Wanted:











GPs earn a lot less than other medical specialists, yet their expected range of care for patients seems to be pushed wider by the day.
It should come as no surprise that bulk-billing rates in general practice have been in free-fall.
GPs have been sounding the alarm for years about the challenge of providing good primary care while keeping the lights on, but it’s been like background noise during the pandemic.
Now we have (another) attempt by government to sort the mess –optimistically called ‘strengthening’ Medicare – when perhaps ‘SOS’ might have been closer to the mark.
The newly-formed lobby group Primary Care Business Council, with seven member corporates, says bulk-billing rates for standard consultations have fallen from 74% in 2019 to 61%, and that’s set to continue heading south.
The RACGP recently offered some GPs 40 CPD points to “critically review” whether they should be bulk-billing patients and its outgoing president Professor Karen Price has actively urged colleagues to private bill wherever possible.

While the finger of blame has many targets, the flatlining of Medicare rebates is an obvious one. In the last MBS increase in July this year, the patient rebate for a standard level B consultation went up a meagre 65 cents – from $39.10 to $39.75.
GPs earn a lot less than other medical specialists, yet their expected range of care for patients seems to be pushed wider by the day.
This month Medical Forum gives the floor to some key players in primary care, with some offering candid insights and home-truths about what needs to be done.
There is no quick fix here, but many argue it’s now or never.
Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL
This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.
Q&A Australian Health Minister
Butler
Close-up: Professor Bruce Robinson
Kidney disease surge

Healthy urban design

Fair go for GPs
Cathy O’Leary
& Views
brief
Cover Story – Saving General Practice
Too precious to lose – Emeritus Professor Geoff Riley
that money won’t fix? – Dr Brenda Murrison
starts with medical school – Dr Nahal Maviddat
Pulse-raising passions
Car review: BMW i4 EV
Dr Mike Civil
Wine review: Knee Deep
Dr Louis Papaelias
system needs us – Dr Sean Stevens
clock is ticking – Learne Durrington
Enduring values
Dr Joe Kosterich


As we enjoy the first hints of spring, the lucky winner of our August doctors dozen from Nikola Wines is GP Dr Stuart Paterson from Ellen Health.
month, Dr Louis Papaelias shares his tasting notes on some epic whites and reds from Knee Deep Wines, with his review on page 66. For your chance to win a dozen bottles, go to www.mforum.com.au or use the QR code on this page.
Fonda Grapsas – Director


Tony Jones – Director tonyj@mforum.com.au






Editor
Cathy O'Leary

0430 322 066 editor@mforum.com.au
Production Editor
Jan Hallam

08 9203 5222 jan@mforum.com.au


Journalist
Eric Martin
08 9203 5222 eric@mforum.com.au


Clinical Editor

Dr Joe Kosterich

0417 998 697 joe@mforum.com.au
Marketing
Quinn Hampton quinn@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Andrew Bowyer
0424 883 071 andrew@mforum.com.au
Clinical Services Directory
Andrew Bowyer
08 9203 5222 andrew@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
It’s the million-dollar question when it comes to exercise – how much is best? Is it better to do a little every day, or a lot a few times a week?

Professor Ken Nosaka’s study has found that it is best to exercise daily, rather than do 2-3 intense sessions per week.
Professor Nosaka garnered a lot of attention earlier this year with his three-second weight training study, which found that lifting weights for as little as three seconds a day could have a positive impact on muscle strength.
In the latest study, three groups performed an arm resistance exercise and changes in muscle strength and muscle thickness were measured and compared.
Two groups performed 30 contractions a week, with one group doing six contractions a day for five days a week (6x5 group), while the other crammed all 30 into a single day, once a week (30x1 group).
Another group only performed six contractions one day a week.
After four weeks, the group doing 30 contractions in a single day did not show any increase in muscle strength, nor did the group doing six contractions once a week.
But the 6x5 group saw significant increases in muscle strength of more than 10%, with an increase in muscle thickness similar to the 30x1 group.
Professor Nosaka said the studies suggested very manageable amounts of exercise done regularly could have a real effect on people’s strength.
“People think they have to do a lengthy session of resistance training in the gym, but that’s not the case,” he said. “Just lowering a heavy dumbbell slowly once or six times a day is enough.”
Health researchers have renewed calls for more pill-testing facilities to avoid potential overdoses and drug-related deaths, as festivals return to Australia’s summer calendar after a two-year absence.
An Edith Cowan University study examined the behaviour of festival goers in Victoria when given access to a community-led pill testing service. It found the vast majority would discard their drugs if they contained unexpected substances.
Almost 11% of the pills tested didn’t have any of the substance the owner believed they had purchased. Of the people in possession of these pills, only 9% said they planned to consume the drug after finding out the composition.
Other pills were found to contain the expected substance, but also other unknown substances the attendees were unaware of. Less than half of these people said they still planned to take them.
Researcher Dr Stephen Bright said further analysis showed some of the discarded pills contained a dangerous combination of drugs that were known to have been involved in several deaths in Melbourne in 2017.
“When they were told there was a chance their drugs could be from the same batch, most people chose to get rid of them,” he said.
Doctors and other health practitioners are being urged to use a confidential hotline to report socalled “cosmetic surgery cowboys” who are practising unsafely.
Patients can also use the line –1300 261 041 – if they believe they have been harmed by cosmetic surgery procedures in Australia. The hotline has been set up by the newly established Cosmetic Surgery Enforcement Unit, as a response by Ahpra and the Medical Board of Australia to an independent review into the regulation of medical practitioners who perform cosmetic surgery.
It is aimed at making it less challenging for patients who are unsure about whether to report their experiences and where to report them. The hotline, which is staffed by a specialist team, makes it easier for practitioners to make notifications when they know about specific unsafe practices.
‘We want patients to use the hotline, as well as registered health practitioners, so their concerns can be investigated,” Ahpra CEO Martin Fletcher said. “When we know about poor behaviour and unsafe practice, we can act.”

A new alliance has been formed in WA to boost women’s health and research.
Funded by the National Women’s Health Research, Translation and Impact Network – an initiative of the Australian Health Research Alliance – the Women’s Health Research Alliance WA aims to leverage large-scale national efforts to improve women’s health and

focus
deliver research, translation and impact in priority areas.
These areas include preconception, pregnancy, postpartum and intrapartum health, reproductive health, sexual health, healthy lifestyle, nutrition and obesity prevention. They also cover violence and abuse prevention and recovery, Indigenous health, mental health, chronic disease prevention and healthy ageing.
Dr Jacqueline Frayne said the network was a great opportunity for a collaborative approach, including consumers, to research for women and girls nationally.

“My research interests include pregnancy care, chronic disease and mental health, with an emphasis on severe mental illnesses, chronic diseases including endometriosis, hypertension, diabetes and breast cancer and lifestyle risk reduction,” she said.
“As a general practitioner, I believe that aspects of women’s health research are lacking in the primary

More than 270 WA families have registered their relatives on the Safe & Found database in its first 12 months of operation, resulting in 29 rapid searches by police.
The database was developed by WA Police, in partnership with the MedicAlert Foundation, to help police quickly locate vulnerable people with dementia, autism or a cognitive impairment that increases their chances of going missing.
Having access to information such as ‘lost person behaviour’ or a recent photo of the missing person can make a significant difference to the early stages of a land search operation and improves the chances of finding the missing person.
In 2017, WA Police conducted 46 searches for people with dementia who had become lost. By 2020 that number increased to 73 searches and there were 170 searches last year. So far in 2022 there have been more than 143 searches, and this could reach as many as 200 searches by the end of the year.

Doctors are encouraged to make this service known to their patients. www.safeandfound.org.au
Dr Simon Towler has wound up his time as clinical lead for End-of-Life Care as he takes on his new role as WA Health’s Chief Medical Officer from mid-September.
Ear Science Institute Australia founding director Professor Marcus Atlas is the inaugural Chair of Translational Ear Science at Curtin University, while ESIA has appointed Rob Gordon as its board chair.

Psychiatrist Dr Roger Paterson has been awarded a meritorious service award by the Royal Australian and New Zealand College of Psychiatrists’ WA Branch at its annual conference. It recognises his many years of service as a leader in the field of ADHD.
Professor of paediatrics and cofounder of the ORIGINs project, Professor Desiree Silva, is the inaugural Director of Research at Joondalup Health Campus.
Perth Rotarian Ron Geary has been awarded the 2021 John Curtin Medal for his work to improve the health of children globally through polio vaccination clinics in India and plastic and reconstructive surgery in Fiji.
Arthritis and Osteoporosis WA Foundation and Edith Cowan University have signed a deal which will develop digital information to promote bone and joint health in young people, for use by educators and sporting groups.
As a practising emergency physician with a side interest in medico-legal work, I’ve seen many situations where poor discharge practices can leave doctors vulnerable to complaints and litigation.
Being discharged from hospital is generally an experience that patients and their doctors look forward to, but it’s not without risk. This is particularly so for patients discharged from the emergency department (ED) where the interaction has frequently been brief; the investigations limited; and the certainty around the diagnosis may be unclear.
Research suggests that fewer than 50 per cent of patients discharged from the ED with non-specific complaints will have a correct diagnosis at discharge.
Patients generally have faith in the diagnosis made in a hospital setting, and in the care provided. And doctors, particularly junior doctors, often feel compelled to come to a definite diagnosis prior to sending a patient home. Wanting to be right and wanting to do something are inherent traits in most doctors. It fits in with our high-achieving personalities and the desire to help. That’s why many of us studied medicine.
Having the confidence and maturity to acknowledge uncertainty is an important component of practising good medicine. When a patient is determined to be well enough to be discharged home but uncertainty remains about the diagnosis, it’s much safer if both the patient and the ongoing healthcare providers are aware of it. This makes it much more likely that the patient will seek review if their condition changes or doesn’t improve as expected. It also gives the outpatient healthcare provider (usually the GP) an awareness that further investigation, treatment or referral might be necessary.
Some simple steps can reduce the risk of serious misadventure after a patient leaves hospital, either from the ED or following an in-patient stay.
Make sure the patient knows with whom they should follow up, when they should follow up, and the purpose of the follow-up.
Whether there is diagnostic certainty or not, make sure the patient understands what you think is wrong with them and how certain you are about this. In my practice, if I’m unsure about the diagnosis, I tell the patient that I’m not exactly sure about the cause of their symptoms, but I’m reasonably
confident that all acute sinister causes have been excluded – but this means they do need to be alert for any change in their condition and seek review if necessary.
Make sure they understand any medications they have been prescribed including dosage, frequency, and possible side effects.
Step 3: Explain what you expect will happen
Again, this somewhat depends on your diagnostic certainty, but you should be able to provide a reasonable estimate of how their condition will progress. For instance, if you’ve diagnosed a community-acquired pneumonia and you’re discharging them on oral antibiotics, they should understand that it will be a few days before their symptoms improve significantly, but they shouldn’t get any worse.
Step 4: Tell them when to come back or get reviewed
This is probably the most important part of safe discharge planning. Give the patient both general and specific symptoms they should watch out for, and which of these should lead them back for further medical review. For instance, in the case of the pneumonia patient, general advice would include “come back if you feel too systemically unwell to manage at home due to poor oral intake, fatigue or pain”. But specifically, “come back immediately if your shortness of breath worsens, you have persistent vomiting, or you feel confused”.
Step 5: Write it all down Even with the best medical care and best discharge planning, things will sometimes go wrong. Your best defence is to document ALL of the above and to also provide the patient with written discharge advice. Make sure the GP (or appropriate ongoing provider) receives a copy of the discharge information.
Finally, keep the door open for the patient to come back. Regardless of how minimal their complaint may seem and how confident you are that there’s nothing serious going on, always encourage them to seek further review if they have any concerns.
A simple mnemonic to summarise safe discharge planning: Health literacy – does the patient understand the diagnosis?
Organise follow-up
Medications – make sure the patient understands the timing and dose of new medications, and the important side effects
E xpectations – what to do if symptoms get worse or are no better in the expected timeframe.
health care space, particularly. “I understand that research career advancement can be challenging for many women, and this is even more so during the COVID pandemic. Workplace interruptions can be hard, especially for clinicians.”
Dr Frayne said the alliance welcomed the involvement of people interested in women’s health research. https://wahtn. org/platforms/womens-healthresearch-alliance-wa-whrl/
In a first for public hospitals nationally, patients at Royal Perth Hospital can now obtain electronic prescriptions that can be dispensed at community pharmacies.
A joint project between RPH, WA Heath Support Services and the Australian Digital Health Agency, the service will be rolled out to all specialties at the hospital following an initial 12-week trial in haematology, immunology, anaesthesia, pain medicine, gastroenterology and liver outpatient clinics.
During the trial, registered prescribers can generate an electronic prescription when needed for their patients.
Patients will receive an SMS or email message with a token they
can either present in person or forward electronically to their local pharmacy to receive supply of their medicine.
While this is the first trial of electronic prescriptions in a metropolitan hospital setting, about 72 million electronic prescriptions have been issued across the country.
More than 45,000 prescribers –GPs and nurse practitioners – have issued e-prescriptions to patients and more than 98% of community pharmacies around the country are dispensing them.
A study has found that the Northern Territory has the worst economic outcomes for remote Indigenous people of any state or territory in Australia, by some margin.
The Centre for Independent Studies said that while the deprivation experienced by Indigenous people was well known, the statistics were issued as a single national category, obscuring the degrees of deprivation.
Author Peter Gregory analysed how States and territories performed in terms of the economic wellbeing of Indigenous people in remote and very remote communities and based on the data, South Australian ranked the best for economic outcomes, followed by Western Australia, then Queensland and New South Wales.
A study by Silverchain and Fiona Stanley Hospital, which aims to improve health outcomes for home-care patients, has attracted international recognition.
The study focused on patients with serious infections who receive intravenous antibiotics at home via outpatient parenteral antimicrobial therapy (OPAT). It identified risk factors that could contribute to these patients developing catheter-related thrombosis.
The study was named in the top 10 OPAT studies in 2021 in a recent journal article published by the Infectious Diseases Society of America
The project is expected to not only improve health outcomes of home-cared OPAT patients, but also reduce pressure on hospitals, with the OPAT home service freeing up about 25 beds a day at Fiona Stanley Hospital alone.

A University of Sydney study examining the climate impact of low value health-care activity in Australia has found that unnecessary vitamin D tests generated carbon emissions equivalent to a car driving from Sydney to Perth 59 times.
The researchers say unnecessary vitamin D tests in Australia cost the healthcare system over $87 million and had a carbon footprint of 28,000kg to 42,000kg of carbon dioxide equivalent emissions.
Health care has a significant carbon footprint: in 36 major countries it is responsible for 4% of annual global CO2e emissions. In Australia, health care represents 7% of national CO2e emissions.
Low value care represents about 30% of health care. It is defined as health services that have limited or no benefit to patients but carry risks or costs for patients and the health system.
Researchers said about 76% of Australia’s vitamin D tests provided no net health benefit, meaning there were 3.4 million unnecessary tests done in 2020.
Silverchain’s Hospital at the Home medical director Dr Leena Patel said the research would help reduce the risk of catheter-related thrombosis for these patients.
“Giving care to patients in their home in a ‘virtual ward’ setting is becoming more common, therefore it is increasingly important to ensure that this type of care provides patients with the best health outcomes,” she said.



After serving as Minister for Mental Health and Ageing in the Gillard Government a decade ago, Mark Butler now has the challenging health and aged care portfolios to sort in the Albanese Government.

