their life for 14 days and stay home. “The vast majority of people we speak with are accepting because they understand the broader context, the broader benefit to all West Australians.”
The contact tracers Understanding the history of contact tracing and the processes are all well and good, yet who are the people undertaking this vital work? Clinical nurses Honey Lawton and Jane Newcomb are part of WA Public Health Operations’ (WA PHO) contact tracing team currently assisting Victoria Health. Prior to becoming a contact tracer, Mrs Lawton told Medical Forum she worked as a clinical nurse in a tertiary hospital for 15 years where she recognised the importance of public health in disease prevention. When the opportunity was presented to become a contact tracer, she jumped at it. Mrs Newcomb was a clinical nurse at the Australian Council of Healthcare Standards – travelling around Australia assessing mandatory standards. When she was asked to assist, she thought it was an opportunity to do her bit to help out in a pandemic.
Most of the contact tracers in the WA PHO are registered nurses, yet, according to Mrs Newcomb, the role not only requires clinical skills, education, and experience but also effective communication and investigative skills. “It helps to be able to pick up clues over the phone, including being able identify any problems or concerns as we’re talking to people. We need to have good problemsolving skills and be something of a historian to trace people’s movements in their incubation and infectious period.” The WA PHO has four working teams – WA contact tracing, ongoing management (of WA cases and close contacts), quarantine management and Victoria contact tracing. “Staff will then rotate within these teams to allow everyone to remain efficient and up-to-date on new processes within each area. No two cases are alike – and each case is interviewed individually,” Mrs Lawton said. A day in the life of a contact tracer can vary depending on the amount of cases or new cases, Mrs Newcomb said. “If you are interviewing a newly confirmed case, you’re identifying their movements and any close contacts who could potentially put the community at risk. These people then need to be contacted and informed of the need to isolate for 14 days, preferably away from others in their household so as not to put them at risk. “Each case is followed up individually, although sometimes with family members in the one household, one key person (such as mum or dad) will provide the information for the family.” When a person has been identified as a close contact with a confirmed case, contact tracers are often the first to inform them, which can be challenging, said Mrs Lawton. “They usually handle it well, although for some people being asked to quarantine for 14 days can cause them some stress, as this can obviously have an impact on their ability to earn an income.” Mrs Newcomb underscores why effective communication skills
WA clinical nurses Honey Lawton (left) and Jane Newcomb.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
continued on Page 27
SEPTEMBER 2020 | 25
MRI | CT | PET- CT | Ultrasound | X-Ray | NucMed | Dental
Envision. Artificial Intelligence At Envision, we routinely use AI to enhance all Chest CT interpretation
Siemens AI-Rad Comparison
Artificial Intelligence reconstruction for improved pulmonary nodule detection
Envision. Much more than a picture. 178-190 Cambridge Street | Wembley | 6382 3888 | envisionmi.com.au 26 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
FEATURE
Tracing the source continued from Page 25 are so important for contact tracers: “Informing someone of their contact with a case and what it means for them regarding quarantine can be stressful, so compassion, understanding and empathy is important, as well as being informative about what quarantine means to the person and their family.” According to the Department of Health, all of WA’s recent COVID-19 cases have occurred in people who have come from overseas and have been required to quarantine in a hotel upon arrival. Therefore, their close contacts have been minimal and easily traced. “Only a small portion of our case load is focused on active COVID-19 cases as we have low numbers In WA at present. We are in contact with our active cases daily to monitor their health and symptoms,” Mrs Lawton said. Although WA’s only cases are currently from overseas, Victoria has significant numbers of new cases from community transmission. The WA PHO team has been tasked with assisting the contact tracing effort currently under way by the Victorian Department of Health and Human Services (DHHS) and Australian Defence Forces. “We are given roughly 20 to 30 cases daily via a live database that
lists relevant contact information. With this information we then contact trace positive cases and close contacts, at the end of each day a progress report and any issues with follow-up is provided back to Victoria,” Mrs Lawton said. Mrs Newcomb offers some insight into the situation in Victoria: “I have been the team lead for Victorian cases and developed a rapport with some of the team leads there. I phone them first thing in the morning our time to see if there have been any changes in direction or processes that we needed to be aware of. “We then check cases allocated to us and look at our capacity to do above that. I believe that WA has collaborated with Victoria to help as much as we can.” Back in 1576, Andrea Gratiolo had no methodology or process, this is not the case today.
“Each contact tracer follows the current operating procedures which guide us on what information we need. However, the actual interview itself can become quite a personalised process. It is important to establish a good rapport with the client as it will shape all future interactions with them,” explained Mrs Lawton. However, with the rapidly expanding body of knowledge surrounding COVID-19, the WA PHO must be agile as processes can change often. “We have developed set processes for contact tracing, however, with COVID-19, specific regulations for people coming to WA around testing and quarantined are changed and updated frequently, so the team must ensure they keep up to date with these changes daily,” said Mrs Newcomb.
Medical Forum 2020 readership survey Which of the following publications best delivers WA medical news to you? Medical Forum Medicus AusDoc The Medical Republic Other 0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Our readers tell us that Medical Forum is the trusted publication to deliver WA medical news.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 27
BACK TO CONTENTS
OBITUARY
Something about Harry Last month, RACGP President Dr Harry Nespolon passed away aged 57 following a battle with pancreatic cancer.
In his tenure he earned the respect of all who worked with him. Here is what they said. Dr Sean Stevens, Victoria Park GP and Chair of the WA faculty of the RACGP Harry’s work ethic was amazing. Early in his presidency I invited him to attend a WA council strategic planning day, which he accepted without hesitation. What I didn’t know is that the day before he was in Townsville and flew on the redeye to attend the meeting. He was a strong contributor to our meeting that day. If you asked him to do something, it was done, even during the late stages of his illness. He insisted that he didn't want people to know about his illness because he didn't want anyone going easy on him. He wanted people to keep treating him the same. He will be sorely missed. He was an amazing advocate for general practice. He never shied away from the difficult issues. He never took a backward step and he made no apologies. If you need somebody to represent general practice in these difficult times, I can't think of anyone better than Harry.
28 | SEPTEMBER 2020
Dr John Deery, chair Australian GP Alliance
Christine Nixon, chair of the RACGP board
Harry lead the RACGP and represented the interests of general practice with energy and commitment, and was particularly inspirational during the last six months. General practice is the cornerstone of primary health care in Australia, and Dr Harry Nespolon understood the critical importance for it to be both vibrant and viable to deliver the high quality of primary healthcare that Australians expect.
A Sydney-based GP and practice owner, Dr Nespolon was elected RACGP President in July 2018. Dr Nespolon promised to affect genuine change as president, and he delivered. He displayed extraordinary leadership during the unprecedented COVID-19 pandemic, advocating on behalf of GPs and the general practice profession to ensure Australia’s primary health clinicians can deliver patients the best possible care.
He worked hard to maintain funding at a critical time and to ensure that the small businesses that are GP practices are viable business entities. Harry was well aware that unless these businesses were viable, the platform to deliver high quality primary healthcare would not exist, and the health of Australians will suffer accordingly. General practice has lost a committed leader, and while the profession will continue to deliver the healthcare that Australians need, for this moment we pause in reflection of a life well lived in support of Australia and the profession.
