14
Leading the way in AI
The Mayo Clinic, in the U.S., is building one of the world’s largest repositories of data to fuel the development of AI solutions. It’s starting with 11.2 million records culled from its own patients.
Page 5
Fraser Health’s AI assistant Fraser Health, in BC, has deployed AI-driven intelligent assistants that help clinicians and staff cut the time needed to answer questions about using the organization’s new EHR.
Page 8
Analytics at the UHN
Data is so entrenched in everyday activities at the UHN, that it has launched a staff data literacy program. Moreover, new leaders entering the organization are given an introductory course on data literacy.
Page 18

New PET-CT reduces full-body scan to 14 minutes
St. Joseph’s Health Care London, in London, Ont., has deployed the state-of-the-art
machine is fast -- decreasing the time it takes for a scan from 45 minutes to less than 14 minutes, from head
toe. Patients are exposed to less radiation, and the ability to precisely detect disease and tiny abnormalities is said to be unparalleled.
RNAO, PointClickCare digitize LTC resident assessments
BY JERRY ZEIDENBERG
Apartnership between the Registered Nurses Association of Ontario and PointClickCare, of Toronto, has been shifting the resident assessments done in Ontario’s nursing homes from paper to digital.
In the process, the transformation has resulted in faster and more accurate assessments, as nurses and other professionals make use of automated and standardized electronic forms.
It has also led to remarkable rates of satisfaction from the users.
“Everyone I’ve talked to has had a good experience with the digital admission tool,” said Tess Romain, president and CEO of Partners Community Health, which opened Wellbrook Place, two long-term care homes in Mississauga, Ont.
With a combined capacity of 632 beds,
the two sites were opened last November. By the end of February 2024, the organization had filled 550 of those beds.
“The [PointClickCare] system is very efficient, and the nurses just have to follow the prompts. That way they don’t miss any questions,” said Romain.
The patient assessment tool is integrated into the PointClickCare resident management system, an electronic patient record solution for LTC. Romain noted that PointClickCare is fully mobile and can be used by staff and clinicians on their notebook computers and smartphones.
Using digital assessments, nurses at Wellbrook Place can bring in new residents faster than ever before.
Moreover, the solution offers a dash-
board, providing long-term care managers and planners with real-time information about the residents coming into their homes, comparisons over time, and comparisons with other facilities if the organization has more than one site.
Nurses at the facility told Romain that they wouldn’t have been able to move 550 residents into the new centre – the largest LTC in Canada – so quickly without the use of an automated admissions tool. “It used to be done on paper,” she said. “There’s no way they could have brought in so many residents using pen and paper.”
On the regulatory front, long-term care homes in Ontario and most other jurisdictions must send data from various kinds of assessments to government health departments. For years, it was done on paper.
In addition to information that must be
CONTINUED ON PAGE 2
Omni 2 Legend PET-CT from GE Healthcare. The
to
SEE STORY ON PAGE 14.
PHOTO: COURTESY ST. JOSEPH’S HEALTH CARE, LONDON
INSIDE:
Publications Mail Agreement #40018238 FEATURE REPORT: ELECTRONIC HEALTH RECORDS – SEE PAGE 18 CANADA’S MAGAZINE FOR MANAGERS AND USERS OF INFORMATION SYSTEMS IN HEALTHCARE VOL. 29, NO. 4 MAY 2024 PRECISION MEDICINE
PAGE
RNAO, PointClickCare digitize and improve LTC resident assessments
collected for government purposes, most LTC homes have strived to incorporate evidence-based practices into their documents, to create the best care plans for their residents.
Historically, this was done on an ad hoc basis, with many organizations dedicating staff and countless hours to re-inventing the wheel – basically recreating what others had done, with their own spin on it.
“Staff would be assigned to research and create assessments,” said Stuart Feldman, senior vice president and market leader, Canada, at PointClickCare. “The efforts were not always well organized, and what they came up with was not always long-term care based. They’d take what they could find. And it could take hundreds of hours.”
In response, in 1998 the RNAO’s CEO, Dr. Doris Grinspun, envisioned a program that would create Best Practice Guidelines (BPG) for use throughout the province.
It was funded by the Ontario’s Ministry of Health and launched in 1999 to provide the best available evidence for patient care
across all health sectors and settings, with more than 50 guidelines developed to date.
While still on paper, these assessments became known as the best available.
“They’ve had tons of success with them, including outside of Ontario,” said Feldman. “They’re used in many non-Englishspeaking countries,” which acquire them and have them translated.
What PointClickCare did, however, was to start digitizing these evidence-based assessment tools and incorporating them into its own system, which is widely used in the nursing home and post-acute care sector.
In Canada, PointClickCare is deployed in 2,600 homes, with very extensive usage in Ontario, Alberta and British Columbia.
PointClickCare is also deeply entrenched in the United States, where it has 27,000 deployments in LTC homes.
In the U.S., care facilities have long been incentivized to include digital assessments in their systems as a quality and performance measure. As a result, PointClickCare has been offering the feature there for years and has expertise in integrating them with its clinical and administrative systems.
Its recent partnership with the RNAO
Creating the pathway to connected care.

has been a quick success. In 12 months, the digitized admissions tool has been adopted by nearly 170 long term care homes in Ontario. “One-third of the province is already using it.”
“We’re told that it’s reducing admission times by 30 to 60 minutes for each resident,” said Feldman. “And the homes are starting with best practices right at the gate.”
Under the agreement with the RNAO, the association – along with partners like InterRAI – creates the content and PointClickCare produces digital versions that are integrated into the electronic patient record system.
It’s a three-year contract that extends until March 2026. The goal at that point is to have all 600 or so of Ontario long-term care facilities using the tool.
This digital solution is known as RNAO Clinical Pathways. As the RNAO website notes, “RNAO Clinical Pathways are based on BPGs (best practice guidelines) and delivered by PointClickCare’s new Nursing Advantage platform. They promote safe, high-quality resident care, improve staff efficiency and support legislative and regulatory compliance.”
Feldman said discussions are under way with other provinces, to introduce the computerized tool there, too. “Many Ontario operators have homes in other provinces, so they know the benefits,” he commented.
Deborah Johnston, director of Canadian healthcare strategy at PointClickCare, observed that standardized assessments are powerful tools because “they let the data tell the story” by answering the key questions.
Using standardized assessments, clinicians are no longer using only personal observations, but can rely on time-tested best practices. “It’s evidence-based care,” she said.
The admissions assessment tool is one of several that’s currently available in digital form. Others include:
•Pressure ulcer risk scale
•Palliative performance scale
•My personhood summary
•Delirium screening, assessment and management
•Resident and family centred care
•Falls screening, assessment and management
•Post falls assessment
•Pain screening, assessment and management
•Opioid therapy
Coming soon, Johnson said, are:
•Heat risk assessment
•Re-admission assessment
•Palliative screening assessment and management
•End of life care
•Dementia screening assessment and management
•Depression screening assessment and management
PointClickCare has been training new users on the tools in waves, with 30 to 70 customers congregating at one time, on three occasions each year. They work with their peers and with RNAO trainers and become well versed in the use of the RNAO Clinical Pathways.
Publisher & Editor
Jerry Zeidenberg jerryz@canhealth.com
Address all correspondence to Canadian Healthcare Technology, 1118 Centre Street, Suite 204, Thornhill ON L4J 7R9
709-2330. Fax: (905) 709-2258. Internet: www.canhealth.com. E-mail: info2@canhealth.com. Canadian Healthcare Technology will publish eight issues in 2024. Feature schedule and advertising kits available upon request. Canadian Healthcare Technology is sent free of charge to physicians and managers in hospitals, clinics and nursing homes. All others:
Office Manager Neil Zeidenberg neilz@canhealth.com
Contributing Editors
Dianne Craig dcraigcreative@yahoo.ca
Dianne Daniel dianne.l.daniel@gmail.com
Dr. Sunny Malhotra Twitter: @drsunnymalhotra
Norm Tollinsky tollinskyn@gmail.com
Art Director
Walter Caniparoli art@canhealth.com
Art Assistant
Joanne Jubas joanne@canhealth.com
Canada. Telephone: (905)
$67.80 per year
Registration number 899059430 RT. ©2024 by Canadian Healthcare Technology. The content of Canadian Healthcare Technology is subject to copyright. Reproduction in whole or in part without prior written permission is strictly prohibited.
requests for permission to Jerry Zeidenberg, Publisher. Publications Mail Agreement No. 40018238. Return undeliverable Canadian addresses to Canadian Healthcare Technology, 1118 Centre Street, Suite 204, Thornhill ON L4J 7R9. E-mail: jerryz@canhealth.com. ISSN 1486-7133 CANADA’S MAGAZINE FOR MANAGERS AND USERS OF INFORMATION TECHNOLOGY IN HEALTHCARE Volume 29, Number 4 May 2024
($60 + $7.80 HST).
Send all
CONTINUED FROM PAGE 1
Tess Romain, CEO, Partners Community Health
2 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024 www.canhealth.com Funded by the Government of Canada
Infoway is at the forefront of advancing connected care across Canada, harnessing digital solutions to improve care coordination, streamline communication, and empower patients with improved access to health information. Read our Roadmap to learn more.
SAVE THE DATE
October 19, 2024

Imaging Forum 2024: Meaningful Innovations in Radiology
Introducing a new educational experience coming soon to your location in Toronto and Vancouver, Canada. Renowned global speakers and experts in CT, MRI, and Healthcare IT will share their experiences, insights, and perspectives on the latest applications and AI-assisted technologies enhancing productivity and patient care.
Canon Medical is committed to AI innovation through our solutions powered by Altivity.
ca.medical.canon
Click here to learn more about our upcoming education event!

The Bridge to Patient Care
Close the gap between and IT with an imaging solution that delivers on both sides of the business.
Integrated seamlessly with your EHR, our Enterprise Imaging latform enhances the EHR by providing clinicians, across specialties with all of the pat ent’s imaging data enabling a comprehensive and historical view of the patient’s imaging history. Expedite image access while optimizing system efficiency and performance.
more at: agfahealthcare.com That’s life in flow.
Learn
EHR benefit realization within reach with right evaluation framework
BY MEGAN STOWE
After adopting new digital practices, healthcare teams start to experience some early benefits that come with an electronic health record system (EHR), including better connectivity and information sharing. To unlock the full breadth of benefits requires an evaluation framework to drive value for patients, clients, families, healthcare teams and the wider healthcare system.
The Clinical and Systems Transformation (CST) project, in British Columbia, is considered one of the largest Oracle Health programs in North America in terms of scope (i.e. functionality).
The project’s clinical information system has been implemented at more than 46 healthcare sites to over 42,000 users. As a joint initiative between Provincial Health Services Authority, Vancouver Coastal Health and Providence Health Care, its project board recently appointed a team independent of the project itself to develop an evaluation framework.
The resulting framework, including everything from clinical user experience to quality and safety, reflects these organizations’ shared healthcare priorities in alignment with the Institute for Healthcare Improvement’s Quintuple Aim. Widely referenced within healthcare, the Quintuple Aim is a go-to imperative for value-based care.
By leveraging this framework, the evaluation team distilled hundreds of possible performance indicators down to several dozen of the most relevant to healthcare priorities and then applied select metrics. Their
AI
at
work incorporated a combination of industry-standard benchmarks with recommendations from peer-reviewed health research.
Many performance indicators were drawn from benchmarks upheld by professional associations and practice institutes, an example being computerized provider order entry (CPOE). This refers to the use of electronic ordering by healthcare providers, which has known benefits for medication safety when completed at a rate of at least 85 percent; for CST Cerner users, the average CPOE rate recorded over a six month period was 95 percent.
To evaluate patient experience, the team looked at the volume of unnecessary lab tests, a known healthcare system issue with a potential harmful impact for patients and waste of health system funding. At relevant sites using the CST Cerner system, EHR-enabled practices were shown to reduce the number of redundant lab tests by nearly 25,000 per year.
The evaluation team also looked closely at transitions of care, i.e. patient handover or discharge, which requires accurate and timely communication to avoid adverse medical events and readmissions. Their research examined indicators such as percentage documentation of discharge instructions and usage of digital handover tools such I-PASS (Illness severity, Patient summary, Action list, Situation planning, and Synthesis) used by providers.
Dr. Sean Virani is vice president, Medical and Academic Affairs for Provincial Health Services Authority. He also practices as a physician and program director at Providence Health Care’s Heart Centre at St. Paul’s Hospital.
According to Dr. Virani,“My ability to document transitions in care notes into one electronic health record wasn’t possible before we introduced CST Cerner.”
He added, “The electronic health record system is integrated between our three health organizations so that the patient’s entire healthcare team has access to the right information at the right time.
“For providers, having this type of visibility into the patient’s journey across our digitally connected health organizations marks such a significant improvement, it’s hard to fully quantify the positive impact,” noted Dr. Virani.