Here he talks to Medical Forum about his top priority to reform Medicare, and fix primary care which he argues is “in worse shape than it’s been in the entire Medicare era.”
MF: Minister Butler, you have said primary health care is in crisis in Australia. What has got it to that point?
MB: What we’re seeing today is the unfortunate result of nine years of neglect. Primary care is in its worst shape since Medicare began. Across the country we hear stories of Australians not being able to get in to see a bulkbilling doctor or GPs changing from bulk billing to mixed billing. It’s never been harder or more expensive for Australians to see a GP.
The former government froze the Medicare rebate for six years, ripping billions of dollars out of primary care and causing gap fees to skyrocket.
MF: How will the outcome of the Strengthening Medicare Taskforce differ from the former government’s 10-Year Primary Health Care Plan and not become just another report?
MB: The Strengthening Medicare Taskforce is backed by genuine investment to support its work. It will provide recommendations to the government on the highest priority investments in primary care by the end of 2022.
We have committed to the $750 million Strengthening Medicare Fund from 2023-24 to to support the priorities identified by the taskforce and the government will respond to its recommendations in the 2023-24 Budget.
GPs don’t need headlines and a truckload of statistics to tell them what they live with everyday of their working lives – general practice is in a parlous, and some says perilous, state.
Despite a string of health ministers paying the timehonoured lip service that primary care, with GPs at the heart of it, are the cornerstone of our health system, they have presided over an ever-expanding bureaucracy while watching real-term Medicare rebates plummet, workforce recruitment and retention dive and bluntinstrument policy pit health professionals against each other.
While Minister Butler has thrown down the gauntlet to the newly appointed Strengthening Medicare Taskforce to find $750 million worth of solutions, Medical Forum
has asked some Western Australian GPs for their views on the challenges and solutions that will return general practice to the jewel in our health care crown. Read their views in the following pages.
We have also sent out a poll in our weekly digital newsletter. Some of those views are also published here.
There is no overnight solution to these systemic ills, but we want to continue to share your views that have been informed by experience and commitment. Email your comments to the editor, Cathy O’Leary, editor@mforum.com.au
– Jan HallamMF: Only about 15% of medical graduates are choosing general practice (in Western Australia, this has fallen from about 40% in the early 2000s). What can be done to make this career path more appealing?
MB: I have already brought together representatives from across Australia’s health workforce, including unions, employers and other stakeholders to discuss how best to grow and support this vital sector.
Over the next two months I will continue to meet with frontline health care workers, including students and those who have recently left their positions, to understand their issues and what governments can do better.
This work will inform and advise our new Health Workforce Taskforce as well as the Jobs and Skills Summit process.
The Government is working towards the transition of the Australian General Practice Training program to a college-led model by 1 February 2023. The transition will provide the GP colleges with direct responsibility for the delivery of training including marketing of the program. As part of the marketing and delivery of the program, the GP colleges will play a central role in making a career in general practice more attractive to junior doctors.
The Government is progressing a program of work to further support junior doctors to consider a career in general practice.
Significant incentives are also in place to support GPs and GP practices – such as the workforce incentive program. How these
are shaped and targeted is to be considered as part of the Strengthening Medicare Taskforce.
MF: Many GPs are finding it economically unviable to bulk bill their patients and patients are facing higher out-of-pocket costs. Can you ease financial pressure for both GPs and their patients?
MB: The Government has committed to new investments of more than $1 billion in general practice and primary care.
This includes:
• the $750m Strengthening Medicare Fund
• $220 million for Strengthening Medicare GP grants of up to $50,000 per practice (see below)
• $146 million in support of rural community access to primary care.
The Strengthening Medicare Taskforce is made up of a diverse group of health experts and consumer representatives who will provide practical advice to help us start fixing our health care and make it easier for Australians to see a doctor.
It will identify the best ways to boost affordability, improve access, and deliver better support for patients with ongoing and chronic illness.
MF: The government’s reforms to Medicare include $220 million for a GP grants program. How will that help practices in real terms?
MB: The $220 million Strengthening Medicare GP grants program will support general practices through one-off grants of up to $50,000 to:
• enhance digital health capability;
• upgrade infection prevention and control arrangements to ensure infectious respiratory disease (e.g. COVID, influenza) patients can be safely seen faceto-face; and/or
• support practices to maintain and/or achieve accreditation against the Royal Australian College of General Practitioners Standards for General Practice, under the General Practice Accreditation Scheme – to promote quality and safety in general practice.
Further detail is expected to be announced in the context of the October 2022 Budget.
MF: With almost half of Australians having at least one chronic health condition and needing continuity of care, does the current funding model for general practice need to change – i.e. moving to a blended funding model or an annual budget for a patient’s care from their GP?
MB: The Strengthening Medicare Taskforce is considering the sustainability of general practice and in that context possible changes to funding models to support quality of care and better outcomes for patients.
Emeritus Professor Geoff Riley has been clinician, academic and advocate for general practice for over five decades. He knows how much the system depends on primary care.

The estimable Professor Barbara Starfield, the former head of the Division of Health Policy at the Johns Hopkins University School of Hygiene and Public Health dedicated her career researching the impact of primary care on health services. She published three key findings:
1. Primary care improves equity, or ‘health security’, through reasonably local ‘access to high-quality medical care’. But access is not just geographical – critically the access concept includes affordability.
2. A health system with high quality medical primary care produces significantly better health outcomes for patients.
3. It saves the nation enormous money.
Starfield makes these observations in the context of the US health system, which is regarded as the worst in the developed world. The US system costs nearly twice the average cost of the other 38 OECD nations and produces among the worst health outcomes measured by standard indices of population health, including maternal mortality, infant mortality, obesity, life expectancy and suicide rates.

Hospitals, medical insurance and ‘Big Pharma’ are largely privatised, and public health is a small rump. Of course, the corporate owners of the health system have no interest in a universal health care system and probably pay a lot to maintain the status quo.
US doctors are as well trained as anywhere, and this includes their family physicians. However, a major
impediment to efficiency and effectiveness is the absence of gatekeeping.
This means that the health system loses the ‘efficiency dividend’ provided by an excellent family physician service, and patients forgo the key health benefits of primary care – bespoke service, with continuity of care.
‘The Commonwealth Fund’ is a US health think tank. In 2021 it published its most recent version of the ‘Mirror Mirror’ report, which summarised its conclusions as follows:
“The top-performing countries overall are Norway, the Netherlands and Australia. The United States ranks last overall, despite spending far more of its gross domestic product on health care. The US ranks last on access to care, administrative efficiency, equity, and health care outcomes, but second on measures of care process.”
So, the care is good! The doctors are fine, but only if you are wealthy. The problem is the system.
By comparison, at least in the major centres, the Chinese health system has very high-quality tertiary hospitals staffed by doctors who for several generations have trained in Western medicine.
China also has universal medical insurance to the tune of 70% of fees, with a range of safety nets and other supports for patients with chronic disease, disabilities and the like. What China lacks is a modern general practice. It knows this, understands the urgent
need, and is rapidly ramping up the training of Westernstyle general practitioners in the medical universities.
“When the dragon rises, it does so quickly,” but they know that it will take several generations before they can introduce universal gatekeeping. Meanwhile in its absence, hospitals in the more remote regions are assailed every morning by a crush of literally hundreds of patients, who arrive early at the ground floor and are eventually seen by very junior and poorly trained doctors. Perhaps some of the bigger centres may have a few specialists, but in the absence of triage, an elderly woman seeking advice regarding her shoulder pain may be seen by the ophthalmologist, while a young woman seeking contraception advice might find herself talking to an excellent orthopaedic surgeon.
The Australian Health System is routinely rated as one of the best in the world. Our specialists and general practitioners are among the best.
Gatekeeping is an unfortunate term, but it results in substantial efficiencies. According to the Australian Bureau of Statistics, GPs see about 82% of all new contacts in the health system and they manage the great majority locally without referral to secondary or tertiary services.
This process of filtration, local management and triage, ‘protects’ the expensive tertiary system from unnecessary Emergency

Department presentations, preventable admissions and outpatient appointments, and saves money by reducing overdiagnosis, overinvestigation and overtreatment. Our tertiary hospitals reap huge benefit from general practice through ‘gatekeeping’.
So why is general practice so efficient and effective?
It’s all about the personal and continuing relationship. Research has confirmed that being remembered, known, listened to, heard, believed, respected and properly responded to, are critical to patients.
This is not unique to general practice, I hear you say. And that’s correct. What is characteristic of general practice is a long-term, continuing relationship, resulting from earned trust and reinforced over sometimes years of contact.
G. Gayle Stephens, a doyen of US family medicine said that this relationship is characterised by “intimacy, mutuality, durability and born of the human need for other”. And he, like Michael Balint and legions of others observed that the relationship itself is therapeutic. Indeed Stephens explicitly recommended to family physicians “the emphatic use of the self as a therapeutic agent.”
Beyond that, General practice is characterised by:
• Generalism: comprehensive coverage of all ages, genders, cultures, diseases, organ systems, acuity and so on
• Early presentations of
undifferentiated illness
• Safety-oriented diagnostic reasoning, including a ‘rule out’ approach, probabilistic thinking and use of base rates and Bayes Theorem
• Particular awareness of the psychological and mind-body interaction, styles of helpseeking behaviour, illness and non-disease, and social determinants of suffering
• Holistic, (whole person), ‘known’, understood worldview and sources of meaning.
• Personalised, bespoke care
• A biographical approach. The remembered ‘backstory’ saves time and money
• Opportunistic and planned health maintenance and disease prevention
• Coordination of care, advocacy, (referral and return) and integration of care (multimorbidity) and chronic disease management
• Maintenance of the most comprehensive health record.
The list could go on.
So general practice is critical to successful health systems and works very well, but in Australia it is now in crisis. ‘Crisis’ has come to mean ‘pending catastrophe’, but its etymology is based in the simple idea of ‘decision point’. Both meanings are relevant here. It is time for proper funding of general practice.
It is simply unfathomable that successive Australian Governments, far from properly funding general practice have been stripping money
out of it for decades at the same time as pushing our system towards the failed US model. And it's also pertinent to note that the very existence of gatekeeping comes with a moral imperative to ensure that general practice services are viable and therefore accessible and affordable.
It's useful here to observe the parallels between teachers and GPs. Both largely comprise vocationally committed individuals doing very demanding front-line work with long hours, increasingly overburdened by bureaucratic administration, which significantly interferes with their core roles and their family demands.
Meanwhile, they’re feeling chronically underappreciated, undervalued and underpaid.
Clearly the last straw was the pandemic. Both groups are exhausted and disillusioned and, not surprisingly, both are leaving the professions in droves, creating an entirely predictable crisis.
Trainee teachers are walking away before they even complete their degree because they start to see what the future holds, and young medical graduates are not choosing careers in general practice for the same reason. Why would they?
Medicare rebates for general practice must be substantially increased. Now.

It is impossible to run GP in remote rural and povertystricken areas
Dr Brenda Murrison is a regional GP who has developed a network of practices throughout the southern regions of the state and in Perth.

Everyone will have an opinion on the reasons we have a crisis and many factors contribute to the reasons why, but the short answer is money – Medicare funding specifically.

Everyone knows that Medicare funding has not kept up with health inflation.

From 2010-19 health inflation was about 5% a year. State health, pharmacy funding and private health insurance all increased by about 5%. Medicare general practice funding increased by 0.5% by comparison.
Unsurprisingly, with so little money going into primary care, it has had a flow-on effect to recruitment and retention of GPs, specifically the number of registrars coming into the profession, which has nosedived from in excess of 50% or graduates a decade ago to less than 15% now.
Hospital wages have kept better pace with inflation so registrars in many cases need to take a pay cut to come to general practice, clearly this is not acceptable. By the time most registrars are heading into general practice they have other responsibilities to think about –cars, mortgages, student debt, weddings, partner, children and then the exam itself, which is an enormous expense particularly if you supplement this with the many expensive training courses around.
Just as well that general practice is the best career in the world!
I have no doubt that this was the case when I graduated and still is! Cradle-to-grave care offers variety,
flexibility and infinite opportunities – as wide as your imagination.
I think this is time of great hope and promise of change. Early 2023, for the first time in 20 years, RACGP will be taking training back in-house, not just for GP registrars but for the other training pathways that International Medical Graduates (IMGs) must travel to get their fellowship here.
What we need to do is not copy what has happened for the last 25 years. Registrars and IMGs must train where they feel comfortable and supported – they should not be forced by conscription to work in the most rural, regional and remote areas.
Asking people to give up all their support networks involuntarily to work remotely is not and has never been the answer. However, money is again the answer.
To ask registrars and IMGs to give up all the entitlements they have accumulated is not fair. I am referring to their annual leave, sick leave and long service leave.
A better system would be for the hospital to sub-contract the doctors-in-training to suitable general practices at the base rate that they were on in the hospital, much like the PGPPP worked in the past. The practices keep the money that was billed by the doctors, which will hopefully cover the cost of their wages, in most cases it would.
Solutions are not simple though, and the obvious flaw in this
scenario is what would happen to all those rural, regional and remote towns if we were to implement this?
Again, money is the answer. Medicare incentive payments need to be tiered depending on how remote the location is. The bulk billing incentive needs to be massively increased for the most remote locations. To be frank, if GPs feel appreciated and their skills rewarded by fair and equitable pay, they will return to these remote locations.
It’s not just a branding issue. General practitioners take a roasting from our specialist colleagues – you know who you are! GPs are not your interns, we are specialists based in the community who deal with literally everything and not one niche area. We need the support of our specialist colleagues – if there aren’t enough of us out there, who is going to refer to you? Or who will keep the hoards away from hospital?
But it is not just specialists’ support we need right now. We need to protect ourselves from the insidious creep of other professionals into the general practice space.
There is some sense to the argument that other people can do parts of our job description. Pharmacists, physiotherapists, nurses, paramedics, dietitians, the list could go on but none of them
has done the training that specialist GPs have done.
Let me be clear on this, I do think that everyone should work to the full ability of their scope, but it needs to be done in a coordinated way, ideally through multidisciplinary teams based in general practice.
But first we need to save general practice as a business and this is another complex issue.
General practice business viability has eroded as the rebates have stagnated to the point that many practices are not viable, particularly vulnerable are the smaller practices. The costs of running a business are so high that you really need six to seven GPs working together as a minimum to be viable or accept, that as an owner, you will likely take home a smaller percentage than the contract doctors who work for you.
The only exception to that is to
become procedural, which is no doubt why so many GPs do so much skin or cosmetic work to supplement their revenues. On top of that, practice owners have to worry about pay roll tax (6% in WA) and the threat of our contractors being reclassified as employees with a tax debt going back seven years. We are dependent on pathology incomes to remain viable, yet this is also under attack by the so-called Red Book pathology.
But I do strongly feel that hope is on the horizon.
We again have an opportunity right now in the Strengthening Medicare Taskforce, which is reviewing everything. I hope that they come to the obvious conclusion, feefor-service has given Australia the reputation of being one of the best health care systems in the world. Our system has been admired by everyone.
Investing in primary care by
normalising the Medicare rebates to where they should be and augmenting with patient registration – continuity of care should not be fragmented any more than it already is – and tiering Medicare rebates for rural and regional Australia would fix our problems of recruitment and retention and would have the welcome side effect of reducing pressure on our already stretched, expensive tertiary care services.
Common sense solutions? Too simplistic? Maybe, but we need to start somewhere and too many people are far too happy to criticise without any giving solutions.
Invest in Primary Care! The obvious solution.
More responses from the poll in our weekly newsletter.
Q If you are considering leaving general practice, what would make you stay?

Nothing that I can see happening. I’m off soon Anything to make the job easier – as my patients have aged, my work has become increasingly complex, and every day is a slog Love for medicine and helping patients
Access to salaried employment with paid leave benefits and super I am a solo GP and have not had a holiday longer than two weeks in 38 years. This year I have only been able to take a three-day holiday
Q What is a key long-term solution for the health system’s current woes?
Increased rebates for GP urgent care and better funding for coordinating care Halve the bulk-billing rate BUT double it for patients who are registered with a practice Start by engaging GPs in government policy decision making. We know how to make the system work better for patients, providers and government. Ask us how Show that GPs are really valued for their skills and not treat them like referral makers and sickness certificate fillers. Encourage our specialist colleagues to see their own GPs to understand what we do instead of self-referral after a corridor consultation with another specialist
I earn more money as a hospital registrar than
I do as a specialist GP. Start there
Combining state and federal health to create a national service
Associate Professor Nahal Mavaddat is UWA’s Head of Discipline of General Practice and offers a medical school perspective.

General practice is in a crisis in Australia.
We are suffering a major shortage of general practitioners, especially in outer urban and rural areas. Our emergency departments and hospitals are not coping, in part due to lack of access to timely community care for patients. Many Australian GPs are considering leaving clinical practice or retiring altogether. Many of those who remain report significant burnout. GPs feel overworked but underrecognised despite their recent herculean efforts in the face of the COVID-19 pandemic.
What is a worrying prospect for the future of health care, though, is not only that GPs are leaving but that they are not being replaced, with only 15% of medical students across Australia currently choosing general practice as a specialty.
Discussions about bulk billing and remuneration for GPs are important. As an example, for the same time spent with a patient, mental health care provided by a GP is remunerated by Medicare at only one third of the fee for a psychiatrist.
While choice of specialty by a medical student may not be based solely on potential future salary, financial remuneration does play a role in student decisions about specialty training. Disparity of income between specialists and general practitioners, who typically spend a similar time in disciplinespecific training, strongly signals a disparity in professional status, with the assumption that higher pay equates to greater knowledge and value of contribution.
It is frequently assumed that specialisation requires greater intellectual skill and academic prowess and that medical students
who are not smart enough to enter the specialties choose general practice. This is a fallacy not supported by assessment of academic or junior medical officer workbased performance.
General practice attracts some of the smartest and most well-rounded students. Nevertheless, some of the best may reject general practice due to seeing it as a less competitive and intellectually stimulating career choice. (Manski-Nankervis et al. 2020).
The Australian Medical Schools Outcomes Database (MSOD) 2021 is often quoted as reporting intellectual content as one of the most important to medical student speciality choice.