He was fundamental to the college’s successful efforts in securing $500m for general practice to fight coronavirus, helping to expand telehealth for all patients and bring about the most far-reaching change for general practice in a generation. Despite his deteriorating health, Dr Nespolon was able to achieve a remarkable amount during the COVID-19 pandemic, and leaves an exceptional legacy. The board is in awe of everything Harry has been able to achieve, particularly over the past seven months. The RACGP and general practice was such a big part of his life, and he gave so much of
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
Vale Dr Harry Nespolon By Dr Joe Kosterich, Clinical Editor Although diagnosed with pancreatic cancer in October 2019, Harry Nespolon continued to live life as normally as possible. This captures the essence of the man. His passion for general practice, his family and life in general was unabated. He was a man of absolute integrity with a razor-sharp mind, remarkable work ethic, but above all – a great guy. First meeting in 1995, we were mates from day one. Maybe it was a common heritage – both being sons of post-war European migrants, a love of footy (AFL) or a love of red wine – who knows. I remain grateful that our paths crossed. The ability to see issues from different angles and think laterally set him apart and enabled him to see solutions where others saw problems. This was applied in all his varied roles in medicine, both at the practice, organisation and policy level. His engaging manner and brilliant mind enabled him to succeed where others failed. True to his Italian ancestry, Harry loved a good meal and we shared many at a multitude of restaurants, generally with a bottle of red – South Australian shiraz being his preference. We would laugh ourselves silly at some of the antics of those who take themselves too seriously.
A passionate Carlton fan, Harry saw the glory days of the 1980s and longed to see the Blues rise again. He enjoyed travel including trips back to the north of Italy and long lunches with relatives. Later in life, one would not find a more devoted father to his two girls or loving partner. Harry’s life was full, and he touched the lives of thousands. His legacy will live on. In show biz they say you should leave them wanting more. Harry, I speak for us all in saying we wanted you to have more years. Rest in peace.
himself to advocating for the central role of general practice to the health of Australians.
Institute for Respiratory Health Clinical Trials
Minister for Health, Greg Hunt Dr Nespolon worked very closely with myself and the Government. He was a passionate but also reasoned advocate for GPs and, above all, for their patients. His tenure as president coincided with a period of reform and then, of emergency – both the bushfire emergency and more recently the ongoing COVID-19 pandemic. Throughout these challenges, and his own personal battle with cancer over the past nine months, he remained tireless, eloquent and cogent in his leadership and drive for positive change. He will long be remembered for his intellect, passion, dedication and professionalism.
Could a clinical trial help your patients? Help turn medical breakthroughs into life-changing treatments. Our Clinical Trials Unit conducts phase 1 to 3 trials for the folloiwng conditions: • • • •
Alpha-1 antitrypsin deficiency Asthma Bronchiectasis Chronic obstructive pulmonary disease
• • •
Cystic fibrosis Idiopathic pulmonary fibrosis Pulmonary hypertension
To find out more please contact us: www.resphealth.org.au or call 6151 0888
Above all, Harry was partner to Lindy, and a father to two beautiful young girls. They should be immensely proud of him. He will be irreplaceable. His passing is a great loss to the RACGP, to general practice, and to all Australians. MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
institute for
RESPIRATORY HEALTH
QEII Medical Centre Level 2, 6 Verdun Street, Nedlands WA 6009 admin@resphealth.uwa.edu.au | 6151 0888
SEPTEMBER 2020 | 29
Feet first for new clinic The northern suburbs are now serviced by a multidisciplinary foot ulcer clinic and it is changing lives. Jan Hallam reports. In May last year, SCGH opened its multidisciplinary foot ulcer (MDFU) clinic, joining clinics at RPH and FSH in delivering some spectacular results for patients with complex, high-risk, diabetesrelated foot complications. The SCGH clinic serves the northern corridor and is a weekly outpatient clinic bringing together vascular surgeons, infectious disease physicians, endocrinologists, podiatrists and Silver Chain nurses to help these patients save their limbs and heal recalcitrant ulcers. SCGH Podiatry Head of Department Dr Mendel Baba, told Medical Forum that the service in its first 12 months had received more than 150 referrals from GPs and other services and
that demand was increasing as it became more widely known. Multidisciplinary foot ulcer clinics are regarded as gold standard for the management of diabetes related foot complications and it was a team effort to pull together the necessary specialties. Mendel credits Vascular Surgeon Dr Robert Ma and Infectious Diseases specialist Dr Ronan Murray with getting the ball rolling, which now shows no sign of slowing down. Referrals of complex cases to the clinic have come from within the hospital system, from GPs and community podiatry services. “For example, a GP might have a diabetic patient with a chronic non-healing foot wound who needs more specialist input. A senior podiatrist will assess the patient,
who might then require further imaging or blood tests. Then the patient is booked into our MDFU service,” Mendel said. “At that appointment, the patient will be seen by all the specialties – Vascular, Infectious Diseases, Endocrinology, Podiatry, and often the Silver Chain Liaison nurse as well. They all contribute to provide a treatment plan.
Securing the future “It’s working really well. The service is still evolving and developing and we're working towards accreditation. We are also looking to establish a business case for the implementation of an inpatient Diabetic Foot Unit, so there are dedicated beds for patients admitted with diabetes-related foot disease, which will improve
New medical centres Specialist rooms available. Secure your place. Contact Michelle Evans call: 9334 1451 email: medservices@stjohnwa.com.au visit: stjohnhealth.com.au/careers/specialists
30 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
NEWS
BACK TO CONTENTS
NEWS toe, which they declared a miracle. But last July, the left foot reinfected and I developed osteomyelitis.
Some of the SCGH podiatrists working at the MDFU clinic.
management of this multifaceted condition.
me at the Charlie’s foot ulcer clinic,” he said.
With the prevalence of diabetes increasing, diabetes-related foot disease is a rapidly growing problem and complications can be severe with amputation of toes and limbs not uncommon.
One-stop care
One of the first patients seen at the clinic was Mr Grantley McManus, who agreed to talk to Medical Forum. He knows just how serious diabetic foot disease can be. Mr McManus has been battling diabetic foot ulcers for about two years and last year developed osteomyelitis. “I don't mind admitting, I avoided the hospital like the plague because I was always scared of getting MRSA. I was seeing my GP and a private podiatrist but eventually my podiatrist made an appointment for
“It was all upwards from there. I saw the infectious disease guy, the vascular people, the diabetes people and Silver Chain, and this service had just started. It was fantastic, you know, pronto. “There was no having to make another appointment. It was all bang and go. “They got me to Home Link and Silver Chain came all weekend dressing the ulcer then I was back at the hospital on the Monday when they put in a PICC line and I started on six weeks of antibiotics. “Two years ago, I had bilateral ulcers on both feet, but they thought they'd have to amputate my toe on the right foot. I kept my
“I went into ED and they wanted to amputate but after four days in hospital to stabilise the leg, I left with another seven weeks of liquid antibiotics. I'm still on antibiotics after a year but I still have my leg. Ronan (infectious diseases physician Dr Ronan Murray) declared the left leg a miracle, but I didn't go to church enough so we’re still working on it.” Mendel said the clinic team was in the business of saving limbs and reducing the morbidity and mortality associated with diabetic foot disease. “We want to avoid any unnecessary hospital admissions and reduce the length of stays. And we really want to provide comprehensive, integrated care to these patients with complex foot disease,” she said. “There’s a lot of components to getting foot ulcers healed and patients go up and down in their progress, it's rarely a nice linear resolution. But patients are keeping their limbs which also means they’re preserving their mobility and independence.”