For other metrics with inherent nuances and emerging standards, such as within health equity, benchmarks may not yet be widely accepted. To add further complexity, many benchmarks vary according to care setting, a simple example being medication reconciliation times within acute, outpatient or longterm care.
Certain performance indicators are also shifting with medical advances and changes in patient populations, highlighting the importance of incorporating the latest evidence-based research and literature. Despite incongruencies within healthcare metrics, organizations should continue to forge the path of evaluation with transparency while committing to refining metric standards over time.
the Mayo Clinic: The leading edge of curating data
BY JERRY ZEIDENBERG
ORLANDO, FLA. – We know that the usefulness of AIdriven solutions is tied to both the quality and quantity of the data used. It’s not just a matter of garbage in, garbage out. You’ve got to have a massive amount of high-quality data to train the algorithms – that’s how to get results that will work with a broad range of patients. For this reason, the Mayo Clinic is building one of the largest repositories of clinical data in the world.
“Everything starts with data,” asserted Dr. John Halamka, president of the Mayo Clinic Platform, which is focused on transforming healthcare through the use of AI, connected devices and a network of partners.
He explained in a presentation at the recent HIMSS conference that you need accurate data and a lot of it. A colleague at another organization told him that his facility had 5,000 patient records with which they will build AI algorithms. “That’s not enough breadth,” warned Halamka.
For its part, the Mayo Clinic has 11.2 million patients with electronic records.
And it’s not stopping there. The hospital chain is building a global, federated network of partner hospitals and patient records that can be drawn upon for building apps.
Already, it has 242 algorithms under development. The goal is to improve the art and science of medicine around the world.
“You need a global network to deliver on a global basis,” said Halamka. So, the Mayo Clinic has been creating alliances with other large hospitals and health organizations to share data. They include Toronto’s University Health Network, along with the Apollo chain of 73 hospitals in India and the Albert Einstein hospital in Brazil.
The data are de-identified and they never actually leave the host site – instead, metrics about the anonymous patients are shared.
That protects patient privacy. And the sharing of data over a wide range of geographies and ethnicities helps avoid bias in the data, as much as possible, when building AI models.
Nevertheless, said Halamka, “every algorithm will have a bias. We create and test the algorithms, recognize the bias, and then adjust.”
Another important benefit felt indirectly by patients in Canada as it contributes to the wider economy is cost savings. Some costs related to quality and safety are difficult to quantify (consider loss of life in the case of clinical intervention).
Nonetheless, industry costing methods applied to the patient journey and experience pointing to factors like fewer readmissions have useful applications. The number of lab tests avoided by removal from electronic orders at CST Cerner live sites demonstrated annual cost savings of $1.3 million per year.
With reduced medication errors associated with CPOE adoption, the evaluation team estimated current cost savings of $5 million to $7.5 million per year across all sites using the CST Cerner system.
Referring to researched costing methods, the CST project team uncovered cost savings examples within its operations, a significant amount linked to streamlined documentation and fewer registration errors within patient health information. Additionally, efficiencies realized in the pharmacy supply chain were estimated at $1.6 million annual cost savings within balance sheet adjustments.
Much like EHR uptake in this country, there is no one-size-fits-all approach to evaluation and benefits realization. By sharing findings and best practices to develop a clear evaluation framework, health organizations have an opportunity to move the needle forward and continue striving for better results.
Megan Stowe is chief, Regional Digital Solutions, Provincial Health Services Authority.
and building apps
For example, the Mayo Clinic has a cardiology algorithm that can predict patient mortality. “It’s very accurate for people with low BMI, but not for those with a high BMI. Is it ethical to use it?,” he asked.
“Yes, for people with low BMI. That’s why you have to test and account for biases.”

And in the early days of generative AI – which is right now – it must also be recognized that the quality of genAI depends a great deal on the prompts or questions that are asked. Halamka talked about one instance of generative AI where “it could be accurate, or it could kill the patient.”
He cited the case of a 59-year-old patient with chest pain, shortness of breath and left leg radiation. ChatGPT was asked for a diagnosis and responded that the patient had likely suffered a mild cardiac infarction and that anti-coagulants should be introduced immediately.
ChatGPT was then asked, what possi-
ble diagnosis may have been missed? It responded with “aortic aneurysm”.
The problem, however, is that if only the first diagnosis had been followed, anti-coagulants could have killed a patient with an aortic dissection – it would have aggravated the bleeding.
Such hair-raising possibilities and serious risks beg the question, where should organizations start when creating AI-powered apps?
Best to start with low-risk apps, said Halamka, suggesting things like clinical documentation as the low-hanging fruit.
“With ambient listening, we’re reducing the pajama time for clinicians who otherwise spend hours documenting at home.”
He added, “It works well. You read the notes, edit and sign off. It’s low risk and high-benefit, even if it misses something.”
Email management is another useful app – AI can scan one’s emails and draft responses, saving the user a great amount of time. A clinician can then check the AI’s work, edit as needed, and send the emails off.
AI can even improve the writing of people – especially those who studied the sciences in school rather than liberal
John Halamka
NEWS AND TRENDS
Megan Stowe
CONTINUED ON PAGE 22 www.canhealth.com MAY 2024 CANADIAN HEALTHCARE TECHNOLOGY 5
Clinical informatics team at STEGH transforms hospital’s processes
ST. THOMAS, ONT. – The team supporting digital health transformation at St. Thomas Elgin General Hospital (STEGH) was recently enhanced to meet the demands of the facility, which serves a growing population and, increasingly, more medically challenging patients.
In light of ongoing challenges, there is a growing demand for digital innovation, creative thinking, and transformative solutions.
Similar to many hospitals, digitizing solutions and thinking of new ways to meet patient care needs, creating efficiencies for clinicians, and staying current with technology has become paramount. While this work is essential, the task of attracting appropriate individuals and aligning people, processes, and technology can present its own set of challenges.
To meet these challenges, STEGH has been on a continuous journey to re-build and create a highly skilled Digital Health Team that understands the interplay of people, process and technology, while putting the needs of patients first. Ultimately, the end goal is to adopt new technology that contributes to the evolution of healthcare.
Over the last eight months, STEGH’s Digital Health Team had the opportunity to review its staffing compliment, the composition of the team, and the skill set required to support the hospital.
Additionally, this allowed the team time to step back, pause, reflect and understand the current and future state business requirements, potential gaps, opportunities, and clinical/hospital workflow.
To support this review, an in-depth assessment based on STEGH’s Lean philosophies was conducted to determine if the team was performing the right work, building digital capacity, leveraging the right tools and technology, and ultimately meeting the needs of patients and clinicians.
One of the guiding principles underpinning this change was to create a Digital Health Team that sees technology through the eyes of patients and staff.
This allowed the team to be reminded, in today’s current environment, what it is


like to work at the bedside, how technology needs to be incorporated into clinical workflow, and the impact of change for clinicians and patients.
STEGH’s Digital Health Team has four clinical informatics members, all regulated healthcare professionals comprised of nursing staff with a personal stake in digital health. The harmonization of the two has been beneficial and impactful as the team has a thorough understanding of the issues faced by clinicians, clinical/hospital workflow, and pain points. They’re also able to offer solutions that benefit the care team.
To further enhance and support the relationship between the Digital Health Team and clinical staff, the Digital Health Team conducts regular rounding in clinical areas and attends huddles (another Lean principle at STEGH).
These strategies have allowed the team to provide real-time support, address issues in the moment, and explain the “why” and benefits of technology (patient safety, improved communication, transparency of information, creating standards and efficiencies).
“Creating this team definitely took some time, but the benefits are paying off,”

said Jeanette Fidler, manager of Digital Health. “The organization is seeing the growth of the team, and more importantly, understanding the benefits of leveraging digital health tools. Staff are asking to digitize their existing paper processes and inquiring about how to leverage our Electronic Health Record (EHR) to support workflows. This is music to our ears.”
The EHR is a large investment for most organizations, so it is important to have a
The Digital Health Team converted many of the manual reports to electronic format, leveraging data in the EHR.
strong Digital Health Team in place to evaluate current use, identify opportunities for improvement, and implement solutions that lead to improved patient care and more efficient clinical workflows.
The work that has been completed over the last eight months is impressive considering the team consists of just four individuals. “Leveraging the hospital’s Lean principles and core values, like account-
ability and collaboration, has been instrumental in our success,” said Monica Olanski, VP Patient Care Services and chief information officer.
Some of the accomplishments over the last eight months include implementing Ocean in the Mental Health Program, improvements to admission and discharge processes, an electronic dashboard to support communication between Diagnostic Imaging I and the Emergency Department, specimen collection and barcode scanning, and automatic microbiology result notification to Infection Prevention and Control.
Many of these improvements have been achieved through maximizing the use of existing or previously unused functionality within the Oracle/Cerner EHR.
A review of clinical reporting found many areas of the organization were reliant on manually tracking for their metrics. The Digital Health Team converted many of these manual reports to electronic format, leveraging the data found within the EHR.
Improved analytics and reporting enabled clinicians to gain valuable insights from the data within the EHR and aided in their decision-making and process improvements.
“Embarking on this digital health transformation represents a pivotal step for St. Thomas Elgin General Hospital and our patients, said Dr. Samer Chehade, Internal Medicine and Physician Digital Lead. “Despite the inherent challenges, this transition is fundamental in enhancing patient care and operational efficiency. It’s a journey we’re committed to, and I’m thrilled to be part of this transformative team.”
As the hospital continues to grow and evolve, STEGH is now in a better position to embrace technology and implement in a timelier and more effective process.
“While there is always room for improvement, STEGH is definitely heading in the right direction, and we look forward to our continued digital and transformational journey to meet the evolving needs of our patients, staff and community,” said Olanski.
Widget mania hits radiology, with widgets giving access to AI results
BY JERRY ZEIDENBERG
Radiology Partners, the largest physician-owned radiology group in the United States, reads 53 million exams a year. Of those, 20 million are now being run through AI applications, with the results sent back to radiologists.
While those results are useful, it’s important to shield referring physicians from them before they’ve been reviewed by the radiologists.
“AI systems are not correct 100 percent of the time,” said Dr. Kent Hutson, a neuroradiologist and director of innovation clinical operations at Radiology Partners. Dr. Hutson spoke at the RSNA conference in Chicago last November.
“So, we try to keep that information in front of the radiologist and not until the radiologist has reviewed the study do we release the information to the clinician. And if the [AI] information is wrong, we don’t let them see it at all.”
Dr. Hutson explained that you might have a patient in the Emergency Department with a broken leg. The radiology system might be using an AI algorithm to determine whether there’s really a fracture. However, if the algorithm gets it wrong, and says, “no fracture”, the ED physician might act on that information if he or she has access to it.
“It’s called automation bias, and the tendency to believe in AI [by some] will tend to make them act on that,” said Dr. Hutson. “It may not have been inter-
preted yet by a radiologist, who is really the one that is responsible for the interpretation of that image.”
For that reason, radiologists at Radiology Partners have a widget on their desk-
“AI systems are not correct 100 percent of the time,” so the data isn’t released until reviewed by a radiologist.
tops that provides access to the AI interpretations of images. The widgets give them and them alone access to the AI results.
Or as Dr. Hutson put it, “It’s for the radiologists’ eyes only.”
In addition to yes/no answers, the
widget will also give the radiologist additional information, such as confidence levels in the answers.
But the widgets are creating their own challenges for radiologists. With so many AI applications being used, from so many different vendors, there can be many widgets on the desktop. “We’re beginning to experience widget mania,” said Dr. Hutson.
The logical solution, he said, will be to create one widget that rules them all.
That will require the AI vendors to start using standards, so their solutions can communicate in a common way.
“That sounds like 30 years ago, when we were starting to use DICOM to bring the images of different vendors into the PACS,” said Dr. Hutson.
NEWS AND TRENDS
Dr. Samer Chehade Jeanette Fidler
Monica Olanski
www.canhealth.com 6 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024

























Where cancer and care connect.