In a UK study published earlier this year in BMC Medical Education, (Misky, et al.), studying perspectives of medical students, found they associated specialists with ‘broader influence’ and ‘academic work’, while generalists were assigned ‘lower prestige’, as ‘gatekeepers’ with a ‘lack of academic opportunities’ and if conducting research only doing so “if they had the time” and “without remuneration”.
Such perspectives are frequently reinforced within our own health care system. Many specialists reflect that they could never do the challenging daily work of a GP, yet the medical contribution of GPs is often minimised, with errors or omissions by GPs frequently being the only times medical students hear about GPs during their hospital rotations.

The low ratio of professors and higher-level academics within general practice compared to specialist departments at Australian
universities is also telling. The academic GP workforce is ageing in Australia with a number of professors of general practice across the country having recently retired or taken redundancy without being replaced.
A loss of research-informed GP leadership within strong GP academic departments conveys to medical students that general practice “lacks rigour” (HODS Report 2021) and is not one to be chosen by those looking for an intellectually stimulating career.
So, what can medical schools do in this crisis to raise the status of general practice in the eyes of students?
Firstly, all medical schools must recognise their role in moderating health care workforce issues through perspectives acquired by students during their undergraduate medical training and act to address these.
In the case of promoting general practice, active steps to include GP teaching early in the curriculum, improving the quality of this teaching and role-modelling of good practice have all been identified as important to student choice of general practice as a future career and should be supported.
Thankfully, through the efforts of excellent teachers and GP preceptors at UWA, GP teaching comes early in the curriculum, includes opportunities for mentorship and pre-internship experience, and is highly valued by students.
Further, medical schools should take steps to value the discipline of
general practice and demonstrate this through example. A “zerotolerance approach to denigration of any specialty” by those involved in teaching medical students has been espoused. (Carlin 2021). This should not only be enforced in all teaching settings – formal or informal – but the merits of general practice highlighted whenever opportunities arise. Attempts should also be made by medical schools to strengthen GP academic departments, bringing these in line with larger specialist research departments, thus allowing medical students to view general practice no differently to any other specialty in terms of intellectual content and opportunities for academic progression.
Specialist medical knowledge and skills have meant that our sickest receive the best medical care that scientific advancements and technology can offer. However, this achievement is not reflected in the overall health of our population. Chronic diseases, including obesity-related illnesses, and an ageing population with multiple comorbidities continue to ravage the Australian population.
Solutions to these pervasive healthcare problems require new models of care. Item and fee-forprocedure-based remuneration, with an overreliance on sub-speciality treatments, have contributed to the US becoming the most expensive health care system in the world without evidence of world-leading outcomes.
Analysis of cost-effectiveness and value in health care suggests the essential role primary care must serve, highlighting it as the best place to invest financially to produce better and more equitable health outcomes.
Proposed models must also support a radically different approach to the management of chronic disease. This cannot be achieved by sixminute “one appointment, one problem” medicine. Universities and medical schools have a role in proposing such models and evaluating them.
However, the real contribution of medical schools in addressing the current health-care crises at a fundamental level may not lie in endorsing any particular model of care, but rather in promoting generalism within medical school
curricula as an engaging and intellectually stimulating academic discipline in its own right, with its own methodologies and applications.
The world outside medicine has already acknowledged that we may have swung too far in the direction of specialisation and reductionist approaches to the solution of complex problems and is supporting a return to generalist knowledge, looking at the wider picture and of systems thinking – that is understanding the relationships between parts.

In the context of health, this means more than simply knowing the factors that impact on health and disease, but rather knowing how they interact. Medical sciences though “remain largely taught according to a specialist-based, compartmentalised approach”. (Fleming et al. 2017).
When generalism is valued and taught during training, and matched in the clinical environment with appropriate remuneration for the significant intellectual contribution made to patient welfare, we may see more choosing general practice.
References on request
We don’t yet know everything about the link between physical and mental health. But with our evidence based approach, we’re constantly reviewing new evidence to inform our treatment of those people injured at work.

A systematic review conducted by the British Journal of Sports Medicine considered if physical activity could protect against depression and found that physical activity was associated with lower odds of subclinical depressive symptoms.
We believe that exercise is vital in assisting those with mental stress or ill health. Even those suffering a physical injury because of a work accident can find their mental health affected by their injury and the rehabilitation process. A prescriptive exercise treatment designed to increase work capacity and self motivation can increase the likelihood of a return to work, or normal daily life.

Our mobile, community-based model means we can see your patients

their home, local gym
park,
patients under compensable
even the

 BY RYDGES
BY RYDGES
Health West


I’ve been in general practice for 25 years. Throughout that time, we have repeatedly been “at the crossroads” and “in crisis”, yet somehow we always seem to pull through.
In the 1970 and ’80s, the Labor party was going to nationalise medicine with this draconian beast called Medicare. Vocational registration was introduced enforcing “unreasonable and unpaid” requirements on the profession. In the ’90s, accreditation of practices was another “unnecessary layer of bureaucracy”, and compulsory GP training was “unnecessary and unreasonable”, the rapid corporatisation in the late ’90s and early 2000s was going to “destroy the fabric of general practice forever”, and I could go on.
Today we face increased subspecialisation of our medical colleagues; scope creep from allied health, inadequate indexation of Medicare rebates, increasing chronic disease, the COVID pandemic and dwindling numbers of doctors entering our profession.
I am, however, supremely confident we are up to the task, just as we were in the past.
We are the cornerstone of the medical system, ensuring that our patients are seen, treated and appropriately triaged. Unlike America, patients can’t refer themselves off to an ENT for tonsillitis and end up with an MRI,
serum rhubarb and a tonsillectomy!
General practice is the most efficient part of the health system, and, despite taking us for granted, the Federal Government knows it, and we shouldn’t forget that.
So, how would I suggest that we save general practice?
I think the first thing we need to do is break the reliance on bulk billing. There’s one thing I can guarantee –the Government will NEVER reindex the lost Medicare Freeze, and it will continue to index Medicare well below inflation.
I think of it like counselling our patients. You can’t make the other person change, you can only change your own behaviour. The RACGP and AMA will not get traction on these issues while the rates of bulk billing are so high.
Next, I would encourage more junior doctors into a career in general practice.
I think GP is the best job in the world, and we just sell it poorly. If we look at the determinates of a happy life, general practice has them in spades – family relationships, work fulfilment, community and friends, leisure time.
Yes, our procedural colleagues will earn more, but they suffer much higher rates of divorce and burnout and have much less time for
community, friends and leisure time.
I don’t think another advertising program is going to solve this issue. The key is providing exposure in the pre-vocational years to highquality mentors and practices who have a positive outlook on the profession. These attachments will show junior doctors what we do before they get polluted by the jaundiced view that pervades some areas of the tertiary system.
Concerning scope creep, I think having more GPs will help provide the services that allied health are seeking to take from us. I also believe we must stick to our argument of patient safety first.
The view that treating a UTI, for example, is a simple intervention that doesn’t need a GP is erroneous. Only GPs can screen for other illnesses, conduct preventative health, order the appropriate investigations and follow the patient up.



I completely agree with my colleagues that we are facing some strong headwinds, but I do not believe they are any worse than they have been in past times.
We, in general practice, remain the cornerstone of the health system, and while we do have some work to do, I still believe we have the best job in the world.
Recent media headlines reflect increasing concern over the vulnerable state of primary care, causing too many patients to either fall through the cracks or inappropriately present at emergency departments. These patients have chronic and complex care needs which can be well managed in a thriving primary care setting.

A perfect storm is brewing, with more medical graduates rejecting general practice as a career option – for every new GP there are 10

new non-GP medical specialists – and a projected GP workforce shortfall of 11,000 by 2032, representing almost 30% of the GP workforce.
Equally concerning is the rapidly declining bulk billing rate in general practice, as more and more practices find this financial model untenable against a backdrop of increasing chronic disease and relentless cost of living pressures, which are hitting those who need

access to primary care the hardest.
The skills of many health professionals are not being used, funding models do not encourage general practice outreach and nor do they reward multidisciplinary care.
During a recent conversation I had with health economist Dr Stephen Duckett, he reflected that while the world has changed since Medicare was introduced in 1984, primary care
Treatment-resistant depression clinic:
a. CBT and DBT treatment
b. rTMS powered by Modalis
c. Esketamine approved site.
First responders’ clinics: DVA/ADF
Drug and Alcohol Support Network: In liaison with Cockburn Wellbeing providing home detox and ongoing support.

ADHD Clinic: Assessment and Pharmacotherapy, OnTrac ADHD Groups and 1:1 session
Australian disability support services: One-stop-shop for psycho-social disabilities.
We are looking forward to extending our model of care for: Child and Adolescent clinics • Memory Clinic • Complex, neurodiverse development clinics • Civil Forensic Psychiatry • Rural and remote psychiatric clinics
Work in your area of interest, closer to home, great financial incentives for private practice starters in competitively priced rooms. Consortium arrangement for established practices.
The clinical governance model of all essential practice policies and procedures to help reduce private practice risks and complexities.
In-house peer review, great referral base, cloud-based software, marketing campaigns and multiple other benefits. Neurologists, behavioural pediatricians and geriatricians are welcome to invite.
Locations: Cockburn, Como, Rockingham, Mandurah
To express interest, or have a friendly chat please email tajsingh@murdochpsychiatry.org or call 0434 252 672
MURDOCH PSYCHIATRY is looking for multiple psychiatrists to join our, dynamic MDT team of psychiatrists, nurses, TMS clinicians, registrar psychologists, and occupational therapists.
professional psychiatry services provide accessible and innovative evidence-based care at locations across southern Perth.
It’s
for Medicare reform, says WA Primary Health Alliance CEO and Strengthening Medicare Taskforce member Learne Durrington
funding, governance arrangements, and systems have not.
The Australian Government’s recently established Strengthening Medicare Taskforce clearly has its work cut out to identify the highest priority reforms, referencing the Primary Health Care 10 Year Plan by the year end.
A strong signal of the government’s commitment is the leadership of Minister for Health and Aged Care Mark Butler at each meeting, and, reading the room of health leaders
representing a cross section of primary care perspectives, there is a spirit of optimism, partnership and collaboration.
Taskforce members recognise and respect the challenges of demarcated spaces and have a genuine intent to work through these in the interests of improving equity and access, and better supporting people with chronic and complex health conditions.
While my appointment to the taskforce is as an individual, I will represent the national Primary Health Network program. I also have an ear to the ground within WA thanks to a GP advisory panel, a joint initiative of WAPHA, Rural Health West and the RACGP WA, and various community reference groups.
Prior to the first taskforce meeting, members were asked to articulate their vision for the primary care system in the future. I am hopeful that we can continue to strive towards an integrated, co-ordinated primary health care system that delivers high quality patient-centred care with leaders across the health system united in
Tattoo-free radiation therapy now available at GenesisCare, Wembley
GenesisCare, Wembley offers the latest stereotactic treatments with the implementation of the Versa HD Linac and CRAD (surface-guided RT) technology.
Tattoo-free radiation therapy - eliminating the emotional impact of permanent marks on patients’ skin.

With a holistic approach to cancer care, GenesisCare, Wembley offers extensive support services:

Exercise clinic
Allied health
Accommodation packages
Onsite parking
For more information, please contact our team and GenesisCare: 24 Salvado Road, Wembley WA 6014 Tel: (08) 6318 2868
genesiscare.com
the pursuit of the Quintuple Aim – best possible health outcomes, best use of resources, workforce experience, patient experience, equity and accessibility.
We cannot take a one-size-fitsall approach to general practice funding, business models and models of care. It is equally important to have variety and status for GPs (working to top of scope) to redefine it as a profession of choice.
New business models shouldn’t result in over or underservicing and data must be used to demonstrate the value of primary care against the Quintuple Aim.
Taskforce recommendations for changes to primary care must be actionable and sustainable, with $750 million on the table to turn the proposals into concrete actions for a person-centred primary care system.
Dr Bruce Robinson is a doctor, researcher and leader who staunchly believes in seeking to make a difference in the lives of others – including fathers. He knows that if dads do a good job with their kids, the world will be better off.
 By Ara Jansen
By Ara Jansen
Dr Bruce Robinson is involved in so many professional projects, one look at his email signature is dizzying.
The lung specialist with nine sets of letters after his name is a Professor of Medicine at UWA, a respiratory physician at Sir Charles Gairdner Hospital and a senior investigator at the National Centre for Asbestos Related Diseases. He’s also the Director of the Early Digital and Drug Intervention for COVID-19 Program and has been a regular volunteer doctor in natural disaster zones.
Somehow the list feels a little inadequate for all the work he has done, but what is clearly important is a deep sense of responsibility to make the world a better place.
“When you look at all the things I do at once, it looks like a lot,” says Bruce. “It makes me sound better than I am. In any case it’s not just me, there’s always a team of wonderful people working alongside me. But it is also true to say that I often hit a wall and run out of steam. I’m not an energiser bunny. My operating principle is that if I think I can make a difference, I go for it. If I can’t, I don’t do it.
“I push on through the inevitable tiredness, disappointment and disillusionment that occurs when you do those sorts of things. If the opportunity to make a difference is great, I push on, helped by the encouraging people around me – I get carried along by their enthusiasm.”
Any opportunity to make a difference, he says, is a like a coin – the flipside is the responsibility to stick with things and see them through. They go hand in hand.
On the lengthy list of achievements, perhaps the work which speaks best to his heart is The Fathering Project, which he founded in 2013 and has now become a successful national organisation with a footprint in many cities and regions around Australia.
Bruce is joined on the board by notable Perth locals including co-founder of the Margaret River Chocolate Factory Martin Black, former federal MP Tim Hammond, businessman Craig Heatley (PwC) and a number of corporate leaders in the eastern states, including chairman Geoff Lloyd.
The aim of the project is to help men understand just how important their role as a father is, and to promote positive and healthy relationships between fathers and children. Its mission is to educate, connect and empower fathers and father figures to prevent long-term social, emotional and cognitive difficulties and create the conditions for children to thrive.
Schools, workplaces and communities across the country now use its prevention and intervention programs.
The Fathering Project was a joyful accident which came out of Bruce’s medical work almost two decades ago.
“As a lung specialist, I have to break the bad news to people who are going to die. I also take the journey with them and help them along the way. One of the biggest regrets I heard from men was not spending enough time with their kids and that they couldn’t get that time back again.”
In response, Bruce wrote a book called Fathering from the Fast Lane in 2001. It offered practical ideas for busy dads around how to
rearrange their lives so they could do meaningful things with their kids and how to make the best use of their limited time.
“I didn’t think much more about it, but it turned into a bestseller and now we have this organisation which is active in hundreds of schools, workplaces and community groups and a social media reach of over one million.”
Lots of this work continues to be done through local schools – many of them have their own Facebook pages and sections on the school website for information and also on how to join the school’s dads’ group.
“The Fathering Project has been dubbed by a former deputy Prime Minister as ‘the most powerful force in Australia at the moment to change the future of our kids’. When you examine the data and talk to experts about crime, teen depression, bullying or drug and alcohol abuse, while it doesn’t guarantee to protect kids completely, a good dad is the most powerful missing force to reduce these risks in kids.”
Bruce says the statistics tell us that if children have a good relationship with their fathers, there would be a 50% reduction in drug and alcohol abuse, 30% reduction in teen depression and suicide and a 95% reduction in crime.
“Dads can help teach their kids integrity and respect for others and

help kids feel that they are worthy. They also demonstrate those values in how they treat their mum.”
Despite being so busy, Bruce has always had a life outside of medicine. Football has been a large part of his life starting at Bassendean, then the University Football Club, where he is a life member. From player to coach and mentor, among other things he’s co-patron of the Swan Districts Football Club and is active in their community programs for at-risk children.
“I’ve always competed or watched AFL. It’s a big part of my life. I love it and it has taught me a lot about life, leadership, teamwork and how to handle disappointment and defeat.”
His life as a “hard-nosed, analytical scientist” has existed, since university days, alongside a journey of faith. As a Christian he sees life not as a freeway but a meandering route through hills and valleys, always offering an opportunity to learn, change and grow, no matter what your age. At 72, Bruce says he’s surprised that he’s still capable of enormous personal growth.
When he was a young doctor, his faith caused him to recalibrate his definition of success. His measure of success was not academic, financial, nor by validation, but by whether or not he had made a difference with the opportunities and abilities he had been given.
We have a social and moral responsibility, he says, to use our hearts and minds to solve problems, like cures for certain types of cancer such as asbestos-induced cancer and share those treatments the world.
Bruce is married with three adult children (and a healthy clutch of grandchildren). His work with The Fathering Project taught him a few lessons to take home and apply as a dad and a now-granddad.
“I have always invested in family. It’s the most important part of my life – by far. My heart still skips a beat when I see the kids walking up our garden path. Occasionally I lost sight of that and had gotten too sucked in by work. Fortunately, I had influences in life which allowed for rapid course-correction. My big






lesson has been one of balance and investment – in being there for them, loving them independent of performance and helping each child appreciate just how special and unique they are.
“As a father I wish I had done some things differently,” he admits. “I would get too focused on what I was doing and lost the capacity at times to focus on my kids and wife. The Fathering Project helped me and has been a source of continual reflection.
“I got a good early kick in the bum about this when my oldest son was just two-years old. I was working in the US and I heard a speaker talk about fathering, not expecting much. But I was rivetted. He was talking good, logical sense, offering useful strategies. I became a better dad from then on, for which I am grateful.
“That experience also caused me to reflect on my own dad, who had some drinking issues, was a chain smoker and experienced severe mid-life depression. But he was also a good dad. He spent time with us and was happy to have man-to-man discussions with my brother and I about things like sex and respect for women.
“Despite his working-class background and personal problems, he loved his kids and worked hard to be a good dad. I was grateful to have him rather than an absent or distant dad.”
After his father died of a heart attack aged 66, Bruce found the letter he had written to him telling him what a good dad he had been. He was brought to tears to see it had been obviously read many times, despite his dad ever mentioning it.
Alongside numerous prestigious medical and research awards, in 2013 Bruce was named Western Australian of the Year and received an Order of Australia for his service to community. The next year he was the WA finalist for Australian of the Year.