COMPREHENSIVE MRI SERVICES
Serving GPs and Specialists north and south with MRI at Madeley and Canning Vale • Latest Siemens cardiac-capable scanners delivering excellent image quality across the board. • Sub-specialised reporting - MSK, Neuro, Body delivered in 24-48 hours electronically. • High-detail imaging of large and small joints (wrist, hand & fingers) at all locations, every day. • Fast access to daily appointments and direct access to radiology team. All Medicare rebatable items (including procedures) are Bulk-Billed* when referred by GP or Specialist. Contact reception for pricing guidance. Western Radiology providing Advanced Diagnostic Imaging & Interventions in the community.
*MRI not Medicare rebatable.
9200 2777
9200 2778
www.wradi.com.au MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 31
OPINION
Breathe easier There is an old joke about a discussion between different parts of the body as to which is the most important – the tail end of the alimentary canal is derided and then goes on strike to demonstrate that it matters as much as the rest. It could be argued that first among equals is the respiratory system. Life (outside the womb) is deemed to start when the first breath is taken. We think of death as taking your last breath. This does not make the respiratory system more vital to life than the cardiovascular, nervous or other body systems. It is, however, true to say that the body can go longer without food, rest or water than without air. Different cultures look at the breath in different ways. In our society we don’t think much about it all. In Eastern cultures the breath is part of a person’s spiritual life as well as their physical one. It is a good thing that we don’t have to continuously think about breathing as it would be difficult to get much else done. Equally, a few slow deep breaths whilst not thinking about anything else can be a great stress buster!
In this respiratory health edition, there are articles looking at different aspects of lung health. Lung cancer remains a condition with stubbornly low five-year survival. There is an update on staging and treatments. By the same token, increased imaging throws up lots of ‘incidentalomas’. It is a challenge, requiring at times the proverbial wisdom of Solomon to balance the need to find cancer early with the risk of over diagnosis and subjecting people to harms for no net gain. This is discussed, too, together with a piece on thoracoscopy. We also look at how problems from the gastrointestinal system can manifest in the respiratory system.
it is interesting to recall that back in March there was concern about a shortage of ventilators. It increasingly emerged (especially in the USA) that the virus did not affect lung function as much as anticipated. There was a metabolic aspect to its effect.
For a change of pace there are updates on oral issues and rethinking mental health in the light of the current pandemic.
Look after your own health. Aim each day to do three or four slow deep breaths and clear the mind.
This brings us back to the start. All body organ systems are important as is the overall wellbeing of the person. Doctors are as prone to stress as anyone else. We need to apply the airline principle – when oxygen is needed fit your own mask before helping others. This is not to deny oxygen to others but to say that you can’t help others if you are not getting air yourself.
Now six months into COVID-19
Professor Richard Naunton Morgan — General Surgeon MBBS FRCS AMC FRACS
South Perth Hospital is pleased to advise Professor Richard Naunton Morgan, General Surgeon, has commenced a General Surgical service. Professor Naunton Morgan consults at 72 South Terrace, South Perth. Consultation bookings: 0466 342 100 Postal address: PO Box 214, Como WA 6952 Professor Naunton Morgan and his anaesthetist are no gap providers.
32 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
Dr Joe Kosterich | Clinical Editor
BACK TO CONTENTS
Clinical Updates Respiratory Health 35 REFLUX-INDUCED RESPIRATORY DISEASE Dr Michael Prichard
40 INCIDENTAL FINDINGS ON CARDIAC CTs
37 LUNG CANCER STAGING Dr Hilman Harryanto
45 VIDEO THORACOSCOPY IN EMPYEMA
39 RETHINKING MENTAL HEALTH IN COVID-19
Dr Jenny Brockis
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
Dr Scott Claxton
Dr Parshotam Gera
47 ORAL MANIFESTATIONS OF IBD
Dr Amanda Phoon Nguyen
SEPTEMBER 2020 | 33
PoLetti road
No
cockburN MeNtaL heaLth Service
rt hL
ak
er
oa d
cockburN traiN StatioN
the arc
Cockburn Mental Health Service 45 bed inpatient unit, Wellness & Recovery Centre, group day therapy, consulting suites, ECT, TMS NEW, innovative services incorporating e-health
Bridging the gap between hospital and community services Excellent location. On-site parking and public transport walking distance 34 | SEPTEMBER 2020
Would you like to be part of Perth’s newest Mental Health Service? Join a multi-disciplinary team of psychiatrists and mental health professionals at the first private Mental Health Service south of the river. Psychiatrists and Registrars are encouraged to enquire via email. For more information, subscribe to our mailing list via the Bethesda website. cockburnmhs@bethesda.org.au www.bethesda.org.au | 08 9340 6300 25 Queenslea Drive, Claremont WA 6010 MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
Reflux-induced respiratory disease By Dr Michael Prichard, Respiratory Physician, Perth Reflux of gastric contents into the oesophagus may occur during intermittent relaxation of the lower oesophageal sphincter (LOS). Occasionally there is free reflux through an incompetent LOS, sometimes associated with a hiatus hernia. Reflux into the lower oesophagus when upright is cleared readily by swallowing, peristalsis, gravity. Local mucosal factors help protect against intermittent acid injury (epithelial lining fluid and saliva, carbonic anhydrase). Reflux symptoms (regurgitation, belching, heartburn) are common and not necessarily pathological. However, recurrent reflux can result in chronic aerodigestive disease. Gastro-oesophageal reflux disease (GORD) is usually considered an oesophageal disease, affecting about 20% of the population, but may also present with upper and lower respiratory manifestations (Table 1). Most reflux-induced airway and lung injury occurs as a result of high reflux and micro-aspiration during sleep. While sleeping, there is reduced oesophageal sphincter tone, increased evening acid production, delayed gastric emptying, impaired oesophageal
Anecdotally, single interventions tend to be less effective than combination therapy, however, there are no randomised controlled trials. Combination therapy includes proton pump inhibitors (PPI) at night, H2R blocker, promotility agent, dietary modification (avoid eating late, small evening meal, avoid certain food groups), raised head of bed, weight loss. Fig 1. Penetrated PA chest x-ray demonstrating a retrocardiac opacity with air fluid level (blue arrow): moderate hiatus hernia.
clearance of acid and reduced swallowing and saliva production. Obstructive sleep apnoea (OSA) is a key risk factor for nocturnal reflux due to increased transdiaphragmatic pressure. Acid and pepsin are additive in causing respiratory mucosal injury. Barium swallow and upper GI endoscopy are useful when positive but have limited sensitivity. Oesophageal pH studies are more useful for oesophageal disease. Measurement of pepsin or bile acids in respiratory secretions are generally diagnostic, but not yet readily available. The best ‘diagnostic test’ is response to combination therapy.