Personalized cancer care through innovative technologies and intelligent data management



GE HealthCare's oncology solutions help cancer care providers gain the upper hand. At GE HealthCare,
Collaborative care with smart workflows




Broad access to precision care



Care that has no limits


© 2024 GE HealthCare Technologies Canada. GE is a trademark of General Electric Company used under trademark license. JB01064CA
we are committed to supporting clinicians with flexible, comprehensive and personalized solutions through every stage of the cancer care.
Canadian studies improving care for prostate cancer patients worldwide
BY LISE DIEBEL
Hamilton Health Sciences (HHS) researcher Dr. Gregory Pond is the lead statistician and co-investigator for two clinical trials that are transforming the way prostate cancer is managed around the world. Both multi-centre studies used magnetic resonance imaging (MRI) to improve the diagnosis and treatment for men going through a prostate cancer diagnosis.
MRI uses a powerful magnet and radiofrequency waves to make cross-sectional images that can show cancer missed by other tests. It can help identify the size and location of cancer and whether it has spread; it can also help specialists plan treatments such as radiation therapy.
The first study, called ASIST, ran from 2010 to 2015. It examined whether MRI found additional high-risk cancers when used with the standard-of-care systematic biopsy, where 10 to 12 tissue samples are taken from random places in the prostate to check for cancer.
Due to the positive results observed in ASIST, a second study, called PRECISE, ran from 2015 to 2017. It studied whether MRI could determine if a biopsy was actually needed.
Improving how prostate cancer is diagnosed: One in eight men will be diagnosed with prostate cancer in their lifetime, making it the most common cancer to affect men in Canada, according to the Canadian Cancer Society.
Suspected cases of prostate cancer are

Mtypically identified through a prostate-specific antigen (PSA) blood test or rectal exam by a family doctor. In Canada and many parts of the world, a systematic biopsy is the standard of care for helping to diagnose prostate cancer.
“A biopsy is a very invasive procedure, and because these 10 to 12 samples are taken randomly, there’s still a risk of missing cancer,” said Pond, director of the Escarpment Cancer Research Institute (ECRI), a joint institute of HHS and McMaster University. Based at HHS Juravinski Hospital and Cancer Centre (JHCC), ECRI’s work focuses on research that has an impact on patient outcomes.
Biopsies can cause side effects including
rectal bleeding, blood in the semen or urine, difficulty urinating, and infection, including potentially deadly sepsis in rare cases.
The ASIST and PRECISE studies are playing a major role in changing the pathway for these patients for the better, said Pond, who is also an associate director of the Ontario Clinical Oncology Group (OCOG) based at JHCC, which ran and sponsored both the ASIST and PRECISE trials.
Running these trials required a large team at OCOG, said Pond, who is also a professor in the oncology department at McMaster and an Ontario Institute for Cancer Research (OICR) investigator.
OICR is a cancer research and development institute dedicated to the prevention,
early detection, diagnosis and treatment of cancer, with members across the province, including Hamilton.
ASIST-ing in finding the best pathway: ASIST was a randomized clinical trial involving 273 patients with prostate cancer. It aimed to determine whether using MRI in addition to a systematic biopsy guided by ultrasound could detect prostate cancer that was at risk of developing into aggressive disease at a different rate than when using ultrasound-guided biopsy process alone.
The study’s findings showed that MRI could potentially be used to help decide which patients would benefit from aggressive treatment versus which patients would be better suited for regular monitoring, since many prostate cancers aren’t aggressive.
PRECISE change for the better: PRECISE was a randomized clinical trial involving 453 men. It used MRI to determine that not all men suspected of having prostate cancer need to undergo a biopsy. In addition, using an MRI allowed for two to four tissue samples to be targeted, instead of 10 to 12 random tissue samples, meaning they were taken from areas that MRI identified as appearing cancerous.
This targeted approach means that even in patients who do need a biopsy, it is less invasive, allowing for a faster recovery and fewer side effects. As well as improving the ability to identify which men had high-risk disease, the study also helped lower-risk patients avoid radical treatment.
“This work is changing the diagnostic pathway, worldwide, for all men suspected of having prostate cancer,” said Pond.
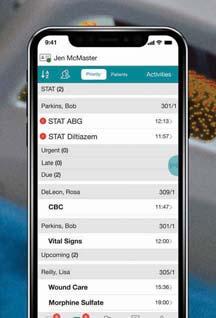
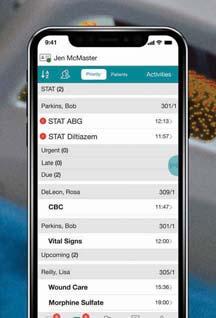
Transforming healthcare training: How Fraser Health is using AI
odernizing a health authority’s clinical system is a massive undertaking. Not only are there millions of patient files, but tens of thousands of staff and medical staff to train in order to become proficient on the new system. The efforts are worth it, however, as the systems provide streamlined workflows and improved clinical decision support, resulting in better patient care.
In 2022, Fraser Health adopted a new electronic health record system to serve over two million people in 20 communities in British Columbia. With tens of thousands of clinicians learning the new system, they also required a quick way to get questions answered and troubleshoot issues. Otherwise, staff might need to manually sort through more than 350 reference and resource documents or flood Fraser Health’s IT help desk with calls.
The Digital Patient and Provider Experience Team knew artificial intelligence (AI) could help solve the problem.
They turned to Amazon Web Services’ (AWS) robust set of AI and machine learning (ML) solutions to create a powerful virtual AI assistant that could sift through vast amounts of information and provide instant answers. Within four months, the virtual AI assistant was running, adhering to Fraser Health’s rigorous privacy and security requirements.
The virtual assistant uses several AWS AI and ML services to ingest, analyze and respond to staff members’ queries by presenting them with the information they needed to complete their tasks.
For example, Amazon Lex creates a conversational interface where users can write their questions, Amazon SageMaker builds, trains, and hosts machine learning models, and Amazon Kendra enables intelligent searches across different content repositories.
What once took an average of 15 minutes to find now takes mere seconds, significantly reducing troubleshooting and boosting time spent on patient care across the network.
“Since day one we’ve heard from users how much time they’re saving by using this system, and how much it’s improved their workflow,” said Alim Sunderji, executive director, Digital Technology Services at Fraser Health.
Fraser Health staff and medical staff have welcomed the virtual assistant. As users are onboarded to the new clinical system, at least 300 so far, they are praising its efficiency and convenience, highlighting its ability to expedite problem-solving processes effectively and enabling them to stay focused on patient care. Overall, the impact has been overwhelmingly positive.
“It was nothing short of remarkable
how quickly we were able to get the Virtual AI Assistant implemented,” Sunderji continued.
Today, thousands of healthcare and life science customers globally turn to AWS, with a growing number adopting AI and generative AI solutions, to transform back-office functions, such as billing and chart coding, to frontline patient care, such as helping doctors take notes during appointments.
“Organizations are turning to AWS to develop chatbots and AI solutions to han-
A virtual assistant, powered by AWS, enables staff to answer their questions about the new EHR in a matter of seconds.
dle challenges in staff engagement, development and upskilling, to assist with large scale transformations or day-to-day operational support,” said Elizabeth Keller, Healthcare Business Development Lead, AWS Canada. “Fraser Health’s virtual assistant is a great example of how AWS’ AL and ML services can positively impact workflow and patient experiences.”
Spurred by this success, Fraser Health is already looking towards the future, developing a second-generation virtual as-
sistant that will incorporate generative artificial intelligence and a Large Language Model (LLM) to continuously improve on the tool, like answering strategic queries, better anticipating follow-up questions, and engaging users in a more conversational manner to further enhance its utility and user experience.
“We find that 99.9 percent of users are engaging with the Virtual AI in English by typing, but what’s amazing about this system is that it’s equipped with Amazon Translate to provide high-quality translations in a multitude of languages if required, and can also respond to user voice prompting,” said Mike Chiu, director, Technology and Architecture at Fraser Health. “As we expand out across the health authority, we anticipate diverse user needs, so we’ve built the system to anticipate a multitude of user needs and experience expectations.”
Fraser Health’s adoption of chatbot technology marks a significant milestone in the evolution of healthcare training and efficiency. By harnessing AI’s power, they have not only streamlined processes but also set a new standard for innovation in the industry. As the healthcare landscape continues to evolve, embracing such transformative technologies will be essential for staying ahead of the curve and delivering optimal patient care.
PHOTO: OWEN THOMAS
NEWS AND TRENDS
Dr. Gregory Pond is co-investigator for two clinical trials that are refining prostate cancer care worldwide.
www.canhealth.com 8 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024








MEDITECH’s AI-powered technology is designed to safely enhance the experience for patients, care teams, and health systems. AI solutions are built on a secure, agile, scalable cloud architecture that makes patient data easily accessible, helping clinicians find relevant information, efficiently document encounters, and enable top of license practice for improved patient care.

Expanse search and summarization, powered by Google Health
• Quickly finds and synthesizes meaningful data from structured and unstructured sources in an easy-to-read format to support clinical decision-making
Auto generation of clinical documentation
• Reduces burden by gathering and presenting information saved in the EHR to draft documentation for clinician review and editing
• Use cases include nurse hand-off and hospital course summary (currently in deployment at Fraser Health Authority)
Conversational AI and ambient listening
• Expanse Virtual Assistant allows physicians to verbally dictate orders and find information they need with a simple verbal prompt
• Ambient listening captures the conversation between patient and provider to auto-generate visit notes for review and editing by the clinician
Discover more about how MEDITECH is leveraging AI in its Expanse platform at its eHealth session, Breaking Barriers: Advancing Integration of MEDITECH Expanse and AI in Digital Health, on Monday, May 27, at 12:30 p.m.
(781)821-3000 • www.meditech.com • info@meditech.com • Connect with us: Delivering the Next Level of Care with MEDITECH Expanse AI Solutions
MEDITECH hospitals lay the foundation for bi-directional data sharing
BY JERRY ZEIDENBERG
ORLANDO, FLA. – MEDITECH’s Traverse Exchange Canada, which connects hospitals using the company’s electronic health record, along with those deploying Oracle and Epic, to longterm care centres using PointClickCare, now links 32 hospitals and 400 long-term care organizations.
What were previously siloes of data are now able to communicate, allowing caregivers to share data in both directions. One of the most important use cases is expected to be medication reconciliation, making sure that patients who are transferred from LTC to the hospital, and back again, are taking the right meds.
“It’s not just the medication that you want to know about,” said Bob Molloy, director of Canadian market and product strategy for MEDITECH. “You want to
FHIR
know when the patient has last taken the medication and the dose,” he said. In this way, clinicians can more accurately provide new doses and avoid over-medication or adverse reactions.
Sharing data in this way will also save care-givers time and trouble. “We’re going to run out of human resources soon,” said Peter Bak, PhD, CIO at Toronto’s Humber River Health, speaking at a panel discussion at the March HIMSS conference.
Data sharing can make an immense difference, he noted, as information will be at the hands of clinicians and they won’t need to spend hours tracking it down.
Instead, they can spend more of their time on clinical issues with patients.
Traverse Exchange Canada is a component of the interoperability effort in Ontario called Project AMPLIFI.
AMPLIFI started with a pilot project in Hamilton, Ont., and is now rolling out across Ontario. It’s connecting data from hospitals using MEDITECH, Epic and Oracle/Cerner, along with LTC centres using the PointClickCare system.
While AMPLIFI is a provincial project, MEDITECH’s Traverse Exchange Canada aims to connect facilities across the country.
For years, healthcare providers, patients and many others dreamed of the day when disparate, digital health records could be connected. That day appears to be at hand.
In part, it’s because the design of these new networks is innovative, using a federated model, as is in place with the Traverse Exchange Canada network.
It means that all data remain in their original location, with their ‘custodian’. But by using the FHIR standard that’s baked into the architecture, clinicians can query for the information they need, as they require it.
This contrasts with earlier attempts at networking, which relied on HL7. “With HL7-2, you can’t query things, it’s a big hindrance,” said Derek Plansky, senior VP, Product Management with Health Gorilla, a cloud-based interoperability network provider company that’s enabling the Traverse Exchange Canada network. “FHIR is all about the ability to query the EMRs.”
The speakers emphasized that FHIR is a major advance. “Twenty years ago, people thought they could solve the interoperability problem, but they couldn’t,” said Bak. “Now, the right technology is here. It’s so much simpler.”
Unfortunately, said Bak, HL7 is ‘pushbased’ and gives you massive amounts of data that you probably don’t need. And

you can’t query for specific types of data on an ad hoc basis.
The ability to reach out for data, as needed, using a federated model is also part of the philosophical debate that’s going on in Ontario at this time. There’s a big drive to make data from various parts of the health continuum available to clinicians –including data from hospitals, long-term care, primary care and others.
Some would like to build huge repositories that constantly receive feeds to update the information. Panelist Mike Cordeiro, senior director of interoperability at MEDITECH, asserted that it’s more effective to use the federated model. “It’s better not to create large data warehouses,” he said. “Data should only be brought in when there’s a need for it.”
Bak noted that it’s far cheaper, too, to use a federated model that keeps data in the place in which it was generated. “It costs hundreds of millions of dollars to build large repositories,” he said. “You can create a federated network at a fraction of that cost.”
Moreover, he asserted that large, allencompassing repositories tend to stifle innovation. “With federated models, on the other hand, we’re all working on different types of innovation to produce better results,” said Bak. Different teams may approach the same problem in different ways; in these cases, the best solution will win.
For example, the members of the collaborative are experimenting with different types of ‘mini-records’, so that clinicians aren’t overwhelmed with too much data when they make queries.
Purpose-Built for Healthcare Mobility


Molloy noted that group members are currently working on a form of the Continuity of Care Document, which is a structured document using certain patient data elements. These could include problems, allergies, medications and immunizations (PAMI).
Bak said clinicians do not want to see 30 pages of notes. For this reason, it’s important to create formats that will be easy to navigate with information that quickly gives the clinician the answer he or she is looking for.
Molloy indicated that MEDITECH is evaluating the application of AI tools to the workflow to help manage the cognitive load on physicians.
For his part, Bak observed that ChatGPT is certainly not the answer. “If we put it into play, we’ll be slapped with 10,000 pieces of information.”
However, more refined uses of AI could, he said, be developed to seek out just what a clinician is looking for, based on the condition of the patient and the questions that are being asked. “AI could even suggest to you what you need for the patient,” said Bak. “I can see this happening even a year from now.”
NEWS AND TRENDS
Peter Bak, CIO at Humber River Health, leads a team that is implementing new forms of interoperability.
healthcare workers with powerful mobile computing solutions
C HC Mobile omputers
T4x-HC Tablet Learn more at zebra.com/healthcare www.canhealth.com 10 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024
Empower
•
•
technology is enabling a revolution in interoperability.
technology is here. It’s so much simpler.”
“Now, the right

