While he’s thankful for all the awards he’s received, they don’t matter as
much as the things he does to try to make a difference.
“Authenticity is important to me. When I talk to groups or media, I don’t think about how I want them to see me, but I speak from the heart, letting the chips fall where they may. I just try to be honest and say what I really feel.”
Bruce has noticed that many of the people he meets, including doctors who look successful from the outside, are living hollow lives – they look like chocolate on the outside but inside they are hollow. Instead, he says we should seek what he calls a “Caramello life” – it’s chocolate on the outside but inside there is a rich golden core.
That rich golden core might include honest, close, caring relationships with partners, kids and friends, sacrificial service to those in need and attention to personal wellbeing. This includes health and genuine self-awareness.
“It’s easy to get trapped by overwork in medicine because it attracts people with good hearts and causes so many people to react to challenges out of kindness. It’s our biggest strength. We also have the temptation of making money or getting recognition for our medical work, leadership or research.
“The question remains, if you are working long hours, what are you losing out on? Is it quality and quantity time with your kids?”
Over the years Bruce has travelled to some 40 countries for work, holidays and humanitarian reasons but he’s grateful to have been born and living in WA. His recent

camping trip into the North West further entrenched his love for the state.
“It’s a beautiful place and a great place to raise kids. When I finished my doctorate in Washington, I was offered jobs in the US and UK, but we came back here to raise our kids. I’m very grateful for the opportunities I’ve had here.”
Born and raised in the then factory suburb of Bassendean, Bruce has friends dating back 65 years and they still get together regularly. He describes his childhood as a Tom Sawyer experience – very free: hanging out with those friends, riding bikes, playing in the river, getting into trouble and exploring their neighbourhood bushland.
“I think that growing up in a working-class environment has helped me a lot when talking to dads. I’m comfortable talking to anyone, including blue collar workers, because I grew up similarly to them. Most people find that talking to a room full of men is tough, but I love it.
“I’m not a natural but I spent so much time as a football coach that I learnt how to do it. I can now eyeball them and know how their brains work. I feel comfortable doing that.”
Bruce’s ancestors were Swan River colony pioneers and he believes Western Australia is and can continue to be a state of the sort of wild audaciousness that saw the pioneers, as well as modern refugees, get on boats and courageously seek a new life. He says this entrepreneurial attitude will not only help generate new, big ideas in medical research, which can take us beyond the resources boom, but also in the arts, science, engineering and technology.
“WA can be a hub for an audacious future, not just be an outpost. For example, in my field of medical research, we want to discover new things and become the hub for treatments and research that flow from them. People would come here because WA has bold ideas, courageous funders, dedicated talented people and are succeeding.”

What are the options for chronic kidney disease sufferers and what does the future hold?
Suzanne Harrison speaks with those at the coalface.
On Christmas Day 1996, Shaun Johnson was admitted to hospital with severe stomach pain. Doctors immediately suspected it was kidney stones. Fit, young and a new father, they were surprised to learn this was not the case.
In fact, Shaun’s kidneys were functioning at only 10% and his life would never be the same again, a story sadly familiar to many more people now than ever before.
Kidney disease in Australia – and the world over – is becoming more prevalent, affecting 1.7 million Australians, while a staggering 1.5 million are not even aware they have it, according to Kidney Health Australia (KHA).

One in three Australians are at increased risk of kidney disease, with factors including diabetes, high blood pressure, smoking, obesity, family history, being over the age of 60 (or over the age of 30 if you are of Aboriginal or Torres Strait Islander origin) and have a previous acute kidney injury or history of heart problems.
Shaun is far from being a typical chronic kidney disease (CKD) candidate. He worked a physical job and was a keen footballer, wasn’t overweight and didn’t smoke. However, he and his wife Michelle were soon told he had “the bad sh** luck disease”, as Shaun now calls it, more formally known as glomerulonephritis, an inflammation and damage to the glomerulus, the filtering part of the kidneys
As a teenager, Shaun’s father suffered from bowel cancer, so at that time, doctors testing his vitals found he had high blood pressure. At the time, Shaun was young and healthy, and doctors were more interested in his bowel health. Glomerulonephritis isn’t common, so it went unnoticed.
“It’s not hereditary,” Shaun told Medical Forum, nursing a coffee with Michelle and a picture of good health at the age of 54. He is doing well with a second successful kidney transplant and runs WA-based social and support group Dialysis and Renal Transplant (DART).
“So, it came as a shock. I realised I’d been operating on only about 10% kidney function since I was probably 15.”
Advised he would need dialysis within two months, Shaun decided first on a dramatic shift in his diet, moving to
very low protein for two years before starting hospital-based dialysis, despite his doctor’s protestations. Shaun and Michelle held the view this better prepared his body for what was to come.
Twenty-six years later, Shaun recalls an often-arduous journey – being sacked by his employers when they learned of his condition (and taking them to arbitration for unfair dismissal), forced to then take work as a cleaner and, later, retraining as a truck driver while undergoing thrice-weekly haemodialysis in hospital. There were skin cancers – of which he has a greater risk due to transplant medication – overwhelming tiredness and, when they travelled interstate to watch their then teenage son compete in tennis competitions, the cost of dialysis on the move. But still, Shaun is one of the luckier ones.
“Right now, I have a bit of brain fog and the drugs can be frustrating, but I don’t even think about it (since his most recent transplant in 2019),” he said. “Michelle and I have been together for 30 years, and she has looked after me for 26 of them. It’s hard on the partner. With kidney disease, you need that support. I couldn’t have done it without her.”
In Shaun’s case, alongside millions of others, by the time he was diagnosed
with CKD, it was too advanced to stop its progression. Kidney Health Australia says a person can lose 90% of kidney function without experiencing any visible symptoms, so early detection is paramount.
“Kidney disease is a silent killer,” according to Dr Hemant Kulkarni, a renal physician with Wexford Medical Centre in Murdoch. “Once a patient presents with symptoms, you have a problem,” he said. “Then, you’re either on the wait list for a transplant and are on dialysis, or you withdraw from dialysis and accept that is it. It’s not a ‘sexy’ disease and in the news, this doesn’t get a lot of attention.”

The number of Australians waiting for a kidney transplant is 13 times higher than the number waiting for a lung and 19 times higher than the number of individuals waiting for a heart transplant, according to KHA.
There are also differences of opinion on dialysis, joining the ever-present problem of geographical challenges for those in remote communities.
As of December 31, 2018, there were 13,399 people with end-stage kidney disease on dialysis treatment in Australia, with centre-based haemodialysis as the predominant therapy at 75%, and home-based
at 25% (30% of those are on haemodialysis and 70% on home peritoneal dialysis). Dr Kulkarni says that in WA, about 1000 people are on dialysis and only about 250 of those undergo home treatment.
“There is a shortage of beds for dialysis in WA,” Dr Kulkarni said, another issue for kidney patients, which he argues needs be radically addressed.

Yet more home-based dialysis may not be an easy solution. St John of God Health Care nephrologist Dr Kevin Warr said these numbers had stalled for a reason. To treat yourself at home, you must have a minimum level of ability to self-care and be supported, and for much older patients, this isn’t always possible.
“When we were dialysing predominately 60- to 70-year-olds that wasn’t a problem (but) now we are dialysing 80- to 90-year-olds and even 90-plus, so self-care becomes a significant issue,” Dr Warr said.
He believes it’s easier to choose satellite haemodialysis in dedicated
centres or hospitals and undergo dialysis by a nurse three times per week.
“It’s no surprise, then, that home dialysis numbers remain stagnant,” he said. “There are issues with who and how home dialysis is provided and surgical access issues.”
Dr Warr adds there is now a new generation of consultants who have “little or no access” to gain experience in looking after home patients, except when admitted to
hospital with complications.
Still, for 62-year-old Carol Chamney, home dialysis has proved to be her saviour. Unlike Shaun, Carol prefers it, saying she enjoys the freedom of being able to do treatment in her own home, but also being able to use it when she and her husband are travelling.

Carol is one of life’s optimists. Diagnosed with type 1 diabetes 46 years ago, she has since lost a leg, a foot and – after taking eight weeks
The number of Australians receiving kidney replacement therapy more than doubled between 2000 and 2020, from 11,700 to 27,700 according to the AIHW report, Chronic kidney disease: Australian facts.
More than half (53% or 14,600) of those receiving kidney replacement therapy were on dialysis and the remainder had functioning kidney transplants that required ongoing follow-up care.
AIHW spokesperson Miriam Lum On said it was estimated that 1.7 million Australians were living with early signs of kidney disease, but many Australians were unaware due to the initially asymptomatic and progressive nature of CKD.
Dialysis was the most common reason for hospitalisation in Australia in 2019–20, with about 1.5 million hospitalisations (accounting for 14% of all hospitalisations in Australia). Each dialysis treatment is recorded as a hospitalisation, with most people undergoing three dialysis treatments a week.
Among Aboriginal and Torres Strait Islander people, about 2,500 received kidney replacement therapy in 2020, a rate of 284 per 100,000, with more than one in four (26%) receiving treatment close to home.
A total of 885 kidney transplant operations were performed in Australia in 2020, with nine in 10 being for first time recipients. Of all transplanted kidneys, 704 (80%) were from deceased donors and 181 (20%) were from living donors.
Ms On said data showed the COVID-19 pandemic substantially impacted organ donation and transplantation activity in Australia. Adult kidney transplant programs were suspended from 24 March 2020 to mid-May 2020. This resulted in an 18% drop in the number of kidney transplants from deceased donors compared with 2019 (704 and 857 transplants, respectively). There was a further decrease of 6.8% in 2021 compared with 2020 (656 transplants).
of training – has undergone home dialysis for six years for CKD brought on by diabetes.
Despite her health issues, Carol leads an active life, including aqua walking in the local swimming pool three times a week, quilting, joining other DART members for quiz nights and caravanning around Australia with her husband, Terry. Because of complications from diabetes, she is not suitable for a kidney transplant.
A mother, grandmother and former nurse, Carol finds the home treatment fits in much better with her lifestyle.
“It gives me a bit of freedom,” she said from her Armadale home. “In the caravan, I put the machine next to the bed and as long as you’re careful with cleanliness and do your research before you go – and we’ve been across the Nullabor and on a car ferry to Tasmania – it can work well.”
Carol says it’s challenging at first, but there are 24-hour hotlines for home dialysis patients.
“I just want to make the most of my life,” she told Medical Forum. “Home
is not suitable for everyone, but I am very lucky that my husband does a lot for me. And I don’t let things get me down.”
For those in regional and rural areas, there is also the tyranny of distance when it comes to dialysis, with many having to travel to receive care. During COVID border closures, dialysis unit closures in some remote communities meant people were reportedly left with no option but to relocate thousands of kilometres away from home for treatment.
Dr Kulkarni stresses that continuity of care between patient and doctor is paramount to a successful journey from dialysis to transplant, an extra challenge for rural and/or remote patients relying on visiting physicians.
However, researchers have recently undertaken a transplant using a pig’s kidney with encouraging initial results. (The recipient was a braindead patient who had donated his own kidneys). While it’s early days, they’re working on eliminating risk from viruses and, as Dr Kulkarni says, there are hopes for “a future possibility of using kidneys from animals”.
Elsewhere, stem cell-based therapies could one day resolve the issue of an insufficient number of donor kidneys, reduce the likelihood of organs being rejected following transplants and reduce patient’s reliance on dialysis, according to Pharmaceutical Technology
Last year, Perth-based group Proteomics announced it had developed a simple blood test to predict and diagnose whether a patient will develop diabetic kidney disease up to four years before clinical symptoms appear.
For Shaun, he would simply like people to know more about the importance of kidney health.
“I’d like more awareness about the fact it’s a silent killer,” he said. “You hear about cancer every three seconds, but not kidney disease.”
ED: The 24th World Transplant Games will be held in Perth next April. First held in 1978 in Portsmouth, UK, the Games have grown to become the world's largest awareness event for the gift of life and a beacon for transplant recipients, their families and supporters, donor families and living donors.
Details at www.wtgf.org

Perth-based transport planner Ben Haddock argues that when it comes to what people want and expect from the environment around them, it’s not rocket science.
“Humans are pretty simple, we want to feel happy with a perception of safety, feel a connection and have clean air, so it’s not that complicated,” he says.
As future mobility lead designer in Australasia for engineering and planning consultancy Arup, Mr Haddock’s work focuses on connecting energy, transport and the environment in a low-emission space – essentially smarter urban design.

He has more than 20 years’ experience managing transport projects around the world, working with clients to help them understand and quantify how decarbonisation and clean fuels impacts cities and regions.
Earlier this year, he was guest speaker at a webinar organised by WA safety advocacy organisation Injury Matters, where he discussed the urban environment and design measures that can create a safer community.
The presentation was told that people’s mobility habits had changed significantly during the pandemic, with a 63% increase in cycling during COVID restrictions and more time spent locally. This had contributed to a 36% reduction in harmful emissions at street level, by limiting access by polluting cars to urban places.
On the downside, there had been a 29% increase in cyclist fatalities.
Mr Haddock told Medical Forum that while urban design had been part of the planning process for some time, what people were now realising was the actual impact of decisions made.
“Traditionally there has been a bit of a nod and an understanding of the potentials of a project to cause environmental harm and societal difficulties,” he said. “It has been more of a checked box exercise to get on the project, whereas now there’s a huge shift towards ‘what is the impact and why should we continue with the project’.
“We’re starting to see these things laid out in project briefs, that we need to quantify our impact, and that’s everything from a building through to a piece of infrastructure or a new road or bridge.

More than ever, our environment is impacting how we live – and vice versa, as Cathy O’Leary discovers.
“We need to consider who will be using the streets, and how they will do it, so we have to think about the user now, and we haven’t done that much in the past.”
Mr Haddock said it was obviously harder to retro-fit environments, where there was established infrastructure such as a road, footway or park that people had been using since it was installed. It created certain behaviours such as people using their car or avoiding walking across a street because it was wide and felt unsafe.
“So that’s a challenge. You have a whole group of stakeholders who already use a street but want it to be safer and a more pleasant environment that is more accessible and healthier,” he says. “But then there’s another group of stakeholders who don’t want it to change, perhaps they drive through that street and have no connection with it and want it to stay as is.”
While there were people who did not want change such as lower speed limits in local streets, WA was on the cusp of a monumental shift in how people travelled and how they perceived the need to travel.
“With COVID we’ve had a significant number of people in Perth who are travelling to and from the CBD far less than they would usually, and going to their local centre more,” Mr Haddock says.
“They’re travelling within an environment that’s 15 minutes from where they live because it’s easier. But there are other people who are travelling a significant amount more than they were in the past – such as delivery drivers and tradies.
“Other people are realising that jumping in their car is not necessarily the best option – so they’re walking and cycling more, and they’re waking up to the fact
Two Perth-based architects are behind a book which argues the case for improving the quality of mediumdensity housing in Australia – and quality of life.
Simon Anderson, who has taught architecture at the University of WA since 1989, and UWA professor of architecture Geoffrey London, explain in Designs on Density how housing remains in a state of rapid change, even crisis.
This is linked to increasing environmental consciousness, demographic movements, affordability pressures and new technologies in the building industry, the workplace and in the house itself.