Table 1: Extra-oesophageal disorders secondary to gastro-oesophageal reflux. Location
Disorders
Oropharyngeal
dental erosion postnasal irritation chronic rhinitis
otalgia sleep disordered breathing
Laryngeal
Globus sensation Frequent throat clearing Dysphonia
Paroxysmal reflex laryngospasm Subglottic stenosis Laryngeal carcinoma
Bronchopulmonary
Chronic cough Chronic bronchitis Recurrent respiratory infections
Chronic bronchiolitis Community-acquired pneumonia Aspiration pneumonia, abscess Acute lung injury Exacerbation of chronic lung disease
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
Case study A 45-year-old woman has a fiveyear history of gradually increasing cough, initially dry, and more recently productive of mucoid sputum. Her cough tended to be worse in the morning, sometimes caused sleep disturbance and, rarely, she woke from sleep with a choking sensation. Weight increased 18kg in the past decade, recently her voice was hoarse, and she noted wheeze and shortness of breath, unresponsive to overthe-counter salbutamol. She complained of waking unrefreshed in the morning and daytime sleepiness. There was a history of snoring but not asthma. On examination, she was overweight (BMI = 32), had noticeable dysphonia, mild pharyngeal erythema and reduced pharyngeal volume (Malampatti class IV). Respiratory examination: wheeze on forced expiration. Spirometry demonstrated moderate volume loss with no bronchodilator response. Chest x-ray showed a moderate hiatus hernia (Fig 1). This is a typical presentation of reflux induced cough and asthmalike symptoms in an adult. A sleep study demonstrated severe OSA which responded to CPAP. Prior to commencing CPAP, she was treated with PPI, pro-motility agent at night and dietary modification and her cough, wheeze and dysphonia resolved over three weeks. Author competing interests – nil
SEPTEMBER 2020 | 35
36 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
Lung cancer staging – a snapshot of diagnostic pathway By Dr Hilman Harryanto, Respiratory Physician, Nedlands Lung cancer remains the leading cause of cancer death in Australia with the five-year survival rate remaining at a disappointing 18%. Morbidity and survival outcomes are highly dependent on early diagnosis. The National Lung Cancer Optimal Pathway endorsed by state and federal governments recommend six weeks as the time from initial identification of potential lung cancer to complete staging and diagnosis and receiving first treatment. It can be challenging to meet this. The current recommended staging pathway (see below) is a stepwise approach. First step is a wholebody 18F-fluorodeoxyglucose (FDG) PET scan (can be omitted if baseline CT has already identified metastatic disease) to identify whether the patient has locally advanced disease (stage I-III) or systemic disease (stage IV). If stage IV disease is identified (approximately 40% incidence),
Key messages
Lung cancer survival outcomes highly depend on early diagnosis
First step is a whole-body
18F-fluorodeoxyglucose (FDG) PET scan staging (unless metastatic disease identified on baseline CT chest) EBUS-TBNA significantly increases mediastinal lymph node staging accuracy. it is generally advised that histopathological tissue diagnosis is obtained from distant metastatic sites (where most accessible and least invasive to obtain), either via ultrasound or CT-guided biopsy. A positive biopsy of the primary lung lesion on its own will not answer the question of whether the distant metastatic deposits are from lung origin or in the offchance, might have arisen from a separate synchronous malignancy.
Lung nodule/mass suspected to be lung cancer – with no evidence of metastasis disease on baseline CT-chest
18F-FDG PET scan
Negative nodes on PET/CT with small peripheral lesion
N2/N3 enlarged nodes on CT or positive on PET
Lowest risk diagnostic procedure (navigational bronchoscopy, CT biopsy, or excisional biopsy)
Normal N2/N3 nodes on CT/ PET but central, large tumour (3cm) or N1 positive node
Mediastinal lymph node staging with EBUS-TBNA bronchoscopy
Thoracic multidisciplinary meeting
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
Stage IV on PET
Least invasive tissue biopsy
Whereas tissue diagnosis from other metastatic sites can be traced back to lung where it exhibits typical immunohistochemical markers (i.e. TTF-1). If no distant metastatic disease site is identified on staging scan and the disease is found to be stage IA (primary tumour size <3cm and no suspicious node was identified on FDG-PET scan – approximately 10% incidence), it is generally advised that the histopathological tissue diagnosed is obtained directly from the primary site via navigational bronchoscopy or CT-guided biopsy. Where a larger tumour or suspicious node is identified on staging scan, a diagnostic bronchoscopy with linear endobronchial ultrasound (EBUS) transbronchial needle aspirate (TBNA) is recommended. This is a minimally invasive technique to biopsy mediastinal lymph node. Staging scan alone cannot accurately stage the disease, given associated high false positive (FP) and false negative (FN) rates. In radiographically identified N2/N3 nodal disease (metastasis involving lymph nodes beyond mediastinal or subcarinal in location), 40% FP rate is associated with CT and 15% FP and 25% FN with PET. Conversely, in cases of large central tumours (>3cm) with only radiographical positive N1 nodal disease and negative N2/N3 disease, a 25% FN rate of lymph node metastasis is associated with CT and PET; and 15% FP with PET. EBUS-TBNA significantly increases the accuracy of mediastinal lymph node staging (specificity 100%, sensitivity 93%). Once appropriate staging has been performed, each lung cancer case should be referred to a lung cancer multidisciplinary meeting for complete optimal discussion on staging and treatment options. Author competing interests – nil relevant disclosures.
SEPTEMBER 2020 | 37
Your sleep health experts with heart ResSleep Western Australia is a leading sleep health clinic. For over 20 years, we have been providing professional, outcome-focused care for the treatment of snoring, sleep apnea and more. Every day, we earn our reputation by putting our patients first. With our team of friendly, knowledgeable staff and a comprehensive range of products, we are ready to help your patients achieve healthy sleep. We’re also proud to be a ResMed Authorised Dealer for the Department of Veteran’s Affairs and an NDIS affiliate.
What we offer: •
CPAP therapy equipment and support
•
Bi-level and ASV equipment trials
•
Alternative sleep health products
•
One-on-one education sessions
•
Telehealth and sleep coach services
•
CPAP Rescue Program
•
After hours phone support
•
Commercial driving management program
We’ll look after your patients At ResSleep, helping ensure patients have all they need for therapy is our key priority. Our virtual hub, PlaceofDreams.com.au, for example, enables them to book virtual consults, browse all our products and even read the latest sleep health advice online. And if you have patients who have trouble staying on CPAP therapy, please ask us about our CPAP Rescue Program. We’ll be glad to help them get back on track.