PointClickCare is bringing its technological successes back to Canada
BY JERRY ZEIDENBERG
NEW ORLEANS – PointClickCare cofounder and CEO Dave Wessinger bounds up to the stage of the cavernous Ernest Morial Convention Centre in New Orleans. In the fashion of today’s
conventions, there’s thunderous rock n’ roll music and applause from his adoring employees and customers. Unlike most CEOs, he does a somersault when he hits the stage.
“My back is still aching from the rehearsal yesterday,” he cracked, in his folksy, self-effacing manner.
Wessinger was kicking-off the company’s annual summit, a gathering of staff, cus-
It’s not too often that you’ll see this kind of flip from the chief executive officer of a company that generates revenues of more than $500 million a year.
The finance, HR, and supply chain system that adapts to changes in healthcare.
In healthcare today, agility alone isn’t enough. To keep up with whatever comes your way, healthcare organizations need to plan continuously and prepare for all possibilities. Workday allows you to do just that by providing real-time visibility to reduce costs and boost revenues without compromising care. Workday. For a changing world.™
tomers and business partners for education, business and a bit of fun. Well, a lot of fun.
PointClickCare was created by Dave Wessinger and his brother Mike about 30 years ago in the Toronto area. It’s now one of the largest healthcare IT providers in North America. It now supplies long-term care software – and more – to 2.600 LTC homes in Canada and about 27,000 in the United States.
Moreover, PCC software connects with more than 2,800 U.S. hospitals, 3,600 ambulatory centres and 70 state and government agencies south of the border. “We’re the largest care collaboration network in the U.S. and Canada,” Wessinger asserted.
It’s the leading software vendor in the long-term care sector, and it appears to have gotten to the top with a mixture of cutting-edge technology and a warm company culture. The summit in New Orleans – with over 2,000 attendees –seemed part family get-together. There was much hugging to be seen, and frequent mentions by Wessinger of his brother Mike, who used to be CEO and now serves as Chairman.
Dave Wessinger also spoke fondly of mom, Sheila, who also worked at PCC for

many years. “She must have done a thousand installs,” said Wessinger.
A key point, as noted by the CEO, is that the company is no slouch on technology development. It invests about $140 million a year in research and development, and nearly 20 percent of that goes into data and technology foundation IT work, including AI.
“Companies act like AI is something new,” said Wessinger in an interview with CHT. “We’ve been doing it for years.”
For that reason, the company has already launched two AI-driven products and has three more major applications in the pipeline.
B.J. Boyle, chief product officer, described a new application that’s essentially an early warning system for long-term care facilities. One of the users, Lisa Leatherwood, noted in a video presentation how one of her patients rocketed over a weekend from a score of 32 to 68. By flagging the resident, staff were immediately able to take special care and eliminated a trip to the Emergency Department.
In the United States, PCC has implemented a secure, instant messaging system that ties LTC to clinicians. In the case of the EWS patient who was crashing, staff were able to quickly contact a physician.
Called Secure Conversations, the process can be actuated with one click of the key-
NEWS AND TRENDS
© 2021 Workday, Inc. All rights reserved. Workday, the Workday logo, and “Workday. For a changing world.” are trademarks of Workday, Inc., registered in the United States and elsewhere.
CONTINUED ON PAGE 22 www.canhealth.com 12 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024
PointClickCare CEO Dave Wessinger at the summit.
The quickest way from a billion points of data to a point of view
In a world that produces more data than ever, find answers 30 times faster than ever. SAS® Viya® is the AI and analytics platform that also lowers cloud operating costs by an average of 86%, so you can build models faster and scale further.*
Start turning data into insights at sas.com/viya.
Top-tier PET/CT scanner reduces exam time to 14 minutes, head to toe
LONDON, ONT. – Ashmeet Gill had her first PET-CT scan shortly after being diagnosed with Hodgkin’s lymphoma, a cancer of the body’s immune system. She was nervous. Claustrophobia is an issue for the young Stratford resident and the scan, necessary to determine if the cancer had spread beyond the lymph nodes in her neck, would take 34 to 45 minutes, she was told.
Wrapped in a sheet and tucked inside the tube of the PET-CT at St. Joseph’s Health Care London (St. Joseph’s), Ashmeet, then 24, steeled herself to remain calm. But near the end of the scan, a sense of panic set in.
“It was not pleasant, but I endured it. I made it through.”
Ashmeet’s next PET-CT scan would be six months later, after six cycles of chemotherapy, to determine if the treatment had worked. She was terrified of another panic episode.
By then, however, St. Joseph’s had a brand-new PET-CT. And not just any machine – Canada’s first next-generation, state-of-the-art Omni 2 Legend PET-CT from GE HealthCare.
This time, Ashmeet’s scan took “barely 15 to 20 minutes,” she recalled.
“I thought, seriously? I couldn’t believe I was done. I was so happy.”
With the very first patients scanned with St. Joseph’s new PET-CT machine, it was obvious the breakthrough technology was living up to high expectations.
The machine is fast – decreasing the time it takes for a scan from 45 minutes to less than 14 – head to toe. Patients are exposed to less radiation, and the ability to precisely detect disease and tiny abnormalities is unparalleled.

“This is what we have been waiting for,” says Ting Yim Lee, a pioneer in the use of machines like PET-CT to gather new, vital information about diseases. “St. Joseph’s new Omni 2 Legend by GE HealthCare is answering the call for patients, clinicians and researchers alike.”
PET-CT is the medical ace in imaging for the assessment and treatment of cancer, neurodegenerative disorders, mental health, and metabolic and cardiovascular diseases.
And at St. Joseph’s, the possibilities of this technology took a giant leap forward in August 2023, thanks in part to the generosity of donors and a $1 million contribution from St. Joseph’s Health Care Foundation.
With the arrival of the new system, St. Joseph’s is set to become Canada’s first national GE centre of excellence in molecular
imaging and theranostics – a two-pronged approach to diagnosing and treating cancers and other diseases that merges molecular imaging with the use of radiopharmaceuticals to identify the location and extent of diseased tissues and selectively destroy the abnormal cells.
“The speed at which we can now do exams means a dramatically lower radiation dose and significantly improved comfort for patients while the exceptional image quality changes the game in the hunt for cancerous lesions,” explains Ting, director of PET/CT Research at Lawson Health Research Institute (Lawson) and medical physicist at St. Joseph’s Hospital.
For young adults undergoing repeat PET-CT exams due to their medical conditions, the reduction in radiation dose is
critical,” explains Dr. Narinder Paul, Lawson scientist and chief, Medical Imaging, at St. Joseph’s. “These individuals already face an elevated life-time risk of developing cancer from radiation, and this risk further increases with additional exposures.”
For older adults, the time it takes for the examination is also of great concern. Lying still for long periods can be a hardship due to pain from bone metastases or other conditions, and is a challenge for those who have dementia, are claustrophobic or experiencing other issues, adds Dr. Paul.
“Reducing the exam by four times is a huge improvement in the patient experience for these individuals.”
At age 75, Shirley Pryde was beyond grateful for the shorter scan time. The senior, who is being treated for cancer of the urinary tract system, had previously suffered a traumatic experience with an MRI scan, which also requires patients to lie still inside a tube. This left her very apprehensive about the PET-CT she recently needed to assess the extent of the cancer.
“I was very nervous but when I called to book the scan at St. Joseph’s, the procedure was described to me and I was put at ease,” says Shirley. “And once I got there, the technologist was wonderful. Amazingly, the total amount of time I was in the machine was only about 10 minutes. I was very relieved. I can go for the next scan without the worry.”
While patients hail the new PET-CT experience, clinicians and scientists are raving about the machine’s imaging prowess. The advanced AI-driven image formation technology now empowers the precise detection of cancer within lymph nodes and other anatomical structures, “achieving remarkable accuracy even at sizes as small as two to three millimeters,” says Dr. Paul.
Positron emission tomography – a game changer for cancer patients
BY DR. SANDOR DEMETER
Although the nuclear medicine technology known as positron emission tomography (PET) has existed since the 1950s, technological advances in the last two decades have made PET imaging a game changer for cancer patients. PET is now imaging at the sub-cellular level and has become essential in guiding treatment for patients with many common cancers, including lung and lymphoma.
PET patients are injected with trace amounts of radiopharmaceuticals (radiotracers) and imaged in PET scanners, which look like computed tomography (CT) scanners.
Since the 1990s, the first routinely used PET radiotracer was a form of radioactive sugar – fludeoxyglucose F18, or FDG –which measures metabolic activity.
Many cancers crave more sugar as an energy source than normal tissues. This results in cancers sopping up more FDG and lighting up on PET images.
Four major advancements in PET technologies and radiotracers over the
last decade have greatly benefited cancer patients.
Game changer 1 - PET significantly influences patient management: Early results demonstrated FDG PET imaging significantly altered therapy – overall by about 27 percent, for many common cancers.
FDG PET imaging is especially useful for lung cancer. In 2002 Gambir et al. reported that lung cancer management changed in more than 40 percent of patients who had both FDG PET and CT imaging versus CT alone. FDG PET was more sensitive in demonstrating how far the lung cancer had spread and commonly demonstrated disease that was not seen on CT alone. Many patients avoided major surgery that would not have benefited them.
Very few imaging studies have had such an impact on cancer therapy. FDG PET imaging has become a standard of care for finding many common cancers, determining how far they have spread
(staging), assessing response to treatment (prognosis) and monitoring patients for recurrence.
Game changer 2 - Hybrid imaging: PET scanning demonstrates how the body functions (physiology) rather than what it looks like (anatomy). For example, CT and MRI imaging primarily demonstrate anatomy.
Both functional and anatomic imaging provide crucial information to guide patient management. It would be ideal to capture physiological and anatomic imaging in one technology. Enter the era of hybrid PET/CT and PET/MRI imaging technologies.
While training in nuclear medicine, I vividly remember having to swing my head between FDG PET and CT scans to try to fuse them in my mind. It is important to know precisely where the PET abnormalities are. Is the FDG uptake in a blood vessel, a neighbouring lymph node, or something else? It makes a difference, and it can be exhausting to try to fuse images with your eyes alone.
Around the mid-1990s, hybrid PET/CT scanners became commercially available and shortly thereafter became the standard configuration.

PET/CT hybrid units allow software fusion of PET and CT imaging, resulting in precise anatomic localization of pathology. You can view pure PET or pure CT images and anything in between. No more fusion with your eyes bouncing between PET and CT images on different displays.
PET/MRI hybrid units came on the market around 2010. Although they demonstrated exquisite anatomy, especially in the pelvis or
PRECISION MEDICINE
At the launch of the Omni 2 Legend PET-CT: From left are: Dr. Justin Amann, Site Chief, Medical Imaging; Karen Perkin, Vice President Patient Care and Chief Nurse Executive; Ting Yim Lee, Director of PET/CT Research at Lawson Health Research Institute; Dr. Narinder Paul, Chief, Medical Imaging; Stephen Nelli, Director, Medical Imaging; and Dr. Jonathan Romsa, Chair/Chief, Division of Nuclear Medicine.
CONTINUED ON PAGE 22 www.canhealth.com 14 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024
Biotech leader BioAro welcomes first-ever Chief Healthspan Officer
BY NEIL ZEIDENBERG
CALGARY – BioAro (www.bioaro.com), a global leader in precision health, healthspan and longevity, has announced that Ms. Raman Kapoor will be taking on the role of the world’s first Chief Healthspan Officer.
Healthspan refers to the length of time in which a person is healthy and free from chronic disease. The goal at BioAro is to help people achieve longevity and to stay healthy for as long as possible.
“When focusing on healthspan, we all have a proactive role to play in our own health. We want to help contribute to a healthier future and a vibrant world. And I wanted to be part of the solution,” said Kapoor.
For its part, BioAro sequences and develops a map of your entire genome and specifically analyzes over 20,000 genes known to be involved in various diseases.
The company’s testing starts with a simple at-home sample (blood, swab, or stool). The process begins at www.bioaro.com. Once you have ordered your test, a prepaid return collection kit will be sent directly to you. It can then be dropped off at one of the BioAro labs, or mailed back, for sequencing and analysis.