The pair are well-credentialled, with Anderson a multiaward-winning architect, and London holding the positions of Victorian Government Architect from 200814 and WA Government Architect before that.
They argue the state of flux in general housing has re-invigorated debate, including how new materials and methods of construction can be best used in house-building, and how housing can help respond to environmental changes.
Their book calls for a diversity in medium-density housing types, with their main focus being on existing lots, and they include projects by a selection of Australia’s most innovative residential architects that are aimed at the majority of the population, rather than the luxury housing market.
Many of the projects featured are mixed-use buildings in the case of apartment buildings, or contain spaces on the ground floor that can be used for home offices in the case of houses on their own lots.
that some of the infrastructure that is around them, near their home, isn’t up to scratch. It’s not safe or it is an environment where you would not let your seven-year-old run free.”
Mr Haddock said his company had adopted the practice of trying to design with the eyes of a child –putting themselves at the eye level of a seven-year-old, with all their vulnerabilities. That environment was very different to what was currently in the suburbs and, in particular, the CBD.
“You can’t have everything designed through the eyes of a seven-year-old, but if you bring them into the conversation, you might have a better, safer environment,” he says.
“Children are a unifying factor and being engaged with the
continued on Page 32
There are often few apartments per floor, and they have multiple external walls and aspects and are designed to maximise angle and distance of view, access to sun and breeze, and quietness.
“Rather than champion density per se, we try to understand how to do density well at the level of the individual lot,” the authors argue. “Densification is occurring – and much of it is of a low quality, leaving a poor legacy and diminishing the suburbs where infill is occurring.
“This book has drawn together a number of examples from around Australia that each carry some lessons for how to use design intelligence to do density better.”
ED: Designs on Density, UWA Publishing, RRP $59.99

environment and community means that people attract people, so with more people you feel safer, especially at night.”
Mr Haddock said this change in approach did not have to be expensive, and cost-wise it was preferable to get it right at the start rather than having to retro-fit down the track.
“The CBD is a bit different because it’s never complete. It’s a different economic model, but in places where people live, and local centres around schools, if you get it wrong, it’s a significant cost to fix it.
“Spending a bit of time designing a safer street early on will certainly pay dividends.”
Before COVID, about 30% of all public transport users across Australia achieved 30 minutes of exercise every weekday, walking to and from their transport. During COVID restrictions, few
achieved that because people weren’t walking to the train station anymore. They needed to find their physical activity in other ways.
“Working from home has had an impact, because you don’t have to run for the train to go to work. But when you log off at 5pm, you don’t want to just transition to the couch, you need to take a break and go for a walk,” he said.
“You also can’t over-control humans. We’re organic and we make mistakes. What we really need to do is flip the narrative from designing for cars, buses and trains and design for people.
“We have to use the emotive language that’s already common in the medical environment but is not common in the built environment. It might be as simple as asking developers and governments how many people they are willing to see hurt by this scheme.”
The link with doctors advocating for

healthy environments is timely, given they have a long track record of speaking up to protect public health.
In the lead-up to the recent Federal election, 10 medical groups— including the RACGP and the Australasian College for Emergency Medicine – penned an open letter calling on politicians to address the effects of climate change, including the recent floods in NSW and Queensland.
“We are a broad group of doctors and physicians, and we’re seeing the impacts of climate change on health first-hand, supporting our communities in the aftermath of horrific bushfires and devastating floods,” they wrote.
“We’re also seeing the impacts of extreme heat, particularly on older people. Paediatricians and obstetricians are concerned about how climate change will affect the lives of their young patients as they grow. GPs and psychiatrists are witnessing the mental health impacts of climate change and
extreme weather events on people of all ages. And specialist physicians across the country are bracing for an onslaught of illness caused by the impacts of climate change.”
Dr Omar Khorshid, the former Australian Medical Association national president, said doctors had a responsibility as professionals to advocate to improve the health of their patients.
“When I’m assessing my trainees, health advocacy is one of the domains that we use. It’s absolutely a core part of our profession,” he told Medical Forum
“And while some people might say why is the AMA talking about climate change, we say it’s already having a very significant impact on the health of Australians, and is going to have a huge impact on the health of people in Pacific nations.
“The future is bleak if we don’t act.”
And while the voices of health experts have gone largely unheard by developers in the past, that could be changing, as more research is done into the impact of bad urban design.
Results from a global study on urban health released in May this year found that Australian cities wanted design to make residents healthy.
Their low density and walkability meant they failed to meet health and sustainability thresholds, according to The Lancet Global Health’s Urban Design, Transport and Health Series.
It found that people often lived in areas where it was difficult to walk or cycle to shops and services, and access healthy food, so the chances of meeting the World Health Organisation’s physical activity guidelines were stacked against them.
Led by RMIT University, the study assessed the daily impact of urban design, transport and health policies in 25 cities globally.
The Australian cities studied –Melbourne, Adelaide and Sydney – failed to meet health and sustainability thresholds, let down by poor access to public transport and car-centric designs.
Mr Haddock told Medical Forum that the time was ripe for change,
because more people were thinking about their local environments because of COVID.
“Everyone has different lived experiences, and we should be bringing that into the discussion and that’s different from what we’ve done in the past, which is minimal consultation and then going ahead and doing it anyway.

“What we know is that the link between transport and health is direct, and the health of my child going to school is all about transport, safety, accessibility and being confident in their environment.
“So, you have to look at the whole life cycle cost. If you’re creating an environment that’s unsafe, it’s a lot costlier than a safe one, even if it doesn’t look like that at the start. We’re talking about better lighting, footpaths, safer crossings, or a covered pathway.
“There are some really big decisions to be made, and others around the world are tackling this, and Perth needs to get on and tackle these decisions too.”




Australian classrooms are likely to be impacted by developmental language disorders, according to Curtin University researchers Dr Sam Calder and Dr Lizz Hill.
It is estimated that two children in every mainstream classroom are likely affected by a neurodevelopmental condition called Developmental Language Disorder (DLD).
Previously known by other labels such as Specific Language Impairment, Language Learning Impairment, and Primary Language Impairment, DLD is diagnosed when a child demonstrates difficulties understanding and/or producing language compared to children their own age.
Diagnostic criteria for DLD are outlined in both the DSM-5 and the ICD-11, and include persistent difficulties in the acquisition of language; language abilities that are substantially and quantifiably below what is expected for the child’s age, which cause significant functional limitations; difficulties that are not attributed to another biomedical condition such as autism, sensorineural hearing loss, or intellectual disability, and; the onset of symptoms arising during the early developmental period.
DLD is typically diagnosed by a speech pathologist in concert with paediatricians, educational and developmental psychologists, and educators. Children are often identified for assessment of DLD once they begin formal schooling and their difficulties communicating their wants and needs and understanding classroom instructions become pronounced compared to their peers.
Previous research in Englishspeaking countries (both the US and UK) has estimated the prevalence of DLD at about 7% in early childhood (4-5 years). Although existing Australian research has looked at the number of children with reduced language skills, our study was the first to apply the latest diagnostic criteria for DLD to an Australian population-based study.
It was also the first – to our knowledge – to provide an estimate
of DLD in middle childhood at 10 years of age. We found the prevalence rate of DLD was 6.4%, indicating the persistence of DLD from early to middle childhood. Previous research has also indicated that children, adolescents, and adults with DLD experience lower success on social, academic, wellbeing and vocational outcomes compared with those who have not experienced childhood language difficulties.
Collectively, these findings suggest children with DLD are at risk of lifelong challenges associated with their language disorder.
Early identification is critical in providing timely, targeted and effective support aimed at mitigating the functional challenges associated with the disorder. We tend to see more males being referred to these clinical services, and this is mirrored in the research.
However, our study indicates that there are no differences between the number of males and females who meet diagnostic criteria for DLD. This speaks to a referral bias for males, which is particularly alarming when we consider that females with DLD are three times more likely to experience negative outcomes such as sexual abuse compared to those without language difficulties.
It is important to understand what factors place a child at risk of language disorder in order to increase the likelihood of early identification and timely support. Consequently, we also examined potential perinatal and environmental risk factors that may predict a diagnosis of DLD at 10 years.
We found that having a mother who smoked while pregnant was the only significant risk factor of DLD at 10. While it was not possible to draw a causal link between exposure to environmental teratogens in utero and later neurodevelopmental disorder in our study, we believe this finding adds weight to public health
messages for mothers to avoid smoking, especially while pregnant.
Additionally, there is research to suggest that the relationship between language disorder and smoking in pregnancy is reflective of a shared association with social and/or financial disadvantage. Consequently, it is critical that families experiencing socioeconomic disadvantage receive targeted and consistent financial and social support.

We know that the early developmental period is associated with enormous individual variability. This means that it is difficult for professionals to reliably identify a child with DLD before the age of four years. In fact, Australian research has indicated that late language emergence (aka late talkers) is not a reliable predictor of language disorder in later childhood. Despite this, there are some things that medical practitioners can look out for that may help identify a child with DLD.
We would recommend referring the family to a speech pathologist if a child has not met early communication and language milestones. The speech pathologist can assess for early language difficulties.
If a child has commenced formal schooling and is experiencing difficulties socialising, following instructions, and/or engaging in the classroom, a speech pathologist can help determine whether language difficulties are contributing to these problems. Involving a speech pathologist can increase the chances that a child will receive targeted and effective support as early as possible.
Oral language skills form the foundation for socioemotional development and academic success. If a child is facing challenges within and beyond the classroom, let’s go to the potential source: language.

New horizons lie ahead for the management of spinal cord injuries, according to eminent Perth researcher Emeritus Professor Byron Kakulas
Injury of the spinal cord resulting in complete or partial paralysis of the lower limbs (paraplegia) or all four limbs (tetraplegia) is a devastating life-changing event. Spinal cord injuries (SCI) pose a massive worldwide problem, in both human and economic terms.
It is estimated that there are 20,800 people in Australia living with SCI and between 250,000 and 500,000 worldwide. Most spinal cord injuries are due to preventable causes such as road traffic crashes, diving accidents, falls or violence. The economic burden of SCI in Australia is calculated to be $74.5 billion, representing health care costs and loss of productivity.

The standard treatment of SCI in the acute phase is surgical decompression undertaken as soon as possible after injury followed by intensive clinical care. Rehabilitation begins when the injury is stabilised.
Partial recovery of neurological functions is usual in the weeks and months post-injury and some further improvement may be expected for up to a year.
Many years ago, in pioneering work, Sir Ludwig Guttmann in London and our own Sir George Bedbrook in Perth concluded from their own experience that early surgical decompression is of no apparent benefit in promoting recovery and may even aggravate the neurological state of the patient. Their experience is supported by the neuropathology of SCI which demonstrates that there is no lesion in the damaged spinal cord or vertebral column which would benefit from surgery.
The usual and conventional view of those attending to SCI is that the spinal cord is totally transected due to the trauma in ‘complete SCI’. However, this view was shattered by the neurophysiological findings of my long-time collaborator,
Professor Milan Dimitrijevic of Baylor Medical College, Houston, Texas, who clearly demonstrated that neurological signals may pass through the level of injury both in caudal and rostral directions.
He coined the term ‘discomplete SCI’ to describe this clinical state. Professor Dimitrijevic’s findings were considered so radical that initially he had great difficulty in having his observations published.
This situation changed when it was shown from my post-mortem studies that of a total of 220 SCI autopsies, 53 (24%) were in fact anatomically discomplete with some degree of white matter being found to traverse the level of the lesion, thus supporting Professor Dimitrijevic’s observations and most importantly the preserved nerve fibres providing a substrate for the application of the methods of restorative neurology.
Most prominent among the restorative techniques is epidural spinal cord electrical stimulation,
which when applied to patients with complete paralysis improves neurological function below the level of injury with a return of voluntary movement in the paralysed lower limbs. In a number of SCI cases, the effect of electrical stimulation is so dramatic that complete SCI becomes incomplete.
Epidural electrical treatments are of great benefit in SCI rehabilitation. Since the early discoveries, electrical stimulation has been refined to the extent that transcutaneous stimulation is effective. Furthermore, in recent years, Professor Dimitrijevic’s work has been widely accepted and improved upon all around the world.
ED: Emeritus Professor Byron Kakulas, who turned 90 this year, is founding director of the Perron Institute for Neurological and Translational Science.

invited to explore the ways MRI-guided Transcranial Magnetic Stimulation (TMS) can benefit your patients during a complimentary Coffee ‘n’ Conversation session with a psychiatrist from sentien sentien’s dedicated team is utilising TMS to make headway in the treatment of depression and other psychiatric conditions, including Obsessive-Compulsive Disorder (OCD) and Post-Traumatic Stress Disorder (PTSD).
can also improve the burden of physical pain and has even been utilised for medical rehabilitation (e.g. post-stroke recovery), managing fibromyalgia and relieving the symptoms of tinnitus.
procedure is:
the MBS for treatment-resistant
you would like to find out more, one of sentien’s TMS experts would be delighted

attend your practice
an in-person
Video conferences
also be arranged, should you prefer.
interest.
There are more than eight million reasons to celebrate the 30year journey of the Perth-based Meningitis Centre Australia, says its co-founder, Bruce Langoulant

When Professor Fiona Stanley called a group of parents and health professionals to explore the opportunity for a local meningitis advocacy group in 1991, her inspiration was to protect WA babies from a deadly disease.
Meningitis was not well known or well understood, and it was killing and disabling very young children regularly across our state and nation.
Those parents who assembled knew this. The health professionals did too and were fighting its symptoms often with little time. Meningitis progresses quickly and dangerously especially in our very young children.
The motivation for the meeting was the pending arrival of the first infant vaccine for Hib – a bacterial infection causing 40% of the meningitis cases in the early 1990s – and the need to raise public awareness.
The Meningitis Centre was created with a mix of these clinicians and parents and launched on April 24, 1992, in Perth by Prof Stanley, with me, a parent, as its chair.
The centre set about raising awareness of the early signs and symptoms of meningitis and providing support to families. It also launched the ‘Wipe it Out’ campaign to get the Hib vaccine onto the state’s vaccine schedule, and make it free for all babies.
The WA Government decided to introduce and fund the Hib vaccine and it was subsequently added to the National Immunisation Plan (NIP) for all Australian babies born.
Since its introduction in 1993, an estimated 8.1 million babies have received the Hib vaccine free and Hib meningitis today is rarely seen. It remains on the NIP. Every year, the estimated 300,000 babies born have the Hib vaccine as
part of the free and routine infant vaccine program.
As Meningitis Centre Australia (MCA) celebrates its 30th anniversary, it can also celebrate the addition of the pneumococcal vaccine in 2005 for infants and the meningococcal ACWY vaccine in 2016-18 for infants and for teens. Both were added to the NIP and are free and part of the routine schedule.
MCA campaigned with parents and survivors and medical professionals for several years to achieve these life-saving successes. The participation of those impacted by telling their stories to the media and key decision makers was instrumental in the governments of the day taking positive action.
While the primary messages of looking out for the early signs and symptoms – and parents know their child best – are still hallmarks of the 30 years of MCA today, the addition of lifesaving vaccines has been the big gain.
As the founding and current chair, I have shared my daughter’s
incredible survival from pneumococcal meningitis in 1989 over this time. Ashleigh’s life has been dramatically impacted and has been the driving force for me to protect others.
It’s a legacy which MCA has embraced and continues with its team to consistently remind parents in particular to Know Act Vax –know the signs and symptoms, act immediately if concerned and vaccinate for protection.

MCA has the latest in resources and is regularly giving presentations at schools and daycare centres and for CALD and indigenous groups.
Australian families and their doctors and at least the 8.1 million babies born so far since 1993 are in a safer place due to MCA’s persistent work and the key decisions made to launch the centre in 1992.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act. https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
This column is written the day the world lost Queen Elizabeth II. For many (myself included), she was on the throne before we were born.
Former Prime Minister Paul Keating (a republican) said in a statement that she was “an exemplar of public leadership” and that “with her passing her example of public service remains with us as a lesson in dedication to a lifelong mission in what she saw as the value of what is both enduringly good and right.”
In no way is our role as doctors the same as the monarch. However, we too are duty bound to do what is both enduringly good and right for our patients. For centuries the medical profession fought for its independence and its right to act in the best interest of the patient in front of us.
Over the past three decades the will to defend the independence of the profession has waned. Over the past two years, our will to even be questioning edicts has diminished. It is useful to look back in history at the results of medicine becoming a tool of the state.