For simply better sleep 08 6168 1450 | adminwa@ressleep.com.au www.placeofdreams.com.au Perth | Murdoch | Mandurah | Joondalup 38 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
CLINICAL OPINION
Rethinking mental health in COVID-19 By Dr Jenny Brockis, GP and workplace consultant, City Beach Uncertainty, fear and a growing sense of isolation is leading to the next public health crisis as measures taken to respond to the pandemic take a toll on resilience and mental wellbeing. Heightened anxiety early in the pandemic saw a rapid rise in demand for psychological services. Now there is a more worrying trend of increasing despair and depression. Are more prescriptions for anxiolytics and antidepressants the best we can do in the face of increasing levels of psychological distress in our society? Can we find better long-term solutions to mental health problems? It’s time to think outside the square and ask questions. How can we get better at recognising who is at risk, better at understanding the significant role physiology,
Key messages
Mental health problems are increasing
We need to ask questions “outside the square” Evaluate and manage the whole person.
emotional wellbeing and social determinants play in risk management and better at educating our patients about the importance of looking after their mental health? How can we get better at advising on simple practical tools to improve or stabilise mood, and develop a smart integrated system that partners with a variety of health and community resources to
enable every patient to access the appropriate level of care and service needed in a timely manner?
Restoring mental wellbeing As Benjamin Franklin said, “A pound of prevention is worth an ounce of cure.” In times of crisis it’s natural to seek reassurance and to follow leaders we can trust. As health practitioners we can assist our patients by helping them understand what is normal to experience in these unusual times, what is possible for them to focus on to improve their state of mind, and how to become proactive and self-reliant to build long-term resilience.
continued on Page 40
NEW CLINIC – DUNCRAIG For your patients, a good night’s sleep begins with comfort. Get in touch today Murdoch Specialist Centre 78 Farrington Rd Leeming 6149
At SleepMed, we understand the value of a good night’s sleep. As Perth’s first accredited and licensed sleep investigation centre outside of a hospital, we focus on individual and holistic care to diagnose sleep disorders including snoring, sleep apnoea, and insomnia. Our highly trained sleep experts and therapists then develop personalised treatment solutions, prioritising the comfort of our patients at all times. Both insured and non-insured patients can access our professional Level-1 sleep studies, now in the comfort of a non-hospital environment.
New Clinic Glengarry Private Hospital 53 Arnisdale Road Duncraig 6023 T (08) 6161 7647 F (08) 6162 0547 E info@sleepmed.com.au Online referral welcome: www.sleepmed.com.au
Accredited by:
Licensed Day Hospital SleepMed Healthcare
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 39
Incidental findings on cardiac CTs By Dr Scott Claxton, Respiratory Physician, Joondalup Jennifer is 63 and complained of chest pain. She has a family history of ischaemic heart disease and a history of intermittent smoking for a few years. A CT calcium score didn’t show any coronary artery calcification but an incidental ground-glass nodule was seen in her left upper lobe (Fig 1).
other times they may be early stage disease or entirely benign. Incidental imaging of the lung fields brings them to attention. In turn the lung abnormality will need to be assessed on its own merits. Cardiac disease and respiratory disease share risk factors (smoking, increased age) and so abnormality in both is to be expected.
This was followed up over a twoyear period when it showed the development of a solid component (Fig 2).She was referred for resection and pathology identified an adenocarcinoma. CT-based investigation for diagnosing coronary artery disease and assessment of cardiac risk is increasing. As a result, coincidental imaging of the lung fields is also increasing. This has led to increased identification of clinically silent but not necessarily clinically irrelevant, non-cardiac abnormalities. These can comprise findings in the chest wall, breasts, skeleton, lung, pulmonary vasculature, mediastinum and non-coronary vasculature. Some will be clearly significant requiring prompt assessment. For others, the shortand long-term risk is not so clear and follow-up probably with further imaging will be required. Even in health, the respiratory
Fig 1.
system is exposed to numerous, potentially irritating or noxious challenges. Respiratory infection is common and over time these can lead to abnormalities in lung tissue that may be identifiable radiologically. With normal ageing comes changes in lung function and histology, a loss of elastic recoil, increased collagen deposition, loss of small airway supports. In addition, other more well-defined factors can impact on lung structure and function (cigarette smoke, pollution, asbestos etc.). While sometimes these may cause symptoms and be recognised,
Non-cardiac (and for the purposes of this discussion – pulmonary) incidental findings on cardiac CTs are generally grouped as either significant or non-significant. The former can include lung nodules and masses, pulmonary emboli, aortic abnormalities, breast masses, pleural masses and effusions. Non-significant, or perhaps better referred to as less immediately significant, findings include emphysematous change, small (<6mm nodules), pleural thickening, interstitial lung abnormalities. In one large study of 2050 scans, 5% had significant, non-cardiac findings. The most common were lung nodule (<3cm) or lung mass (>3cm). In a patient with a history of cigarette smoke exposure there is the concern that these lesions may represent early malignancy. For
Rethinking mental health in COVID-19 continued from Page 39 Every consultation is the chance to ask, “how are things going for you, really?” Remembering to check in on a person especially if they live alone, have little social support, have lost their job or are finding the ongoing situation increasingly difficult to manage. Doctors can provide accurate and trustworthy information to combat the hype, misinformation and conspiracy theories and reaffirm the positive aspect of healthy lifestyle choices.
40 | SEPTEMBER 2020
Use a brief questionnaire (e.g. Short Warwick-Edinburgh Mental Wellbeing Scale) and or subjective wellbeing questionnaire as a form of rapid assessment of mental wellbeing. Evaluate wellbeing on the basis of how people feel and function on a personal and social level, and how they evaluate their lives as a whole. Provide additional ongoing support via telehealth. This facilitates tracking patient progress, especially for those previously diagnosed with complex or severe mental health
challenges or considered vulnerable to poorer mental health. Making mental wellbeing part of a regular health check has the potential to reduce the prevalence of mood disorders in our community. Now that would be something to celebrate. Author competing interests - nil
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
BACK TO CONTENTS
CLINICAL UPDATE be related to previous cigarette or other (e.g. occupational) exposures. Often these abnormalities may be asymptomatic, or the symptoms accepted as part of growing older.
Key messages
The lungs are exposed to challenges and assaults, which can leave their mark. With the growing use of cardiac CT, these findings will be more frequent. The specific nature of the findings will determine the need and extent of follow-up.
large masses, further investigation (e.g. biopsy) may be indicated. For smaller nodules, further CT followup may be required. The specific program of follow-up varies depending on the nature of the nodule (ground glass, semi-solid, solid) and the risk of underlying malignancy (age, smoking history, nodule size, number of nodules, past history of malignancy). Data from lung cancer screening programs and other cohort studies has allowed the development of follow-up algorithms for pulmonary nodules dependent on the risk of malignancy (e.g. Fleischner
Initial clinical assessment and lung function testing may be indicated. Follow-up assessment either radiological or physiological (lung function) may be required to identify progression or development of disease especially with interstitial lung abnormalities.
Fig 2.
Society). These aim for a balance between accurate and timely detection of malignancy and limiting radiation exposure by repeat scanning. Other incidental pulmonary findings such as bronchial wall thickening, emphysema and fibrosis may represent age-related changes. This may include exposure to environmental pollution (i.e. urban compared to rural living) or
The timing of this is less clear than with nodules but may not need to be any more frequent than annually. Assessment of the potential cause is necessary. A history of occupational or environmental exposure (e.g. asbestos) may help with planning of follow-up. Prior imaging is always useful. – References available on request Author competing interests – nil
At SKG Radiology, we know your patient’s welfare, as well as your own, is very important to you. We recognise the continuing need to provide the same great quality service across our practice, so we are bulk-billing all out-patient Medicare rebateable services*, during this time of crisis. * Some exceptions do apply.