Upon completion of the comprehensive analysis, clients receive their personalized digital report, in a confidential and secure format. Samples can be collected from anywhere, worldwide.
BioAro’s microbiome analysis includes the gut, vaginal, skin, and oral microbiomes through home collection kits. Their microbiome services can inform you of the composition and diversity of your microbiome, allowing you to understand how “healthy” and “unhealthy” bacteria levels may impact your body, diet, and mental health.
Customers can also order tests to target specific areas of concern, such as panels related to the most prevalent diseases affecting Canadians, including cancer, heart disease, diabetes, and mental illnesses, or more wellness-focused information like food sensitivities, vitamin uptake, and rare genetic disorders.
When asked how she’ll help improve our health, Kapoor explained, it’s about getting back to basics – and starting healthy habits. That means eating better food, drinking enough water, getting quality sleep, and exercising regularly.
“And by understanding a person’s genetic make up we can tailor treatments to those individuals based on actual evidence avoiding any negative side effects. We focus on personalized healthcare, specific to you.”
Kapoor is a registered dietitian by trade and brings a wealth of knowledge regarding precision-driving research and cutting-edge solutions. “Understanding that one size doesn’t fit all, it’s exciting to be focusing on healthcare – not disease care. Although we can’t slow a person’s chronological age, perhaps we can slow their biological age.”
BioAro is a global leader in precision
medicine, specializing in genomics, proteomics, cancer screening, lab testing, and medical devices. Headquartered in Calgary, BioAro has become successful internationally. “Yes, we’re Alberta-based but our target markets include Canada, United States, and the Middle East. Moreover,
many of our services are accessible from anywhere in the world.”
By analyzing our microbiomes, you can gain valuable insight into your own health conditions. As an example, data from the gut microbiome can be used to improve digestion, manage weight, improve energy
levels, mood, and mental health. The oral microbiome includes all the microbes living inside your mouth, and impacts your dental health, your ability to absorb nutrients from food, cognition, and the immune system.
Using BioAro’s PanOmic technology, the












PRECISION MEDICINE
Innovation that connects Imagine better outcomes and patient experiences across the continuum of care. With Vocera now part of Stryker—it’s possible. Explore next-gen nursing Learn more > CONTINUED ON PAGE 23 www.canhealth.com MAY 2024 CANADIAN HEALTHCARE TECHNOLOGY 15
Raman Kapoor
Fixing the current healthcare system: Data, transparency, and accountability
For the public system to perform better for Canadians, better reporting and data is required at all levels.
WILL FALK AND JORDANN THIRGOOD
To improve the delivery of healthcare, more and better data is needed. The 2023 federal/provincial funding accord strengthened and resourced a national data standardization and sharing program that is anchored by the Pan-Canadian Healthcare Organizations, chiefly Canada Health Infoway and the Canadian Institute for Health Information.
Unfortunately, the accord was not aggressive enough in insisting that all data be moved to common digital formats by a certain date. Much good work is being done in regions, but a coordinated push towards a modern system with target dates is needed.
Canada can adopt or align with existing standards that are currently used in Europe and the United States. Strong data-sharing rules, common data formats, and enforced privacy rules are now globally recognized and are critical to national security, trade competition, and next pandemic preparedness.
For the public system to perform better for Canadians, better reporting and data is required at all levels. Canadians should expect control of their own data, modern communications systems, and transparent performance reporting.
Interoperability and standardization efforts initiated by Infoway, CIHI, and others are important steps but require a greater sense of urgency to keep pace with a rapidly changing environment.
A national set of data standards should be pursued with provision for only limited variation. Such data standards are more achievable now than ever before, with a concentration of data resources in major IT companies within Canada.
At the same time, these companies must be regulated for data liquidity and competitiveness – recent reports from the Competition Bureau recognize how data blocking and market power can benefit corpo-
rate interests at the expense of better care, transparency, and innovation.
However, no existing Pan-Canadian Health Organization has this oversight responsibility in their mandate.
Transparent reporting is necessary for accountability in any publicly financed healthcare system. Unlike private-pay healthcare solutions, public systems cannot rely on competition and the market to correct underperformance.
Every principle that guides funding decisions needs to be reported on publicly in a fashion that is


understandable and usable, providing a feedback loop and check by which these systems are monitored and improved.
However, governments in Canada are often reluctant to establish and report on health quality targets.
As history has shown, central planning without transparency degrades over time – funds and programs become captured by provider interests, and, even where well-intentioned, programs may not meet the needs of healthcare consumers.
Transparency alone is not the solution to the system’s failures, but without transparency, publicly financed systems fail.
When wait times become too long, healthcare consumers will pay out-of-pocket to go elsewhere or
employers will cover the services. When cross-border virtual care is blocked, private providers step in to provide primary care services.
In these cases, a market opportunity exists because of poor performance on the Canada Health Act’s guiding principles.
Canada has a special complexity in transparent public reporting due to the provincial delivery of healthcare under the Constitution. While the national solution to this challenge has been the PanCanadian Health Organizations, the federal government has received several external reports in recent years that recommend consolidating and restructuring these organizations.
Each of these reports identify similar issues: there are too many of these organizations, they are in one another’s way, and Canada is spending too much as a result.
This article is excerpted from the CSA report, Healthcare’s Next Evolution: Rethinking Social Factors in Financing. Healthcare’s Next Evolution: Rethinking Social Factors in Financing - CSA Group It was published in February 2024. Will Falk B.Sc., MPPM has spent 25 years as a strategist and advisor in New York and Toronto advising top academic centres, governments, and innovative companies in healthcare. Since retiring from the PwC partnership in 2017, Will has had several roles, including as an Executive in Residence at the Rotman School of Management at the University of Toronto where he has taught since 2008. Jordann Thirgood is Manager, Public Policy, CSA Group, where she leads research projects at the CSA Public Policy Centre. Jordann has held policy positions both inside and outside of government, most recently at the City of Toronto where she advised on policy priorities including the regulation of emerging technologies, COVID-19 economic recovery planning, and housing initiatives. She holds a Master’s degree in Public Policy from the University of Toronto.
How AI is powering the efficiency and accuracy of full-body MRI
BY DR. NIRAV PATEL AND DR. KEYUR SHAH
Full-body MRI scans have become a buzzy headline in healthcare thanks to the virality of Kim Kardashian’s endorsement. While some view them as part of the future of preventative healthcare, others in the medical community have expressed reservations, particularly regarding their diagnostic accuracy.
Having built the protocol for our full-body MRI scan from the ground up, we know that AI-powered, fullbody MRI scans hold great promise in addressing concerns from the medical community. While AI can enhance many aspects of the MRI process, its greatest impact to date is in increasing the efficiency of the scan and improving its diagnostic accuracy.
A primary concern around fullbody MRI scans is diagnostic accuracy. Unlike a prostate or breast MRI screening which focuses on one body part, a full-body scan looks at all of the vital organs and large joints in one scan. Doing a full-body MRI with standard MRI technology is a disservice to the patient; either the patient experience suffers as the scan will require hours to take enough images to ensure diagnostic accuracy, or the diagnostic accuracy suffers as fewer images are taken to avoid having the patient stay still for a prolonged period of time.
Lower diagnostic accuracy is dangerous and is where much of the criticism for full-body MRIs stems from. The lack of accuracy can mean that something crucial is missed and the patient will feel a
false sense of safety or, on the flip side, an issue will be identified and require further testing only to determine something is benign. This begs the question: do these risks outweigh the potential for a patient to catch cancer or disease early?
A full-body MRI scan looks at all of the patient’s vital organs and large joints in a single scan.
Generally, the earlier the disease or cancer is caught, the better the odds of addressing it and therefore the higher the rate of survival. However, for many physicians, this is outweighed by the number of patients who will have something benign
flagged in their scan. Not only will this cause the patient unnecessary anxiety, but it will also require extensive and potentially invasive testing to conclude that it is benign.
Especially in Canada where our healthcare system is overburdened as is, experts argue that the value of a full-body MRI does not outweigh the risks and cost to our healthcare system.
This is where the introduction of AI into full-body MRIs is a gamechanger. Full-body MRI scan providers must invest in AI to achieve the best of both worlds – efficiency for a seamless patient experience and quality imaging for diagnostic accuracy.
AI can enhance image quality while reducing scan time, enabling rapid
BY
VIEWPOINT
Will Falk Jordann Thirgood
CONTINUED ON PAGE 23 www.canhealth.com 16 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024
Interoperable health records transformative in Canadian healthcare
BY DR. RASHAAD BHYAT
In the dynamic landscape of Canadian healthcare, technology has assumed an increasingly meaningful role, with interoperable electronic medical (EMRs) and health records (EHRs) gradually emerging as indispensable tools for enabling stronger patient outcomes.
As a family physician navigating modern healthcare complexities, I’ve witnessed firsthand the transformative power of these systems in shaping patient outcomes and enhancing efficiency within our healthcare infrastructure. Amidst the backdrop of a healthcare human resource shortage, well-designed digital health solutions have the potential to bolster and support our overextended healthcare providers.
The journey of jurisdictional EHRs in Canada began in the early 2000s, marking a new chapter in healthcare. Across provinces and territories, we’ve seen varying degrees of integration of these systems with community-based EMRs, providing clinicians like myself with more timely access to critical patient data – be it diagnostic imaging and lab results, or medication histories.
Interoperability is increasing the availability of essential patient information at
Interoperable records are making it easier for clinicians to access records. In turn, they can make better-informed decisions.
the point of care, allowing clinicians to make better informed decisions, while minimizing workflow disruptions and redundant ordering of tests.
What has this incremental digital health transformation meant for Canada? Improving efficiency, more connected care, and a near future healthcare system that will work for Canadians when, where, and how they need it.
What’s more, I can see this near future in my day-to-day. Just recently, one of my patients underwent an emergency room visit, resulting in a new prescription from the attending physician. Unfortunately, my patient was unable to remember the name of the medication, and we also couldn’t get through to their pharmacist. Fortunately, because I recently onboarded a digital tool that allows me to quickly query dispensed medications, I was able to find their recently prescribed medication. These seemingly small yet impactful technological solutions not only inspire physicians like me to continue pursuing the future we envision, but they are also the innovations that will continue transforming our healthcare system.
Looking beyond our borders, nations such as Estonia and Denmark have pioneered national EHR systems, achieving significant efficiencies in healthcare delivery and patient satisfaction.
These countries showcase the power of interoperable platforms to facilitate modern data exchange among healthcare providers, thereby minimizing medical er-
rors, enhancing care coordination, and boosting patient safety. While these nations have obvious differences from Canada, such as their small populations and nationally based healthcare systems, Canada can learn from their successes to prioritize the adoption of connected care solutions.
With the right solutions in place, access to EMRs and EHRs can benefit everyone in the health system. According to the 2023 Nurses Survey Results released this May, 9 in 10 nurses currently use electronic patient records across Canada.
From 2020 to 2023 alone, there has been over an 11-percentage point increase in the proportion of nurses who use electronic records only – as opposed to using a combination of paper and electronic or paper
only. This highlights the accelerating adoption of electronic patient records, underscoring the paradigm shift towards technology-enriched healthcare solutions and laying the foundations for safer, data informed care.

Dr. Rashaad
While Canada continues its journey towards interoperable health information systems guided by the Shared panCanadian Interoperability Roadmap, there is an undeniable need to address data gaps and ensure equitable access to technology across regions.
Continued investment in digital infrastructure, clinician training, and patientfocused education will be crucial in ensuring that we realize the full potential of health information technology across our country and in our daily lives.
As a physician dedicated to patient-centered care, I truly feel optimistic about the future of healthcare technology in Canada. Embracing innovation and collaboration, we can bid farewell to traditional paperbased systems and welcome in a new era of precision medicine and personalized care, supported by emerging technologies, ultimately building a healthier future for all Canadians.
Powering the future of healthcare starts with innovation
Building a sense of community among Workday’s healthcare customers is a key method of supporting and enabling success. We work to create educational opportunities for our customers to learn about emerging technologies, share industry best practices with their peers, and collaborate with us on opportunities for innovation.
To that end, we hosted our Workday Healthcare Provider and Payor Summit last fall. At the event, customers learned from Workday leaders how technology can enhance the future of healthcare. Below, we dive deeper into key takeaways from the summit.
How AI can improve every aspect of healthcare: AI and ML are impacting all sectors. Joe Wilson, global chief technology officer at Workday, said, “AI applied ethically and responsibly can change lives.”
At Workday, our core value of integrity guides the ethical application of AI and ML to support customers. Wilson, addressing customers at the Healthcare Summit, said, “We’re treating your data – yours, not ours – with the utmost respect. We’re doing so ethically, so that we can give you the copilot you deserve, to move faster and be better.”
John Kravitz, vice president and global head of healthcare at Workday, gave advice to customers on how to prepare for the future. “Implement new technology. Focus on agility and flexibility. Take work off your people, so they can focus on the strategic business problems.”
Kravitz, with a background in clinical enterprise technology, said, “AI and ML help take the physician’s fingers off the keyboard, and allow them to interact more with patients.”
How organizations thrive amidst supply chain disruption: Supply chain challenges persist in our post-pandemic world, said Keith Lohkamp, senior director of industry strategy for healthcare at Workday. “We thought after coming
out of the COVID-19 pandemic that supply chain management would go back to normal. But, we’re still seeing significant amounts of back orders and the need for substitutes.”
To remedy challenges, Lohkamp added, “It starts with customers doing the basic block-building to give visibility into inventory. Monitoring orders and turning on capabilities to automate substitutes in the system is key.”
Based on discussions with clients, Lohkamp said, “Our customers are looking to drive greater efficiency and
“Take work off your people, so they can focus on the strategic business problems,” says Kravitz.
reduce cost. We encourage health systems to use demand-planning tools and match supply with demand to prevent surgery delays.”
Building a resilient framework and moving forward with efficiency remain priorities for customers, Lohkamp said, adding that to further insulate against risk, many customers are implementing frameworks to identify and tag the most critical products based on clinical and supply chain factors.
How the right technology adoption can reduce costs and improve outcomes: The healthcare industry has continued to transform itself. “Organizations that we think of as insurers or retailers are now moving into home care and primary care. New players are emerging while existing healthcare systems are evolving via mergers and acquisitions,” said Lohkamp. “Now more than ever, it’s important to have a platform technology approach that allows for innovation.”
Kravtiz said, “Moving from best of breed to a unified platform can save a lot of money in the long-term. Not only in terms of the budget saved on the systems, but in terms of the overall costs of the organization.
“Think about the resources needed to customize an application – because the cost of integration, testing, and validation for an upgrade can have a huge financial impact,” Kravtiz noted, adding that having an up-to-date platform can help reduce and optimize those costs.
Learn how healthcare organizations are using technology to improve agility and better support patient care. Read this report: https://blog.workday.com/enus/2023/start-with-innovation.html#improve-healthcare
This