This month’s theme is musculoskeletal health. Regular physical activity is good for both physical and mental health. Among the many harms of lockdowns was the inability of people to exercise. A new paper in the British Journal of Sports Medicine concluded: “Regular physical activity seems to be related to a lower likelihood of adverse COVID-19 outcomes. Our findings highlight the protective effects of engaging in sufficient physical activity as a public health strategy, with potential benefits to reduce the risk of severe COVID-19.”
An exhaustive review published in July found “no consistent evidence in the main avenues of serotonin research that there is an association between serotonin and depression, and we found no support for the hypothesis that lower serotonin activity or concentrations are responsible for depression.”
Breakfast as the most important meal of the day was an advertising slogan as was 10,000 steps per day. The pharmaceutical industry has more than three lobbyists per each member of the US congress, spending three times that of the oil and gas industry in 2021.
We are starting to ask questions about what we have accepted unquestioningly.
Queen Elizabeth was both a traditionalist and a realist. Her approach to matters changed over 70 years but her underlying values did not. How we do things in medicine changes but our values and what is enduring right and good must not.
Vale Queen Elizabeth – an exemplary life.
Over the past three decades the will to defend the independence of the profession has waned.
Over the past two years, our will to even be questioning edicts has diminished.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act. https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Patients should now expect a better range of motion, function and survivorship of their knee replacement. A combination of better implants, improved surgical technique and optimised pain management and rehabilitation have resulted in these better outcomes.
The current treatment aim is a forgotten joint, with minimal discomfort and full function. More patients are achieving this.
Knee replacements were always said to last 10 years. This is no longer the case. The Australian Orthopaedic Association National Joint Replacement Registry monitors the survivorship of all knee replacement surgery performed in Australia over the past 20 years.
It can demonstrate the better and poorer performing implants, allowing surgeons to choose a well-performing knee replacement. Currently over 90% of knee replacements would be expected to survive for more than 20 years. Caution still needs to be exercised in younger and larger patients who have been shown to have higher revision rates.


Multi-modal analgesia has become the norm in knee replacement
Knee replacement surgery remains the best treatment for end stage knee osteoarthritis
Outcomes from total knee replacement have improved markedly Technology is enhancing individualised treatment.
surgery. This most commonly involves a spinal anaesthetic, sedation or GA, peripheral nerve blocks, local anaesthetic infiltration, simple analgesia, pregabalin, NSAIDs and judicious use of narcotics.
This enables quicker rehabilitation with earlier hospital discharge. Current hospital stays average between two to four days, with only those lacking social support or multiple co-morbidities requiring a stint in the rehabilitation unit prior to discharge home.
Improvements to instrumentation and technology have optimised surgical technique. The most recent advance is the introduction of surgical robots. These vary from the robots used for prostatic surgery. These ‘soft tissue’ robots
enable the surgeons to improve their dexterity and surgical precision.
Orthopaedic or ‘hard tissue’ robots build a three-dimensional model of the limb and allow surgery to be planned virtually. Soft tissue balance can be considered in this model intra-operatively and the plan individualised. The robotic arm assists the surgeon by executing the required bone cuts. Robotic knee replacement has been shown to decrease soft tissue damage during the procedure, decreasing pain and opioid requirements. This technology is now being used in over 20% of all knee replacements in Australia.
Individualised alignment in knee replacement is an area of intense clinical research. Previously, all patients received a knee replacement positioned in the same alignment. Now, it is commonly accepted that there is wide variation in the native alignment of patient’s legs.
Tools and techniques exist to enable individual plans for alignment. The challenge is to identify the ideal alignment for each patient. Advanced technologies such as computer navigation and robotics are assisting assessment of individual alignment and allowing data collection to further optimise this process in the near future.
Infection control plays a vital part in decreasing post-operative complications. Skin decolonisation together with optimisation of co-morbidities such as diabetes has decreased infection rates, but joint infection remains a major complication in just under 1% of patients.
A combination of early mobilisation, surgical technique and prophylaxis has seen a decrease in the rates of thromboembolic disease postsurgery. The major complication of knee replacement remains pain and



Technology and technique advancements over the past decade have seen two big game changers – the rise of minimally invasive foot surgery and improved total ankle replacement.
Minimally invasive (MI) foot and ankle surgery has revolutionised my practice in recent years, particularly for forefoot deformities.
Previously, the mainstay of bunion (hallux valgus) and toe deformity correction surgery involved open approaches, often with significant stripping of the periosteal blood supply to bones and more risk of soft tissue damage. Bigger cuts result in more swelling and scar tissue, which can create stiffness, wound healing issues and pain.
Respect for the soft tissues in a foot is always paramount given
Minimally invasive foot surgery techniques offer the ability to correct a range of deformities through keyhole incisions
Total ankle replacement outcomes and survivorship are significantly improving with new implant systems and better instrumentation including 3D printing technology
Studies now show similar pain relief with ankle replacement vs fusion, with TAR providing the advantage of a more normal gait cycle and foot biomechanics.
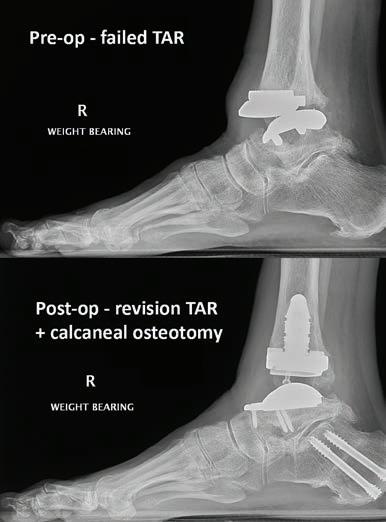
the relative paucity of soft-tissue coverage over the bones and the proximity of neurovascular
structures, no matter which part of the foot is being operated on.
MI cutting burrs under x-ray guidance allows us to address a range of foot problems using small keyhole incisions. This includes bunions, bunionettes (the bunion equivalent at the fifth toe), hammer/claw toes, and metatarsal deformities. We can remove bone spurs around arthritic joints (such as with big toe arthritis) and undertake calcaneal slide osteotomies (often done as part of a flatfoot or higharched foot procedure).
In diabetics with peripheral neuropathy, MI techniques now allow removal of bony prominences causing pressure areas or ulcers through tiny incisions, diminishing wound healing problems and infection in these high-risk feet. We can even do some major deformity corrections in a Charcot foot using only small incisions along with percutaneous fixation.
Minimally invasive foot surgery usually results in less swelling, pain, scarring, and wound healing issues, as well as providing better cosmesis. MI techniques compared with open techniques have also been found to better correct forefoot deformities, particularly bunions and hammer toes.

Ankle joint arthritis is significantly disabling and has similar impacts on quality of life and pain compared with hip and knee arthritis. Most ankle arthritis is post-traumatic as opposed to osteoarthritis in the hip and knee. This results in ankle arthritis patients being on average younger and higher demand, leading to significantly increased forces going through a much smaller joint.
For over 50 years, ankle fusion has been the mainstay of surgical treatment for end-stage ankle arthritis. While total ankle replacement (TAR) was first

performed in the 1970s, early generations of ankle replacements had high failure rates, leaving some surgeons to wonder whether it was even possible to replace the ankle joint with the same success that we see in the hip, knee, and shoulder.
In the last decade, big advances have been made in the implant technology and instrumentation for TAR, along with a deeper understanding of foot biomechanics and why earlier generations of implants failed.
One of the current fourthgeneration ankle replacement systems allows patients to undergo a pre-operative CT scan which is
used to create custom 3D-printed patient-specific cutting guides, allowing the TAR to be implanted with increased accuracy, while also reducing surgical time. Stemmed options are available, which can be used for better implant fixation in poor quality bone.
Perhaps most importantly, revision implant options are better developed, giving us the ability to keep a patient’s ankle joint moving with another replacement in the case of failure, as opposed to converting to a challenging hindfoot fusion or even below knee amputation.
A better understanding of foot biomechanics and why previous TAR designs failed is also leading to improved longevity. I half joke with patients that my hip and knee colleagues have it easy, with one bone above and one bone below their replacements – we have to balance two bones above, and 24 bones below! We now know that replacing an ankle without addressing deformity of the foot below the ankle is a recipe for failure – a plantigrade foot under an ankle replacement is a must for a longterm good outcome.
Author competing interests – nil
stiffness. Optimising pain control and early rehabilitation remains key to preventing this. Early referral back to the surgeon if any concern regarding possible complications is always the safest management.
Functional outcomes after knee replacement have improved dramatically over the past 20 years, largely due to improved range of motion achieved. Although directly related to pre-operative range, the average patient should expect full extension and over 120 degrees of flexion allowing all ADLs to be achieved.
Over 50% of patients should be able to kneel. Return to social sport should be expected in those fit enough to do so and patients should be able to walk for over 60 minutes without discomfort. Return to work should occur between six and 12 weeks, depending on occupation.
Unfortunately, knee osteoarthritis (OA) is not likely to have a cure in the medium term and knee replacement will remain the mainstay of treatment for end stage knee OA.
We will see continued improvement
in surgical technique and optimised individualisation of that technique. Knee OA is also likely to be one of the first areas where big data and machine learning will assist, with treatment algorithms helping guide both doctors and patients on the optimal treatment at different stages of the disease, as well as the optimal surgical management when the time for knee replacement occurs.
Author competing interests – the author is a research and development consultant for the manufacturer of Mako robot.

At SKG, we care about your patient’s welfare

A 54-year-old woman presents with a palpable abnormality in the right breast. She has no personal or family history of breast cancer. A palpable lump is present in the right breast at the 5 o’clock retroareolar position. There are no skin changes, nipple discharge or palpable axillary nodes.

Her routine screening mammogram a year ago was reported as normal. Her current diagnostic bilateral 3D breast tomosynthesis study showed extreme breast density. The right breast mammogram showed a noncalcified density with a partially circumscribed margin correlating with the palpable lump. The diagnostic ultrasound demonstrates a suspicious mass lesion in the right breast 5 o'clock position (Figure 1A) with right axillary lymphadenopathy (Figure 1C).
A specialist breast radiologist’s role is to address the referrer’s clinical questions and correlate the clinical symptoms with imaging and histopathology. The triple test assessment should be completed when dealing with all breast disease including screening and symptomatic issues.
The ‘triple test’ assessment is comprised of three fundamental diagnostic components:
1. Medical history and clinical breast examination (CBE) including
The role of imaging is to answer a clinical question
Dual referral for imaging and procedure can be expeditious
The biopsy is generally safe with
INR under 1.6.
clinical findings, nature, and duration of the symptoms, the exact lesion location, personal and family history of breast cancer, presence of breast implants, information regarding anticoagulation and HRT medications, and any previous radiotherapy or chemotherapy.
2. Imaging – mammogram and/or ultrasound
3. Non-excisional biopsy – fine needle aspiration (FNA) cytology and/or core biopsy.
Managing patients with a suspicious mass on imaging can be expedited if a referral to perform an imageguided breast procedure at the time of the patient’s radiology appointment was available. Ultrasound-guided core biopsy is the preferred method for sampling (Figure 1B).
Unfortunately, this patient did not have a biopsy request and the referrer was not available on the day, thus biopsy procedure was
organised the following week. This can be challenging in remote or rural areas. If the patient is taking anticoagulants, discuss this with the radiologist before organising a possible biopsy procedure. A biopsy is considered safe where INR is < 1.6. Patients taking other anticoagulants are generally advised to stop these two to three days before their appointment.
There are three types of imageguided breast procedures: fine needle aspiration, core biopsy and vacuum-assisted core biopsy.
Fine needle aspiration is a minimally invasive procedure to remove cells or fluid from a breast lesion using a 21-27 gauge needle. It is done to aspirate symptomatic breast cysts and atypical cysts, drain an abscess or seroma and sample an abnormallooking axillary lymph node (Figure 1D). FNA is an alternative sampling method for patients taking anticoagulants in rare situations.
Breast core biopsy is done to collect small cores of tissue using a 14-18 gauge hollow needle from an abnormal area. The procedure provides more specificity as compared to FNA, it has the additional advantage of ancillary tests and comments on the histopathological prognostic and hormonal markers. This is indicated in patients with breast lesions that are not palpable, small, and calcified. A core biopsy is recommended for inconclusive or non-diagnostic FNA and to differentiate between carcinoma in situ (DCIS/LCIS) and invasive carcinoma (IDC/ILC).
Vacuum-assisted core biopsy (VACB) uses a vacuum-powered device to obtain tissue samples from the breast using a 7-12 gauge needle. It is performed percutaneously under local anaesthesia as an outpatient procedure under ultrasound, mammogram or MRI guidance.
This is indicated to sample
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act. https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

The glenohumeral joint is the most frequently dislocated joint and usually occurs following an injury such as a fall or in a collision during sports including AFL, basketball or rugby. The direction of dislocation is usually anterior and most will self-reduce, but it is estimated 3040% require a formal reduction.
The most common injury associated with a traumatic shoulder dislocation is tear of the fibrous labrum that surrounds the glenoid (Bankart lesion). Associated injuries include a fracture of the rim of the glenoid (bony Bankart lesion), an impaction fracture on the back of the humeral head (Hill Sachs lesion) and nerve injury, typically to the axillary nerve.
Tears of the rotator cuff tendons also may occur, usually in patients over 45 years and it is recommended to obtain imaging for these patients.
These injuries can cause permanent shoulder dysfunction if they are not identified and properly treated. The main problem following a shoulder dislocation is recurrent instability.
Patients under 30 years of age, and those that play collision or overhead sports, have a 70-95% risk of recurrent instability.
The glenohumeral joint is the most frequently dislocated joint
Treatment is based on the unique circumstances of the individual, with physiotherapy first line
Stabilisation surgery is generally for recurrent dislocations.
Patients with this recurrent instability have difficulty because the shoulder feels weak or unstable in the overhead position, even if it does not frankly dislocate. In published series the long-term prognosis after a single anterior dislocation found at 25 years, two thirds of patients had arthritic changes on x-rays.
Treatment is based on the patient’s unique combination of age, symptoms and functional requirements. Physiotherapy is the first line treatment for most cases, even though it does not address the labral tear. The aim is to improve the strength and coordination of the dynamic stabilisers that surround the glenohumeral joint and improve scapula control.
The patient should rest their arm in a sling for one week or until comfortable following a first-time dislocation. Physiotherapy can begin in the first week following injury and return to full contact sports can be expected at around three months.
Stabilisation surgery is generally reserved for patients who either have had recurrent dislocations or are at high risk of developing recurrent instability.
A dislocation with associated fracture, rotator cuff tear or nerve injury would require prompt review. A first dislocation in a patient under 30 years and playing contact or high-risk sport, in the military, or with a job which involves climbing or overhead lifting may prefer the option of stabilisation surgery to reduce the likelihood of a further dislocation and subsequent time off sport or work.
Second (or greater) traumatic dislocation, persistent pain, weakness, or lack of confidence in the shoulder despite physiotherapy would indicate a failure of nonoperative treatment and warrant further work-up.
Author competing interests – nil
indeterminate calcifications, small mass or architectural distortion only seen on MRI or mammogram and a previous core biopsy (14g) considered non-diagnostic. There is no post-procedure care with FNA.
For core biopsy and VACB, the skin incision will be secured with steristrips and covered with a waterproof dressing. An icepack is placed over the biopsy site to avoid further bruising. Patients are advised to take paracetamol for pain relief (not aspirin).
There are no absolute contraindications to FNA and core biopsy unless sampling needs to be performed under MRI guidance.
FNA has a theoretical risk of damaging breast implants, but this is avoided with imaging guidance performed by experienced specialist breast radiologist.
Core biopsy and VACB are relatively contraindicated in patients taking anticoagulants such as warfarin to avoid bleeding, obesity due to prone tables weight limitation and lactation which has a very small risk
of developing milk fistula.
All three procedures exhibit common adverse effects (less likely in FNA) such as bruising, haematoma formation (less than 1%), infection (less than 0.1%), and breast pain. Pain can be relieved by the intake of paracetamol. There is a rare possibility of secondary haemorrhage from arterial bleeding in core biopsy and VACB which is usually controlled by local pressure. However, if this is not successful, a surgical intervention may be needed.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act. https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act. https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments



In rectal cancer management, the main application of radiotherapy (RT) is in the neoadjuvant setting in Stage III (T3-4, node positive) and selected Stage II cancers.
A multidisciplinary approach is imperative to ensure all patients and cancer factors are carefully discussed. The American Society for Radiation Oncology (ASTRO) practice guidelines recommend that surgery occurs within 6-11 weeks post chemo radiation.
There is evidence of increasing perioperative complications between 7-11 weeks, but strong evidence in favour of a higher pathological complete response (pCR) rate if the surgical interval post chemoradiation is over six weeks. For shortcourse radiotherapy patients, an interval before surgery of less than three days or 4-8 weeks is recommended.
The common RT fractionation schedule is 50-50.4Gy in 25-28 fractions over 5-6 weeks (longcourse), and 25Gy in five fractions (short-course). Long-course chemo radiation is commonly utilised over short-course RT, as recommended by the St Gallen European Organisation Research and Treatment of Cancer (EORTC) panel.
It is also generally advised if the circumferential resection margin and/or the margin resection status is likely to be compromised. Recent ASTRO clinical practice guidelines support both long-course and short-course RT in patients requiring neoadjuvant therapy. Randomised studies suggest similar efficacy and patient-reported quality of life outcomes with either approach.
Interest is increasing towards a total neoadjuvant therapy (TNT) approach. Total neoadjuvant therapy involves the delivery upfront of multi-agent chemotherapy then chemoradiation followed by definitive surgery. The rationale of TNT is to induce
A multidisciplinary approach to management is key Interest in total neo-adjuvant treatment (TNT) is growing
Radiation techniques have greatly evolved in the last decade.
a higher rate of pCR, and hence improved downstaging. It is also possibly better tolerated compared to the standard approach.
However, despite reports of enhanced disease-free survival, an overall survival benefit with TNT is not yet proven. Several trials have investigated different TNT approaches and their benefits.
The option of ‘watchful waiting’ or non-operative management is also gaining interest in patients who achieve a complete clinical response (cCR), as most patients would understandably prefer to avoid surgery or a stoma. However, surgery remains the definitive treatment for cure.
Watchful waiting is feasible in a selected cohort of patients under multidisciplinary management if they are compliant with regular surveillance and investigations aimed at ruling out recurrence or enabling early salvage treatment. In a meta-analysis, the only risk factor associated with regrowth was the initial T stage. A distant metastasis rate of 5% to 9% has also been reported with watchful waiting. The TNT approach may allow a larger proportion of patients to undergo watchful waiting within a carefully shared decision-making process.
The frequency and modality of investigations remains variable from institution to institution. Response is assessed typically 2-3 months after treatment and the definition of cCR is based on clinical examination: digital rectal examination (DRE), endoscopic features, and imaging studies, specifically rectal MRI.
As tumour regrowth is most
frequent in the first two years after radiotherapy, current protocols recommend DRE and flexible sigmoidoscopy every three months for the first two years and then every 6-12 months for the next three years. These patients also require surveillance CT chest, abdomen, and pelvis every 6-12 months for the first two years, and then annually to rule out the development of distant metastases.
RT is also useful in the treatment of Stage IV colorectal cancers with either aggressive intent in the oligometastatic setting (under five sites of metastatic disease), or with palliative intent to relieve symptoms, such as bleeding or pain. The recent COMETSABR trial supports the use of stereotactic body radiotherapy (SBRT) to metastatic tumours in oligometastatic disease due to improved progression-free survival and median overall survival (50 vs 28 months).
Radiation techniques have greatly evolved in recent decades. RT is now delivered in a modulated technique with either intensitymodulated radiation therapy (IMRT) or volumetric-modulated arc therapy (VMAT). Such techniques enhance conformity and enable dose to be maximised to the target while minimising its delivery to surrounding organs, such as the bladder, sexual organs, normal bowel, and pelvic bones. This has been shown to reduce the incidence of acute and late toxicities, particularly in the bowel. Radiation oncology has made great progress in the last decade. In colorectal cancer, RT remains an important part of the multidisciplinary armamentarium. Our challenge now as clinicians and researchers is to continually advance and improve treatment techniques to maximise the equally important patient-reported outcomes.

An anterior cruciate ligament (ACL) injury presents short and long-term challenges to the patient and the health system.
In Australia, ACL rupture is generally treated with a surgical reconstruction (ACLR), with an annual incidence of 77.4 reconstructions per 100,000 population (2015). This is a 43% increase since 2000 and, more importantly, a 74% increase in those under 25. Concerningly, while the peak in 2015 was in the 20-24 age bracket for men and 15-19 for women, the annual growth incidence was greatest in the 5-14-year-old bracket.
Short-term challenges are highlighted by return-to-sport rates, with only 82% of patients returning to some kind of sports participation following ACLR, and only 44% returning to competitive sport. Long-term, an increased risk of knee osteoarthritis (OA) (tibiofemoral and patellofemoral) after ACL injury is well established.
With rates of injury and reconstruction continuing to rise, the cost of ACL injury and reconstruction to the Australian health system is estimated at $315 million by 2030-2031 (excluding indirect costs of OA/persistent knee disability).
Exercise rehabilitation protocols significantly improve physical function following ACLR. However, even with protocols targeting muscle strength and function, quadriceps and hamstring strength impairments often persist.
Rehabilitation efforts tend to focus on the knee directly, minimising swelling, regaining range and quadriceps strength. Unfortunately, if the rehabilitation focus is solely on the injured joint, there is a risk ignoring a vital component of the rehabilitation journey, the brain.
Patients and rehabilitation providers need to understand the mechanisms by which the brain is affected by ACL injury and ACLR, how this can influence rehabilitation outcomes and the interventions available to
ACL injury induces central nervous system adaption, which may adversely influence rehabilitation outcomes, contributing to persistent quadriceps and hamstring weakness
Rehabilitation should incorporate techniques that can mitigate maladaptive processes and enhance beneficial neuroplasticity
Transcranial direct current stimulation (tDCS) may help overcome the central inhibition driving arthrogenic muscle inhibition.
address this. Transcranial direct current stimulation (tDCS), a form of non-invasive brain stimulation, may play a role in mitigating early maladaptive processes seen in ACL injury and ACLR.

It is well established that a joint injury, such as a knee injury, can lead to arthrogenic muscle inhibition,
which in part is a centrally mediated process. ACL rupture can also be considered a deafferentation injury, given the loss of joint proprioceptive information from the ACL.
Individuals with an ACL injury have been shown to have increased corticospinal inhibition, associated with decreased quadriceps strength. Not surprisingly an ACL rehabilitation program only addressing peripheral injury (i.e., knee effusion and range) and not central adaptations to an injury can see persisting impairments in quadriceps and hamstring strength.
Multiple rehabilitation techniques and interventions are available to address or mitigate deleterious central adaptation to injury and to maximise beneficial neuroplasticity during recovery. Eccentric crossexercise (exercising the contralateral limb) may improve muscle recruitment and strength in the injured limb due to bilateral motor pathway changes.
Motor imagery (the mental practice of a motor action) can increase excitability and activation of motor cortex (and spinal) neurons. Utilising
an external focus of attention can decrease motor cortex inhibition (i.e., “push the ground away forcefully” is an external focus cue, compared to “extend your knees and hips forcefully” for internal focus).
Transcranial direct current stimulation (tDCS) is a safe, noninvasive form of brain stimulation that passes a weak direct electrical current (typically ≤ 2 mA, compared
to 800-900mA for ECT) between an anodal and cathodal electrode placed on the scalp. Generally, cortical excitability is increased with anodal tDCS (anode applied to the target cortical region).
There is evidence that tDCS application to the primary motor cortex may promote an increase in muscular maximal voluntary contraction and possibly muscular endurance, improve balance performance, gait retraining, multi-task performance and motor learning of sport-specific skills and tasks.
The potential benefits of tDCS application align with ACL rehabilitation goals, namely preventing the loss of/regaining muscular strength, regaining, and improving neuromuscular control, and re-introducing sport-specific movements and tasks.
SportsMed Subiaco, in conjunction with Edith Cowan University, the Orthopaedic Research Fund of Western Australia (ORFWA) and researchers from Murdoch University and La Trobe University, have started the TACL Study (The impact of Transcranial direct current stimulation during rehabilitation
following Anterior Cruciate Ligament (ACL) reconstruction on functional outcomes and return to play timelines. A double-blind, randomised controlled trial).
Suitable participants with an acute ACL rupture will undergo transcranial magnetic stimulation assessment pre-op, post-op and throughout rehabilitation to measure changes in corticospinal excitability, intracranial inhibition and facilitation. Sports physiotherapists at SportsMed Subiaco will provide free standardised ACL rehabilitation.

Participants will be randomised to either real or sham tDCS, to be applied three times a week from week two to week eight postoperatively. If tDCS application can mitigate the quadriceps inhibition seen post-injury/reconstruction, it may become another tool in the arsenal for rehabilitation providers. In ACL rehab, at least some of it is in your head.
The author acknowledges ECU (Dr Myles Murphy) and the Orthopaedic Research Foundation of WA (Dr Peter D’Alessandro).
Author competing interests – the author is involved in the research described
Led by Dermatologists
one of Australia’s longest running laser and non-surgical skin solution clinics.

team
made up of accredited and highly
Consultants.


In 1993, we had one paediatric patient with Sickle Cell Disease (SCD) at PMH. We now have 55 patients under age 17. That may not sound like many, but this is a chronic disease with many challenges facing the patients, their families and the staff caring for them through their lifetime.
The pathophysiology is of an acute and chronic vasculopathy and hence comparable to diabetes. If we manage these patients well as infants, children and adolescents, they will become healthy adults.
Specialised multidisciplinary hospital service provision, research and education is lagging behind the change in demographics over the past 30 years with migrants and refugees from countries where the incidence of SCD is higher.
Sickle Cell Anaemia (Hb SS) is a multisystem disease associated with episodes of acute illness and progressive organ damage. There is a single mutation in the beta globin gene resulting in replacement of glutamic acid by valine in position 6 of the beta chain. If present in one gene, the patient has a sickle cell trait (Hb S) and is largely symptomfree. If in both genes, the patient has Hb SS. Sickle disease is any condition in which the inheritance of Hb S can lead to the sickle shape of red blood cells and therefore includes co-inheritance of Hb S with another beta globin chain defect, such as Hb C or a beta thalassaemia.
This disease largely affects people with African and Middle Eastern ethnicity as the malaria parasite does not enjoy Hb SS. These patients are not immune to malaria and still require prophylaxis when heading to a malarial risk area.
The global burden of SCD is over six million cases including 300,000 births annually. Australia does not have a coordinated approach to antenatal/newborn screening. Early diagnosis and introduction of therapy can prevent complications. A full blood picture may have normal indices. The film features should detect some sickle cells,
Demographic changes have seen a steep rise in SCD prevalence in Australia
Better treatments are improving survival
Australian guidelines are being developed as are new treatments.
target cells and may show signs of hyposplenism depending on age.
The diagnosis in a high-risk individual can be made at any age by performing a full blood picture and haemoglobin study to detect the sickle haemoglobin in a carrier (there will be normal Hb A) and an individual with SCD (who will show a peak where the Hb S is detected).

Regardless of age, an urgent sickle solubility test can be performed to detect the presence of Hb S on a sample. This cannot differentiate a sickle trait from SCD.
SCD has been recognised as an acute and chronic inflammatory disease. Multiple cell types
and molecules are involved in its inflammatory pathways. The complications of this pathophysiology are multiple and affect all organs (Fig. 1) and any age group. When a vaso-occlusive crisis occurs, the patient presents in severe pain. They require urgent therapy (including hydration, pain relief). In some cultures, this disease is still stigmatised and there may be family denial.
There are international guidelines for standards and recommendations for acute emergency presentations and ongoing therapy and surveillance. Australian guidelines are in development.
One of the main changes to infant and childhood mortality from SCD has been the international early introduction of prophylactic penicillin and immunisation against encapsulated organisms.
Up to 98% of children with SCD will now survive to age 18. However, these children would have ongoing complications from the vasculopathy were it not for the introduction
of oral hydoxyurea, an effective (few side effects) and relatively inexpensive therapy optimally introduced at about nine months of age, when the fetal haemoglobin falls and the Hb S rises to a more critical level.
Its main mechanism is to increase production of Hb F (adults usually have <1% Hb F) thus reducing the total amount of Hb S. Hydroxyurea causes a mild neutropenia reducing some inflammatory aspects of the disease. Studies have shown, hydroxyurea reduces vaso-occlusive crises, hospital admissions, anaemia, haemolysis, strokes and improves survival.
Regular surveillance for vasculopathy is also a part of the international guideline. This involves transcranial doppler (for evidence of cerebral stenosis), head and hip MRI, renal, ophthalmology, cardiac, dental, respiratory, neurodevelopmental, and endocrine surveillance.
Families may have come to Australia as refugees with additional trauma due to war and conflict, with English not their first language. Interpreter services, clinical psychology, occupational therapy and social work services are essential to an integrated, focused multidisciplinary approach.
Despite adequate hydroxyurea doses, some patients (10-15%) still experience complications – cerebral vasculopathy, acute chest syndrome and recurrent vaso-occlusive disease. These patients require regular red cell transfusion to reduce the Hb SS. Automated red cell exchange using apheresis is currently used as an emergency procedure at PCH (acute chest syndrome, acute neurological presentation and severe vasoocclusive crisis not responding to usual therapy).
However, it is now considered the standard of care internationally for patients having regular red cell transfusions for SCD. This allows longer intervals between transfusions, lowers Hb S most efficiently, lowers pro-inflammatory markers and has a possible reduction of allo-immunisation. It also lowers iron stores and patients do not have to take oral iron chelation therapy.
Apheresis is faster, but it also requires skilled nursing, is more expensive than standard transfusion, sometimes requires central venous access and may have an increased donor red cell exposure. The apheresis team are currently working on an apheresis service for PCH that can deliver this procedure, but it requires funding and trained staff.

Child and adult survival with SCD is improving but there is much work to be done. Transition to adult care (recognised as a time of risk) in WA is a problem as there is no funding for any adult specialised SCD haematology service. The Australian Sickle Cell Advocacy group is available as a support for patients and families.
Australian guidelines and new treatments are on the horizon giving grounds for optimism.
By Mr Peter Ammon Foot Ankle & Knee Surgery


St John of God Medical Centre
10, 100 Murdoch Drive
WA 6150
(08) 6332 6300
(08) 6332 6301
Sexual Health North, in Joondalup, we offer a wide range of services for our patients from the diagnosis and management of STIs, HIV, PrEP, Hepatitis B & C, trans and gender diverse health care for those over 18 years old, genital skin conditions and vulvovaginal medicine. Newer services include the provision of long acting reversible contraception (LARC) including intrauterine deviceshormonal and non hormonal.
As our service grows, we will expand and offer further services. Our clinic strives to create a friendly and knowledgeable service in an open-minded atmosphere. We aim to work with our colleagues in primary care and specialist settings for the total wellbeing of our mutual patients. We would also be happy to take calls about your patients.
MBChB (U. of Auckland), FAChSHM
Dr Christine Dykstra trained and completed her fellowship at Royal Perth Hospital, where she has been a specialist sexual health physician for over a decade. With a keen interest in improving sexual health care in Perth, Christine has provided sexual health medical education at various universities and postgraduate programs in Perth.
Her most recent role in research was as the principal investigator for the Royal Perth Hospital site of the WA PrEPIT trial for the provision of HIV pre-exposure prophylaxis in Western Australia. Having lived in Perth’s northern suburbs for many years, Christine is happy to finally bring specialist sexual health care to the Joondalup and Wanneroo regions.


MBChB (U. of Liverpool, UK), FAChSHM, MRCP (UK), DIP G-U-MED, DFSRH
Dr Michelle Yong initially gained her experience in sexual health and HIV management at Royal Liverpool University Hospital, UK. Moving to Perth in 2012, she continues to develop her clinical skills at Royal Perth Hospital including transgender medicine.
Sexual health issues can feel embarrassing for many patients. Michelle excels at putting patients at ease with her non-judgmental and empathetic manner along with a healthy dose of humour. She would like to put her expertise to good use by setting up specialist sexual health service to serve the communities of the Northern suburbs.
In order to help reduce the rates of STIs in our community, we offer our patients the opportunity for on-site consultation, pathology / investigations , and medication dispensing with many acute STI treatments. For acute STIs, we try to keep fees to a minimum. You can contact our friendly team to discuss your patient’s needs.

Commonly asked questions are ‘When is it safe for patients to resume exercise post-COVID?’ and ‘what are suitable exercise programs for patients not working due to long-COVID?’