When y o u d ep e n d o n t h e r igh t r e su lt, t he c ho i ce i s cle ar, S K G R adio lo gy. MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 41
42 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 43
Genea Hollywood Fertility provides a comprehensive individualised range of fertility treatments for Western Australians. Our specialist team has up to 30 years’ experience in fertility treatments. Our patients have access to Genea’s world leading science. All patients have individualised assessment and treatment Genetic testing is available where needed Our treatment charges are transparent Our clinicians, scientists and support staff are committed to achieving successful outcomes.
Dr Simon Turner
Prof Lincoln Brett
MBBS, FRANZCOG, FRCOG
BMedSc, BSc (Hon, MBBS, FRANZCOG
Dr Julia Barton
Dr Michael Allen
Dr Joo P. Teoh
MBBS, FRANZCOG,
MBBS (UWA), FRANZCOG, MRMed
FRANZCOG, MRCP (Ire), MRCOG, MBBCh, Msc (Lon), MD (Glasgow) Subspecialty Repromed (UK)
FRCOG
Genea Hollywood Fertility means high success rates, understanding staff and individual care. Genea Hollywood Fertility Level 2, 190 Cambridge Street, Wembley WA 6014 p (08) 9389 4200 w wa.genea.com.au 44 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
Video thoracoscopy in empyema By Clin A/Prof Parshotam Gera, Paediatric Surgeon, West Leederville Pneumonic infection and the associated inflammation of the pleural lining leads to an exudative uncomplicated parapneumonic pleural effusion. This effusion becomes complicated if there is invasion of the pleural space by bacteria. The term ‘empyema’ is derived from the Greek words pyon, meaning pus, and empyein, meaning pusproducing. Thus, the presence of pus in the pleural space is consistent with the diagnosis of empyema. Empyema complicates pneumonia (incidence 1.0-4.5 cases/100 children) in around 0.6% of children and can result in significant morbidity. There are three stages of empyema. These are exudative phase (early empyema), fibrinopurulent phase (loculations) and organising phase (thick
Key messages
Empyema: pus in pleural cavity Chest drain with Fibrinolysis and VATS are accepted interventions in paediatric empyema VATS is a preferable to open thoracotomy in empyema.
Fibrinous peel in empyema.
fibrinous peel, presence of peel may hinder lung re-expansion). Various therapeutic options are available. Medical management (antibiotics) and surgical interventions. These include percutaneous aspiration and chest drain insertion (with or without intra-pleural fibrinolytic agents) ,video-assisted thoracoscopic surgery (VATS) and thoracotomy with decortication Surgical intervention is indicated when sepsis and infected fluid are not effectively controlled with antibiotics alone. Both VATS and chest drain with fibrinolysis (CDF) are accepted surgical interventions in a paediatric age group. In most paediatric centres VATS is considered only after treatment failure with CDF. VATS was described by Kern et al. in 1993 and provides access to the entire pleural space offering direct video-controlled imaging for visceral and parietal pleural debridement and decortication. Anaesthetic airway management is critical during VATS to prevent endobronchial aspiration and intraoperative hypoxaemia in lateral decubitus position.
other two ports are placed in accordance with triangularisation (ergonomics). The procedure involves disrupting all loculated fluid collections and to make multilocular empyema into a single communicating space. After aspirating the liquified exudate, the fibrin deposits/ peel is removed with grasper. Intermittent irrigation is useful to allow improved visualisation of pleural space. A small-bore chest tube is inserted at the end of the procedure. The lung is mobilised from apical pleural region, posterior costomediastinal gutter, anterior pulmonomediastinal recess and the entire diaphragmatic surface of the lung. Conversion to open thoracotomy might be required in advanced phase or with complications such as bleeding. VATS require surgical expertise which may not be available in all centres particularly non-tertiary hospitals. Contraindications to VATS include an inability to develop a pleural window to access the pleural cavity. Furthermore, VATS has several advantages over open thoracotomy including less postoperative pain, shorter hospital stay and better cosmetic result. Author competing interests – nil
VATS is performed by three (5mm) port incisions; one for 30-degree scope and the other two for instrumentation (laparoscopic graspers, suction).
Fibrinous peel.
The initial camera port is inferior most mid-axillary level and the
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 45
46 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
CLINICAL UPDATE
Oral manifestations of inflammatory bowel disease By Dr Amanda Phoon Nguyen, Oral Medicine Specialist, Perth Inflammatory bowel disease (IBD) is a broad term that consists of conditions with recurring and chronic inflammation of the gastrointestinal tract, represented mainly by the disease entities Crohn’s disease (CD) and ulcerative colitis (UC). There is an approximate equal distribution of the two clinically definable entities, although in 15% of patients with UC, the distinction is not clear, and these patients are classified as having indeterminate colitis. The distribution of the inflammation in the gastrointestinal tract involves only the large bowel in UC, and most commonly the ileum and colon in CD. IBD is more common in males and is seen increasingly in children. Australia has more than 80,000 Australians living with these conditions, with numbers expected to increase to more than 100,000 by 2022. It is not uncommon for patients with IBD to describe a long
Key messages
Oral manifestations of IBD may precede gastrointestinal symptoms. It may be the only presenting sign of IBD. IBD may have negative effects on oral and dental health. diagnostic process taking months or even years. Oral manifestations are not uncommon with an estimated prevalence rate of between 20% and 50%, (more common in CD than UC). In adults, the oral symptoms appear less often than in children, and a higher degree of perianal involvement in patients with oral symptoms has been reported. In a minority of cases, oral involvement may precede the intestinal lesions. The oral manifestations may also be the only presenting sign in a small percentage of affected patients.
17-year-old female with a 4 week history of a lower lip swelling (a), which was accompanied by: (b) Lip fissuring (c) Mucosal cobblestoning (d) “Staghorning”
A
While oral lesions might be more severe during active intestinal disease, approximately 30% of patients may continue to manifest oral lesions despite intestinal disease activity being controlled.
Specific oral lesions Mucogingivitis (gingival swelling, erythema and there may be ulceration present) is the most common. Others include mucosal tags (small, localised, firm nodules which are often asymptomatic), cobblestoning of the buccal mucosa (mucosal nodularity where the mucosa can appear hyperplastic with corrugation), oral ulceration (which is usually linear, running the length of the buccal sulcus or alveolar mucosa), firm lip swelling (usually the lower lip) and vertical fissures involving the lip. Non-specific oral lesions include aphthous-like ulceration, ‘staghorn sign’ (swelling in the floor of mouth), pyostomatitis vegetans, angular cheilitis, persistent submandibular lymphadenopathy, gingival hyperplasia, taste changes and oral candidiosis. Orofacial granulomatosis may present a diagnostic challenge, as it can present very similarly to the above. Besides the above, there is also increased risk of dental decay, periodontitis and oral infection.