VIEWPOINT
Dr. Rashaad Bhyat is Senior Physician Leader at Canada Health Infoway.
article was supplied by Workday.
Bhyat
John Kravitz, vice president and global head of healthcare at Workday, speaks at the Fall summit.
www.canhealth.com MAY 2024 CANADIAN HEALTHCARE TECHNOLOGY 17
Data and analytics help UHN to better understand patients, clinicians and staff
Data management has become so important that new hires are required to undertake data literacy training.
BY DIANNE DANIEL
How long do ED patients wait for specialty consults? Is there a change in a patient’s acuity that requires attention? How many staff members are likely to call in sick tomorrow? What patient volume is expected today? What are the best retention strategies to prevent employee turnover and when should they be implemented?
These are the kinds of data-driven questions that Toronto’s University Health Network (UHN) team is answering each week to improve operational, clinical and financial performance. The goal is to understand complex situations simply, using data, and thanks to a strong commitment to maintain the highest standards in healthcare analytics, they are succeeding at it.
“We spent a lot of time a decade ago really pushing the electronic record. Now we’re at a point where we’re at critical mass. All of these digital systems are creating data, and we’re in the next phase of what do we do with the data to make sure it’s benefitting the organization and the patients we serve,” said UHN Chief Data and Analytics Officer Michael Caesar, whose team is leading a cross-functional, collaborative initiative to use data more effectively across the institution.
Management System Society (HIMSS) Adoption Model for Analytics Maturity (AMAM) Level 6 distinction. The achievement demonstrates the hospital’s ability to capture, govern and manage trusted data from multiple domains and apply it in meaningful ways.
Data is so entrenched in everyday activities, UHN has launched a staff data literacy program that in-
clinical and human resources systems, clean it and apply it to create analytical dashboards that support data-driven decisions.
In addition to accessing data available from UHN’s recent transition to the Epic electronic health record, Caesar’s team also maintains a separate electronic data warehouse, applies business intelligence and automation tools, and is investigating how to apply artificial intelligence to enhance data analysis.

cludes on-line learning and in-person sessions, and the onboarding process for new leaders entering the organization now includes an introductory data literacy course.
At the end of 2023, UHN became the first academic and research network of its size in Canada to earn the prestigious Healthcare Information and
A great deal of “data wrangling” goes on behind the scenes, requiring specialized data expertise to pull information out of key finance, administrative,
“It’s a natural evolution, now that we have the tools in place, and now that we’re creating this data output. We’re working on how to use it, to make sure we’re doing better today than we did yesterday,” said Caesar.
Prior to implementing Epic in 2022, emergency departments at UHN’s Toronto General and Toronto Western sites were operating primarily on paper, making it difficult to extract the information required to support real-time analytics. As part of its HIMSS validation, UHN showed how data is now driving decisions around emergency workload, patient volume, capacity, sick calls and patient acuity through the use of dashboards and analytics.
Planning and performance data are also used to track specialty consults, including how long a patient waits to be seen, as well as to analyze frequent users of the emergency department with the goal of
New system at Canuck Place will enable better analysis of data
Accessing data is one of the driving factors behind a B.C. children’s hospice decision to implement a customizable electronic health record solution from Healwell AI Inc.’s newly acquired Intrahealth Systems Ltd. subsidiary.
Located in Vancouver, Canuck Place Children’s Hospice provides pediatric palliative care programs throughout B.C. and the Yukon, caring for about 850 children and families through illness and bereavement. They were looking for a digital solution that would simplify communication and record sharing across multiple locations, and support in-depth reporting based on custom data views.
On average, Canuck Place follows a child for five to seven years through illness, and then supports their family for another three years in bereavement. Because their highly specialized service spans different care sectors, from hospitalization to community-based clinics to home care, across different regional health authorities, they were looking for an EHR platform that could easily
adapt to support custom workflows.
“We were suspecting there wasn’t going to be an easily available offthe-shelf product that was going to meet all of our needs,” said Canuck Place clinical program director Kristina Boyer.
The project with Profile involves digitizing paper-based forms and improving processes as they work to implement connected electronic patient charts. Profile will be the single source of truth to ensure information is consistent as data is both pulled in from various systems and pushed out to populate the provincial CareConnect EHR platform.
“From a data analysis perspective and documentation perspective, we want this to support good communication and continuity of care so clinicians have access to the information that helps them look after people,” said Boyer.
The shift to Profile is a big change, yet a welcome one, she added. Clinicians are excited by the fact that families will no longer have to relay their stories multiple times because their
information will be available in one place, regardless of whether it originates in a pediatrician’s office, a community nursing centre or a specialized children’s hospital.
In the paper-based system, clinicians have to rely on phone calls and requesting the information they need from their peers in other sectors.
“We have a lot of duplicate systems for communication and hand
A new EHR enables Canuck Place to access patient data across many locations.
over. It’s not very efficient and yet we do it because it has such an important value,” explained Boyer. “The opportunity to streamline all of those processes is really exciting.”
As it builds out its Profile implementation with Intrahealth, Canuck Place is also looking forward to using aggregated data to drive improvements in its processes. Working with paper
records, they were forced to collect administrative data in a separate database. If they wanted to run a report, they had to manually open records and do an audit, a labour-intensive activity that was limited in scope.
When the digital system goes live, data collection will be automated and data analysis will be simplified. For the first time, the hospice will be able to ask clinically driven or administrative questions and extract data for analysis in “a much more streamlined and efficient way,” said Boyer, a change that opens up new possibilities such as analyzing pain assessment from a clinical domain to determine the best practices to help children feel the most comfortable.
In the next phase of their Profile implementation, Canuck Place will also be looking to develop a patient portal so that patients and their families can easily access relevant data, including their child’s most up-todate medication profile.
“Once we’re providing care for you, we’re connected and we’re going to stay connected over time,” she said.
FEATURE REPORT
ILLUSTRATION: LINDA WEISS www.canhealth.com 18 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024
better understanding their chronic needs to develop new, more effective services or care pathways.
“We’ve done a lot of analysis in collaboration with our social medicine program to understand those patient populations, to see if we can serve them better,” asserted Caesar.
The UHN People and Culture team is another area working to apply real-time data analytics. At first, it was the COVID pandemic that urged them to move the needle on reporting as they faced challenges related to staffing and stocking personal protective equipment (PPE).
Using data from the Human Resources and Health Services information systems, they partnered with the Data and Analytics group to generate dashboards to show employee numbers and health status, including percent COVID positivity and expected return to work. As a result, they were able to hold proactive conversations about operational impact to better prepare for and respond to staffing issues.
They also created an inventory data model to track PPE items such as face masks, gloves, gowns, N95 masks and hand sanitizer at a unit level, based in part on past usage data. The resulting risk chart used red, yellow and green indicators to show the quantity on hand at any given time and warn when supplies were low or when changes to ordering schedules were required.
Since then, data capabilities are continuing to evolve at UHN, with one example being a strong partnership between the People and Culture and the Data and Analytics departments.
“When it comes to UHN’s people data, we now have a common language as an organization through the creation of a single source of truth (a master data file), and a team of analysts across People and Culture teams that help with all requests,” said UHN senior director, Talent and Learning, Jessica Marangos. “I think that’s been a pretty big win for collaboration across People and Culture and the organization.”
For example, to help with attracting and retaining employees, People and Culture now uses talent acquisition and employee turnover dashboards that refresh on a monthly basis, tracking everything from number of applications from prospective employees to conversion rates to who’s leaving the organization.
The information provides valuable insights to help with recruiting and retention activities at a unit level, helping leaders to understand their current head count, including which employees might be considering leaving and what positions they should be focused on hiring.
When data analysis uncovered that employees typically decide whether to stay or leave UHN after two years of employment or less, the People and Culture team was able to develop a toolkit designed to support ‘stay interviews’ at key intervals as a retention strategy.
“We really have used data to make more tailored interventions instead of just painting everything with the same paintbrush,” said Marangos, adding that data is also helping to dispel myths.
“We hear people say turnover is increasing or things aren’t improving, but now we can say, actually, things have been improving,” she said. “Here’s our trend line over
the past two years … We’ve actually looked at the data and we don’t see that across the board… And here are the pockets to focus on that aren’t improving at the same rate.”
Marangos considers the Data and Analytics team a centre of excellence that is setting data standards and creating a collaborative environment that allows everyone to work together to understand their data better. Moving forward, she said Peo-
ple and Culture intends to combine quantitative analysis from the dashboards with more qualitative data coming from employee engagement, new hire and exit surveys, to further enhance decision-making.
The goal, said Caesar, is to continue telling stories with data and make data-driven improvement, a task that requires a highly skilled team of data analysts, data engineers, statisticians and data scientists.
Anyone in the organization can “put up their hand and say they have an interesting problem they want to explore,” he added, and Data and Analytics will partner with them to think it through on a priority basis.
“It’s not just ‘give me the data and I’ll go figure it out,’” said Caesar. “There’s a lot of complexity and nuances, standards and processes that need to be untangled to tell a good story with data.”


ELECTRONIC HEALTH RECORDS
www.canhealth.com MAY 2024 CANADIAN HEALTHCARE TECHNOLOGY 19
EHR trends at e-Health: Cyber-security,AI,interoperability and more
Aquick look through the 170+ presentations scheduled for e-Health 2024 (May 26-28) reveals a wealth of new ideas and insights on how we can continue to improve healthcare delivery for Canadians using technology and data. Provincial electronic health records (EHR) support and enable many of the innovations on the schedule at e-Health 2024. A workable EHR is at the root of connected care and telemonitoring; enables patient engagement and empowerment; and contributes to progress in health data management and security.
Data security and privacy is one of the hot-button issues on the e-Health 2024 schedule, with presentations offering tips for cybersecurity resilience to healthcare delivery organizations working to safeguard data in an era of unprecedented public data breaches. Two presentations offer guidance on safeguarding patient care/healthcare: Building Cyber Resilience in Healthcare, and A Prescription for Cybersecurity Resilience. This presentation will share details of a cybersecurity and privacy web-based self-learning program designed by physicians, nurses, and security experts to support clinicians and their staff to better grasp the Canadian healthcare cybersecurity and privacy landscape and to empower informed decision-making while working with information systems.
In addition, Ariane Siegel, OntarioMD, general counsel and chief privacy officer, will speak to how primary and community care physicians can respond to cybersecurity threats and protect their data – and their practices. This presentation will pro-

vide an overview of the emerging trends in cybersecurity that can disrupt primary care and community care physician practices and result in adverse events for patients. Patient engagement and empowerment in relation to an individual’s own health information is another innovation trend on the agenda at e-Health 2024. Cultivating Patient Empowerment: Evaluating and Enhancing a Province-Wide Personal Health Records Application will show how designing and implementing province-wide personal health record (PHR) applications can help more patients manage their own health and be engaged in shared decision making.
“I Consent” – The Patient Perspective on Consent and Digital Health Tools explores health data management and tech-
nology’s role in patient care highlighting service design research to understand public views on data management and consent. Working toward interoperability is at the core of many health data stewards’ efforts. Representatives from Canada Health Infoway will be at e-Health 2024 with an update on their Pan-Canadian efforts to improve interoperability and the goal of bringing Canadians a digitally enabled health system where they can have access to their own electronic health information, and where health data can be safely shared to support patient care, research and innovation.
Exploring primary care integration in a health information system: An innovative approach will share insights and best practices on innovative primary care engagement approaches for spread and scale pur-
poses in other jurisdictions. And, while interoperability has now been made a reality between Ontario hospitals and long-term care (LTC) homes, much work remains to achieve true interoperability. A Provincial Interoperability Journey to Streamline Resident Transitions between Hospital & Long-Term Care will look at the provincial data integration project that enabled the bidirectional exchange of patient information between health information systems.
The Opening Keynote presentation on May 27, presented by CMA president Dr. Kathleen Ross, will focus on Healthcare Human Resources: What Physicians, Nurses, and Healthcare Providers Need to Make Their Jobs Easier and Manage Burnout, Technology, the Administrative Burden of Health, and the Impact on Human Resources.
The opening Plenary Session on Tuesday, May 28 will feature a panel of experts discussing Artificial Intelligence in Health and Public Health Data: Balancing Possibilities and Accountabilities in a Secure Environment. Key points the panel will discuss include showcasing the transformative potential of Artificial Intelligence in healthcare, exploring the ethical and regulatory accountabilities in leveraging Artificial Intelligence for public health data, and emphasizing the critical importance of security measures in safeguarding health-related information. e-Health 2024 Emcee Avis Favaro – Canada’s leading health journalist – will introduce both sessions.
e-Health 2024 takes place in Vancouver from May 26-28. Visit e-healthconference.com for more information about sessions and speakers.
OntarioMD’s strategic approach to combat physician burnout
OntarioMD, a subsidiary of the Ontario Medical Association and funded by Ontario Health, focuses on helping doctors use technology to ease their administrative burden and enhance patient care. Artificial intelligence or augmented intelligence (AI) has emerged as a promising technology that can potentially improve and transform the collection of health information by physicians during patient visits.
OntarioMD is actively exploring the AI market, evaluating AI solutions for family doctors to determine how best to integrate them with doctors’ workflows to mitigate burnout. Our work provides an initial assessment of AI’s role to support charting and improve the doctor and patient experience during visits.
OntarioMD’s multifaceted AI strategy is about:
•Partnership: We collaborate with clinicians, industry, research entities and governments to create an innovative ecosystem. An AI community of practice and an innovation lab serve as a knowledge exchange platform for testing and refining AI solutions. The creation of
a common set of training data and AI models will reduce barriers to innovation.
•Implementation: Support for physicians in realizing the full potential of AI solutions is important. OntarioMD conducts evaluation projects, such as our recent AI Scribe Pilot Study, to understand the practical, legal and privacy implications of AI integration. We are developing AI implementation toolkits covering requirements, change management, and project plans.
OntarioMD provides input on health system guidelines to promote the responsible use of AI, and strategies for spreading and scaling AI solutions, including validating or certifying these technologies.
•Education: To help doctors understand AI solutions, OntarioMD offers comprehensive education in various formats. We offer environmental scans, market research, webinars, white papers, articles, and presentations. Sign up for our Digital Health eTips newsletter to learn more.
AI solutions environmental scan: OntarioMD produced its Environmental Scan in early 2023 to explore AI-powered solutions for primary care. The scan examined the current AI technology landscape, evaluating functionality, ben-
efits, and roles within healthcare operations. The scan reviewed diverse sources to categorize AI tools based on their impact on primary care, particularly regarding workflow efficiency, decision support, automation, and physician workload reduction.
Over 137 solutions were examined