Physical activity is a key component of long-term recovery from illness, and it has profound physical and mental health benefits. Patients recovering from COVID will require guidance through a gradual reintroduction of activity, with due consideration given to possible complications.
The RACGP has developed guidelines for all primary care practitioners to assist with safe return of patients to physical activity. In a study of 3000 Australians diagnosed with COVID-19, it was found that approximately 5% continued to experience symptoms after three months.
The World Health Organization has developed a clinical case definition for ‘post–COVID-19 condition’: Post-COVID-19 condition occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually three months from the onset of symptoms that last for at least two months and cannot be explained by an alternative diagnosis.
Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others and generally have an impact on everyday functioning. Symptoms may be new onset following initial recovery from an acute COVID-19 episode or persist from the initial illness. Symptoms may also fluctuate or relapse over time.
Another suggested definition that describes a range of postacute COVID-19 symptoms is ‘chronic COVID-19’ or ‘post–COVID syndrome’; that is, illness extending beyond 12-weeks from initial symptoms. The term ‘long-
Physical activity is important in recovering from COVID-19 and the harms of inactivity during recovery well documented
A GP consultation within six weeks of release from isolation is recommended for all patients providing opportunity for early referral to allied health professionals if required
Exercise prescription for patients with long-COVID or postCOVID-19 conditions but must be done gradually and safely.
COVID’ has been commonly used to describe COVID-19 symptoms following acute illness, irrespective of how long the symptoms take to resolve, and could be used in referring to either of the above two conditions.
Studies have identified that patients are at higher risk of post-COVID-19 conditions if they;
• have experienced severe illness during their acute COVID-19 illness
• have pre-existing comorbidities
• are of older age
• are female
• are high performing in their sport or work role where activities can be taxing
A GP consultation within six weeks of release from isolation is recommended for all patients, in particular those of higher risk as noted. These consultations provide an opportunity to assess for any
reoccurring or ongoing symptoms, the need for additional supports, and to update management of pre-existing conditions or screening that might have been impacted by their illness. This provides an opportunity for early referral to allied health professionals if required
We agree that COVID-19 is multisystem impacting therefore we are aware of the multitude of factors which may present for individuals. The health benefits of being physically active in recovering from illness are well established. Conversely, the harms of physical inactivity have also been well documented since the pandemic began, driving the necessity in provision of guidance, advice and supervision with exercise prescription and gradual return to pre-illness activities.
Exercise is important in recovery for patients with either long-COVID or post-COVID-19 conditions but must be done gradually and safely. The following phases may be implemented if close consideration is given to the intensity and duration of activity prescribed based on the severity of symptom experiences. An individual’s Rate of Perceived Exertion (RPE via the 20-pt Borg Scale) is globally used to monitor such intensity within each phase and can dictate fluid progression or regression through stages during an exercise program as needed.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act. https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Cosmetic, non-invasive treatments for the skin, especially the face and neck, are increasing exponentially throughout the world. Australia is no exception.
Aesthetic lasers have become ubiquitous since the recent downregulation of industry requirements in Western Australia to own or operate these devices. There is a plethora of devices, clinics, and operators of varying standards.
An understanding of this area should assist doctors when asked, to appropriately guide their patients.
Lasers are used for the treatment of a variety skin conditions, depending upon the device and experience of the operator. Tattoo removal and hair reduction are the most common treatments. Other skin treatments include wrinkle reduction, rejuvenation, resurfacing, pigmentation reduction and scar improvement.
The treatment of vascular lesions is less known. Laser treatment of many vascular lesions is a safe, effective, and cheaper alternative to surgery.
Laser emits coherent light of a single wavelength and controlled energy. This light is used as a treatment modality.

Light penetrates variably through the skin, and this is determined by the wavelength and the diameter of the beam.


Demand for non-invasive cosmetic treatments is increasing
Specific Laser treatment targets
haemoglobin
Laser therapy has a role in treating various skin concerns, including vascular lesions.
In 1960, Theodore Maiman developed the first (ruby) laser for clinical application. Then, in 1963, Goldman demonstrated the effects of Maiman’s laser in selective photo destruction of pigmented skin elements such as black hair.
Rapidly, ruby and Q-switched lasers were developed for tattoo removal and pigmented lesions, the argon laser for vascular lesions and carbon dioxide lasers for skin lesion destruction. Ultimately the Nd: YAG laser (1064nm) and the Alexandrite (755nm) were developed.
Both the 755nm and 1064nm wavelengths target haemoglobin. In turn, haemoglobin absorbs the laser light which is converted to heat that diffuses to vessel walls. These walls become damaged and collapse upon themselves and then reabsorbed over several weeks.
The 1064nm laser is usually used for the treatment of vascular lesions
as it is not absorbed by the melanin as much as 755nm, therefore minimising risk of epidermal damage. The 1064nm can be used to treat all Fitzpatrick* skin types.
It penetrates more deeply than 755nm and is therefore used for deeper, larger vessels (up to 3mm in diameter). As haemoglobin absorption of 755nm is double that of 1064nm, it is more effective vessel heating.
The 755nm is appropriate for treatment by experienced operators for vascular lesions in patients with Fitzpatrick I-III only.
Commonly treated vascular lesions include:

• Facial telangiectasia, small, dilated vessels (diameters between 0. 1 and 1. 0mm)

• Leg or ‘spider’ veins. These affect approximately 80% of women with age hormones and genetics as contributing factors. Veins under 2mm will respond best
• Haemangioma – the most common benign tumours of childhood
• Port wine stain – are usually congenital and are composed of ectatic capillary malformation in the upper layer of the dermis
• The laser treatment of vascular lesions is best undertaken by experienced operators using high quality devices in a clinic with excellent quality control.
Alternatives to laser treatment of vascular lesions such as surgery or sclerotherapy should also be considered in the management of patients seeking advice on such lesions.
Any clinic operating a cosmetic laser and undertaking such work should refer the patient to their GP if the lesion the patient is concerned about is not suitable.

– References available on request

Author competing interests – the author owns a non-surgical cosmetic clinic.
Telangiectasia
Author Rosie Richards has written 100 books for Mills & Boon, telling imaginative romantic stories of doctors, nurses, midwives and those in the medical profession.
By Ara JansenSomeone once told Rosie Richards that a surgeon read her books in between operating because they enabled him to relieve stress and get away for a while.
“We absolutely need escapism at the moment,” says the New Zealand author, who writes for Mills & Boon. “I’ve always been a huge fan of the happy ending. Fiction can be life with a feeling of hope and humanity. I want to feel good when I put a book down – or at least hopeful.”
Founded in 1908, Mills & Boon is one of the world’s most successful publisher of romance novels and Rosie, writing as Alison Roberts, is one of their regular and longtime writers who pens novels in their medical romance series.



It’s believed that the first medical themed Mills & Boon romance was 1917’s Days of Probation by Louise Gerard with the first Australian author published being Joan Blair who wrote Sister of the Nelson Ward, published in 1937.
By 1955, the company’s catalogue included a section on doctor stories which suggests these stories had developed into a genre, possibly fuelled by the development of the NHS in the UK and the emergence of medical TV drama such as Emergency Ward Ten. As both the NHS and medical TV shows continued to grow over the coming decades, it has only added fuel to what became called the medical series in the M&B catalogue.
According to M&B, doctors and nurses have long been popular heroes and heroines because they save lives and work in intense and emotional environments, making their stories ideal for drama, romance and the escapism of falling in love.
Though sometimes sneered at for their romantic notions, being lightweight reading and titles like Her Secret Rio Baby, From Nightshift to Forever, Taming the Hot-Shot Doc and Marriage Miracle in Emergency, Mills & Boon releases about 700 new titles annually, sells millions of copies, has millions more read through libraries and books are translated into over 25 languages.
Rosie Richards, who lives in Christchurch, has been writing medical themed romances for M&B for decades and has chalked up 10 million in sales. She writes five books a year – 50,000 words every 10 weeks – and this year published her one hundredth romance for the company.
“When I first came across Mills & Boon, I thought they were all bodice-ripping princes and sheriffs but the medical books were realistic and relatable, a bit like some of those long-running medical TV series,” she says.
“I think one of the reasons my books have been successful is because I know what people are
looking for, because I’m looking for it myself. I’ve not found my happy ending yet and I think romance in your life is important.”
While she loves writing, it’s also Rosie’s job, so she writes every day in order to hit her deadlines. She lived and wrote in France before COVID brought her back to New Zealand.
Around her fourth book, Rosie became a volunteer paramedic for 20 hours a week which gave her an added insight into the technical aspects of the job, enabling her to write with practical understanding. Her father and ex-husband were both doctors which also added to her knowledge base.
While medical experience is not essential, M&B has current and previous doctors, nurses, paramedics, midwives and physiotherapists authoring books for them. Others just love writing romances in a medical setting and thrive on doing the research. While the company welcomes a diverse author base, most of the M&B authors are female, though there has been the odd male.

“I have always wanted to be authentic,” says Rosie, who is in her 60s. “Doctors have read my books and I have never had complaints about inaccuracy.
“My writing has always been very instinctive. I have a reader which sits
on my shoulder and if they don’t like what’s happening, something has to change. There’s a movie director on the other shoulder who is arranging the scene, while I’m inside the characters’ heads. So, I juggle all of that and somehow it comes together.
“People want the same thing but different, which is the challenge for us as authors. I challenge myself to improve my writing and do something that’s different each book. I couldn’t do the same thing over and over again.
“I have great fun playing with timing, characters and turning things around to make them interesting. The secret baby trope is popular, and I think I was the first romance author to turn that around with a character who had donated her eggs to a friend and didn’t know about the baby.
“Because these books are set in the medical arena with patients, you can deal with darker and heavier issues compared to other romances, like a GP who has Huntington’s and therefore won’t get involved with anyone. But you can put a character in his path which changes his outlook or forces people together or creates an energy that sends them in different directions.”
The Vet’s Unexpected Family is Rosie’s one hundredth book and features a celebrity vet instead of a doctor and an overweight heroine. She’s also been interested to watch the cultural changes which affect writing and how Mills & Boon books have reflected that.
Now it’s acceptable to have samesex couples, mentions of IVF, characters in wheelchairs or even throuples, which weren’t part of storylines when she started writing.
“It’s a great career and I have made a living from it,” says the mother of one and former primary school teacher. “I’m also writing a mainstream romance and have set it in a small, old town in France, which is the home of my soul, as opposed to New Zealand, which is the home of my heart.”
For those wanting to inject some romance in their lives or just escape between patients, there are more than 1250 Mills & Boon medical romance titles available in Australia.
For the first time, Dr Mike Civil gets to review a fully electric car, and now he feels one beckoning – when he finds room in his garage.
Well, this is a first for me. Having been someone who has ranted on and on about the aural delights of rumbling V8s or blow-off valves on highperforming turbo-boosted rally cars, it is time to go over to the dark (or should that be green) side.
One of the first (and potentially most important) impressions about the BMW i4, is that it does not yell at you “I’m an EV!” The ‘electric’ side of the i4 is very understated. It looks just like a normal BMW.
A closer look at the front grill will reveal many missing holes! Any hopes of aggressively designed exhausts will be dashed immediately. Nothing to see there! But as a whole package you would not pick this as an electric car.

The control features will be familiar to anyone who has driven a BMW. Yes, the touch screen is longer and larger than previous BMWs, but again it is somehow understated. There are touch screen controls, but there is still the reassuring dial-up control by our auto box gear lever. You still have familiar electric window controls, indicators, windscreen wipers, cruise control, etc.
Time to turn this novel experience on.
We have a few ‘bars’ of sound, not really sure how to describe them, and you know that things are now active. No need to wait for engine oils to warm and circulate, we are good to go.

As expected, it is all eerily quiet, we just glide away. At low speed this is particularly noticeable. Are we still switched on, or just rolling down the driveway? But yes, we are motorvating. Once the car is moving a little more rapidly, we have road noise and wind, but that is barely noticeable. Chatting to someone on a mobile phone while driving will not be taxing my aged hearing.
The car doesn’t feel heavy, it feels responsive and pin sharp. We have a choice of driving modes, as always in a BMW. We are still in “Comfort”, but we have the joys of “Sport” and the responsible “Economy.”
One immediate difference in this car over a petrol-driven sibling is the braking effect of the electric motors. When driving in ‘D’ on the auto box, the car will glide, if coasting off the accelerator, like a petrol version, but less than expected and this is especially noticeable at slower speeds.
It is not a concern, or problem, it is just a little different. If you shift the auto box over to ‘B’, this activates the energy charging effect that the electric motors give when breaking. I guess this is the equivalent of the Kinetic Energy Recovery System (KERS) on Formula 1 cars. When in B (Battery), electric motor breaking is much more noticeable, but again, when familiar with it, it is not an issue and those batteries will last just that little bit longer.
Speaking of batteries, what is the range? Well, the helpful display tells me we have 500km available on this fully charged battery. I drove around all weekend and covered a fair number of kilometres and didn’t approach half charge. There are various different charging leads in the boot – one for household standard sockets, one for BMW charging units and there is a socket on the car for the fast-charging filling stations. I did have a go charging at home, but mainly to see what was involved. More of that later.
Back to the car. The driving experience, from a performance perspective, was excellent. Great ride, smooth, precise and confidence-inspiring.
Nothing out of the ordinary from a BMW, but, even in Comfort mode, the acceleration was very impressive, back up to speed limits
in the blink of an eye. Move on to Sport, the touch screen dash develops its red-mist colour, and suddenly the performance jumps up a notch, speeding-fine territory rapidly becomes licencelosing territory. Not quite “to infinity and beyond” but very impressive acceleration, all the same.
Of course, Sport mode and a heavy right foot will see those batteries drain faster than Comfort or Economy mode, but nice to know that the all-important driving experience is still very positive. I just can’t get over the fact that this car looks like a normal BMW, certainly goes like a high-performing BMW, is as well-appointed as a normal BMW, but it gets its energy from the grid.
When back from the dizzy heights of great performance, it is time to plug her into the wall. When manoeuvring the BMW at home, there are a plethora of camera angles and mirrors to help you reverse.

Our new home has a narrow driveway, and our golden retriever is curious as to what Dad has just driven up in. The clever brain in the car will not allow me to run over our beautiful dog, fortunately! After the alarms say she has got too close, the car brakes!
Another ‘driver assist’ gadget was the step-up from old-fashioned
cruise control. When going down the freeway on the way home, the fancy cruise control will not only manage your speed, but will also stop you drifting off course, and tailgating the car in front is definitely off the agenda.
You only need to offer little input for the car to drive itself. The car (and my passenger) may get a little nervous if you take your hands off the steering wheel – the car just prompts you to put your hands back! I know selfdrive cars will be common at some stage in the future, but hopefully by then I will have lost the ability to ‘enjoy the drive’ and won’t be bothered. For now, my interest in all things four-wheeled will always direct me to driver experience, not just the going from A to B.
Back to charging – obviously, I only have the car for the weekend, so no BMW charger gadget on the wall at home. I plug into the trusty wall socket. It takes a while (overnight) but charge she does.
We have recently had a large solar array installed at home and this is part of my interest in wanting to review a quality EV as I will be going down the electric car vehicle path at some stage. At present, I still have a few too many toys in the shed to justify an extra vehicle. But it isn’t going to be too long before I hang up the racing boots. An EV will beckon then.
Having been unimpressed with other manufacturers offerings in the EV space, I had been patiently waiting for the right car to come along. The technology has been well tested by others and range has come a long way (to excuse the pun). Now the latest tech is in a quality package and BMW still remembers the importance of driver experience.
Just in case you were wondering, my Evo 9 went a few months ago, after our run in Targa Tasmania. But there is still a classic 1970 Capri Perana and a Birkin Clubman sitting in the shed to tempt me out on a petrochemical dash.
But when one of those goes to its next owner, I know what will be taking its place and being plugged in – the BMW i4.

This tongue-in-cheek name coined by founder surgeon Philip Childs in 2000 hints at the passion behind people’s drive to make wine in this beautiful part of the world.

The winery, located on Harman’s Mill Road, is now in the hands of new owners Matt and Clair Holden who have maintained and improved on the overall quality of the wines. Grapes are sourced from five longstanding contracted growers in the Margaret River appellation ensuring consistency and stability.
Current winemaker is Kate Morgan whose expertise and experience is widely acknowledged in the wine industry. The five wines tasted all impressed with their distinctive varietal characters and overall deliciousness, so typical of the Margaret River region.
There was no hardness or harshness anywhere to be seen. Thankfully, alcohol levels have been kept to modest levels.
Review by Dr Louis PapaeliasLovely and plentiful aromas of lychee, citrus and grassy gooseberries. This is a delicious and refreshing drink. I am an unashamed fan of young wines and while it will keep, my preference is to enjoy the attractive note that it has to offer right now. 11.5% alcohol, $24.99.
With its faint coppery tinge, this has real mouthfeel thanks to a touch of oak fermentation of the skins. There is a pleasing texture underlying the citrussy freshness. A genuine alternative to chardonnay as a food wine. Like the previous wine, very enjoyable right now. Alcohol 13%, $24.99.
This has lifted aromas of peach and grapefruit citrus with a background of oak ferment. Flavourful and crisp. At a modest 11.5% alcohol it is satisfyingly restrained and a joy to drink now, $39.
This soft attractive wine avoids the touch of hardness that I often see in Margaret River Shiraz. It has a lovely plumminess that is gently balanced by a background of fine French oak. Savoury spice is there aplenty. Overall, a very satisfying and elegant shiraz which finishes long on the palate. 14% alcohol, $39.

A flagship wine coming from a cool vintage in Margaret River. This has all the hallmarks of what is so distinctive about Cabernet from this area. Vibrant fruitiness of cassis and plums, a lick of olive and a fine tannin structure that gives freshness and backbone to the overall finish. Beautifully handled and a pleasure to drink now and in the future. 13.5% alcohol, $59.




