B
Patients at risk should be encouraged to maintain frequent preventive and routine dental care. Gingival bleeding is common, occurring in about 20% of patients. Oral lesions associated with IBD generally resolve once the gastrointestinal disease is under control. If symptomatic, the use of topical anaesthetics such as lidocaine, topical and/or systemic corticosteroid therapy may be indicated, however, liaison with the patient’s gastroenterologist is recommended.
C
D
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
Author competing interests – nil
SEPTEMBER 2020 | 47
Smoking in underground metal mines Smoking in the workplace has been banned for years, except, it seems, in the world underground.
Emeritus Professor Odwyn Jones explains.
It is time to explore the health effects of environment tobacco smoke (ETS) in addition to existing diesel engine exhaust fumes and other carcinogenic dusts in underground metal mines. And in that inquiry, address the hazard of smoking cigarettes in mines which are subject to rare and unpredictable inflows of flammable gas from previously unknown methane pockets/bubbles within surrounding strata. Whereas the Davy Safety Lamp was a life saver for those working in underground coal mines, carbide lamps with their open flames continued to be in use in metal mines until the development of the highly efficient electric battery cap lamps. Not surprisingly, therefore, metal miners were, and still are, allowed in many jurisdictions to smoke at underground worksites. The question is, bearing in mind our updated knowledge of its health effects etc. and possibility of igniting inflammable methane/air mixtures, should it continue to be allowed.
Health effects of ETS in breathable air already polluted by other carcinogenic dusts, vapours and fumes Whilst there is nothing in WA’s Mines Safety and Inspection Act 1994 or its regulations regarding the practice of smoking tobacco products in underground metal mines, apart from a brief reference in Regulation 8.13(1) to the prohibition of smoking within eight metres of activities 48 | SEPTEMBER 2020
involving explosives, there is reference by Worksafe to legislative interpretations. It answers the question put by a mine manager regarding how the Smoke-Free Places Act applies to smokers who work underground and it is quite revealing. Worksafe stated that, based on the definition of ‘indoor workplaces’, the act applies in an underground mine. However, it goes on to state, given that: • Flow through ventilation is efficient in removing diesel emissions to ensure safe breathable air for miners, it is assumed that any ETS generated in areas of flow-through ventilation will be removed along with the diesel emissions. • It is also recognised that it would be impractical for smokers to leave underground areas for a smoke-break. It therefore concludes that “smoking will be allowed in an underground environment in areas with flow-through ventilation, but is not allowed in lunchrooms and refuge stations”. Furthermore, it states that “this interpretation does not prevent the employer from exceeding its requirements”. The underlying premise that flowthrough ventilation at underground worksites is efficient in removing diesel emissions is and has always been false. As stated by Adrian Barnett: “it’s safe to say there is no safe level of air pollution” and recent NHMRC-sponsored research of underground miners’ exposure to diesel exhaust fumes, which
has been estimated in 2011 for an underground miner’s working lifetime to be associated with 38 extra lung cancer deaths per 1000 males.
Toxicity and Health effects of ETS ETS is smoke from burning tobacco, which permeates the surrounding environment and other persons can breathe. It is sometimes referred to as ‘secondhand smoke’. ETS is a complex mixture of particles, vapours and gases, and includes more than 4000 compounds of which 60 are known carcinogens. These include carbon monoxide, nicotine, polycyclic aromatic hydrocarbons, hydrogen cyanide, pesticides, toxic metals and radioactive substances. The health effects of breathing ETS include: • Increased risk of lung cancer • Increased risk of heart disease and stroke • Increased respiratory problems, especially for asthmatics • Eye irritation, coughing and headaches etc. As a complex chemical mixture, ETS does not have an occupational exposure standard. Suffice to say, breathing second-hand tobacco smoke increases the risk of cardiovascular disease, lung cancer and other respiratory illnesses and can worsen existing illnesses such as asthma and bronchitis. An interesting related scientific article published in BMC Public Health (2017) concluded that “there are no multiplicative interactions
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
GUEST COLUMN
BACK TO CONTENTS
GUEST COLUMN between tobacco smoking and occupational lung carcinogens (asbestos, crystalline silica and diesel engine exhaust emissions). It is also important to highlight that background radon and cigarette smoking have synergistic and multiplicative effect on lung cancer. Even though, specific programs should be developed and promoted to reduce concomitantly the exposure to occupational lung carcinogens and tobacco smoking”.
Department of Consumer and Employment Protection, Mines Safety Bulletin (2005), “the effects of such gas explosions can be severe. In South Africa, multiple fatalities involving 25 deaths over a 10-year period have occurred as the result of methane explosions in the gold mining industry. While there has been no recent loss of life in WA, fires, equipment damage and loss of production have resulted from methane intersections.”
Nevertheless, a much earlier study in 1957 concluded that in urban areas, heavily polluted with motor exhaust fumes and general urban air pollution, cigarette smokers’ incidence rate of lung cancer was fourfold higher than among smokers in rural areas.
Looking to localised occurrences we note the following extract from the Department of Mines Annual Report, WA, 1961: • “Three occurrences of methane were investigated during the year. All of these were in workings off the main shaft of North Kalgoorlie Ltd. In each case the gas was escaping from diamond drill holes which were collared on the 15, 17 and 18 levels. Flow from the holes was of short duration.”
This suggests that such high incidence of alarming respiratory hazard may be due to the combined and cumulative effects of urban pollution in conjunction with the chronic action of tobacco smoke. The NHMRC-sponsored research carried out recently at UWA highlighted that of the total cohort of 153,898 surface and underground miners, 54% of them were ever-smokers, indicating the heavy incidence of smokers employed in the industry. Hazard of smoking cigarettes in metal mines subject to unpredictable inflows of flammable gas Many unwanted gases are encountered in underground mines, be they combustible, toxic or asphyxiant types. These include methane (CH4), carbon monoxide (CO), oxides of nitrogen (NOx), hydrogen sulphide (H2S) and sulphur dioxide (SO2). Methane is most commonly associated with coal mining, but it is not unknown in metal mines. Whilst it isn’t common, it can and is encountered unexpectedly in metal mines, particularly when drilling intersects so-called methane gas bubbles. Such encounters have occurred at various underground mines in the Eastern Goldfields, as well as at surface exploratory drilling sites.
Another reference of note is contained in the above Mines Safety Bulletin: • “Although gas occurrences continue to be reported to Resources Safety, the inspectorate has become increasingly concerned about recent notifications that have resulted in fires and the burning of gases. • In one case, a flame about one metre high coming from the muck-pile was noticed during bogging operations in an underground development heading. In another case, a drill hole caught fire at the surface diamond drilling operation after methane was intersected. Flames were observed at the drill hole and extended to the top of the drill mast. The fire continued to
burn for about 24 hours. • A few years ago, flammable gas exploded in an underground stope void. The gas was believed to have built up in the unventilated stope prior to the incident (Significant Incident Report No. 85, October 1997). • It has been determined that certain mineralogy may indicate the presence of gases. As such, geological data should be reviewed to ascertain if the strata intersected have the potential to release gases.” Nowadays, gas monitors are located at all drill sites and are routinely used by shift-bosses as they carry out their supervisory tasks. Nevertheless, cigarette smoking is an unnecessary hazard in such dangerous environments.