and grouped into three categories based on primary care workflows:
•Patient Engagement: Tools for appointment scheduling, reminders, and virtual health assistance, with an emphasis on personalized education and remote health monitoring, to enhance patient access and engagement and facilitate ongoing patient care and management.
•Clinical Improvement AI scribes for
clinical documentation, diagnostic and treatment support tools, and predictive analytics for risk assessment: These solutions aim to improve the quality of in-person visits, support clinical decisions, and to prepare healthcare providers for patient visits, leading to enhanced patient outcomes.
•Administrative Efficiency: EMR inbox management, medical coding, and billing optimization tools to streamline post-visit processes and reduce the administrative burden on health-care professionals, allowing them to dedicate more time to patient care.
Our Environmental Scan acts as a catalyst for the seamless integration of AI into primary care, offering crucial insights derived from market analysis; this underscores its importance in enhancing patient and provider experiences and aligning with health-care needs for optimal delivery.
Piloting the AI scribe - A step towards understanding its impact: In late 2023, OntarioMD, in collaboration with the Ontario Medical Association and WELL Health, conducted a preliminary study to measure the effectiveness of AI scribe in mitigating physician burnout through the automation of clinical doc-
ELECTRONIC HEALTH RECORDS
DR. ABBAS ZAVAR AND SIMON LING
Dr. Abbas Zavar Simon Ling
CONTINUED ON PAGE 23 www.canhealth.com 20 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024
With technology,patient engagement can bridge gaps in primary care
“A
patient who has no access is a patient who will do anything,” says Professor Isabelle Gaboury, Director of Research in the Department of Family Medicine at the University of Sherbrooke, Quebec. That powerful advocacy for better access to primary care comes at a moment when resources and healthcare workers are stretched thin.
Adding to the complexity are the multitude of challenges they encounter in participating in their own care. In particular, relatively few primary care clinics offer the electronic tools allowing patients to help manage their own care. Are we facing an equation impossible to solve?
“Patient engagement is not an additional problem”, replies Gaboury. “It can be part of the solution.”
In fact, the advanced access model relies on patient-centered interventions, such as open-access scheduling and education, which make the care journey easier to understand and, therefore, easier to navigate. Everyone has a role to play in an efficient model of the continuum of care, including the patient who is an active participant in his own right.
But Gaboury draws the line: “patient empowerment ends where clinician empowerment begins.”
Patient engagement: A new pillar to the advanced access model: “Patient engagement is the active involvement of patients in their care, including their contribution to improve the clinical practice,” said Professor Mylaine Breton, Canada Research Chair in Clinical Governance of Primary Care Services. Most patients are eager to actively engage in their care journey with the dual benefit of alleviating the burden on the healthcare system and enhancing their satisfaction through a sense of empowerment.
In a 2022 article, Professor Breton revisits the primary care advanced access model with the addition of a new pillar: communication about advanced access and its functionalities.
In this revised model, patient engagement is a two-way collaboration that includes access to educational material for patients. As technological platforms mature, they not only enable, but actively foster close collaboration among healthcare stakeholders.
This advancement streamlines processes and addresses the pervasive administrative burden that has plagued professionals since our healthcare system’s digitalization.
By creating a seamless interface between care providers and patients, electronic medical record (EMR) technology facilitates such engagement with patient portal features such as MEDFAR’s MYLE online booking, secured messaging and document exchange.
The state of patient engagement: According to Canada Health Infoway’s 2023 report, “Quantifying the Benefits of Patient Access to Their Own Health Information”, 4 out of 5 Canadians desire electronic access to their personal health information (PHI).
However, only 3 in 10 currently indicate having such access. From the same survey, among Canadians who do have online access to their PHI, 88 percent feel more informed about their health, and 82 percent