Conclusions In view of the complexity of carcinogenic dusts and fumes that most hard rock underground mineworkers are exposed to, it is vitally important to inform them of these facts and for scientific researchers to investigate the synergistic and holistic health hazards of the polluted air breathed by most underground metal mineworkers on a regular basis. It is also time to acknowledge the unnecessary hazard created by underground metal mineworkers smoking cigarettes in environments subject to sudden, rare, but unannounced inflows of flammable gas from surrounding strata. Surely, therefore, it’s time to discontinue the current practice of underground metal miners being allowed to smoke cigarettes at worksites. – References on request
These occurrences can be particularly hazardous since methane, when mixed with air at concentrations between 5% and 15%, is explosive if a naked flame or high temperature sparks are present. Indeed, as pointed out in the MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 49
BACK TO CONTENTS
ARTS
Doctors hit the high notes COVID-19 has plunged theatres and concerts halls into the dark. The WA Doctors Orchestra switches on the light, writes Dr Jenny Fay. It’s out of the scrubs and masks, and into the orchestra! September 20 is the date for the ninth WA Doctors Orchestra Charity concert.
concert can go ahead. It will be one of the first orchestral concerts to be performed in Perth and, indeed, in Australia.
In what has a been such a challenging year for the medical fraternity, many of us turn to other platforms for respite from the sad and relentless issues presented by COVID-19.
This year the orchestra is bigger than ever. One suspects it’s because no one is away travelling for a change!
It has served as extra motivation for the doctors of the orchestra who are all excited that their planned
The orchestra performs every second year, for both wellbeing and pleasure, and for a nominated charity. This year the funds raised will go to Breast Cancer Care WA. This is an important local charity provides specialist breast care nursing, counselling and financial and practical support and care to all West Australians affected by breast cancer and their families. It is BCCWA’s 20th anniversary and the orchestra is especially happy to give it a financial boost
as many of its celebrations and fundraising activities have been set aside owing to the COVID event restrictions. That makes the WA Doctor’s Orchestra concert even more important and the orchestra is delighted to support them. Conductor Mark Coughlan will be at the helm for the fifth time and it is truly wonderful to have a masterful and engaging person out front. The program of Beethoven Symphony No. 7 and Rachmaninoff Piano Concerto No. 3 is sure to please. This year the soloist is UWA medical student, Alexander Chua. One wonders how he finds the time – he certainly has the talent. The concert starts at 2pm, Sunday, September 20, at St Hilda’s College (Joy Shepherd Performing Arts Centre). Tickets are $35 for adults, and $30 for concession card holders and school students.
For tickets... www.trybooking.com/BKWZG. Please come along and support. For more information contact Jenny Fay on 0407 599 188 or visit the Facebook page at @wadoctorsorchestra
50 | SEPTEMBER 2020
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
BACK TO CONTENTS
WINE REVIEW
Review by Dr Craig Drummond Master of Wine
Schild Estate – pure Barossa It is so pleasing that Schild Estate have entered their wines for the past four years for our tastings as they are consistently of high quality
vineyards are wonderful 150-year-old Shiraz and Grenache vines which are survivors of the catastrophic government-sponsored 1980s Vine Pull Scheme, initiated when grape prices plummeted due to oversupply. These dry-grown, deep-rooted, old-bush pruned vines give low yields resulting in concentrated juice that produce the most incredibly intense wines. The ‘jewel in the crown’ is the famous Moorooroo Block which produces Shiraz wines definitely for that most special occasion.
This Barossa Valley estate has been a family business since 1952 over which time they have amassed more than 160ha of vines across the cooler southern end of the valley, around the town of Lyndoch. Their cellar door is situated in the old ANZ bank in Lyndoch and is well worth a visit when that border finally opens. The family, now third generation, focuses predominantly on red wines – the Barossa’s forte. Amongst their
Schild Estate Barossa Valley Narrow Road Vineyard 2017 Small Batch Shiraz Cabernet (RRP $70) Another great wine! The marriage of Shiraz and Cabernet varieties must be uniquely Australian as I don’t recollect seeing it anywhere else in the world. This wine, as the name implies, is from a single site and produced in small quantity. The wine did not start well for me due to the traditionally styled capsule which I found difficult to remove as was the cork. However, the wine that followed was delightful. A sublime, supple, poised, balanced wine that just glides across the palate. Aromas of dark fruits and spice followed by smooth flavours of blackcurrant, black plum. Oak is so structurally integrated, the tannins so fine, smooth and velvety, the finish so clean and long. A 10-year wine.
Schild Estate Barossa Valley 2018 Shiraz (RRP $25) A very drinkable medium-bodied Shiraz. The nose is inviting with fruit, pepper and spice to the fore. Leads to a palate of dark plum, blueberry, a touch of clove and white pepper. Oak is subtle from ageing in the larger, seasoned hogshead barrels. Enjoyable now, but has a few more years.
'S EWER REVI
PICK
Schild Estate Barossa Valley 2018 Grenache Mouvedre Shiraz (RRP $25) This blend of three very complementary varieties, which originate from the Southern Rhone Valley, has become a highly recognised Barossa style. The focus is on retained fruit character with oak only in the background if there at all. This wine is dominated by the characters of Grenache with its beetroot red colour, confectioned and spicy nose, softness and rounded fruit flavours, and the warmth from alcohol 14.5%. A welcoming wine, easy drinking, showing blackberry and allspice, brambly, with savoury edges. Drinks well now, but will be enjoyable for a further few years.
Schild Estate Barossa Valley Ben Schild Reserve Single Vineyard 2017 Shiraz (RRP $36)
This is a step up the quality ladder. Vibrant deep ruby red in colour; aromas ethereal, spicy, complex, oaky, intense; flavours rich and concentrated with blackberry, black olive and menthol. It’s structural, yet mellow with ripe tannins, balanced acidity and integrating oak. A wonderful lingering fruity finish. Wow – a wine great now but has a 15 to 20-year journey ahead of it. Tuck some of this away in the cellar.
MEDICAL FORUM | RESPIR ATORY HEALTH ISSUE
SEPTEMBER 2020 | 51
You don’t buy a practice every week, but we do
It’s a big decision, Huge. For most, it’s a once in a lifetime proposition. We take this very seriously too. So much so, that over the last 25 years we’ve developed a process for medical professionals looking to go out on their own. But we don’t just look at you, we look at the business as a whole. We act as your partners in ensuring that it is a viable and profitable opportunity. We assess everything - location, competition, client-base and growth potential. Then, and only then, we tailor a loan to meet your needs. Forgive the pun, but we have a lot of practice when it comes to buying a practice. Visit us at boqspecialist.com.au or speak to your local finance specialist on 1300 131 141.
Car loans | Commercial property | Credit cards | Equipment finance | Fit-out finance | Foreign exchange | Home loans | Personal loans | Practice purchase | Practice set-up | Savings accounts | SMSF | Transaction accounts | Term deposits | Vehicle finance The issuer of these products and services is BOQ Specialist – a division of Bank of Queensland Limited ABN 32 009 656 740 AFSL no. 244616 (“BOQ Specialist”).