believe they are better equipped to manage their health.
These findings indicate that a majority of Canadians are prepared to actively engage in their healthcare and see benefits in doing so.
As patients assume greater responsibility for their care and navigate the system, they need guidance. Professor Gaboury ex-
plained: “By promoting self-care and assisting patients in making informed choices, such as selecting the right healthcare professional … the relevant appointments are directed towards patients who require more pressing care. Supporting patients in their healthcare utilization and providing them with strategies are integral
aspects of self-care. That’s where we can make progress.”
With that empowerment and increased responsibility on the patient side, comes the risk that some of them may not be able to adapt.
“We recommend not setting appointments months in advance”, confirms Breton. “It unloads the [healthcare] system and makes it more efficient. We eliminate all the back-and-forth phone calls. But we need to be careful with patients who might not get back [to the clinic].”
Both Breton and Gaboury concur that patients with chronic conditions need to be tracked to avoid discontinuity of care.
Technology can provide a safety net by integrating powerful data insight tools into the EMR, such as MYLE Analytics. Clinics are able to identify their more vulnerable patients, create dashboards, and ensure that these patients are closely monitored.
“When we can segment our patient population with an EMR solution or a dashboard, we can identify those who haven’t been seen in the year, particularly
How to improve the use of chatbots in healthcare
BY MICHAEL MILLAR
Chatbots are everywhere these days. Almost everyone has interacted with one, from changing an airline booking to getting support for enterprise software. Increasingly, we are starting to see them being used in healthcare.
It’s no surprise to see this novel use of the technology. Chatbots can perform a “triage” function that can save time for clinicians before they interact with the patient, pre-populating key information and escalating to the right resource.
At a time of unprecedented clinician burnout, you can understand why they are so seductive. Some chatbots are designed to be a care delivery option in and of themselves, especially in mental health where they can offer a judgmentfree place to talk through feelings. The appeal is obvious: chatbots offer 24/7, anonymous support for people in crisis.
Patients seem ready to adopt this familiar technology, but is healthcare ready? Today, most chatbots operate as disconnected, standalone apps. That is to say they do not have access to the patient’s records and clinical history from EMRs, clinical databases, or other places where relevant information is stored.
As a result, many begin each patient interaction with the same prompts and pre-screening questions.
A recent study published in JAMA Internal Medicine found that 1 in 3 prescreening questions asked to patients were “excessive.” If these chatbots are simply mirroring in-person interactions, the same excessive screening will be built into the workflow.
Patients are already frustrated answering the same questions over and
over again and for those in crisis, the smallest barriers may prevent them from seeking the help they need.
But as frustrating as repetitive questions might be, the generic nature of advice provided by chatbots is often their biggest flaw when it comes to delivering personalized care.
The reason why so many mental health chatbots deliver generic advice is because healthcare organizations are notoriously risk-averse. This is perfectly understandable, as the liability a healthcare organization would be exposed to if a chatbot gave inappropriate or harmful advice to someone in crisis is significant.
These challenges are not insur-
Chatbots should be primed with relevant information pulled from the patient’s e-record.
mountable. Both risk and the generic nature of advice can be addressed through a thoughtful reconceptualization of the foundational technology that supports chatbots.
Firstly, chatbots must exist within any healthcare organization’s existing technology ecosystem. That is to say they can not operate as siloed point solutions, they must be an integrated piece of the existing environment.
By “priming” the chatbots with relevant information about patients from existing health data (EMRs, labs, wearables) healthcare organizations can avoid repetitive screening questions and provide more personalized and relevant advice and support.
Another benefit is that bypassing the initial screening questions shortens the interaction with the patient and the shorter the interaction the less risk the healthcare organization is exposed to.
However, the biggest risk with chatbots today is that a purely LLM-powered tool can be susceptible to “hallucinations.” LLM hallucinations are the generation of content that is irrelevant, madeup, or inconsistent with the input data.
They arise from a combination of factors, including source-reference divergence in training data, reliance on incomplete or contradictory datasets, and the model’s propensity to guess based on patterns rather than factual accuracy.
The risk here is substantial and potentially deadly. The best way to eliminate the risk of hallucinations is to limit what type of responses can be created using generative AI. Although Large Language Models can generate new answers and conversations in a generative format, they can also be deployed to make predictions and guide conversations down to a predefined classification of acceptable chat outcomes.
All that needs to be done to set an organization up for a successful mental health chatbot is a solid understanding of the risk involved and a willingness to drive true interoperability between their data sources to enable pertinent, personalized care.
Michael Millar is an Adjunct Lecturer at the Institute of Health Policy, Management, and Evaluation at the University of Toronto and the CEO and Founder of Verto Inc., a Toronto-based digital health organization that specializes in AI-enabled digital twins for population and mental health.
ELECTRONIC HEALTH RECORDS
CONTINUED ON PAGE 23 www.canhealth.com MAY 2024 CANADIAN HEALTHCARE TECHNOLOGY 21
board, and a clinician is available for consultation around the clock.
“You don’t have to rush the patient to Emergency at 2 am,” said Boyle, explaining that help is always at hand. As well as this text-based service, PCC also enables virtual care with physicians, again supporting patients and staff in emergencies.
Addressing the issue of staff shortages and burnout, PCC last year launched an AI-powered clinical summaries app that dramatically reduces the time nurses spend on documentation.
The app guides the nurse as he or she is documenting, making sure they’re not missing anything. As one care home director put it, “standardized assessment is critical.” It enables managers to track how individual patients are doing and to see wider trends over time and across facilities.
Where does AI come in? PCC demonstrated how its LLM can create full progress notes, pulling from days of assessments to find the key points and produce a succinct clinical summary.
The application, said Boyle, has just been released to early users. As it’s rolled out to additional customers, it’s expected to make a significant impact by reducing the time spent by nurses on documentation.
While AI is certainly today’s technological wunderkind, Wessinger also emphasizes the advantages that PCC’s extensive network offers to customers. In the United States, it offers a free system that connects the data of long-term care facilities with acute care, government agencies, pharmacies and public health. “We run the largest connected provider network in the U.S.,” Wessinger says, with pride.
It’s through this system that tremendous gains can be made, he said. Especially when you add a layer of intelligence that provides analytics and insights.
“You can easily connect the acute care provider with the long-term care centre to
PET: Game changer
brain, they have not achieved significant market penetration.
In Canada, there has been a 19 percent increase in the number of PET/CT units over the last seven years, to a total of 56 units. The number of PET/MRI units has increased from two to six over the same time period; they are primarily used for research purposes (according to the CADTH Medical Imaging Inventory 2022-2023).
Game changer 3 - Precision medicine and the age of theranostics: Theranostic radiotracers have two elements. One attaches to a specific cell structure, such as a surface receptor on the outer cell membrane, and the other carries a radioactive substance that can be swapped out for either imaging or therapy. Such diagnostic and therapy theranostic “pairs” have been developed for prostate and neuroendocrine tumours.
For example, a patient with advanced prostate cancer might be a candidate for Health Canada’s recently approved prostate cancer radiotracer treatment (marketed as Pluvicto by Advanced Ac-
perform a medication reconciliation,” said Wessinger, noting that many re-hospitalizations occur due to medication mismatches and errors.
Users can also see if patients are getting opioids from multiple pharmacies, or if certain patients are visiting EDs at different hospitals. You can even drill down further, he explained, to see if the patient has a history of behavioural health issues. “You can then take steps to care for the person afterwards, to get them the right attention, or else they’ll be right back in the emergency department,” said Wessinger.
It’s this kind of value that a connected network can add, he said. Of course, the connected network makes it so much easier to move documents when patients are
moved from a skilled nursing facility to hospital, or vice versa. Indeed, it was largely to facilitate this process that PCC created its network in the first place.
“It was quite startling when we realized that at discharge from hospital, an LTC pa-
PointClickCare is bringing to Canada many of the technologies it developed in the U.S., including interoperability solutions.
tient would have the hospital record stapled to his sheets on the gurney,” said Bill Charnetski, executive VP of health system solutions and government affairs. Not only
could the document be easily lost, but “someone would have to re-input the data. That pulls people away from care and leads to new sources of error,” added Charnetski.
To some extent, PCC is now taking technologies it has developed in the United States and it’s bringing them to Canada. Its networking technology is at the heart of Project AMPLIFI, which started as a demonstration project to link the Epic health information system at St. Joseph’s Health Care Hamilton to a local skilled nursing facility using PCC.
The project has been so successful that it was quickly expanded by the province. It currently reaches 47 Ontario hospitals and 367 long-term care centres, although more are being added.
AI at the Mayo Clinic: The leading edge of curating data
arts. Halamka said in this respect, AI has done wonders for his own writing.
On the other hand, the Mayo Clinic is avoiding high-risk apps, such as deploying clinical AI to patients. “The results could have serious repercussions for patients,” he said, especially if there are errors in the results. It’s early days for the technology, and it’s imperfect.
Still, AI is a moving target and improvements are emerging quickly. Halamka said that if AI is able, in two years, to read chest X-rays, and if an algorithm can spot polyps five times better than a GI specialist, why not make use of these tools? At least as intelligent assistants.
Halamka stated that a monumental use of AI would be to analyze the genome for various diseases, correlate with the experiences and outcomes of patients, and to then prescribe the best tests, medications and therapies.
He asked the audience how many have had their genome sequenced – and a few raised their hands. “So, you’ve had your
celerator Applications Inc.).
Before embarking on treatment, the patient should have two PET scans. The first is an FDG PET scan to demonstrate all the prostate cancer diseases. The second is prostate (68 Ga PSMA) PET, which will demonstrate prostate cancer cells that demonstrate specific cell receptors (i.e., prostate-specific membrane antigens or PSMA).
If the prostate-specific PET looks the same as the FDG PET scan, therapy can be entertained. If the FDG PET scan shows more disease than the prostate PET scan, the patient might not benefit from this therapy, as many of his prostate cancer cells will have lost their receptors and will not benefit from this treatment.
With theranostic agents, treatment is tailored at the individual patient level.
In a similar vein, there are theranostic agents for treating neuroendocrine tumours (e.g., 68 Ga DOTA for PET imaging and 177 Lu Octreotide for therapy).
Game changer 4 - PET/CT to guide therapy in advanced breast cancer: Precision medicine, also known as personalized medicine, tailors therapy to individuals and their unique genetics and other characteristics and results in the
three billion base pairs sequenced,” said Halamka. “That costs $500. But to interpret it would cost $1 million.” That seems like a good project for Mayo, he added.
The possibilities of such a project are mind-boggling. Halamka recounted the experience of his father-in-law, who was diagnosed with Stage Four pancreatic cancer –
A great task for AI would be to analyze an individual’s genome for diseases, then find matches with the best therapies.
the point at which it can no longer be cured. The problem, he said, is that pancreatic cancer usually isn’t detected until Stage Four.
But using AI, “what if you can detect it at Stage 0?”
“If you have a risk for pancreatic cancer, wouldn’t you want a test for it?”
That comment opened a lively discussion with the audience. One member asked, “Just because you can do something, such as a test, should you do it?”
“right treatments to the right patients at the right time.” (U.S. Food and Drug Administration)
Breast cancer is the second most common cancer in women, affecting one in eight and killing one in 34.
Breast cancer therapy is largely driven by cancer cell receptor status (e.g., estrogen, progesterone, and HER-2).
A study at Toronto’s Princess Margaret Hospital demonstrated that you cannot
In Canada, there has been a 19 percent increase in the number of PET/CT units in the last seven years.
trust the receptor status of the original breast tumour to predict the receptor status of metastases. That’s why it is recommended that all cancer sites be biopsied.
However, in advanced breast cancer, biopsying every cancer site, especially if the cancer has spread to bone, is not always feasible.
A new FDA-approved PET estrogen receptor agent (Cerianna, marketed by GE HealthCare), solves this problem. This is a paradigm shift, as this is the
Halamka noted that it was an excellent question, and that some people would answer yes and some no.
For example, he mentioned the experience of his own mother, who has frontal lobe dementia and is in a memory clinic. She is now in her 80s and there is no known cure for her disease.
“Would you want to know in your 60s that you’ll have this in your 80s?,” asked Halamka. “Some people would, and some people wouldn’t.”
For its part, the Mayo Clinic is currently running a trial on a cohort that has an increased risk of pancreatic cancer. According to the hospital, the model is performing with 97 percent accuracy.
“Most people with an increased risk want to know,” said Dr. Matt Callstrom, chair of the Mayo Clinic’s Department of Radiology in Rochester, Minn.
Halamka observed that if you can catch pancreatic cancer in its early stages, it would save lives and reduce costs for the healthcare system. For these reasons, he added, it would make sense for insurers to fund trials of this kind.
first PET radiotracer to replace and complement invasive tissue sampling when biopsy is not feasible. There are no Health Canada-approved estrogen receptor agents at this time.
Again, an FDG PET scan will demonstrate all the disease, and the breast estrogen receptor PET scan will demonstrate how many cells have estrogen receptors. If much of the cancer has lost its estrogen receptor status, anti-estrogen therapy might not be beneficial, and alternate therapies can be considered.
After 20 years of being limited to FDG PET scanning, many new PET imaging agents are being developed and their use has expanded beyond cancer to include cardiology, neurology and inflammatory/infectious conditions.
PET technologies and novel PET radiotracers are leading the field of precision medicine.
Dr. Sandor Demeter is a Winnipeg nuclear medicine physician, an associate professor in the Department of Community Health Sciences at the University of Manitoba and a graduate of the Dalla Lana School of Public Health Global Journalism program at the University of Toronto.
CONTINUED FROM PAGE 5
CONTINUED FROM PAGE 14 PointClickCare CONTINUED FROM PAGE 12 www.canhealth.com 22 CANADIAN HEALTHCARE TECHNOLOGY MAY 2024
With technology,patient engagement can bridge gaps in primary care
those with chronic illnesses, and reduce oversight”, confirms Professor Gaboury.
Is technology the end-all and be-all of patient engagement? In the final report of the largest pan-Canadian conversation about the future of primary care, produced by the MAP Centre for Urban Health Solutions earlier this year, the input of nearly 10,000 patients is clear: patient engagement is key to evaluate the adequacy of primary care.
It also emphasizes that primary care teams should be connected with community and social services, working together to support individuals’ physical, mental, and social well-being.
A sentiment echoed by Professor Breton: “The system needs to be better connected with patients, especially vulnerable ones. They require more than just medications and dietary recommendations. Community resources are essential. The integration of social prescribing into EMRs is the direction we are heading towards.”
The diverse array of resources necessary
for efficiently managing patient care underscores the importance of integrating technology as an enabler. Connecting all stakeholders is crucial to grant them access
Primary care teams should be connected with community and social services, working together to support patients.
to pertinent information with the right guidance, resources and tools for supporting patients.
Hence, technology enables clinics to easily monitor and support outliers as well, from super users to disengaged patients, covering the entire spectrum of engagement.
Charting the future of primary care technology: The advanced access model aims to enhance the efficiency and accessibility of our primary care. It relies on patient engagement to optimize healthcare utilization.
AI powers full-body MRI efficiency
acquisition of comprehensive single-body MRI scans. This includes obtaining a similar number of images in various sequences and planes but with improved acquisition time and augmented image quality, often improving upon the standard procedure for routine MRI scans ordered by physicians. This is the key differentiator which makes our scan accurate and minimizes callbacks, further work-ups, and incidental findings.
A continuous challenge for reading MRI images is the noise caused by operator performance, equipment and the environment, which can lead to inaccuracies. AI algorithms can be used to detect and remove noise in the images produced by the scan, as well as to reconstruct images so important details are not lost.
At Whole Body MRI, we invested in SIEMENS Healthineers’ Deep Resolve Pro Package, which combines their three applications: Deep Resolve Gain, Deep Resolve Sharp and Deep Resolve Boost. Deep Resolve Gain is a great example of applying AI to improve image quality, using a targeted algorithm to detect and remove noise in the image. Noise detection and removal are performed optimized for the individual scan in order to address spatially varying noise of the specific acquisition. This method enables the enhancement of the signal-to-noise ratio, which can be leveraged to improve resolution or increase productivity.
Using intelligent reconstruction algorithms and deep learning networks, AI can also reconstruct accelerated images with a higher signal-to-noise ratio and produce better image sharpness.
AI-powered image reconstruction technology can also deeply improve the efficiency of MRI scans without sacrificing diagnostic accuracy. Faster image acquisition leads to improved patient comfort, workflow efficiency, and energy efficiency. As a result, radiologists can better read the images produced by the scan
Technology plays a crucial role in facilitating this empowerment, connecting all the stakeholders and offering tools to address challenges at both ends of the spectrum.
On the one hand, it enables clinics to track patients who might otherwise be lost to follow-up and, on the other hand, it provides guidance and education to those who heavily utilize healthcare services.
Forward-thinking EMR provider MEDFAR Clinical Solutions has taken heed. Building on years of innovation grounded in a clear vision, MEDFAR designed a distinctive solution with a unique confluence of patient-centric functionalities. The upcoming MYLE Health mobile application
will represent another significant advancement, empowering patients by placing control in their hands and streamlining processes for healthcare professionals.
This offers a promising solution to the challenges of Canadian healthcare delivery, with patient engagement serving as a key component.
This article was supplied by MEDFAR Clinical Solutions, of Montreal. The company, with customers in Quebec and British Columbia, provides an advanced EMR that offers electronic tools enabling patients to comanage their health alongside their healthcare professionals. www.medfarsolutions.com
BioAro welcomes Chief Healthspan Officer
cutting-edge platform enables comprehensive analysis of diverse ‘omic’ data types, including genomics, transcriptomics, proteomics, and metabolomics, all within a single, seamless interface, empowering people to be the CEO of their own health.
and accurately identify any concerns. While AI can go a long way in improving image quality, it is important to note that it will not compensate for a bad image acquisition chain. To deliver on the promise of full-body MRI scans to accurately detect early-stage cancers and diseases, providers need to invest first in quality hardware. AI then plays an important role in enhancing the process by improving the efficiency of the scan and the quality of the images it produces.
Dr. Nirav Patel and Dr. Keyur Shah, are cofounders and co-Chiefs of Radiology at Whole Body MRI.
OntarioMD
umentation of patient encounters for physician review.
Based on the input of 30 physicians using the WELL AI Voice solution, the pilot revealed the potential for the AI application to reduce cognitive burdens and time spent on administrative documentation, saving an average of 3.4 minutes per patient encounter.
This time savings could be reallocated from administrative tasks to patient interactions. Pilot results indicated improved workflow efficiency and reduced administrative burden.
Doctors reported enhanced patient interactions due to less time spent on documentation and more time connecting with patients. Although these results are promising, the pilot’s small sample size might not fully represent all doctors’ perspectives and may contain biases. We need more extensive studies to validate the findings and identify and address risks before widespread AI scribe adoption.
The AI Scribe pilot identified legal and privacy considerations that need clarification with respect to accountability for
Currently, BioAro offers precision health clinics in Canada where they offer precision cardiology, precision nutrition, and precision skin along with a unique precision-based, multi-disciplinary, integrated approach to gut health.
This 12-week journey helps individuals understand the role lifestyle along with the role their gut microbiome plays in IBS, diabetes, and obesity. This innovative approach combines the expertise of registered dietitians, clinical psychologists, kinesiologists, and precision medicine using a comparative analysis of gut microbiome, and an interactive virtual education platform.
Over the next few years, precision medicine is expected to have a larger presence
personal and health information to comply with privacy laws such as PHIPA.
Key concerns included requirements regarding data retention, subcontractor responsibilities, and safeguarding (including encryption, and guardrails on secondary data use).
The pilot highlighted the need for clear roles and responsibilities for doctors, vendors, and AI developers, emphasizing the
Using an AI scribe solution, doctors reported enhanced interactions and less time spent on documentation.
importance of transparent agreements and consent processes. Streamlining these processes and enhancing patient consent procedures were important insights for efficiency and regulatory compliance in future implementations.
Looking forward: OntarioMD plays a leadership role in AI in primary care with our groundbreaking work to date. The Environmental Scan, along with the AI scribe pilot insights, lay a solid foundation for future AI initiatives.
As OntarioMD continues to innovate
in Canada. More specifically, they’ll be working in real-time, bringing virtual longevity worldwide and demonstrating access to people’s own health. People can live healthier, for longer by learning more about their DNA secrets, using tools such as whole genome sequencing, microbiome testing, telomere testing, DNA methylation as well as other testing strategies. This will
People can live healthier, for longer, by learning more about their DNA secrets with tools such as genome sequencing.
allow individuals to make the right decisions about their own health.
“It’s not merely a fleeting trend; rather, it symbolizes a significant shift towards prioritizing longevity and optimizing healthspan through precision and personalization. Our mission is substantial – to empower individuals to achieve enduring vitality and well-being,” she said.
and collaborate with partners to decrease doctors’ administrative load, we will continue to assess AI’s efficiency and ease of use for doctors. We are on the path to a better work-life balance for doctors. To get to the balance doctors require, it is important to thoroughly evaluate and continuously improve AI tools. AI can have the potential to enhance patient care and support the interaction between doctors and patients.
Abbas Zavar, MD, is Digital Health Research Lead, Partnerships and Stakeholders, at OntarioMD. Simon Ling is a digital health expert with over 18 years of leadership experience at both provincial and pan-Canadian levels. Currently serving as the Executive Director of Partnerships and Stakeholders at OntarioMD, he leads the advancement of partnerships and strategic alliances with industry and health system to address intricate challenges and deliver innovative solutions.
Disclaimer: This article is intended for informational purposes only and does not constitute professional advice. None of the products/services referenced herein are a substitute for medical judgment or an opinion on any issue.
CONTINUED FROM PAGE 20
CONTINUED FROM PAGE 16
CONTINUED FROM PAGE 21
www.canhealth.com MAY 2024 CANADIAN HEALTHCARE TECHNOLOGY 23
CONTINUED FROM PAGE 15